Abstract
Purpose
Vaccination toward coronavirus disease (COVID-19) has been recommended and adopted as one of the measures of reducing the spread of this novel disease worldwide. Despite this, vaccine uptake among the Ugandan population has been low with reasons surrounding this being unknown. This study aimed to investigate the factors associated with COVID-19 vaccine hesitancy in Uganda.
Methods
A cross-sectional study was conducted on a total of 1042 adults in the districts of Mukono, Kiboga, Kumi, Soroti, Gulu, Amuru, Mbarara and Sheema from June to November 2021. Data were analyzed using STATA v.15. Barriers to vaccination were analyzed descriptively, while a binary logistic regression model was used to establish the factors associated with COVID-19 vaccine hesitancy.
Results
Overall, COVID-19 vaccine hesitancy was 58.6% (611). Respondents from urban areas and those in the eastern or northern region had increased odds of vaccine hesitancy. Further, higher education level and having knowledge on how COVID-19 is transmitted significantly reduced the odds of vaccine hesitancy. The study also noted individual perception such as COVID-19 kills only people with underlying medical conditions, as well as limited awareness on vaccine types or vaccination areas as the main reasons to vaccine hesitancy. Relatedly, other misconceptions like the ability of the vaccine to cause infertility, or spreading the virus into the body, and acknowledgment of alcohol as a possible cure were other reasons for vaccine hesitancy.
Conclusion
The proportion of COVID-19 vaccine hesitancy is still high among the population with this varying across regions. This is driven by low education level and limited awareness on the vaccination as well as perceived myths and misconceptions. The study recommends mass sensitization of the population on the benefits of vaccination using various channels as well as rolling out community-based outreach vaccination campaigns across the country.
Keywords: COVID-19, vaccination, hesitancy, barriers, pandemic, Uganda
Introduction
The World Health Organization (WHO) identified vaccine hesitancy as one of the top ten threats to global health1 and this remains a challenge to many countries.2,3 Evidently, research shows that vaccination is essential in the prevention of infections, morbidity and reducing mortality for a number of existing infectious diseases.4 Undoubtedly, the COVID-19 pandemic distorted the health, social, economic wellbeing and the quality of life some of which could be averted with vaccinations.5 As one of the measures of reducing the impact of the pandemic globally, the World Health Organization recommended worldwide vaccination of populations against the novel virus. Despite all these measures, the uptake of the COVID-19 vaccine among different populations remains low with limited studies providing the possible explanations.2,3
COVID-19 vaccine hesitancy does not only exist among the common population, but also among health workers despite vaccines being available.6 COVID-19 vaccine hesitancy has been attributed to fear of adverse effects and doubts about the effectiveness of the vaccines.7,8 In addition, in low income countries, COVID-19 vaccine hesitancy has been linked to inaccessibility of vaccination health facilities, global vaccine supply chain dynamics, vaccine preference and perceived misconceptions.3,9–11 It has been documented that higher education level, adequate knowledge about COVID-19 virus and the vaccines, as well as the presence of confirmed COVID-19 infections in the neighborhood significantly reduce the likelihood COVID-19 vaccine hesitancy.7,8 Further, demographic factors such as work place, occupation, parity, age and sex/gender have also shown association with COVID-19 vaccine hesitancy.7,8,12
According to the Ministry of Health, Uganda needed a total of 45 million doses of vaccines (if all vaccines provided were of two doses) to vaccinate a population of about 22 million as well as refugees with the eligibility age of years 18 and above in a phased manner.13 By the end of March 2021, the government had received a total of 964,000 doses though its uptake was very low.13 Previous studies elsewhere have reported a significantly higher proportion of people that want to receive the vaccine given an opportunity.2,3
Given the challenges associated with vaccine hesitancy and the documented evidence of the benefits of vaccination, the development of a proper communication strategy in providing vaccine efficacy information is crucial especially in low income countries.10 In this study we aimed to examine factors associated with COVID-19 vaccine hesitancy in Uganda. Specifically, the study examined: 1) the proportion of the population that was hesitant to vaccination; and 2) the factors associated with COVID-19 vaccine hesitancy. The intended purpose was to provide information for policy guidance and implementation as the vaccines were being rolled throughout the country.
