Abstract
Voiding cystourethrography (VCUG) demonstrates the anatomy of the urinary system and is used to detect the presence/absence of vesicoureteral reflux. It is the most important modality for urological fluoroscopic examination in children. For improved patient care, it is important to understand and perform VCUG appropriately. Therefore, an in-depth review of VCUG protocols and techniques has been presented herein. In addition, tips, tricks, and pitfalls associated with the technique have also been addressed.
Keywords: Children, Cystography, Vesicoureteral Reflux, Urinary Bladder, Urinary Tract
Abstract
배뇨방광요도조영술은 소아의 비뇨기과적 투시 검사에서 가장 중요한 검사이다. 배뇨방광요도조영술로 비뇨기계의 해부학적 구조와, 방광 요관 역류의 유무를 검사할 수 있다. 환자 치료의 궁극적인 목표를 달성하려면 배뇨방광요도조영술을 적절하게 이해하고 수행하는 것이 중요하다. 이에, 심층적인 배뇨방광요도조영술의 술기 순서 및 기법에 대해 소개하였다. 또한, 배뇨방광요도조영술과 관련된 요령과 함정들을 다루었다.
INTRODUCTION
The aim of voiding cystourethrography (VCUG) is to demonstrate the anatomy and function of the bladder and the urethra. It is a dynamic procedure that reflects the function and coordination of the lower urinary system. The most important indication for performing VCUG is to evaluate the presence or absence of vesicoureteral reflux (VUR) (1,2,3). The associated conditions of VUR are congenital anomalies of the urinary tract (anorectal malformation, myelodysplasia, or prune-belly syndrome), febrile urinary tract infection (particularly, if recurrent), hydronephrosis or hydroureter, hematuria, voiding abnormalities (dysuria, dysfunctional voiding such as neurogenic bladder, or incontinence), neonatal ascites, trauma, and postoperative evaluation of urinary tract (Table 1) (1,4).
Table 1. Indications for Voiding Cystourethrography.
| 1. Anomalies of the urinary tract | |
| 1) Anorectal malformation | |
| 2) Myelodysplasia | |
| 3) Prune-belly syndrome | |
| 2. Febrile urinary tract infection, particularly if recurrent | |
| 3. Hydronephrosis or hydroureter | |
| 4. Hematuria | |
| 5. Voiding abnormalities | |
| 1) Dysuria | |
| 2) Dysfunctional voiding such as neurogenic bladder | |
| 3) Incontinence | |
| 6. Neonatal ascites | |
| 7. Trauma | |
| 8. Postoperative evaluation of urinary tract | |
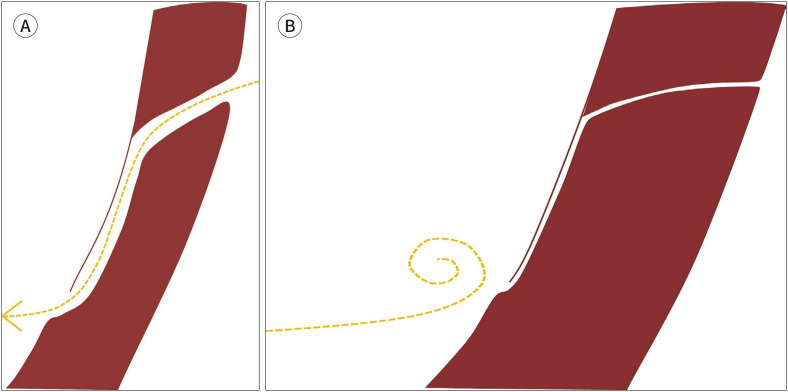
The VUR is defined as the retrograde passage of urine from the urinary bladder into the ureter and often to the calyces. The normal ureterovesical junction (UVJ) is closed by contracture during voiding to protect the upper urinary tract from reflux, which is called the antireflux action of the UVJ (Fig. 1) (1,2,5). Slanted entry and submucosal tunneling of sufficient length in the ureter are the key components involved in the antireflux action (1,2,5). These two components prevent VUR by constriction and compression of intramural ureter when bladder contracts (1,2,5). The causes of VUR are divided into primary and secondary. The primary VUR is caused due to defect in antireflux action, which is a consequence of anomaly of UVJ or immaturity of UVJ in young infants (2,6). The secondary VUR is caused due to malfunction within the urinary system such as bladder-outlet obstruction or neurogenic bladder, and infection (2,3,7). In active urinary tract infection, reversible VUR can occur because infection itself can affect UVJ (2).
Fig. 1. Normal configuration of the vesicoureteral junction and antireflux action of the vesicoureteral reflux.
A. Slanted entering and submucosal tunneling of the ureter of sufficient length is the normal configuration of the vesicoureteral junction. The yellow dotted line represents a downstream flow of the urine.
B. The normal ureterovesical junction is closed during contracture on voiding by constriction and compression of the intramural ureter to protect the upper urinary tract from reflux, which is called the antireflux action of the vesicoureteral junction. The yellow dotted line represents a blocked urine flow without reflux.
To achieve the ultimate medical goal, reviewing previous imaging studies and medical records, and communicating with the referred physicians improve complete performance of VCUG (1). Likewise, in all other X-ray imaging studies, the principle of As Low As Reasonably Achievable (ALARA) should be followed by using pulsed fluoroscopy with last image hold technique (8,9). In addition, understanding and skilled application of protocols and techniques of VCUG is important.
PREPARATION
PSYCHOLOGICAL PREPARATION
Apart from physical preparation, psychological preparation is necessary for both, patients and parents as they may be anxious due to fear of pain and unknown, urethral catheterization, and radiation use (Fig. 2) (1). To help both patients and parents relieve the anxiety from the VCUG, providing a translated explanatory pamphlet provided by The Image Gently Campaign of The Alliance for Radiation Safety in Pediatric Imaging (https://www.imagegently.org) can be used as a solution (1,10). In addition, introducing the procedure to the patients and the parents is also recommended just before the examination (1). Mild sedation can be considered in case of uncooperative patients; however, alert state is preferred for physiologic voiding (11,12).
Fig. 2. Psychological preparation necessary for both patients and parents.
SUPPLIES
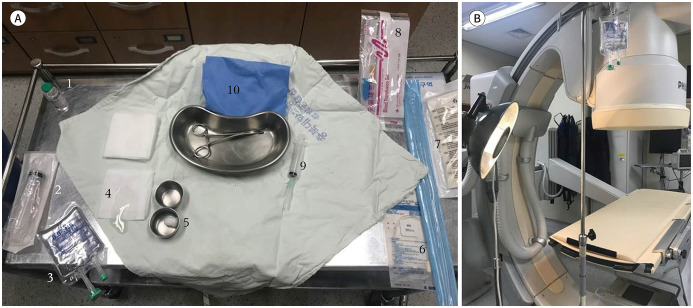
Before the examination, the supplies should be prepared (Fig. 3A). The contrast for VCUG at our institute is prepared by mixing 30 mL of iodine-containing contrast (300 or 350 mg I/mL, Iohexol; BONOREX, Central Medical Service, Seoul, Korea) with 100 mL saline. A tip for contrast is to keep concentration under 30% to avoid chemical irritation (12). Five-French feeding tubes for infants, 8-French feeding tubes for children, or a catheter larger than 8-French feeding tube for adolescents should be used (4). Also, few chlorhexidine balls for skin sterilization, sterile lubricant gel for coating catheter, a plastic extension tubing, a syringe for regurgitating urine bladder, one inch of tape for anchoring catheter to the skin, and sterile surgical drape having a hole are used. A warmer for maintaining body temperature of infant and light for better visibility during catheter insertion are also helpful (Fig. 3B).
