Abstract
In the current study, we used a sample of predominantly African-American women with high rates of trauma exposure (N = 434) to examine psychometric properties of the Personality Inventory for DSM-5-Brief Form (PID-5-BF). We compared model fit between a model with five correlated latent factors and a higher-order model in which the five latent factors were used to estimate a single “general pathology” factor. Additionally, we computed estimates of internal consistency and domain interrelations and examined indices of convergent/discriminant validity of the PID-5-BF domains by examining their relations to relevant criterion variables. The expected five-factor structure demonstrated good fit indices in a confirmatory factor analysis, and the more parsimonious, higher-order model was retained. Within this higher-order model, the first-order factors accounted for more variance in the criterion variables than the general pathology factor in most instances. The PID-5-BF domains were highly interrelated (rs = .38 to .66), and convergent/discriminant validity of the domains varied: Negative Affectivity and Detachment generally showed the hypothesized pattern of relations with external criteria, while Antagonism and Disinhibition displayed less consistent and discriminant relations. Results are discussed in terms of the costs and benefits of using brief pathological trait measures in samples characterized by high levels of psychopathology.
Section III of the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013a) introduced an Alternative Model of personality disorder (AMPD) diagnosis developed as a response to longstanding criticism of categorical personality disorder models (e.g., Widiger, 1993). The AMPD is a trait-based, quasi-dimensional nosology of personality pathology, wherein elevations in certain traits are used as diagnostic indicators, along with evidence of personality dysfunction. The Personality Inventory for DSM-5 (PID-5; Krueger, Derringer, Markon, Watson, & Skodol, 2012) is a 220-item self-report assessment measure that was developed and introduced to capture these 25 pathological traits.1 For example, a diagnosis of Narcissistic Personality Disorder would be appropriate for an individual who meet type-specific criteria, including elevated levels of the traits Grandiosity and Attention-Seeking, as well as moderate or greater impairment in pertinent areas of personality functioning such as impaired empathy (American Psychiatric Association, 2013b; Skodol, Morey, Bender, & Oldham, 2015). The PID-5 yields a five-factor solution, namely Negative Affectivity, Detachment, Antagonism, Disinhibition, and Psychoticism as well as 25 facets. Although the constituent traits have different names, the PID-5 is generally considered a pathological variant of the seminal Five-Factor Model (FFM; Costa & McCrae, 1992), and these models have similar relations to external criteria (e.g., Sleep, Hyatt, Lamkin, Maples-Keller, & Miller, 2018; Suzuki, Griffin, & Samuel, 2017).
Since its publication, there have been numerous investigations into the psychometric properties of the full version of the PID-5 (e.g., Anderson et al., 2015; Gore & Widiger, 2013; Quilty, Ayearst, Chmielewski, Pollock, & Bagby, 2013; Suzuki et al., 2018; Wright et al., 2012). A recent review concluded that the PID-5 demonstrates acceptable internal consistency, test-retest reliability, and that the majority of the factor analyses performed on the PID-5 have yielded a common five-factor structure (Al-Dajani, Gralnick, & Bagby, 2016). Although the psychometric properties of the PID-5 are generally good, albeit with some concerns about the relative lack of discriminant validity due to the highly related domains (Crego, Gore, Rojas, & Widiger, 2015), relatively few comparable efforts have been made for the Brief Form of the PID-5 (PID-5-BF), a 25-item abbreviated version of the full measure that uses five items to assess each of the five domains. The PID-5-BF was created, in part, to assist clinical intervention: in the clinician instruction section that accompanies the published version of this measure (American Psychiatric Association, 2013b), the PID-5-BF is to be used by clinicians to “think of the patient’s personality dysfunction relative to the observed norms,” and this measure can be administered repeatedly to “track change in severity of the individual’s personality dysfunction over time.”
Beyond its potential for clinical applications, the brevity of the PID-5-BF makes it an appealing option for researchers with limited time to devote to personality assessment. However, its psychometric properties are not as well-established as its longer counterparts. In support of the PID-5-BF, several studies have demonstrated that the PID-5 and the PID-5-BF exhibit very similar patterns of correlations with external criterion variables, such as DSM-IV personality disorders, depression, and externalizing psychopathology; moreover, the five-factor structure has also been replicated (e.g., Anderson, Sellbom, & Salekin, 2018; Bach, Maples-Keller, Bo, & Simonsen, 2016; Fossati, Krueger, Markon, Borroni, & Maffei, 2013). However, the PID-5-BF has shown poorer model fit to a five-factor solution than the full PID-5 (Bach et al., 2016). Furthermore, unlike its longer counterparts, the PID-5-BF is also not able to capture all 25 PID-5 facets (American Psychiatric Association, 2013b), which is a limitation given research suggesting facet-level data is better suited to capture nuanced variance in psychopathology than broad domain-level data (e.g., Samuel & Widiger, 2008).
The goal of the current investigation is to assess the psychometric properties of the PID-5-BF in a highly traumatized urban sample, predominantly composed of African-American women. Although this sample is relatively demographically homogenous in this respect, we believe there is much to gain from examining indices of validity and reliability for a measure in a wide range of samples to examine if it displays similar properties across populations. Across previous studies we reviewed on the PID-5, the highest percentage of the sample that identifies as African-American is 34% (Wright & Simms, 2014). However, this study used the full 220-item version of the PID-5; in studies on the PID-5-BF, the percentage of African-Americans in the sample was less than 10%, or in some cases, this information was not reported. In addition to consideration of race, it is important to investigate how the PID-5-BF functions in samples characterized by greater levels of psychopathology than undergraduate or community samples commonly used in personality research. From these perspectives, we believe that is paramount to understand the psychometric properties of the PID-5-BF in this population, given that this sample is unique in terms of racial composition as well as rates of psychopathology. Finally, we believe that the current study offers an insightful take on the effectiveness (c.f., efficacy) of this measure as it performs within the context of a large-scale research/clinical consortium. We believe that the setting where this research was conducted is an exemplar of the type of setting where PID-5 measures may be used (i.e., where data is gathered simultaneously for research purposes and to inform clinical intervention), and thus the current data are indicative of how this measure may perform in an ecologically valid setting. Moreover, we believe the abbreviated scale length of the PID-5-BF may be attractive to researchers in large, inter-disciplinary consortia, and we are able to examine how this measure functions in such a setting.
We conducted confirmatory factor analyses to examine the factor structure of the PID-5-BF, and present descriptive information about domain internal consistency and interrelations. Subsequently, we assess the convergent and discriminant validity of the PID-5-BF by assessing the degree to which the five pathological traits demonstrate specific relations with indices of psychopathology. These indices were chosen from a larger battery of self-report measures in order to test hypothesized relations regarding how certain traits would be related to different forms of psychopathology. Finally, we empirically compare the relations of the AMPD traits with the criteria by using multivariate regression analyses and Steiger’s z-tests.
