Abstract
Objective
Approximately 225,000 children sustain injuries requiring hospitalization annually. Posttraumatic stress disorder (PTSD) and depression are prevalent among pediatric patients and caregivers post-injury. Most U.S. trauma centers do not address patients’ mental health needs. Better models of care are needed to address emotional recovery. This article describes the engagement and recovery trajectories of pediatric patients enrolled in the Trauma Resilience and Recovery Program (TRRP), a stepped-care model to accelerate emotional recovery following hospitalization.
Methods
TRRP is designed to (a) provide in-hospital education about post-injury emotional recovery and assess child and caregiver distress; (b) track mental health symptoms via a 30-day text-messaging program; (c) complete 30-day PTSD and depression phone screens; and (d) provide evidence-based treatment via telehealth or in-person services or referrals, if needed. All 154 families approached were offered TRRP services, 96% of whom agreed to enroll in TRRP. Most patients were boys (59.8%), and average age was 9.12 years [standard deviation (SD) = 5.42]. Most injuries (45.8%) were sustained from motor vehicle accidents.
Results
In hospital, 68.5% of caregivers and 78.3% of children reported clinically significant distress levels. Over 60% of families enrolled in the texting service. TRRP re-engaged 40.1% of families for the 30-day screen, 35.5% of whom reported clinically significant PTSD (M = 13.90, SD = 11.42) and/or depression (M = 13.35, SD = 11.16). Most (76%) patients with clinically significant symptomology agreed to treatment.
Conclusions
Our intervention model was feasible and increased reach to families who needed services. Efforts to improve follow-up engagement are discussed, as are initial successes in implementing this model in other pediatric trauma centers.
Keywords: accidents and injuries, computer applications/eHealth, mental health
More than 20 million children experience unintentional injuries annually, with approximately 225,000 children sustaining injuries so severe they require hospitalization (Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2012). In addition to the physical and medical burdens incurred, mental health difficulties such as posttraumatic stress disorder (PTSD) and depression are prevalent in this population post-injury, with 20–30% of pediatric traumatic injury (PTI) patients reporting mental health symptoms and/or decreased quality of life up to 1-year post-injury (De Young, Kenardy, Cobham, & Kimble, 2012; Kassam-Adams & Winston, 2004; Kassam-Adams, Bakker, Marsac, Fein, & Winston, 2015; Kassam-Adams, Marsac, Hildenbrand, & Winston, 2013; Zatzick & Grossman, 2011; Zatzick et al., 2006). Children’s untreated PTSD and depression are major risk factors for deficits in other domains, including physical recovery, social functioning, and quality of life (Bryant et al., 2010; Fakhry et al., 2017; Zatzick et al., 2007). Assessment and treatment of these difficulties are particularly important among PTI patients given their potential impacts on social, cognitive, and emotional development and academic functioning.
Caregivers are a key source of support for children following PTI, and caregivers’ own emotional health is strongly correlated with children’s outcomes (Brown, De Young, Kimble, & Kenardy, 2018; Hall et al., 2006; Young et al., 2003). Significant depressive and/or PTSD symptoms have been found in 20–40% of caregivers of children with traumatic injuries, with caregiver symptoms being inversely related to children’s emotional recovery (Kassam-Adams et al., 2015; Meiser-Stedman, Yule, Dalgleish, Smith, & Glucksman, 2006; Nugent, Ostrowski, Christopher, & Delahanty, 2007). Highly distressed caregivers may demonstrate avoidance behaviors (e.g., avoid talking to their children about the event and avoid trauma reminders) and/or reinforce children’s maladaptive coping strategies following pediatric trauma and potentially maintain children’s trauma-related symptoms (Kichline, Kassam-Adams, Weiss, Herbers, & Marsac, 2017). Thus, it is increasingly important to identify and treat mental health difficulties not only among PTI patients but also among their caregivers.
Most U.S. trauma centers do not address patients’ mental health needs after traumatic injury (Fakhry et al., 2017; Love & Zatzick, 2014), and even fewer trauma centers adequately monitor and address the mental health needs of PTI patients and their caregivers. Access to and quality of trauma care nationwide has improved over the years. However, most of this progress has occurred in trauma centers during the acute recovery phase, with reduced mortality rates in trauma centers compared to non-trauma centers (Celso et al., 2006; MacKenzie et al., 2006; Pracht et al., 2008). Still, much of the focus of trauma centers is on patients’ physical recovery, with little effort dedicated to mental health recovery despite calls to implement a trauma-informed approach in pediatric healthcare networks (Marsac et al., 2016). Better follow-up care is imperative for PTI patients, and has potential to save billions of dollars each year in medical expenses and lost productivity and vastly improve overall functioning (Graves, Rivara, & Vavilala, 2015; Zonfrillo, Spicer, Lawrence, & Miller, 2018).
In an attempt to meet this need, in September 2015 we developed and implemented the Trauma Resilience and Recovery Program (TRRP) in a Level I trauma center and state-verified pediatric trauma center in the southeastern U.S. to address mental health recovery for traumatic injury patients using a stepped model of care. Stepped models of care have the advantage of being cost-efficient because delivery of each step of care is determined by need. TRRP is rooted in cognitive behavioral principles based on evidence that injured trauma survivors may respond to cognitive behavioral therapy (CBT) with early, secondary prevention strategies demonstrating value for this population (Roberts, deRoon-Cassini, & Brasel, 2010; Rothbaum et al., 2012; Rothbaum et al., 2014; Zatzick et al., 2013; Zatzick et al., 2004). The purpose of this article is to introduce this stepped care service model and describe the engagement and short-term recovery trajectories of PTI patients enrolled in TRRP clinical services during the first 2 years of the program.