Fig. 3. Supplies for voiding cystourethrography.
A. From the left upper corner in a counterclockwise direction: 1) iodine-containing contrast (300 or 350 mg/mL); 2) syringe for contrast mixing; 3) saline bag; 4) sterile lubricant gel; 5) chlorhexidine balls; 6) 5- and 8-French catheters; 7) sterile surgical gloves; 8) plastic extension tubing; 9) syringe for regurgitation of urine; and (10) sterile surgical drape with a hole.
B. Warmer for maintaining the body temperature in young infants and light for better visibility during catheter insertion.
IMAGING
CATHETERIZATION WITH GENTLE HANDLING
Parents are recommended to stand beside their children for comforting them during the procedure. If the patient's mother is pregnant, she is advised to be with the patient only during catheter insertion. For girls, sterilization of perineal skin and interlabial area with chlorhexidine balls is the first step. Next, a surgical drape having a hole should be secured and a catheter coated with lubricant gel should be inserted gently. Anchoring a catheter with tape on the inner thigh is recommended in girls. Often, the labial adhesion is encountered. Unless the urethral opening is exposed, VCUG can be performed after treating labial adhesion and reassessing the need for VCUG (1).
For boys, sterilization of perineal and penile skin including penile tip after retracting foreskin with chlorhexidine balls is the first step. The next step is to secure a surgical drape having a hole, followed by insertion of a catheter coated with lubricant gel, and anchoring catheter with tape to lower abdominal skin and penis. The foreskin is common in an infant, which makes it difficult to insert a catheter. Therefore, retracting the foreskin and exposing the urethral opening is a tip for successful insertion of catheter in boys (1). After finishing catheterization, the foreskin should be reduced. If foreskin is retracted unnecessarily for a longer time, it gets trapped behind the glans, causing edema of the glans (4). Insert the catheter as much as you need by winding it, once inside the urinary bladder. Excessive catheter insertion can trigger knotting within the urinary bladder and may need longer removal time (4). Then, drain naturally or regurgitate urine with a syringe to empty the urinary bladder (12).
INSTILLING CONTRAST INTO EMPTIED BLADDER TILL FILLED TO NEAR CAPACITY
Contrast and saline mixture is hanged about 1 m above the table to naturally instill it into the emptied bladder. Do not squeeze plastic bag containing contrast and saline mixture to instill faster because manual pressure can produce artificial VUR. Instill contrast and saline mixture to near full capacity. The estimate of the near full capacity of the urinary bladder is different in children of different ages. Approximate volume of the urinary bladder can be calculated by the formulas (1):
(Kg × 7) mL in an infant
[(age + 2) × 30] mL in children
For example, approximate volume of the urinary bladder is 35 mL in 5 kg infants, 70 mL in 10 kg infant, and 100 mL in 1.5-year-old children. When the bladder is full, the infants begin crying and flexing their toes.
IMAGE OPTIMIZATION
Under the ‘ALARA’ principle, performers should store focused images of critical areas and conditions. Pulsed fluoroscopy with last image hold technique and adjustment of collimators are key strategies to avoid unnecessary exposure to radiation (9). Continuous fluoroscopy should be avoided during filling of urinary bladder; brief and intermittent fluoroscopy is sufficient. Increasing the distance between the child and the X-ray source and removing the antiscatter grid for small patients are also recommended (13). Antiscatter grid itself is source of scattered radiation and is less useful in small patients, because smaller patient leads to less scattered radiation. Moreover, reducing patient dose is closely related to staff protection by reducing scattered radiation from a patient which is proportional to staff radiation.
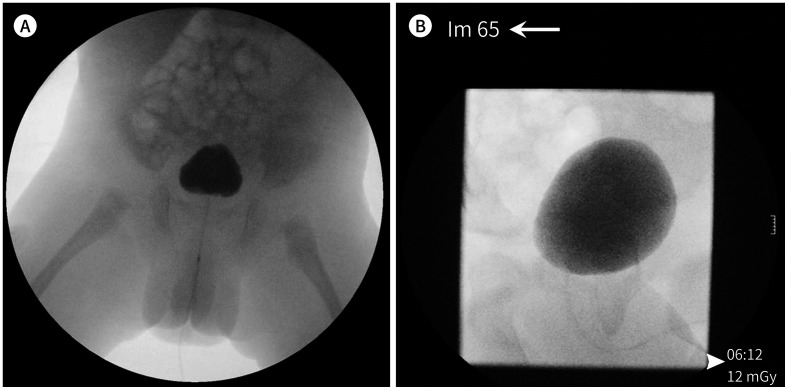
STORING FOCUSED IMAGING OF CRITICAL AREAS AND CONDITIONS
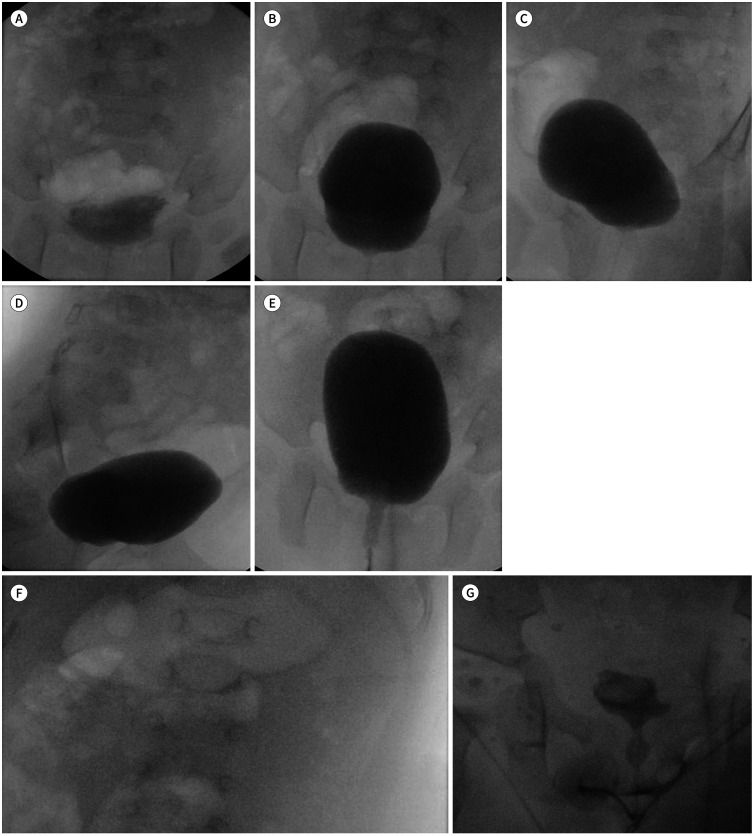
A standardized evaluation of critical areas and conditions should be ensured and are categorized into anteroposterior (AP) projection of urinary bladder during early filling phase (Fig. 4A), full filling phase of urinary bladder (Fig. 4B), the oblique projection of urinary bladder focusing both UVJs (Fig. 4C, D), an AP projection of urinary bladder during voiding (Fig. 4E), renal collecting system with or without presence of reflux (Fig. 4F), an AP projection of urinary bladder post voiding (Fig. 4G), and lateral projection for urethra during voiding in boys. A scout image is not a significant image in the management decision although its dose is low (14). Therefore, obtaining a routine scout image is not recommended. In the early filling phase, the AP image of urinary bladder demonstrates ureteroceles (Fig. 5). If any abnormality is observed, oblique projections of the urinary bladder to evaluate further distal ureters should be used (Fig. 6A). The presence of ureteroceles with or without eversion, or diverticulum is demonstrated on oblique images clearly (Fig. 6B, C). To grade VUR using VCUG, focused images targeting renal collecting system are essential. In the absence of VUR, capturing images at renal collecting system is recommended for the evidence of negative VUR. Images for the urethra, especially in boys, are easy to be missed, however, it is important. To evaluate urethra, lateral projection during voiding is standardly used. The fluoroscopic time and dose-area product are documented on the last image of study (Fig. 4G). Dimming of room lights, being patient and calm, erect positioning, the sound of flowing water, instilling water on the toes or perineum, and encouragement can be helpful when older girls or adolescents hesitate to void (1). Occasionally, infants void after removal of catheter (11).