Our hypotheses are based in previous research on the PID-5-BF, the longer versions of the PID-5, as well as findings from the relatively larger FFM literature. First, we hypothesized that Negative Affectivity and Detachment would exhibit large, positive relations to indices of internalizing psychopathology (e.g., anxiety, depression). Multiple meta-analyses have linked FFM traits Neuroticism and (low) Extraversion to this cluster of disorders (Kotov, Gamez, Schmidt, & Watson, 2010; Malouff, Thorsteinsson, & Schutte, 2005), and there is evidence to suggest that AMPD traits display similar relations to internalizing psychopathology as their FFM counterparts (Sleep, Hyatt, et al., 2018). Thus, we used self-reports of anxiety, depression, emotion dysregulation, and positive and negative emotionality as convergent and discriminant validity references for the PID-5-BF. Additionally, we use number of symptoms of Borderline Personality Disorder (BPD) as a criterion variable, given recent evidence that it is a characterized largely by negative emotionality (e.g., Distel et al., 2009; Miller et al., 2010; Saulsman & Page, 2004).
Similarly, we hypothesized that Antagonism and Disinhibition would exhibit moderate to large, positive relations to indices of externalizing psychopathology and related constructs, including aggression, anger and sensation-seeking, lifetime alcohol use, and lifetime drug use. The FFM counterparts of these AMPD traits (i.e., low Agreeableness, low Conscientiousness) are the most robust self-report predictors of this cluster of psychopathology (Jones, Miller, & Lynam, 2011), and these AMPD traits have shown these hypothesized relations in an undergraduate sample (Sleep, Hyatt, et al., 2018). Of note, in the recently developed Hierarchical Taxonomy of Psychopathology (HiTOP; Kotov et al., 2017) Antagonism is thought to be more strongly related to disorders of externalizing psychopathology, such as Antisocial Personality Disorder, while Disinhibition is thought to be more closely linked to Substance Use Disorders. As such, we hypothesize that Antagonism and Disinhibition will be more strongly related to aggression and substance use, respectively. Finally, we hypothesized that Psychoticism, a dimensional index of proclivity toward unusual experiences and poor reality testing, would show a moderate to large, positive relation to self-reported dissociative symptoms, which have been meta-analytically linked to extreme manifestations of psychosis, such as psychotic disorders (O’Driscoll, Laing, & Mason, 2014).
Methods
Participants and procedure
Participants were drawn from an ongoing study investigating civilian trauma in a low socioeconomic status, primarily African American, urban population. The 434 participants in this study (mean age = 40.59, SD = 12.37) were women (100%) and primarily African-American (98.8%). In this sample, 19.2% of participants completed less than 12 years of education, 35.6% of participants completed high school or obtained a GED, 25.5% of participants completed some college, and 19.7% of participants obtained a post-secondary degree. In terms of household monthly income, 19.9% of participants reported less than $500 per month, 59.7% reported between $1000 and $1999 per month, and 20.4% reported $2000 or more per month.
Participant recruitment occurred in waiting rooms in the gynecology and primary care medical (non-psychiatric) clinics at Grady Memorial Hospital, a publicly funded hospital in Atlanta, Georgia. Eligibility criteria included being at least 18 years old, not actively psychotic, and able to give informed consent. If interested, participants completed informed consent approved by the Emory University Institutional Review Board (IRB#: 00–104519), and an interview was administered with questionnaires regarding trauma history and other, relevant psychological variables, which took 45–75 minutes to complete. Additionally, participants came in for a separate research visit where they completed additional self-report questionnaires and a semi-structured interview. 37.9% of the current sample met criteria for current Post-Traumatic Stress Disorder (PTSD), 24.7% met for current Major Depressive Disorder (MDD), 62.6% met criteria for a lifetime diagnosis of PTSD, and 53.4% met criteria for lifetime MDD2 (American Psychiatric Association, 2013a). Additionally, 91.8% of participants reported experiencing at least one Criterion A3 trauma in adulthood, with 25.9% reporting experiencing or witnessing five or more different types of trauma (e.g., violent assault by romantic partner) in adulthood. Of note, we did not base recruitment on rates of traumatization, and the rates of trauma are similar to those observed in comparable samples (e.g., Goldmann et al., 2011). For the completion of these self-report measures, participants were read each item by a trained research assistant, and asked to respond to a set of measure-specific response options presented on a laminated sheet of paper. Participants were financially compensated for their time. All graduate and undergraduate research assistants were thoroughly trained in the administration of questionnaires, with an average of 1–2 months of supervised training and shadowing (see Gillespie et al., 2009 for more details on study procedure).
Materials
PID-5-BF
The PID-5-BF (American Psychiatric Association, 2013b) is a 25-item self-report measure of pathological personality traits included in the DSM-5 AMPD. The only PID-5 items collected were from this brief form.
Beck Depression Inventory-II
The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) is a 21 item self-report measure of depressive symptoms. We used the total score in the current study (α = .93).
Anxiety Sensitivity Inventory
The Anxiety Sensitivity Inventory (ASI; Peterson & Reiss, 1992) is a 16-item self-report inventory of sensitivity to symptoms of anxiety. In the current study, the total score was used (α= .88).
Borderline personality disorder semi-structured interview
Semi-structured interviewing was conducted to assess for symptoms of BPD based on the Structured Clinical Interview for DSM-IV (e.g., First & Gibbon, 2004). Participants received a symptom score (i.e., 1 = no evidence of symptom, 2 = sub-threshold, 3 = symptom present) based on the extent to which they were able to provide examples of each symptom from on their personal experiences. The total score was used in the current study (α= .85), and data were available for N = 343 participants.
Difficulties in Emotion Regulation Scale
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report measure of emotional dysregulation. The total score was used in the current study (α= .82).
Positive and Negative Affect Schedule
The Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) is a 20-item self-report measure of positive and negative emotionality. In the current study, participants were instructed to report on the degree to which they generally feel a given emotion, as opposed to the extent to which they currently feel it. Scores were derived for both general positive affect (α = .83) and negative affect (α= .89).
Alcohol Use Disorders Identification Test
The Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, Fuente, & Grant, 1993) is an 18-item self-report measure of past-year and lifetime alcohol use and associated social repercussions related to alcohol use. The total score for lifetime alcohol use was used in the current study. A score of 8 or more is indicative of hazardous drinking, and 32.3% of the current sample met this threshold.
Drug Abuse Screening Test
The Drug Abuse Screening Test (DAST; Skinner, 1982) is a 20-item self-report measure of illicit drug use in the past year and lifetime. The total score for lifetime drug use was used in the current study. A score of 6 or more is indicative of elevated likelihood of a substance use disorder, and 10.3% of the current sample met this threshold.