Description of TRRP Service
Step 1: Patient Recruitment, In-Hospital Education, and TRRP Enrollment
A customized electronic medical record report is generated daily from the trauma registry of a Level I trauma center in the southeastern U.S. that identifies patients who have been admitted following traumatic injury. The trauma center admits over 2,500 trauma patients annually and initiated 1,640 trauma annual activations in recent years. Hospitalized patients are approached by TRRP staff when they are medically stable, alert, and oriented. Average length of hospital stay is approximately 2–4 days. Inclusion criteria were children ages 0–17 who were admitted to the trauma center due to traumatic injury. Exclusion criteria included (a) hospital admission due to self-inflicted injuries, (b) injuries resulting from child maltreatment (due to other services already in place for such patients), and (c) patients whose medical difficulties preclude them from participation (e.g., communication or cognitive deficits) as reported by the medical trauma team in the electronic medical record. Certified medical interpreters were utilized to assist in communicating with non-English speaking patients. Patients and caregivers are approached in the trauma center by a TRRP staff member, which include bachelor’s, master’s, and predoctoral level clinicians who receive training and ongoing direct supervision by licensed clinical psychologists. Once approached, patients and their caregivers are provided brief (∼10 min) verbal education related to child and caregiver emotional and behavioral recovery following pediatric injury (e.g., common acute trauma responses in caregiver and child, potential avoidance behavior and trauma triggers, leveraging social support, value of symptom monitoring and later screening). Contact information is also gathered from interested patients and/or caregivers for a 30-day follow-up mental health screening. A 30-day time period is used to allow for patients’ natural psychological recovery and to allow them to monitor their symptoms to determine if intervention is indeed necessary after 30 days. Baseline information is gathered from patients regarding caregiver and child peritraumatic stress symptoms, as elevated peritraumatic distress is associated with increased risk for PTSD and related psychological difficulties (Gorman, Engel-Rebitzer, Ledoux, Bovin, & Marx, 2014).
Step 2: Tracking Emotional Recovery
“Watchful waiting” (i.e., symptom self-monitoring) is an evidence-based approach to monitoring emotional recovery following a stressor, and is recommended as a frontline intervention during the first 30 days following a traumatic event [e.g., National Collaborating Centre for Mental Health (UK), 2005; Post & Van Stone, 2008]. Watchful waiting provides patients with better insight into their mental health symptoms, may improve engagement in mental health follow-up, and also allows providers to track day-to-day symptom changes (Bakker, Kazantzis, Rickwood, & Rickard, 2016; Bunnell et al., 2019). The second step of our TRRP intervention model utilizes this approach through a text message service, which was initiated roughly halfway through our evaluation period (i.e., it was offered to 65 of 154 patients) as a result of an ongoing quality improvement initiative after TRRP began. Patients seen in hospital are given the option to enroll in the text message service. Enrolled patients or caregivers receive one text daily for 30 days asking them to track their or their child’s symptoms. Each text consists of 1 item drawn from a set of 10 items (6 of which were modeled after the Kessler-6;Kessler et al., 2010) that is sent on a rotating schedule, with questions addressing psychological distress, avoidance, intrusive thoughts, worry, and sleep difficulties.
Step 3: 30-Day Brief Mental Health Phone Screen
Approximately 30 days post-injury, patients (ages 6–17) and caregivers (all child ages) are contacted for a brief telephone screening (∼30 min) by trained bachelor’s and master’s level staff. Once patients are briefly re-oriented to TRRP via telephone, they are administered psychometrically validated measures assessing symptoms of child PTSD and depression (children ages 6–17 only) and caregiver distress (described below). For children below the age of 6, only caregivers complete a distress screen. Patients who screen positive for PTSD or depression advance to Step 4 of the intervention. Patients or caregivers who endorse symptoms of PTSD or depressive symptoms but do not screen positive for probable PTSD or depression are offered brief coping strategies (e.g., breathing skills, brief behavioral parent training, and emotion expression) over the phone to maintain emotional recovery. They are encouraged to contact the clinic if future services are needed.
Step 4: Comprehensive Diagnostic Assessment and Delivery of Best Practice Treatment
TRRP clinic staff offers direct services or referrals for mental health assessment and treatment to patients who screen positive for PTSD or depression at Step 3. Some families receive outside care, others receive face-to-face services through our program, and still others receive home-based telemental health services. TRRP clinicians are licensed mental health professionals (i.e., licensed professional counselors) or are master’s level and predoctoral clinical psychology interns supervised by a licensed clinical psychologist. When families receive formal mental health treatment at Step 4 that is delivered by TRRP clinicians, the most common best-practice interventions delivered to them include trauma-focused CBT (Cohen & Mannarino, 2008; Cohen, Mannarino, & Deblinger, 2012) for children and prolonged exposure (Foa, Chrestman, & Gilboa-Schechtman, 2008; Powers, et al., 2010), cognitive processing therapy (Resick, Monson, & Chard, 2007; Resick & Schnicke, 1993), and brief behavioral activation treatment for depression (Lejuez et al., 2011) for caregivers if needed. The initial assessment and treatment sessions range from 60 to 90 min depending on the treatment, and the length of treatment varies depending on the presenting problems, but typically lasts about 8–12 weeks. Treatment delivered by TRRP clinicians is delivered in-person or via telehealth depending on patient preference. Referrals are provided to established mental health service organizations within patients’ communities for many families. These referrals may occur for a variety of reasons (e.g., geographic proximity for families that prefer face-to-face services, long wait-list, family lives out of state, families are experiencing difficulties such as substance abuse and serious mental illness).
Each step of this clinical service is offered to all trauma-activated patients (excluding those who did not meet our inclusion criteria) who have been admitted to our Level I trauma center following PTI. The remaining sections describe our methodology, enrollment and treatment procedures, and the engagement and short-term recovery trajectories of PTI patients enrolled in the TRRP program.
Methods
This article provides descriptive information on engagement in TRRP clinical services and the recovery trajectory of pediatric injury patients and their caregivers enrolled in TRRP over the first 2 years of clinical operations at our state-verified pediatric trauma center. In consultation with CTSA and IRB, it was concluded that this project was not considered “research” and therefore not under the purview of the IRB, because the goal was to improve our ability to identify and address the mental health needs of high-risk pediatric patients who were previously not receiving any screening or treatment. As such, patient outcomes beyond the 30-day screen were not systematically tracked, and adverse events were not systematically tracked; however, to date no adverse events have been reported to the TRRP team. Chi-square tests of independence were conducted to examine associations between group membership (e.g., treatment acceptors and refusers) and categorical variables (e.g., race, ethnicity, and age) and independent mean T-tests were used to examine group differences on continuous variables (e.g., PTSD severity). Due to the nature of the descriptive analyses and examination of engagement, for the majority of the descriptive analyses only cases with complete data were included. For the remainder of the analyses, listwise deletion was used for missing data. All analyses were conducted using SPSS 24.0.
Procedures
Step 1: In-Hospital Education and TRRP Enrollment
TRRP staff members attempted to approach all admitted patients identified through the trauma registry. However, a number of patients were discharged before staff could visit them. When this occurred, letters were mailed to these patients to orient them to our services and inform them that they would be contacted in approximately 30 days via phone to assess their emotional recovery. In cases where families were reached in-hospital and multiple caregivers were available, families were asked to identify the primary caregiver to complete the questionnaires and enroll in follow-up services through TRRP, if interested.
