Abstract
Coronavirus disease 2019 (COVID-19) is spreading rapidly around the world. Several articles have so far reported on radiological findings of COVID-19 pneumonia. Herein, we present three cases of COVID-19 pneumonia in South Korea, and provide clinical information as well as chest radiograph and chest CT findings.
Keywords: COVID-19; Coronavirus; Pneumonia; Computed Tomography, X-Ray; Radiography, Thoracic; Republic of Korea
Abstract
코로나바이러스감염증-19는 전 세계적에서 급속도로 확산되고 있다. 몇몇 논문에서 코로나바이러스감염증-19의 영상의학적 소견들이 보고되었다. 우리는 한국에서 코로나바이러스감염증-19로 확진된 세 명의 환자에 대한 임상적 소견과 흉부 일반촬영 및 흉부 전산화단층촬영에서 나타난 영상의학적 소견에 대하여 보고하고자 한다.
INTRODUCTION
The coronavirus disease 2019 (COVID-19), which originated in Wuhan, China, is rapidly spreading around the world. It shows various clinical manifestations, including asymptomatic progression, common cold, pneumonia, acute respiratory distress syndrome, and even death (1). In South Korea, the first case of COVID-19 was reported on January 23, and thereafter the number of infected people has been increasing very rapidly, reaching approximately 10000 people by March. Several recent publications reported that COVID-19 pneumonia appeared mainly in the form of multiple patchy areas of mixed ground glass opacity (GGO) and consolidation on chest CT (2,3,4,5,6). In addition, linear opacities, crazy-paving patterns, and a reversed halo sign have been reported (2,3,7). Here, we report on the clinical information and radiological findings of three patients with COVID-19 pneumonia in South Korea.
CASE REPORTS
CASE 1
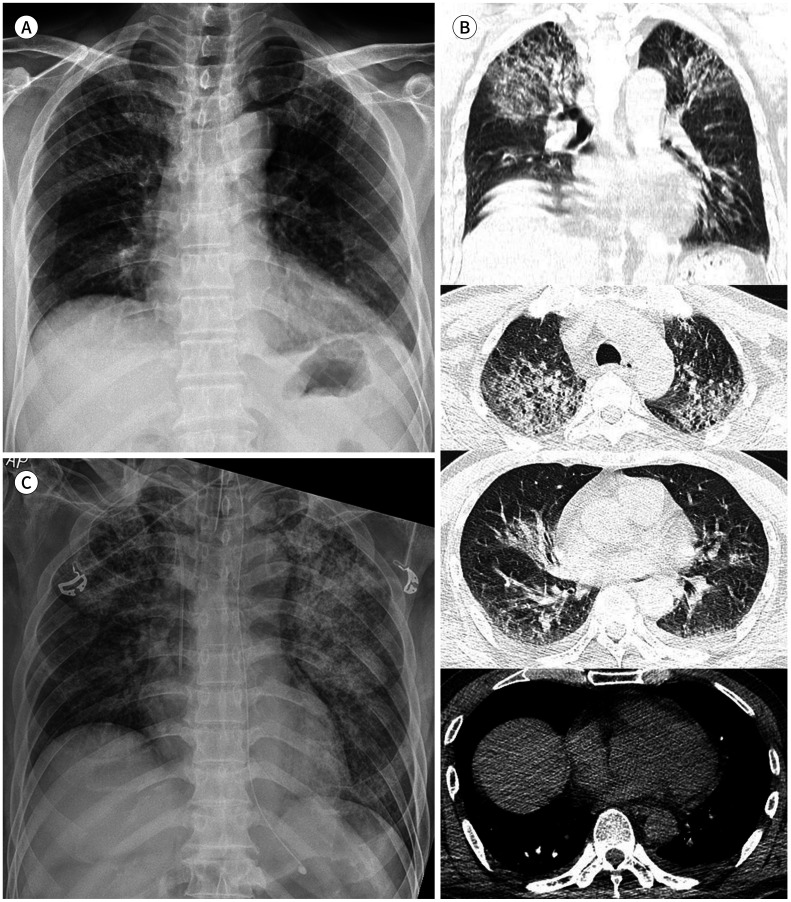
A 57-year-old man had been admitted to a local psychiatric hospital due to alcohol abuse and memory loss. He also had a history of diabetes and dyslipidemia. He complained of fever and dyspnea during hospitalization, and was treated for 5 days for bacterial pneumonia. When he was diagnosed with COVID-19 via real-time reverse-transcriptase-polymerase chain reaction (rRT-PCR), the patient was referred to our institution for further treatment. The chest radiograph taken at the local hospital just before the transfer (6 days after symptom onset) showed subtle GGO in both upper lung zones and right middle lung zone (Fig. 1A). On the same day, chest CT was performed for further evaluation. Large areas of mixed GGO and consolidation involving both upper lungs with underlying pulmonary emphysema were observed on the chest CT images (Fig. 1B). Moreover, a small amount of bilateral pleural and pericardial effusions was noted.
