Abstract
Eosinophilic esophagitis (EoE) is an emerging allergen-mediated disease characterized by symptoms of esophageal dysfunction and eosinophilic inflammation. EoE diagnosis requires 15 eosinophils per high power field (eos/HPF) in tissue biopsies endoscopically obtained. The need for several endoscopies to monitoring the disease and the absence of validated non-invasive biomarkers or tools are the main reasons for the significant burden on affected patients and the healthcare system. There is a critical need for non-invasive or minimally invasive biomarkers. In the last years, several efforts have been made to identify potential biomarkers for diagnosing and monitoring the disease that we summarized in this review. The future of EoE is exciting from both a diagnostic and therapeutic standpoint. Further research is required to confirm pheno-types and histological or serological biomarkers to provide a novel endotype classification based on different cytokine or genetic signatures relevant to precision medicine. (www.actabiomedica.it)
Keywords: eosinophilic esophagitis, biomarkers, cytokines, genes, atopy
Introduction
Eosinophilic gastrointestinal disorders (EGIDs) are emerging inflammatory diseases which may involve any part of the gastrointestinal (GI) tract and lead to the eosinophilic mucosal infiltration in the absence of secondary causes of intestinal eosinophilia (1, 2). Based on the site of the eosinophil inflammations, EGIDs are classified into eosinophilic esophagi-tis (EoE) and nonesophageal EGIDs, distinct in eo-sinophilic gastritis (EoG), gastroenteritis (EoGE), and colitis (EoC) (1). While nonesophageal EGIDs still represent a clinical enigma for clinicians, EoE is considered the prototype of EGIDs with standardized guidelines (1, 3). EoE is a chronic/remittent, allergen-mediated disease characterized by esophageal dysfunction and eosinophilic infiltration, affecting both children and adults, with a male-female ratio of 3:1 (4). The prevalence of EoE is significantly increased in the last decade. It is currently considered one of the most common causes of upper gastrointestinal morbidity, detected in 12% — 23% of patients undergoing endoscopy for dysphagia and about 50% of subjects with food impaction (4, 5). EoE diagnosis requires 15 eosinophils per high power field (eos/HPF) in tissue biopsies endoscopically obtained, without concomitant eosinophilic infiltration in other GI tracts (3). The need for several endoscopies to monitoring the disease and the absence of validated non-invasive biomarkers or tools are the main reasons for a significant burden on affected patients and the healthcare system (6). In the last years, several efforts have been made to identifypotential non-invasive biomarkers for diagnosing and monitoring the disease. Biomarkers may provide new insight into the understanding of EoE pathogenesis and defining potential endotypes with relevant impact on precision medicine.
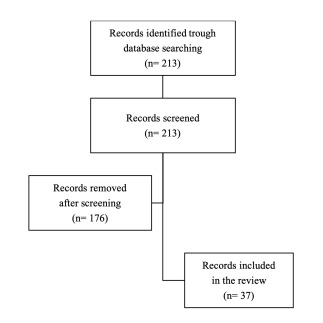
Biomarkers are measures of biological status. According to the Food and Drug Administration (FDA) — National Institutes of Health (NIH) definition, a bi-omarker is a “defined characteristic measured as an indicator of normal biological processes, pathogenic processes or responses to an exposure or intervention” (7). This definition is broad and encompasses therapeutic interventions and molecular, histologic, radiographic, or physiologic characteristics. According to their putative applications, several categories of biomarkers have been identified, and often, they may overlap each other (Table 1) (8). Notably, an ideal biomarker should present different features, such as reasonable costs and a significant impact on clinical management (Table 2). This review aimed to summarize current evidence on non-invasive biomarkers for EoE diagnosis and monitoring, highlighting promising tools and future potential candidates. We performed a non-systematic review of articles via the online database PubMed, combining the terms “eosinophilic esophagitis” AND “biomarkers.” The literature review was performed in May 2021. All studies that met the following criteria were included: 1) case series, cross-sectional and cohort studies, published in English in peer-reviewed journals in the last ten years, 2) participants were children and adult patients diagnosed with EoE, according to current guidelines (3). Articles were also required to assess non-invasive biomarkers. Potentially eligible publications were manually screened and reviewed, and non-relevant publications were excluded (figure 1).
Table 1. Biomarker classification and definition.
| Biomarker classification | Definition |
|---|---|
| Diagnostic Biomarker (DB) | A DB detects or confirms the presence of a disease or identifies an individual with a disease subtype. |
| Monitoring Biomarker (MB) | An MB assesses the status of a disease or detects the clinical (efficacy and safety) and pharmacodynamic effects of treatment (i.e., biological therapy). |
| Predictive Biomarkers (PreB) | A PreB assesses if the exposure to therapy or environmental agent induces favorable or unfavorable effects in a patient or group of individuals. |
| Prognostic Biomarkers (ProB) | A ProB can identify the likelihood of a clinical event, disease recurrence, or progression in affected patients. |
| Risk Biomarker (RB) | An RB indicates the potential for developing a disease in a healthy individual. |
Table 2. Features of an ideal biomarker for the diagnosis and monitoring of EoE.
| Features of an ideal biomarker |
|---|
| Correlate with the EoE state |
| Connect with EoE severity |
| Non-invasive and easy to collect or perform |
| Standardized |
| Have high sensitivity |
| Carry high specificity |
| Cost-effective |
| Low biological variation |
Figure 1. Methods and search strategy.