Fig. 4. Standardized evaluation of voiding cystourethrography in critical areas and conditions.
A. AP projection of the urinary bladder in the early filling phase.
B. AP projection of the urinary bladder in the late filling phase.
C, D. Oblique projection of the urinary bladder focusing on the vesicoureteral junction.
E. AP projection of the urinary bladder during voiding.
F. Renal collecting system with and without the presence of reflux.
G. AP projection of the urinary bladder after voiding.
AP = anteroposterior
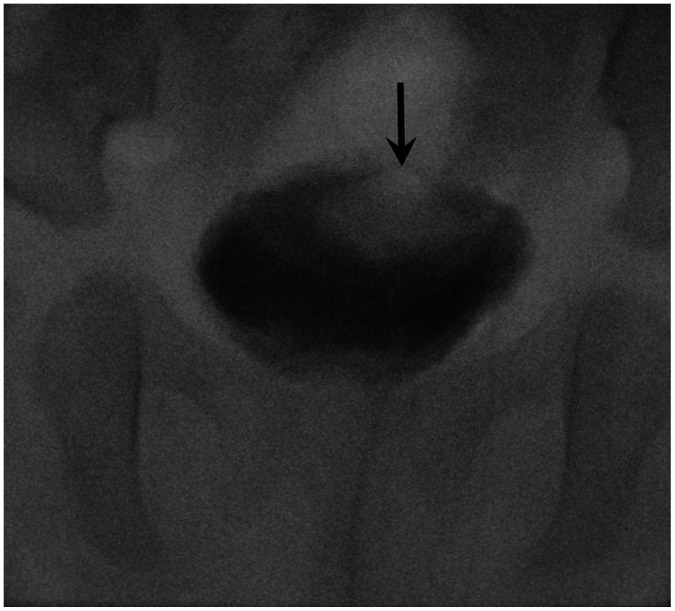
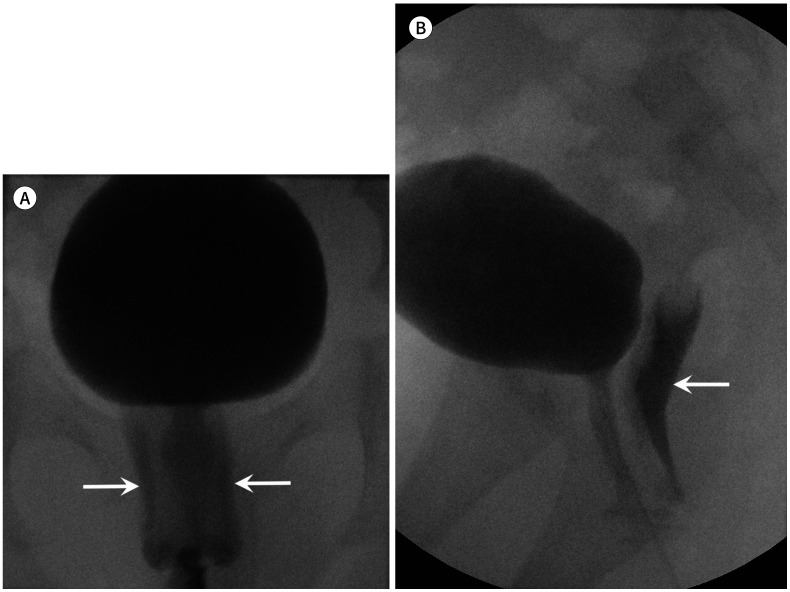
Fig. 5. Anteroposterior image of the urinary bladder demonstrating ureteroceles (arrow) in the early filling phase.
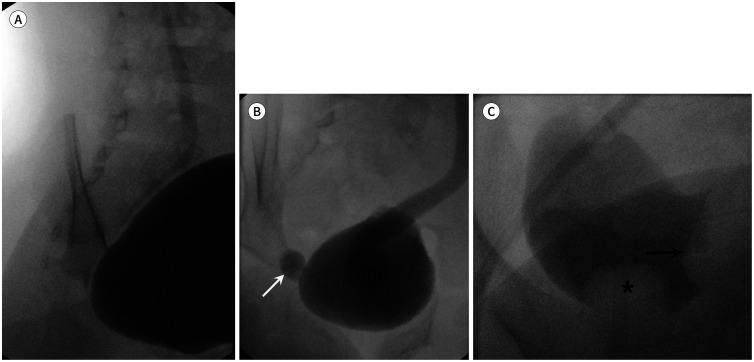
Fig. 6. Value of the oblique projection of the urinary bladder focusing on the vesicoureteral junction.
A. The vesicoureteral reflux is well-demonstrated on oblique projection.
B. The presence of ureteroceles with eversion (arrow) is well-demonstrated on oblique projection.
C. The intravesical simple ureterocele (arrow) is well-demonstrated on oblique projection. The filling defect at the bladder apex (asterisk) is ballooning of the Foley catheter.
The cyclic VCUG is refilling the bladder following voiding in multiple times within the catheter in place and is valuable in infant to avoid missing significant reflux and potential ectopic ureter (Fig. 7) (15,16,17). Refluxed contrast medium is diluted by unopacified urine in the first session. But refluxed contrast medium is better demonstrated on the second session for less dilution. In our institution, two sessions of cyclic VCUG are performed in infants to maximize detection of VUR.
