Abstract
Tubulinopathy commonly refers to complex congenital and non-progressive brain malformations caused by mutations in the tubulin genes. Among tubulin-encoding genes, TUBB3 has rarely been reported as a cause of complex cortical malformations. Herein, we report a case of tubulinopathy in a 21-month-old boy who presented with delayed development. He could not walk on his own and was not able to speak more than five words. Physical examination revealed right esotropia and hypotonia of the lower extremities. MRI showed dysmorphic brainstem and dysmorphic and hypertrophic basal ganglia. The right thalamus was relatively smaller than the left one. The cerebellum showed disorganization of the cerebellar folia. DNA sequencing revealed a missense mutation of the TUBB3 gene.
Keywords: Nervous System Malformations, Brain, Neuroimaging, Tubulin, Microtubules
Abstract
튜불린병증, 즉 튜불린 유전자의 변이는 복합 뇌피질 발달 기형의 원인으로 알려져 있다. 그중에서 TUBB3 유전자가 기형의 원인인 사례는 매우 드물어 이를 보고하고자 한다. 21개월 남아가 발달지연을 주소로 내원하였다. 환아는 혼자 걷지 못하였고 구사 가능한 단어가 5개 이내였다. 신체검사상 우측 내사시와 양하지 근력저하가 관찰되었다. 뇌 자기공명영상에서 뇌간의 이형성, 기저핵의 이형성 및 과형성 소견이 보였고 우측 시상의 크기가 좌측보다 작았으며 붕괴된 소뇌이랑의 소견이 보였다. DNA 염기서열 분석 결과 TUBB3 유전자의 과오돌연변이가 확인되었다.
INTRODUCTION
Microtubules, composed of tubulin are essential for neuronal migration and axon guidance in developing brain. Tubulinopathy is mutations in tubulin genes commonly cause complex congenital and non-progressive brain malformations. Among tubulin-encoding genes, TUBB3 gene has rarely been reported as cause of complex cortical malformation. Here, we report a case of 21-month-old boy with TUBB3 gene mutation presented with delayed development.
CASE REPORT
A 21-month-old boy was admitted to our rehabilitation medicine department with complaints of delayed development. He could stand with holding by himself but not walk by himself and he wasn't able to speak more than five words. On physical exam, he had right esotropia, poor dynamic stability of proximal muscles during gait and muscle power weakness of lower extremities. He was the second child of healthy parents, and his older sister was healthy. He was born at 37 gestational weeks with a birth weight of 2670 g (5th percentile) and his perinatal history was uneventful. Bayley scales of infant development reveled 11 months old in cognitive scale and 9 months old in motor scale.
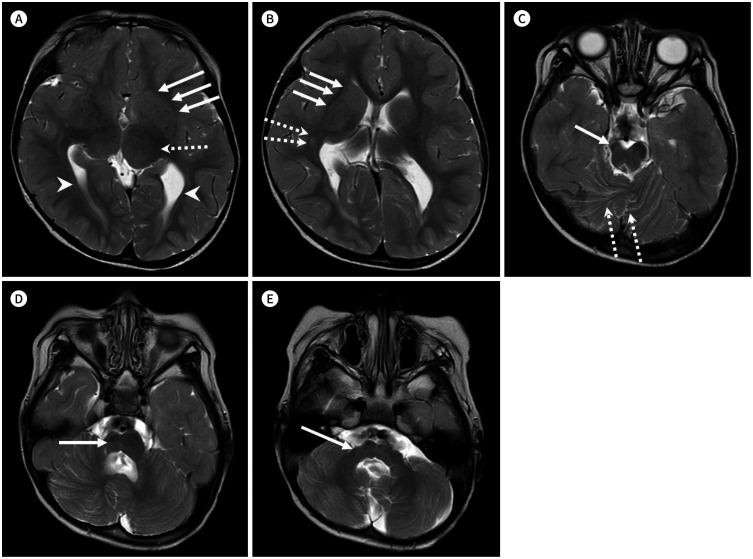
MRI showed dysmorphic and hypertrophic basal ganglia with fusion between the putamen and caudate nucleus with indiscernible anterior limb of both internal capsules (Fig. 1A, B). Asymmetry of both lateral ventricles (Fig. 1A) and both thalamus were seen (Fig. 1A). An iso to slightly high signal intensity lesion at the right peritrigonal white matter indicated thickened external sagittal striatum or heterotopia (Fig. 1B). A disorganization of cerebellar folia was seen (Fig. 1C). The brain stem was dysmorphic with atrophy of right sided brainstem (Fig. 1C, D) and right middle cerebellar peduncle (Fig. 1E). These findings suggested complex cortical malformation caused by tubulinopathy.
Fig. 1. Brain imaging of a 21-month-old boy with delayed development reveals complex cortical malformations.
A. The hypertrophic left basal ganglia shows fusion between the putamen and the caudate nucleus with an indiscernible anterior limb of both the internal capsules (arrows). The left thalamus is relatively larger than the right thalamus (dashed arrow). The lateral ventricles are asymmetric (arrowheads).