Serological and biochemical markers
Blood eosinophils, eosinophil granule, and cell-surface proteins
Considering the allergic pathogenesis, most studies have focused on the rationale that EoE patients may have elevated peripheral eosinophils compared to healthy controls or subjects with gastroesophageal reflux disease (GERD) (Table 3) (9-11). Many of these studies showed that peripheral eosinophil levels might increase during active disease, but whether this marker alone reflected mucosal inflammation is still unclear. Recently, Wechsler et al. have demonstrated that absolute eosinophil count (AEC), together with a panel of plasma biomarkers, such as galectin-10 (GAL-10), eosinophil cationic protein (ECP), eosinophil-derived neurotoxin (EDN), eotaxin-3 (EOT3), and major basic protein 1 (MBP-1) were useful to identify EoE subjects and predicted esophageal eosinophilia (10). Another study showed that AEC, ECP, EDN, and interleukin-(IL)-5 had statistically significant correlations with esophageal eosinophilia (11). Less recently, Rodriguez-Sanchez et al. assessed the potential usefulness of eosinophil activity markers (peripheral eo-sinophils, total serum IgE, ECP) as a predictor of diet response. Authors demonstrated that peripheral blood eosinophils decreased significantly in responders but not in non-responders patients (9).
Table 3. Serum biomarkers of EoE.
| Author, year | Population | Study | Biomarkers | Outcome |
|---|---|---|---|---|
| Rodriguez-Sanchez et al, 2013 (9) | 30Adults | Cross-sectional | ECP, total IgE, peripheral blood eosinophils, and the maximum peak of eosinophils/hpf | Serum total IgE and ECP do not act as markers for EoE activity |
| Wechsler et al, 2021(10) | 71Children and adolescents | Prospective case-control study | Blood AEC.Plasma EDN, ECP, MBP-1,GAL-10, EOT2, EOT3.Urine OPN and MMP-9 | Plasma (GAL-10, ECP, EDN, Eotaxin-3, MBP-1), and urine (OPN) biomarkers were increased in EoE compared to control. Therefore, GAL-10 is a potential biomarker for EoE screening |
| Min et al, 2017 (11) | 115Children and adults | Prospective case-control study | Serum analysis of AEC, EOT3 EDN, ECP, and IL-5 | , AEC, ECP, and EDN were higher in EoE subjects compared to controls and correlated with the degree of esophageal eosinophilia |
| Nguyen et al, 2011 (12) | 77Children and adolescents | Case-control study | CD66b, phospho-STAT1, and phospho-STAT6 | Measurements of CD66b and phospho-STAT levels in peripheral eosinophils may be beneficial for identifying EoE |
| Morris et al, 2017 (13) | 31Children and adolescents | Case-control study | Peripheral blood EoP. | EoP levels were increased in patients with active EoE and significantly correlated with esophageal eosinophilia |
| Johansson et al, 2020 (14) | 25Adults | Prospective study | IIb-integrin (CD41) | CD41 associated with circulating eosinophils is a potential non-invasive biomarker for esophageal eosinophilic inflammation |
| Schwartz et al, 2019 (15) | 31Children and adolescents | Retrospective study | Peripheral blood EoP | Blood EoP correlates with tissue pathology during activeEoE |
| Author, year | Population | Study | Biomarkers | Outcome |
| Henderson et al, 2020 (16) | 34Children and adolescents | Prospective study | Circulating eosinophil progenitors | Blood EoP levels may be used as a biomarker to detect active EoE disease |
| Subbarao et al, 2011 (17) | 80Children and adolescents | Case-control study | Serum IL-5 and EDN | Serum EDN levels were significantly higher in subjects with EoE than controls |
| Schlag et al, 2013 (18) | 15Adults | Prospective observational study | ECP and TRP | ECP but not TRP could be a promising non-invasive biomarker to assess response to topical corticosteroid therapy |
| Domenech Witek et al,2017 (18) | 19Adults | Retrospective study | Serum ECP | The serial determination of ECP was proper to monitor patients with EoE |
| Cengiz, 2019 (20) | 29Adults | Case-control study | Serum ECP | Serum ECP level was significantly higher in patients with EoE than in controls. In addition, ECP is strongly correlated with EREFS and the symptom of food impaction |
| Wright et al, 2018 (21) | 39Adults | Prospective case-control study | Serum EPX | EoE subjects had significantly lower median EPX levels |
| Lu et al, 2018 (23) | 31Children and adolescents | Case-control study | Serum 15-HETE | 15(S)-HETE may aid in the diagnosis of EoE |
| Dellon et al, 2016 (24) Dellon et al, 2015 (25) | 61Adults | Case-control study | Serum periostin. Serum IL-4, IL-5, IL-6, IL-9, IL-13, TGF-a, TGF-P, TNF-a, EOT-1, -2, and -3,TSLP, MBP, and EDN | Serum periostin and cytokines levels were similar in cases and controls, and there were no changes post-treatment |
| Dellon et al, 2017 (27) | 48Adults | Case-control study | Autoantibodies (IgG1 and IgG4) to DSG1, DSG3, and to collagen XVII (NC16A) | Anti-NC16A and anti-DSG3 IgG4 autoantibodies were strongly associated with EoE. Anti-NC16A levels decreased significantly in EoE cases with a histologic response after topical corticosteroid treatment |
AEC, absolute eosinophil count; CD, cluster of differentiation; DSG, desmoglein; ECP, eosinophil cationic protein; EDN, eosinophil-derived neurotoxin; EoPs, eosinophil progenitors; EOT, eotaxin; EPX, eosinophil peroxidase; GAL-10, galectin-10; HETE, hydroxyeicosatetraenoic acid; Ig, immunoglobulin; IL, interleukin; MBP-1, major basic protein-1; MMP, matrix metalloproteinase; OPN, osteopontin; STAT, signal transducer and activator of transcription; TGF, transforming growth factor; TLSP, thymic stromal lymphopoietin; TNF, tumor necrosis factor; TRP, tryptase.