Materials and Methods
Study Design, Setting and Population
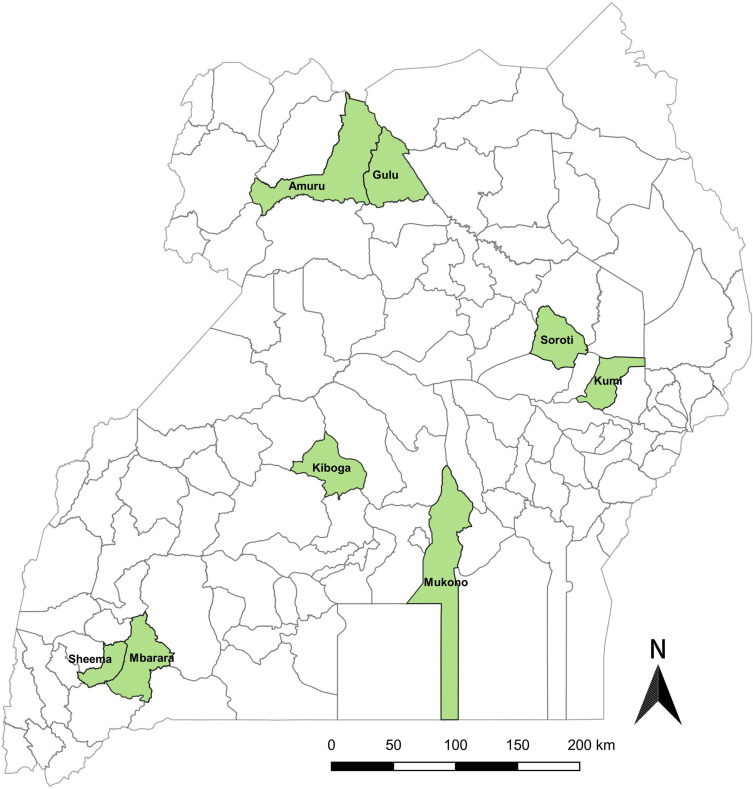
This was a quantitative population-based cross-sectional study carried out in four statistical regions of the country with a total of two districts randomly sampled from each of the regions as presented in Figure 1. The selection of districts was guided by the Ministry of Health-Uganda’s top ten and bottom ten performing districts in COVID-19 vaccine uptake rates. As vaccines were being rolled out the National Immunization Technical Advisory Group (NITAG) and Incident Management Team (IMT) tracked district-based COVID-19 vaccination rates with a ranking for all the 135 districts in the country. Specifically, the sampled districts include Mukono and Kiboga in Central, Kumi and Soroti in East, Gulu and Amuru in North while Mbarara and Sheema from West. Of these, Kiboga, Kumi, Amuru and Mbarara were among the low performing districts while Mukono, Soroti, Gulu and Sheema were ranked as high performers in the vaccine uptake.13 We employed a stratified multistage sampling followed by systematic random sampling method to obtain a representative sample of respondents. At the first stage of sampling, two sub-counties were randomly selected from the respective districts with one being in rural and the other in urban setting. This was then followed by a simple random selection of one parish from the respective sub-counties. The selected parishes acted as enumeration areas where lists of all villages in the respective parishes were used to arrive to respondents at the household level. At household level, a systematic sampling method was used basing on the sampling frame of the household lists generated at the village level.
Figure 1.
Study sites.
The sample size estimation of this study was based on the Leslie Kish’s sampling procedures for cross-sectional studies. The following formula was used:14
 |
Where: n sample size, z = confidence interval (95%),
= confidence interval (95%),  = proportion of COVID-19 uptake in the country (50%),
= proportion of COVID-19 uptake in the country (50%),  =margin of error (5%).
=margin of error (5%).
Thus, adjusting for the sampling design using a design effect of 2 and catering for non-response as well as missing values, a final size of 1042 respondents was generated. The sample size was then distributed basing on the probability proportional to size of the district as well as rural–urban residence. All adults aged 18 and above were eligible for participation in the study.
Data Collection
Data were collected with face to face interview structured questionnaire for each of the sampled households. Experienced and qualified research assistants with at least a Bachelor’s degree were recruited and trained intensively for 5 days on the methods of data collection, sampling and on each of the sections included in the questionnaire. The tool comprised sections on socio-demographic characteristics, knowledge on COVID-19, individual intention on COVID-19 vaccination, as well as concerns, perceptions, attitudes and misconceptions on COVID-19 and the vaccine. The questionnaire was prepared in English and then translated to local languages used in the selected districts (Luganda, Runyankole, Rutoro, Ateso and Acholi). The tool was then uploaded on Android tablets using Kobo collect and data collected electronically by the trained research assistants. A pretest survey was conducted within Kampala district and identified problems during the survey were corrected before the actual survey. Four regional supervisors and the principal investigator supervised the entire data collection process from June to November 2021.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki for studies on human subjects. Authors received ethical clearance from the Uganda National Council of Science and Technology with registration number SS951ES and Mildmay Uganda Research Ethics Committee (MUREC-2021-40) for this study.
