Abstract
Background
During the obturation procedure, sealer extrusion occurs in some cases. iRoot SP is a kind of bioceramic sealer with superior physicochemical and biological properties. This article reports the outcome of iRoot SP extrusion in root canal treatment and the potential factors associated with the outcome.
Methods
Ninety-nine patients and one hundred and eighty-five teeth treated between 2014 and 2020 were included in this retrospective study. All of the cases were filled with a single-cone technique and the iRoot SP sealer. The minimum follow-up visit period was 1 year. The outcome was evaluated by clinical examination and radiographic examination at recall and was classified as healed, healing (success), or not healed (failure).
Results
The overall success rate of all teeth was 96.8%. The success rate of adequately filled teeth was 97.3%, while that of iRoot SP extrusion was 95.8%; the difference was not statistically significant. Factors such as gender, age, tooth position, follow-up visit period, size of periapical lesion, treatment type and extruding sealer amount had no influence on the outcome of iRoot SP extruded teeth.
Conclusions
The results suggested that iRoot SP extrusion has no adverse effect on the outcome of root canal treatment, which may contribute to the endodontic treatment.
Keywords: Root canal treatment, Single-cone technique, iRoot SP sealer, Extrusion, Clinical outcome\
Introduction
Root canal filling is the final procedure of root canal treatment and functions to densely seal the root canal system and the bacteria inside. The quality of filling is closely related to endodontic success. The optimal obturation is achieved by densely sealing and accurately stopping at the apical foramen [1].
Due to inflammatory destruction in the apical foramen or inappropriate root canal preparation from the operator, sealer extrusion occurs in some cases. Previous studies have suggested that extruded sealers or core materials might trigger inflammation, leading to worse outcomes than those cases in which the teeth are adequately filled [2, 3]. Histological examination demonstrated that overextended sealers cause severe inflammation in the short term. In the long run, there is no significant manifestation of infection around the extruded sealers, but proliferation of connective tissues and infiltration of several inflammatory cells [4].
In recent years, as dental materials have developed, bioceramic root canal sealers with good physicochemical and biological properties, such as mineral trioxide aggregate (MTA), have been introduced. Some researchers reported that extruded MTA has no adverse effect on periapical healing [5–8], while others held different opinions [9]. iRoot SP, similar to MTA, is also a kind of bioceramic root canal sealer, which composed of calcium silicate, calcium phosphate, zirconium oxide, calcium hydroxide and so on. It attracts clinical operators’ attention due to its superior properties. Specifically, iRoot SP is more biocompatible than AH Plus and MTA [10–17] and induces a mild inflammatory response in mouse subcutaneous tissue [18]. In addition, iRoot SP possesses an excellent apical sealing ability, which results in less apical microleakage [19–25]. After root canal obturation, it could also play a role in promoting osteogenesis [13, 16, 18, 26, 27] as well as continuously inhibiting bacteria, such as Enterococcus faecalis, Candida albicans, and Staphylococcus aureus, which may be related to its high alkalinity [28–32]. As a result, clinicians have come to a question whether over-obturated iRoot SP affects treatment outcomes. Therefore, this study aims to track our cases of iRoot SP over-obturation and evaluate the effect on periapical healing and tooth outcome.
Material and methods
Case selection and treatment procedure
Patients get the endodontic treatment in the Department of Operative Dentistry and Endodontics, Hospital of Stomatology affiliated to Sun Yat-sen University from 2014 through 2020. The protocol for this study was approved by the Medical Ethics Committee of Hospital of Stomatology, Sun Yat-sen University (approval number: KQEC-2020-05). Written informed consent were obtained from all subjects. The cases were selected or rejected according to the following criteria:
A completely developed tooth that demanded non-surgical root canal treatment or retreatment. The obturation was conducted using the single-cone technique with one gutta-percha and iRoot SP as the sealer.
Preoperative, postoperative, and follow-up radiographs and records documenting the treatments were well preserved.
The tooth was treated with acceptable obturation quality: all canals were prepared and filled within 1–2 mm of the radiographic apex. The gutta-percha was settled within the apical foramen.
The recall was for at least 1 year.
The tooth received adequate coronal restoration in a timely manner after root canal treatment.
The cases were rejected from this study if the following conditions occurred in the tooth: radiograph evidence of severe alveolar bone loss, perforation, cracks extending into canal orifices or vertical root fracture.
All of the selected teeth were treated by one specialist endodontist at two visits. Treatments began with local anesthesia and dental dam isolation. After access, the canal orifices were found under the dental microscope (OPMI PROergo, Zeiss, Oberkochen, Germany), and the working length was determined via an electronic apex locator (Raypex VI, VDW GmbH, Munich Germany). When the working length could not be confirmed by the electronic apex locator, a radiograph was taken. All of the canals were enlarged up to size 30 at least, which was 2–3 sizes larger than the initial canal size, by M3 Ni-Ti rotary instrumentation (Yirui Dental Group, Shanghai, China) using a standardized approach. In retreatment cases, previous obturation materials and canal obstructions were removed using a combination of ultrasonics and a ProTaper retreatment nickel-titanium system (Dentsply Maillefer, Ballaigues, Switzerland). The canals were irrigated with adequate 3% sodium hypochlorite and normal saline using a 31-G side-venting needle (Ultradent Products Inc., UT, US). After the preparation was complete, the canals were dried with paper points and dispensed with ApexCal (Ivoclar Vivadent AG, Schaan, Liechtenstein) as an intracanal medication. Cavition (GC, Tokyo, Japan) was used for temporary coronal sealing. Two weeks later, root canal obturation was performed at the second visit. The ApexCal was removed by both the master apical file and ultrasonics. iRoot SP was injected into the whole root canals, and gutta-percha cones that matched the master apical file were placed into the working length. Excess gutta-percha was cut, and the remaining gutta-percha was vertically packed with a plugger. For those irregular canals, additional cones were passively placed adjacent to the master cone. Excess sealer was removed from the chamber by ultrasonics. Finally, all of the teeth were sealed by permanent or temporary coronal restorations in a timely manner.
