Abstract
Background
During the first year of the COVID-19 pandemic, workers in essential sectors had higher rates of SARS-CoV-2 infection and COVID-19 mortality than those in non-essential sectors. It is unknown whether disparities in pandemic-related mortality across occupational sectors have continued to occur during the periods of SARS-CoV-2 variants and vaccine availability.
Methods
In this longitudinal cohort study, we obtained data from the California Department of Public Health on all deaths occurring in the state of California, USA, from Jan 1, 2016, to Dec 31, 2021. We restricted our analysis to residents of California who were aged 18–65 years at time of death and died of natural causes. We classified the occupational sector into nine essential sectors; non-essential; or unemployed or without an occupation provided on the death certificate. We calculated the number of COVID-19 deaths in total and per capita that occurred in each occupational sector. Separately, using autoregressive integrated moving average models, we estimated total, per-capita, and relative excess natural-cause mortality by week between March 1, 2020, and Nov 30, 2021, stratifying by occupational sector. We additionally stratified analyses of occupational risk into counties with high versus low vaccine uptake, categorising high-uptake regions as counties where at least 50% of the population were fully vaccinated according to US guidelines by Aug 1, 2021.
Findings
From March 1, 2020, to Nov 30, 2021, 24 799 COVID-19 deaths were reported in residents of California aged 18–65 years and an estimated 28 751 (95% prediction interval 27 853–29 653) excess deaths. People working in essential sectors were associated with higher COVID-19 deaths and excess deaths than were those working in non-essential sectors, with the highest per-capita COVID-19 mortality in the agriculture (131·8 per 100 000 people), transportation or logistics (107·1 per 100 000), manufacturing (103·3 per 100 000), facilities (101·1 per 100 000), and emergency (87·8 per 100 000) sectors. Disparities were wider during periods of increased infections, including during the Nov 29, 2020, to Feb 27, 2021, surge in infections, which was driven by the delta variant (B.1.617.2) and occurred during vaccine uptake. During the June 27 to Nov 27, 2021 surge, emergency workers had higher COVID-19 mortality (113·7 per 100 000) than workers from any other sector. Workers in essential sectors had the highest COVID-19 mortality in counties with low vaccination uptake, a difference that was more pronounced during the period of the delta infection surge during Nov 29, 2020, to Feb 27, 2021.
Interpretation
Workers in essential sectors have continued to bear the brunt of high COVID-19 and excess mortality throughout the pandemic, particularly in the agriculture, emergency, manufacturing, facilities, and transportation or logistics sectors. This high death toll has continued during periods of vaccine availability and the delta surge. In an ongoing pandemic without widespread vaccine coverage and with anticipated threats of new variants, the USA must actively adopt policies to more adequately protect workers in essential sectors.
Funding
US National Institute on Aging, Swiss National Science Foundation, and US National Institute on Drug Abuse.
Introduction
Individuals working in essential occupations (ie, in sectors deemed essential to local or regional functions and exempt from public health stay-at-home orders or other restrictions to in-person work during the COVID-19 pandemic) have had a higher risk of SARS-CoV-2 infection and COVID-19 mortality than those working in non-essential sectors.1, 2, 3, 4 An analysis of data from the UK Biobank project found higher risk of severe COVID-19 disease among workers in essential sectors than among workers in non-essential sectors.2 Another study using data from the American Community Survey (ACS) linked to mortality records from the Social Security Administration found that people without work-from-home options had higher mortality during 2020 than those working in occupations that had the option to work from home.5 Although much of the attention to occupational risks has focused on health-care workers, growing evidence on occupational disparities in COVID-19 mortality suggests that particular workers in essential sectors who are not in health care, such as transportation workers, had the highest risk of COVID-19 death in 2020.6, 7 It is unknown whether such disparities have continued to occur during the period of SARS-CoV-2 variants and vaccine availability.
Research in context.