Measures. The Peritraumatic Distress Inventory, Caregiver and Child Versions (PDI; Brunet et al., 2001; Guardia et al., 2013), were used to assess distress among caregivers of traumatically injured children, as well as child distress levels for children aged 6–17 years. This 13-item scale has a cutoff score of 14 (Guardia et al., 2013) used to identify clinically significant distress following traumatic injury. Past research suggests that the PDI-Caregiver and Child versions have adequate internal consistency and predictive validity (Bui et al., 2011). Cronbach’s alpha in the current patient population was 0.73 and 0.80 for the caregiver and child versions, respectively.
Step 2: Tracking Emotional Recovery
Families offered the text messaging service included some caregivers of younger children (<12 years) reporting on their child’s symptomatology. TRRP staff used clinical judgment (e.g., developmental level, caregiver distress, etc.) and discussed with TRRP staff to obtain consensus when determining whether to offer this service to families of young children. For adolescents ages 12–17, youth reported on their own symptoms if they had their own phone, or the caregiver could enroll on their behalf if they did not have their own phone. Patients who enrolled received one text per day over a period of 30 days and each message asked patients to rate the extent to which the child had experienced a particular symptom or behavior during the previous week. A total of 10 questions (see Supplementary Appendix) were administered sequentially over three, repeating 10-day blocks such that each question was administered once per 10-day block for a total of three administrations.
Measures. A total of 10 questions were administered via the text message system on a rotating basis over a 30-day period which included six questions from the Kessler-6 (K-6; Kessler et al., 2002) that assess feelings of nervousness, hopelessness, restlessness/fidgetiness, depression, worthlessness, and perceived effort burden. Four additional questions were developed for the service to assess worrying, avoidance, distress relating to reminders of their traumatic injury, and sleep quality. Each question asked patients to indicate how much of the time the child experienced the emotion/behavior during the past week by responding via a 5-point Likert scale (1 = All to 5 = None).
Steps 3 and 4: 30-Day Brief Mental Health Phone Screen and Comprehensive Diagnostic Assessment and Delivery of Best Practice Treatment
Patients were called approximately 30 days post-injury. Three attempts were made to reach the patients and caregivers via phone, and voice messages were left for those who could not be reached. If there was difficulty reaching patients after three attempts, a letter was sent requesting a phone call. All families, regardless of child age, were called at 30 days and caregivers were screened. However, only children ages six and older received PTSD and depression screens, as these measures are not validated for younger children. Whereas most of these assessment and treatment referrals were for the children who sustained the traumatic injury, a number of these referrals were also for caregivers to help with issues such as parenting following pediatric injury and/or their own distress related to their child’s injury. Children and/or caregivers who screened positive for depression and/or PTSD were offered a referral to complete a comprehensive diagnostic assessment with a TRRP clinician or were offered a treatment referral to a local community mental health center based on patient preference, presenting needs, and other factors.
Measures. The Child PTSD Symptom Scale, Child and Caregiver Versions (CPSS; Foa, Johnson, Feeny, & Treadwell, 2001), includes 26 items assessing PTSD diagnostic criteria and severity in youth ages 6–17. Generally, a clinical cutoff of 15 is used to indicate probable PTSD in children and adolescents. The CPSS-Child and Caregiver forms have both demonstrated strong psychometric properties and adequate reliability in previous work (Hawkins & Radcliffe, 2006). The Cronbach’s alphas were 0.91 and 0.92 for the child and caregiver versions, respectively. The Center for Epidemiological Studies Depression Scale for Children (CESD; Faulstich, Carey, Ruggiero, Enyart, & Gresham, 1986) is a 20-item measure assessing depression in children ages 6–17. A cutoff score of 15 suggests clinically significant depressive symptoms in youth. The CESD has been found to have good test–retest reliability, internal consistency, and concurrent validity (Faulstich et al., 1986). The CESD demonstrated adequate internal consistency (Cronbach’s α = 0.79). The Kessler 6 (Kessler et al., 2003; Kessler et al., 2010) is a well-validated and psychometrically sound (Furukawa, Kessler, Slade, & Andrews, 2003; Kessler et al., 2002; 2003) measure of psychological distress (e.g., “How much of the time today did you feel hopeless?”) that is given to caregivers to assess their own distress levels at 30 days. Scores of above 13 indicate severe psychological distress, scores between 8 and 12 indicate moderate distress, and scores under 7 represent low psychological distress (Furukawa et al., 2003; Kessler et al., 2002; 2003). The K6 demonstrated adequate internal consistency (Cronbach’s α = 0.86).
Results
Child Demographics
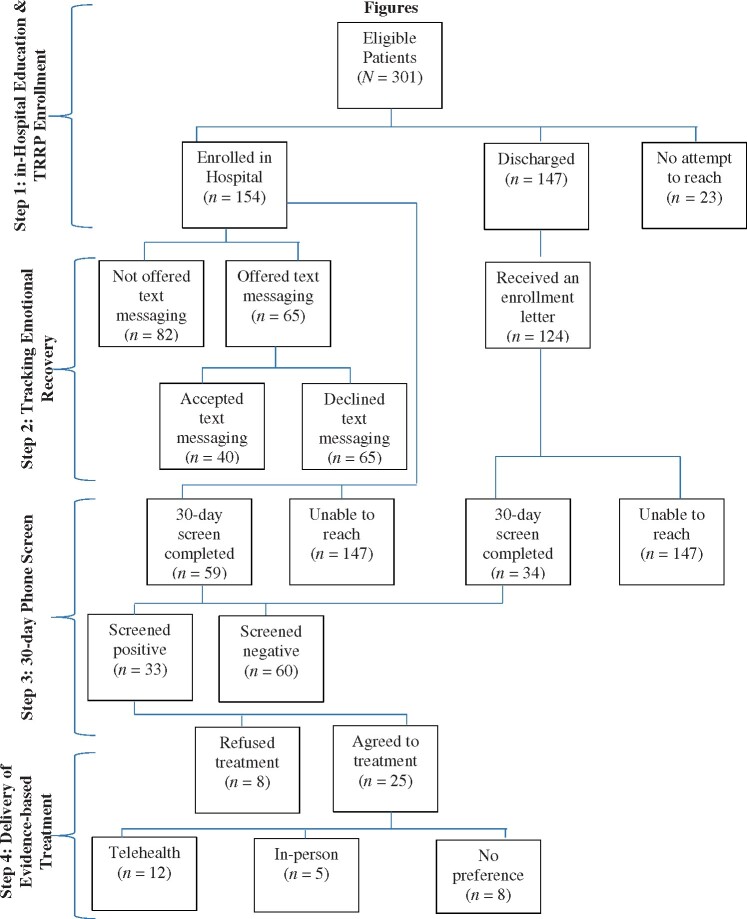
Since the launch of this program in September 2015, 301 pediatric patients were eligible for TRRP enrollment at the time of hospitalization. One-hundred and eighty patients (59.8%) were boys, and the average age was 9.12 years [standard deviation (SD) = 5.42]. Patients’ racial composition was 44.8% Black (n = 135), 41.8% White (n = 126), 10.0% biracial or “other” (n = 30), 1.7% Pacific Islander (n = 5), 1.3% Asian (n = 4), and 0.3% American Indian/Alaska Native (n = 1). The majority of patients (92.0%; n = 277) described their ethnicity as “non-Hispanic.” Most injuries were sustained from motor vehicle accidents (45.8%; n = 139), falls (10.3%; n = 31), pedestrians struck by automobiles (8.3%; n = 25) and gunshot or stab wounds (8.6%; n = 26). See Table I for patient and caregiver characteristics. See Figure 1 for patient flow through each step.
