Abstract
Purpose
To evaluate the optimal measurement location, cut-off value, and diagnostic performance of S-Shearwave in differential diagnosis of breast masses seen on ultrasonography (US).
Materials and Methods
During the study period, 225 breast masses in 197 women were included. S-Shearwave measurements were made by applying a square region-of-interest automatically generated by the US machine. Shearwave elasticity was measured three times at four different locations of the mass, and the highest shearwave elasticity was used for calculating the optimal cut-off value. Diagnostic performance was evaluated by using the area under the receiving operator characteristic curve (AUC).
Results
Of the 225 breast masses, 156 (69.3%) were benign and 69 (30.7%) were malignant. Mean S-Shearwave values were significantly higher for malignant masses (108.0 ± 70.0 kPa vs. 43.4 ± 38.3 kPa; p < 0.001). No significant differences were seen among AUC values at different measurement locations. With a cut-off value of 41.9 kPa, S-Shearwave showed 85.7% sensitivity, 63.9% specificity, 70.7% accuracy, and positive and negative predictive values of 51.7% and 90.8%, respectively. The AUCs for US and S-Shearwave did not show significant differences (p = 0.179).
Conclusion
S-Shearwave shows comparable diagnostic performance to that of grayscale US that can be applied for differential diagnosis of breast masses seen on US.
Keywords: Breast, Ultrasonography, Neoplasm, Elasticity Imaging Techniques
Abstract
목적
S-Shearwave를 이용하여 유방 병변을 감별하는데 있어 최적의 cut-off 값과 종괴 내 위치를 알아보고 진단적 가치를 평가하고자 한다.
대상과 방법
연구 기간 동안 197명의 여성에서 225개의 유방 병변을 평가하였다. S-Shearwave 값은 초음파 기기에서 자동적으로 생성된 사각형의 region-of-interest로 측정하였다. 병변 내 서로 다른 네 군데에서 각각 세 번 측정하였으며 세 개의 중위 값 중 최대 값을 이용해 각각의 위치에서 최적의 cut-off 값을 계산하였다. 진단적 가치는 area under the receiving operator characteristics curve (이하 AUC)를 통해 평가하였다.
결과
총 225개의 유방 병변 중 156개(69.3%)는 양성, 69개(30.7%)는 악성이었다. 평균 S-Shearwave 값은 악성 병변이 양성 병변에 비해 유의미하게 높았다(108.0 ± 70.0 kPa vs. 43.4 ± 38.3 kPa, p < 0.001). 하지만 병변 내 위치에 따른 값의 유의미한 차이는 없었다. Cut-off 값을 41.9 kPa로 사용했을 때, 민감도 85.7%, 특이도 63.9%, 정확도 70.7%, 양성예측도 51.7% 및 음성예측도 90.8%였다. 초음파와 S-Shearwave 간의 AUC는 유의미한 차이를 보이지 않았다(p = 0.179).
결론
S-Shearwave는 유방 병변의 감별진단을 하는데 grayscale 초음파에 필적하는 진단적 가치를 가진다.
INTRODUCTION
High-resolution ultrasonography (US) is nowadays widely spread and routinely used for evaluating causes for various breast symptoms. High-resolution breast US enables detailed morphologic analysis of breast masses seen on US, in which we use to stratify cancer risk. The Breast Imaging Reporting And Data System (BI-RADS) released by the American College of Radiology (ACR) (1) contains morphologic descriptors for breast masses seen on US based on which we categorize the masses according to its estimated malignancy risk, and many studies have shown high performances in differential diagnosis and its usefulness in planning patient management (2,3,4).