Anger and Sensation Seeking Scale
The Anger and Sensation Seeking Scale (AASS) is a 5-item self-report measure of frequency/intensity of anger and tendency to engage in sensation-seeking behaviors (α = .65).
Behavior Questionnaire
The Behavior Questionnaire (BQ) is a 10-item self-report measure of history of engaging in a range of aggressive behaviors (e.g., pushing/shoving, stabbing, shooting; α = .72). The measure was created using the Conflicts Tactics Scale, a commonly used measurement of conflict behaviors (Straus, Hamby, Boney-McCoy, & Sugarman, 1996) and in consultation with researchers specializing in the identification of deviant and aggressive behaviors. Items from the BQ ask participants how often they have perpetrated a particular aggressive act and participants answered using a graded response to each question of “never,” “once,” “several times,” “many times,” or “more times than I can count” (Gillikin et al., 2016).
Multiscale Dissociation Inventory
The Multiscale Dissociation Inventory (MDI; Brière, 2002) is a 30-item self-report measure of recent dissociative symptoms. Participants were instructed to report on symptoms they had experienced in the past month, and the total score was used in the current study (α= .95).
Analyses
Confirmatory Factor Analyses (CFAs) were conducted using Mplus (Muthén & Muthén, 2012). Consistent with previous work on the PID-5, all models were estimated from a polychoric correlation matrix. Model parameters were generated with a diagonally weighted least squares estimator with robust standard errors and a mean and variance adjusted test statistic (i.e., estimator = “WLSMV”). Latent variables were standardized to allow all item loadings to vary freely. Model fit was evaluated using root mean square error of approximation (RMSEA; Browne & Cudeck, 1993) and comparative fit index (CFI; Bentler, 1990). Along with modeling five correlated latent factors (i.e., Negative Affectivity, Detachment, Antagonism, Disinhibition, Psychoticism), a higher-order model, in which the five latent factors are used to estimate a single “general pathology” factor was evaluated. A chi-square difference test for nested models (i.e., “DIFFTEST,” Asparouhov & Muthén, 2010) was used in Mplus (Muthén & Muthén, 2012) to compare model fit. Additionally, we evaluated whether the first-order factors have incremental utility in predicting the criterion variables over the general factor within the higher-order model by comparing R2 values at these two levels of the model.
Next, internal consistency estimates of the PID-5-BF domains were calculated using Cronbach’s alpha, McDonald’s omega, and mean inter-item correlations (mIIC), and domain interrelations are presented as Pearson’s r values. We then widened the nomological networks of the PID-5 domains by examining their relations with the aforementioned criterion variables. Finally, we used two strategies to examine the uniqueness of the relations between the PID-5 domains and the criterion variables. We used multivariate regression analyses in which all five PID-5 domains enter the model simultaneously as predictors of a given criterion variable. Lastly, Steiger’s z-tests were conducted to examine if there were statistically significant differences between hypothesized relations; in other words, these tests were used to determine if one domain displayed a significantly stronger relation to a criterion variable than did another domain at a threshold of p < .01 (Lee & Preacher, 2013).
Results
Factor analyses
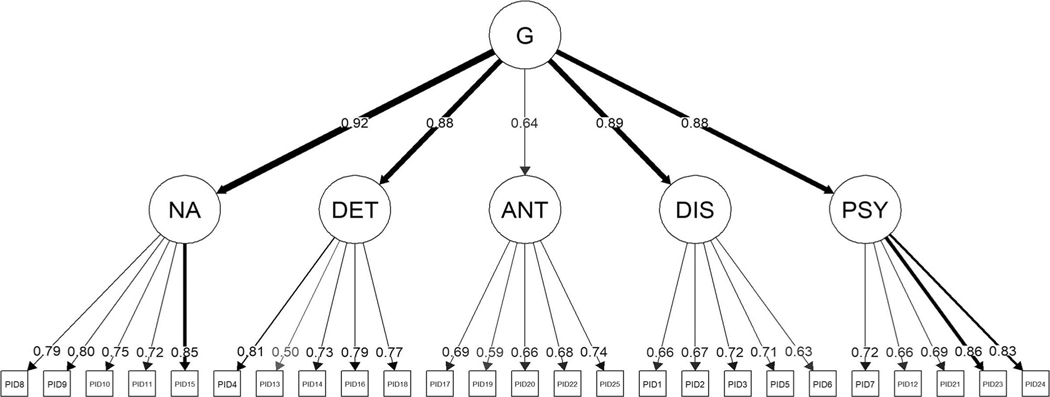
The CFA of the theorized five-factor model yielded acceptable model fit (χ2(265) = 617.24, p = .000; CFI = .954; RMSEA [90% CI] = .056 [.050 – .062]) suggesting it adequately accounts for the data (see Table 1 and Figure 1 for factor loadings). Latent variable correlations ranged from r = .54 (Antagonism and Negative Affect) to r = .83 (Negative Affect and Disinhibition). The higher-order model, which incorporates a second-order “general pathology” factor also revealed acceptable fit (χ2(270) = 613.75, p = .000; CFI = .955; RMSEA [90% CI] = .055 [.049 – .061]). A chi-square difference test for nested models (Asparouhov & Muthén, 2010) revealed no significant difference between the correlated-factors and higher-order models (χ2(5) = 7.3, p = .199). As such, the more parsimonious higher-order model should be retained.
Table 1.
Item loadings and factor intercorrelations for the CFA five-factor solution.
| 1. Negative Affectivity | 2. Detachment | 3. Antagonism | 4. Disinhibition | 5. Psychoticism | |||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||
| # | λ | # | λ | # | λ | # | λ | # | λ |
|
| |||||||||
| 8. | 0.794 | 4. | 0.807 | 17. | 0.691 | 1. | 0.662 | 7. | 0.720 |
| 9. | 0.796 | 13. | 0.505 | 19. | 0.592 | 2. | 0.672 | 12. | 0.656 |
| 10. | 0.751 | 14. | 0.731 | 20. | 0.660 | 3. | 0.717 | 21. | 0.694 |
| 11. | 0.723 | 16. | 0.788 | 22. | 0.680 | 5. | 0.708 | 23. | 0.861 |
| 15. | 0.851 | 18. | 0.774 | 25. | 0.737 | 6. | 0.632 | 24. | 0.830 |
|
r 2. |
.82 | ||||||||
| 3. | .54 | .56 | |||||||
| 4. | .83 | .77 | .64 | ||||||
| 5. | .82 | .78 | .59 | .77 | |||||
Note: # column indicates PID-5-BF item number; λ column indicates item loading. Values below the dashed line indicate the correlation of the latent variables.
Figure 1.
Higher-order factor model.
Note. G = general factor; NA = negative affectivity; DET = detachment; ANT = antagonism; DIS = disinhibition; PSY = psychoticism. Line thickness is determined by loading weight. Figure generated within R using the ‘semPlot’ package (Epskamp, 2015).