Informed Consent and Confidentiality
All respondents were provided with a written summary regarding the research and contact information of the principal investigator. They were assured of the confidentiality of the information collected, and written informed consent was obtained. During the consenting process, the participants were assured of the publication of only anonymized responses or information.
Study Variables
Dependent Variable
The outcome variable for this study was COVID-19 vaccine hesitancy. A binary response question was asked to all participants on whether they were vaccinated (yes/no). All those who were vaccinated were coded 0. As a follow up, those who were not vaccinated were asked whether they would want to be vaccinated if the vaccine is available. This had two possible responses (yes/no). Participants who admitted that they do not want to be vaccinated were automatically considered to be hesitant (coded 1). In addition, those who responded that they would want to be vaccinated were further followed up by the question that required them to state their plan (urgency) to acquire the vaccine dose. This was a scaled response with very likely, likely, unlikely, very unlikely and do not know as possible options. Therefore, respondents who showed their interest to be vaccinated and yet their plan to go for this vaccine dose if made available was not known, unlikely and very unlikely were also assumed to be hesitant and thus coded 1. Those who stated otherwise were coded 0.
Independent Variables
The predictor variables were grouped into two (demographic and socioeconomic factors and COVID-19 awareness factors). Demographic and socioeconomic factors include: age (18–24, 25–34, 35–44, 45–54, 55+), region (Central, East, North, West), gender (male, female), place of residence (rural, urban), and household size (1–2, 3–4, 5+). Other variables include: education level (no education, primary, secondary, higher (tertiary and university), working status (unemployed, employed), religion (Catholic, Protestant, Muslim, Others for Pentecostal/Seventh Day Adventist) and marital status (single, cohabiting, married, separated/divorced/widow or widower). Access to media was also considered and this was measured by a question that required respondents to state the frequency on reading newspapers, listening to radio and watching television. All responses were aggregated to generate an index with three categories for this variable (no exposure, 1 of 3 sources, 2 of 3 sources, access to all sources).
COVID-19 awareness factors include: awareness on any COVID-19 vaccine (respondents were asked whether they know or heard of any COVID-19 vaccine with a binary response of yes or no).
Knowledge on the ways of transmitting COVID-19. With this, respondents were asked to identify the ways in which COVID-19 can be transmitted from one person to another. The possible options were: through droplets or aerosols (as a result of coughing, sneezing or talking) from the infected person; airborne transmission (where the virus can live in the air for up to 3 hours and later enters into the lungs); surface transmission (touching a contaminated surface and then touch the nose, mouth or eyes). This was binary in nature with yes=1 if the respondent was aware on all the three ways and no=0 if otherwise.
Statistical Analysis
All data were cleaned and analyzed using STATA version 15 statistical software. We ran descriptive statistics to summarize the characteristics of the study population. In order to determine the factors associated with COVID-19 vaccine hesitancy, bivariate binary logistic regression analyses were done and the 95% confidence level was used to determine the strength of association between the predictors and dependent variable. Variables whose p-value were less than 0.2 in bivariate level were considered for further analysis and fitted in to multivariate binary logistic regression model. A p-value <0.05 in multivariable analysis was considered as statistically significant.
Results
Table 1 presents the descriptive summary of the selected characteristics among the study participants. In the results, the average age of the study participants was 40 years while 3 in 10 (27%) were aged 25–34 years. Further, the majority of participants were female (56%), residing in rural areas (59%) and employed (86%). Of these, a great number were also from the Central region (36%) with a household size of at least five (71%). The results also show that 38% were either Catholic or Anglican, 50% were married while only 2 in 10 could access all the three forms of media (newspapers, radio and television). In relation to COVID-19, 23% of the study population had knowledge on all the ways of transmitting the virus and a large proportion (51%) was not aware on any COVID-19 vaccines. Relatedly, results also revealed that only 16% were vaccinated and more than half (59%) of the participants were hesitant to COVID-19 vaccination. In addition, out those who were not vaccinated, 15% were not willing to be vaccinated while only about 36% showed urgency for the vaccine (Table 1).
