Abstract
Cancer stem cells (CSCs) are a subpopulation of cancer cells with stem cell properties that sustain cancers, which may be responsible for cancer metastasis or recurrence. Lipid rafts are cholesterol- and sphingolipid-enriched microdomains in the plasma membrane that mediate various intracellular signaling. The occurrence and progression of cancer are closely related to lipid rafts. Emerging evidence indicates that lipid raft levels are significantly enriched in CSCs compared to cancer cells and that most CSC markers such as CD24, CD44, and CD133 are located in lipid rafts. Furthermore, lipid rafts play an essential role in CSCs, specifically in CSC self-renewal, epithelial-mesenchymal transition, drug resistance, and CSC niche. Therefore, lipid rafts are critical regulatory platforms for CSCs and promising therapeutic targets for cancer therapy.
Keywords: Lipid raft, Cancer, Cancer stem cell, Self-renewal, Drug resistance, Epithelial-mesenchymal transition, Cancer stem cell niche
Introduction
According to the Global Burden of Disease (GBD) report in 2017, cancer has been the leading cause of global mortality [1]. Despite advances in cancer prevention, it remains a human nightmare as cures are rare, and most patients have metastasis or recurrence. Cancer stem cells (CSCs) may be to blame because they can resist electromagnetic and chemotherapy through a quiescent state [2]. Meanwhile, as tumor-initiating cells, CSCs supply constant cancer cells for cancers. Therefore, CSCs must be eliminated to eradicate cancer.
Lipid rafts are signaling and transit platforms that are critical in cancer development and progression [3, 4]. Since Simons and Ikonen proposed the lipid raft hypothesis based on the classical membrane fluid mosaic model [5], lipid raft research has gradually deepened. The discussion on lipid rafts at the Keystone Symposium has been agreed upon, “lipid rafts are small (10–200 nm), heterogeneous, highly dynamic, sterol- and sphingolipid-enriched domains that compartmentalize cellular processes. Small rafts can sometimes be stabilized to form larger platforms through protein–protein and protein-lipid interactions” [6]. Lipid rafts, also known as “membrane rafts” or “membrane microdomains,” are divided into caveolae (flask-like invaginations) and planar lipid rafts [7]. Caveolin-1 and flotillins are lipid raft markers [8]. Caveolin-1 is an essential structural protein of caveolae [9], and flotillins are linked to poor cancer prognoses [10].
Cancer cells are previously confirmed to have higher levels of lipid rafts than normal cells [11, 12], while emerging evidence indicates that CSCs contain more lipid rafts than cancer cells. That is, the relative amount of lipid rafts: CSCs > cancer cells > normal cells [13]. Specifically, a study using filipin and conjugated cholera toxin B (CtxB) for plasma membrane cholesterol and GM1 staining showed that the cancer cell lines (PC-3, LNCaP, MCF-7, and MDA-MB-231) have stronger staining than the normal cell lines (PZ-HPV7 and MCF-10A), suggesting higher levels of rafts/ caveolae in the cancer cell lines. Meanwhile, the purified lipid rafts in human prostate cancer cell PC-3 are five times more than in normal cells [11]. Quite similar results have also appeared in melanoma cells, which have 1.5–2 higher lipid rafts levels than non-tumorigenic cells detected by fluorescent probes and flow cytometry [12]. Regarding the lipid rafts of CSCs, the data from CtxB immunostaining and flow cytometry assay have shown that the levels of lipid rafts in CD44high colorectal cancer cells are higher, as the median fluorescence intensity ratio of lipid rafts within CD44high cells is 10%-30% stronger than CD44low cells. Importantly, CtxBhigh cells showed a greater sphere‐forming capacity [13]. In addition, CD133+ pancreatic cancer cells have more caveolin-1and cholesterol than CD133− cells by Western blotting, real-time PCR and Amplex red cholesterol assay, indicating higher levels of lipid rafts in CD133+ CSCs [14]. Moreover, lipid rafts are indispensable for CSCs, and our previous study demonstrated that the suppression of lipid raft formation inhibits CD133+ CSC stemness [15]. Through transmission electron microscopy observation and sphere formation assay, we found that the reduction in caveolae is accompanied by decreased stemness markers CD133, Bmi-1, SOX-2, and spheroids. Interestingly, CSCs die once the lipid rafts are disrupted. A study revealed that miltefosine and other lipid raft‐disrupting drugs such as MβCD and nystatin downregulate the expression of stem‐related genes and upregulate the expression of differentiation marker genes by RT‐qPCR assay. In parallel, immunofluorescence assays and flow cytometry analysis visually confirmed miltefosine reduces lipid raft levels with a disruption of sphere formation. Similar to in vitro assay, immunostaining assays of xenografted tumors have revealed a decrease in CD44high cells along with an increase in apoptotic cells after miltefosine treatment [13]. Meanwhile, several CSC biomarkers have been found in lipid rafts, which are affected by lipid rafts [16–19]. The above studies suggest that targeting lipid rafts on CSCs is a precise strategy for cancer prevention. The relationship between CSCs and lipid rafts has attracted more and more attention.
Cancer stem cell: from controversy to confirmation
As defined by the AACR Workshop, CSC is a cell within a tumor that possesses the capacity to self-renew and cause the heterogeneous lineages of cancer cells that comprise the tumor [20]. It is also known as “tumor-initiating cells” or “tumorigenic cells” [21]. The proposition of CSC theory is aggressive and has long been controversial. But now, a wealth of convincing evidence makes the CSC theory even more tenable. In 1994, T Lapidot et al. found a CD34+ CD38− cell with the ability to initiate acute myeloid leukemia and self-renewal [22]. Since then, CSCs have been found in brain cancer [23], colorectal cancer [24], osteosarcoma cancer [25], breast cancer [26], colon cancer [27], prostate cancer [28], thyroid cancer [29], ovary cancer [30], pancreatic cancer [31], head and neck squamous cell carcinoma [32], and so on. So far, several CSC markers have been discovered that assist in identifying CSCs. Among them, CD133, CD44, and aldehyde dehydrogenase (ALDH) are markers of most solid tumors [33, 34]. In addition, therapies targeting CSCs are nearing maturity. Anti-CSC drugs are in multiple clinical trials. For example, the chemokine receptor-4 (CXCR4) inhibitor Plerixafor increases chemosensitivity in hematologic malignancies; B-cell lymphoma-2 (BCL2) inhibitors Venetoclax for acute myeloid leukemia can target CSC metabolism [35]. Most importantly, CSCs have several stem cell-like properties (Table 1). First, CSCs have similar markers (such as CD133) to stem cells [36, 37] and a higher telomerase activity just like normal stem cells [38, 39]. In particular, CSCs share self-renewal signaling pathways with normal stem cells [40]. Second, CSCs have self-renewal ability that divides symmetrically into two CSC progenies or asymmetrically into one CSC progeny and one non-CSC progeny [41, 42]. When CSCs stop proliferating, CSCs maintain a quiescent or dormant state and undergo reversible cell cycle arrest to escape therapy [43, 44], resulting in cancer relapse or metastasis. Finally, the CSCs have stem cell-like differentiation potential [45]. CSCs can transform into cancer cells. Meanwhile, they can be transdifferentiated into other cell type [46–48], such as vascular endothelial cells. Cancer cells can also dedifferentiate back into CSCs during appropriate processes such as epithelial-mesenchymal transition (EMT) [49, 50]. That is the plasticity of CSCs, which makes CSCs slyer.
Table 1.
Similarities and differences between cancer stem cell and normal stem cell
| Cancer stem cell | Normal stem cell | Reference | |
|---|---|---|---|
| Similarities | Markers: CD133, SSEA3, SSEA4, TRA-1–60, etc. | [51] | |
| Biochemical profile: a higher telomerase activity | [38, 40] | ||
| Proliferation: self-renewal (symmetrically and asymmetrically dividing) | [41, 42] | ||
| Differentiation: differentiate into distinct types of cells | [45] | ||
| Differences | Markers: CD20, CD96, CD55, and TIM-3 are not markers for normal stem cells but for CSCs | [51] | |
| Proliferation: CSCs divide more rapidly than normal stem cells (the cell division rate is an order of magnitude larger) | [40] | ||
| Differentiation: CSCs very few undergo terminal differentiation compared to normal stem cells | [52] | ||
Although CSCs are not well-studied, they may explain why treatment is ineffective. In brief, CSCs maintain cancer growth through self-renewal capacity and avoids therapy in a quiescent state. The CSC niche (microenvironment around stem cells) provides physical shelter for CSCs and allows non-CSCs to dedifferentiate into CSCs through EMT, resulting in relapse. Therefore, this review evaluates the role of lipid rafts in CSC self-renewal, drug resistance, EMT, and stem cell niche (Fig. 1). An in-depth study of the interrelationships and functions between lipid rafts and CSCs will contribute to designing intervention strategies for cancer eradication.
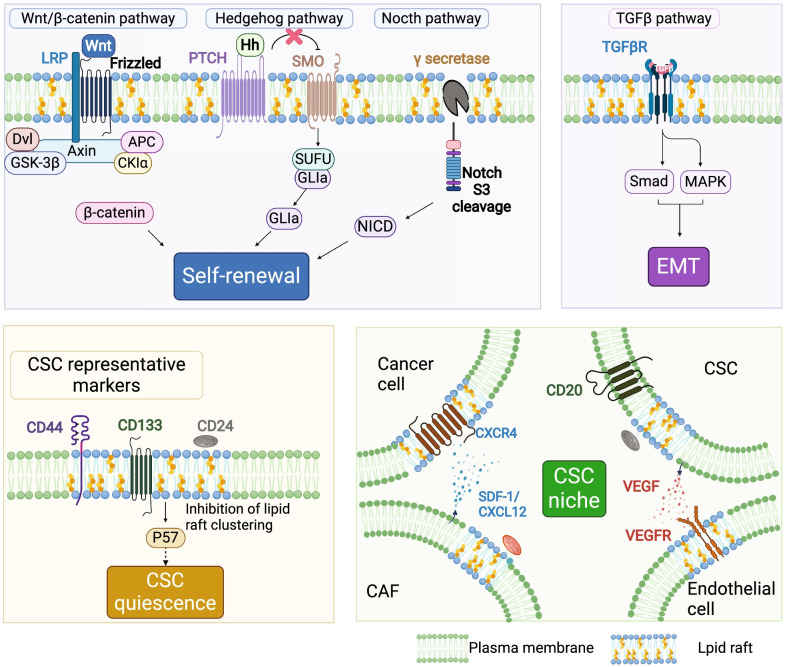
Fig. 1.
Function of lipid rafts in cancer stem cell. Lipid rafts play a crucial role in cancer stem cells (CSCs). CSC self-renewal: lipid rafts promote CSC self-renewal through the Wnt/β-catenin pathway, Notch pathway, and Hedgehog pathway. Wnt/β-catenin pathway: in lipid rafts, Wnt ligand binds to their receptors Fz8 and LRP, phosphorylate the cytoplasmic domain of LRP, and recruits the scaffolding protein Dvl to disassemble the destruction complex (Axin, APC, GSK-3β, and Ck1α), eventually inhibiting degradation of β-catenin, which activate target gene transcription. Hedgehog pathway: in lipid rafts, the Hh ligand binds to its receptor Ptc, and Ptc releases the repression on Smo, allowing GLI to enter the nucleus and stimulate transcription of downstream target genes. Notch pathway: γ-secretase, the key protease of the Notch receptor, exhibits the highest activity in lipid rafts, which mediates the S3 site cleavage of the Notch receptor, and then releases the Notch intracellular domain (NICD) into the nucleus that promotes transcription of the target genes. EMT: lipid rafts regulate CSC EMT through the TGFβ pathway. The TGF-βRI/ TGF-βRII/ TGF-β signaling complex forms in lipid rafts to activate the downstream signal. CSC quiescence: inhibition of lipid raft aggregation upregulate cyclin-dependent kinase inhibitor p57 (Kip2) expression, which might trigger CSC hibernation. CSC niche: lipid rafts mediate cell communication in the CSC niche. For example, VEGF secreted by CSCs binds to VEGFR2 in lipid rafts of endothelial cells, promoting niche angiogenesis and enhancing self-maintenance; CAFs secrete CXCL12, which is recruited to lipid rafts in cancer cells, where it interacts with CXCR4, regulating CSC plasticity
CSC markers and lipid rafts
CSC markers are specialized proteins on the CSC surface or secreted by CSCs that help identify or isolate CSCs [51] and predict poor clinical outcomes [53]. In addition, CSC markers are also necessary for CSC functions. Therefore, targeting cell surface markers to destroy CSCs is available [34]. Encouragingly, agents targeting CSC-related markers are already in clinical trials [35], and some have been approved for clinical use. Studies have shown that many CSC markers are located in or associated with lipid rafts, such as CD24, CD44, CXCR4, and CD133 [54, 55]. The relation between lipid rafts and these CSC markers is evaluated as follows.