Table I.
Patient and Caregiver Characteristics
| Pediatric patients | Caregivers | |
|---|---|---|
| Variables | M (SD) | M (SD) |
| Age | 9.1 (5.42) | 37.16 (9.09) |
| Peritraumatic distress | 20.80 (10.79)a | 20.47 (9.51) |
| PTSD severity (CPSS-child/caregiver) | 13.90 (11.42)/10.46 (11.06) | — |
| Depression severity (CESD) | 13.35 (11.16) | — |
| Caregiver distress (K6) | — | 6.62 (5.68) |
| n (%) | n (%) | |
| Sex | ||
| Male | 180 (59.8) | 13 (15.5) |
| Female | 121 (40.2) | 71 (84.5) |
| Race | ||
| Black | 135 (44.8) | 40 (50.0) |
| Caucasian | 126 (41.8) | 37 (46.3) |
| Other/bi-racial | 30 (10.0) | 2 (2.5) |
| Pacific Islander | 5 (1.7) | 1 (1.2) |
| Asian | 4 (1.3) | 0 (0.0) |
| American Indian | 1 (0.3) | 0 (0.0) |
| Ethnicity | ||
| Non-Hispanic | 277 (92.0) | 73 (88.0) |
| Hispanic | 24 (8.0) | 10 (12.0) |
| Trauma type | ||
| Motor vehicle collision | 139 (45.8) | — |
| ATV/golf cart accident | 22 (7.3) | — |
| Fall | 31 (10.3) | — |
| Gunshot wound/stabbing | 26 (8.6) | — |
| Pedestrian versus auto | 25 (8.3) | — |
| Animal attack/bite | 8 (2.7) | — |
| Burn | 14 (4.7) | — |
| Assault/abuse | 1 (0.3) | — |
| Other | 35 (11.6) | — |
Note. ATV = All-Terrain Vehicle; CESD = Center for Epidemiological Studies Depression Scale for Children; CPSS = Child PTSD Symptom Scale: PDI = peritraumatic distress inventory; PTSD = posttraumatic stress disorder; SD = standard deviation.
aOnly children above the age of 6 were asked to complete the PDI (n = 46).
Figure 1.
Patient flow through the stepped-care process.
Step 1: In-Hospital Education and TRRP Enrollment
The total number of trauma activation patients identified under the age of 18 was 315, 301 of whom were eligible to be approached in the hospital between September 2015 and June 2017. The 14 ineligible patients included children who had severe brain damage as a result of their injuries or suspected child abuse patients, and would, therefore, be unable to complete the stepped-care program. Overall, 271 pediatric patients were enrolled in TRRP (90.0% of eligible patients). We approached 154 (51.2%) pediatric injury patients while in the hospital, 147 (95.5%) of whom agreed to enroll in TRRP services. An additional 147 eligible patients were discharged before we could approach them in the hospital due to limited staffing (i.e., 8 a.m.–5 p.m., Monday–Friday). Most of these patients (n = 124) were sent a letter to orient and enroll them in our services unless the patient decided to opt out of services. We did not institute the discharge letter practice until after the first 23 patients were discharged before contact.
At the time of hospitalization, primary caregivers’ average level of distress was 20.47 (median = 20.00, SD = 9.51) and children’s average level of distress was 22.80 (median = 22.00, SD = 10.79). Of the 55 caregivers who completed the PDI, 68.5% (n = 38) reported clinically significant distress (i.e., PDI > 14). Additionally, 78.3% (n = 36) children who completed the PDI reported clinically significant distress (PDI > 14).
Step 2: Tracking Emotional Recovery
The 30-day text-messaging service was offered to 65 families enrolled after June 2016 when the text-messaging service was initiated. Eighty-two families were seen prior to the initiation of this service, and, therefore, were not offered the service. Of the 65 families offered the service, 40 families enrolled (61.5%). Reasons for declining the service included loss or damage to the phone during the injury-related incident, lack of a phone with text message capabilities, and lack of interest in the service. There were no statistically significant difference between those who accepted the text-messaging service and those who did not on either caregiver peritraumatic distress [t(29) = 0.38, p = .71] or child peritraumatic distress during the in-hospital visit [t(23) = 0.41, p = .69]. There were also no significant differences between those who agreed to the service and those who did not on race [χ2(10, 299) = 10.77, p = .38], ethnicity [χ2 (4, 300) = 1.93, p = .75], sex [χ2 (2, 300) = 1.10, p = .59], age [t(59) = 1.59, p = .12], or trauma type [χ2 (20, 301) = 13.90, p = .84]. Among the families who enrolled in the service, 5 (12.5%) did not receive the service due to technical difficulties; 57% of the families that received the messages responded, whereas 43% did not. More than one-fourth (28.6%) responded to at least half of the messages. The average number of responses was 12.84 (SD = 12.07).