Radiographic and clinical examinations were performed at recall appointments for the treated teeth. The presence of pain, a sinus tract, swelling, reaction to percussion and palpation, mobility and so on were all recorded. Preoperative, postoperative, and follow-up radiographs were evaluated by 2 examiners (not including the operator). The outcomes of the teeth were divided into the following 3 classifications:
Healed: Teeth function without any symptoms. Radiographs show no periapical radiolucency.
Healing: Teeth are asymptomatic and functional. Radiographs show that periapical lesions still exist but are smaller than before.
Non-healed: Teeth fail to function with symptoms, regardless of periapical radiolucency or asymptomatic teeth with unchanged, new, or enlarged periapical lesions. Examples of each outcome category are shown in Figs. 1, 2 and 3.
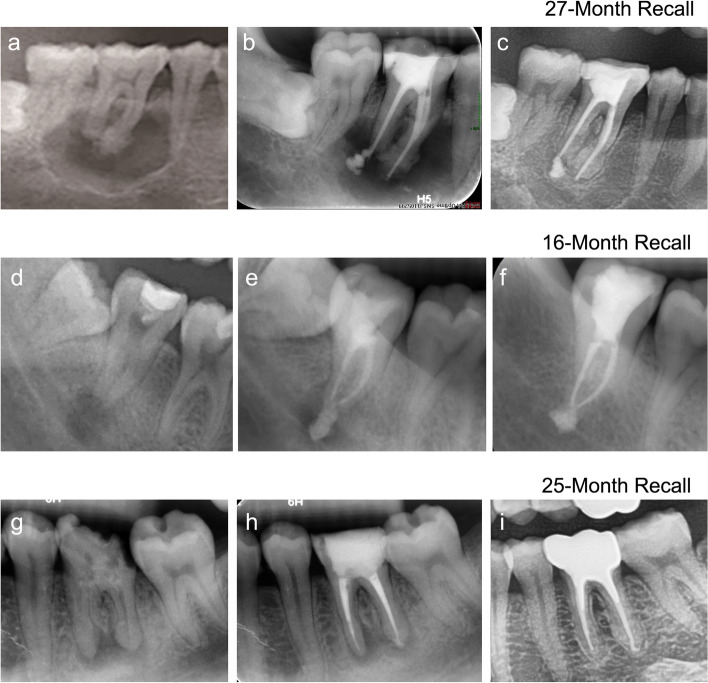
Fig. 1.
Preoperative (a, d and g), postoperative (b, e and h), and recall (c, f and i) radiographs of the outcomes of healed teeth
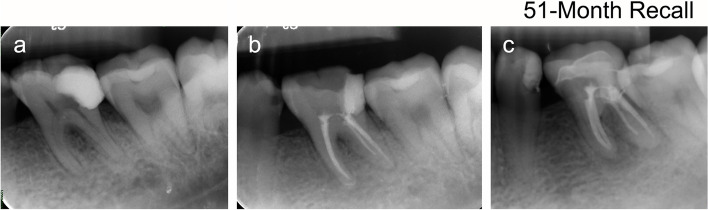
Fig. 2.
Preoperative (a and d), postoperative (b and e), and recall (c and f) radiographs of outcomes of healing teeth
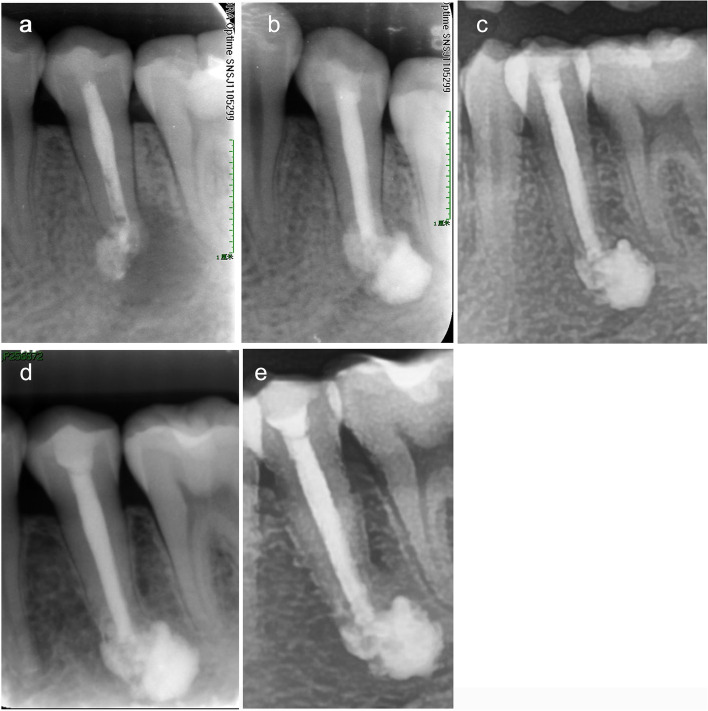
Fig. 3.