The glycosylphosphatidylinositol (GPI)–anchored glycoprotein CD24, a typical raft protein, is highly expressed in CSCs and is considered a CSC marker that maintains cancer stemness [56–58]. CD24 can recruit integrin into lipid rafts that facilitate cancer development. Further studies have found that CD24 enhances integrin-mediated adhesion and invasion by stimulating c-src (a raft resident) activity, and this effect is reversed when the lipid rafts are disrupted [59]. In addition, CD24 can recruit phosphorylated Met into lipid rafts to increase ATP-binding cassette (ABC) transporters expression, resulting in cisplatin resistance [60].
CD44 is a cell surface hyaluronan receptor with signaling functions [61, 62] that maintains the stemness of CSCs [63]. Moreover, CD44 is also highly expressed in various CSCs and is a common CSC marker in solid tumors such as pancreatic and prostate cancers [31, 64, 65]. Previous studies revealed that CD44 exists in lipid rafts [66–68]. Concretely, lipid rafts are isolated using detergent extraction methods combined with isopycnic sucrose density gradient fractionation. Western blotting assay and co-immunoprecipitation detection manifest the expression of CD44 is dramatically higher in lipid raft fractions than in non-lipid raft fractions [68]. Likewise, immunofluorescence observation further shows that CD44 co-localizes with the raft marker caveolin-1 [69]. Meanwhile, the functions of CD44 are dependent on the CD44 cluster to lipid rafts [70]. Following the interaction of hyaluronan with its receptor, CD44 multiprotein complexes assemble in lipid rafts to activate downstream signaling, which is critical for the properties of CSCs [17, 71]. In contrast, lipid raft disruption by depleting cholesterol prevents CD44 from recruiting to lipid rafts, enhances CD44 shedding, and suppresses CD44-dependent cancer cell migration [72].
CD133 (alias prominin-1/AC133), a pentaspan transmembrane glycoprotein, is a marker for stem cells and CSCs, which rarely appears on normal tissue cells [36, 37, 51]. In normal stem cells, CD133 is mainly associated with cell proliferation [73], while in CSCs, it is involved in cancer cell proliferation, carcinogenesis, metastasis, recurrence, and chemoresistance [74, 75]. This critical CSC marker is localized in lipid rafts [14, 76]. CD133 induces EMT and stemness properties by interacting with the Src (lipid raft-related protein) [77]. Similarly, CD133 can activate raft resident Src to phosphorylate focal adhesion kinase (FAK), promoting cell migration [78]. Furthermore, the formation of polarized CD133/ integrin induces lipid raft coalescence and then activates Src to promote β-catenin nuclear translocation and CSC self-renewal [79]. Notably, perturbed lipid raft coalescence abolishes β-catenin activation and the CSC phenotype.
CXCR4 is a G-protein-coupled chemokine receptor for stromal cell-derived factor 1 (SDF-1, also known as CXCL12) and is a crucial CSC marker [80–83]. Increased expression of CXCR4 correlates with chemotaxis, invasiveness, and CSC properties. Downregulated CXCR4 inhibits cancer cell stemness [84]. Studies found that CXCR4 and c-MET (MET proto-oncogene) colocalize with caveolin-1 in lipid rafts, and caveolin 1 is required for CXCL12/ CXCR4-induced c-MET activation that enhances EMT [85]. Ultimately, disruption of lipid rafts blocks CXCL12/ CXCR4 activation [85]. That is, CXCR4 cannot work without lipid rafts.
In sum, CSC markers are present in lipid rafts, and their function is regulated by lipid rafts. The therapeutic antibodies targeting CSC surface markers have been approved for clinical application. Hence, lipid rafts may assist these molecular targeted therapies. Targeting lipid rafts may lead to dysfunction of CSC markers, which also offers exciting possibilities for clear CSCs.
CSC self-renewal and lipid raft
Self-renewal is the ability of stem cells that divide to produce more stem cells [86]. That is why these distinct subpopulations of cancer cells are defined as CSCs. The self-renewal capacity of CSCs is aggressive and uncontrollable, while that of the normal stem cells is orderly. CSC self-renewal involves a lot of signaling pathways, primarily including the Wnt/ β-catenin, Notch, and Hedgehog pathways [87–89]. As a platform for cell signaling transduction, lipid rafts control CSC self-renewal signaling pathways.
The Wnt/ β-catenin pathway is one of the significant signaling pathways involved in stem cell self-renewal. The positive effect of the Wnt/β-catenin pathway on CSC self-renewal has been reported in various cancers [90, 91], such as liver cancer [90], breast cancer [92], colorectal cancer [93], and acute myelogenous leukemia [94, 95]. Wnt ligands can combine with their receptors Frizzled receptors (Fz) and co-receptors low-density lipoprotein receptor-related protein 5 (LRP5)/6, phosphorylating the cytoplasmic domain of LRP and then recruiting the scaffolding protein Disheveled (Dvl) to disassemble the destruction complex. The destruction complex mediates the β-catenin degradation, which includs scaffolding proteins Axin, adenomatous polyposis coli (APC), the kinase proteins glycogen synthase kinase-3β (GSK-3β), and casein kinase 1α (Ck1α). As a result, β-catenin accumulates and activates numerous target gene transcription [96, 97]. However, the binding of Wnt ligand to their receptors Fz8 and LRP 6 predominantly occurs in ordered lipid raft microdomains because Wnt receptor complexes are partially located in lipid rafts [98–100]. The more receptors in lipid rafts, the higher the activity of Wnt/ β-catenin signaling (Data from simulation experiments [101]). In addition, removing LRP6 from lipid rafts to the non-lipid rafts domain suppresses the β-catenin pathway [99], while increasing lipid raft mobility can enhance Wnt-mediated signaling [102]. Collectively, these imply that lipid rafts can regulate CSC self-renewal by mediating the Wnt/β-catenin pathway.
Another way to regulate CSC self-renewal is Hedgehog (Hh) pathway [103]. The Hh pathway can be triggered by Sonic Hedgehog (SHH), Indian Hedgehog (IHH), and Desert Hedgehog (DHH). Upon binding of the above ligands to their receptor Patched (Ptc), and Ptc released the repression on Smoothened (Smo) to allow GLI (a full-length form of glioma-associated oncogene homolog) to enter the nucleus that stimulates downstream target genes transcription (such as PTCH1, GLI1, and Wnt) [104, 105]. Activation of the Hh pathway facilitates CSC self-renewal [106]. However, lipid rafts are critical for high Hh activity transduction because the receptors Ptc and Smo are located in lipid rafts upon Hh stimulation [107–109]. Furthermore, when lipid rafts are disrupted, Hh pathway activity is downregulated, and the higher-order clusters of Smo on the plasma membrane are significantly reduced [107]. Another study has shown that lipid rafts are related to the intracellular transportation of Shh. Specifically, intracellular Shh can form protein complexes with caveolin-1 in the Golgi apparatus to transport lipid raft microdomains [110]. These suggest lipid rafts involve signal transduction and intracellular ligand transportation of Hh signaling, affecting CSC self-renewal.
Further, the Notch pathway is also essential for stem cell self-renewal. There are five Notch ligands (Delta-like (DLL) 1, DLL3, DLL 4, Jagged (JAG) 1, JAG 2) and four receptors (Notch1-Notch4) in mammals. Upon their interaction, proteolytic events of disintegrin and metalloproteinases (ADAMs)-mediated cleavage at the S2 site and γ-secretase-mediated cleavage at the S3 site of the Notch receptor release the Notch intracellular domain (NICD) and enters the nucleus to activate downstream Notch target gene expression [111, 112], governing CSC self-renewal and differentiation [113, 114]. Interestingly, lipid rafts are involved in the action of the protease γ-secretase. The protease γ-secretase assembles into lipid rafts and exhibits the highest activity there, indicating γ-secretase function depends upon its distribution between the raft and non-raft microdomains [115, 116]. Further studies have shown that hypoxia-induced “raft clusters” promote Notch3 partially migrated into lipid rafts, where they interact with γ-secretase, leading to the progression of human prostate cancer by stimulating Notch signaling [117]. Moreover, lipid rafts resident caveolin-1 is related to Notch-1expression. Downregulation of caveolin-1 decreases Notch-1 and NICD expression and inhibits Notch signaling that promotes stem cell differentiation [118]. Meanwhile, Ethanol may inhibit γ-secretase proteolytic activity that suppresses Notch signaling, possibly by decreasing caveolin-1 [119]. Overall, lipid rafts and their associated protein caveolin-1 regulate the downstream cascade of the Notch pathway that affects CSC self-renewal.
Apart from the above-mentioned pathways for CSC self-renewal need lipid rafts. The essential CSC self-renewal protein CD55, an intrinsic cell surface GPI-anchored membrane complement inhibitor that protects cells from complement-mediated lysis [120], also requires GPI-anchoring to lipid rafts for CSC stemness maintenance and cisplatin resistance [18].
CSC self-renewal is critical for cancer propagation. As discussed above, lipid rafts mediate CSC self-renewal, which strongly supports that understanding and manipulating lipid rafts in the plasma membrane holds promise for simultaneously inhibiting three CSC self-renewal related pathways. Our previous study showed that inhibiting lipid raft structural protein caveolin-1 could repress CSC properties by blocking the Wnt/ β-catenin signaling pathway [15], which proves the feasibility of the above perspective.
Drug resistance and lipid raft
Quiescent CSCs are a recognized cause of therapeutic resistance [121]. Cell surface signals control stem cell hibernation or cell cycle re-entry [122]. Lipid rafts are vital for stem cell fate as the signal hub. For example, lipid raft clustering regulates the fate of hematopoietic stem cells (HSC) in vitro [123]. Therefore, eliminating quiescent CSCs is one approach to preventing drug resistance, such as the selective eradication of quiescent human leukemia stem cells by targeting BCL 2-dependent oxidative phosphorylation [124]. In contrast, keeping CSCs in a permanent quiescent state is another approach. As long as CSCs do not enter the cell cycle, their presence does not affect cancer progression. Excitingly, diphenyleneiodonium chloride can induce CSCs quiescence phenotype to make CSC hibernation [125], and this study brings hope for CSCs quiescence strategies. Intriguingly, the inhibition of lipid raft aggregation induces cyclin-dependent kinase inhibitor p57 (Kip2) expression, leading to HSCs hibernation [126], which is theoretically effective to CSCs, based on their similarity to stem cells. That means that we can prohibit lipid raft clusters to keeping CSCs quiescent. Among potential candidates, emodin has been reported to suppress lipid raft clusters [127]. The future will reveal whether such a bold idea will be implemented.
Drug efflux pumps (e.g., ABC transporter) are another mechanism driving drug resistance [128, 129], which expel anti-cancer drugs from CSCs. For example, CD133+ melanoma CSCs resist caffeic acid phenethyl ester because of elevated ABCB5 expression [130]. Likewise, ABCB5 increases resistance in CD133+ glioblastoma multiforme CSCs, and ABCB5 inhibition makes CSCs sensitive to temozolomide [131]. Importantly, these multidrug resistance-associated drug efflux transporters are found in lipid rafts [132], implying that lipid rafts can regulate these resistance-related proteins. Numerous studies confirmed that disrupting lipid rafts can reverse drug resistance. For example, interference with lipid rafts abrogates ABC transporters induced chemoresistance in CD133+ pancreatic CSCs [14]. Depletion of lipid rafts with simvastatin suppresses integrin-β3/FAK signaling, re-sensitizing cancer cells to paclitaxel [133]. Similarly, disrupting the key lipid raft proteins, flotillins, reverses drug resistance in colorectal cancer cells [134].
EMT and lipid raft
EMT is a cell-biological program in which the epithelial phenotype is lost and mesenchymal characteristics are acquired [135]. EMT is generally accepted to be a critical step in the migration and invasion of cancer cells [136]. In the context of CSC theory, EMT programs have been demonstrated to promote CSC stemness [137, 138] or rather generate CSCs [139]. For example, most mesenchymal-like human mammary epithelial cells become CD44+/CD24− neoplastic mammary stem cells after undergoing EMT [139]. Lipid rafts are indispensable for the whole EMT process. EMT-induced motility and stem cell properties require the destabilization of lipid rafts. Generally, lipid raft stability is quantified by measuring miscibility transition temperature: 50% of the vesicles are phase separated. In concrete terms, cells that undergo EMT have reduced phase separation in isolated plasma membrane vesicles, which are divided into liquid-ordered (raft) domain and disordered (non-raft) domain, indicating that cells in the epithelial state possess more stable lipid raft domains. Cell migration, mammosphere formation, and alternate splicing from a variant isoform (CD44v) in epithelial cells to a standard isoform (CD44s) in mesenchymal cells are inhibited when DHA is treated to stabilize raft phase separation, suggesting that EMT and stemness are suppressed [140].