Internal consistency and domain interrelations
Estimates of internal consistency ranged among the PID-5-BF domains, with relatively strong estimates for Negative Affectivity, Detachment, and Psychoticism, and relatively weak estimates for Antagonism (Table 2). The PID-5-BF domains displayed interrelations that varied from medium-to-large in magnitude (mean r = .52, median r = .57), and all interrelations showed positive directionality as expected.
Table 2.
PID-5 domain internal consistency indices and bivariate relations.
| Domain | 1. | 2. | 3. | 4. | 5. | α | ω | mIIC |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1. Negative Affectivity | - | - | - | - | - | .83 | .83 | .49 |
| 2. Detachment | .64 | - | - | - | - | .76 | .77 | .40 |
| 3. Antagonism | .38 | .38 | - | - | - | .58 | .59 | .23 |
| 4. Disinhibition | .61 | .56 | .41 | - | - | .70 | .70 | .32 |
| 5. Psychoticism | .66 | .62 | .40 | .57 | - | .77 | .78 | .41 |
| 6. Age | −.05 | −.02 | −.05 | −.01 | −.03 | - | - | - |
| 7. Education | −.17 | −.17 | −.05 | −.15 | −.14 | - | - | - |
| 8. Income | −.17 | −.13 | −.06 | −.08 | −.08 | - | - | - |
Note. mIIC = Mean Inter-item Correlation Coefficient; bivariate relations presented here are between the scale scores and not the latent domain variables.
The smallest interrelation was found between Antagonism and both Negative Affectivity and Detachment (rs = .38), and the largest interrelation was found between Negative Affectivity and Psychoticism (r = .66).
Convergent and discriminant relations
The Negative Affectivity and Detachment domains displayed large, positive relations with indices of internalizing psychopathology, including depression, anxiety, and emotional dysregulation (Table 3). Negative Affectivity explained the largest share of variance in the multivariate regression models predicting these outcomes, but Steiger’s z-tests suggest these bivariate relations are not statistically significantly different from one another (see Supplemental Table 2 for full information regarding outcomes of Steiger’s z-tests). Negative Affectivity and Detachment also displayed comparably large, positive relations with anger and sensation seeking, as well as recent experiences of dissociation. All PID-5 domains were correlated above r = .25 with symptoms of BPD, but Steiger’s z-tests suggest that Negative Affectivity was the strongest correlate. Of note, the AMPD criteria for BPD include facets from the domains Negative Affectivity (4/7), Disinhibition (2/7), and Antagonism (1/7), so these relations are consistent with this description, but the relations with Detachment and Psychoticism are not predicted by the AMPD description. Similarly, multivariate regression analyses suggest that Negative Affectivity explained the largest portion of variance in BPD symptoms, and Steiger’s z-tests suggest this domain displayed statistically significantly larger relations with BPD symptoms than the other PID-5 domains.
Table 3.
PID-5 domain relations with psychopathological indices.
| Criteria | Negative Affectivity r (β) | Detachmentr (β) | Antagonism r (β) | Disinhibition r (β) | Psychoticism r (β) | Model R2 |
|---|---|---|---|---|---|---|
| BDI | .64 (.42) | .56 (.22) | .22 (−.09) | .46 (.05) | .52 (.12) | .46 |
| ASI | .51 (.29) | .44 (.12) | .16 (−.11) | .42 (.12) | .46 (.18) | .31 |
| BPD Sx | .49 (.33) | .38 (.07) | .25 (.04) | .36 (.06) | .40 (.10) | .26 |
| DERS | .69 (.33) | .64 (.24) | .35 (−.02) | .58 (.16) | .63 (.18) | .58 |
| PANAS PA | −.48 (−.38) | −.48 (−.35) | −.13 (.09) | −.26 (.11) | −.33 (.03) | .30 |
| PANAS NA | .62 (.45) | .53 (.21) | .19 (−.10) | .45 (.09) | .45 (.01) | .41 |
| AUDIT | .27 (.12) | .20 (−.04) | .10 (−.04) | .30 (.22) | .26 (.10) | .11 |
| DAST | .24 (.13) | .15 (−.11) | .11 (−.04) | .28 (.25) | .19 (.05) | .09 |
| AASS | .53 (.44) | .45 (.17) | .27 (.07) | .39 (.02) | .36 (−.09) | .31 |
| BQ | .21 (−.03) | .26 (.13) | .20 (.07) | .28 (.18) | .23 (.05) | .10 |
| MDI | .63 (.21) | .59 (.16) | .25 (−.11) | .52 (.07) | .72 (.48) | .48 |
Note. Pearson’s r values ≥ .50 are bolded; β values represent standardized beta values when all five PID-5 traits are entered in a multivariate regression model simultaneously; BDI = Beck Depression Inventory; ASI = Anxiety Sensitivity Inventory; BPD Sx = composite of number and severity of Borderline Personality Disorder symptoms; DERS = Difficulty in Emotion Regulation Scale; PANAS PA = Positive and Negative Affect Schedule Positive Affect; PANAS NA = Positive and Negative Affect Schedule Negative Affect; AUDIT = Alcohol Use Disorders Identification Test; DAST = Drug Abuse Screening Test; AASS = Anger and Sensation-Seeking Scale; BQ = Behavior Questionnaire; MDI = Multiscale Dissociation Inventory.
Disinhibition displayed large, positive relations to emotion dysregulation and recent dissociation, as well as the medium-to-large relations to depression, anxiety, and anger and sensation-seeking. Contrary to hypotheses, neither Disinhibition nor Antagonism displayed large relations to indices of externalizing psychopathology. The relations between Disinhibition and Antagonism and aggression, alcohol use, and drug use were positive, but generally small-tomedium in magnitude, and relations of similar magnitude were observed for all five PID-5 domains. Multivariate regression analyses suggest that Disinhibition explained the largest share of variance in the externalizing criteria, except anger and sensation-seeking, where Negative Affectivity accounted for the largest portion of variance. Consistent with hypotheses, Disinhibition was a stronger correlate of alcohol and drug use than Antagonism, but these domains displayed comparably large relations to aggression. As hypothesized, Psychoticism demonstrated a large, positive relation with recent dissociation; this domain predicted the largest portion of variance in the multivariate regression analyses, and Steiger’s z-tests suggest that it is a statistically significantly stronger correlate of this criteria than the other PID-5 domains. Additionally, Psychoticism showed large, positive relations to depression and emotion dysregulation.