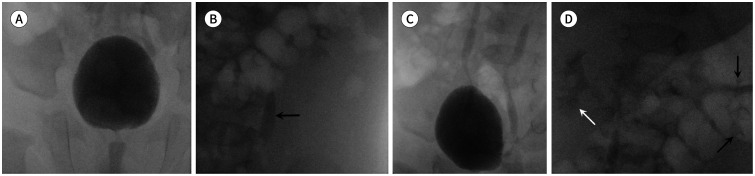
Fig. 7. Value of cyclic VCUG.
A, B. Grade I (arrow, B) of the left VUR is demonstrated in the first session of VCUG. VUR is absent in the right urinary system.
C, D. In the second session of VCUG, the left VUR grade changes from I to II (black arrows, D). The newly developed grade II of the right VUR (white arrow) is demonstrated. Finally, bilateral grade II VUR (white and black arrows) is demonstrated in the second session of VCUG.
VCUG = voiding cystourethrography, VUR = vesicoureteral reflux
INTERPRETATION
GRADING VUR
The grading for severity of VUR is according to the International Reflux Study in Children and is based on VCUG (Table 2) (12). The higher the grade and the prolonged the morbidity, worse is the prognosis. Although, mild VUR (grade I and II) resolves spontaneously with age in the first decade of life, timely detection and immediate intervention of severe VUR (grade III, IV, and V) is critical to prevent sequels such as renal scarring, hypertension, and end-stage renal diseases (2,3,6). To achieve the ultimate goal of VCUG, acquaintance with VUR grading system and appropriate reporting of VUR is essential. Although, the degree of ureteral dilatation depicted in the grading system, criteria for mild, moderate and severe dilatation are not clear (12). The reflux nephropathy (renal scarring) is characterized by atrophy, tubular destruction, and interstitial fibrosis, and almost always accompanies blunting or distortion of the calyx (3,18). Therefore, it is important to examine calyceal blunting clearly.
Table 2. International Criteria for Grading of the VUR Based on Voiding Cystourethrography Findings.
| VUR Grade | Findings |
|---|---|
| Grade I | Ureter only |
| Grade II | Ureter, pelvis and calyces; no dilatation, normal calyceal fornices |
| Grade III | Mild or moderate dilatation and/or tortuosity of the ureter and mild or moderate dilatation of the renal pelvis |
| No or slight blunting of the fornices | |
| Grade IV | Moderate dilatation and/or tortuosity of the ureter and moderate dilatation of the renal pelvis and calyces |
| Complete obliteration of the sharp angle of the fornices but maintenance of the papillary impressions in the majority of calyces | |
| Grade V | Gross dilatation and tortuosity of the ureter. Gross dilatation of the renal pelvis and calyces |
| The papillary impressions are no longer visible in the majority of the calyces |
VUR = vesicoureteral reflux
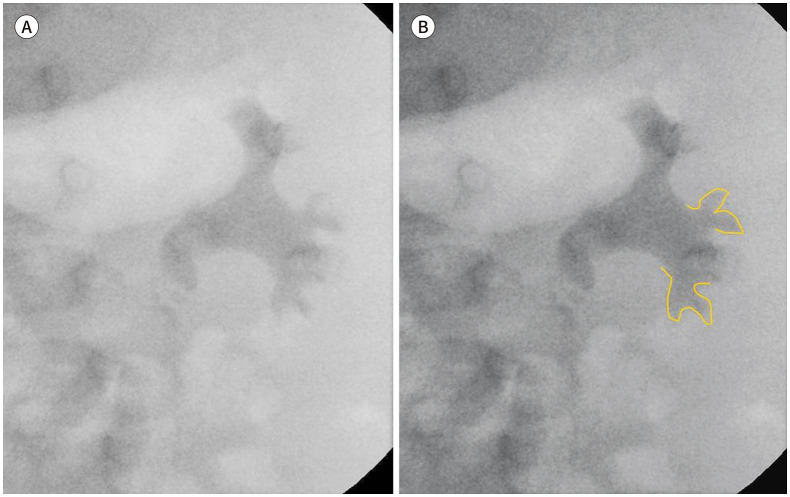
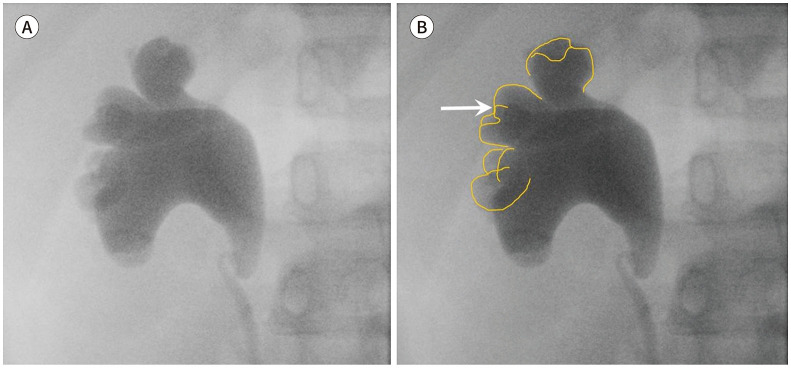
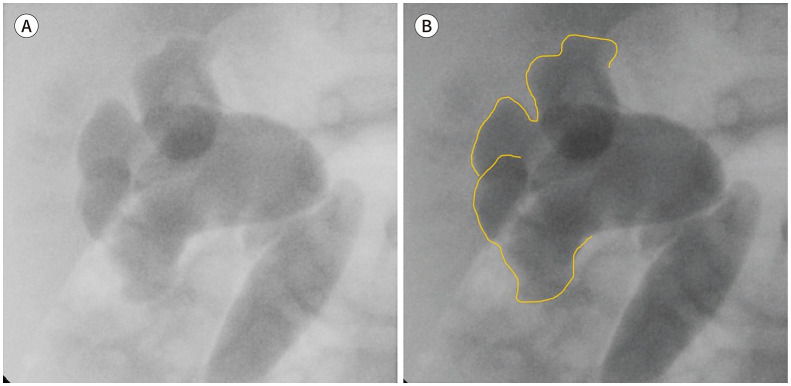
In key features, grade I reflux does not reach the renal pelvis and has a questionable clinical impact (Fig. 8) (2,3). Grade II reflux reaches the renal pelvis but does not dilate fornices (Fig. 9). Grade III reflux does not or minimally deform fornices (Fig. 10). It is borderline grade between grade II and grade IV reflux. Grade IV reflux presents blunt fornices, but the impression of papillae is not visible in majority of papillae (Fig. 11). Grade V reflux is characterized by loss of papillary impression (Fig. 12). In reporting, the maximal degree of VUR is described (12).
Fig. 8. Vesicoureteral reflux grade I.