Transforming growth factor-β (TGF-β) is a potent inducer that drives EMT mainly through the canonical Smad-dependent signaling pathway [141]. TGF-β combines with the TGF-β receptor II (TGF-βRII) to phosphorylate TGF- β receptor I(TGF-βRI). Subsequently, R-smad (receptor-regulated Smad) are activated to form R-Smad/ CO-Smad (common partner Smad) complexes and translocate to the nucleus, where they regulate the transcription of EMT target genes. I-Smad (inhibitory Smad) can interact with TβRI to inhibit TGF-β signaling through ubiquitin-dependent degradation [141, 142]. A previous study has found that TGF-βRII is partially localized in lipid rafts and is internalized for degradation in an I-smad-dependent manner. In particular, TβRII and caveolin-1 colocalize in Mv1Lu cells expressing extracellularly HA-tagged TGF-β type II receptors by three-color immunofluorescence analysis. Similarly, immunoprecipitation and western blotting analysis have also yielded similar results. Furthermore, caveolin-1 can cooperate with Smad7–Smurf2 to enhance receptor degradation in cells transiently transfected with TβRI, TβRII, and Smad7, as detected by immunoprecipitation and immunoblotting assay. The t1/2 of TGF-β receptor is 6 h in cells without caveolin-1 expression, while the t1/2 is reduced to 4 h in cells expressing caveolin-1 [143]. Meanwhile, this I-smad-dependent receptor turnover is blocked when lipid rafts are disrupted [143]. Likewise, the anti-cancer drug sorafenib suppresses TGF-β signaling by inducing caveolae/lipid raft-mediated TGF-βRII degradation, thereby inhibiting EMT [144]. The evidence above indicates lipid rafts negatively regulate TGF- β signaling by promoting TGF-βRII degradation. Conversely, there is a clue that lipid rafts facilitate TGF-β signaling, as lipid rafts seem to provide a platform for TGF-βRII to activate TGF-βRI. TGF-βRI and TGF-βRII are imaged and tracked in living cells by single-molecule imaging. The mobility of TGF-βRI is obviously declined after TGF-β stimulation, which is attributed to the formation of TGF-βRI/ TGF-βRII/ TGF-β signaling complex. However, in cells whose lipid rafts are disrupted by nystatin or MβCD, the diffusion rate of TGF-βRI is not altered by TGF-β treatment, and the phosphorylation level of downstream Smad2 is decreased [145]. In brief, lipid rafts play a role in TGF- β/ Smad signal, yet whether lipid rafts play a positive or negative role during this process requires further investigation. In addition, lipid rafts also positively affect non-canonical TGF- β pathway. Activation of the non-canonical TGF-β/ MAPK (mitogen-activated protein kinase) pathway is dependent on lipid rafts [146]. The disruption of lipid rafts disturbs the localization of TGF-β receptors in lipid rafts and impairs TGF-β–mediated MAPK activation, thereby inhibiting EMT [146].
The lipid raft marker flotillin is also involved in the EMT process [8]. After radiofrequency ablation therapy, the residual hepatocellular carcinoma cells progress rapidly, probably because the residual cell acquires stemness through EMT. Studies have attributed this phenomenon to the upregulation of flotillin-1 and flotillin-2, which promote EMT by activating the Akt/ Wnt/ β-catenin signaling pathway [147]. In early-stage cervical cancer, flotillin-1 is highly expressed and motivates EMT through Wnt/ β-catenin and NF-κB signaling pathway [148]. Likewise, flotillin-2 is upregulated in nasopharyngeal carcinoma and enhances EMT by activating lipid raft resident protein Src, which might be served as a downstream factor of TGF- β, indicating that lipid rafts are closely involved in this process [149].
Notably, the EMT inducer TGF-β has efficiently promoted non-CSC-to-CSC conversion [150]. That is, TGF-β induces CSC plasticity. These interconversions between epithelial non-CSC and mesenchymal/ CSC states proved the impact of EMT on CSC. Lipid raft and its marker flotillin facilitate EMT. That indicates we can prevent non-CSCs poised to become CSCs by disrupting lipid rafts.
CSC niche and lipid raft
The stem cell niche is a dynamic microenvironment surrounding stem cells and is made up of adjacent cells, cytokines, and the extracellular matrix [155]. It is a subcompartment within the tumor microenvironment (TME). Like normal stem cells, CSCs live in niches [156]. CSCs are tightly dependent on their niche, which provides a favorable living environment for CSCs. In particular, lipid rafts transmit signals for the cells in the CSC niche to maintain CSC niche function.
CSCs promote niche angiogenesis and enhance self-maintenance by secreting vascular endothelial growth factor A (VEGF) [157, 158]. VEGF stimulates angiogenic ERK (extracellular regulated protein kinases)/MAPK signaling by binding to VEGF receptor-2 (VEGFR-2). VEGFR-2 has been reported to be located in lipid rafts, and lipid raft disruption can selectively reduce VEGFR2 levels and inhibit the downstream ERK/ MAPK pathway [151].
The ECM, including fibrous proteins, glycoproteins, proteoglycans, and polysaccharides, is an essential structural component of the CSC niche [159]. It can physically shield CSCs from therapeutic agents and modulate CSCs [160]. Integrins are prominent ECM surface receptor proteins that mediate cell-to-cell interactions and communication with the ECM [161], which are critical for the function of CSC [162, 163]. The role of integrin depends a lot on lipid raft to transmit signals. For example, lipid rafts regulate the initial spread of cancer cells by recruiting and modifying adaptor proteins (such as talin, α-actinin, vinculin, paxillin, and FAK) to binding β1 integrins [164]. Notably, lipid raft structure disruption prevents β1 integrin clustering [152].
CAFs are stromal cells of the CSCs niche that sustain cancer stemness and regulate CSCs plasticity via paracrine signaling [165–168]. SDF-1/CXCL12 is the primary secretome of CAFs [169], which promotes cancer growth by interacting with CXCR4 in cancer cells [170, 171]. The function of CXCL12 is recognized to be mediated by lipid rafts [172]. CXCL12 is recruited to lipid rafts, and its operation requires the involvement of raft resident Src-family protein tyrosine kinases [172]. Furthermore, inhibition of lipid rafts blocks CXCL12 signaling [153, 173].
Cellular senescence is the latest addition to the hallmarks of cancer [174]. Treatment-induced senescent cancer cells or other senescent cells in the TME can remodel microenvironments to promote cancer phenotypes through proinflammatory senescence-associated secretory phenotype (SASP) in a paracrine manner [175–178]. Meanwhile, SASP facilitates CSCs by providing chemokines and inflammatory cytokines (such as IL-1β, IL-8, and CXCR1) [179, 180]. The recently published review by our group revealed that lipid rafts and their component protein are integral parts of cellular senescence [154]. For example, caveolin-1 induces senescence by activating P53 though affecting Mdm2 (mouse double minute 2 homolog), PP2A-C (protein phosphatase 2A-C subunit), Sirt1, TrxR1 (thioredoxin reductase 1), Nrf2 (nuclear factor erythroid-2-related factor-2), and EGFR (epidermal growth factor receptor) [154]. It is feasible to manipulate lipid rafts to suppress cellular senescence and minimize the effects of SASP on the CSC niche.
As long as the niche remains intact, CSCs continue to be recreated to maintain cancer homeostasis [181]. The efficient functioning of the CSC niche requires the collaborate of different cells, and cell communication is the way of cooperation. As the signal hub of cells that receive and transmit signals, the absence of lipid rafts would break the niche balance. Considering lipid raft regulates support signals of CSC niche, it might be the one to terminate CSCs.
Lipid raft disrupted agents and anti-CSC strategies
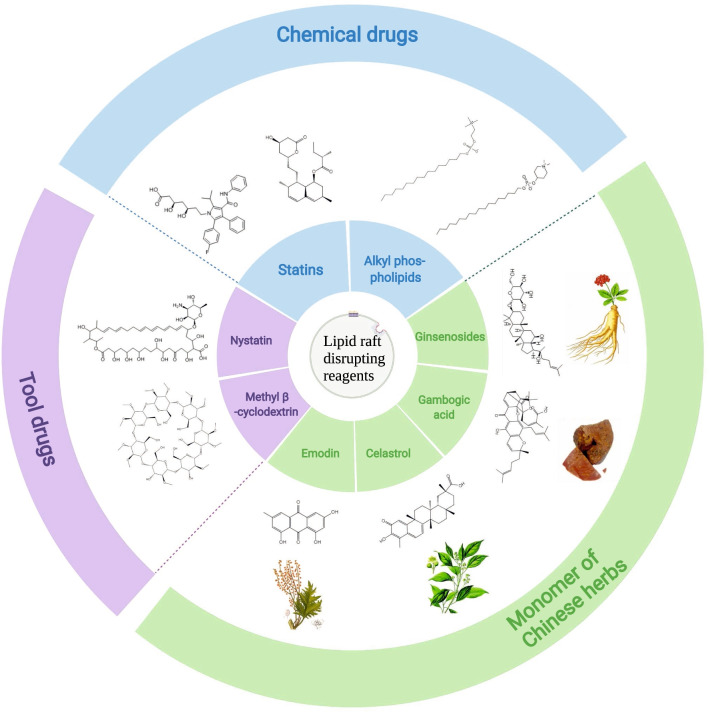
In current therapeutic strategies to eradicate cancer, the combination of traditional anti-cancer drugs and CSC-targeted agents simultaneously kills both CSCs and non-CSCs, preventing cancer recurrence. Targeted lipid raft can thus be a sally port for CSC elimination. That is, the combination of lipid raft-targeted drugs and anti-cancer drugs could eradicate cancer. Therefore, agents targeting lipid rafts (also known as raftophilic) show great anti-cancer potential (Fig. 2). In addition to the tool drugs MβCD and cholesterol-sequestering agent nystatin, the major types of lipid raft disrupting agents are as follows.
Fig. 2.
Lipid raft disrupting reagents. Methyl β -cyclodextrin and nystatin are tool drugs for the disruption of lipid rafts. Statins and alkyl phospholipids are chemicals that can interrupt the integrity of lipid rafts. Moreover, emodin, celastrol, ginsenosides, and gambogic acid are all extracted from the herb
Cholesterol synthesis inhibitor statins disrupt lipid raft by depleting cellular cholesterol. Studies have manifested that lovastatin, one of the statins, decreases the metastatic potential of pancreatic CSCs and increases chemosensitivity by disrupting lipid rafts [14]. Likewise, gambogic acid impairs lipid rafts and inhibits cancer cell adhesion by reducing cellular cholesterol content [182]. Moreover, the cholesterol analogs ginsenosides disrupt lipid rafts by increasing membrane fluidity [183]. The ginsenoside derivative Rp1 has been reported to reverse multidrug resistance by modulating lipid rafts to inactivate ABCB1 (drug effluxes protein in lipid raft) and Src [184]. Endogenous phospholipids analogs, alkyl phospholipids (ALPs), and modified APL derivatives include edelfosine, miltefosine, perifosine, and erufosine interrupt lipid raft integrity by incorporating into lipid raft, thereby inducing cancer cell growth arrest and apoptosis [4, 185–192]. Miltefosine preferentially induces colorectal CSCs death by disrupting lipid raft [13], and the lipid raft-targeted edelfosine has been recently reported to induce apoptosis in pancreatic CSCs by autophagy inhibition [193]. In addition, the major active component of the rhizome of Rheum palmatum L, emodin, has been found to inhibit the lipid raft clustering by reducing cholesterol and sphingolipids, inhibiting cancer cell adhesion [127]. Our group initially demonstrated that celastrol, a pentacyclic triterpene extracted from Tripterygium wilfordii Hook F, decreases caveolae (the subset of lipid raft), resulting in declined stemness of CD133+ CSCs [15]. Targeting lipid raft therapy could eliminate CSCs, eventually resolving many pending issues.
Conclusion and perspective
A complete cure for cancer is the common pursuit of humanity, while CSC stands in the way. Existing evidence demonstrates lipid rafts are associated with CSC self-renewal, quiescence, EMT, and CSC niche. As a platform for protein anchorage, more than half of CSC markers are located in lipid rafts, and drug efflux proteins that contribute to CSC resistance are also present in lipid rafts. That means lipid rafts may regulate these raft-relevant proteins. In particular, lipid rafts regulate CSC self-renewal and EMT by mediating Wnt/ β-catenin pathway, Notch pathway, Hh pathway, and TGF-β pathway. Furthermore, lipid rafts have the potential to intervene in CSC quiescence, and they are also responsible for cellular communications of the CSC niche. Therefore, lipid raft might be an effective target for CSC elimination (Table 2).