Incremental value of first-order factors
In order to evaluate whether the first-order factors (FOF) have incremental utility over the general factor (G) within the higher-order model, the two levels of the model were used to predict each of the criterion variables and R2 values were compared (see Table 4).4 The first-order factors accounted for more variance in 10 of the 11 criterion variables. Only emotion dysregulation was better predicted by the second-order factor (R2G = .630; R2FOF = .619). The second-order factor predicted all criterion variables with associations ranging from β = .204 (AUDIT) to β = .794 (DERS). At the first-order level, negative affectivity and detachment had unique contributions to the prediction of BDI (βNA = .632; βDET = .294) and PANAS PA (βNA = −.521; βDET = .294). Negative affectivity and antagonism had independent associations with PANAS NA (βNA = .736; βANT = −.243). Negative affectivity was the only unique predictor of BPD symptoms (β = .556), DERS (β = .405), and AASS (β = .668). Detachment had a unique negative association with the AUDIT (β = −.412). Disinhibition was uniquely associated with the DAST (β = .448), and negative affectivity (β= .380), antagonism (β= −.258), and psychoticism (β = .599) were independently associated with the MDI. There were no significant predictors of the ASI or the BQ at the first-order level.
Table 4.
Incremental value of factors estimated in higher-order model.
| Criteria | Gβ | r 2 | NAβ | DETβ | ANTβ | DISβ | PSYβ | R 2 | ΔR2 |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| BDI | .665* | .442 | .632* | .294* | −.207 | −.186 | .103 | .511 | .069 |
| ASI | .571* | .326 | .306 | .025 | −.180 | .178 | .229 | .351 | .025 |
| BPD Sx | .521* | .271 | .556* | .103 | −.054 | −.095 | .021 | .304 | .033 |
| DERS | .794* | .630 | .405* | .207 | −.107 | .104 | .198 | .619 | −.011 |
| PANAS PA | −.498* | .248 | −.521* | −.559* | .151 | .382 | .072 | .370 | .122 |
| PANAS NA | .632* | .399 | .736* | .245 | −.243* | −.020 | −.131 | .497 | .098 |
| AUDIT | .204* | .042 | .387 | −.412* | −.038 | .240 | .018 | .111 | .069 |
| DAST | .275* | .075 | −.171 | −.055 | .068 | .448* | .019 | .113 | .038 |
| AASS | .532* | .283 | .668* | .186 | .020 | −.094 | −.229 | .340 | .057 |
| BQ | .342* | .117 | −.198 | .174 | .081 | .366 | −.035 | .148 | .031 |
| MDI | .711* | .505 | .380* | .159 | −.259* | −.199 | .599* | .602 | .097 |
Note. PID-5 factors were estimated within a higher-order model. BDI = Beck Depression Inventory; ASI = Anxiety Sensitivity Inventory; BPD Sx = composite of number and severity of Borderline Personality Disorder symptoms; DERS = Difficulty in Emotion Regulation Scale; PANAS PA = Positive and Negative Affect Schedule Positive Affect; PANAS NA = Positive and Negative Affect Schedule Negative Affect; AUDIT = Alcohol Use Disorders Identification Test; DAST = Drug Abuse Screening Test; AASS = Anger and Sensation-Seeking Scale; BQ = Behavior Questionnaire; MDI = Multiscale Dissociation Inventory.
p < .01.
Discussion
The recent publication of the AMPD was accompanied by the development of several personality measures to capture the pathological traits included in this new dimensional model. In the current study, we examined the psychometric properties of the shortest measure of the AMPD traits to date, the PID-5-BF, in a sample predominantly composed of African-American women with high rates of trauma exposure. In doing so, we examined how this measure functions in an understudied sample that is characterized by more trauma and psychopathology than undergraduate or community samples common in personality research. Moreover, given that this research was conducted in a setting that uses data collection for research purposes and to inform clinical intervention, we believe the current data speak to the effectiveness of this measure in an ecologically valid setting.
Factor structure
Previous evaluations of the PID-5 factor structure have been generally limited to Exploratory Factor Analyses (Bach et al., 2016; Gore & Widiger, 2013; Wright et al., 2012) as the assumption of simple structure is often unrealistic for personality domain scales (Hopwood & Donnellan, 2010). One previous CFA on the full (i.e., 220-item) PID-5 found marginally acceptable fit in a large community sample for a correlated five-factor solution (Fossati et al., 2013), and acceptable fit of a correlated five-factor solution as measured by the PID-5-BF has also been demonstrated in undergraduate and community samples (Anderson et al., 2018). In the present analysis, the five-factor model demonstrated good fit as both the RMSEA and CFI met the minimal fit recommendations of Hu and Bentler (1999). A higher-order model incorporating a second-order factor accounting for the covariance between all five subordinate PID-5 factors was also considered. This model is consistent with findings from the literature on psychiatric quantitative nosology that support the existence of a latent general factor of psychopathology that is meaningfully related to all manifestations of psychopathology (Lahey et al., 2012; Snyder, Young, & Hankin, 2017; Tackett et al., 2013). Widiger and Oltmanns (2017) postulated that similar to the general factor of psychopathology, a general factor of (pathological) personality may represent “nonspecific impairment or dysfunction, irrespective of the etiology or basis for this impairment” (p. 183). Consistent with this hypothesis, the present findings suggest that a single higher-order factor highly associated with Negative Affectivity, Detachment, Disinhibition, and Psychoticism can effectively account for the covariance between the PID-5-BF factors. It is therefore sensible to interpret the core element captured by each of these putatively distinct domains as distress and/or maladaptivity. That said, the five lower-order factors retained predictive utility over a single general factor, and thus the unique contributions of each of the lower-order factors should not be disregarded.
Internal consistency and validity
Overall, the other psychometric properties of the PID-5-BF scales were acceptable, but this varied across domains. In terms of internal consistency, alpha, omega, and mean inter-item correlation estimates for the AMPD traits were good, especially considering the brevity of the measure (i.e., 5 items per trait), with the exception of Antagonism, which showed relatively lower internal consistency estimates. The convergent validity of traits Negative Affectivity and Detachment was good, as these traits demonstrated large, positive relations with indices of internalizing psychopathology (e.g., depression), consistent with hypotheses and with previous findings in undergraduate and community samples (Anderson et al., 2018). Antagonism and Disinhibition did exhibit the hypothesized convergent relations with indices of externalizing psychopathology (e.g., substance use, aggressive behavior), but these effect sizes were notably smaller than those found for internalizing psychopathology (i.e., none of the PID-5-BF domain relations with aggression/antisocial behavior, alcohol use, or drug use reached an effect size above r = .30). This diverges from previous findings in undergraduates suggesting that these traits are large correlates of an externalizing psychopathology composite (Anderson et al., 2018). This issue did not appear to be related to a severe restriction of range issue, as evidenced by the rates for history of problematic substance use and antisocial behavior (e.g., 87% of participants reported a lifetime history of at least one instance of aggression or violence). However, it is noteworthy that overall, the rates of externalizing psychopathology were lower than that of internalizing psychopathology (e.g., lifetime substance us disorder = 10.3% vs. lifetime MDD = 53.4%), and thus, the AMPD traits may perform differently in a sample characterized by higher rates of externalizing psychopathology. Moreover, Disinhibition and Antagonism had the lowest internal consistencies of the five factors, and Antagonism revealed particularly weak factor loadings as a result. The current results suggest that in this population, the PID-5-BF offers somewhat weaker estimates of domains associated with problematic externalizing behaviors; further exploration of the performance of these items in samples such as these is needed.