Fig. 1. A 57-year-old man with COVID-19 pneumonia.
A. Chest radiograph taken just before the transfer to our institution shows subtle GGOs in both upper lung zones and right middle lung zone.
B. Axial and coronal non-enhanced chest CT images, taken immediately after A, show large areas of mixed GGO and consolidation involving both upper lungs with underlying pulmonary emphysema. A small amount of bilateral pleural effusions and pericardial effusion is also visible.
C. Follow-up chest radiograph taken after the patient's arrival at our institution (12 hours after A and B) shows a marked increase in the extent and density of GGOs, progressed into diffuse consolidation in both lungs. Endotracheal intubation, central line insertion, and L-tube insertion were performed for further treatment.
GGO = ground glass opacity
When the patient arrived at our hospital, his mental status was drowsy. His vital signs were as follows: blood pressure of 124/99 mm Hg, pulse rate of 135 beats/min, respiratory rate of 33 breaths/min, body temperature of 37.5℃ and O2 saturation level of 80%. Laboratory tests showed a normal leukocyte level of 9190/µL, an increased neutrophil ratio of 83.1%, a decreased lymphocyte ratio of 9.1%, an increased erythrocyte sedimentation rate (ESR) of 16 mm/hr, and an elevated C-reactive protein (CRP) level of 36.2 mg/L. Even after 15 L O2 mask therapy, the patient's O2 saturation level was still 88%, and his blood pressure dropped to 88/73 mm Hg; endotracheal intubation and central line insertion were therefore performed for further treatment. An O2 saturation level of > 95% was measured after intubation, but bloody sputum had been continuously suctioned from the endotracheal tube. A combination therapy with lopinavir and ritonavir was administered for the treatment of COVID-19.
The chest radiograph taken on hospital day 1 at our institution showed a marked increase in the extent and density of GGOs, progressed into diffuse consolidation in both lungs (Fig. 1C). Also, laboratory tests on hospital day 2 showed an elevated leukocyte level of 16250/µL and a CRP level of 48.8 mg/L. After three days of supportive treatment, the patient expired due to septic shock.
CASE 2
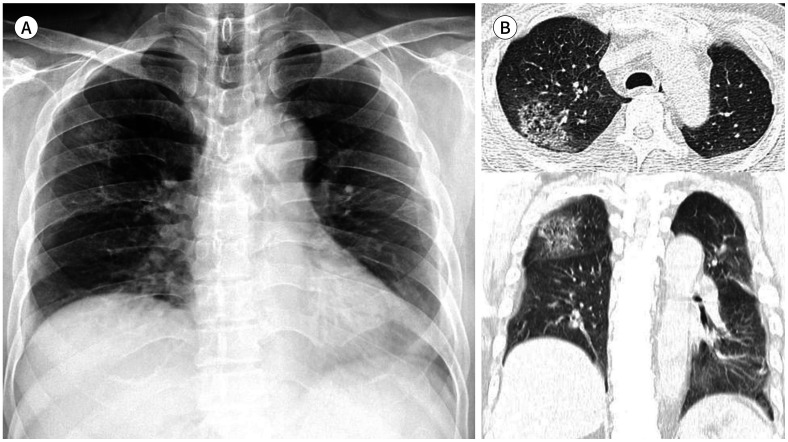
A 59-year-old man had been admitted to the same local hospital as case 1, for schizophrenia. He also had a history of hypertension. He complained of fever and, as he had reported having been in close contact with the patient described in case 1, he underwent a COVID-19 rRT-PCR test that yielded a positive result. The chest radiograph showed no remarkable findings at the time of diagnosis. After 2 days, however, a patchy area of GGO in the right upper lung zone was newly identified on the chest radiograph (Fig. 2A). On the chest CT images obtained on the same day, this lesion showed a reversed halo sign with a central area of GGO surrounded by denser consolidation in the right upper lobe (Fig. 2B). Also, underlying pulmonary emphysema and mild left pleural thickening as post-infectious sequelae were noted. The patient was referred to our institution for further treatment.