Table 2.
Role of lipid raft
| Proteins located in lipid raft | Cell lines | The effect of lipid raft | Lipid raft disrupting reagents | References | |
|---|---|---|---|---|---|
| CSC markers | CD24 | MTLY | Promotes FAK/integrin-mediated adhesion and invasion |
MβCD (methyl-β-cyclodextrin) |
[59] |
| CD24+ hec-1A and hec-108 | Promotes drug resistance | N/A | [60] | ||
| CD44 | U-251 MG | Promotes cancer cell migration | MβCD, simvastatin | [72] | |
| CD133 | CD133+ SAS and OECM1 | Promotes EMT and maintains CSC properties | PP2 (inhibitor of Src activity) | [77] | |
| CD133+ U87MG | Promotes CSC self-renewal | MβCD, knockdown of Par3 and Par6 (perturbed lipid raft coalescence and cell polarization) | [79] | ||
| CXCR4 | MGC-803 | Promotes EMT | Nystatin, knockdown of caveolin-1 | [85] | |
| CSC self-renewal | Fz receptor, LRP | HEK293T | Promote Wnt/ β-catenin pathway | Cholesterol oxidase (deplete cholesterol), myriocin (deplete sphingomyelin), oseltamivir (deplete GM1 ganglioside), membrane cholesterol‐deficient Niemann–Pick C disease cells | [98] |
| Ptc, Smo, | Drosophila S2 cell | Promotes Hedgehog pathway | Eicosapentaenoic acid 20:5(n-3), PUFA (disrupt lipid raft stability) | [107] | |
| Ptc, Caveolin-1 | Chinese hamster ovary cells | Promotes Hedgehog pathway | MβCD | [108] | |
| γ-secretase, Notch3 | LNCaP | Promotes Notch pathway to increase cancer progression | N/A | [117] | |
| Caveolin-1 | Wistar rats MSCs | Promotes Notch pathway by maintaining Notch-1expression | N/A | [118] | |
| Drug resistance | Lipid raft | A549T | Promotes EMT-associated drug resistance | Simvastatin | [14] |
| Flotillins | HCT-15 | Promotes drug resistance | MβCD, knockdown of flotillin-1 and flotillin-2 | [134] | |
| EMT | TGF-βRII | Mv1Lu, R1B, HepG2 | Mediated TβR-II degradation to inhibit EMT by TGF/Smad pathway | Cholesterol, MβCD, nystatin | [144] |
| TGF-βRII and TGF-βRI | HeLa | Promotes TGF-βRII activate TGF-βRI to facilitate EMT by TGF/Smad pathway | MβCD, nystatin | [145] | |
| Flotillins | HCCLM3 | Promotes EMT and metastasis by activating the Akt/ Wnt/ β-catenin pathway | Knockdown of flotillin-1 and flotillin-2 | [147] | |
| Flotillin-1 | Primary Hkc, HeLa, C33A, SiHa | Promotes metastasis through Wnt/ β-catenin and NF-κB pathway-regulated EMT | Knockdown of flotillin-1 | [148] | |
| Flotillin-2, Src | CNE-1, 6–10B | Promotes metastasis through TGFβ-induced EMT | Knockdown of flotillin-2 | [149] | |
| CSC niche | VEGFR-2 | BAECs | Promote angiogenesis by ERK/ MAPK pathway | MβCD, sphingomyelinase, simvastatin | [151] |
| β1 integrin | A375 | Facilitating β1 integrin clustering to promote focal adhesion formation | MβCD | [152] | |
| CXCL4, Rac1 | EC, CE 48 T/VGH, CE 81 T/VGH, CE 146 T/VGH | Promote SDF-1α-induced invasion by Rac1/ PI3K/ Akt pathway | N/A | [153] | |
| Caveolin-1 | NIH 3T3 cells, MEFs, etc. | Promote cellular senescent to build a CSC supporting microenvironment | Knockout of caveolin-1 | [154] |
However, there are still numerous challenges in targeting the lipid raft in CSCs. How to achieve accurate drug delivery of lipid rafts in CSCs to minimize side effects remains to be determined. Although caveolin-1 and flotillin are generally recognized markers of lipid rafts [8], there are no specific markers of lipid rafts for CSCs. CSCs can be distinguished from stem cells or cancer cells if these lipid raft markers are found. An example that matches this point is the differential expression of raft-associated proteins (namely caveolin-1, flotillin-1, vimentin, galectin-3, and glyceraldehyde-3-phosphate dehydrogenase) can clearly distinguish stem cells and leukemia cells [194]. Exploring lipid raft-specific markers in CSCs that differentiate from other cells, such as cancer cells or normal stem cells, would facilitate targeted and accurate drug delivery of lipid rafts. For example, it contributes to the preparation of chemical immune conjugates, which are monoclonal antibodies that recognize CSC lipid raft-specific markers coupled with lipid raft disrupting agents.
The lipid rafts content of CSCs is higher than that of cancer cells [13]. What it means for CSCs is unclear, but it is apparent that lipid rafts contain functional CSC markers and signaling proteins necessary for CSCs. Is this elevated lipid raft phenomenon related to CSC hyperfunction? It is still a mystery. However, there is no doubt that lipid rafts are beneficial to CSCs. In turn, lipid raft disruption is detrimental to CSCs. CSCs can be cleared once targeting lipid rafts on CSCs is resolved. Interestingly, the miltefosine mentioned above preferentially targets higher lipid raft cells [13]. Lipid rafts are abundant on the membranes of CSCs, which is valuable in their elimination. Unfortunately, normal stem cells also have high lipid raft content [195]. To date, few studies compare the lipid raft content of CSCs and normal stem cells. If CSCs have a higher lipid raft content than normal stem cells, it is hypothesized that ALPs drugs can be utilized to target CSCs directly. But if CSCs have a lower or similar lipid raft content than normal stem cells, CSCs must be distinguished from normal stem cells when using ALPs. Therefore, once the selectivity issue between CSCs and normal stem cells is overcome, targeting the CSC lipid raft is feasible. Recent research has already demonstrated the ability to isolate lipid rafts from CSCs [16], which provides a technical guarantee for further investigation. The scent of victory is in the air.
Acknowledgements
Not applicable
Abbreviations
- ABC
ATP-binding cassette
- ADAMs
A disintegrin and metalloproteinases
- ALDH
Aldehyde dehydrogenase
- ALPs
Alkyl phospholipids
- BCL2
B-cell lymphoma-2
- CAFs
Cancer-associated fibroblasts
- c-MET
MET proto-oncogene
- CSCs
Cancer stem cells
- CtxB
Conjugated cholera toxin B
- CXCR4
Chemokine receptor-4
- DHH
Desert Hedgehog
- DLL
Delta-like
- ECM
Extracellular matrix
- EGFR
Epidermal growth factor receptor
- EMT
Epithelial-mesenchymal transition
- EpCAM
Epithelial cell adhesion molecule
- ERK
Extracellular regulated protein kinases
- FAK
Focal adhesion kinase
- Fz
Frizzled receptors
- GLI
Glioma-associated oncogene homolog
- GPI
Glycosylphosphatidylinositol
- Hh
Hedgehog
- HSC
Hematopoietic stem cells
- IHH
Indian Hedgehog
- JAG
Jagged
- LRP
Lipoprotein receptor-related protein
- MAPK
Mitogen-activated protein kinase
- Mdm2
Mouse double minute 2 homolog
- NICD
Notch intracellular domain
- Nrf2
Nuclear factor erythroid-2-related factor-2
- PP2A-C
Protein phosphatase 2A-C subunit
- Ptc
Patched
- SASP
Senescence-associated secretory phenotype
- SDF-1/ CXCL12
Stromal cell-derived factor 1
- SHH
Sonic Hedgehog
- Smo
Smoothened
- TGF-β
Transforming growth factor-β
- TGF-βRI
TGF-β receptor I
- TGF-βRII
TGF-β receptor II
- TME
Tumor microenvironment
- TrxR1
Thioredoxin reductase 1
- VEGF
Vascular endothelial growth factor A
- VEGFR-2
VEGF receptor-2
Author contributions
SZ is a major contributor to writing the manuscript. NZ, JG, CJZ, and HFL assisted with the format of the manuscript. LQ and DFL revised the manuscript and supervised the work. LQ has given final approval to the version to be published. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Sciences Foundation of China [Grant Number 81973668, 81774130]; the Key Project of the Educational Department of Hunan Province [Grant Number 20A375]; Pharmaceutical Open Fund of Domestic First-class Disciplines (cultivation) of Hunan Province [Grant Number 2021YX07]; the Scientific Research Project of Changsha Science and Technology Bureau [Grant Number kq2004060]; Key Project of Hunan Provincial Health Commission [Grant Number202213055529]; Natural Science Foundation of Hunan Province [Grant Number 2022JJ80088]; the Graduate Research innovation project of Hunan University of Chinese Medicine [Grant Number 2021CX48, 2021CX08] and the First-Class Discipline of Pharmaceutical Science of Hunan.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England). 2018;392(10159):1736–88. [DOI] [PMC free article] [PubMed]
- 2.Li L, Bhatia R. Stem cell quiescence. Clin Cancer Res: An Off J Am Assoc Cancer Res. 2011;17(15):4936–4941. doi: 10.1158/1078-0432.CCR-10-1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mollinedo F, Gajate C. Lipid rafts as major platforms for signaling regulation in cancer. Adv Biol Regul. 2015;57:130–146. doi: 10.1016/j.jbior.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Mollinedo F, Gajate C. Lipid rafts as signaling hubs in cancer cell survival/death and invasion: implications in tumor progression and therapy: thematic review series: biology of lipid rafts. J Lipid Res. 2020;61(5):611–635. doi: 10.1194/jlr.TR119000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simons K, Ikonen E. Functional rafts in cell membranes. Nature. 1997;387(6633):569–572. doi: 10.1038/42408. [DOI] [PubMed] [Google Scholar]
- 6.Pike LJ. Rafts defined: a report on the keystone symposium on lipid rafts and cell function. J Lipid Res. 2006;47(7):1597–1598. doi: 10.1194/jlr.E600002-JLR200. [DOI] [PubMed] [Google Scholar]
- 7.Lingwood D, Simons K. Lipid rafts as a membrane-organizing principle. Science (New York, N.Y.) 2010;327(5961):46–50. doi: 10.1126/science.1174621. [DOI] [PubMed] [Google Scholar]
- 8.Yokoyama H, Matsui I. The lipid raft markers stomatin, prohibitin, flotillin, and HflK/C (SPFH)-domain proteins form an operon with NfeD proteins and function with apolar polyisoprenoid lipids. Crit Rev Microbiol. 2020;46(1):38–48. doi: 10.1080/1040841X.2020.1716682. [DOI] [PubMed] [Google Scholar]
- 9.Rothberg KG, Heuser JE, Donzell WC, Ying YS, Glenney JR, Anderson RG. Caveolin, a protein component of caveolae membrane coats. Cell. 1992;68(4):673–682. doi: 10.1016/0092-8674(92)90143-Z. [DOI] [PubMed] [Google Scholar]
- 10.Gauthier-Rouvière C, Bodin S, Comunale F, Planchon D. Flotillin membrane domains in cancer. Cancer Metastasis Rev. 2020;39(2):361–374. doi: 10.1007/s10555-020-09873-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li YC, Park MJ, Ye S, Kim C, Kim Y. Elevated levels of cholesterol-rich lipid rafts in cancer cells are correlated with apoptosis sensitivity induced by cholesterol-depleting agents. The Am J Pathol. 2006;168(4):1107–1118. doi: 10.2353/ajpath.2006.050959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levin-Gromiko U, Koshelev V, Kushnir P, Fedida-Metula S, Voronov E, Fishman D. Amplified lipid rafts of malignant cells constitute a target for inhibition of aberrantly active NFAT and melanoma tumor growth by the aminobisphosphonate zoledronic acid. Carcinogenesis. 2014;35(11):2555–2566. doi: 10.1093/carcin/bgu178. [DOI] [PubMed] [Google Scholar]
- 13.Park S, Kim J, Choi J, Lee C, Lee W, Park S, et al. Lipid raft-disrupting miltefosine preferentially induces the death of colorectal cancer stem-like cells. Clin Transl Med. 2021;11(11):e552. doi: 10.1002/ctm2.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta VK, Sharma NS, Kesh K, Dauer P, Nomura A, Giri B, et al. Metastasis and chemoresistance in CD133 expressing pancreatic cancer cells are dependent on their lipid raft integrity. Cancer Lett. 2018;439:101–112. doi: 10.1016/j.canlet.2018.09.028. [DOI] [PubMed] [Google Scholar]