Step 3: 30-Day Brief Mental Health Phone Screen
Among 147 pediatric patients reached in hospital, 59 (40.1%) were re-engaged 30 days. Among the 124 pediatric patients who were discharged before we could approach them, but were sent discharge letters (n = 124), 34 (27.4%) engaged 30 days post-injury. There were no statistically significant differences in caregiver distress during Step 1 between screen completers and non-completers [t(44) = 1.07, p = .29]. Similarly, there was no significant difference in child peritraumatic distress between those who completed the screen and those who did not [t(37) = 0.65, p = .52]. There were also no significant differences between race [χ2 (5, 257) = 1.68, p = .89], ethnicity [χ2 (2, 257) = 2.12, p = .35], sex [χ2 (2, 257) = 1.03, p = .31], age [t(256) = 1.91, p = .06], and engagement in the 30-day screen. There was, however, a significant association between trauma type and 30-day engagement [χ2 (10, 258) = 18.92, p = .04], suggesting that trauma type interacts with engagement at 30 days. It appears upon a retroactive examination of the cells that gunshot victims were less likely to be re-engaged at follow-up. Additionally, of the 40 families who enrolled in the text-message program, 20 (50.0%) were re-engaged for the 30-day screen, whereas 4 of the 15 (26.7%) families who did not enroll in the text-messaging service were re-engaged at 30 days. There was a significant interaction between agreeing to the text-message service and 30-day call completion [χ2 (1, 65) = 10.37, p = .001].
Of those screened at 30 days (n = 93), 33 (35.5%) children exceeded clinical thresholds for depression and/or PTSD. Caregiver distress (clinical cutoff ≥14) was assessed at the 30-day screen, resulting in a mean of 6.62 (SD = 5.68). Child PTSD (clinical cutoff ≥15) and depression (clinical cutoff ≥15) self-report mean scores were 13.90 (SD = 11.42) and 13.35 (SD = 11.16), respectively. The mean score for caregiver report of child PTSD was 10.46 (SD = 11.06).
Step 4: Comprehensive Diagnostic Assessment and Delivery of Best Practice Treatment
Of the 33 patients who screened positive for PTSD or depression on the 30-day screen, 25 (75.8%) agreed to a more comprehensive diagnostic assessment and treatment referral. Caregiver distress was not significantly different for those who accepted or declined treatment [t(3) = −0.54, p = .63] or between child peritraumatic distress and treatment engagement [t(29) = 0.38, p = .71]. Similarly, child-reported [t(20) = −1.04, p = .31] and caregiver-reported [t(30) = −0.15, p = .88] PTSD symptomatology or child-reported depressive symptomatology [t(18) = −0.44, p = .67] was not significantly different for those who accepted or declined treatment. There were also no significant associations between race [χ2 (2, 36) = 0.80, p = .67], ethnicity [χ2 (2, 36) = 1.33, p = .51], sex [χ2 (1, 36) = 0.04, p = .85], age [t(34) = 0.41, p = .69], or trauma type [χ2 (7, 36) = 4.44, p = .73] and treatment acceptance. Among 25 patients who agreed to treatment, 12 (48.0%) preferred to receive services via telehealth, 5 (20.0%) preferred in-person services, and 8 (32.0%) either did not have a preferred treatment modality or received out-of-state referrals. Of 12 patients who preferred telehealth services, the vast majority (n = 11; 91.7%) owned their own devices (e.g., tablet, computer, and smartphone), whereas 1 (8.3%) received a clinic iPad to use for the duration of treatment.
Discussion
The purpose of this article was to present findings from PTI patients enrolled during the first 2 years in the TRRP, an innovative, interdisciplinary program targeting identification, screening, symptom tracking, follow-up assessment, and referral for evidence-based mental health services for traumatic injury patients hospitalized at a Level 1 Trauma Center. Overall, results suggested that implementation of this program is feasible, and that TRRP has increased reach to families who previously were not receiving trauma center mental health services. To date, we have provided psychoeducation to and enrolled over 95% of the PTI patients approached in the hospital. Although not all PTI patients were approached about the text messaging self-monitoring service due to age, of those approached, over 60% engaged in the service. We reached about 40% of patients at the 30-day phone screen, 35.5% of whom demonstrated positive screens for depression and/or PTSD, thereby emphasizing the unmet emotional health needs of this population. The majority of patients (75.8%) with clinically significant emotional health difficulties agreed to treatment referrals, with nearly half reporting a preference for telehealth-based options.
Despite persistent efforts to contact and re-engage families at 30 days, we were unable to reach over half of families who enrolled in TRRP at the hospital. While this is consistent with previous literature demonstrating difficulties engaging families in follow-up services (Dishion & Patterson, 1996; Gopalan et al. 2010; Mckay et al., 1998; Shaw et al., 2006), this also suggests that efforts should be directed at increasing engagement with this population. This is particularly true given the high rates of positive depression and/or PTSD screens among PTI patients (35.5%), as well as the elevated levels of distress among caregivers both in hospital (68.5% reached clinical significance) and at the 30-day telephone follow-up (33.7% reached clinical significance). In response to these attenuated engagement rates, our team is currently in the process of integrating a brief, tailored, in-hospital risk reduction session for children and caregivers reporting higher peritraumatic distress symptoms to prevent secondary trauma symptom development and to promote service engagement.
Brief interventions targeted to patients and caregivers who endorsed symptomatology, including psychoeducation, the introduction of coping strategies (e.g., relaxation), and brief exposure, may not only promote engagement in follow-up but also reduce distress and promote natural recovery. Early intervention approaches, such as the Multi-tier Approach to Psychological Intervention after Traumatic injury (Hunt, Chesney, Brasel, & deRoon-Cassini, 2018), can be adapted for PTI populations and have great potential to strengthen engagement and follow-up for families at higher risk for symptom development. Our team is working to adapt this model for our PTI population and to examine its feasibility, acceptability, and impact on engagement and outcomes.
These relatively high rates of mental health symptoms and distress levels among children and their caregivers also highlight the importance of implementing routine screening and referrals in pediatric trauma centers nationally. Across Level I and Level II trauma centers in the U.S., less than 50% of all patients are screened for suicidality, 25% for depression, and 7% for PTSD symptoms (Love & Zatzick, 2014). Failure to screen traumatic injury patients for mental health difficulties leaves up to 90% of those with post-injury PTSD or depression without adequate care to address these and related needs (Fakhry et al., 2017). Evidence-based, stepped-care emotional health services are needed in trauma centers to evaluate and support emotional difficulties among PTI patients. These approaches are cost efficient because multiple levels of intervention are delivered only to patients with unmet needs.
Furthermore, in addition to traditional barriers (e.g., stigma, cost, time commitments, and transportation), families affected by PTI experience unique challenges such as numerous competing time demands (e.g., medical appointments, physical recovery, and academic challenges) as well as mobility difficulties post-injury (Branas, 2005; Chandra et al., 2008; Fakhry et al., 2017; Wiseman, Foster, & Curtis, 2013). Home-based telehealth services have the potential to address many of these barriers (Acierno et al., 2017). TRRP attempts to reduce barriers to care for families who need it most by offering direct clinical services via telehealth modalities. This is particularly true for various racial and cultural groups who often face significant barriers to receiving mental health care (Priester et al., 2016). With over half of our current sample reporting African American or biracial race, it is critical to ensure that trauma-focused interventions like TRRP are designed to increase reach and promote engagement among different racial and cultural groups. Technology-enhanced mental health resources have great potential to mitigate these barriers and reduce access disparities through various platforms such as telemental health, technology-mediated self-help, symptom tracking, and mobile applications (Ralston, Andrews, & Hope, 2019). TRRP leverages technology at multiple steps to increase ease of access to services which may reduce health disparities.