Other studies have evaluated blood eosinophil progenitors (EoP) and eosinophil-surface markers with promising results (12-14). Johansson et al. recently reported that platelet activation and platelet-eosinophil association pathways might be involved in EoE patho-genesis, showing that CD41 (aIIb-integrin subunit) expressed on eosinophils surface was a potential non-invasive biomarker for esophageal eosinophilic inflammation (14). Another study examined whether phe-notypic analysis of eosinophil surface markers could distinguish treated from untreated disease. In 2011, Nguyen et al. found elevated surface CD66 intracellu-lar phospho-STAT1 and phospho-STAT6, which differentiated children with active EoE from treated and healthy controls (12, 15, 16). Three studies recently assessed the levels of blood EoP as potential biomarkers of active EoE, esophageal inflammation, and response to treatments both in children both adults (13, 15, 16).
Eosinophil granule proteins have been investigated as other potential markers of disease, showing inconsistent and conflicting results (17-21). Subbarao et al. determined that EDN levels provided a sustained decrease following treatment in 66 children with EoE (17). More recently, a small prospective study of 15 adults showed that serum ECP, but not tryptase (TRP), significantly correlated with tissue eosinophils after swallowed steroid therapy (18). Moreover, ECP was high in adults with EoE, and its serial determination was also helpful in monitoring the disease (1920).
Recent evidence suggested a pathogenetic role for arachidonate 15-lipooxygenase (ALOX15) in EoE. ALOX15 is upregulated and overexpressed in mu-cosal biopsies of EoE patients (22). 15(S)-hydroxye-icosatetraenoic acid (15(S)-HETE), a metabolite of ALOX15, detectable in peripheral blood, was found elevated in the EoE compared to the non-EoE group, suggesting its potential role as a disease indicator (23).
Type 2 (T2) cytokines
With an advanced understanding of EoE patho-genesis, several studies sought to assess whether T2 cy-tokines, including interleukin (IL)-4, IL-5, IL-6, IL-9, IL-13, TGF-a, transforming growth factor (TGF)-P, tumor necrosis factor (TNF)-a, EOT-1, -2, -3, thymic stromal lymphopoietin (TSLP) and periostin were increased in the peripheral circulation of affected patients (24, 25). Therefore, peripheral cytokine measurements did not consistently characterize the esopha-geal inflammation or disease activity. In addition, the results of these studies are limited by the confounding influence of other concomitant allergic diseases.
Autoantibodies
EoE has been associated with a range of autoimmune conditions, such as inflammatory bowel diseases, coeliac disease, vasculitis, or type 1 diabetes mellitus (26). Moreover, esophageal epithelial barrier dysfunction is essential in EoE pathogenesis. Antibodies against epithelial adhesion molecules are founded in several autoimmune skin conditions. Therefore, EoE may even be associated with these specific au-toantibodies. Dellon et al. recently demonstrated that anti-collagen XVII (NC16A) and anti-desmoglein 3 (DSG3) IgG4 autoantibodies were strongly associated with EoE. Moreover, anti-NC16A levels decreased significantly in EoE patients after topical corticoster-oid treatment (27).
Histopathological biomarkers
Immunohistsochemical markers
Diagnosis of EoE requires more than 15 eos/HPF in the esophageal tracts. Therefore, other diagnostic histological findings, including a thickened mucosa with basal layer hyperplasia and papillary lengthening, eosin-ophil surface layering, and eosinophilic microabscesses, have been proposed (28). Several studies assessing his-tological biomarkers have been reported. Extracellular deposition of eosinophil granule proteins, such as eo-sinophil peroxidase (EPX), is present in the esophagus of patients with EoE and positively correlates with the peak of tissue eosinophils (Table 4) (29, 30). Moreover, EPX levels decreased in treatment responders (29). On the contrary, Schroeder et al. demonstrated that the less invasive assessment of pharyngeal EPX did not correlate with the esophageal eosinophil count in children with EoE compared to healthy controls (31).
Table 4. Immunohistochemical biomarkers.