Preoperative (a), postoperative (b), and recall (c) radiographs of outcomes of unhealed teeth
Outcome assessment
The three outcome classifications were divided into two groups. Both healed and healing teeth were considered successful cases, and non-healed teeth were considered failure cases. To evaluate the factors that affected the outcome of the sealer-extruded teeth, we analyzed several possible variables, including the patients’ age, gender, tooth type, tooth position, presence of periapical lesion, lesion size, initial treatment or retreatment, follow-up time and extruding sealer amount.
Data analysis
For statistical analysis, Fisher’s exact test were used to analyze the effect of each prognostic factor after the data were grouped. A P value < 0.05 was considered significant, and all tests were 2-sided. Statistical tests were performed with SPSS v25.0 software (IBM Corp, Armonk, NY).
Results
Ninety-nine patients (twenty-one males and seventy-eight females) and one hundred and eighty-five teeth, which consisted of 61.1% teeth without sealer extrusion (113/185) and 38.9% teeth with sealer extrusion (72/185), were included for analysis. The average time to recall is 30.46 months. The other demographic characteristics of the patient pool are summarized in Table 1.
Table 1.
Population demographics
| Demographic | Sealer extrusion | |
|---|---|---|
| Absent, n(%) | Present, n(%) | |
| Total | 113 (61.1) | 72 (38.9) |
| Age (yrs) | ||
| <40 | 59 (31.9) | 51 (27.6) |
| 40–70 | 54 (29.2) | 21 (11.3) |
| Sex | ||
| Male | 22 (11.9) | 14 (7.6) |
| Female | 91 (49.2) | 58 (31.3) |
| Tooth type | ||
| Anterior | 34 (18.4) | 27 (14.6) |
| posterior | 79 (42.7) | 45 (24.3) |
| Tooth location | ||
| Maxillary | 74 (40.0) | 42 (22.7) |
| Mandibular | 39 (21.1) | 30 (16.2) |
| Time to recall (y) | ||
| 1–2 | 40 (21.6) | 29 (15.7) |
| 2–4 | 54 (29.2) | 31 (16.7) |
| > 4 | 19 (10.3) | 12 (6.5) |
|
Average time to recall |
30.46 | |
| Treatment type | ||
| Initial RCT | 86 (46.5) | 55 (29.7) |
| ReTx | 27 (14.6) | 17 (9.2) |
RCT Root canal treatment, ReTx Retreatment
The overall success rate of all teeth was 96.8%. The success rate of teeth without sealer extrusion was 97.3%, with 88.5% healed, 8.8% healing, and 2.7% not healed. The overall success rate for teeth with sealer extrusion was 95.8%, with 69.4% healed, 26.4% healing, and 4.2% unhealed. No significant difference was found between the two types. Table 2 shows the outcomes of the comparison of teeth with and without sealer extrusion according to the prognostic factors. None of the most common factors showed a significant influence on the outcome of the two types of treated teeth. Because no failure was found among the cases with or without sealer extrusion according to the tooth type (anterior), the success rates in both groups were 100% and could not be compared. The exact numbers can be found in Table 2.
Table 2.
Relation of prognostic factors to treatment results of teeth with or without sealer extrusion in root canals filled with gutta-percha and iRoot SP
| Factor | Without sealer extrusion | With sealer extrusion | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Healed, n(%) | Healing, n(%) | Not healed, n(%) | Success, n(%) | Healed, n(%) | Healing, n(%) | Not healed, n(%) | Success, n(%) | ||
| Total | 100 (88.5) | 10 (8.8) | 3 (2.7) | 110 (97.3) | 50 (69.4) | 19 (26.4) | 3 (4.2) | 69 (95.8) | 0.679 |
| Age | |||||||||
| <40 | 49 (83.0) | 8 (13.6) | 2 (3.4) | 57 (96.6) | 34 (66.7) | 14 (27.4) | 3 (5.9) | 48 (94.1) | 0.661 |
| 40–70 | 51 (94.4) | 2 (3.7) | 1 (1.9) | 53 (98.1) | 16 (76.2) | 5 (23.8) | 0 (0) | 21 (100.0) | 1.000 |
| Sex | |||||||||
| Male | 17 (77.3) | 4 (18.2) | 1 (4.5) | 21 (95.5) | 10 (71.4) | 4 (28.6) | 0 (0) | 14 (100.0) | 1.000 |