In addition to morphologic features, elastography, which is an additional imaging modality that visualizes the intrinsic stiffness of a target mass has been introduced and applied to characterizing breast masses (5). Various elastographic techniques are currently utilized along with grayscale US features, ranging from strain elastography that shows the relative stiffness of a target breast mass to the surrounding breast parenchyma, to shearwave elastography (SWE) that enables measurement of quantitative elasticity values of the mass. SWE is considered as more reproducible and reliable data since SWE remotely induces mechanical vibrations by acoustic radiation force generated by the machine (6,7). Regardless to the type of elastography techniques, studies have commonly shown that applying elastography improves the diagnostic performances of breast US (8,9,10,11). A new SWE technique, ‘S-Shearwave,’ has been developed and applied to breast US imaging. Compared with other SWE, S-Shearwave provides reliability measurement index (RMI), which is a parameter computing the reliability of the measurement to support selection of measured values (12). However, there are no studies showing the optimal cut-off levels for S-Shearwave or the diagnostic performances of S-Shearwave. Also, there are no guidelines on the measurement location for accurate SWE measurements, since there are little data on how the diagnostic performances of SWE differ according to the measurement location.
Based on this, the purpose of this study is to evaluate the optimal cut-off value for S-Shearwave along with the optimal location for SWE measurement, and compare the diagnostic performances of S-Shearwave for differential diagnosis of breast masses seen on US according to various measurement locations.
MATERIALS AND METHODS
PATIENTS
This study is of a prospective design, and was approved by our Institutional Review Board (1-2017-0013). Informed consent was obtained from all patients for study inclusion.
From July to September 2017, 225 breast masses from 197 women who had undergone breast US examinations were included in this study. All breast masses met the following inclusion criteria: 1) pathologically diagnosed with US-guided percutaneous biopsy or surgical excision, 2) stable on follow up images for more than 24 months after being diagnosed as benign on US-guided core biopsy, 3) typically benign US features according to the ACR BI-RADS for US (1). Mean size of the 225 breast masses were 14.6 ± 10.3 mm (range, 5–62 mm). Mean age of the 197 women was 47.8 ± 11.0 years (range, 20–74 years).
US EXAMINATION AND BIOPSY
Grayscale US and elastography images were obtained using a 3–12 MHz linear transducer (RS80A with Prestiage, Samsung Medison, Seoul, Korea) by a radiologist with 10 years of experience (J.H.Y.) in breast imaging. After a breast mass was located, S-Shearwave was generated for elastography measurements. US images were assessed by the radiologist according to the final assessments of the ACR BI-RADS (1). BI-RADS final assessments and elastography measurements were recorded, prospectively. Biopsy was performed afterwards, if required.
S-SHEARWAVE APPLICATION AND ELASTOGRAPHY MEASUREMENT
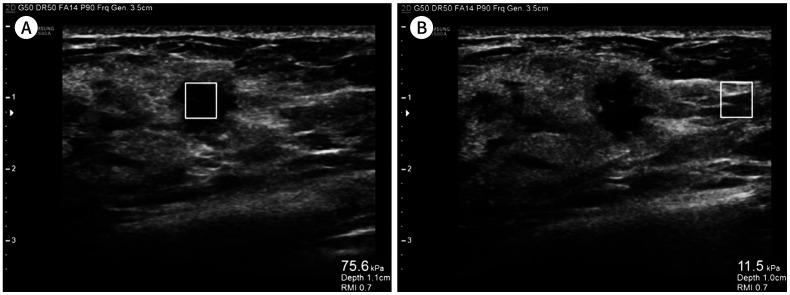
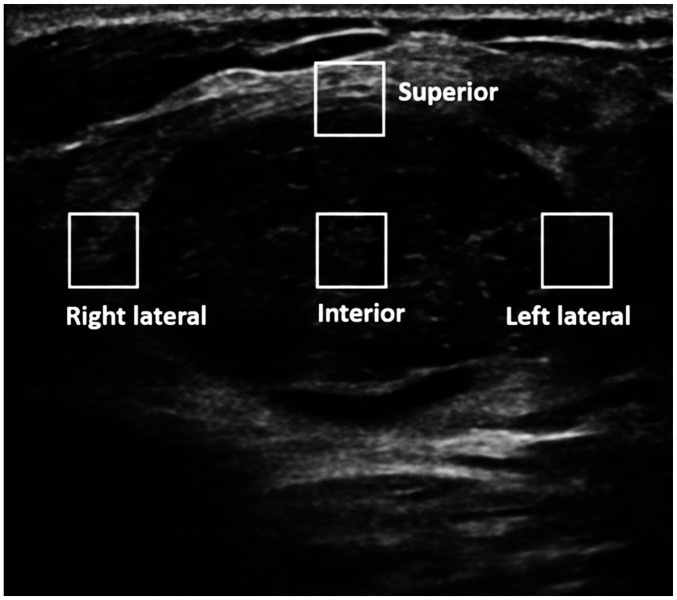