Table 1.
Distribution of the Study Population by Socioeconomic and Demographic Characteristics
| Variable | Frequency (N=1042) | Percentage (%) |
|---|---|---|
| Age | ||
| 18–24 | 168 | 16.1 |
| 25–34 | 283 | 27.2 |
| 35–44 | 229 | 22.0 |
| 45–54 | 165 | 15.8 |
| 55+ | 197 | 18.9 |
| Place of residence | ||
| Rural | 610 | 58.5 |
| Urban | 432 | 41.5 |
| Region | ||
| Central | 378 | 36.3 |
| East | 254 | 24.4 |
| North | 195 | 18.7 |
| West | 215 | 20.6 |
| Sex | ||
| Female | 580 | 55.7 |
| Male | 462 | 44.3 |
| Education level | ||
| No education | 109 | 10.5 |
| Primary | 397 | 38.1 |
| Secondary | 327 | 31.4 |
| Higher | 209 | 20.1 |
| Working status | ||
| Unemployed | 142 | 13.6 |
| Employed | 900 | 86.4 |
| Household size | ||
| 1–2 | 78 | 7.5 |
| 3–4 | 221 | 21.2 |
| 5+ | 743 | 71.3 |
| Access to media | ||
| No exposure | 114 | 10.9 |
| 1 of 3 sources | 405 | 38.9 |
| 2 of 3 sources | 299 | 28.7 |
| All sources | 224 | 21.5 |
| Religion | ||
| Catholic | 391 | 37.5 |
| Anglican | 394 | 37.8 |
| Muslim | 90 | 8.6 |
| Other | 167 | 16.0 |
| Marital status | ||
| Single | 177 | 17.0 |
| Cohabiting | 195 | 18.7 |
| Married | 522 | 50.1 |
| Separated/divorced/widowed | 148 | 14.2 |
| Knowledge on the ways of transmitting COVID-19 | ||
| No | 802 | 77.0 |
| Yes | 240 | 23.0 |
| Awareness of any COVID-19 vaccine | ||
| No | 534 | 51.2 |
| Yes | 508 | 48.8 |
| Are you currently vaccinated? | ||
| No | 878 | 84.3 |
| Yes | 164 | 15.7 |
| Would you want to be vaccinated for COVID-19? | ||
| No | 127 | 14.5 |
| Yes | 751 | 85.5 |
| What is your plan to receive the vaccine in case it is available? | ||
| Very likely | 89 | 11.8 |
| Likely | 178 | 23.7 |
| Very unlikely | 84 | 11.2 |
| Unlikely | 276 | 36.8 |
| Not sure/do not know | 124 | 16.5 |
| COVID-19 vaccine hesitancy | ||
| No | 431 | 41.4 |
| Yes | 611 | 58.6 |
Reasons for COVID-19 Refusal and Hesitancy
All participants who were hesitant in receiving the COVID-19 vaccine were asked about their reasons for refusal (Table 2). The majority of the respondents (70%) did not know of any vaccination sites in their respective districts while more than half (55%) lacked awareness on any vaccine type. Also, a bigger proportion (68%) believe that government officials should be immunized first before rolling out to the entire population. Other reasons were attributed to the myths and misconceptions about the virus and the vaccine itself. In the survey, 15% acknowledged that the vaccine could make people infertile or the vaccine could spread the virus into their bodies thus getting them infected. Relatedly, 8%, 10% and close to 1 in 5 perceived that COVID-19 is not a serious illness, that the vaccine does not work and COVID-19 kills only people with underlying medical conditions respectively. Drinking alcohol protects against COVID-19 (31%) and eating garlic as a cure for COVID-19 (41%) were also prominent reasons for refusal or vaccination hesitancy.
Table 2.