Evidence before this study
Research on occupational sector disparities in COVID-19 mortality has been limited by data availability. We searched PubMed from March 1, 2020, to June 15, 2022, using the search terms “COVID-19” AND “mortality” AND “occupation”. This search yielded 474 results, which included 103 publications with substantive relevance to occupational sector disparities in COVID-19 mortality, the majority of which were focused on COVID-19 risks among health-care workers. A small number (23 studies) focused on occupational disparities in COVID-19 mortality for other essential and non-essential workers; however, only 15 of these studies measured both occupation or sector and COVID-19 infection or mortality at the individual level. The sparse available evidence that uses individual data highlights the vulnerability of older workers and suggests that COVID-19 mortality risk reflects occupational stratification, with workers in lower socioeconomic positions and migrant workers at greatest risk of death. In all studies, occupations were grouped into broad categories based on industry or sector, front-line or essential status, or risk of exposure, and then compared or modelled as a covariate. Only one study included data covering the period since widespread vaccine availability and none of the studies examined change in occupational disparities from more than one timepoint during the pandemic. Whether occupation shapes COVID-19 mortality, and how to reduce mortality disparities between workers, are not known.
Added value of this study
Our study considers disparities across occupational groups in SARS-CoV-2 mortality during the dominance of the delta (B.1.617.2) SARS-CoV-2 variant and during vaccine availability. We found high per-capita COVID-19 mortality in the agriculture, transportation or logistics, facilities, emergency, and manufacturing sectors. Disparities were wider during periods with a high rate of COVID-19 mortality, including during the dominance of the delta variant and during vaccine uptake. Among essential workers, per-capita COVID-19 mortality was higher among residents in regions with low vaccine uptake regions than among those in regions with high vaccine uptake, particularly during the June 27, 2021, to Nov 27, 2021 surge in infections.
Implications of all the available evidence
Our study is consistent with a growing body of research suggesting that workers in essential sectors face higher risks for SARS-CoV-2 infection and death than other workers. This study suggests that vaccine uptake has helped reduce these risks among essential workers; however, the levels of uptake have been insufficient to erase disparities. Increased protection of essential workers should involve increased vaccine uptake and other measures, including policies such as sick leave and workplace protections (eg, masks and ventilation).
We previously reported on COVID-19 and excess mortality by occupation in California, USA, from March 7 (the start of the pandemic) to Nov 28, 2020.1 We found that people in essential sectors had an increased risk of COVID-19 and excess mortality during this period compared with those in non-essential sectors.1 We also found that people working in four essential sectors—namely, food and agriculture, manufacturing, transportation and logistics, and facilities—had particularly high excess mortality. Three major contextual changes have occurred since this study was published. First, there have been surges in COVID-19 cases and deaths, led by SARS-CoV-2 variants, from December, 2020, to April, 2021, and from August to December, 2021. Second, SARS-CoV-2 vaccines became available from Dec 14, 2020, in California with prioritisation for workers in essential sectors in many jurisdictions. In California, health-care workers were immediately prioritised for vaccination, followed by workers in other essential sectors, including food and agriculture. Third, California became less reliant on shelter-in-place restrictions—aside from a restriction from Dec 3, 2020, to Jan 25, 2021, there were no other shelter-in-place restrictions in the state in 2021. It is unclear whether disparities in COVID-19 and excess mortality have persisted throughout these changes.
The objective of this study is to examine whether disparities in excess mortality and COVID-19 mortality across occupational sectors have persisted in the face of major contextual changes to the pandemic and the pandemic response and to explore whether disparities differ by regional vaccine uptake. We add three major updates to the previous study.1 We extended the time window of interest through to Nov 27, 2021, in which an increased amount of SARS-CoV-2 variants were found and vaccines became available. We additionally disaggregated data for two essential sectors that we had previously combined (health and emergency, and food and agriculture). In this Article, we note that different policies and behaviours between sectors—such as between health workers and emergency workers (first responders)—might have translated to differences in risk. We also report on differences in COVID-19 mortality between regions with low or high vaccination uptake.
Methods
Study design and participants
In this longitudinal cohort study, we obtained data from the California Department of Public Health, Sacramento, CA, USA, on deaths occurring in the state from Jan 1, 2016, to Dec 31, 2021. We restricted our analyses to residents of California who were aged 18–65 years (inclusive of endpoints) at the time of death and who died of natural causes. We only included participants with natural-cause deaths so that our estimates of excess mortality would more plausibly identify unrecognised or unrecorded COVID-19 deaths.
Our use of the death data was approved by the State of California Committee for the Protection of Human Subjects.