Although the AMPD traits generally demonstrated good convergent validity, discriminant validity was more limited in this sample. For example, four of the five AMPD traits (i.e., not Antagonism) demonstrated medium-to-large, positive relations with indices of anxiety, depression, and dissociative symptoms, which contrasts with previous work where relations to internalizing psychopathology were more specific to Negative Affectivity, although positive relations were observed for all PID-5-BF domains here as well (Anderson et al., 2018). This general lack of divergence, which has been a concern for the longer versions of the PID-5 (Crego & Widiger, 2016), is consistent with the present finding that a general factor can reasonably account for the covariance between domains. Indeed, four of the five PID-5-BF traits were correlated with emotion dysregulation at r ≥ .60, which is central to many manifestations of psychopathology (Sheppes, Suri, & Gross, 2015). This suggests that each PID-5-BF domain is, to some degree, capturing distress and/or impairment related to emotional dysregulation.
Although the multivariate regression analyses allow a glimpse into the unique relations that each domain has with the criterion variables once its shared variance with the other traits is removed, the high interrelations between the traits make it difficult to know what a trait represents once it has been statistically altered in this way. For example, when you control for the variance that Negative Affectivity shares with Psychoticism in the current data, almost 44% of the variance is removed, making the interpretation of these partialed variables problematic (e.g., Lynam, Hoyle, & Newman, 2006; Sleep, Lynam, Hyatt, & Miller, 2017). More importantly, there is no established way to use such partialed scores in an actual clinical setting, thus making these kinds of examinations far more relevant to research-based questions than applied, clinical questions (e.g., treatment planning). In sum, although there is little doubt that the AMPD traits as measured by the PID-5-BF are broadly related to symptoms of psychopathology, the degree to which the AMPD traits are able to differentially capture distinct forms of psychopathology in the hypothesized fashion appears more limited in this type of sample.
Limitations
With the exception of a semi-structured interview for BPD symptoms, the majority of the measures examined herein were self-report. Since the AMPD and the associated measures were developed to be able to be used by both researchers and clinicians alike, we believe that examining these traits with reference to clinical indices of psychological functioning (e.g., clinician-rated symptomatology, response to treatment, relapse rate) would be immensely valuable. Additionally, we believe that it is especially important to investigate how AMPD traits relate to variables measured by other common research methodologies (e.g., behavioral task), given the potential for shared method variance to partially account for the current results. Furthermore, the unique method of self-report (i.e., providing verbal responses to orally presented item prompts) is discrepant from the more traditional “paper and pencil” or electronic method of self-report that is typically employed in personality research, and this must be noted as a consideration in interpreting the current data. Given the low levels of education in the current sample and the general dearth of research on how pathological trait measures function in demographically similar samples, we believe this alternative method of administration is justified in order to maximize the generalizability and accuracy of the findings.
Relatedly, our analyses are limited in their ability to speak to the similarities and differences that the AMPD traits display in unexamined criteria. In other words, there may be important differences in the pattern of relations that the AMPD traits show to a psychophysiological index or treatment outcome, but our data cannot speak to this directly. However, given the high AMPD trait interrelations reported herein, the principle of parsimony would not suggest that these traits, as measured, have vastly disparate nomological networks. We believe that longer measures of the AMPD traits, while somewhat more onerous on participants, may demonstrate improved indices of validity. Of course, this is an unanswered empirical question, and a distinction must be made between model and measure: research on the degree to which AMPD traits measured by longer, more robust assessments display differential relations to external criteria is nascent, and more work is needed to enrich the nomological networks underlying these traits as captured by different measures.
Finally, the generalizability of our findings is also limited by our sample, which was largely low-income, African-American women with high rates of trauma exposure. However, we believe the benefits of examining personality and psychopathology in this population outweigh the limitations in two main respects. First, this specific population is generally understudied, despite evidence indicating significantly higher rates of trauma than that of the general population (e.g., Gillespie et al., 2009). Second, we believe that social science research has long over-relied on demographically homogenous samples (e.g., WEIRD samples; Henrich, Heine, & Norenzayan, 2010), such as predominantly white, wealthy undergraduates, and thus we view the use of a sample composed of individuals with minority ethnicity status and low socioeconomic background as a major strength, not a demerit.
Conclusions and future directions
In sum, the current results suggest that in populations characterized by elevated levels of psychopathology, the PID-5-BF displays somewhat mixed psychometric properties across a range of examined indices. We believe clinicians should interpret the results of the PID-5-BF with caution, given the very large overlap in the nomological networks of these traits. While it may be useful as a screening measure, an elevation in one of the PID-5 domains as measured by the PID-5-BF may not provide unique information about a client’s propensity to experience a particular form of symptomatology. Moreover, given the lack of discriminant validity among the PID-5 domains as measured by the PID-5-BF, this measure alone may not be optimally suited to assist in specific treatment planning, unlike longer, more well-validated clinical instruments (e.g., NEO PI-R, Costa & McCrae, 1992; Sanderson & Clarkin, 2002; MMPI-II RF, Butcher, 1990; Tellegen & Ben-Porath, 2011). Longer, more robust measures of the AMPD traits (e.g., 100 item version; Maples et al., 2015) may prove much more useful in treatment planning, especially since they are able to capture facets as well as domains. As multiple lines of evidence converge that personality and psychopathology are inextricably linked across multiple levels of analysis (e.g., DeYoung & Krueger, 2018; Hyatt et al., 2019; Wright & Simms, 2016), we encourage researchers to carefully consider the measures of personality they include, bearing in mind the strengths and limitations that accompany each assessment.
Supplementary Material
Footnotes
Of note, an abbreviated 100-item measure has also been developed (Maples et al., 2015).
These diagnostic rates are based on structured clinical interviews using the Clinician-Administered PTSD Scale for DSM-5 (Weathers et al., 2015) and the Mini International Neuropsychiatric Interview for Major Depressive Disorder (American Psychiatric Association, 2013a, 2013b).
Note: Criterion A for a diagnosis of PTSD (i.e., traumatic experience; see DSM-5, American Psychiatric Association, 2013a, 2013b) should not be confused with Criterion A for a diagnosis of a personality disorder under the AMPD model.