S-Shearwave was performed by applying a fixed, square region-of-interest (ROI) of 5×5 mm that is automatically generated by the US machine. By setting the ROI at a specific location, the elasticity properties were automatically generated by the US machine, visualized in kPa (Fig. 1). With the elasticity values, RMI is visualized in the elasticity image, ranging from 0–1, higher values suggestive of high quality elasticity measurements and optimal RMI values suggested as > 0.5. Shearwave elasticity was measured three times at four different locations of the mass—at the center of the mass (mass center), at the superior border of the mass (superior margin), at the right lateral border of the mass (right lateral margin), and at the left lateral border of the mass (left lateral margin) (Fig. 2). In cases when invalid elasticity measurements occurred, repeated S-Shearwave measurements were performed until a valid numeric value was obtained. Shearwave elasticity of the normal breast parenchyma adjacent to the breast mass was also measured, by placing the ROI at the breast parenchyma adjacent to, and within the similar depth to the mass.
Fig. 1. Example of application of S-Shearwave to breast ultrasonography examination.
A. A square ROI is set at the center of the breast mass for shearwave elasticity measurement.
B. An ROI is set at the normal breast parenchyma adjacent to the breast mass, with the ROI set at the same depth as that of the breast mass.
ROI = region-of-interest
Fig. 2. After generating the S-Shearwave, shearwave elasticity is measured three times at four different locations of the mass by applying square regions-of-interest – interior (mass center), superior border, right lateral border, and left lateral border of the mass.
DATA AND STATISTICAL ANALYSIS
Histopathologic results from US-guided biopsy or surgical excision were considered the reference standard. Final pathologic diagnosis of high-risk lesions such as atypical ductal hyperplasia, atypical lobular hyperplasia/lobular carcinoma in situ, intraductal papilloma, mucocele like lesion or radial scar, were based on surgical excision, which was then considered benign for statistical analysis.
Independent two sample t-test was used for comparison of continuous variables. For statistical analysis, BI-RADS final assessment categories 2 and 3 were considered as negative, and categories 4a to 5 were considered as positive. The maximum shearwave elasticity among the median value calculated from the three elasticity measurements obtained from the four locations was used to calculate the optimal cut-off value for S-Shearwave. Youden's index was used to calculate the optimal cut-off levels for differentiating between benign and malignant masses for S-Shearwave in general, and for each measurement location. For the cut-off value to be used generally regardless of the measurement location, the maximum shearwave elasticity among the median elasticity value obtained from each of the four measurement locations was used to represent each breast mass, calculated as 41.9 kPa. Diagnostic performances including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy was calculated and compared using generalized estimating equation method. Area under the receiver operating characteristics (AUC) curve was calculated and compared using the Delong's method.
Statistical analysis was performed using SAS software (version 9.2, SAS Inc., Cary, NC, USA). All tests were two sided, and p < 0.05 was considered to indicate statistical significance.
RESULTS
Of the 225 breast masses, 156 (69.3%) were benign and 69 (30.7%) were malignant. Mean size of the malignant masses was significantly larger than the benign ones, 21.1 ± 13.1 mm to 11.5 ± 6.7 mm (p < 0.001). Among the 225 breast masses, final assessment categories were as follows: 47 (20.9%) as category 2, 45 (20.0%) as category 3, 72 (32.0%) as category 4a, 4 (1.8%) as category 4b, 37 (16.4%) as category 4c, and 20 (8.9%) as category 5.