Procedures
We identified recorded COVID-19 deaths by searching through all 20 cause-of-death variables available to us, defining a COVID-19 death as any occurrence of the code U07 of the International Classification of Diseases (tenth version). Reporting of COVID-19 deaths has been a source of controversy because people who had a suspected COVID-19 death had not been consistently tested for COVID-19. Therefore, under-reporting of COVID-19 mortality was a concern, particularly in low-socioeconomic areas and areas with more Black residents.8
Data on occupation were recorded on death certificates via free-text responses. We converted these free-text data to US Census codes using the US National Institute for Occupational Safety and Health's Industry & Occupation Computerized Coding System. A team of three researchers (Y-HC, KAD, and ARR) then categorised each unique code into one of 11 occupational sectors: agriculture, emergency services, facilities, government or community, health, manufacturing, restaurant, retail, transportation or logistics, not essential, and unemployed or missing data (this category includes homemakers, retirees, and students). The codes were initially categorised by one researcher (Y-HC); the codes were then divided among the three researchers who all audited the initial categorisations. Our choice of sectors was guided by the 13 sectors identified by California officials as comprising the state's essential workforce.9 We classified three sectors from the California list as not essential: defence, communications or information technology, and financial services. We de-emphasised the defence sector because, under the California definition, it includes occupations that overlap with non-essential sectors (eg, communications and information technology), and we de-emphasised communications or information technology and financial services because they were less likely to involve on-site work during the pandemic than the other sectors. Some occupations within an essential sector did not necessarily involve on-site work during the pandemic; we did not consider this to be misclassification in that our use of the term essential was consistent with California's definition and is always used to refer to sectors. We combined individuals with missing occupation data and individuals who were unemployed because it was difficult to differentiate between the groups via free-text response. For example, if a next of kin indicated that the occupation was unknown, it was possible that the decedent might have been, or not been, in employment. We reasoned that the small proportion of decedents with an unknown status were unlikely to meaningfully affect the results of the combined missing data or unemployed group, or any other occupational group.
Outcomes
The primary outcomes were excess natural-cause deaths and COVID-19 deaths. A sensitivity analysis was done on the definition of high and low vaccine uptake regions.
Statistical analysis
Our time period of interest was March 1, 2020, to Nov 30, 2021. In time-stratified analysis, we divided the time window into four phases: March 1 to Nov 28, 2020 (phase 1); Nov 29, 2020, to Feb 27, 2021 (phase 2); Feb 28 to June 26, 2021 (phase 3); and June 27 to Nov 27, 2021 (phase 4). Vaccines became available to health workers in California near the beginning of phase 2, whereas vaccines became available to emergency workers and workers in other essential sectors near the beginning of phase 3.10 Phase 2 and phase 4 correspond to surges in COVID-19 cases and deaths.
In the secondary analysis, we stratified by California counties with low or high vaccine uptake among working-age individuals, using data from the US Centers for Disease Control and Prevention.11 We defined counties with low vaccination as counties with less than 50% of the population fully vaccinated according to US guidelines by Aug 1, 2021. High vaccine uptake counties were defined as counties with 50% or more uptake of full vaccination by Aug 1, 2021.
In a sensitivity analysis, we employed an alternative cutoff point that would improve the consistency of the low and high vaccine uptake definition over time. For the cutoff of the sensitivity analysis, we defined counties with a high uptake of vaccination as the 15 counties with the highest uptake on Aug 1, 2021, Low-uptake counties were defined as those not in the top 15 of vaccine uptake on Aug 1, 2021. Because differences between occupational sectors could be affected by differences in age and sex, we also did a sensitivity analysis with age-stratified (18–35 years, 36–55 years, and 56–65 years) and sex-stratified (male or female) data.
For each group of interest: we calculated the number of COVID-19 deaths occurring in total and per capita—that is, divided by the estimated population size of the group—in each week, over the entire time window, and in each phase; we obtained subgroup-specific population estimates, for the per-capita numbers, from the 2019 ACS, which was a large, randomised sample of US addresses administered by the US Census Bureau; and we fitted dynamic harmonic regression models with autoregressive integrated moving average errors for the number of deaths per week,12 using deaths occurring in the group between Jan 3, 2016, and Feb 29, 2020 (ie, before the surge of COVID-19 cases). Using the resulting model, we forecasted the number of deaths for each unit of time, along with corresponding 95% prediction intervals. To obtain the total number of excess deaths for the entire time window and during each phase, we subtracted the total number of expected deaths from the total number of observed deaths. We obtained a 95% prediction interval for the total by simulating the model 10 000 times, selecting the 97·5% and 2·5% quantiles, and subtracting from the total number of observed deaths.