- 15.Zhang C, Zhu N, Wang Y, Liu L, Zhao T, Wu H, et al. Celastrol attenuates lipid accumulation and stemness of clear cell renal cell carcinoma via CAV-1/LOX-1 pathway. Front Pharmacol. 2021;12:658092. doi: 10.3389/fphar.2021.658092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta VK, Banerjee S. Isolation of lipid raft proteins from CD133+ cancer stem cells. Methods Mol Biol (Clifton, N.J.) 2017;1609:25–31. doi: 10.1007/978-1-4939-6996-8_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Toole BP. The CD147-hyaluronan axis in cancer. Anat Rec (Hoboken, N.J.) 2020;303(6):1573–1583. doi: 10.1002/ar.24147. [DOI] [PubMed] [Google Scholar]
- 18.Saygin C, Wiechert A, Rao VS, Alluri R, Connor E, Thiagarajan PS, et al. CD55 regulates self-renewal and cisplatin resistance in endometrioid tumors. J Exp Med. 2017;214(9):2715–2732. doi: 10.1084/jem.20170438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karbanová J, Lorico A, Bornhäuser M, Corbeil D, Fargeas CA. Prominin-1/CD133: lipid raft association, detergent resistance, and Immunodetection. Stem Cells Transl Med. 2018;7(2):155–160. doi: 10.1002/sctm.17-0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clarke MF, Dick JE, Dirks PB, Eaves CJ, Jamieson CHM, Jones DL, et al. Cancer stem cells–perspectives on current status and future directions: AACR Workshop on cancer stem cells. Cancer Res. 2006;66(19):9339–9344. doi: 10.1158/0008-5472.CAN-06-3126. [DOI] [PubMed] [Google Scholar]
- 21.Valent P, Bonnet D, De Maria R, Lapidot T, Copland M, Melo JV, et al. Cancer stem cell definitions and terminology: the devil is in the details. Nat Rev Cancer. 2012;12(11):767–775. doi: 10.1038/nrc3368. [DOI] [PubMed] [Google Scholar]
- 22.Lapidot T, Sirard C, Vormoor J, Murdoch B, Hoang T, Caceres-Cortes J, et al. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature. 1994;367(6464):645–648. doi: 10.1038/367645a0. [DOI] [PubMed] [Google Scholar]
- 23.Lathia JD, Mack SC, Mulkearns-Hubert EE, Valentim CLL, Rich JN. Cancer stem cells in glioblastoma. Gene Dev. 2015;29(12):1203–1217. doi: 10.1101/gad.261982.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeuner A, Todaro M, Stassi G, De Maria R. Colorectal cancer stem cells: from the crypt to the clinic. Cell Stem Cell. 2014;15(6):692–705. doi: 10.1016/j.stem.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 25.Brown HK, Tellez-Gabriel M, Heymann D. Cancer stem cells in osteosarcoma. Cancer Lett. 2017;386:189–195. doi: 10.1016/j.canlet.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 26.Hua Z, White J, Zhou J. Cancer stem cells in TNBC. Semin Cancer Biol. 2022;82:26–34. doi: 10.1016/j.semcancer.2021.06.015. [DOI] [PubMed] [Google Scholar]
- 27.Shimokawa M, Ohta Y, Nishikori S, Matano M, Takano A, Fujii M, et al. Visualization and targeting of LGR5(+) human colon cancer stem cells. Nature. 2017;545(7653):187–192. doi: 10.1038/nature22081. [DOI] [PubMed] [Google Scholar]
- 28.Li JJ, Shen MM. Prostate stem cells and cancer stem cells. CSH Perspect Med. 2019 doi: 10.1101/cshperspect.a030395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin R. Thyroid cancer stem cells. Nat Rev Endocrinol. 2011;7(10):609–616. doi: 10.1038/nrendo.2011.127. [DOI] [PubMed] [Google Scholar]
- 30.Ng A, Barker N. Ovary and fimbrial stem cells: biology, niche and cancer origins. Nat Rev Mol Cell Biol. 2015;16(10):625–638. doi: 10.1038/nrm4056. [DOI] [PubMed] [Google Scholar]
- 31.Li C, Heidt DG, Dalerba P, Burant CF, Zhang L, Adsay V, et al. Identification of pancreatic cancer stem cells. Cancer Res. 2007;67(3):1030–1037. doi: 10.1158/0008-5472.CAN-06-2030. [DOI] [PubMed] [Google Scholar]
- 32.Prince ME, Sivanandan R, Kaczorowski A, Wolf GT, Kaplan MJ, Dalerba P, et al. Identification of a subpopulation of cells with cancer stem cell properties in head and neck squamous cell carcinoma. P Natl Acad Sci USA. 2007;104(3):973–978. doi: 10.1073/pnas.0610117104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ginestier C, Hur MH, Charafe-Jauffret E, Monville F, Dutcher J, Brown M, et al. ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell. 2007;1(5):555–567. doi: 10.1016/j.stem.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, et al. Identification of human brain tumour initiating cells. Nature. 2004;432(7015):396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 35.Saygin C, Matei D, Majeti R, Reizes O, Lathia JD. Targeting cancer stemness in the clinic: from hype to hope. Cell Stem Cell. 2019;24(1):25–40. doi: 10.1016/j.stem.2018.11.017. [DOI] [PubMed] [Google Scholar]
- 36.Yin AH, Miraglia S, Zanjani ED, Almeida-Porada G, Ogawa M, Leary AG, et al. AC133, a novel marker for human hematopoietic stem and progenitor cells. Blood. 1997;90(12):5002–5012. doi: 10.1182/blood.V90.12.5002. [DOI] [PubMed] [Google Scholar]
- 37.Grosse-Gehling P, Fargeas CA, Dittfeld C, Garbe Y, Alison MR, Corbeil D, et al. CD133 as a biomarker for putative cancer stem cells in solid tumours: limitations, problems and challenges. J Pathol. 2013;229(3):355–378. doi: 10.1002/path.4086. [DOI] [PubMed] [Google Scholar]
- 38.Chen K, Guo Y, Li L, Qu S, Zhao W, Lu Q, et al. Cancer stem cell-like characteristics and telomerase activity of the nasopharyngeal carcinoma radioresistant cell line CNE-2R. Cancer Med-US. 2018;7(9):4755–4764. doi: 10.1002/cam4.1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang X, Komaki R, Wang L, Fang B, Chang JY. Treatment of radioresistant stem-like esophageal cancer cells by an apoptotic gene-armed, telomerase-specific oncolytic adenovirus. Clin Cancer Res: An Off J Am Assoc Cancer Res. 2008;14(9):2813–2823. doi: 10.1158/1078-0432.CCR-07-1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beck B, Blanpain C. Unravelling cancer stem cell potential. Nat Rev Cancer. 2013;13(10):727–738. doi: 10.1038/nrc3597. [DOI] [PubMed] [Google Scholar]
- 41.Clevers H. The cancer stem cell: premises, promises and challenges. Nat Med. 2011;17(3):313–319. doi: 10.1038/nm.2304. [DOI] [PubMed] [Google Scholar]
- 42.Batlle E, Clevers H. Cancer stem cells revisited. Nat Med. 2017;23(10):1124–1134. doi: 10.1038/nm.4409. [DOI] [PubMed] [Google Scholar]
- 43.Bai X, Ni J, Beretov J, Graham P, Li Y. Cancer stem cell in breast cancer therapeutic resistance. Cancer Treat Rev. 2018;69:152–163. doi: 10.1016/j.ctrv.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 44.Chen K, Zhang C, Ling S, Wei R, Wang J, Xu X. The metabolic flexibility of quiescent CSC: implications for chemotherapy resistance. Cell Death Dis. 2021;12(9):835. doi: 10.1038/s41419-021-04116-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang Z, Wu T, Liu AY, Ouyang G. Differentiation and transdifferentiation potentials of cancer stem cells. Oncotarget. 2015;6(37):39550–39563. doi: 10.18632/oncotarget.6098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu S, Cong Y, Wang D, Sun Y, Deng L, Liu Y, et al. Breast cancer stem cells transition between epithelial and mesenchymal states reflective of their normal counterparts. Stem Cell Rep. 2014;2(1):78–91. doi: 10.1016/j.stemcr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ricci-Vitiani L, Pallini R, Biffoni M, Todaro M, Invernici G, Cenci T, et al. Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature. 2010;468(7325):824–828. doi: 10.1038/nature09557. [DOI] [PubMed] [Google Scholar]
- 48.Cheng L, Huang Z, Zhou W, Wu Q, Donnola S, Liu JK, et al. Glioblastoma stem cells generate vascular pericytes to support vessel function and tumor growth. Cell. 2013;153(1):139–152. doi: 10.1016/j.cell.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Friedmann-Morvinski D, Bushong EA, Ke E, Soda Y, Marumoto T, Singer O, et al. Dedifferentiation of neurons and astrocytes by oncogenes can induce gliomas in mice. Science (New York, N.Y.) 2012;338(6110):1080–1084. doi: 10.1126/science.1226929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schwitalla S, Fingerle AA, Cammareri P, Nebelsiek T, Göktuna SI, Ziegler PK, et al. Intestinal tumorigenesis initiated by dedifferentiation and acquisition of stem-cell-like properties. Cell. 2013;152(1–2):25–38. doi: 10.1016/j.cell.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 51.Kim W, Ryu CJ. Cancer stem cell surface markers on normal stem cells. BMB Rep. 2017;50(6):285–298. doi: 10.5483/BMBRep.2017.50.6.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Driessens G, Beck B, Caauwe A, Simons BD, Blanpain C. Defining the mode of tumour growth by clonal analysis. Nature. 2012;488(7412):527–530. doi: 10.1038/nature11344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walcher L, Kistenmacher A, Suo H, Kitte R, Dluczek S, Strauß A, et al. Cancer stem cells-origins and biomarkers: perspectives for targeted personalized therapies. Front Immunol. 2020;11:1280. doi: 10.3389/fimmu.2020.01280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gombos I, Steinbach G, Pomozi I, Balogh A, Vámosi G, Gansen A, et al. Some new faces of membrane microdomains: a complex confocal fluorescence, differential polarization, and FCS imaging study on live immune cells. Cytometry A. 2008;73(3):220–229. doi: 10.1002/cyto.a.20516. [DOI] [PubMed] [Google Scholar]
- 55.Bahnassy AA, Fawzy M, El-Wakil M, Zekri AN, Abdel-Sayed A, Sheta M. Aberrant expression of cancer stem cell markers (CD44, CD90, and CD133) contributes to disease progression and reduced survival in hepatoblastoma patients: 4-year survival data. Transl Res: The J Lab Clin Med. 2015;165(3):396–406. doi: 10.1016/j.trsl.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 56.Lesley J, Hyman R. CD44 structure and function. Front Biosci. 1998;3:d616–d630. doi: 10.2741/A306. [DOI] [PubMed] [Google Scholar]
- 57.Yu X, Wang J, Feizpour A, Reinhard BM. Illuminating the lateral organization of cell-surface CD24 and CD44 through plasmon coupling between Au nanoparticle immunolabels. Anal Chem. 2013;85(3):1290–1294. doi: 10.1021/ac303310j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ooki A, VandenBussche CJ, Kates M, Hahn NM, Matoso A, McConkey DJ, et al. CD24 regulates cancer stem cell (CSC)-like traits and a panel of CSC-related molecules serves as a non-invasive urinary biomarker for the detection of bladder cancer. Br J Cancer. 2018;119(8):961–970. doi: 10.1038/s41416-018-0291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baumann P, Thiele W, Cremers N, Muppala S, Krachulec J, Diefenbacher M, et al. CD24 interacts with and promotes the activity of c-src within lipid rafts in breast cancer cells, thereby increasing integrin-dependent adhesion. Cell Mol Life Sci: CMLS. 2012;69(3):435–448. doi: 10.1007/s00018-011-0756-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ono YJ, Tanabe A, Tanaka T, Tanaka Y, Hayashi M, Terai Y, et al. Met signaling cascade is amplified by the recruitment of phosphorylated met to lipid rafts via CD24 and leads to drug resistance in endometrial cancer cell lines. Mol Cancer Ther. 2015;14(10):2353–2363. doi: 10.1158/1535-7163.MCT-15-0187. [DOI] [PubMed] [Google Scholar]
- 61.Naor D, Sionov RV, Ish-Shalom D. CD44: structure, function, and association with the malignant process. Adv Cancer Res. 1997;71:241–319. doi: 10.1016/S0065-230X(08)60101-3. [DOI] [PubMed] [Google Scholar]
- 62.Aruffo A, Stamenkovic I, Melnick M, Underhill CB, Seed B. CD44 is the principal cell surface receptor for hyaluronate. Cell. 1990;61(7):1303–1313. doi: 10.1016/0092-8674(90)90694-A. [DOI] [PubMed] [Google Scholar]