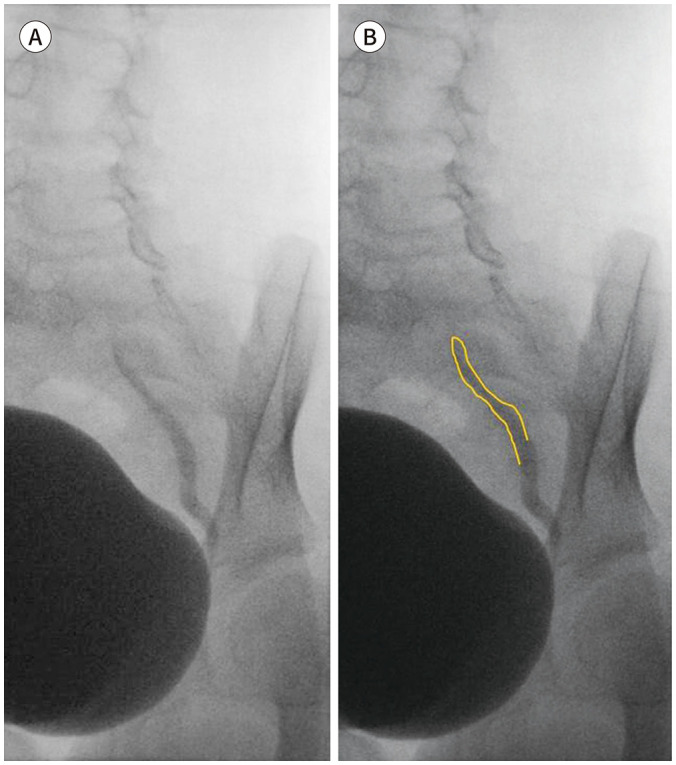
A. Vesicoureteral reflux grade I: ureter.
B. The border of refluxed contrast is marked with yellow line.
Fig. 9. Vesicoureteral reflux grade II.
A, B. Vesicoureteral reflux grade II: ureter, pelvis, and calyces; no dilatation; normal calyceal fornices.
Fig. 10. Vesicoureteral reflux grade III.
A, B. Vesicoureteral reflux grade III: mild to moderate dilatation and/or tortuosity of the ureter and mild to moderate dilatation of the renal pelvis; no or slight blunting of the fornices.
Fig. 11. Vesicoureteral reflux grade IV.
A, B. Vesicoureteral reflux grade IV: moderate dilatation and/or tortuosity of the ureter and moderate dilatation of the renal pelvis and calyces; complete obliteration of the sharp angle of the fornices but maintenance of the papillary impressions (arrow, B) in most calyces.
Fig. 12. Vesicoureteral reflux grade V.
A, B. Gross dilatation and tortuosity of the ureter and gross dilatation of the renal pelvis and calyces; papillary impressions are no longer visible in most calyces.
BLADDER AND URETHRA
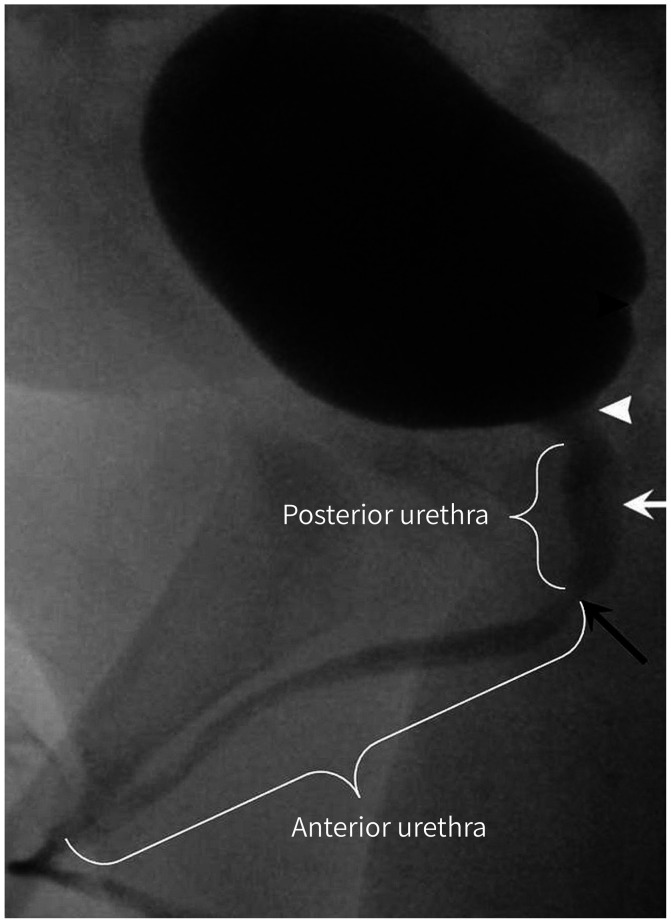
On VCUG, the inner wall of urinary bladder on AP projection is smooth and its contour is round. The interureteric ridge which is the elevated border of trigone in cephalad, is visible on the lateral projection at about distal one-quarter of the posteroinferior urinary bladder (Fig. 13). Any other space occupying lesions, fistulous or diverticular structures suggesting mass, urachal remnant, or diverticulum observed during VCUG should be reported.
Fig. 13. Lateral anatomy of the urinary bladder and urethra. The interureteric ridge (black arrowhead) is the elevated border of the trigone toward the head. It is visible on lateral projection in approximately the distal one-quarter of the posteroinferior urinary bladder. The cone-shaped portion is the bladder neck (white arrowhead), which is continuous with the bladder apex. The elongated, faint filling defect below the bladder neck is the verumontanum (white arrow), which is the rounded eminence of the urethral crest in the posterior wall of the mid prostatic urethra. The shortest (about 1 cm long) and narrowest portion of the urethra is the membranous urethra (black arrow). The urethra is divided into the anterior and posterior urethra at the lower end of the membranous urethra; distal to the lower end of the membranous urethra is the anterior urethra, while proximal to the lower end of the membranous urethra is the posterior urethra.
Urethral evaluation is critical in boys (Fig. 13). Therefore, it is better to prepare the field of view and lateral position to demonstrate optimal view of urethra (4). Posterior urethral valve is the result of remaining and fused anterior mucosal folds which should be absorbed during normal development. Posterior urethral valve may lead to decompensation of the urinary bladder, distal ureteral obstruction, and end-stage renal disease (1). Oligohydramnios, bladder distention, bilateral hydroureteronephrosis, and occasionally fetal ascites are the manifestation of the severe obstruction of posterior urethral valve (1,2). Normal fold at posterior urethra is often seen, therefore, along with flap-like filling defect, disproportional dilatation of posterior urethra during voiding is also observed in posterior urethral valve (1). Removal of the catheter during voiding is recommended for proper evaluation of posterior urethral valve (1).
MISCELLANEOUS CONDITIONS
LOW-PRESSURE VUR
VUR commonly occurs during voiding; however, reflux can occur in a low-pressure condition during early phase of bladder filling (Fig. 14) (2). As published, VUR with low-pressure during early filling is associated with poor resolution and increased risk for acute pyelonephritis (19,20).
Fig. 14. Low-pressure vesicoureteral reflux. The vesicoureteral reflux occurred in the early phase of bladder filling. Vesicoureteral reflux with low-pressure and early filling is associated with poor resolution and increased risk for acute pyelonephritis.