In addition to the estimated number of excess deaths (calculated as the observed number of deaths minus expected number of deaths), we calculated and report excess deaths per capita. Excess deaths per capita was calculated with the observed number of deaths minus the expected number of deaths, divided by the estimated population size. We calculated relative excess mortality as the observed number of deaths divided by the expected number of deaths. A relative excess mortality ratio of 1·5 would indicate that there were 50% more deaths observed during the pandemic than we would have expected had the pandemic not occurred. Per-capita excess mortality can be interpreted as a risk difference for mortality, whereas relative excess can be interpreted as a risk ratio for mortality. In both cases, the comparison is between the pandemic and non-occurrence of the pandemic (the reference group is non-occurrence of the pandemic).
Our reported deaths per-capita data are annualised, obtained by dividing the per-capita measure by the number of weeks and multiplying by 52. We did all analyses in R (version 4.1.3).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
There were 342 625 deaths reported among individuals who were residents in California between Jan 3, 2016, and Nov 27, 2021. Between March 1, 2020, and Nov 27, 2021, there were 24 799 COVID-19 deaths reported among people aged 18–65 years who were residents in California and an estimated 28 751 (95% prediction interval 27 853–29 653) excess deaths (table 1 ). We focus on our findings on COVID-19 deaths and view the estimates of excess mortality as sensitivity checks of the COVID-19 deaths, particularly given discrepancies between COVID-19 mortality and estimated excess mortality early in the pandemic, which we believe to be primarily due to unrecognised or unreported COVID-19 deaths.
Table 1.
Excess natural-cause mortality among individuals aged 18–65 years who are residents in California, by occupational sector, March 1, 2020, to Nov 27, 2021
|
Deaths from COVID-19 |
Excess deaths |
|||||
|---|---|---|---|---|---|---|
| Population size* | Total deaths | Deaths per 100 000 people | Total (95% prediction interval) | Per capita† (95% prediction interval) | Relative (95% prediction interval) | |
| Entire state | 25 220 309 | 24 799 | 56·2 | 28 751 (27 853–29 653) | 65·1 (63·1–67·2) | 1·31 (1·30–1·33) |
| Agriculture | 438 722 | 1012 | 131·8 | 1223 (1148–1298) | 159·3 (149·6–169·1) | 1·61 (1·55–1·67) |
| Emergency services | 419 799 | 645 | 87·8 | 756 (667–845) | 102·9 (90·7–115·0) | 1·40 (1·33–1·47) |
| Facilities | 2 557 851 | 4527 | 101·1 | 5487 (5147–5826) | 122·6 (115·0–130·2) | 1·37 (1·34–1·40) |
| Government or community | 2 312 880 | 1592 | 39·3 | 1917 (1680–2151) | 47·4 (41·5–53·1) | 1·29 (1·24–1·33) |
| Health | 1 604 590 | 1065 | 37·9 | 1003 (864–1141) | 35·7 (30·8–40·6) | 1·21 (1·18–1·25) |
| Manufacturing | 1 156 113 | 2089 | 103·3 | 1954 (1816–2091) | 96·6 (89·8–103·4) | 1·37 (1·33–1·40) |
| Restaurant | 1 447 496 | 1344 | 53·1 | 1882 (1639 to 2121) | 74·3 (64·7 to 83·7) | 1·46 (1·38 to 1·55) |
| Retail | 1 582 935 | 1262 | 45·6 | 1443 (1302–1583) | 52·1 (47·0–57·1) | 1·28 (1·25–1·32) |
| Transportation or logistics | 1 803 861 | 3381 | 107·1 | 4160 (3963–4356) | 131·8 (125·5–138·0) | 1·45 (1·42–1·48) |
| Not essential | 7 804 074 | 3761 | 27·5 | 3702 (2243–5128) | 27·1 (16·4–37·5) | 1·17 (1·10–1·26) |
| Unemployed or missing data | 4 091 988 | 4121 | 57·5 | 4876 (4602–5150) | 68·1 (64·3–71·9) | 1·29 (1·27–1·31) |
Estimated population size.
Data annualised.