- 63.Chanmee T, Ontong P, Kimata K, Itano N. Key roles of hyaluronan and its CD44 receptor in the stemness and survival of cancer stem cells. Front Oncol. 2015;5:180. doi: 10.3389/fonc.2015.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ. Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res. 2005;65(23):10946–10951. doi: 10.1158/0008-5472.CAN-05-2018. [DOI] [PubMed] [Google Scholar]
- 65.Zhang C, Zhu N, Liu C, Wu H, Yin Y, Shi Y, et al. Steroid receptor RNA activator inhibits the migration, invasion and stemness characteristics of renal cell carcinoma cells. Int J Mol Med. 2020;46(5):1765–1776. doi: 10.3892/ijmm.2020.4730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Oliferenko S, Paiha K, Harder T, Gerke V, Schwärzler C, Schwarz H, et al. Analysis of CD44-containing lipid rafts: Recruitment of annexin II and stabilization by the actin cytoskeleton. J Cell Biol. 1999;146(4):843–854. doi: 10.1083/jcb.146.4.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wei Q, Zhang F, Richardson MM, Roy NH, Rodgers W, Liu Y, et al. CD82 restrains pathological angiogenesis by altering lipid raft clustering and CD44 trafficking in endothelial cells. Circulation. 2014;130(17):1493–1504. doi: 10.1161/CIRCULATIONAHA.114.011096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Donatello S, Babina IS, Hazelwood LD, Hill ADK, Nabi IR, Hopkins AM. Lipid raft association restricts CD44-ezrin interaction and promotion of breast cancer cell migration. Am J Pathol. 2012;181(6):2172–2187. doi: 10.1016/j.ajpath.2012.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee J, Wang M, Sudhir P, Chen J. CD44 engagement promotes matrix-derived survival through the CD44-SRC-integrin axis in lipid rafts. Mol Cell Biol. 2008;28(18):5710–5723. doi: 10.1128/MCB.00186-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thankamony SP, Knudson W. Acylation of CD44 and its association with lipid rafts are required for receptor and hyaluronan endocytosis. J Biol Chem. 2006;281(45):34601–34609. doi: 10.1074/jbc.M601530200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Grass GD, Dai L, Qin Z, Parsons C, Toole BP. CD147: regulator of hyaluronan signaling in invasiveness and chemoresistance. Adv Cancer Res. 2014;123:351–373. doi: 10.1016/B978-0-12-800092-2.00013-7. [DOI] [PubMed] [Google Scholar]
- 72.Murai T, Maruyama Y, Mio K, Nishiyama H, Suga M, Sato C. Low cholesterol triggers membrane microdomain-dependent CD44 shedding and suppresses tumor cell migration. J Biol Chem. 2011;286(3):1999–2007. doi: 10.1074/jbc.M110.184010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang H, Gong P, Li J, Fu Y, Zhou Z, Liu L. Role of CD133 in human embryonic stem cell proliferation and teratoma formation. Stem Cell Res Ther. 2020;11(1):208. doi: 10.1186/s13287-020-01729-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jang J, Song Y, Kim S, Kim J, Seo HR. Potential mechanisms of CD133 in cancer stem cells. Life Sci. 2017;184:25–29. doi: 10.1016/j.lfs.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 75.Liu F, Qian Y. The role of CD133 in hepatocellular carcinoma. Cancer Biol Ther. 2021;22(4):291–300. doi: 10.1080/15384047.2021.1916381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Giebel B, Corbeil D, Beckmann J, Höhn J, Freund D, Giesen K, et al. Segregation of lipid raft markers including CD133 in polarized human hematopoietic stem and progenitor cells. Blood. 2004;104(8):2332–2338. doi: 10.1182/blood-2004-02-0511. [DOI] [PubMed] [Google Scholar]
- 77.Chen Y, Wu M, Huang C, Lin S, Chuang T, Yu C, et al. CD133/Src axis mediates tumor initiating property and epithelial-mesenchymal transition of head and neck cancer. PLoS ONE. 2011;6(11):e28053. doi: 10.1371/journal.pone.0028053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liu C, Li Y, Xing Y, Cao B, Yang F, Yang T, et al. The Interaction between cancer stem cell marker CD133 and Src protein promotes focal adhesion kinase (FAK) phosphorylation and cell migration. J Biol Chem. 2016;291(30):15540–15550. doi: 10.1074/jbc.M115.712976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Su Y, Lin W, Chang Y, Wei K, Liang C, Chen S, et al. Polarized cell migration induces cancer type-specific CD133/integrin/Src/Akt/GSK3β/β-catenin signaling required for maintenance of cancer stem cell properties. Oncotarget. 2015;6(35):38029–38045. doi: 10.18632/oncotarget.5703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Teicher BA, Fricker SP. CXCL12 (SDF-1)/CXCR4 pathway in cancer. Clin Cancer Res: An Off J Am Assoc Cancer Res. 2010;16(11):2927–2931. doi: 10.1158/1078-0432.CCR-09-2329. [DOI] [PubMed] [Google Scholar]
- 81.Sun Y, Yoshida T, Okabe M, Zhou K, Wang F, Soko C, et al. Isolation of stem-like cancer cells in primary endometrial cancer using cell surface markers CD133 and CXCR4. Transl Oncol. 2017;10(6):976–987. doi: 10.1016/j.tranon.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, et al. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1(3):313–323. doi: 10.1016/j.stem.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 83.Mardani A, Gheytanchi E, Mousavie SH, Madjd Jabari Z, Shooshtarizadeh T. Clinical significance of cancer stem cell markers CD133 and CXCR4 in osteosarcomas. Asian Pac J Cancer Prev: APJCP. 2020;21(1):67–73. doi: 10.31557/APJCP.2020.21.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cheng C, Liao W, Chen P, Yu J, Shiau H, Hsieh Y, et al. MiR-139 modulates cancer stem cell function of human breast cancer through targeting CXCR4. Cancers. 2021 doi: 10.3390/cancers13112582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cheng Y, Song Y, Qu J, Che X, Song N, Fan Y, et al. The chemokine receptor CXCR4 and c-MET cooperatively promote epithelial-mesenchymal transition in gastric cancer cells. Transl Oncol. 2018;11(2):487–497. doi: 10.1016/j.tranon.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.He S, Nakada D, Morrison SJ. Mechanisms of stem cell self-renewal. Ann Rev Cell Dev Bi. 2009;25:377–406. doi: 10.1146/annurev.cellbio.042308.113248. [DOI] [PubMed] [Google Scholar]
- 87.O’Brien CA, Kreso A, Jamieson CHM. Cancer stem cells and self-renewal. Clin Cancer Res: An Off J Am Assoc Cancer Res. 2010;16(12):3113–3120. doi: 10.1158/1078-0432.CCR-09-2824. [DOI] [PubMed] [Google Scholar]
- 88.Takebe N, Harris PJ, Warren RQ, Ivy SP. Targeting cancer stem cells by inhibiting Wnt, Notch, and Hedgehog pathways. Nat Rev Clin Oncol. 2011;8(2):97–106. doi: 10.1038/nrclinonc.2010.196. [DOI] [PubMed] [Google Scholar]
- 89.Clara JA, Monge C, Yang Y, Takebe N. Targeting signalling pathways and the immune microenvironment of cancer stem cells - a clinical update. Nat Rev Clin Oncol. 2020;17(4):204–232. doi: 10.1038/s41571-019-0293-2. [DOI] [PubMed] [Google Scholar]
- 90.Fu X, Zhu X, Qin F, Zhang Y, Lin J, Ding Y, et al. Linc00210 drives Wnt/β-catenin signaling activation and liver tumor progression through CTNNBIP1-dependent manner. Mol Cancer. 2018;17(1):73. doi: 10.1186/s12943-018-0783-3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 91.Zhang K, Guo Y, Wang X, Zhao H, Ji Z, Cheng C, et al. WNT/β-catenin directs self-renewal symmetric cell division of hTERT(high) prostate cancer stem cells. Cancer Res. 2017;77(9):2534–2547. doi: 10.1158/0008-5472.CAN-16-1887. [DOI] [PubMed] [Google Scholar]
- 92.Li Y, Zhang T, Korkaya H, Liu S, Lee H, Newman B, et al. Sulforaphane, a dietary component of broccoli/broccoli sprouts, inhibits breast cancer stem cells. Clin Cancer Res: An Off J Am Assoc Cancer Res. 2010;16(9):2580–2590. doi: 10.1158/1078-0432.CCR-09-2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen J, Luo X, Xiang L, Li H, Zha L, Li N, et al. EZH2 promotes colorectal cancer stem-like cell expansion by activating p21cip1-Wnt/β-catenin signaling. Oncotarget. 2016;7(27):41540–41558. doi: 10.18632/oncotarget.9236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang Y, Krivtsov AV, Sinha AU, North TE, Goessling W, Feng Z, et al. The Wnt/beta-catenin pathway is required for the development of leukemia stem cells in AML. Science (New York, N.Y.) 2010;327(5973):1650–1653. doi: 10.1126/science.1186624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yan H, Wang Z, Sun Y, Hu L, Bu P. Cytoplasmic NEAT1 Suppresses AML Stem Cell Self-Renewal and Leukemogenesis through Inactivation of Wnt Signaling. Adv Sci (Weinheim, Baden-Wurttemberg, Germany) 2021;8(22):2100914. doi: 10.1002/advs.202100914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Clevers H, Loh KM, Nusse R. Stem cell signaling. An integral program for tissue renewal and regeneration: Wnt signaling and stem cell control. Science (New York, N.Y.). 2014;346(6205):1248012. [DOI] [PubMed]
- 97.Matsui WH. Cancer stem cell signaling pathways. Medicine. 2016;95(1 Suppl 1):S8–19. doi: 10.1097/MD.0000000000004765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sato A, Yamamoto H, Sakane H, Koyama H, Kikuchi A. Wnt5a regulates distinct signalling pathways by binding to Frizzled2. EMBO J. 2010;29(1):41–54. doi: 10.1038/emboj.2009.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Özhan G, Sezgin E, Wehner D, Pfister AS, Kühl SJ, Kagermeier-Schenk B, et al. Lypd6 enhances Wnt/β-catenin signaling by promoting Lrp6 phosphorylation in raft plasma membrane domains. Dev Cell. 2013;26(4):331–345. doi: 10.1016/j.devcel.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 100.Sezgin E, Azbazdar Y, Ng XW, Teh C, Simons K, Weidinger G, et al. Binding of canonical Wnt ligands to their receptor complexes occurs in ordered plasma membrane environments. FEBS J. 2017;284(15):2513–2526. doi: 10.1111/febs.14139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Haack F, Köster T, Uhrmacher AM. Receptor/Raft ratio is a determinant for LRP6 phosphorylation and WNT/β-Catenin signaling. Front cell Dev Biol. 2021;9:706731. doi: 10.3389/fcell.2021.706731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Newcomb CJ, Sur S, Lee SS, Yu JM, Zhou Y, Snead ML, et al. Supramolecular nanofibers enhance growth factor signaling by increasing lipid raft mobility. Nano Lett. 2016;16(5):3042–3050. doi: 10.1021/acs.nanolett.6b00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cochrane CR, Szczepny A, Watkins DN, Cain JE. Hedgehog signaling in the maintenance of cancer stem cells. Cancers. 2015;7(3):1554–1585. doi: 10.3390/cancers7030851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rohatgi R, Scott MP. Patching the gaps in Hedgehog signalling. Nat Cell Biol. 2007;9(9):1005–1009. doi: 10.1038/ncb435. [DOI] [PubMed] [Google Scholar]
- 105.Sigafoos AN, Paradise BD, Fernandez-Zapico ME. Hedgehog/GLI signaling pathway: transduction, regulation, and implications for disease. Cancers. 2021 doi: 10.3390/cancers13143410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Clement V, Sanchez P, de Tribolet N, Radovanovic I, RuiziAltaba A. HEDGEHOG-GLI1 signaling regulates human glioma growth, cancer stem cell self-renewal, and tumorigenicity. Curr Biol: CB. 2007;17(2):165–172. doi: 10.1016/j.cub.2006.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Shi D, Lv X, Zhang Z, Yang X, Zhou Z, Zhang L, et al. Smoothened oligomerization/higher order clustering in lipid rafts is essential for high Hedgehog activity transduction. J Biol Chem. 2013;288(18):12605–12614. doi: 10.1074/jbc.M112.399477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Karpen HE, Bukowski JT, Hughes T, Gratton JP, Sessa WC, Gailani MR. The sonic hedgehog receptor patched associates with caveolin-1 in cholesterol-rich microdomains of the plasma membrane. J Biol Chem. 2001;276(22):19503–19511. doi: 10.1074/jbc.M010832200. [DOI] [PubMed] [Google Scholar]