CONTRAST REFLUX OR INADVERTENT CATHETER INSERTION INTO THE VAGINA
It is important to insert the catheter via urethral opening and check that the catheter is properly inserted before infusing the contrast. If the catheter enters the vagina, remove it immediately. During voiding, contrast reflux into the vagina is common in girls (Fig. 15). There are various causes of vaginal reflux which are not clear; however, adhesions of the labia minora, ectopic ureteral insertion, and dysfunctional pelvic floor musculature are discussed (2,21).
Fig. 15. Contrast reflux in the vagina.
A, B. Contrast reflux in the vagina (arrows), which is common in girls during voiding, is noted on anteroposterior (A) and lateral (B) projections.
INTRA-RENAL REFLUX
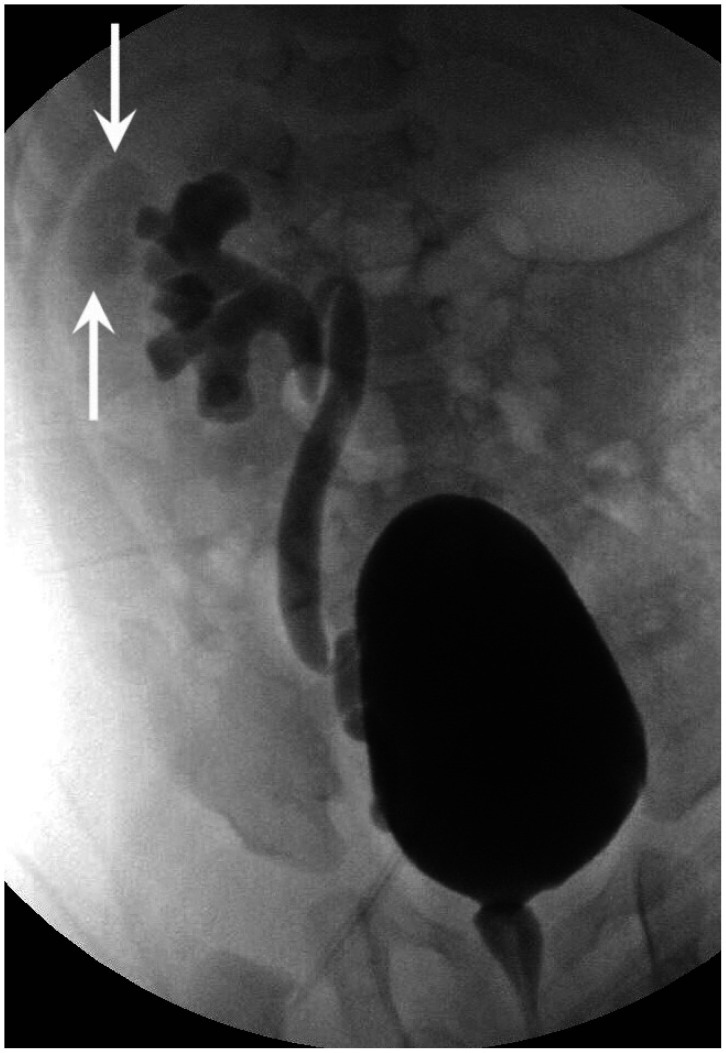
Intra-renal reflux refers to reflux of contrast into renal papilla via ducts of Bellini (1). It is not included in the international criteria for grading VUR; however, it should be described separately because it is an important factor for renal scarring in ascending infection (1). The prevailing sites for intrarenal reflux are upper pole and lower pole of the kidney, respectively, due to presence of compound papillae (Fig. 16) (2).
Fig. 16. Intra-renal reflux. The intra-renal reflux refers to the reflux of contrast in the renal papilla via the ducts of Bellini (arrows). It is not included in the international criteria for grading of vesicoureteral reflux; however, it should be described, as it is an important factor for renal scarring in ascending infection.
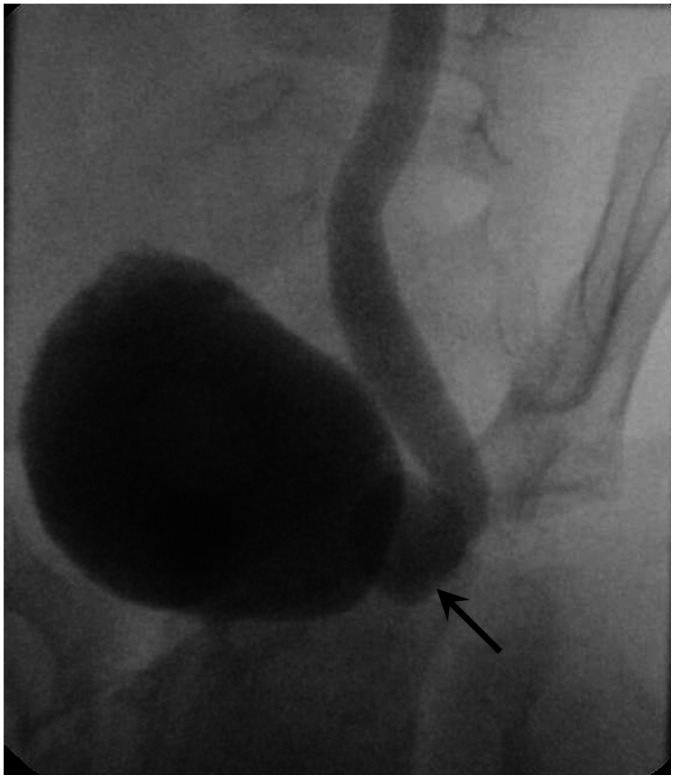
PARAURETERAL (HUTCH) DIVERTICULUM
Diverticulum at UVJ is called paraureteral or Hutch diverticulum (Fig. 17). It is associated with VUR by negating normal arrangement of UVJ (Fig. 18) (2). Therefore, VUR from Hutch diverticulum does not resolve without surgical correction and leaves renal scar (2). In this regard, radiologists are recommended to capture images of the urinary bladder in oblique projection focusing UVJ and should report the presence of Hutch diverticulum.
Fig. 17. Paraureteral (Hutch) diverticulum. Diverticulum at the ureterovesical junction is called the paraureteral or Hutch diverticulum (arrow). The vesicoureteral reflux is associated with the Hutch diverticulum. The vesicoureteral reflux from the Hutch diverticulum does not resolve without surgical correction and leaves causes renal scarring.