Mean S-Shearwave values are significantly higher for malignant masses to benign ones, 108.0 ± 70.0 kPa to 43.4 ± 38.3 kPa (p < 0.001). Among the 225 breast masses, 178 (79.1%) measured < 20 mm and 47 (20.9%) measured ≥ 20 mm. Mean S-Shearwave values were significantly higher in malignant masses to benign in breast masses for both size ranges, 1) < 20 mm: 83.8 ± 55.5 kPa to 42.1 ± 55.5 kPa (p = 0.006), 2) ≥ 20 mm: 139.4 ± 75.1 kPa to 53.9 ± 29.3 kPa (p < 0.001), respectively. Table 1 summarizes the mean S-Shearwave values between benign and malignant masses according to measurement location. Mean S-Shearwave values showed significantly higher elasticity in malignancy compared to benign masses in all 4 measurement locations (all p < 0.001). Mean S-Shearwave value for normal breast parenchyma was significantly lower than the values for benign or malignant breast masses at all four locations (all p < 0.001, respectively).
Table 1. Comparison of Mean S-Shearwave Values between Breast Masses.
| Benign (n = 156) | Malignancy (n = 69) | p † | |||||
|---|---|---|---|---|---|---|---|
| Mass | Parenchyma | p * | Mass | Parenchyma | p * | ||
| Mass center | 29.0 ± 30.0 | 18.3 ± 15.3 | < 0.001 | 72.0 ± 67.4 | 13.1 ± 9.2 | < 0.001 | < 0.001 |
| Superior margin | 33.9 ± 77.8 | 18.3 ± 15.3 | < 0.001 | 77.6 ± 58.1 | 13.1 ± 9.2 | < 0.001 | < 0.001 |
| Right lateral margin | 26.8 ± 26.8 | 18.3 ± 15.3 | < 0.001 | 52.0 ± 47.4 | 13.1 ± 9.2 | < 0.001 | < 0.001 |
| Left lateral margin | 27.2 ± 27.7 | 18.3 ± 15.3 | < 0.001 | 53.4 ± 41.5 | 13.1 ± 9.2 | < 0.001 | < 0.001 |
Data are displayed as mean ± standard deviation (kPa).
*Comparison of mean elasticity values between benign masses and surrounding parenchyma.
†Comparison of mean elasticity values between benign and malignant masses in the four measurement locations.
S-SHEARWAVE MEASUREMENTS ACCORDING TO LOCATION
Optimal cut-off level for each measurement location was calculated as follows: 25.8 kPa for mass center, 32.2 kPa for superior margin, 24.1 for right lateral margin, 29.5 kPa for left lateral margin, respectively. The diagnostic performances using these cut-off values at each measurement location is summarized in Table 2. Sensitivity and NPV was highest at the superior margin, 82.9% and 89.2%, respectively. Specificity, PPV, and accuracy was highest at the left lateral margin, 74.2%, 55.1%, and 72.9%, respectively. Sensitivity was significantly higher for superior margin compared to left lateral margin (p = 0.008). Specificity for the left lateral margin was significantly higher compared to the specificity at mass center (63.2%) and superior margin (63.9%, p = 0.004 and p = 0.014, respectively). No significant differences were seen among the AUC values between the any of the measurement locations.
Table 2. Diagnostic Performance of S-Shearwave According to Measurement Location.
| Mass Center | Superior Margin | Right Lateral Margin | Left Lateral Margin | Overall p | |
|---|---|---|---|---|---|
| Cut-off level* (kPa) | > 25.8 | > 32.2 | > 24.1 | > 29.5 | - |
| Sensitivity | 80.0 (70.6–89.4) | 82.9 (74.0–91.7) | 68.6 (57.7–79.5) | 70.0 (59.3–80.7) | 0.024 |
| Specificity | 63.2 (55.6–70.8) | 63.9 (56.3–71.4) | 70.3 (63.1–77.5) | 74.2 (67.3–81.1) | 0.014 |
| PPV | 49.6 (40.3–58.8) | 50.9 (41.7–60.1) | 51.1 (41.0–61.2) | 55.1 (44.7–65.4) | 0.521 |
| NPV | 87.5 (81.4–93.6) | 89.2 (83.4–95.0) | 83.2 (76.8–89.6) | 84.6 (78.5–90.6) | 0.189 |
| Accuracy | 68.4 (62.4–74.5) | 69.8 (68.8–75.8) | 69.8 (63.8–75.8) | 72.9 (67.1–78.7) | 0.586 |
| AUC | 0.716 (0.656–0.777) | 0.734 (0.675–0.792) | 0.695 (0.629–0.760) | 0.721 (0.657–0.785) | > 0.999 |
95% confidence intervals are in parentheses.