Successful implementation of a stepped-care mental health service embedded within trauma centers requires coordinated services provided by interprofessional teams to comprehensively address patients’ needs. In our own work, partnerships between pediatric trauma surgery, mental health, and nursing have been essential for facilitating access to patients and successful program implementation. This may require ongoing education for nurses, residents, and surgeons about common emotional and behavioral health difficulties among PTI patients and their caregivers, in addition to the importance of routine screening and service referral for those who need it. This education should also include the importance of trauma-informed care (TIC) for this population to build provider competence in delivering TIC and enhancing provider knowledge regarding the potential impacts of trauma on patients, families, and staff (Bruce et al., 2018; Substance Abuse and Mental Health Services Administration, 2015). It is also important to provide assessments and referrals for caregivers of PTI patients given the potential negative impacts of caregiver distress on child emotional health recovery (Brown et al., 2018; Hall et al., 2006; Young et al., 2003). Ongoing education regarding impacts of caregiver distress on child outcomes should be embedded in interprofessional team trainings to emphasize caregivers’ important roles in traumatically injured children’s overall recovery.
Limitations
The TRRP service model provides screening and follow-up care for patients who previously did not receive any mental health services (Fakhry et al., 2017). As a novel clinical service, the model has evolved somewhat since the initiation of the program because we have made continuous efforts to better meet patient needs. This approach differs from a more protocolized, systematic evaluation of an intervention in a research study. The information presented in this manuscript is therefore limited by these changes and inconsistencies overtime, including initiation of TRRP components (e.g., discharge letters and SMS program) months after initial implementation, lack of data on treatment completion, and changes in protocol resulting in patients not being contacted for follow-up. However, these program changes may present opportunities to compare engagement outcomes across major service iterations, resulting in significant improvements to the program. An additional limitation is that we do not include data on patient satisfaction or cost-effectiveness. However, as an evolving clinical service designed to improve patient care and program scalability, our team is beginning to track these variables to better meet patients’ needs.
Future Directions
TRRP uses a stepped-care intervention model to meet patients’ needs in a cost-efficient way, guided by the evidence base and best practices in trauma care. As a result of our successful implementation of this program in our trauma center, we have partnered with three additional Level I/II trauma centers in the state to implement TRRP directly in their trauma centers. We have completed qualitative interviews with key stakeholders (e.g., trauma medical directors, program managers, social workers, and patients) to assess best strategies for implementing TRRP at each center.
We have identified a set of priorities designed to better serve our PTI population as we disseminate and implement TRRP in additional trauma centers. One major priority is the need to tailor each step of our clinical service to meet the needs of specific populations, such as rural families with reduced service access, gunshot victims who may require unique approaches to education and service engagement and treatment, and traumatically injured children under age 12 and their families, for whom most intervention elements may need to be caregiver-driven. We have taken initial steps to address the needs of pre-adolescent children by conducting semi-structured qualitative interviews with caregivers to inform plans to develop a scalable, technology-enhanced resource for caregivers of young PTI patients to better meet their needs in a way that is cost effective and acceptable to other pediatric trauma centers. We will continue focusing efforts on decreasing barriers and strengthening facilitators to TRRP implementation to bring this service to scale across the trauma system and increase awareness of its potential to provide improved follow-up care for families impacted by PTI.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Supplementary Material
Acknowledgments
The authors wish to acknowledge TRRP staff for their tireless efforts toward improving the emotional recovery of our patients.
Funding
This work was supported by funding from the Medical University of South Carolina (MUSC) Center for Telehealth and the South Carolina Telehealth Alliance.
Conflicts of interest: None declared.
Contributor Information
Leigh E Ridings, College of Nursing, Medical University of South Carolina.
Margaret T Anton, College of Nursing, Medical University of South Carolina.
Jennifer Winkelmann, College of Nursing, Medical University of South Carolina.
Tatiana M Davidson, College of Nursing, Medical University of South Carolina.
Lauren Wray, Department of Psychiatry and Behavioral Sciences, National Crime Victims Center, Medical University of South Carolina.
Christian J Streck, Department of Surgery, College of Medicine, Medical University of South Carolina.
Kenneth J Ruggiero, College of Nursing, Medical University of South Carolina.