| Female | 83 (91.2) | 6 (6.6) | 2 (2.2) | 89 (97.8) | 40 (69.0) | 15 (25.9) | 3 (5.1) | 55 (94.9) | 0.378 |
| Tooth type | |||||||||
| Anterior | 29 (85.3) | 5 (14.7) | 0 (0) | 34 (100.0) | 19 (70.4) | 8 (29.6) | 0 (0) | 27 (100.0) | – |
| posterior | 71 (89.9) | 5 (6.3) | 3 (3.8) | 76 (96.2) | 31 (68.9) | 11 (24.4) | 3 (6.7) | 42 (93.3) | 0.667 |
| Tooth Location | |||||||||
| Maxillary | 66 (89.2) | 7 (9.5) | 1 (1.3) | 73 (98.7) | 32 (76.2) | 10 (23.8) | 0 (0) | 42 (100.0) | 1.000 |
| Mandibular | 34 (87.2) | 3 (7.7) | 2 (5.1) | 37 (94.9) | 18 (60.0) | 9 (30.0) | 3 (10.0) | 27 (100.0) | 0.646 |
| Time to recall | |||||||||
| 1–2 | 32 (80.0) | 7 (17.5) | 1 (2.5) | 39 (97.5) | 12 (41.4) | 16 (55.2) | 1 (3.4) | 28 (96.6) | 1.000 |
| 2–4 | 52 (96.2) | 1 (1.9) | 1 (1.9) | 53 (98.1) | 29 (93.6) | 1 (3.2) | 1 (3.2) | 30 (96.8) | 1.000 |
| > 4 | 16 (84.2) | 2 (10.5) | 1 (5.3) | 18 (94.7) | 9 (75.0) | 2 (16.7) | 1 (8.3) | 11 (91.3) | 1.000 |
| Treatment type | |||||||||
| Initial RCT | 77 (89.5) | 8 (9.3) | 1 (1.2) | 85 (98.8) | 39 (70.9) | 13 (23.6) | 3 (5.5) | 52 (94.5) | 0.299 |
| ReTx | 23 (85.2) | 2 (7.4) | 2 (7.4) | 25 (92.6) | 11 (64.7) | 6 (35.3) | 0 (0) | 17 (100.0) | 0.515 |
| Lesion | |||||||||
| Absent | 57 (96.6) | 0 (0) | 2 (3.4) | 57 (96.6) | 27 (100.0) | 0 (0) | 0 (0) | 27 (100.0) | 1.000 |
| Present | 43 (79.6) | 10 (18.5) | 1 (1.9) | 53 (98.1) | 23 (51.1) | 19 (42.2) | 3 (6.7) | 42 (93.3) | 0.327 |
| Lesion size | |||||||||
| ≤ 5 mm | 33 (82.5) | 6 (15.0) | 1 (2.5) | 39 (97.5) | 16 (72.8) | 5 (22.7) | 1 (4.5) | 21 (95.5) | 1.000 |
| > 5 mm | 10 (71.4) | 4 (28.6) | 0 (0) | 14 (100.0) | 7 (30.4) | 14 (60.9) | 2 (8.7) | 21 (91.3) | 0.517 |
We also analyzed whether the potential factors affected the success rate of the teeth with sealer extrusion, and the outcomes are shown in Table 3. All factors show no significant effect on the success rate of teeth with sealer extrusion. Among 72 extruding cases, none of the overfilling iRoot SP was completely absorbed during the recall time. 40.3% of them were partially absorbed and 59.7% appealed no absorption, showed in Table 4.
Table 3.
Relation of prognostic factors to treatment results of teeth with sealer extrusion in root canals filled with gutta-percha and iRoot SP
| Factor | Healed, n(%) | Healing, n(%) | Not healed, n(%) | Success, n(%) | P value |
|---|---|---|---|---|---|
| Age (yrs) | 0.551 | ||||
| <40 | 34 (66.7) | 14 (27.4) | 3 (5.9) | 48 (94.1) | |
| 40–70 | 16 (76.2) | 5 (23.8) | 0 (0) | 21 (100.0) | |
| Sex | 1.000 | ||||
| Male | 10 (71.4) | 4 (28.6) | 0 (0) | 14 (100.0) | |
| Female | 40 (69.0) | 15 (25.9) | 3 (5.1) | 55 (94.9) | |
| Tooth type | 0.287 | ||||
| Anterior | 19 (70.4) | 8 (29.6) | 0 (0) | 27 (100.0) | |
| Posterior | 31 (68.9) | 11 (24.4) | 3 (6.7) | 42 (93.3) | |
| Tooth Location | 0.068 | ||||
| Maxillary | 32 (76.2) | 10 (23.8) | 0 (0) | 42 (100.0) | |
| Mandibular | 18 (60.0) | 9 (30.0) | 3 (10.0) | 27 (100.0) | |
| Time to recall (y) | 0.563 | ||||
| 1–2 | 12 (41.4) | 16 (55.2) | 1 (3.4) | 28 (96.6) | |
| 2–4 | 29 (93.6) | 1 (3.2) | 1 (3.2) | 30 (96.8) | |
| > 4 | 9 (75.0) | 2 (16.7) | 1 (8.3) | 11 (91.3) | |
| Treatment type | 1.000 | ||||
| Initial RCT | 39 (70.9) | 13 (23.6) | 3 (5.5) | 52 (94.5) | |
| ReTx | 11 (64.7) | 6 (35.3) | 0 (0) | 17 (100.0) | |
| Lesion | 0.287 | ||||
| Absent | 27 (100.0) | 0 (0) | 0 (0) | 27 (100.0) | |
| Present | 23 (51.1) | 19 (42.2) | 3 (6.7) | 42 (93.3) | |
| Lesion size | 1.000 | ||||
| ≤ 5 mm | 16 (72.8) | 5 (22.7) | 1 (4.5) | 21 (95.5) | |
| > 5 mm | 7 (30.4) | 14 (60.9) | 2 (8.7) | 21 (91.3) | |
| Extruded sealer size | 0.239 | ||||
| ≤ 1 mm | 29 (80.6) | 7 (19.4) | 0 (0) | 36 (100.0) | |
| > 1 mm | 21 (58.4) | 12 (33.3) | 3 (8.3) | 33 (91.7) |
Table 4.