B. The hypertrophic right basal ganglia shows fusion between the putamen and the caudate nucleus with an indiscernible anterior limb of both the internal capsules (arrows). An iso- to slightly high signal intensity lesion at the right peritrigonal white matter indicates a thickened external sagittal striatum or heterotopia (dashed arrows).
C. Dysmorphic brainstem with atrophy of the right midbrain (arrow) and disorganization of the cerebellar folia (dashed arrows) are seen.
D. The right pons shows atrophic changes (arrow).
E. The right middle cerebellar peduncle shows atrophic changes (arrow).
The malformation of cortical development targeted sequencing revealed a missense mutation of TUBB3 gene, c.646G>A (p.Glu216Lys) (Table 1).
Table 1. Results of Targeted Gene Sequencing for Malformations of Cortical Development.
| ACMG Classification | Gene | Accession | Nucleotide | Amino Acid | Zygosity | Inheritance |
|---|---|---|---|---|---|---|
| Likely pathogenic | TUBB3 | NM_001197181.1 | c.646G>A | p.Glu216Lys | Hetero | AD |
ACMG = American College of Medical Genetics and Genomics, AD = autosomal dominant
DISCUSSION
Tubulins compose microtubule, a filamentous structure, which is critical to the processes of mitosis, axon navigation, and neuron migration, all key factors in brain development (1). Thus mutations in tubulin genes can alter the normal function and structure of microtubules, leading to complex congenital and non-progressive disorders of brain development characterized by severe brain malformations (2). Disorders caused by mutations in the tubulin gene family were recognized as tubulinopathy.
Among tubulin encoding genes, diseases caused by mutations in TUBB3 are rare, and only 15 TUBB3 mutations have been identified (3). TUBB3 encodes beta tubulin isotype 3, a neuron-specific component of microtubules. Heterozygous missense mutations in TUBB3 have been reported to be associated with decreased microtubule stability (4).
Clinical symptoms result from hypoplasia of the oculomotor nerve are esotropia, nystagmus and paralytic eye movement disorder, such as congenital fibrosis of extraocular muscle, CFEOM3 (5). Patients show gross motor delays associated with axial hypotonia, sensorimotor polyneuropathy and intellectual disability (4).
In radiologic finding, tubulinopathy results in multiple malformations including microcephaly, lissencephaly, cerebellar hypoplasia, band heterotopia and other types of cortical dysgenesis due to impaired neuronal migration. Impaired axonal pathfinding lead anomalies of white matter pathways and anomalies of cranial nerves. Other findings are hypoplasia or absence of the corpus callosum, a small asymmetric brain stem, fused striatum due to absence of various parts of the internal capsule (most commonly the anterior limb). These are some characteristic features to be recognized on routine MR imaging (1).
In our case, the patient had symptoms indicated tubulinopathy, such as right esotropia, hypotonia of lower extremities, intellectual disability and delayed development. MRI showed dysmorphic basal ganglia with fusion of the caudate and putamen and hypoplastic and dysmorphic brain stem. Additionally in our case, the cerebellum showed disorganization of cerebellar folia. In our knowledge this finding was not yet reported.
Based on our review, the MRI findings play essential role in diagnosis of tubulinopathy. Thus, in a patient with combination of delayed development, dysgyria, dysmorphic basal ganglia and brain stem, the tubulinopathy should be considered.
Footnotes
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
- Conceptualization, P.N.H.
- supervision, P.N.H.
- writing—original draft, L.Y.H.
- writing—review & editing, P.N.H.
References
- 1.Mutch CA, Poduri A, Sahin M, Barry B, Walsh CA, Barkovich AJ. Disorders of microtubule function in neurons: imaging correlates. AJNR Am J Neuroradiol. 2016;37:528–535. doi: 10.3174/ajnr.A4552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arrigoni F, Romaniello R, Peruzzo D, Poretti A, Bassi MT, Pierpaoli C, et al. The spectrum of brainstem malformations associated to mutations of the tubulin genes family: MRI and DTI analysis. Eur Radiol. 2019;29:770–782. doi: 10.1007/s00330-018-5610-0. [DOI] [PubMed] [Google Scholar]
- 3.Shimojima K, Okamoto N, Yamamoto T. A novel TUBB3 mutation in a sporadic patient with asymmetric cortical dysplasia. Am J Med Genet A. 2016;170A:1076–1079. doi: 10.1002/ajmg.a.37545. [DOI] [PubMed] [Google Scholar]
- 4.Whitman MC, Andrews C, Chan WM, Tischfield MA, Stasheff SF, Brancati F, et al. Two unique TUBB3 mutations cause both CFEOM3 and malformations of cortical development. Am J Med Genet A. 2016;170A:297–305. doi: 10.1002/ajmg.a.37362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bahi-Buisson N, Poirier K, Fourniol F, Saillour Y, Valence S, Lebrun N, et al. The wide spectrum of tubulinopathies: what are the key features for the diagnosis? Brain. 2014;137:1676–1700. doi: 10.1093/brain/awu082. [DOI] [PubMed] [Google Scholar]