Across occupational groups, workers in the agriculture, transportation or logistics, manufacturing, facilities, and emergency sectors had the highest per-capita COVID-19 mortality, per-capita excess mortality, and relative excess mortality. Among agriculture workers, there were 131·8 reported COVID-19 deaths per 100 000 people and an estimated 159·3 (95% prediction interval 149·6–169·1) excess deaths per 100 000 people; the relative excess mortality among agriculture workers was 1·61 (1·55–1·67). Workers in non-essential sectors had the lowest per-capita COVID-19 mortality (27·5 deaths per 100 000), per-capita excess mortality (27·1 [16·4 to 37·5] deaths per 100 000), and relative excess mortality (1·17 [1·10–1·26] deaths per 100 000).
We classified 27 counties as having a high vaccine uptake and 23 counties as having a low vaccine uptake. Although our definition was somewhat arbitrary, differentiation between the high-uptake and low-uptake counties was fairly consistent for 95 continuous days. The appendix (p 1) shows vaccine uptake in each of the 50 counties included in the analysis. At the end of the study period, the median vaccine uptake was 73·0% (range 60·4–89·0%) in high-uptake counties and 56·6% (range 31·6–66·8%) in low-uptake counties.
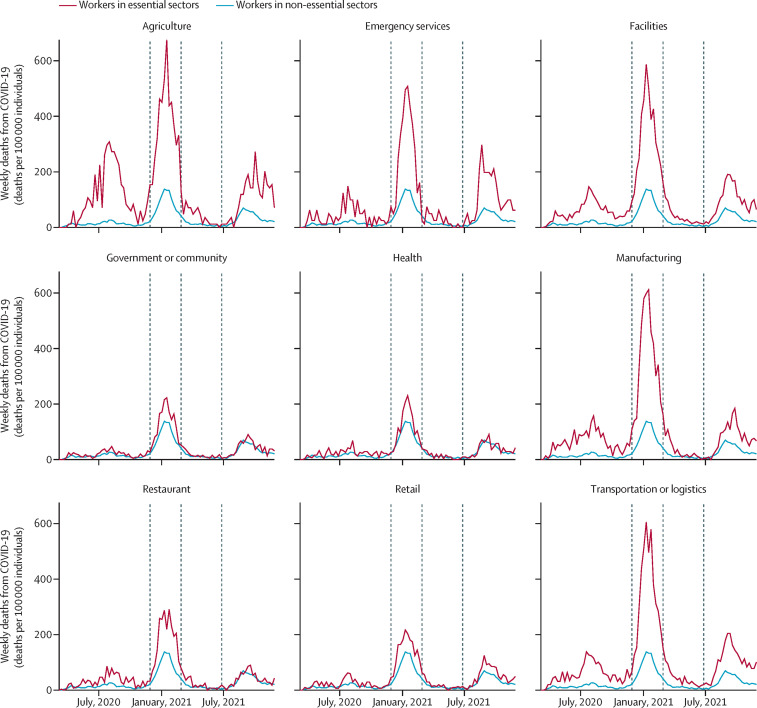
Per-capita COVID-19 mortality varied over time, peaking in phase 2 (from Nov 29, 2020, to Feb 27, 2021) and in phase 4 (June 27 to Nov 27, 2021; figure 1 ). Across time, there were disparities in per-person COVID-19 mortality between workers in essential sectors and workers in non-essential sectors; these persisted across the four phases of the analysis. The differences were particularly large when comparing workers in non-essential sectors to workers in the agriculture, emergency, facilities, manufacturing, and transportation or logistics sectors.
Figure 1.
Per-capita COVID-19 mortality among individuals aged 18–65 years living in California, by occupational sector
Data from March 1, 2020, to Nov 27, 2021. Data are annualised. Dashed vertical lines differentiate the four phases of the analysis. Phase 2 and phase 4 correspond to surges in COVID-19 cases and deaths.
During the Nov 29, 2020, to Feb 27, 2021 surge in deaths (phase 2), per-capita COVID-19 mortality was highest among workers in the agriculture (373·8 deaths per 100 000 people), manufacturing (367·8 deaths per 100 000), transportation or logistics (350·8 deaths per 100 000), facilities (330·9 deaths per 100 000), and emergency services (269·7 deaths per 100 000 people) sectors (table 2 ). These sectors all had reduced per-capita COVID-19 mortality during phase 4. Absolute disparities in per-capita COVID-19 mortality between workers in essential sectors and workers in non-essential sectors increased during a period of time when vaccines were available, during the June 27 to Nov 27, 2021 surge (phase 4). For example, the absolute disparity between transportation or logistics workers and workers in non-essential sectors was 29·6 deaths per 100 000 people during phase 3 and 71·8 deaths per 100 000 people during phase 4. Similarly, between phase 3 and phase 4, the absolute disparity between agriculture workers and workers in non-essential sectors increased from 26·7 deaths per 100 000 people to 77·9 deaths per 100 000 people.