*Cut-off level is calculated by Youden's index with the maximum S-Shearwave elasticity among the median values calculated from the three elasticity measurements obtained from each location.
AUC = area under the receiver operator characteristics curve, NPV = negative predictive value, PPV = positive predictive value
DIAGNOSTIC PERFORMANCES OF US AND S-SHEARWAVE
Optimal cut-off for S-Shearwave in general was calculated as 41.9 kPa. Using this cut-off value, diagnostic performances of S-Shearwave were as follows: sensitivity 85.7%, specificity 63.9%, PPV 51.7%, NPV 90.8%, and accuracy 70.7%. Table 3 summarizes the diagnostic performances of US and S-Shearwave in the diagnosis of the 225 breast masses in this study. Sensitivity (98.6% to 85.7%, p = 0.002) and NPV (98.9% to 90.8%, p = 0.002) of US alone shows significantly higher values compared to S-Shearwave, without significant differences for specificity, PPV, or accuracy (all p > 0.05). AUC for US and S-Shearwave do not show significant differences, 0.794 to 0.748, respectively (p = 0.179).
Table 3. Diagnostic Performance of S-Shearwave and US for the 225 Breast Masses.
| S-Shearwave* | US Alone | p | |
|---|---|---|---|
| Sensitivity | 85.7 (77.5–93.9) | 98.6 (96,2–100.0) | 0.002 |
| Specificity | 63.9 (56.3–71.4) | 58.3 (51.0–66.5) | 0.332 |
| PPV | 51.7 (42.6–60.8) | 51.1 (43.8–60.7) | 0.888 |
| NPV | 90.8 (85.4–96.2) | 98.9 (96.2–100.0) | 0.002 |
| Accuracy | 70.7 (64.7–76.6) | 70.7 (65.7–77.5) | 0.821 |
| AUC | 0.748 (0.692–0.804) | 0.794 (0.755–0.832) | 0.179 |
95% confidence intervals are in parentheses.
*Cut-off level of S-Shearwave in general is used as 41.9 kPa.
AUC = area under the receiver operator characteristics curve, NPV = negative predictive value, PPV = positive predictive value, US = ultrasonograpy
DISCUSSION
S-Shearwave showed differences in diagnostic performances according to the measurement location, results of our study show that the sensitivity and NPV is highest when the ROI is set at the superior margin, and specificity, PPV, and accuracy is highest when set at the left lateral margin. The level at which SWE parameters are measured are not strictly defined. The potential for increase in artifacts caused by reflection and refraction due to the large variation of shearwave velocity between normal breast parenchyma and breast masses have been suggested for marginal measurements (13), while measurement failure was more often experienced during internal measurements in other recent studies (14,15). The same factors may have affected the SWE values of our study, which may have been the cause for differences in sensitivity, NPV, and specificity, PPV, accuracy according to measurement locations. Although there are some differences, the AUC value among the different measurement locations did not show statistically significant differences, based on which we can conclude that the measurement location does not affect the overall diagnostic performances of SWE. To our knowledge, our study is the first to show that there is a potential for different performances according to measurement location in S-Shearwave, which we can consider during application of breast US examinations. Also, mean elasticity values were 1) significantly higher for malignancy compared to benign in all four measurement locations, and 2) significantly higher for breast masses compared to the adjacent normal breast parenchyma (Table 1), consistent to the results of prior studies (14,15,16).