The absorption extent of iRoot SP in the teeth with sealer extrusion
| Extent | Time to Recall (y) | ||
|---|---|---|---|
| 1–2, n% | 2–4, n% | > 4, n% | |
| Partial Absorption | 7 (9.7) | 18 (25.0) | 4 (5.6) |
| No Absorption | 22 (30.5) | 13 (18.1) | 8 (11.1) |
Typical case
A 31-year-old female patient complained that intermittent pain occurred in relation to the lower left posterior teeth over a month after treated in a dental clinic (Fig. 4). Clinical examination found pulp access cavity on tooth #35, with slight knocking pain. Diagnostic X-ray showed that tooth #35 had overfilling intracanal medication and large periapical lesion (Fig. 4a). According to the above results, we diagnosed the patient with chronic apical periodontitis. Endodontic retreatment was scheduled. After completed the root canal therapy of tooth #35, a larger amount of iRoot SP extruded due to the severe bone loss of periapical tissues (Fig. 4b). Subsequently, the tooth was reconstructed with direct composite resin. The 12-month recall observation showed that periapical lesions were smaller according to the X-ray results, without any symptoms (Fig. 4c). The radiographic follow-ups at 36 and 60 months showed periapical lesions disappeared and the over-filling iRoot SP appealed no obvious absorption radiographically (Fig. 4d-e).
Fig. 4.
The radiographs of tooth #35. a The preoperative radiograph, showed that tooth #35 had large periapical lesion and overfilling intracanal medication. b The postoperative radiograph, showed that a larger amount of iRoot SP extruded. c The 12-month observation showed that periapical lesions were smaller according to the X-ray results. d The 36-month recall observation showed that periapical lesions disappeared radiographically. e Radiography results of 60-month following-up showed periapical lesions were invisible on tooth #35 and functioned without any symptoms. The over-filling iRoot SP appealed no absorption radiographically
Discussion
In this study, a single-cone obturation technique with iRoot SP as the sealer was used for all of the cases, and the overall success rate of all teeth was 96.8%. This result coincided with the report of Chybowski et al. [33] that they followed 307 teeth with a single-cone technique for at least 1 year and found that the overall success rate was up to 90.9% compared to the cumulative success rate of 86% in the initial treatment with the vertically compacted warm gutta-percha technique [34]. This result demonstrates that the single-cone obturation technique is a viable option while sealers with superior properties remain in demand [33]. iRoot SP is a kind of bioceramic sealer with good biocompatibility, hydrophilicity and slight setting expansion, allowing it to be used in a single-cone technique. This technique enhances the clinical operation efficiency of root canal obturation and might even improve the success rate of endodontic therapy.
Within the limitations of this study, the overall success rate of adequately filled teeth was 97.3%, while that of iRoot SP extrusion was 95.8%; the difference was not statistically significant. More specifically, factors such as gender, age, tooth position, follow-up visit period, size of periapical lesions, and treatment type had no influence on the healing of the periapical tissues between the iRoot SP adequately filled group and the extrusion group. Further results showed that in the iRoot SP extrusion group, the factors mentioned before, including the amount of added extruding sealer, had little impact on the success rate of root canal treatment. These results were in contradiction with previous reports stating that extrusion of root filling material might interfere with the repair process [35–37]. However, Sari et al. [38] tracked 87 root canals for a 4-year follow-up period, demonstrating that extruded AH Plus does not prevent periapical healing but can be a delaying factor for healing in children. Zemener et al. [39] observed 10 cases that were overfilled with the methacrylate resin-based sealer EndoREZ and no adverse effect on the outcome. Ricucci et al. [40] found that all of the overextension teeth without periapical lesions healed within a 4-year follow-up period, while 79% of the overextension teeth with periapical lesions healed. These contradictions might be attributed to differences in tissue compatibility among the sealers. With the evolution of dental instruments and materials, bioceramic-based sealers have become widely used. Both Chang et al. [6] and Nagmode et al. [7] reported that the MTA extrusions in apexification did not affect the healing of periapical tissues and that the patients did not suffer. Asgary and Ehsani [8] reported a case in which extruding MTA was completely absorbed 7 years posttreatment and periapical tissues healed well. Nosrat et al. [41] reported 3 cases of MTA extrusions: MTA was absorbed in one case, and periapical healing was favorable after 4 years; in the other two cases, the teeth were persistently swelling and were sensitive to percussion. Thus, the outcome is unpredictable in the case of MTA overextension. Chybowski et al. [33] followed 307 teeth with a single-cone technique, and 47.4% of those teeth were iRoot SP overextended. After an average follow-up visit of 30.1 months, the results showed that iRoot SP extrusion had no significant influence on periapical tissue healing.
Our results, as well as those in a previous study [33], showed that iRoot SP extrusion has no adverse effect on the healing of periapical tissues. Its favorable properties might be one of the critical reasons. iRoot SP has been reported to be less toxic [10–17] than AH Plus and MTA and to induce a relatively milder inflammatory response [18]. Furthermore, the excellent apical sealing ability of iRoot SP also accounts for the favorable outcome, which results in less apical microleakage of bacteria [19–25]. Additionally, this ability plays a role in continuously inhibiting bacteria [28–32], as well as promoting osteogenesis after root canal obturation [13, 16, 18, 26, 27].
The overfilling sealers might dissolve in periapical tissue liquids and then be phagocytosed or wrapped by fibrous tissues. The outcome depends on the sealer’s composition and extrusion amount. Histological examination revealed that an obvious inflammatory response might occur in periapical tissues shortly after sealer extrusion [4]. However, except for several remarkably toxic sealers, once the sealers set, the toxicity vanishes. Consequently, there is no significant infection around the extruding sealer, but there is proliferation of fibrous connective tissue and sporadic infiltration of inflammatory cells [4].