Reasons for Vaccination Refusal or Hesitancy (N=611)
| Reason | True (%) | False (%) |
|---|---|---|
| Knows any vaccination place in the district | 186 (30.4) | 425 (69.6) |
| Does not know any COVID-19 vaccine | 336 (55.0) | 275 (45.0) |
| COVID-19 vaccine will not work | 63 (10.3) | 548 (89.7) |
| COVID-19 vaccine will make people infertile | 92 (15.1) | 519 (84.9) |
| Government officials should be immunized first | 418 (68.4) | 193 (31.6) |
| COVID-19 vaccine will spread COVID-19 virus into my body | 89 (14.6) | 522 (85.4) |
| COVID-19 is not a serious illness | 51 (8.3) | 560 (91.7) |
| Drinking alcohol protects against COVID-19 | 181 (31.3) | 420 (68.7) |
| Swallowing antibiotics cures COVID-19 | 94 (15.4) | 517 (84.6) |
| Eating garlic cures COVID-19 | 251 (41.1) | 360 (58.9) |
| COVID-19 kills only people with underlying medical conditions | 93 (15.2) | 518 (84.8) |
Factors Associated with COVID-19 Vaccine Hesitancy
The unadjusted results in Table 3 indicate that the following factors were significantly associated with increased odds of having vaccine hesitancy: western region, household size of five or more, being separated/divorced/widowed and having an awareness on the vaccine. On the other hand, odds ratio of COVID-19 vaccine hesitancy reduced as: education level increased, access to more sources of information, as well as having knowledge on the ways of transmitting the virus. Relatedly, participants living in urban setting, those from the eastern and northern region as well as male sex were less likely to be hesitant. Respondent’s age, working status and religion were dropped in the final model (multivariate analysis) because of their high p-values (p-value>0.2).
Table 3.
Multivariate Analysis of COVID-19 Vaccination Hesitancy and the Selected Variables
| Variable | cOR [95% CI] | aOR [95% CI] |
|---|---|---|
| Age | ||
| 18–24 | Ref | |
| 25–34 | 1.06 [0.72,1.56] | |
| 35–44 | 0.86 [0.57,1.28] | |
| 45–54 | 0.95 [0.61,1.46] | |
| 55+ | 1.24 [0.81,1.89] | |
| Place of residence | ||
| Rural | Ref | |
| Urban | 0.53 [0.41,0.68]*** | 0.74 [0.55,0.99]* |
| Region | ||
| Central | Ref | |
| East | 0.71 [0.51,0.97]* | 0.66 [0.46,0.95]* |
| North | 0.68 [0.48,0.96]* | 0.55 [0.35,0.83]** |
| West | 1.82 [1.26,2.62]** | 1.63 [1.07,2.43]* |
| Sex | ||
| Female | Ref | |
| Male | 0.62 [0.48,0.79]*** | 0.77 [0.58,1.02] |
| Education level | ||
| No education | Ref | |
| Primary | 0.57 [0.35,0.93]* | 0.72 [0.42,1.22] |
| Secondary | 0.36 [0.22,0.59]*** | 0.64 [0.36,1.11] |
| Higher | 0.21 [0.13,0.36]*** | 0.50 [0.27,0.93]* |
| Working status | ||
| Unemployed | Ref | |
| Employed | 0.91 [0.63,1.31] | |
| Household size | ||
| 1–2 | Ref | |
| 3–4 | 1.67 [1.00,2.82] | 1.18 [0.66,2.12] |
| 5+ | 1.62 [1.01,2.58]* | 1.26 [0.74,2.15] |
| Access to media | ||
| No exposure | Ref | |
| 1 of 3 sources | 1.22 [0.79,1.87] | 1.37 [0.84,2.21] |
| 2 of 3 sources | 0.87 [0.56,1.36] | 0.95 [0.56,1.64] |
| All sources | 0.51 [0.32,0.80]** | 0.80 [0.44,1.45] |
| Religion | ||
| Catholic | Ref | |
| Anglican | 1.21 [0.75, 1.94] | |
| Muslim | 1.01 [0.76, 1.35] | |
| Other | 0.84 [0.58, 1.21] | |
| Marital status | ||
| Single | Ref | |
| Cohabiting | 1.16 [0.77,1.75] | 1.17 [0.75,1.84] |
| Married | 1.12 [0.80,1.58] | 1.08 [0.74,1.59] |
| Separated/divorced/widowed | 1.99 [1.26,3.16]** | 1.34 [0.80,2.23] |
| Knowledge on the ways of transmitting COVID-19 | ||
| No | Ref | |
| Yes | 0.38 [0.28,0.51]*** | 0.47 [0.34,0.64]*** |
| Awareness on any COVID-19 vaccine | ||
| No | Ref | |
| Yes | 1.84 [1.43,2.36]*** | 1.35 [1.01,1.80] |
Notes: Ref is a Reference category; cOR is the crude/unadjusted odds ratio; aOR is the adjusted odds ratio, 95% CI is the confidence interval, *p<0.05, **p<0.01, ***p<0.001.