- 109.Luo Y, Wan G, Zhang X, Zhou X, Wang Q, Fan J, et al. Cryo-EM study of patched in lipid nanodisc suggests a structural basis for its clustering in caveolae. Structure (London, England: 1993) 2021;29(11):1286–1294. doi: 10.1016/j.str.2021.06.004. [DOI] [PubMed] [Google Scholar]
- 110.Mao H, Diehl AM, Li Y. Sonic hedgehog ligand partners with caveolin-1 for intracellular transport. Lab Investig; A J Tech Methods Pathol. 2009;89(3):290–300. doi: 10.1038/labinvest.2008.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Artavanis-Tsakonas S, Rand MD, Lake RJ. Notch signaling: cell fate control and signal integration in development. Science (New York, N.Y.) 1999;284(5415):770–776. doi: 10.1126/science.284.5415.770. [DOI] [PubMed] [Google Scholar]
- 112.Kopan R, Ilagan MXG. The canonical Notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137(2):216–233. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rajakulendran N, Rowland KJ, Selvadurai HJ, Ahmadi M, Park NI, Naumenko S, et al. Wnt and Notch signaling govern self-renewal and differentiation in a subset of human glioblastoma stem cells. Gene Dev. 2019;33(9–10):498–510. doi: 10.1101/gad.321968.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sikandar SS, Pate KT, Anderson S, Dizon D, Edwards RA, Waterman ML, et al. NOTCH signaling is required for formation and self-renewal of tumor-initiating cells and for repression of secretory cell differentiation in colon cancer. Cancer Res. 2010;70(4):1469–1478. doi: 10.1158/0008-5472.CAN-09-2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Osenkowski P, Ye W, Wang R, Wolfe MS, Selkoe DJ. Direct and potent regulation of gamma-secretase by its lipid microenvironment. J Biol Chem. 2008;283(33):22529–22540. doi: 10.1074/jbc.M801925200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Urano Y, Hayashi I, Isoo N, Reid PC, Shibasaki Y, Noguchi N, et al. Association of active gamma-secretase complex with lipid rafts. J Lipid Res. 2005;46(5):904–912. doi: 10.1194/jlr.M400333-JLR200. [DOI] [PubMed] [Google Scholar]
- 117.Danza G, Di Serio C, Ambrosio MR, Sturli N, Lonetto G, Rosati F, et al. Notch3 is activated by chronic hypoxia and contributes to the progression of human prostate cancer. Int J Cancer. 2013;133(11):2577–2586. doi: 10.1002/ijc.28293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang S, Kan Q, Sun Y, Han R, Zhang G, Peng T, et al. Caveolin-1 regulates neural differentiation of rat bone mesenchymal stem cells into neurons by modulating Notch signaling. Int J Dev Neurosci : The Off J Int Soc Dev Neurosci. 2013;31(1):30–35. doi: 10.1016/j.ijdevneu.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 119.Hatch E, Morrow D, Liu W, Cahill PA, Redmond EM. Ethanol inhibits γ-secretase proteolytic activity in vascular smooth muscle cells. Alcohol Clin Exp Res. 2015;39(11):2115–2122. doi: 10.1111/acer.12875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lukacik P, Roversi P, White J, Esser D, Smith GP, Billington J, et al. Complement regulation at the molecular level: the structure of decay-accelerating factor. P Natl Acad Sci USA. 2004;101(5):1279–1284. doi: 10.1073/pnas.0307200101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Steinbichler TB, Dudás J, Skvortsov S, Ganswindt U, Riechelmann H, Skvortsova I. Therapy resistance mediated by cancer stem cells. Semin Cancer Biol. 2018;53:156–167. doi: 10.1016/j.semcancer.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 122.Fuchs E, Tumbar T, Guasch G. Socializing with the neighbors: stem cells and their niche. Cell. 2004;116(6):769–778. doi: 10.1016/S0092-8674(04)00255-7. [DOI] [PubMed] [Google Scholar]
- 123.Vannini N, Roch A, Naveiras O, Griffa A, Kobel S, Lutolf MP. Identification of in vitro HSC fate regulators by differential lipid raft clustering. Cell Cycle (Georgetown, Tex.) 2012;11(8):1535–1543. doi: 10.4161/cc.19900. [DOI] [PubMed] [Google Scholar]
- 124.Lagadinou ED, Sach A, Callahan K, Rossi RM, Neering SJ, Minhajuddin M, et al. BCL-2 inhibition targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells. Cell Stem Cell. 2013;12(3):329–341. doi: 10.1016/j.stem.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ozsvari B, Bonuccelli G, Sanchez-Alvarez R, Foster R, Sotgia F, Lisanti MP. Targeting flavin-containing enzymes eliminates cancer stem cells (CSCs), by inhibiting mitochondrial respiration: vitamin B2 (Riboflavin) in cancer therapy. Aging. 2017;9(12):2610–2628. doi: 10.18632/aging.101351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yamazaki S, Iwama A, Morita Y, Eto K, Ema H, Nakauchi H. Cytokine signaling, lipid raft clustering, and HSC hibernation. Ann NY Acad Sci. 2007;1106:54–63. doi: 10.1196/annals.1392.017. [DOI] [PubMed] [Google Scholar]
- 127.Huang Q, Shen H, Shui G, Wenk MR, Ong C. Emodin inhibits tumor cell adhesion through disruption of the membrane lipid Raft-associated integrin signaling pathway. Cancer Res. 2006;66(11):5807–5815. doi: 10.1158/0008-5472.CAN-06-0077. [DOI] [PubMed] [Google Scholar]
- 128.Garcia-Mayea Y, Mir C, Masson F, Paciucci R, LLeonart ME. Insights into new mechanisms and models of cancer stem cell multidrug resistance. Semin Cancer Biol. 2020;60:166–180. doi: 10.1016/j.semcancer.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 129.Begicevic R, Falasca M. ABC transporters in cancer stem cells: beyond chemoresistance. Int J Mol Sci. 2017;18(11):2362. doi: 10.3390/ijms18112362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.El-Khattouti A, Sheehan NT, Monico J, Drummond HA, Haikel Y, Brodell RT, et al. CD133+ melanoma subpopulation acquired resistance to caffeic acid phenethyl ester-induced apoptosis is attributed to the elevated expression of ABCB5: significance for melanoma treatment. Cancer Lett. 2015;357(1):83–104. doi: 10.1016/j.canlet.2014.10.043. [DOI] [PubMed] [Google Scholar]
- 131.Lee CAA, Banerjee P, Wilson BJ, Wu S, Guo Q, Berg G, et al. Targeting the ABC transporter ABCB5 sensitizes glioblastoma to temozolomide-induced apoptosis through a cell-cycle checkpoint regulation mechanism. J Biol Chem. 2020;295(22):7774–7788. doi: 10.1074/jbc.RA120.013778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Klappe K, Hummel I, Hoekstra D, Kok JW. Lipid dependence of ABC transporter localization and function. Chem Phys Lipids. 2009;161(2):57–64. doi: 10.1016/j.chemphyslip.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 133.Jin H, He Y, Zhao P, Hu Y, Tao J, Chen J, et al. Targeting lipid metabolism to overcome EMT-associated drug resistance via integrin β3/FAK pathway and tumor-associated macrophage repolarization using legumain-activatable delivery. Theranostics. 2019;9(1):265–278. doi: 10.7150/thno.27246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ye DM, Ye SC, Yu SQ, Shu FF, Xu SS, Chen QQ, et al. Drug-resistance reversal in colorectal cancer cells by destruction of flotillins, the key lipid rafts proteins. Neoplasma. 2019;66(4):576–583. doi: 10.4149/neo_2018_180820N633. [DOI] [PubMed] [Google Scholar]
- 135.Nieto MA, Huang RY, Jackson RA, Thiery JP. EMT: 2016. Cell. 2016;166(1):21–45. doi: 10.1016/j.cell.2016.06.028. [DOI] [PubMed] [Google Scholar]
- 136.Brabletz T, Kalluri R, Nieto MA, Weinberg RA. EMT in cancer. Nat Rev Cancer. 2018;18(2):128–134. doi: 10.1038/nrc.2017.118. [DOI] [PubMed] [Google Scholar]
- 137.Wilson MM, Weinberg RA, Lees JA, Guen VJ. Emerging mechanisms by which EMT programs control stemness. Trends in cancer. 2020;6(9):775–780. doi: 10.1016/j.trecan.2020.03.011. [DOI] [PubMed] [Google Scholar]
- 138.Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009;9(4):265–273. doi: 10.1038/nrc2620. [DOI] [PubMed] [Google Scholar]
- 139.Mani SA, Guo W, Liao M, Eaton EN, Ayyanan A, Zhou AY, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133(4):704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tisza MJ, Zhao W, Fuentes JSR, Prijic S, Chen X, Levental I, et al. Motility and stem cell properties induced by the epithelial-mesenchymal transition require destabilization of lipid rafts. Oncotarget. 2016;7(32):51553–51568. doi: 10.18632/oncotarget.9928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Xu J, Lamouille S, Derynck R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 2009;19(2):156–172. doi: 10.1038/cr.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Shi Y, Massagué J. Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell. 2003;113(6):685–700. doi: 10.1016/S0092-8674(03)00432-X. [DOI] [PubMed] [Google Scholar]
- 143.Di Guglielmo GM, Le Roy C, Goodfellow AF, Wrana JL. Distinct endocytic pathways regulate TGF-beta receptor signalling and turnover. Nat Cell Biol. 2003;5(5):410–421. doi: 10.1038/ncb975. [DOI] [PubMed] [Google Scholar]
- 144.Chung C, Wang S, Sun W, Shu C, Kao Y, Shiao M, et al. Sorafenib suppresses TGF-β responses by inducing caveolae/lipid raft-mediated internalization/degradation of cell-surface type II TGF-β receptors: implications in development of effective adjunctive therapy for hepatocellular carcinoma. Biochem Pharmacol. 2018;154:39–53. doi: 10.1016/j.bcp.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 145.Ma X, Wang Q, Jiang Y, Xiao Z, Fang X, Chen Y. Lateral diffusion of TGF-beta type I receptor studied by single-molecule imaging. Biochem Bioph Res Co. 2007;356(1):67–71. doi: 10.1016/j.bbrc.2007.02.080. [DOI] [PubMed] [Google Scholar]
- 146.Zuo W, Chen Y. Specific activation of mitogen-activated protein kinase by transforming growth factor-beta receptors in lipid rafts is required for epithelial cell plasticity. Mol Biol Cell. 2009;20(3):1020–1029. doi: 10.1091/mbc.e08-09-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhang N, Li H, Qin C, Ma D, Zhao Y, Zhu W, et al. Insufficient radiofrequency ablation promotes the metastasis of residual hepatocellular carcinoma cells via upregulating flotillin proteins. J Cancer Res Clin. 2019;145(4):895–907. doi: 10.1007/s00432-019-02852-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Li Z, Yang Y, Gao Y, Wu X, Yang X, Zhu Y, et al. Elevated expression of flotillin-1 is associated with lymph node metastasis and poor prognosis in early-stage cervical cancer. Am J Cancer Res. 2016;6(1):38–50. doi: 10.1158/1538-7445.TUMMET15-B38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zhao L, Lin L, Pan C, Shi M, Liao Y, Bin J, et al. Flotillin-2 promotes nasopharyngeal carcinoma metastasis and is necessary for the epithelial-mesenchymal transition induced by transforming growth factor-β. Oncotarget. 2015;6(12):9781–9793. doi: 10.18632/oncotarget.3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Chaffer CL, Marjanovic ND, Lee T, Bell G, Kleer CG, Reinhardt F, et al. Poised chromatin at the ZEB1 promoter enables breast cancer cell plasticity and enhances tumorigenicity. Cell. 2013;154(1):61–74. doi: 10.1016/j.cell.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zabroski IO, Nugent MA. Lipid raft association stabilizes VEGF receptor 2 in endothelial cells. Int J Mol Sci. 2021;22(2):798. doi: 10.3390/ijms22020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bi J, Wang R, Zhang Y, Han X, Ampah KK, Liu W, et al. Identification of nucleolin as a lipid-raft-dependent β1-integrin-interacting protein in A375 cell migration. Mol Cells. 2013;36(6):507–517. doi: 10.1007/s10059-013-0149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lin M, Lu Y, Chen H, Lee C, Chung J, Chen S. Suppressing the formation of lipid raft-associated Rac1/PI3K/Akt signaling complexes by curcumin inhibits SDF-1α-induced invasion of human esophageal carcinoma cells. Mol Carcinogen. 2014;53(5):360–379. doi: 10.1002/mc.21984. [DOI] [PubMed] [Google Scholar]