| Author, year | Population | Study | Biomarkers | Outcome |
|---|---|---|---|---|
| Wright et al,2021(29) | 87Adults | Case-control study | EPX | EPX was strongly correlated with tissue eosinophils accurately identified subjects with EoE and decreases in treatment responders |
| Saffari et al, 2017 (30) | 36Adults | Case-control study | EPX | EPX levels from esophageal mucosal samples correlated with eosinophilic inflammation |
| Schroeder etal, 2017 (31) | 21Children and adolescents | Case-control study | Pharyngeal andnasal EPX | EPX levels from the throat swabs do not correlate with esophageal eosinophil counts |
| Peterson et al,2019 (32) | 34Adults | Retrospective study | MBP1 | MBP1 is increased in esophageal biopsy specimens from symptomatic patients with EoE and may be a marker of disease activity |
| Kim et al, 2019 (33) | 72Adults | Retrospective study | TRP, EDN, and EOT3 | TRP, EDN, and EOT3 could be promising biomarkers for disease activity, symptoms, and endoscopic response |
| Dellon et al,2020 (34) | 110Adults | Retrospective study | MBP, EOT3, andTRP | Pretreatment MBP, EOT3, and TRP levels were not strongly associated with response to topical steroids. In contrast, elevated TRP levels may be associated with nonresponse compared with complete response |
| Dellon et al, 2014 (35) | 196Adults | Case-control study | MBP, EOT3, andTRP | Esophageal tissues from patients with EoE have substantially higher MBP, EOT3, and tryptase than controls |
| Dellon et al,2012 (36) | 105Children and adults | Case-control study | MBP and EOT3 | Patients with EoE had substantially higher levels of MBP and EOT3 staining than GERD patients |
| Smadi et al,2018 (37) | 94Children and adults | Prospectivecross-sectionalstudy | EDN | EDN in brushing samples is significantly higher in patients having active EoE compared to healthy controls, GERD, and EoE in remission |
| Hui et al,2017 (39) | 21Children and adolescents | Retrospective case-control study | ALOX15 | ALOX15 immunohistochemistry helped support the diagnosis of EoE in situations with strong clinical suspicion |
| Clayton et al, 2014 (40) | 30Adults | Retrospective case-control study | IgG4 | The level of IgG4-positive plasma cells was increased in the lamina propria and granular extracellular IgG4 deposits |
| Zukerberg etal, 2016 (41) | 46Adults | Case-control study | IgG4 deposits | 76% of EoE cases showed int extracellular IgG4 deposits, whereas all GERD cases were negative |
| Rosenberg etal, 2018 (42) | 36Children and adolescents | Case-control study | IgG4 | Tissue IgG4 levels correlated with esophageal eosinophil counts, histologic grade, stage scores, IL-4, IL-10, IL-13 expression, and had strong associations with a subset of the EoE transcriptome |
| ALOX, arachidonate lipoxygenase; EDN, eosinophil-derived neurotoxin; EPX, eosinophil peroxidase; GERD, gastroesophageal reflux disease; Ig, immunoglobulin; IL, interleukin; MBP-1, major basic protein-1; TRP, tryptase. | ||||
Other eosinophil granule proteins, such as MBP-1, TRP, EDN, and EOT-3, have been evaluated as potential histological biomarkers of EoE and response to therapy, with conflicting results. (32-36). Notably, EDN in brushing samples obtained with the nasogas-tric endoscopy was significantly higher in children and young adults with active EoE than patients in remission, healthy controls, and GERD. (37).
Other tissue markers
ALOX15 plays an essential role in the metabolism of fatty acids and the production of various cytokines and chemokines. ALOX15 is expressed in blood eosinophils and respiratory epithelium. ALOX15 is also upregulated in the esophageal epithelium from patients with active EoE in contrast to esophageal fragments from patients in remission, subjects with GERD, or healthy controls (38). Thus, ALOX15 immunohistochemistry may be helpful in the diagnosis of cases with clinical features of EoE but that do not meet the histological criteria (39).
IgG4
The role of immunoglobulin G4 (IgG4) in EoE pathogenesis has not been precisely defined, and available studies reported conflicting data. One of the first studies showed an increased level of IgG4-positive plasma cells (IgG4-PC) in the lamina pro-pria and granular extracellular IgG4 deposits (40). Zuckeberg et al. reported IgG4 deposits between the squamous cells in biopsies from patients with EoE.
Moreover, IgG4 in the esophagus showed a positive correlation with concurrent peak tissue eosino-philia, histological grade, and stage according to the EoE histology scoring system (EoEHSS) (42). However, the high amount of IgG4 in esophageal mucosa still represents a conundrum. Thus, current data do not conclusively determine if high tissue IgG4 titers could be good predictors of diet response in EoE patients.
Microribonucleic acids (miRNAs) and DNA methylation
MiRNAs are single-stranded RNA molecules of 19-25 nucleotides involved in the post-transcriptional gene silencing. Several studies reported that EoE patients had a marked change in tissue-specific gene expression (Table 5). Lu et al. investigated esophageal miRNA expression profile in patients with active disease and responsive to steroids, finding that the expression levels of the most upregulated miRNAs (miR-21 and miR-223) and the most downregulated miRNA (miR-375) strongly correlated with esophageal eosin-ophil levels (43). More recently, Bhardwaj et al. found that the expression of salivary miR-4668 is higher in EoE compared to non-EoE subjects, suggesting its potential role as a non-invasive biomarker (44).
Table 5. Epigenetic biomarkers.
| Author, year | Population | Study | Biomarkers | Outcome |
| Lu et al, 2012 (43) | 29Children and adolescents | Case-control study | miRNAs | The expression levels of the most upregulated miRNAs (miR-21 and miR-223) and the most downregulated miRNA (miR-375) were strongly correlated with esophageal inflammation |
| Bhardwaj et al, 2020 (44) | 44Adults | Case-control study | Salivary miR-4668-5p | The expression of miR-4668 is higher in EoE vs. non-EoE subjects, suggesting its potential role as a non-invasive biomarker |
| Strisciuglio et al, 2021 (45) | 20Children and adolescents | Case-control study | Mucosal DNAmethylationprofile | Analyses revealed striking disease-associated differences in mucosal DNA methylation profiles in children diagnosed with EoE compared to controls |
| Jensen et al, 2020 (46) | 36Children and adults | Case-control study | DNAmethylation profile | EoE patients that respond versus do not respond to treatment have differences in their methylation profile |
DNA, deoxyribonucleic acid; RNA, ribonucleic acid.