After adjusting and controlling for possible confounders, results in Table 3 show that people in the urban areas were less likely to experience vaccine hesitancy compared to their counterparts in the rural areas (AOR=0.74, 95% CI=0.55–0.99). Findings also showed that individuals from the eastern (AOR=0.66, 95% CI=0.46–0.95) or northern region (AOR=0.55, 95% CI=0.35–0.83) had reduced odds of vaccine hesitancy while their counterparts in the west experienced the reverse (AOR=1.63, 95% CI=1.07–2.43). Additionally, individuals with higher education level (AOR=0.50, 95% CI=0.27–0.93) and those having knowledge on the ways of transmitting the virus (AOR=0.47, 95% CI=0.34–0.64) were less likely to have COVID-19 vaccine hesitancy.
Discussion
We conducted a study on COVID-19 vaccine hesitancy and its associated factors among 1042 individuals across the four main regions of the country. Of these, 58.6% were reported to be hesitant implying a lower acceptance rate which is in contrast to findings in other countries.3–10 The study also found substantial regional and residential variations in the COVID-19 vaccination hesitancy among the population.12,15 Findings show that people in urban areas were less likely to experience vaccination hesitancy compared to their counterparts in the rural areas which correlates with previous studies elsewhere.12 The reason for this could be that access to information and vaccination points is limited among rural people which could partly explain their low uptake.
We also found out that individuals from the eastern or northern region were less likely to be hesitant toward COVID-19 vaccine compared to those in other regions. This regional variation within a country has also been reported in different countries elsewhere.15 The possible reason could be that information on COVID-19 vaccine had been rolled out in the eastern and northern regions and therefore misconception on the vaccine was low.
In accordance with other studies on COVID-19 vaccination hesitancy12,15–17 individuals with higher education level were less likely to be hesitant toward the vaccine as compared to their counterparts with low education levels. Educated people are likely to have access to information from all different avenues and therefore are able to make informed decisions compared to those who are not able to read and write. Secondly, education demystifies misconceptions and cultural practices.
Still, having knowledge on the ways of transmitting the virus was significantly associated with lower COVID-9 vaccination hesitancy, which was in line with other findings.14,17 Schwarzinger et al revealed that having had an experience with COVID-19 such as symptoms or knowing someone with COVID-19 partly prompts more people to take up the vaccination.15 People who are knowledgeable are empowered in making informed choices compared to those who do not and this could partly explain this finding.
According to the reasons for vaccine refusal and hesitancy reported by the participants, three quarters did not know of any vaccination place in their respective districts while more than half lacked awareness on any vaccine type. Relatedly, many of the respondents were waiting for government officials to be immunized. It was also shown that people believe in swallowing antibiotics or garlic as one of the measures of curing COVID-19, while others believed in drinking alcohol. Still, a significant proportion also have misconceptions that the vaccine can spread the virus in the body, that the virus kills only people with underlying conditions or the vaccine makes people infertile. Others also had doubts on the existence of the virus and the safety of the vaccine itself. Some of these similar reasons of rejecting the vaccine have also been presented in previous studies elsewhere.6,8,17,18,19,20
Strength and Limitation
The cross-sectional nature that cannot permit the establishment of causality. Also, the time the survey was done, there could have been limited information about the different types of COVID-19 vaccines and vaccination locations. Therefore, people’s vaccination intentions might have changed over time with new information on the vaccines. Nevertheless, this being one of the first few studies that involved physical interaction with the population regarding COVID-19 vaccination truly reflects the factors associated with COVID-19 vaccine hesitancy and the reasons for refusal in Uganda.
Conclusion
The proportion of COVID-19 vaccination hesitancy is still high among the population. Region, place of residence, education level and knowledge about the virus were associated with vaccine hesitancy. The reasons for refusal were attributed to: limited awareness on the vaccination centres and the vaccine brands as well as myths and conceptions on both the virus and the vaccines. The study recommends, mass sensitization of the population on the benefits of vaccination using various channels as well as rolling out community-based outreach vaccination campaigns across the country.