References
- Acierno R., Knapp R., Tuerk P., Gilmore A. K., Lejuez C., Ruggiero K., Foa E. B. (2017). A non-inferiority trial of prolonged exposure for posttraumatic stress disorder: in person versus home-based telehealth. Behaviour Research and Therapy, 89, 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker D., Kazantzis, N., Rickwood, D., & Rickard, N. (2016). Mental health smartphone apps: Review and evidence-based recommendations for future developments. JMIR Mental health, 3, e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branas C. C. (2005). Access to trauma centers in the United States. Journal of the American Medical Association, 293, 2626.. [DOI] [PubMed] [Google Scholar]
- Brown E. A., De Young A., Kimble R., Kenardy J. (2018). Review of a parent's influence on pediatric procedural distress and recovery. Clinical Child and Family Psychology Review, 21, 224–245. [DOI] [PubMed] [Google Scholar]
- Bruce M. M., Kassam-Adams N., Rogers M., Anderson K. M., Sluys K. P., Richmond T. S. (2018). Trauma providers’ knowledge, views, and practice of trauma-informed care. Journal of Trauma Nursing, 25, 131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet A., Weiss D. S., Metzler T. J., Best S. R., Neylan T. C., Rogers C., Marmar C. R. (2001). The peritraumatic distress inventory: a proposed measure of PTSD criterion A2. American Journal of Psychiatry, 158, 1480–1485. [DOI] [PubMed] [Google Scholar]
- Bryant R. A., O'Donnell M. L., Creamer M., McFarlane A. C., Clark C. R., Silove D. (2010). The psychiatric sequelae of traumatic injury. American Journal of Psychiatry, 167, 312–320. [DOI] [PubMed] [Google Scholar]
- Bui E., Brunet, A., Olliac, B., Very, E., Allenou, C., Raynaud, J.-P., … & Birmes, P. (2011). Validation of the Peritraumatic Dissociative Experiences Questionnaire and Peritraumatic Distress Inventory in school-aged victims of road traffic accidents. European Psychiatry, 26(2), 108–111. [DOI] [PubMed] [Google Scholar]
- Bunnell B. E., Davidson T. M., Winkelmann J. R., Maples-Keller J. L., Ridings L. E., Dahne J., Ruggiero K. J. (2019). Implementation and utility of an automated text messaging system to facilitate symptom self-monitoring and identify risk for posttraumatic stress disorder and depression in trauma center patients. Telemedicine and e-Health. doi:10.1089/tmj.2018.0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celso B., Tepas J., Langland-Orban B., Pracht E., Papa L., Lottenberg L., Flint L. (2006). A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. Journal of Trauma-Injury Infection & Critical Care, 60, 371–378. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. (2012). National action plan for child injury prevention. Atlanta, GA: CDC, NCIPC. [Google Scholar]
- Chandra A., Marshall G. N., Shetty V., Paddock S. M., Wong E. C., Zatzick D., Yamashita D.-D. R. (2008). Barriers to seeking mental health care after treatment for orofacial injury at a large, urban medical center: concordance of patient and provider perspectives. Journal of Trauma: Injury, Infection, and Critical Care, 65, 196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A., Mannarino A. P. (2008). Trauma‐focused cognitive behavioural therapy for children and parents. Child and Adolescent Mental Health, 13, 158–162. [DOI] [PubMed] [Google Scholar]
- Cohen J. A., Mannarino A. P., Deblinger E. (Eds.). (2012). Trauma-focused CBT for children and adolescents: treatment applications. New York, NY: Guilford Press. [Google Scholar]
- De Young A. C., Kenardy J. A., Cobham V. E., Kimble R. (2012). Prevalence, comorbidity and course of trauma reactions in young burn-injured children. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 53, 56–63. [DOI] [PubMed] [Google Scholar]
- Dishion T. J., Patterson S. G. (1996). Preventive parenting with love, encouragement, and limits: the preschool years. Eugene, OR: Castalia. [Google Scholar]
- Fakhry S. M., Ferguson P. L., Olsen J. L., Haughney J. J., Resnick H. S., Ruggiero K. J. (2017). Continuing trauma: the unmet needs of trauma patients in the post-acute care setting. The American Surgeon, 83, 1308–1314. [PubMed] [Google Scholar]
- Faulstich M. E., Carey M. P., Ruggiero L., Enyart P., Gresham F. (1986). Assessment of depression in childhood and adolescence: an evaluation of the Center for Epidemiological Studies Depression Scale for Children (CES-DC). The American Journal of Psychiatry, 143, 1024–1027. [DOI] [PubMed] [Google Scholar]
- Foa E. B., Chrestman K. R., Gilboa-Schechtman E. (2008). Prolonged exposure therapy for adolescents with PTSD emotional processing of traumatic experiences, therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Foa E. B., Johnson K. M., Feeny N. C., Treadwell K. R. H. (2001). The Child PTSD Symptom Scale: a preliminary examination of its psychometric properties. Journal of Clinical Child Psychology, 30, 376–384. [DOI] [PubMed] [Google Scholar]
- Furukawa T. A., Kessler R. C., Slade T., Andrews G. (2003). The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychological Medicine, 33, 357–362. [DOI] [PubMed] [Google Scholar]
- Gopalan G., Goldstein L., Klingenstein K., Sicher C., Blake C., McKay M. M. (2010). Engaging families into child mental health treatment: updates and special considerations. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 19, 182–196. [PMC free article] [PubMed] [Google Scholar]
- Gorman K. R., Engel-Rebitzer E., Ledoux A. M., Bovin M. J., Marx B. P. (2014). Peritraumatic experience and traumatic stress. Comprehensive Guide to Post-Traumatic Stress Disorder, 1–15. https://link.springer.com/content/pdf/10.1007/978-3-319-08613-2_73-1.pdf and doi: DOI 10.1007/978-3-319-08613-2_73-1 [Google Scholar]
- Graves J. M., Rivara F. P., Vavilala M. S. (2015). Health care costs 1 year after pediatric traumatic brain injury. American Journal of Public Health, 105, e35–e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guardia D., Brunet A., Duhamel A., Ducrocq F., Demarty A.-L., Vaiva G. (2013). Prediction of trauma-related disorders: a proposed cutoff score for the peritraumatic distress inventory. The Primary Care Companion for CNS Disorders, 15, PCC.12l01406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall E., Saxe G., Stoddard F., Kaplow J., Koenen K., Chawla N., King D. (2006). Posttraumatic stress symptoms in parents of children with acute burns. Journal of Pediatric Psychology, 31, 403–412. [DOI] [PubMed] [Google Scholar]
- Hawkins S. S., Radcliffe J. (2006). Current measures of PTSD for children and adolescents. Journal of Pediatric Psychology, 31, 420–430. [DOI] [PubMed] [Google Scholar]
- Hunt J. C., Chesney S. A., Brasel K., deRoon-Cassini T. (2018). Six-month follow-up of the injured trauma survivor screen: clinical implications and future directions. Journal of Trauma and Acute Care Surgery, 85, 263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams N., Bakker A., Marsac M. L., Fein J. A., Winston F. K. (2015). Traumatic stress, depression, and recovery: child and parent responses after emergency medical care for unintentional injury. Pediatric Emergency Care, 31, 737–742. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N., Marsac M. L., Hildenbrand A., Winston F. (2013). Posttraumatic stress following pediatric injury: update on diagnosis, risk factors, and intervention. Journal of the American Medical Association Pediatrics, 167, 1158–1165. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N., Winston F. K. (2004). Predicting child PTSD: the relationship between acute stress disorder and PTSD in injured children. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 403–411. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Andrews G., Colpe L. J., Hiripi E., Mroczek D. K., Normand S.-L. T., Zaslavsky A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32, 959–976. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Barker P. R., Colpe L. J., Epstein J. F., Gfroerer J. C., Hiripi E., Zaslavsky A. M. (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60, 184–189. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Green J. G., Gruber M. J., Sampson N. A., Bromet E., Cuitan M., Zaslavsky A. M. (2010). Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. International Journal of Methods in Psychiatric Research, 19, 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kichline T., Kassam-Adams N., Weiss D., Herbers J. E., Marsac M. L. (2017). Parent peri-trauma posttraumatic stress symptoms, appraisals, and coaching of avoidance coping: a multi-method approach. Journal of Family Studies, 26, 2879–2888. [Google Scholar]