Other epigenetic mechanisms, different from miRNA and involved in EoE pathogenesis or response to therapies, have been recently assessed. For example, pediatric patients with EoE showed differences in mucosal DNA methylation profiles compared to controls(45). Moreover, DNA methylation differences have also been found in responder and non-responder patients(46)
Other non-invasive biomarkers
Exhaled nitric oxide
Fractional exhaled nitric oxide (FeNO) is a bio-marker of eosinophilic asthma (47). However, considering the common atopic etiology, FeNO was also measured in a prospective study of 11 non-asthmatic subjects with active esophagitis before and after treatment, without any supporting role in the management of EoE (Table 6) (48). Moreover, FeNO did not help distinguish EoE from GERD (48). Therefore, no studies have shown a potential role of FeNO in EoE diagnosis and monitoring (49).
Table 6. Other non-invasive biomarkers.
| Author, year | Population | Study | Biomarkers | Outcome |
| Leung et al, 2013 (48) | 11Children and adults | Prospective study | FeNO | No supporting role for FeNO determination in the management of EoE |
| Lanz et al, 2012 (49) | 55Children and adolescents | Case-control study | FeNO | Measurement of FeNO does not help identify EoE from GERD |
| Moye et al, 2019 (50) | 24Children and adolescents | Prospectivecase-controlstudy | Plasmametabolomicsprofile | Notable candidate biomarkers include dimethylarginine, putrescine, and N-acetylputrescine |
| Cunnion et al, 2016 (51) | 75Children and adults | Case-control study | Urinary 3-BT | Median normalized 3-BT levels were increased 93-fold in patients with EoE compared to controls |
BT, bromotyrosine; FeNO, Fractionated exhaled nitric oxide; GERD, gastroesophageal reflux disease.
Metabolomics
Only one study assessed the metabolomic profile in patients with EoE. However, Moye et al. showed that plasma urea cycle metabolites (dimethylarginine, putrescine, and N-acetylputrescine) are elevated in children with EoE, and their levels are modified by proton pump inhibitor treatment (50).
3-Bromotyrosine (3-BT) is a chemical marker of eosinophil activation and is high in patients with asthma. Cunnion et al. found that 3-BT levels were increased 93-fold in patients with EoE compared to controls, providing proof of concept testing urine by a mass spectrometry method (Eosinophil Quantitated Urine Kinetic, EoQUIK) can provide a non-invasive tool to evaluate eosinophil degranulation in EoE (51).
Genetic risk loci
Eosinophilic esophagitis is a multifactorial disease. Although recent evidence suggested a fundamental pathogenetic role of the environmental factors, several studies have also reported that genetic predisposition is a significant risk factor in the development of EoE (52). Different studies, including candidate-gene identification and genome-wide association studies (GWAS), have identified gene loci that have been associated explicitly with EoE (53). These gene loci are categorized into four major groups: 1) genes involved in Type 2 (T2) inflammation, 2) epithelial barrier dysfunction, 3) enhanced fibrosis, and 4) altered immune response (54). The main genes are TSLP, calpain 14 (CAPN14), CCL26, EMSY, LRRC32, STAT6, and ANKRD27 Table 7. Additional studies founded mutations within the filaggrin gene and the promoter region of TGFB1 (55, 56). TSLP is released by activated epithelial cells and plays a fundamental role in promoting T2 differentiation (57). Levels of TLSP are increased in patients with atopic diseases, including EoE (58). CAPN14 is a cysteine protease and plays a fundamental role in the integrity of the esophageal epithelial barrier. Furthermore, its expression is only limited to the esophageal mucosa (59). However, CAPN14 expression was almost 4-fold increased in EoE patients compared to controls. Higher levels of CAPN14 expression are associated with the downregulation of DSG-1, filaggrin, and zonulin, which are pivotal proteins of the epithelial barrier (59) . CCL26 gene, which encodes for EOT3, is the most highly overexpressed esophageal transcript in patients with EoE and is critical in disease pathogenesis (60) . STAT6 is essential for T2 development and is a signaling intermediate for IL-4 and IL-13 post-IL-4 receptor alpha (IL-4Ra) engagement (53). LRRC32 is a TGF-beta binding protein, and EMSY is involved in transcriptional regulation (53). In this context, the Cincinnati Children’s Hospital researchers developed a specific diagnostic panel comprising a 96-gene quantitative PCR array to identify patients with EoE, monitor the disease and response to therapy, and improve the diagnosis and treatment (61).
Conclusion
EoE is an emerging disease affecting patients at any age and is currently considered one of the upper GI tract disorders with a relevant burden on patients and the healthcare systems (6). To date, the GI endos-copy is the gold standard for the diagnosis and follow-up of patients with EoE. Therefore, there is a critical need for non-invasive biomarkers to replace such invasive monitoring. Although this review showed promising non-invasive biomarkers, none of these has been incorporated into guideline recommendations. Despite several signs of progress in understanding EoE pathogenesis, we have more to learn as we strive to improve diagnostic modalities, discover more effective and patient-targeted therapeutic strategies, and develop more accurate disease monitoring systems. We are hopeful that the growing number of genetic, molecular expression, and immunologic analyses, in conjunction with increased differentiation of clinical phenotypes and biomarker supported endotypes, will help us explain differing therapeutic responses, predict clinical response, guide individual therapies, and improve patient outcomes. The future of EoE is exciting from both a diagnostic and therapeutic standpoint. Therefore, further research is required to confirm phe-notypes and histological or serological biomarkers to provide a novel endotype classification based on different cytokine or genetic signatures.