Acknowledgments
This study was funded by the Government of Uganda through the special COVID-19 funding to the Research and Innovations Fund (RIF) of Makerere University. We are grateful to Ministry of Health, Uganda, all study participants, the District Health Officers, field guides, district health teams, district and local council leaders, team leaders and the research assistants.
Funding Statement
This study was funded by the Government of Uganda through the special COVID-19 funding to the Research and Innovations Fund (RIF) of Makerere University. The funder had no role in the design of the study, data collection, analysis, interpretation of data and in writing of the manuscript.
Disclosure
Evelyne B Nyachwo reports grants from Government of Uganda through Makerere University Research and Innovations Fund, during the conduct of the study. Juliet Nabirye reports grants from Government of Uganda, during the conduct of the study. Leonard K Atuhaire reports grants from Uganda Government, during the conduct of the study. The authors declare no other potential conflicts of interest in relation to this work.
References
- 1.World Health Organization. Ten threats to global health in 2019; 2019. Available from: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. Accessed 4 Mar 2022.
- 2.Williams L, Gallant AJ, Rasmussen S, et al. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020;25:1039–1054. doi: 10.1111/bjhp.12468 [DOI] [PubMed] [Google Scholar]
- 3.Sherman SM, Smith LE, Sim J, et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021;17:1612–1621. doi: 10.1080/21645515.2020.1846397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alqudeimat Y, Alenezi D, AlHajri B, et al. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. 2021;30:262–271. doi: 10.1159/000514636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9:1–14. doi: 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-elimat T, Abualsamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021;18:e0250555. doi: 10.1371/journal.pone.0250555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gbeasor-Komlanvi F, Afanvi K, Konu Y, et al. Prevalence and factors associated with COVID-19 vaccine hesitancy in health professionals in Togo, 2021. Public Heal Pract. 2020;2:1–6. doi: 10.1016/j.puhip.2021.100220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saied SM, Saied EM, Kabbash IA, Islam OK, Hossain MA. Vaccine hesitancy: beliefs and barriers associated with COVID‐19 vaccination among Egyptian medical students. J Med Virol. 2021;93:1–12. doi: 10.1002/jmv.26910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noushad M, Al-Awar MS, Al-Saqqaf IS, Nassani MZ, Alrubaiee GG, Rastam S. Lack of access to COVID-19 vaccines could be a greater threat than vaccine hesitancy in low-income and conflict nations: the case of Yemen. Clin Infect Dis. 2022;ciac088. doi: 10.1093/cid/ciac088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karlsson LC, Soveri A, Lewandowsky S, et al. Fearing the disease or the vaccine: the case of COVID-19. Pers Individ Dif. 2021;172:110590. doi: 10.1016/j.paid.2020.110590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin C, Tu P, Beitsch LM. Confidence and receptivity for covid‐19 vaccines: a rapid systematic review. Vaccines. 2021;9:1–32. doi: 10.3390/vaccines9010016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Ayyadhi N, Ramadan MM, Al-Tayar E, Al-Mathkouri R, Al-Awadhi S. Determinants of hesitancy towards COVID-19 vaccines in State of Kuwait: an exploratory internet-based survey. Risk Manag Healthc Policy. 2021;14:4967–4981. doi: 10.2147/RMHP.S338520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministry of Health. Corona virus Pandemic. Available from: https://www.health.go.ug/covid/. Accessed 10 May 2022.
- 14.Harapan H, Wagner AL, Yufika A, Winardi W, Sofyan H, Mudatsir M. Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Heal. 2020;8:1–8. doi: 10.3389/fpubh.2020.00381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kish L. Survey Sampling. New York: Chichester: Wiley; 1965. [Google Scholar]
- 16.Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: beliefs and barriers associated with COVID‐19 vaccination among Egyptian medical students. J Med Virol. 2021;93:4280–4291. doi: 10.1002/jmv.26910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malik AA, Mcfadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Heal. 2021;6:210–221. doi: 10.1016/S2468-2667(21)00012-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bajos N, Spire A, Silberzan L. The social specificities of hostility toward vaccination against Covid-19 in France. PLoS One. 2022;17:e0262192. doi: 10.1371/journal.pone.0262192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paudel S, Palaian S, Shankar PR, Subedi N. Risk perception and hesitancy toward COVID-19 vaccination among healthcare workers and staff at a medical college in Nepal. Risk Manag Healthc Policy. 2021;14:2253–2261. doi: 10.2147/RMHP.S310289 [DOI] [PMC free article] [PubMed] [Google Scholar]