Fig. 2. A 59-year-old man with COVID-19 pneumonia.
A. Chest radiograph shows a patchy area of GGO in the right upper lung zone.
B. Axial and coronal non-enhanced chest CT images show a central area of GGO surrounded by denser consolidation in the right upper lobe, representing a reversed halo sign. Pulmonary emphysema in both lungs is also visible.
GGO = ground glass opacity
When the patient arrived at our institution, he complained of dyspnea. His vital signs were within the normal range, and his O2 saturation level was 100%. Laboratory tests showed a normal leukocyte level of 6890/µL, an increased neutrophil ratio of 70.8%, a decreased lymphocyte ratio of 17.2%, an increased ESR of 18 mm/hr, and an elevated CRP level of 15.6 mg/L. The patient underwent a combination therapy with lopinavir and ritonavir.
The chest radiograph on hospital day 3 showed that the patchy GGO in the right upper lung zone disappeared. A follow-up COVID-19 rRT-PCR test on hospital day 7 yielded a negative result. The COVID-19 rRT-PCR test conducted on hospital day 8, however, showed a positive result, without any symptoms of the patient.
The patient did not have any complaints since then. Daily chest radiographs showed no significant abnormalities, and follow-up laboratory tests showed a continuous decrease in CRP levels. The COVID-19 rRT-PCR test conducted on hospital day 22 and a series of tests after that showed consistently negative results. On hospital day 27, the patient was discharged.
CASE 3
A 61-year-old man visited our institution with myalgia, chilling, cough, and sputum that started 2 days ago. He had hypertension and was undergoing hemodialysis for polycystic kidney disease. The patient had also been in close contact with a patient confirmed with COVID-19. After being diagnosed with COVID-19 via rRT-PCR, he was admitted for treatment in isolation. At admission, his vital signs were as follows: blood pressure of 178/99 mm Hg, pulse rate of 61 beats/min, respiratory rate of 14 breaths/min, body temperature of 36.0℃, and O2 saturation level of 99%. Laboratory tests showed a decreased leukocyte level of 3460/µL, a normal neutrophil ratio of 55.0%, a normal lymphocyte ratio of 29.9%, an increased serum creatinine level of 10.54 mg/dL, an increased ESR of 18 mm/hr, and an elevated CRP level of 4.0 mg/L. An initial chest radiograph showed cardiomegaly, but no remarkable findings in both lungs (Fig. 3A). The patient underwent hemodialysis and combination therapy with lopinavir and ritonavir.
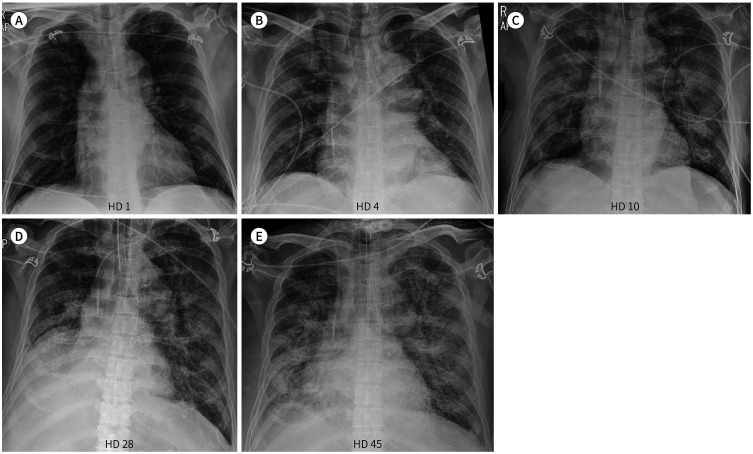
Fig. 3. A 61-year-old man with COVID-19 pneumonia.