Table 2.
Deaths from COVID-19 per 100 000 among individuals aged 18–65 years who are residents in California, by occupational sector and phase, March 1, 2020, to Nov 27, 2021
|
Phase 1 |
Phase 2 |
Phase 3 |
Phase 4 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deaths from COVID-19 per 100 000 people | Rank | Risk difference* | Deaths from COVID-19 per 100 000 people | Rank | Risk difference* | Deaths from COVID-19 per 100 000 people | Rank | Risk difference* | Deaths from COVID-19 per 100 000 people | Rank | Risk difference* | |
| Entire state | 29·9 | .. | .. | 182·9 | .. | .. | 20·1 | .. | .. | 55·8 | .. | .. |
| Agriculture | 103·6 | 1 | 91·5 | 373·8 | 1 | 288·7 | 37·6 | 2 | 26·7 | 111·5 | 2 | 77·9 |
| Emergency services | 40·0 | 5 | 27·9 | 269·7 | 5 | 184·5 | 24·8 | 5 | 13·8 | 113·7 | 1 | 80·1 |
| Facilities | 55·6 | 4 | 43·4 | 330·9 | 4 | 245·8 | 36·0 | 3 | 25·1 | 96·5 | 4 | 62·9 |
| Government or community | 18·1 | 10 | 5·9 | 130·9 | 9 | 45·8 | 15·5 | 9 | 4·5 | 41·3 | 8 | 7·7 |
| Health | 21·9 | 8 | 9·7 | 119·9 | 10 | 34·8 | 12·2 | 10 | 1·3 | 37·9 | 10 | 4·3 |
| Manufacturing | 61·4 | 2 | 49·2 | 367·8 | 2 | 282·6 | 29·6 | 4 | 18·7 | 78·1 | 5 | 44·5 |
| Restaurant | 30·2 | 7 | 18·0 | 186·5 | 7 | 101·4 | 20·1 | 7 | 9·1 | 40·2 | 9 | 6·6 |
| Retail | 21·6 | 9 | 9·4 | 143·8 | 8 | 58·6 | 16·4 | 8 | 5·5 | 52·6 | 7 | 19·0 |
| Transportation or logistics | 55·9 | 3 | 43·7 | 350·8 | 3 | 265·7 | 40·5 | 1 | 29·6 | 105·3 | 3 | 71·8 |
| Not essential | 12·2 | 11 | Ref | 85·1 | 11 | Ref | 10·9 | 11 | Ref | 33·6 | 11 | Ref |
| Unemployed or missing data | 31·3 | 6 | 19·1 | 189·2 | 6 | 104·1 | 20·6 | 6 | 9·7 | 54·8 | 6 | 21·2 |
Data are annualised. Rank indicates the rank of the per-capita COVID-19 mortality from highest to lowest. Phase 1: March 1 to Nov 28, 2020; phase 2: Nov 29, 2020, to Feb 27, 2021; phase 3: Feb 28 to June 26, 2021; and phase 4: June 27 to Nov 27, 2021.
The difference in deaths from COVID-19 per 100 000 relative to workers in non-essential sectors.
On a relative scale, disparities between workers in essential sectors and workers in non-essential sectors generally decreased over time. For example, over the four phases of our analysis, COVID-19 relative excess mortality among workers in the manufacturing sector was 5·04, 4·32, 2·71, and 2·33 times that among workers in non-essential sectors in phase 1, phase 2, phase 3, and phase 4, respectively (data not shown). This decline was not observed among emergency workers: the relative disparity in per-capita COVID-19 mortality between emergency sectors and workers in non-essential sectors was 3·29 in phase 1, 3·17 in phase 2, 2·27 in phase 3, and 3·39 in phase 4. There were also increases in the relative disparity in per-capita COVID-19 mortality between emergency services workers and health workers; this discrepancy was 1·83 in phase 1, 2·25 in phase 2, 2·03 in phase 3, and 3·00 in phase 4. Emergency services emerged during phase 4 as the sector with the highest per-capita COVID-19 mortality (113·7 per 100 000 people).