In this study, among the iRoot SP extruding teeth, none presented complete absorption of extruding iRoot SP, whereas the periapical tissues healed or were healing. It is suggested that iRoot SP overextension is not the critical factor in periapical healing, which is in accord with the study of Lin et al. [42], who stated that extrusion of the sealer cannot be a factor in the failure of endodontic treatment and that the canal filler is likely less than microbial factors to cause irritation to periradicular tissue. In addition, sealer extrusion does not always lead to clinical symptoms nor is it the direct cause of postoperative pain, which might be associated with infection in root canals and periapical tissues. Moreover, sealer extrusion is likely to occur on those teeth with root apex absorption or canal over-preparation, which results in compromised sealing and microleakages at the apical foramen [43]. When the root canals are over-prepared, dental debris and necrotic pulp tissues containing bacteria might be pushed out into the periapical tissues. Under the above situations, bacteria transferred into the periapical tissues might multiply again and cause clinical symptoms. In addition, we don’t support the iRoot SP sealer extrusion because it may lead to facial paresthesia or maxillary sinusitis after the filling materials extrusion into the maxillary sinus or inferior alveolar canal [44, 45]. This article aims to further provide clinical data support to the operators, by reporting specifically on the clinical success of iRoot SP extrusion in root canal therapy and the potential factors affecting the outcomes. As a retrospective study, it is limited by bias. The inherent selection bias of retrospective studies might alter the outcome [46]. In this study, patients were regularly invited to recall visits, but many refused due to inconvenience. Thus, patients with symptoms were more willing to participate in subsequent visits, which decreased the success rate. In addition, our sample size was greatly reduced. Specifically, among the 99 patients, 78.8% were women. Women might pay more attention to their personal health than men do.
Conclusion
Within the limitations of this study, the overall success rate of the iRoot SP extrusion group was 95.8% and was not statistically significant when compared to that of the iRoot SP adequately filled group. Factors such as gender, age, tooth position, follow-up visit period, size of periapical lesions, and treatment type had no influence on the healing of the periapical tissues between the iRoot SP adequately filled group and the extrusion group. In the iRoot SP extrusion group, the factors mentioned before with the addition of the extruding sealer amount had little impact on the success rate. To make our study more convincing, more follow-up recall cases and longer recall periods are needed in the future. Last, but not least, this study does not aim to advocate for sealer extrusion but suggests that operators could be optimistic when applying iRoot SP extrusion, except in special situations such as nerve injuries. The operators should pay more attention to root canal preparation and infection control.
Acknowledgements
Not applicable.
Authors’ contributions
Jing Li: Conceptualization, Methodology, Data collection and analysis, Writing - Original draft preparation. Liuchi Chen: Conceptualization, Methodology, Data collection and analysis, Writing - Original draft preparation. Chunmei Zeng: Methodology, Cases selection, Data collection, Writing – Review & Editing. Yiwen Liu: Cases selection, Data collection, Writing – Review & Editing. Qimei Gong: Conceptualization, Methodology, Cases selection, Writing – Review & Editing. Hongwei Jiang: Conceptualization, Methodology, Cases selection, Data collection, Writing – Review & Editing. All authors read and approved the final manuscript.
Funding
This study was financially supported by the Natural Science Foundation of Guangdong Province (project no. 2017A030313713), the National Natural Science Foundation of China (project no. 81870750) and the Guangdong Financial Fund for High-Caliber Hospital Construction (project no. 174–2018-XMZC-0001-03-0125/A-01).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The Medical Ethics Committee of the Hospital of Stomatology of Sun Yat-sen University granted approval for this study (approval number: KQEC-2020-05).
Consent for publication
Written informed consent for publication were obtained from the patients.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jing Li and Liuchi Chen contributed equally to this work.
Contributor Information
Qimei Gong, Email: gongqim@mail.sysu.edu.cn.
Hongwei Jiang, Email: jhongw@mail.sysu.edu.cn.