To calculate the diagnostic performances of S-Shearwave, a separate cut-off value was calculated regardless of the measurement location. The highest shearwave elasticity among the median value calculated from the three elasticity measurements obtained from the four locations was used to calculate this generally applicable cut-off value, calculated as 41.9 kPa. This calculation was based on the results of other studies in that high diagnostic performances were obtained when the higher of internal or marginal values were adopted (14,16,17). Similar to the prior studies, the diagnostic performances of S-Shearwave has highest AUC value (0.748) compared to the performances obtained from four different measurement locations. AUC values for S-Shearwave and US do not show significant differences, 0.748 to 0.794 (p = 0.179) in our study, showing comparable performances of S-Shearwave to grayscale morphologic assessments of US for the differential diagnosis of breast masses. Our results are in line to previous studies using SWE, showing that SWE alone cannot replace grayscale US for differential diagnosis of breast lesions detected on US, but as an adjunctive imaging tool (11,18).
RMI which was used in this study, is a unique value provided automatically in S-Shearwave which enables performers in selecting elasticity values obtained in adequate conditions, for example, hard compression force applied when performing SWE significantly affects values obtained. As SWE provides quantitative elasticity values, it has been considered to be more objective than conventional elastography, but even SWE values vary according to the clinical factors of the patient and also the performer especially during data acquisition (7). Applying RMI may enable acquisition of more reliable SWE data, reducing variability among performers, but further investigation is needed to reveal the true benefit of RMI in SWE.
There are some limitations to this study. First, one radiologist was involved in S-Shearwave measurement and grayscale US interpretation, and different results may have been obtained if more radiologists were involved in SWE measurement and US interpretation. Second, in order to avoid missing data, S-Shearwave measurement was repeatedly performed until a valid numeric elasticity was obtained, which may have affected the SWE data accuracy and also the optimal cut-off levels. Prior studies mention the inclusion of ‘non-numeric’ values (15,17), in which technical advances are required for more accurate data measurement. In addition, since we did not have an optimal cut-off level set during data acquisition, how S-Shearwave changes the diagnostic performances of breast US examinations has not been evaluated in this study. Further studies revealing the role of S-Shearwave on breast US are anticipated. Last, due to the limited number of breast lesions included, we could not provide a guideline for the optimal measurement location.
In conclusion, S-Shearwave has comparable diagnostic performances to grayscale US regardless of measurement location, that can be applied for differential diagnosis of breast masses seen on US.
Acknowledgments
This study has been supported by the research fund of Samsung Medison, Co. Ltd.
Footnotes
- Conceptualization, Y.J.H., K.E.
- data curation, Y.J.H., K.E.
- formal analysis, L.E.J., K.H.Y.
- investigation, L.M.H., Y.J.H.
- methodology, Y.J.H., K.E.
- project administration, Y.J.H., K.E.
- resources, Y.J.H.
- software, Y.J.H., L.E.J., K.H.Y.
- writing—original draft, L.M.H., Y.J.H.
- writing—review & editing, all authors.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.American College of Radiology. Breast imaging reporting and data system. 5th ed. Reston, VA: American College of Radiology; 2013. [Google Scholar]
- 2.Hong AS, Rosen EL, Soo MS, Baker JA. BI-RADS for sonography: positive and negative predictive values of sonographic features. AJR Am J Roentgenol. 2005;184:1260–1265. doi: 10.2214/ajr.184.4.01841260. [DOI] [PubMed] [Google Scholar]