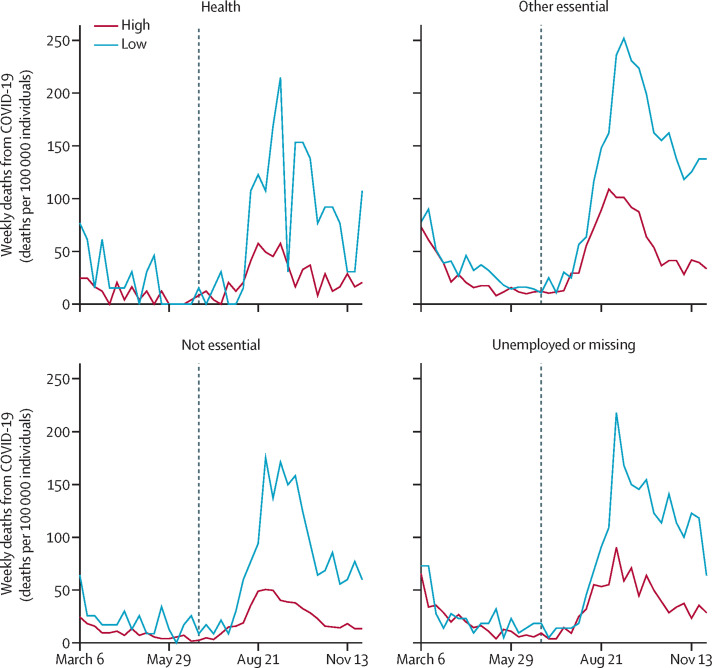
Among the counties included in the vaccine-stratified analysis, 4409 (58·0%) of the total 7592 COVID-19 deaths were in high-uptake counties (after vaccines became available) and 3183 (42·0%) of COVID-19 deaths were in low-uptake counties. Per-capita COVID-19 mortality was 30·0 per 100 000 people in high-uptake counties and 75·0 per 100 000 people in low-uptake counties. In phase 3, per-capita COVID-19 mortality was similar between counties that subsequently had low and high vaccine uptake, regardless of the occupational sector (figure 2 ). However, COVID-19 mortality in low and high vaccination regions diverged during the surge in phase 4. Among workers in essential sectors other than health workers, the difference in annualised per-capita COVID-19 mortality between high-uptake and low-uptake regions was 9·6 per 100 000 people in phase 3 and 78·8 per 100 000 individuals in phase 4. In sensitivity analyses of our definition of low-uptake and high-uptake vaccine regions, we obtained similar results to the vaccine-stratified analysis, with no meaningful differences (appendix p 3). Although this dichotomy involved a poorer balance between the two groups (as measured via the number of counties represented and geographical representation) than in the main analysis, it prioritised consistency of the definition and higher uptake. For example, the sensitivity analysis excluded several counties from the high-uptake group that did not reach 65% uptake by Nov 30, 2021: Nevada (60·4% uptake), El Dorado (62·0% uptake), San Diego (62·2% uptake), and Humboldt (63·1% uptake). The sensitivity analysis definition also excluded several counties from the high-uptake group that did not reach 50% uptake until July 12, 2021, or later: Fresno (July 12, 2021), Nevada (July 21, 2021), Colusa (July 21, 2021), and San Diego (July 27, 2021). All of the counties in the high-uptake group under the sensitivity analysis reached 50% uptake by May 28, 2021.
Figure 2.
Per-capita COVID-19 mortality among individuals aged 18–65 years living in California, by occupational sector and regions of low or high vaccine uptake, March 6 to Nov 27, 2021
Data are annualised. The vertical dashed line distinguishes phase 3 from phase 4.
In the sensitivity analysis stratified by age group or by sex, we found higher per-capita COVID-19 mortality among workers in essential sectors than among workers in non-essential sectors. For example, among individuals aged 18–35 years, annualised per-capita COVID-19 mortality was highest among workers in the emergency (15·4 per 100 000 individuals), transportation or logistics (13·0 per 100 000), and manufacturing (11·4 per 100 000) sectors, and lowest among workers in non-essential sectors (3·6 per 100 000). Similarly, among individuals aged 56–65 years, per-capita COVID-19 mortality was highest among workers in the agriculture (468·1 per 100 000), transportation or logistics (330·4 per 100 000), and manufacturing (327·3 per 100 000) sectors, and lowest among workers in non-essential sectors (85·2 per 100 000). Among female workers, per-capita COVID-19 mortality was highest in the agriculture (60·4 per 100 000), manufacturing (54·2 per 100 000), and emergency (48·1 per 100 000) sectors, and lowest in non-essential sectors (21·3 per 100 000). Among male workers, per-capita COVID-19 mortality was highest in the agriculture (168·4 per 100 000), manufacturing (124·7 per 100 000), and transportation or logistics (123·4 per 100 000) sectors, and lowest in non-essential sectors (34·1 per 100 000). The full results by sex are provided in the appendix (p 4).