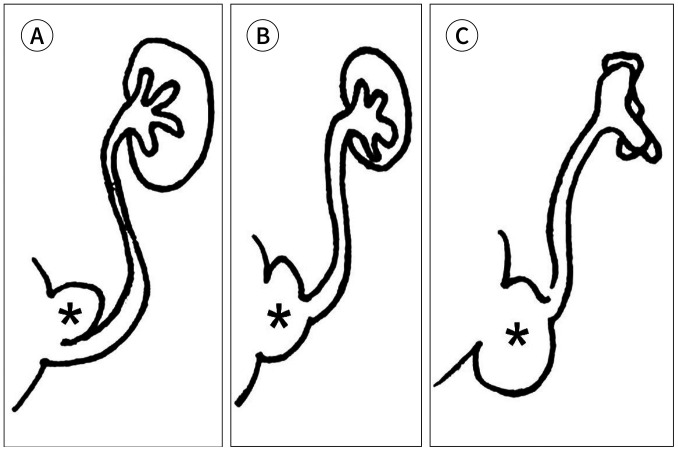
Fig. 18. Physiology and time course of the vesicoureteral reflux associated with the paraureteral diverticulum (asterisks).
A. When the ureter opens on the rim of the diverticulum, and the bladder is completely distended, the ureteral orifice is incorporated transiently in the bladder diverticulum.
B. When the ureter enters the diverticulum directly, the ureteral orifice is incorporated permanently in the bladder diverticulum.
C. In both A and B, the antireflux ureterovesical mechanism is rendered incompetent and leads to secondary vesicoureteral reflux and endstage renal disease.
ERRONEOUS PERFORMANCE
Obtaining images without collimation (Fig. 19A) and excessive number of images are common errors made by beginners (Fig. 19B). Radiologists need to remember the required adjustments to achieve ALARA principle in practice before performing VCUG.
Fig. 19. Erroneous performance.
A. Obtaining images without collimation.
B. Obtaining excessive number of images (arrow) and taking excessive fluoroscopic time (arrowhead).
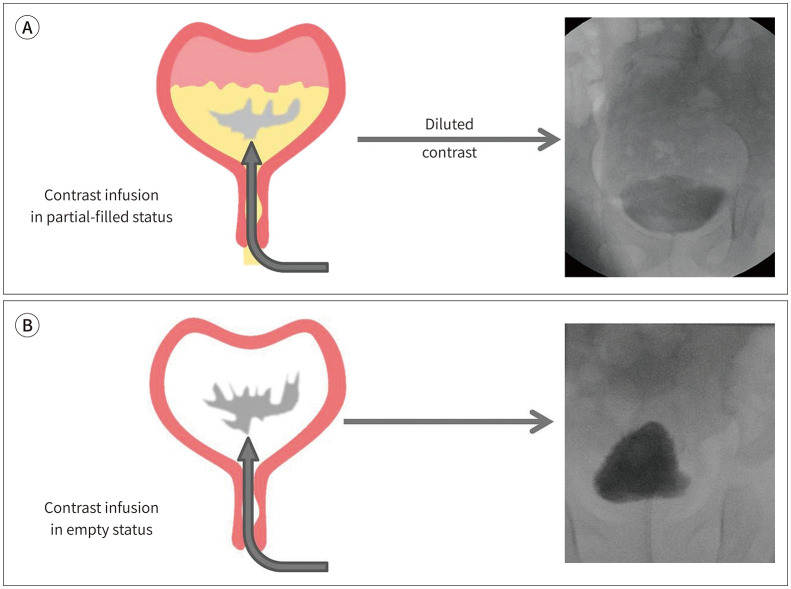
Although, contrast mixture was strictly prepared according to the standards, insufficient opacity of contrast may be due to its dilution with remaining urine in the bladder (Fig. 20A). Therefore, natural drainage or regurgitation with the syringe after anchoring catheter on the skin is necessary (Fig. 20B).
Fig. 20. Contrast diluted with the remaining urine.
A. Although the contrast mixture was strictly made using the standard recipe, insufficient opacification of the contrast may be associated with dilution with the remaining urine in the bladder.
B. Emptying the bladder through natural drainage or regurgitation with a syringe after the anchoring catheter renders sufficient opacification.
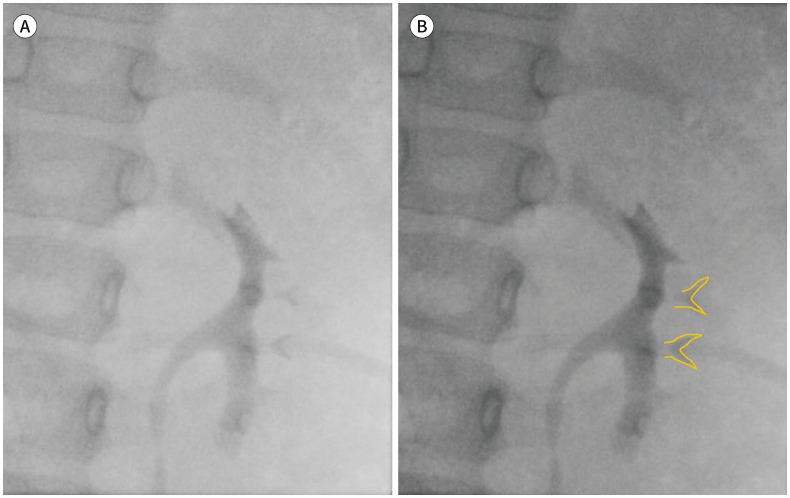
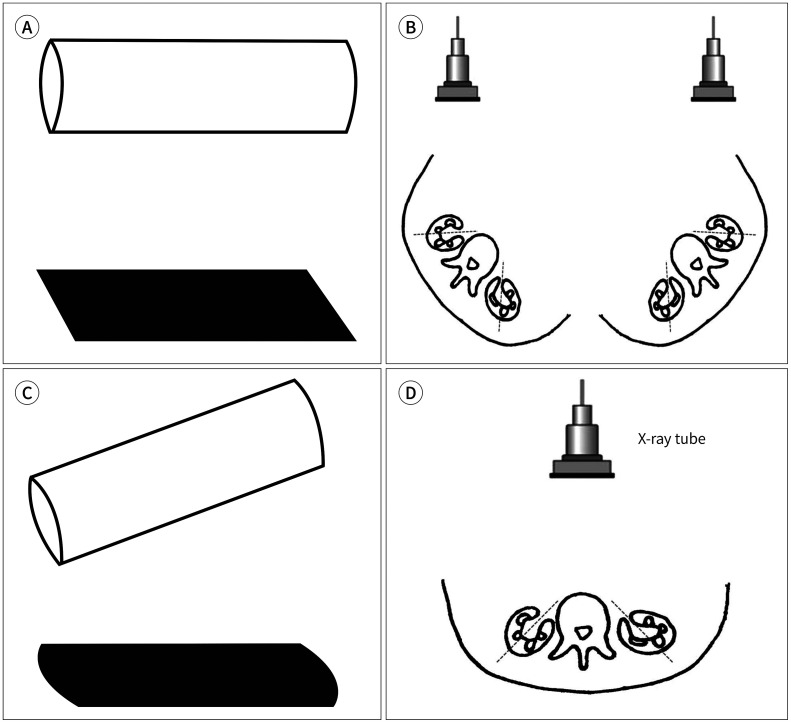
The presence or absence of calyceal blunting is an important factor in determining VUR grading. The orthographic projection is a method in which an object is imaged using projection parallel to the principle axes (Fig. 21A, B) (22). The actual contour of calyx can be altered by oblique projection (Fig. 21C, D). Therefore, an accurate evaluation of the orthogonal plane is required. The orthogonal plane for calyceal evaluation is tangential to the renal hilar axis which is directed anteromedially (Fig. 21B). It is recommended to prepare the patient's body for the tangential projection of the expected renal hilum.