The models could not be compared in a step-wise fashion, as predicting the criterion variables from all latent variables (i.e., the first- and second-order factors) simultaneously resulted in an under-identified model. As such, two models were run for each of the 11 criterion variables. One higher-order model in which the general factor was used to predict the criterion, then a second higher-order model in which the five first-order factors were used to predict the criterion. Given the high number of tests, a p-value of .01 was used for these analyses.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the contents of this report do not represent the views of the Department of Veterans Affairs or the United States Government.
Supplemental data for this article is available online at https://doi.org/10.1080/00223891.2020.1713138.
References
- Al-Dajani N, Gralnick TM, & Bagby RM (2016). A psychometric review of the Personality Inventory for DSM–5 (PID–5): Current status and future directions. Journal of Personality Assessment, 98(1), 62–81. doi: 10.1080/00223891.2015.1107572. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association. (2013b). The Personality Inventory for DSM–5—Brief Form (PID-5-BF)—Adult. Retrieved from http://www.psychiatry.org/practice/dsm/dsm5/online-assessment-measures#Personality
- Anderson JL, Sellbom M, Ayearst L, Quilty LC, Chmielewski M, & Bagby RM (2015). Associations between DSM-5 Section III personality traits and the Minnesota Multiphasic Personality Inventory 2-Restructured Form (MMPI-2-RF) scales in a psychiatric patient sample. Psychological Assessment, 27(3), 801–815. doi: 10.1037/pas0000096 [DOI] [PubMed] [Google Scholar]
- Anderson JL, Sellbom M, & Salekin RT (2018). Utility of the Personality Inventory for DSM-5–Brief Form (PID-5-BF) in the measurement of maladaptive personality and psychopathology. Assessment, 25(5), 596–607. [DOI] [PubMed] [Google Scholar]
- Asparouhov T, & Muthén B. (2010). Simple second-order chi-square correction (pp. 1–8, Technical Report). Los Angeles, CA: Muthén and Muthén. [Google Scholar]
- Bach B, Maples-Keller JL, Bo S, & Simonsen E. (2016). The alternative DSM–5 personality disorder traits criterion: A comparative examination of three self-report forms in a Danish population. Personality Disorders: Theory, Research, and Treatment, 7(2), 124–136. doi: 10.1037/per0000162 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78, 490–498. [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. [DOI] [PubMed] [Google Scholar]
- Briére J. (2002). MDI, Multiscale dissociation inventory: Professional manual. Odessa, FL: Psychological Assessment Resources, Incorporated. [Google Scholar]
- Browne MW, & Cudeck R. (1993). Alternative ways of assessing model fit. Sage Focus Editions, 154, 136–136. [Google Scholar]
- Butcher JN (1990). The MMPI-2 in psychological treatment. New York, NY: Oxford University Press. [Google Scholar]
- Costa PT, & McCrae R. (1992). Revised NEO Personality Inventory (NEO-PI-R) and NEO five factor model (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Center. [Google Scholar]
- Crego C, Gore WL, Rojas SL, & Widiger TA (2015). The discriminant (and convergent) validity of the Personality Inventory for DSM–5. Personality Disorders: Theory, Research, and Treatment, 6(4), 321–335. doi: 10.1037/per0000118 [DOI] [PubMed] [Google Scholar]
- Crego C, & Widiger TA (2016). Convergent and discriminant validity of alternative measures of maladaptive personality traits. Psychological Assessment, 28, 1561–1575. [DOI] [PubMed] [Google Scholar]
- DeYoung CG, & Krueger RF (2018). A cybernetic theory of psychopathology. Psychological Inquiry, 29(3), 117–138. doi: 10.1080/1047840X.2018.1513680 [DOI] [Google Scholar]
- Distel MA, Trull TJ, Willemsen G, Vink JM, Derom CA, Lynskey M, … Boomsma DI (2009). The five-factor model of personality and borderline personality disorder: A genetic analysis of comorbidity. Biological Psychiatry, 66(12), 1131–1138. doi: 10.1016/j.biopsych.2009.07.017 [DOI] [PubMed] [Google Scholar]
- Eid M, Geiser C, Koch T, & Heene M. (2017). Anomalous results in g-factor models: Explanations and alternatives. Psychological Methods, 22(3), 541–562. doi: 10.1037/met0000083 [DOI] [PubMed] [Google Scholar]
- Epskamp S. (2015). semPlot: Unified visualizations of structural equation models. Structural Equation Modeling: A Multidisciplinary Journal, 22(3), 474–483. doi: 10.1080/10705511.2014.937847 [DOI] [Google Scholar]
- First MB, & Gibbon M. (2004). The Structured Clinical Interview for DSM-IV axis I disorders (SCID-I) and the Structured Clinical Interview for DSM-IV axis II disorders (SCID-II). In Hilsenroth MJ & Segal DL (Eds.), Comprehensive handbook of psychological assessment, Vol. 2. Personality assessment (pp. 134–143). Hoboken, NJ: John Wiley & Sons Inc. [Google Scholar]
- Fossati A, Krueger RF, Markon KE, Borroni S, & Maffei C. (2013). Reliability and validity of the Personality Inventory for DSM-5 (PID-5) predicting DSM-IV personality disorders and psychopathy in community-dwelling Italian adults. Assessment, 20(6), 689–708. [DOI] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, … Ressler KJ (2009). Trauma exposure and stressrelated disorders in inner city primary care patients. General Hospital Psychiatry, 31(6), 505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillikin C, Habib L, Evces M, Bradley B, Ressler KJ, & Sanders J. (2016). Trauma exposure and PTSD symptoms associate with violence in inner city civilians. Journal of Psychiatric Research, 83, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E, Aiello A, Uddin M, Delva J, Koenen K, Gant LM, & Galea S. (2011). Pervasive exposure to violence and post-traumatic stress disorder in a predominantly African American Urban Community: The Detroit Neighborhood Health Study.Journal of Traumatic Stress, 24(6), 747–751. doi: 10.1002/jts.20705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore WL, & Widiger TA (2013). The DSM-5 dimensional trait model and five-factor models of general personality. Journal of Abnormal Psychology, 122(3), 816–821. doi: 10.1037./a0032822 [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. doi: 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Henrich J, Heine SJ, & Norenzayan A. (2010). The weirdest people in the world? The Behavioral and Brain Sciences, 33(2–3), 61–83. doi: 10.1017/S0140525X0999152X [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, & Donnellan MB (2010). How should the internal structure of personality inventories be evaluated? Personality and Social Psychology Review, 14(3), 332–346. doi: 10.1177/1088868310361240 [DOI] [PubMed] [Google Scholar]