- 3.Kim EK, Ko KH, Oh KK, Kwak JY, You JK, Kim MJ, et al. Clinical application of the BI-RADS final assessment to breast sonography in conjunction with mammography. AJR Am J Roentgenol. 2008;190:1209–1215. doi: 10.2214/AJR.07.3259. [DOI] [PubMed] [Google Scholar]
- 4.Costantini M, Belli P, Lombardi R, Franceschini G, Mulè A, Bonomo L. Characterization of solid breast masses: use of the sonographic breast imaging reporting and data system lexicon. J Ultrasound Med. 2006;25:649–659. doi: 10.7863/jum.2006.25.5.649. quiz 661. [DOI] [PubMed] [Google Scholar]
- 5.Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–350. doi: 10.1148/radiol.2391041676. [DOI] [PubMed] [Google Scholar]
- 6.Lee EJ, Jung HK, Ko KH, Lee JT, Yoon JH. Diagnostic performances of shear wave elastography: which parameter to use in differential diagnosis of solid breast masses? Eur Radiol. 2013;23:1803–1811. doi: 10.1007/s00330-013-2782-5. [DOI] [PubMed] [Google Scholar]
- 7.Yoon JH, Jung HK, Lee JT, Ko KH. Shear-wave elastography in the diagnosis of solid breast masses: what leads to false-negative or false-positive results? Eur Radiol. 2013;23:2432–2440. doi: 10.1007/s00330-013-2854-6. [DOI] [PubMed] [Google Scholar]
- 8.Berg WA, Cosgrove DO, Doré CJ, Schäfer FK, Svensson WE, Hooley RJ, et al. Shear-wave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Radiology. 2012;262:435–449. doi: 10.1148/radiol.11110640. [DOI] [PubMed] [Google Scholar]
- 9.Burnside ES, Hall TJ, Sommer AM, Hesley GK, Sisney GA, Svensson WE, et al. Differentiating benign from malignant solid breast masses with US strain imaging. Radiology. 2007;245:401–410. doi: 10.1148/radiol.2452061805. [DOI] [PubMed] [Google Scholar]
- 10.Cho N, Moon WK, Kim HY, Chang JM, Park SH, Lyou CY. Sonoelastographic strain index for differentiation of benign and malignant nonpalpable breast masses. J Ultrasound Med. 2010;29:1–7. doi: 10.7863/jum.2010.29.1.1. [DOI] [PubMed] [Google Scholar]
- 11.Chang JM, Moon WK, Cho N, Yi A, Koo HR, Han W, et al. Clinical application of shear wave elastography (SWE) in the diagnosis of benign and malignant breast diseases. Breast Cancer Res Treat. 2011;129:89–97. doi: 10.1007/s10549-011-1627-7. [DOI] [PubMed] [Google Scholar]
- 12.Choi K, Kong D, Hah Z, Lee HK. A reliability index of shear wave speed measurement for shear wave elastography. Piscataway: IEEE; 2015. [Google Scholar]
- 13.Deffieux T, Gennisson JL, Bercoff J, Tanter M. On the effects of reflected waves in transient shear wave elastography. IEEE Trans Ultrason Ferroelectr Freq Control. 2011;58:2032–2035. doi: 10.1109/TUFFC.2011.2052. [DOI] [PubMed] [Google Scholar]
- 14.Tozaki M, Isobe S, Fukuma E. Preliminary study of ultrasonographic tissue quantification of the breast using the acoustic radiation force impulse (ARFI) technology. Eur J Radiol. 2011;80:e182–e187. doi: 10.1016/j.ejrad.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Wojcinski S, Brandhorst K, Sadigh G, Hillemanns P, Degenhardt F. Acoustic radiation force impulse imaging with Virtual Touch™ tissue quantification: mean shear wave velocity of malignant and benign breast masses. Int J Womens Health. 2013;5:619–627. doi: 10.2147/IJWH.S50953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tozaki M, Isobe S, Sakamoto M. Combination of elastography and tissue quantification using the acoustic radiation force impulse (ARFI) technology for differential diagnosis of breast masses. Jpn J Radiol. 2012;30:659–670. doi: 10.1007/s11604-012-0106-3. [DOI] [PubMed] [Google Scholar]
- 17.Teke M, Göya C, Teke F, Uslukaya Ö, Hamidi C, Çetinçakmak MG, et al. Combination of virtual touch tissue imaging and virtual touch tissue quantification for differential diagnosis of breast lesions. J Ultrasound Med. 2015;34:1201–1208. doi: 10.7863/ultra.34.7.1201. [DOI] [PubMed] [Google Scholar]
- 18.Evans A, Whelehan P, Thomson K, McLean D, Brauer K, Purdie C, et al. Quantitative shear wave ultrasound elastography: initial experience in solid breast masses. Breast Cancer Res. 2010;12:R104. doi: 10.1186/bcr2787. [DOI] [PMC free article] [PubMed] [Google Scholar]