References
- 1.Kim S, Jung H, Kim S, et al. The influence of an isthmus on the outcomes of surgically treated molars: a retrospective study. J Endod. 2016;42(7):1029–1034. doi: 10.1016/j.joen.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 2.Ricucci D, Langeland K. Apical limit of root canal instrumentation and obturation, part 2. A histological study. Int Endod J. 1998;31(6):394–409. doi: 10.1046/j.1365-2591.1998.00183.x. [DOI] [PubMed] [Google Scholar]
- 3.Holland R, Mazuqueli L, de Souza V, et al. Influence of the type of vehicle and limit of obturation on apical and periapical tissue response in dogs’ teeth after root canal filling with mineral trioxide aggregate. J Endod. 2007;33(6):693–697. doi: 10.1016/j.joen.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 4.Giardino L, Pontieri F, Savoldi E, et al. Aspergillus mycetoma of the maxillary sinus secondary to overfilling of a root canal. J Endod. 2006;32(7):692–694. doi: 10.1016/j.joen.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Molven O, Halse A, Fristad I, et al. Periapical changes following root-canal treatment observed 20-27 years postoperatively. Int Endod J. 2002;35(9):784–790. doi: 10.1046/j.1365-2591.2002.00568.x. [DOI] [PubMed] [Google Scholar]
- 6.Chang SW, Oh TS, Lee W, et al. Long-term observation of the mineral trioxide aggregate extrusion into the periapical lesion: a case series. Int J Oral Sci. 2013;5(1):54–57. doi: 10.1038/ijos.2013.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagmode PS, Satpute AB, Patel AV, et al. The effect of mineral trioxide aggregate on the periapical tissues after unintentional extrusion beyond the apical foramen. Case Rep Dent. 2016;2016:3590680. doi: 10.1155/2016/3590680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asgary S, Ehsani S. MTA resorption and periradicular healing in an open-apex incisor: a case report. Saudi Dent J. 2012;24(1):55–59. doi: 10.1016/j.sdentj.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bryan TE, Khechen K, Brackett MG, et al. In vitro osteogenic potential of an experimental calcium silicate-based root canal sealer. J Endod. 2010;36(7):1163–1169. doi: 10.1016/j.joen.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 10.Zhang W, Li Z, Peng B. Ex vivo cytotoxicity of a new calcium silicate-based canal filling material. Int Endod J. 2010;43(9):769–774. doi: 10.1111/j.1365-2591.2010.01733.x. [DOI] [PubMed] [Google Scholar]
- 11.Er K, Ayar A, Kalkan OF, et al. Neurotoxicity evaluation of three root canal sealers on cultured rat trigeminal ganglion neurons. J Clin Exp Dent. 2017;9(1):e34–ee9. doi: 10.4317/jced.52901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mukhtar-Fayyad D. Cytocompatibility of new bioceramic-based materials on human fibroblast cells (MRC-5) Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(6):e137–e142. doi: 10.1016/j.tripleo.2011.05.042. [DOI] [PubMed] [Google Scholar]
- 13.Chang SW, Lee SY, Kang SK, et al. In vitro biocompatibility, inflammatory response, and osteogenic potential of 4 root canal sealers: Sealapex, Sankin apatite root sealer, MTA Fillapex, and iRoot SP root canal sealer. J Endod. 2014;40(10):1642–1648. doi: 10.1016/j.joen.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Collado-Gonzalez M, Garcia-Bernal D, Onate-Sanchez RE, et al. Biocompatibility of three new calcium silicate-based endodontic sealers on human periodontal ligament stem cells. Int Endod J. 2017;50(9):875–884. doi: 10.1111/iej.12703. [DOI] [PubMed] [Google Scholar]
- 15.Guven EP, Yalvac ME, Kayahan MB, et al. Human tooth germ stem cell response to calcium-silicate based endodontic cements. J Appl Oral Sci. 2013;21(4):351–357. doi: 10.1590/1678-775720130047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guven EP, Tasli PN, Yalvac ME, et al. In vitro comparison of induction capacity and biomineralization ability of mineral trioxide aggregate and a bioceramic root canal sealer. Int Endod J. 2013;46(12):1173–1182. doi: 10.1111/iej.12115. [DOI] [PubMed] [Google Scholar]
- 17.Bosio CC, Felippe GS, Bortoluzzi EA, et al. Subcutaneous connective tissue reactions to iRoot SP, mineral trioxide aggregate (MTA) Fillapex, DiaRoot BioAggregate and MTA. Int Endod J. 2014;47(7):667–674. doi: 10.1111/iej.12203. [DOI] [PubMed] [Google Scholar]
- 18.Zhang W, Peng B. Tissue reactions after subcutaneous and intraosseous implantation of iRoot SP, MTA and AH plus. Dent Mater J. 2015;34(6):774–780. doi: 10.4012/dmj.2014-271. [DOI] [PubMed] [Google Scholar]
- 19.Akcay M, Arslan H, Durmus N, et al. Dentinal tubule penetration of AH plus, iRoot SP, MTA fillapex, and guttaflow bioseal root canal sealers after different final irrigation procedures: a confocal microscopic study. Lasers Surg Med. 2016;48(1):70–76. doi: 10.1002/lsm.22446. [DOI] [PubMed] [Google Scholar]
- 20.Paragliola R, Franco V, Fabiani C, et al. Final rinse optimization: influence of different agitation protocols. J Endod. 2010;36(2):282–285. doi: 10.1016/j.joen.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Shokouhinejad N, Gorjestani H, Nasseh AA, et al. Push-out bond strength of gutta-percha with a new bioceramic sealer in the presence or absence of smear layer. Aust Endod J. 2013;39(3):102–106. doi: 10.1111/j.1747-4477.2011.00310.x. [DOI] [PubMed] [Google Scholar]
- 22.Ulusoy Öİ, Nayir Y, ÇElik K, et al. Apical microleakage of different root canal sealers after use of maleic acid and EDTA as final irrigants. Braz Oral Res. 2014;28(1):1–6. doi: 10.1590/1807-3107BOR-2014.vol28.0048. [DOI] [PubMed] [Google Scholar]
- 23.Bidar M, Sadeghalhoseini N, Forghani M, et al. Effect of the smear layer on apical seals produced by two calcium silicate-based endodontic sealers. J Oral Sci. 2014;56(3):215–219. doi: 10.2334/josnusd.56.215. [DOI] [PubMed] [Google Scholar]