Fig. 21. Value of the orthographic projection and application on calyceal evaluation.
A. In the orthographic projection, objects are represented on parallel projection to the principal axes. An accurate evaluation of the actual contour of objection is demonstrated by the orthogonal plane.
B. The orthogonal plane for calyceal evaluation is tangential to the renal hilar axis, which is directed anteromedially. It is recommended to prepare the patient's body for the tangential projection of the expected renal hilum.
C. The actual contour of the object can be altered using the oblique projection.
D. Calyceal blunting can be distorted in the anteroposterior projection to the body which is oblique projection to calyces.
CONCLUSION
VCUG is the most common and standard test demonstrating VUR. Radiologists need to know the clinical issues of VCUG in advance, prepare the proper supplies, and take appropriate action and judgment accordingly. They should be familiar with the essential elements of grading, calyceal blunting, papillary impressions, and various conditions that may be associated with it.
Footnotes
- Conceptualization, K.Y.J.
- data curation, K.Y.J.
- funding acquisition, K.Y.J.
- investigation, all authors.
- project administration, K.Y.J.
- supervision, K.Y.J.
- visualization, K.Y.J.
- writing—original draft, K.Y.J.
- writing—review & editing, K.Y.J.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Kirks DR, Griscom NT. Practical pediatric imaging: diagnostic radiology of infants and children. 3rd ed. Philadelphia: Lippincott-Raven; 1998. pp. 1009–1160. [Google Scholar]
- 2.Swischuk LE. Imaging of the newborn, infant, and young child. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 590–723. [Google Scholar]
- 3.Coley BD. Caffey's pediatric diagnostic imaging. 12th ed. Philadelphia: Saunders; 2013. p. 1243. [Google Scholar]
- 4.American College of Radiology. ACR–SPR practice parameter for the performance of voiding cystourethrography in children. [Accessed Jan 31, 2019]. Available at. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/VoidingCysto.pdf. Published 1995.
- 5.Arena S, Iacona R, Impellizzeri P, Russo T, Marseglia L, Gitto E, et al. Physiopathology of vesico-ureteral reflux. Ital J Pediatr. 2016;42:103. doi: 10.1186/s13052-016-0316-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams G, Fletcher JT, Alexander SI, Craig JC. Vesicoureteral reflux. J Am Soc Nephrol. 2008;19:847–862. doi: 10.1681/ASN.2007020245. [DOI] [PubMed] [Google Scholar]
- 7.Brereton RJ, Narayanan R, Ratnatunga C. Ureteric re-implantation in the neuropathic bladder. Br J Surg. 1987;74:1107–1110. doi: 10.1002/bjs.1800741211. [DOI] [PubMed] [Google Scholar]
- 8.Hernandez RJ, Goodsitt MM. Reduction of radiation dose in pediatric patients using pulsed fluoroscopy. AJR Am J Roentgenol. 1996;167:1247–1253. doi: 10.2214/ajr.167.5.8911190. [DOI] [PubMed] [Google Scholar]
- 9.Hernanz-Schulman M, Goske MJ, Bercha IH, Strauss KJ. Pause and pulse: ten steps that help manage radiation dose during pediatric fluoroscopy. AJR Am J Roentgenol. 2011;197:475–481. doi: 10.2214/AJR.10.6122. [DOI] [PubMed] [Google Scholar]
- 10.Lachenmyer LL, Anderson JJ, Clayton DB, Thomas JC, Pope JC, 4th, Adams MC, et al. Analysis of an intervention to reduce parental anxiety prior to voiding cystourethrogram. J Pediatr Urol. 2013;9:1223–1228. doi: 10.1016/j.jpurol.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Riccabona M. Pediatric urogenital radiology-medical radiology. Diagnostic imaging. 3rd ed. New York: Springer International Publishing; 2018. pp. 20–23. [Google Scholar]
- 12.Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. International reflux study in children. Pediatr Radiol. 1985;15:105–110. doi: 10.1007/BF02388714. [DOI] [PubMed] [Google Scholar]
- 13.Ward VL. Patient dose reduction during voiding cystourethrography. Pediatr Radiol. 2006;36 Suppl 2:168–172. doi: 10.1007/s00247-006-0213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Domina JG, Sanchez R, Meesa IR, Christodoulou E. Evaluation of pediatric VCUG at an academic children’s hospital: is the radiographic scout image necessary? Pediatr Radiol. 2015;45:855–861. doi: 10.1007/s00247-014-3241-4. [DOI] [PubMed] [Google Scholar]
- 15.Paltiel HJ, Rupich RC, Kiruluta HG. Enhanced detection of vesicoureteral reflux in infants and children with use of cyclic voiding cystourethrography. Radiology. 1992;184:753–755. doi: 10.1148/radiology.184.3.1509062. [DOI] [PubMed] [Google Scholar]
- 16.Papadopoulou F, Efremidis SC, Oiconomou A, Badouraki M, Panteleli M, Papachristou F, et al. Cyclic voiding cystourethrography: is vesicoureteral reflux missed with standard voiding cystourethrography? Eur Radiol. 2002;12:666–670. doi: 10.1007/s003300101108. [DOI] [PubMed] [Google Scholar]
- 17.Wyly JB, Lebowitz RL. Refluxing urethral ectopic ureters: recognition by the cyclic voiding cystourethrogram. AJR Am J Roentgenol. 1984;142:1263–1267. doi: 10.2214/ajr.142.6.1263. [DOI] [PubMed] [Google Scholar]
- 18.Hodson CJ, Maling TM, McManamon PJ, Lewis MG. The pathogenesis of reflux nephropathy (chronic atrophic pyelonephritis) Br J Radiol. 1975;Suppl 13:1–26. [PubMed] [Google Scholar]
- 19.Papachristou F, Printza N, Doumas A, Koliakos G. Urinary bladder volume and pressure at reflux as prognostic factors of vesicoureteral reflux outcome. Pediatr Radiol. 2004;34:556–559. doi: 10.1007/s00247-004-1211-y. [DOI] [PubMed] [Google Scholar]
- 20.Alexander SE, Arlen AM, Storm DW, Kieran K, Cooper CS. Bladder volume at onset of vesicoureteral reflux is an independent risk factor for breakthrough febrile urinary tract infection. J Urol. 2015;193:1342–1346. doi: 10.1016/j.juro.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Snyder EM, Nguyen RA, Young KJ, Coley BD. Vesicovaginal reflux mimicking obstructive hydrocolpos. J Ultrasound Med. 2007;26:1781–1784. doi: 10.7863/jum.2007.26.12.1781. [DOI] [PubMed] [Google Scholar]
- 22.Maynard P. Drawing distinctions: the varieties of graphic expression. Ithaca: Cornell University Press; 2005. p. 22. [Google Scholar]