References
- Licari A, Votto M, D’Auria E, et al. Eosinophilic gastrointestinal diseases in children: a practical review. Curr Pediatr Rev. 2020;16:106–114. doi: 10.2174/1573396315666191022154432. [DOI] [PubMed] [Google Scholar]
- 2..Licari A, Votto M, Scudeller L. et al. Epidemiology of nonesophageal eosinophilic gastrointestinal diseases in symptomatic patients: a systematic review and meta-analy- sis. J Allergy Clin Immunol Pract. 2020;8:1994–2003. doi: 10.1016/j.jaip.2020.01.060. [DOI] [PubMed] [Google Scholar]
- Dellon ES, Liacouras CA, Molina-Infante J. Updated international consensus diagnostic criteria for eosinophilic esophagitis: proceedings of the AGREE conference. Gastroenterology. 2018;155:1022–1033. doi: 10.1053/j.gastro.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuta GT, Katzka DA. Eosinophilic esophagitis. N Engl J Med. 2015;373:1640–8. doi: 10.1056/NEJMra1502863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellon ES, Hirano I. Epidemiology and natural history of eosinophilic esophagitis. Gastroenterology. 2018;154:319–332. doi: 10.1053/j.gastro.2017.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Votto M, Castagnoli R, De Filippo M, et al. Behavioral issues and quality of life in children with eosinophilic esophagitis. Minerva Pediatr. 2020;72:424–432. doi: 10.23736/S0026-4946.20.05913-7. [DOI] [PubMed] [Google Scholar]
- FDA-NIH Biomarker Working Group . Silver Spring (MD): Food and Drug Administration (US) Bethesda (MD): National Institutes of Health (US) 2016 [Google Scholar]
- Califf RM. Biomarker definitions and their applications. Exp Biol Med (Maywood). 2018;243:213–221. doi: 10.1177/1535370217750088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Sanchez J, Gomez-Torrijos E, De-la-Santa- Belda E. et al. Effectiveness of serological markers of eosinophil activity in monitoring eosinophilic esophagitis. Rev Esp Enferm Dig. 2013;105:462–7. doi: 10.4321/s1130-01082013000800004. [DOI] [PubMed] [Google Scholar]
- Wechsler JB, Ackerman SJ, Chehade M, et al. Non-invasive biomarkers identify eosinophilic esophagitis: a prospective longitudinal study in children. Allergy. 2021 doi: 10.1111/all.14874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min SB, Nylund CM, Baker TP, et al. Longitudinal evaluation of noninvasive biomarkers for eosinophilic esophagitis. J Clin Gastroenterol. 2017;51:127–135. doi: 10.1097/MCG.0000000000000621. [DOI] [PubMed] [Google Scholar]
- Nguyen T, Gernez Y, Fuentebella J, et al. Immunophenotyping of peripheral eosinophils demonstrates activation in eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2011;53:40–47. doi: 10.1097/MPG.0b013e318212647a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris DW, Stucke EM, Martin LJ, et al. Eosinophil progenitor levels are increased in patients with active pediatric eosinophilic esophagitis. J Allergy Clin Immunol. 2016;138:915–918. doi: 10.1016/j.jaci.2016.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson MW, McKernan EM, Fichtinger PS, et al. IIb- Integrin (CD41) associated with blood eosinophils is a potential biomarker for disease activity in eosinophilic esophagitis. J Allergy Clin Immunol. 2020;145:1699–1701. doi: 10.1016/j.jaci.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz JT, Morris DW, Collins MH, et al. Eosinophil progenitor levels correlate with tissue pathology in pediatric eosinophilic esophagitis. J Allergy Clin Immunol. 2019;143:1221–1224. doi: 10.1016/j.jaci.2018.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson A, Magier A, Schwartz JT, et al. Monitoring eosinophilic esophagitis disease activity with blood eosinophil progenitor levels. J Pediatr Gastroenterol Nutr. 2020;70:482–488. doi: 10.1097/MPG.0000000000002583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbarao G, Rosenman MB, Ohnuki L, et al. Exploring potential non-invasive biomarkers in eosinophilic esophagitis in children. J Pediatr Gastroenterol Nutr. 2011;53:651–658. doi: 10.1097/MPG.0b013e318228cee6. [DOI] [PubMed] [Google Scholar]
- Schlag C, Pfefferkorn S, Brockow K, et al. Serum eosinophil cationic protein is superior to mast cell tryptase as a marker for response to topical corticosteroid therapy in eosinophilic esophagitis. J Clin Gastroenterol. 2014;48:600–606. doi: 10.1097/01.mcg.0000436439.67768.8d. [DOI] [PubMed] [Google Scholar]
- Domenech Witek J, Jover Cerda V, Gil Guillen V, et al. Assessing eosinophilic cationic protein as a biomarker for monitoring patients with eosinophilic esophagitis treated with specific exclusion diets. World Allergy Organ J. 2017;10:12. doi: 10.1186/s40413-017-0143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cengiz C. Serum eosinophilic cationic protein is correlated with food impaction and endoscopic severity in eosinophilic esophagitis. Turk J Gastroenterol. 2019;30:345–349. doi: 10.5152/tjg.2019.18529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright BL, Ochkur SI, Olson NS. et al. Normalized serum eosinophil peroxidase levels are inversely correlated with esophageal eosinophilia in eosinophilic esophagitis. Dis Esophagus. 