- Lejuez C. W., Hopko D. R., Acierno R., Daughters S. B., Pagoto S. L. (2011). Ten year revision of the brief behavioral activation treatment for depression: revised treatment manual. Behavior Modification, 35, 111–161. [DOI] [PubMed] [Google Scholar]
- Love J., Zatzick D. (2014). A survey of screening & intervention for comorbid alcohol, drugs, suicidality, depression & PTSD at trauma centers. Psychiatric Services (Washington, D.C.), 65, 918–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKenzie E. J., Rivara F. P., Jurkovich G. J., Nathens A. B., Frey K. P., Egleston B. L., Scharfstein D. O. (2006). A national evaluation of the effect of trauma-center care on mortality. New England Journal of Medicine, 354, 366–378. [DOI] [PubMed] [Google Scholar]
- Marsac M. L., Kassam-Adams N., Hildenbrand A. K., Nicholls E., Winston F. K., Leff S. S., Fein J. (2016). Implementing a trauma-informed approach in pediatric healthcare networks. JAMA Pediatrics, 170, 70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay M., Stoewe J., McCadam K., Gonzales J. (1998). Increasing access to child mental health services for urban children and their caregivers. Health & Social Work, 23, 9–15. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R. A., Yule W., Dalgleish T., Smith P., Glucksman E. (2006). The role of the family in child and adolescent posttraumatic stress following attendance at an emergency department. Journal of Pediatric Psychology, 31, 397–402. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Mental Health (UK). (2005). Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. Leicester, UK: Gaskell; (NICE Clinical Guidelines, No. 26). [PubMed] [Google Scholar]
- Nugent N. R., Ostrowski S., Christopher N. C., Delahanty D. L. (2007). Parental posttraumatic stress symptoms as a moderator of child’s acute biological response and subsequent posttraumatic stress symptoms in pediatric injury patients. Journal of Pediatric Psychology, 32, 309–318. [DOI] [PubMed] [Google Scholar]
- Post E. P., Van Stone W. W. (2008). Veterans Health Administration primary care-mental health integration initiative. North Carolina Medical Journal, 69, 49–52. [PubMed] [Google Scholar]
- Powers M. B., Halpern J. M., Ferenschak M. P., Gillihan S. J., Foa E. B. (2010). A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30, 635–641. [DOI] [PubMed] [Google Scholar]
- Pracht E. E., Tepas J. J., Langland-Orban B., Simpson L., Pieper P., Flint L. M. (2008). Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? Journal of Pediatric Surgery, 43, 212–221. [DOI] [PubMed] [Google Scholar]
- Priester M. A., Browne T., Iachini A., Clone S., DeHart D., Seay K. D. (2016). Treatment access barriers and disparities among individuals with co‐occurring mental health and Substance Use Disorders: an integrative literature review. Journal of Substance Abuse Treatment, 61, 47–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralston A. L., Andrews A. R. III, Hope D. A. (2019). Fulfilling the promise of mental health technology to reduce public health disparities: review and research agenda. Clinical Psychology: Science and Practice, 26, 1–14. [Google Scholar]
- Resick P. A., Monson C. M., Chard K. M. (2007). Cognitive processing therapy: veteran/military version. Washington, DC: Department of Veterans' Affairs. [Google Scholar]
- Resick P. A., Schnicke M. (1993). Cognitive processing therapy for rape victims: a treatment manual. (Vol. 4). Newbury Park, CA: Sage. [Google Scholar]
- Roberts J. C., deRoon-Cassini T. A., Brasel K. J. (2010). Posttraumatic stress disorder: a primer for trauma surgeons. Journal of Trauma, 69, 231–237. [DOI] [PubMed] [Google Scholar]
- Rothbaum B. O., Kearns M. C., Price M., Malcoun E., Davis M., Ressler K. J., Houry D. (2012). Early intervention may prevent the development of posttraumatic stress disorder; A randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry, 72, 957–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum B. O., Kearns M. C., Reiser E., Davis J. S., Kerley K. A., Rothbaum A. O., Ressler K. J. (2014). Early intervention following trauma may mitigate genetic risk for PTSD in civilians: a pilot prospective emergency department study. Journal of Clinical Psychiatry, 75, 1380–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2015). Trauma-informed approach and trauma-specific interventions. Retrieved from https://www.samhsa.gov/samhsaNewsLetter/Volume_22_Number_2/trauma_tip/.
- Shaw D. S., Dishion T. J., Supplee L., Gardner F., Arnds K. (2006). Randomized trial of a family-centered approach to the prevention of early conduct problems: 2-year effects of the family check-up in early childhood. Journal of Consulting and Clinical Psychology, 74, 1.. [DOI] [PubMed] [Google Scholar]
- Wiseman T., Foster K., Curtis K. (2013). Mental health following traumatic physical injury: an integrative literature review. Injury, 44, 1383–1390. [DOI] [PubMed] [Google Scholar]
- Young G. S., Mintzer L. L., Seacord D., Castan Eda M., Mesrkhani V., Stuber M .L. (2003). Symptoms of post traumatic stress disorder in parents of transplant recipients: incidence, severity, and related factors. Pediatrics, 111, e725–e731. [DOI] [PubMed] [Google Scholar]
- Zatzick D. F., Grossman D. C. (2011). Association between traumatic injury and psychiatric disorders and medication prescription to youths aged 10–19. Psychiatric Services, 62, 264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D. F., Grossman D. C., Russo J., Pynoos R., Berliner L., Jurkovich G., Rivara F. P. (2006). Predicting posttraumatic stress symptoms longitudinally in a representative sample of hospitalized injured adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 45, 1188–1195. [DOI] [PubMed] [Google Scholar]
- Zatzick D., Jurkovich G., Rivara F. P., Russo J., Wagner A., Wang J., Katon W. (2013). A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of Surgery, 257, 390–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D. F., Rivara F. P., Nathens A. B., Jurkovich G. J., Wang J. I. N., Fan M.-Y., Mackenzie E. J. (2007). A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychological Medicine, 37, 1469–1480. [DOI] [PubMed] [Google Scholar]
- Zatzick D., Roy-Byrne P., Russo J., Rivara F., Droesch R., Wagner A., Katon W. (2004). A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Archives of General Psychiatry, 61, 498–506. [DOI] [PubMed] [Google Scholar]
- Zonfrillo M. R., Spicer R. S., Lawrence B. A., Miller T. R. (2018). Incidence and costs of injuries to children and adults in the United States. Injury Epidemiology, 5, 37–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.