- Hyatt CS, Owens MM, Gray JC, Carter NT, MacKillop J, Sweet LH, & Miller JD (2019). Personality traits share overlapping neuroanatomical correlates with internalizing and externalizing psychopathology. Journal of Abnormal Psychology, 1, 1–11. [DOI] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jones SE, Miller JD, & Lynam DR (2011). Personality, antisocial behavior, and aggression: A meta-analytic review. Journal of Criminal Justice, 39(4), 329–337. doi: 10.1016/j.jcrimjus.2011.03.004 [DOI] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D. (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136(5), 768–821. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … Zimmerman M. (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. doi: 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, & Skodol AE (2012). Initial construction of a maladaptive personality trait model and inventory for DSM–5. Psychological Medicine, 42(9), 1879–1890. doi: 10.1017/S0033291711002674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, & Rathouz PJ (2012). Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology, 121(4), 971–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee IA, & Preacher KJ (2013). Calculation for the test of the difference between two dependent correlations with one variable in common. Retrieved from http://quantpsy.org
- Lynam DR, Hoyle RH, & Newman JP (2006). The perils of partialling: Cautionary tales from aggression and psychopathy. Assessment, 13(3), 328–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, & Schutte NS (2005). The relationship between the five- factor model of personality and symptoms of clinical disorders: A meta-analysis. Journal of Psychopathology and Behavioral Assessment, 27(2), 101–114. [Google Scholar]
- Maples JL, Carter NT, Few LR, Crego C, Gore WL, Samuel DB, … Miller JD (2015). Testing whether the DSM-5 personality disorder trait model can be measured with a reduced set of items: An item response theory investigation of the Personality Inventory for DSM-5. Psychological Assessment, 27(4), 1195–1210. doi: 10.1037/pas0000120 [DOI] [PubMed] [Google Scholar]
- Miller JD, Dir A, Gentile B, Wilson L, Pryor LR, & Campbell WK (2010). Searching for a vulnerable dark triad: Comparing factor 2 psychopathy, vulnerable narcissism, and borderline personality disorder. Journal of Personality, 78(5), 1529–1564. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén [Google Scholar]
- O’Driscoll C, Laing J, & Mason O. (2014). Cognitive emotion regulation strategies, alexithymia and dissociation in schizophrenia, a review and meta-analysis. Clinical Psychology Review, 34, 482–495. [DOI] [PubMed] [Google Scholar]
- Peterson RA, & Reiss S. (1992). Anxiety Sensitivity Index Manual (2nd ed.). Worthington, OH: International Diagnostic Systems. [Google Scholar]
- Quilty LC, Ayearst L, Chmielewski M, Pollock BG, & Bagby RM (2013). The psychometric properties of the Personality Inventory for DSM-5 in an APA DSM-5 field trial sample. Assessment, 20(3), 362–369. doi: 10.1177/1073191113486183. [DOI] [PubMed] [Google Scholar]
- Samuel DB, & Widiger TA (2008). A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review, 28(8), 1326–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson C, & Clarkin JF (2002). Further use of the NEO-PI-R personality dimensions in differential treatment planning. In Costa PT Jr. & Widiger TA (Eds.), Personality disorders and the five-factor model of personality (pp. 351–375). Washington, DC: American Psychological Association. [Google Scholar]
- Saulsman LM, & Page AC (2004). The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review, 23(8), 1055–1085. doi: 10.1016/j.cpr.2002.09.001 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, & Grant M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption- II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Sheppes G, Suri G, & Gross JJ (2015). Emotion regulation and psychopathology. Annual Review of Clinical Psychology, 11(1), 379–405. [DOI] [PubMed] [Google Scholar]
- Skinner HA (1982). The drug abuse screening test. Addictive Behaviors, 7(4), 363–371. doi: 10.1016/0306-4603(82)90005-3 [DOI] [PubMed] [Google Scholar]
- Skodol AE, Morey LC, Bender DS, & Oldham JM (2015). The alternative DSM-5 model for personality disorders: A clinical application. American Journal of Psychiatry, 172(7), 606–613. doi: 10.1176/appi.ajp.2015.14101220. [DOI] [PubMed] [Google Scholar]
- Sleep CE, Hyatt CS, Lamkin J, Maples-Keller JL, & Miller JD (2018). Examining the relations among the DSM–5 Alternative Model of Personality, the Five-Factor Model, and externalizing and internalizing behavior. Personality Disorders: Theory, Research, and Treatment, 9(4), 379–384. doi: 10.1037/per0000240. [DOI] [PubMed] [Google Scholar]
- Sleep CE, Lynam DR, Hyatt CS, & Miller JD (2017). Perils of partialing redux: The case of the Dark Triad. Journal of Abnormal Psychology, 126(7), 939–950. doi: 10.1037/abn0000278 [DOI] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017). Strong homotypic continuity in common psychopathology-, internalizing-, and externalizing-specific factors over time in adolescents. Clinical Psychological Science, 5(1), 98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of Family Issues, 17(3), 283–316. [Google Scholar]
- Suzuki T, Griffin SA, & Samuel DB (2017). Capturing the DSM5 alternative personality disorder model traits in the five-factor model’s nomological net. Journal of Personality, 85(2), 220–231. doi: 10.1111/jopy.12235 [DOI] [PubMed] [Google Scholar]
- Suzuki T, South SC, Samuel DB, Wright AGC, Yalch MM, Hopwood CJ, & Thomas KM (2018). Measurement invariance of the DSM–5 Section III pathological personality trait model across sex. Personality Disorders: Theory, Research, and Treatment, 10, 114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, Van Hulle C, Waldman I, Krueger RF, & Rathouz PJ (2013). Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of Abnormal Psychology, 122(4), 1142–1153. doi: 10.1037/a0034151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellegen A, & Ben-Porath YS (2011). MMPI-2-RF: Minnesota Multiphasic Personality Inventory-2 Restructured Form: Technical manual. Minneapolis, MN: University of Minnesota Press. [Google Scholar]
- Watters CA, & Bagby RM (2018). A meta-analysis of the fivefactor internal structure of the Personality Inventory for DSM–5. Psychological Assessment, 30(9), 1255–1260. doi: 10.1037/pas0000605 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2015). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) – Past month. Retrieved from https://www.ptsd.va.gov/
- Widiger TA (1993). The DSM-III-R categorical personality disorder diagnoses: A critique and an alternative. Psychological Inquiry, 4(2), 75–90. doi: 10.1207/s15327965pli0402_1 [DOI] [Google Scholar]
- Widiger TA, & Oltmanns JR (2017). The general factor of psychopathology and personality. Clinical Psychological Science, 5(1), 182–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, & Simms LJ (2014). On the structure of personality disorder traits: Conjoint analyses of the CAT–PD, PID–5, and NEO–PI–3 trait models. Personality Disorders: Theory, Research, and Treatment, 5(1), 43–54. doi: 10.1037/per0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, & Simms LJ (2016). Stability and fluctuation of personality disorder features in daily life. Journal of Abnormal Psychology, 125(5), 641–656. doi: 10.1037/abn0000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, & Krueger RF (2012). The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology, 121(4), 951–957. doi: 10.1037/a0027669. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.