2018;31:dox139. doi: 10.1093/dote/dox139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen T, Stucke EM, Grotjan TM, et al. Molecular diagnosis of eosinophilic esophagitis by gene expression profiling. Gastroenterology. 2013;145:1289–1299. doi: 10.1053/j.gastro.2013.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu S, Herzlinger M, Cao W, et al. Utility of 15(S)-HETE as a serological marker for eosinophilic esophagitis. Sci Rep. 2018;8:14498. doi: 10.1038/s41598-018-32944-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellon ES, Rusin S, Gebhart JH, et al. Utility of a non- invasive serum biomarker panel for diagnosis and monitoring of eosinophilic esophagitis: a prospective study. Am J Gastroenterol. 2015;110:821–7. doi: 10.1038/ajg.2015.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellon ES, Higgins LL, Beitia R, et al. Prospective assessment of serum periostin as a biomarker for diagnosis and monitoring of eosinophilic oesophagitis. Aliment Pharmacol Ther. 2016;44:189–97. doi: 10.1111/apt.13672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capucilli P, Cianferoni A, Grundmeier RW, et al. Comparison of comorbid diagnoses in children with and without eosinophilic esophagitis in a large population. Ann Allergy Asthma Immunol. 2018;121:711–716. doi: 10.1016/j.anai.2018.08.022. [DOI] [PubMed] [Google Scholar]
- Dellon ES, Lin L, Beitia R, et al. Serum autoantibodies against epithelial cell adhesion molecules as disease biomarkers of eosinophilic esophagitis. Clin Exp Allergy. 2018;48:343–346. doi: 10.1111/cea.13070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins MH. Histopathologic features of eosinophilic esophagitis. Gastrointest Endosc Clin N Am. 2008;18:59–71. doi: 10.1016/j.giec.2007.09.014. [DOI] [PubMed] [Google Scholar]
- Wright BL, Doyle AD, Shim KP, et al. Image analysis of eosinophil peroxidase immunohistochemistry for diagnosis of eosinophilic esophagitis. Dig Dis Sci. 2021;66:775–783. doi: 10.1007/s10620-020-06230-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffari H, Leiferman KM, Clayton F, et al. Measurement of inflammation in eosinophilic esophagitis using an eosinophil peroxidase assay. Am J Gastroenterol. 2016;111:933–939. doi: 10.1038/ajg.2016.184. [DOI] [PubMed] [Google Scholar]
- Schroeder S, Ochkur SI, Shim KP, et al. Throat-derived eosinophil peroxidase is not a reliable biomarker of pediatric eosinophilic esophagitis. J Allergy Clin Immunol Pract. 2017;5:1804–1805. doi: 10.1016/j.jaip.2017.07.043. [DOI] [PubMed] [Google Scholar]
- Peterson KA, Gleich GJ, Limaye NS. Eosinophil granule major basic protein 1 deposition in eosinophilic esophagitis correlates with symptoms independent of eosinophil counts. Dis Esophagus. 2019;32:doz055. doi: 10.1093/dote/doz055. [DOI] [PubMed] [Google Scholar]
- Kim GH, Park YS, Jung KW. An increasing trend of eosinophilic esophagitis in Korea and the clinical implication of the biomarkers to determine disease activity and treatment response in eosinophilic esophagitis. J Neurogas- troenterol Motil. 2019;25:525–533. doi: 10.5056/jnm19066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellon ES, Woosley JT, McGee SJ, et al. Utility of major basic protein, eotaxin-3, and mast cell tryptase staining for prediction of response to topical steroid treatment in eosinophilic esophagitis: analysis of a randomized, double-blind, double dummy clinical trial. Dis Esophagus. 2020;33:doaa003. doi: 10.1093/dote/doaa003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellon ES, Speck O, Woodward K, et al. Markers of eosinophilic inflammation for diagnosis of eosinophilic esophagitis and proton pump inhibitor-responsive esophageal eosinophilia: a prospective study. Clin Gastroenterol Hepatol. 2014;12:2015–2022. doi: 10.1016/j.cgh.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellon ES, Chen X, Miller CR, et al. Diagnostic utility of major basic protein, eotaxin-3, and leukotriene enzyme staining in eosinophilic esophagitis. Am J Gastroenterol. 2012;107:1503–1511. doi: 10.1038/ajg.2012.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smadi Y, Deb C, Bornstein J, et al. Blind esophageal brushing offers a safe and accurate method to monitor inflammation in children and young adults with eosinophilic esophagitis. Dis Esophagus. 2018:31. doi: 10.1093/dote/doy056. [DOI] [PubMed] [Google Scholar]
- Matoso A, Mukkada VA, Lu S, et al. Expression microarray analysis identifies novel epithelial-derived protein markers in eosinophilic esophagitis. Mod Pathol. 2013;26:665–676. doi: 10.1038/modpathol.2013.41. [DOI] [PubMed] [Google Scholar]
- Hui Y, Chen S, Lombardo KA, et al. ALOX15 immunohistochemistry aids in the diagnosis of eosinophilic esophagitis on paucieosinophilic biopsies in children. Pediatr Dev Pathol. 2017;20:375–380. doi: 10.1177/1093526617693106. [DOI] [PubMed] [Google Scholar]
- Clayton F, Fang JC, Gleich GJ, et al. Eosinophilic esophagitis in adults is associated with IgG4 and not mediated by IgE. Gastroenterology. 2014;147:602–609. doi: 10.1053/j.gastro.2014.05.036. [DOI] [PubMed] [Google Scholar]