- 24.Gandhi B, Halebathi-Gowdra R. Comparative evaluation of the apical sealing ability of a ceramic based sealer and MTA as root-end filling materials - an in-vitro study. J Clin Exp Dent. 2017;9(7):e901–e9e5. doi: 10.4317/jced.53903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fernandez R, Restrepo JS, Aristizabal DC, et al. Evaluation of the filling ability of artificial lateral canals using calcium silicate-based and epoxy resin-based endodontic sealers and two gutta-percha filling techniques. Int Endod J. 2016;49(4):365–373. doi: 10.1111/iej.12454. [DOI] [PubMed] [Google Scholar]
- 26.Zhang W, Li Z, Peng B. Effects of iRoot SP on mineralization-related genes expression in MG63 cells. J Endodont. 2010;36(12):1978–1982. doi: 10.1016/j.joen.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 27.Zaki DY, Zaazou MH, Khallaf ME, et al. In vivo comparative evaluation of periapical healing in response to a calcium silicate and calcium hydroxide based endodontic sealers. Open Access Macedonian J Med Sci. 2018;6(8):1475–1479. doi: 10.3889/oamjms.2018.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nirupama DN, Nainan MT, Ramaswamy R, et al. In vitro evaluation of the antimicrobial efficacy of four endodontic biomaterials against enterococcus faecalis, Candida albicans, and Staphylococcus aureus. Int J Biomater. 2014;2014:383756. doi: 10.1155/2014/383756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang H, Shen Y, Ruse ND, et al. Antibacterial activity of endodontic sealers by modified direct contact test against enterococcus faecalis. J Endod. 2009;35(7):1051–1055. doi: 10.1016/j.joen.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 30.Candeiro GTM, Moura-Netto C, D'Almeida-Couto RS, et al. Cytotoxicity, genotoxicity and antibacterial effectiveness of a bioceramic endodontic sealer. Int Endod J. 2016;49(9):858–864. doi: 10.1111/iej.12523. [DOI] [PubMed] [Google Scholar]
- 31.Wang Z, Shen Y, Haapasalo M. Dentin extends the antibacterial effect of endodontic sealers against enterococcus faecalis biofilms. J Endod. 2014;40(4):505–508. doi: 10.1016/j.joen.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 32.Ozcan E, Yula E, Arslanoglu Z, et al. Antifungal activity of several root canal sealers against Candida albicans. Acta Odontol Scand. 2013;71(6):1481–1485. doi: 10.3109/00016357.2013.771405. [DOI] [PubMed] [Google Scholar]
- 33.Chybowski EA, Glickman GN, Patel Y, et al. Clinical outcome of non-surgical root canal treatment using a single-cone technique with Endosequence bioceramic sealer: a retrospective analysis. J Endod. 2018;44(6):941–945. doi: 10.1016/j.joen.2018.02.019. [DOI] [PubMed] [Google Scholar]
- 34.de Chevigny C, Dao TT, Basrani BR, et al. Treatment outcome in endodontics: the Toronto study--phase 4: initial treatment. J Endod. 2008;34(3):258–263. doi: 10.1016/j.joen.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 35.Leonardo MR, da Silva LA, Almeida WA, et al. Tissue response to an epoxy resin-based root canal sealer. Endod Dent Traumatol. 1999;15(1):28–32. doi: 10.1111/j.1600-9657.1999.tb00745.x. [DOI] [PubMed] [Google Scholar]
- 36.Grecca FS, Leonardo MR, da Silva LA, et al. Radiographic evaluation of periradicular repair after endodontic treatment of dog's teeth with induced periradicular periodontitis. J Endod. 2001;27(10):610–612. doi: 10.1097/00004770-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Kerekes K, Tronstad L. Long-term results of endodontic treatment performed with a standardized technique. J Endod. 1979;5(3):83–90. doi: 10.1016/S0099-2399(79)80154-5. [DOI] [PubMed] [Google Scholar]
- 38.Sari S, Duruturk L. Radiographic evaluation of periapical healing of permanent teeth with periapical lesions after extrusion of AH plus sealer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(3):e54–e59. doi: 10.1016/j.tripleo.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 39.Zmener O, Pameijer CH. Clinical and radiographic evaluation of a resin-based root canal sealer: an eight-year update. J Endod. 2010;36(8):1311–1314. doi: 10.1016/j.joen.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 40.Ricucci D, Rocas IN, Alves FR, et al. Apically extruded sealers: fate and influence on treatment outcome. J Endod. 2016;42(2):243–249. doi: 10.1016/j.joen.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 41.Nosrat A, Nekoofar MH, Bolhari B, et al. Unintentional extrusion of mineral trioxide aggregate: a report of three cases. Int Endod J. 2012;45(12):1165–1176. doi: 10.1111/j.1365-2591.2012.02082.x. [DOI] [PubMed] [Google Scholar]
- 42.Lin LM, Skribner JE, Gaengler P. Factors associated with endodontic treatment failures. J Endod. 1992;18(12):625–627. doi: 10.1016/S0099-2399(06)81335-X. [DOI] [PubMed] [Google Scholar]
- 43.Escoda-Francoli J, Canalda-Sahli C, Soler A, et al. Inferior alveolar nerve damage because of overextended endodontic material: a problem of sealer cement biocompatibility? J Endod. 2007;33(12):1484–1489. doi: 10.1016/j.joen.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 44.Pasqualini D, Scotti N, Ambrogio P, et al. Atypical facial pain related to apical fenestration and overfilling. Int Endod J. 2012;45(7):670–677. doi: 10.1111/j.1365-2591.2012.02021.x. [DOI] [PubMed] [Google Scholar]
- 45.Gonzalez-Martin M, Torres-Lagares D, Gutierrez-Perez JL, et al. Inferior alveolar nerve paresthesia after overfilling of endodontic sealer into the mandibular canal. J Endod. 2010;36(8):1419–1421. doi: 10.1016/j.joen.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 46.Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–625. doi: 10.1097/01.ede.0000135174.63482.43. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.