A. Initial chest radiograph shows no significant abnormalities except cardiomegaly.
B. Chest radiograph on HD 4 shows new subtle patchy areas of GGO in the right upper and lower lung zones. Central line insertion was performed for further treatment.
C. Chest radiograph on HD 10 shows diffuse consolidation in both lungs, suggesting progression of pneumonia. Endotracheal intubation and L-tube insertion were performed for further treatment.
D. Chest radiograph on HD 28 shows no significant interval changes of diffuse consolidation in both lungs. Combined atelectasis of right middle and lower lobes is newly noted.
E. Chest radiograph on HD 45 shows an increase in extent of diffuse consolidation in both lungs, while combined atelectasis of right middle and lower lobes improves.
GGO = ground glass opacity, HD = hospital day
On hospital day 3, high-flow O2 therapy was initiated because the patient showed dyspnea and had a low O2 saturation level of 92–93%, and symptoms subsequently regressed. The chest radiograph on hospital day 4 showed new subtle patchy areas of GGO in the right upper and lower lung zones (Fig. 3B). On hospital day 6, the patient's CRP level increased to 117.2 mg/L.
On hospital day 10, despite the application of an O2 mask, the patient again showed dyspnea and a low O2 saturation level of 79%, requiring endotracheal intubation and mechanical ventilation. O2 saturation levels then increased to > 95%. Laboratory tests still showed an elevated CRP level of 112 mg/L. The chest radiograph after endotracheal intubation revealed diffuse consolidation in both lungs, suggesting progression of pneumonia (Fig. 3C).
On hospital day 13, continuous intravenous infusion of vasopressor (norepinephrine) was started, because of the patient's low blood pressure of 62/56 mm Hg. Laboratory tests showed an increased leukocyte level of 23220/µL, an increased neutrophil ratio of 93.6%, a decreased lymphocyte ratio of 2.4%, and an elevated CRP level of 166.7 mg/L. The chest radiograph showed diffuse consolidation in both lungs without significant interval changes.
After that, the patient was treated conservatively with mechanical ventilation, vasopressor infusion, and hemodialysis. The chest radiograph on hospital day 28 showed no significant interval changes in diffuse consolidation in both lungs, but combined atelectasis of right middle and lower lobes was newly noted (Fig. 3D). Laboratory tests showed an increased leukocyte level of 11350/µL, an increased neutrophil ratio of 91.2%, a decreased lymphocyte ratio of 4.3%, and an elevated CRP level of 135.3 mg/L. COVID-19 rRT-PCR tests were conducted every other day during the patient's hospitalization, and yielded continuously positive results until hospital day 29. From hospital day 31 to hospital day 39, the COVID-19 rRT-PCR tests showed indeterminate results, followed by a negative result on hospital day 41. However, on hospital day 45, laboratory tests still showed an increased leukocyte level of 15510/µL, an increased neutrophil ratio of 90.6%, a decreased lymphocyte ratio of 4.8%, and an elevated CRP level of 155.5 mg/L. The chest radiograph revealed that while combined atelectasis of right middle and lower lobes improved, the extent of diffuse consolidation in both lungs increased (Fig. 3E). The supportive treatment for the patient was maintained until submission of this manuscript (45 days of hospitalization).
DISCUSSION
The 2019-nCoV virus is a member of the coronavirus family, and has been classified as belonging to the same family as the former Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) viruses (1). Early patients were mainly found in Wuhan, China, but the disease is now affecting people in a number of countries all around the world, including South Korea, Italy, and Iran. There were 1511104 confirmed cases of COVID-19 as of April 9, and 88338 patients have already died from the virus. South Korea has reported 10423 cases and 204 deaths so far.
Several articles about chest imaging findings of COVID-19 pneumonia have recently been published. Chung et al. (3) reported that 18 out of 21 patients showed GGO, consolidation, or both on chest CT. Yoon et al. (2) demonstrated that mixed GGO and consolidative lesions (20 of 40 lesions) were mostly seen in patients with COVID-19. These findings do well correlate with the three cases we report here. All of our cases had radiologic findings of GGO and consolidation.