- Zukerberg L, Mahadevan K, Selig M, et al. Oesophageal intrasquamous IgG4 deposits: an adjunctive marker to distinguish eosinophilic oesophagitis from reflux oesophagitis. Histopathology. 2016;68:968–976. doi: 10.1111/his.12892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg CE, Mingler MK, Caldwell JM, et al. Esophageal IgG4 levels correlate with histopathologic and tran- scriptomic features in eosinophilic esophagitis. Allergy. 2018;73:1892–1901. doi: 10.1111/all.13486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu TX, Sherrill JD, Wen T, et al. MicroRNA signature in patients with eosinophilic esophagitis, reversibility with glucocorticoids, and assessment as disease biomarkers. J Allergy Clin Immunol. 2019;129:1064–1075. doi: 10.1016/j.jaci.2012.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhardwaj N, Sena M, Ghaffari G, Ishmael F. MiR-4668 as a novel potential biomarker for eosinophilic esophagitis. Allergy Rhinol (Providence) 2020;11:2152656720953378. doi: 10.1177/2152656720953378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strisciuglio C, Payne F, Nayak K, et al. Disease-associated DNA methylation signatures in esophageal biopsies of children diagnosed with eosinophilic esophagitis. Clin Epigenetics. 2021;13:81. doi: 10.1186/s13148-021-01072-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen ET, Langefeld CD, Zimmerman KD, et al. Epigenetic methylation in eosinophilic esophagitis: molecular ageing and novel biomarkers for treatment response. Clin Exp Allergy. 2020;50:1372–1380. doi: 10.1111/cea.13748. [DOI] [PubMed] [Google Scholar]
- Votto M, De Filippo M, Licari A, Marseglia A, De Amici M, Marseglia GL. Biological therapies in children and adolescents with severe uncontrolled asthma: a practical review. Biologics. 2021;15:133–142. doi: 10.2147/BTT.S252574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung J, Nguyen-Traxler A, Lee EM, et al. Assessment of fractionated exhaled nitric oxide as a biomarker for the treatment of eosinophilic esophagitis. Allergy Asthma Proc. 2012;33:519–524. doi: 10.2500/aap.2012.33.3606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanz MJ, Guerrero RA, Gonzalez-Vallina R. Measurement of exhaled nitric oxide in the evaluation for eosinophilic esophagitis in children. Ann Allergy Asthma Immunol. 2012;109:81–82. doi: 10.1016/j.anai.2012.05.009. [DOI] [PubMed] [Google Scholar]
- Moye LM, Liu Y, Coarfa C, et al. Plasma urea cycle metabolites may be useful biomarkers in children with eosinophilic esophagitis. Front Pediatr. 2019;6:423. doi: 10.3389/fped.2018.00423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunnion KM, Willis LK, Minto HB, et al. Eosinophil quantitated urine kinetic: a novel assay for assessment of eosinophilic esophagitis. Ann Allergy Asthma Immunol. 2016;116:435–439. doi: 10.1016/j.anai.2016.02.011. [DOI] [PubMed] [Google Scholar]
- Votto M, Marseglia GL, De Filippo M, et al. Early life risk factors in pediatric EoE: could we prevent this modern disease? Front Pediatr. 2020;8:263. doi: 10.3389/fped.2020.00263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea KM, Aceves SS, Dellon ES, et al. Pathophysiology of eosinophilic esophagitis. Gastroenterology. 2018;154:333–345. doi: 10.1053/j.gastro.2017.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffner MA, Cianferoni A. Phenotypes and endotypes in eosinophilic esophagitis. Ann Allergy Asthma Immunol. 2020;124:233–239. doi: 10.1016/j.anai.2019.12.011. [DOI] [PubMed] [Google Scholar]
- Blanchard C, Stucke EM, Burwinkel K, et al. Coordinate interaction between IL-13 and epithelial differentiation cluster genes in eosinophilic esophagitis. J Immunol. 2010;184:4033–4041. doi: 10.4049/jimmunol.0903069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aceves SS, Newbury RO, Chen D, et al. Resolution of remodeling in eosinophilic esophagitis correlates with epithelial response to topical corticosteroids. Allergy. 2010;65:109–116. doi: 10.1111/j.1398-9995.2009.02142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitajima M, Lee HC, Nakayama T, et al. TSLP enhances the function of helper type 2 cells. Eur J Immunol. 2011;41:1862–1871. doi: 10.1002/eji.201041195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui CC, Rusta-Sallehy S, Asher I, et al. The effects of thymic stromal lymphopoietin and IL-3 on human eosinophilbasophil lineage commitment: relevance to atopic sensitization. Immun Inflamm Dis. 2014;2:44–55. doi: 10.1002/iid3.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleiman PM, Wang ML, Cianferoni A, et al. GWAS identifies four novel eosinophilic esophagitis loci. Nat Commun. 2014;5:5593. doi: 10.1038/ncomms6593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard C, Wang N, Stringer KF, et al. Eotaxin-3 and a uniquely conserved gene-expression profile in eosinophilic esophagitis. J Clin Invest. 2006;116:536–547. doi: 10.1172/JCI26679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen T, Rothenberg ME. Clinical applications of the eosinophilic esophagitis diagnostic panel. Front Med (Lausanne) 2017;4:108. doi: 10.3389/fmed.2017.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]