- 154.Zhang S, Zhu N, Gu J, Li H, Qiu Y, Liao D, et al. Crosstalk between lipid rafts and aging: new frontiers for delaying aging. Aging Dis. 2022;13:1042. doi: 10.14336/AD.2022.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Voog J, Jones DL. Stem cells and the niche: a dynamic duo. Cell Stem Cell. 2010;6(2):103–115. doi: 10.1016/j.stem.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Fessler E, Dijkgraaf FE, De Sousa E, Melo F, Medema JP. Cancer stem cell dynamics in tumor progression and metastasis: is the microenvironment to blame? Cancer Lett. 2013;341(1):97–104. doi: 10.1016/j.canlet.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 157.Folkins C, Shaked Y, Man S, Tang T, Lee CR, Zhu Z, et al. Glioma tumor stem-like cells promote tumor angiogenesis and vasculogenesis via vascular endothelial growth factor and stromal-derived factor 1. Cancer Res. 2009;69(18):7243–7251. doi: 10.1158/0008-5472.CAN-09-0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Xu C, Wu X, Zhu J. VEGF promotes proliferation of human glioblastoma multiforme stem-like cells through VEGF receptor 2. The Sci World J. 2013;2013:417413. doi: 10.1155/2013/417413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Nallanthighal S, Heiserman JP, Cheon D. The role of the extracellular matrix in cancer stemness. Front Cell Dev Biol. 2019;7:86. doi: 10.3389/fcell.2019.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Brown Y, Hua S, Tanwar PS. Extracellular matrix-mediated regulation of cancer stem cells and chemoresistance. Int J Biochem Cell Biol. 2019;109:90–104. doi: 10.1016/j.biocel.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 161.Dobson HE, Ruan S, Chang AE, Wicha MS, Li Q. Targeting cancer stem cells via integrin β4. Oncotarget. 2021;12(18):1850–1858. doi: 10.18632/oncotarget.27977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Gardelli C, Russo L, Cipolla L, Moro M, Andriani F, Rondinone O, et al. Differential glycosylation of collagen modulates lung cancer stem cell subsets through β1 integrin-mediated interactions. Cancer Sci. 2021;112(1):217–230. doi: 10.1111/cas.14700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Barnawi R, Al-Khaldi S, Colak D, Tulbah A, Al-Tweigeri T, Fallatah M, et al. β1 Integrin is essential for fascin-mediated breast cancer stem cell function and disease progression. Int J Cancer. 2019;145(3):830–841. doi: 10.1002/ijc.32183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Wang R, Bi J, Ampah KK, Zhang C, Li Z, Jiao Y, et al. Lipid raft regulates the initial spreading of melanoma A375 cells by modulating β1 integrin clustering. Int J Biochem Cell Biol. 2013;45(8):1679–1689. doi: 10.1016/j.biocel.2013.04.031. [DOI] [PubMed] [Google Scholar]
- 165.Sahai E, Astsaturov I, Cukierman E, DeNardo DG, Egeblad M, Evans RM, et al. A framework for advancing our understanding of cancer-associated fibroblasts. Nat Rev Cancer. 2020;20(3):174–186. doi: 10.1038/s41568-019-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chen W, Ho C, Chang Y, Chen H, Lin C, Ling T, et al. Cancer-associated fibroblasts regulate the plasticity of lung cancer stemness via paracrine signalling. Nat Commun. 2014;5:3472. doi: 10.1038/ncomms4472. [DOI] [PubMed] [Google Scholar]
- 167.Su S, Chen J, Yao H, Liu J, Yu S, Lao L, et al. CD10(+)GPR77(+) cancer-associated fibroblasts promote cancer formation and chemoresistance by sustaining cancer stemness. Cell. 2018;172(4):841–856. doi: 10.1016/j.cell.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 168.Giannoni E, Bianchini F, Masieri L, Serni S, Torre E, Calorini L, et al. Reciprocal activation of prostate cancer cells and cancer-associated fibroblasts stimulates epithelial-mesenchymal transition and cancer stemness. Cancer Res. 2010;70(17):6945–6956. doi: 10.1158/0008-5472.CAN-10-0785. [DOI] [PubMed] [Google Scholar]
- 169.Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121(3):335–348. doi: 10.1016/j.cell.2005.02.034. [DOI] [PubMed] [Google Scholar]
- 170.Wald O, Izhar U, Amir G, Kirshberg S, Shlomai Z, Zamir G, et al. Interaction between neoplastic cells and cancer-associated fibroblasts through the CXCL12/CXCR4 axis: role in non-small cell lung cancer tumor proliferation. J Thorac Cardiovasc Surg. 2011;141(6):1503–1512. doi: 10.1016/j.jtcvs.2010.11.056. [DOI] [PubMed] [Google Scholar]
- 171.Zaman SN, Resek ME, Robbins SM. Dual acylation and lipid raft association of Src-family protein tyrosine kinases are required for SDF-1/CXCL12-mediated chemotaxis in the Jurkat human T cell lymphoma cell line. J Leukocyte Biol. 2008;84(4):1082–1091. doi: 10.1189/jlb.1007698. [DOI] [PubMed] [Google Scholar]
- 172.Roura S, Gálvez-Montón C, Pujal JM, Casani L, Fernández MA, Astier L, et al. New insights into lipid raft function regulating myocardial vascularization competency in human idiopathic dilated cardiomyopathy. Atherosclerosis. 2013;230(2):354–364. doi: 10.1016/j.atherosclerosis.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 173.Capitano ML, Hangoc G, Cooper S, Broxmeyer HE. Mild heat treatment primes human CD34(+) cord blood cells for migration toward SDF-1α and enhances engraftment in an NSG mouse model. Stem cells (Dayton, Ohio) 2015;33(6):1975–1984. doi: 10.1002/stem.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Hanahan D. Hallmarks of cancer: new dimensions. Cancer Discov. 2022;12(1):31–46. doi: 10.1158/2159-8290.CD-21-1059. [DOI] [PubMed] [Google Scholar]
- 175.Jeon H, Kim J, Ham SW, Oh S, Kim J, Park J, et al. Irradiation induces glioblastoma cell senescence and senescence-associated secretory phenotype. Tumour Biol: The J Int Soc Oncodev Biol Med. 2016;37(5):5857–5867. doi: 10.1007/s13277-015-4439-2. [DOI] [PubMed] [Google Scholar]
- 176.Faget DV, Ren Q, Stewart SA. Unmasking senescence: context-dependent effects of SASP in cancer. Nat Rev Cancer. 2019;19(8):439–453. doi: 10.1038/s41568-019-0156-2. [DOI] [PubMed] [Google Scholar]
- 177.Hwang HJ, Lee Y, Kang D, Lee HC, Seo HR, Ryu J, et al. Endothelial cells under therapy-induced senescence secrete CXCL11, which increases aggressiveness of breast cancer cells. Cancer Lett. 2020;490:100–110. doi: 10.1016/j.canlet.2020.06.019. [DOI] [PubMed] [Google Scholar]
- 178.Coppé J, Desprez P, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Ann Rev Pathol. 2010;5:99–118. doi: 10.1146/annurev-pathol-121808-102144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li Y, Wang L, Pappan L, Galliher-Beckley A, Shi J. IL-1β promotes stemness and invasiveness of colon cancer cells through Zeb1 activation. Mol Cancer. 2012;11:87. doi: 10.1186/1476-4598-11-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Corrò C, Healy ME, Engler S, Bodenmiller B, Li Z, Schraml P, et al. IL-8 and CXCR1 expression is associated with cancer stem cell-like properties of clear cell renal cancer. J Pathol. 2019;248(3):377–389. doi: 10.1002/path.5267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Fessler E, Borovski T, Medema JP. Endothelial cells induce cancer stem cell features in differentiated glioblastoma cells via bFGF. Mol Cancer. 2015;14:157. doi: 10.1186/s12943-015-0420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Li C, Lu N, Qi Q, Li F, Ling Y, Chen Y, et al. Gambogic acid inhibits tumor cell adhesion by suppressing integrin β1 and membrane lipid rafts-associated integrin signaling pathway. Biochem Pharmacol. 2011;82(12):1873–1883. doi: 10.1016/j.bcp.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 183.Yi J, Choo H, Cho B, Kim H, Kim Y, Ham Y, et al. Ginsenoside Rh2 induces ligand-independent Fas activation via lipid raft disruption. Biochem Bioph Res Co. 2009;385(2):154–159. doi: 10.1016/j.bbrc.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 184.Yun U, Lee J, Koo KH, Ye S, Kim S, Lee C, et al. Lipid raft modulation by Rp1 reverses multidrug resistance via inactivating MDR-1 and Src inhibition. Biochem Pharmacol. 2013;85(10):1441–1453. doi: 10.1016/j.bcp.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 185.Gajate C, Mollinedo F. The antitumor ether lipid ET-18-OCH(3) induces apoptosis through translocation and capping of Fas/CD95 into membrane rafts in human leukemic cells. Blood. 2001;98(13):3860–3863. doi: 10.1182/blood.V98.13.3860. [DOI] [PubMed] [Google Scholar]
- 186.Gajate C, Del Canto-Jañez E, Acuña AU, Amat-Guerri F, Geijo E, Santos-Beneit AM, et al. Intracellular triggering of Fas aggregation and recruitment of apoptotic molecules into Fas-enriched rafts in selective tumor cell apoptosis. J Exp Med. 2004;200(3):353–365. doi: 10.1084/jem.20040213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Mollinedo F, Gajate C. Fas/CD95 death receptor and lipid rafts: new targets for apoptosis-directed cancer therapy. Drug Resist Updates : Rev Comment Antimicrob Anti-Cancer Chemother. 2006;9(1–2):51–73. doi: 10.1016/j.drup.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 188.Gajate C, Mollinedo F. Edelfosine and perifosine induce selective apoptosis in multiple myeloma by recruitment of death receptors and downstream signaling molecules into lipid rafts. Blood. 2007;109(2):711–719. doi: 10.1182/blood-2006-04-016824. [DOI] [PubMed] [Google Scholar]
- 189.Mollinedo F, de la Iglesia-Vicente J, Gajate C, Estella-Hermoso de Mendoza A, Villa-Pulgarin JA, Campanero MA, et al. Lipid raft-targeted therapy in multiple myeloma. Oncogene. 2010;29(26):3748–3757. doi: 10.1038/onc.2010.131. [DOI] [PubMed] [Google Scholar]
- 190.Gajate C, Mollinedo F. Lipid rafts, endoplasmic reticulum and mitochondria in the antitumor action of the alkylphospholipid analog edelfosine. Anti-Cancer Agent ME. 2014;14(4):509–527. doi: 10.2174/1871520614666140309222259. [DOI] [PubMed] [Google Scholar]
- 191.Gajate C, Mollinedo F. Lipid raft-mediated Fas/CD95 apoptotic signaling in leukemic cells and normal leukocytes and therapeutic implications. J Leukocyte Biol. 2015;98(5):739–759. doi: 10.1189/jlb.2MR0215-055R. [DOI] [PubMed] [Google Scholar]
- 192.Mollinedo F, Gajate C. Clusters of apoptotic signaling molecule-enriched rafts, CASMERs: membrane platforms for protein assembly in Fas/CD95 signaling and targets in cancer therapy. Biochem Soc T. 2022;50(3):1105–1118. doi: 10.1042/BST20211115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Gajate C, Gayet O, Fraunhoffer NA, Iovanna J, Dusetti N, Mollinedo F. Induction of apoptosis in human pancreatic cancer stem cells by the endoplasmic reticulum-targeted alkylphospholipid analog edelfosine and potentiation by autophagy inhibition. Cancers. 2021;13(23):6124. doi: 10.3390/cancers13236124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Osterhues A, Liebmann S, Schmid M, Buk D, Huss R, Graeve L, et al. Stem cells and experimental leukemia can be distinguished by lipid raft protein composition. Stem Cells Dev. 2006;15(5):677–686. doi: 10.1089/scd.2006.15.677. [DOI] [PubMed] [Google Scholar]
- 195.Hermetet F, Buffière A, Aznague A, Pais de Barros J, Bastie J, Delva L, et al. High-fat diet disturbs lipid raft/TGF-β signaling-mediated maintenance of hematopoietic stem cells in mouse bone marrow. Nat Commun. 2019;10(1):523. doi: 10.1038/s41467-018-08228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.