In our second case, a reversed halo sign with a central area of GGO surrounded by denser consolidation in the right upper lobe was observed. Several earlier reports also demonstrated a reversed halo sign on chest CT in patients with COVID-19 pneumonia. Yoon et al. (2) reported that one out of nine patients showed the reversed halo sign. Moreover, Li et al. (7) observed the reversed halo sign in two out of 51 patients. The reversed halo sign is known as a common finding in cryptogenic organizing pneumonia and other disease entities such as Wegener granulomatosis, sarcoidosis, viral infections, and mucormycosis (8). Although this sign is not specific, it may be a helpful indicator of the possibility of COVID-19 pneumonia in patients who have been in close contact with an individual confirmed with COVID-19 or in those with fever and/or respiratory symptoms in a COVID-19 epidemic area.
Several reports have evaluated the presence of pleural effusions. According to Yoon et al. (2) and Chung et al. (3), none of their patients showed pleural effusions. Shi et al. (6) reported pleural effusions in four out of 81 patients. In one of those four patients, the chest CT images revealed mild pneumonia on day 5 after symptom onset, and follow-up CT scans 10 days and 15 days later showed rapid progression of pneumonia with bilateral pleural effusions. Our first case, which represents a severe form of COVID-19 pneumonia, also showed a small amount of bilateral pleural effusions on initial chest CT. Although pleural effusions in COVID-19 pneumonia have been reported to be rare, we propose that pleural effusions could occur as pneumonia progresses.
Several earlier publications reported on the progression of COVID-19 pneumonia. Shi et al. (6) demonstrated that the chest CT findings of early COVID-19 pneumonia include unilateral or multifocal GGOs, and that these findings rapidly evolve into bilateral and diffuse GGO or consolidation, between 1 and 3 weeks after the onset of symptoms. Xiong et al. (9) also reported that 35 of 42 patients showed progressive pneumonia on follow-up chest CT images, at an average of 11.6 days after the onset of symptoms. In our second case, which represents a mild form of COVID-19 pneumonia, imaging findings improved within 1 week, and laboratory findings slowly recovered over the course of 1 month. Furthermore, the COVID-19 rRT-PCR test finally showed a negative result on hospital day 22. In contrast, our first and third cases represent severe forms of COVID-19 pneumonia. The first patient quickly deteriorated within 1 week after admission. The vital signs, laboratory tests, and imaging findings of the third patient all worsened in 1 or 2 weeks after admission, and he has not recovered yet. COVID-19 pneumonia show a variety of clinical courses. In case of disease progression, 1 to 2 weeks after the onset of symptoms may be critical time window for close monitoring.
The outbreak of COVID-19 is now a challenging global health emergency. We report clinical information and radiological features of three patients with COVID-19 pneumonia. Further investigations will be required to better understand the role of radiologists in the diagnosis and treatment of COVID-19.
Footnotes
- Conceptualization, K.Y.N., M.J.W.
- data curation, L.H.J., W.J.Y.
- investigation, L.H.J.
- methodology, K.Y.N., M.J.W., W.J.Y.
- project administration, K.Y.N., M.J.W., W.J.Y.
- resources, L.H.J., K.Y.N.
- software, L.H.J., M.J.W.
- supervision, K.Y.N.
- visualization, K.Y.N., M.J.W.
- writing—original draft, L.H.J., K.Y.N., M.J.W.
- writing—review & editing, K.Y.N., M.J.W., W.J.Y.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei J, Xu H, Xiong J, Shen Q, Fan B, Ye C, et al. 2019 novel coronavirus (COVID-19) pneumonia: serial computed tomography findings. Korean J Radiol. 2020;21:501–504. doi: 10.3348/kjr.2020.0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin X, Gong Z, Xiao Z, Xiong J, Fan B, Liu J. Novel coronavirus pneumonia outbreak in 2019: computed tomographic findings in two cases. Korean J Radiol. 2020;21:365–368. doi: 10.3348/kjr.2020.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020 doi: 10.2214/AJR.20.22954. [In press] [DOI] [PubMed] [Google Scholar]
- 8.Godoy MC, Viswanathan C, Marchiori E, Truong MT, Benveniste MF, Rossi S, et al. The reversed halo sign: update and differential diagnosis. Br J Radiol. 2012;85:1226–1235. doi: 10.1259/bjr/54532316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiong Y, Sun D, Liu Y, Fan Y, Zhao L, Li X, et al. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest Radiol. 2020 doi: 10.1097/RLI.0000000000000674. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]