Discussion
This comprehensive analysis of COVID-19 and excess mortality by occupational sector in California from March 1, 2020, to Nov 27, 2021, yields three important sets of findings. First, despite vaccine prioritisation for workers in essential sectors, these workers continued to have high COVID-19 mortality during the period of widely available vaccines (March 6 to Nov 27, 2021) and absolute disparities between workers in essential sectors and workers in non-essential sectors increased within the vaccine era during phase 4. Second, relative disparities in COVID-19 mortality between workers in essential sectors and workers in non-essential sectors have mostly declined over time. However, relative disparities between the emergency sector and workers in non-essential sectors increased when vaccines became available and the emergency sector was the essential sector with the highest per-capita COVID-19 mortality. Among workers in essential sectors, per-capita COVID-19 mortality was higher among residents in low-vaccine uptake counties than those in high-uptake regions, particularly during phase 4.
In this study, per-capita COVID-19 mortality was 2·2 times higher among emergency workers than among health workers during phase 2; this mortality ratio grew to 3·0 during phase 4. Although other explanations are possible (eg, differences in mask wearing), we hypothesise that this widened disparity between emergency and health workers during March 6 to Nov 27, 2021, partly reflects the low levels of vaccine uptake among emergency workers and high levels of vaccine uptake among health workers. In Los Angeles, the state's most populous city, 52% of police officers and 51% of firefighters had received at least one vaccine dose by June 19, 2021.13 In comparison, 77% of health workers across 350 state hospitals had received at least one vaccine dose by July 23, 2021; vaccine mandates are believed to be a contributing factor to the high uptake.14 Our study suggests that vaccination might be particularly crucial for preventing deaths during surge periods. During the June 27 to Nov 27, 2021 surge, the peak per-capita COVID-19 mortality among workers in essential non-health sectors was 251·6 per 100 000 individuals in low-uptake regions and 108·6 per 100 000 individuals in high-uptake regions, corresponding to a relative disparity of 2·3.
Protecting workers whose jobs are essential to crucial functions and infrastructure should be a priority in the pandemic response. However, deaths among workers in essential sectors were still high in our study. Several essential sectors have consistently ranked high in per-capita COVID-19 mortality, including during vaccine availability. These sectors include agriculture, transportation or logistics, facilities, and manufacturing. Although vaccine prioritisation for workers in essential sectors has been effective in prolonging lives (as suggested in our analysis stratifying by regions of low of high vaccine uptake) and might help explain the declines in relative disparities, additional efforts to improve vaccine coverage need to be made. Efforts to increase vaccine uptake among workforces via mandates have been perceived as effective,15, 16 but have faced legal challenges. For example, the US Supreme Court has ruled against the Occupational Safety and Health Administration's emergency temporary standard to require vaccination or testing in workplace settings with at least 100 employees (regardless of the occupational sector).17, 18 In Los Angeles, groups of police officers and firefighters have filed lawsuits in opposition to the city's vaccine mandate.19
In the absence of a national mandate, the USA will have to rely on other strategies. These strategies might include local or private vaccine mandates, such as the vaccine mandates at Tyson Foods and United Airlines.15, 20 Community-based or employer-sponsored21 vaccination efforts can address barriers to vaccine access (eg, transportation and misinformation).22, 23 For example, a coordinated effort, involving the faith community and a mobile clinic, appears to have been effective in improving access and uptake among Black people in San Bernardino County.24 Policies to increase vaccine uptake can and should address the unique challenges and risks that individuals with low income had during the COVID-19 pandemic,25 including job security, financial burdens of health care, and disruptions to schooling. For example, paid sick leave can ensure that workers in essential sectors do not have to choose between financial benefits and health risks.26 Finally, protections against SARS-CoV-2 transmission in workplace settings remain crucial. Given that SARS-CoV-2 can be transmitted via aerosols,27, 28 we urge for free provision of masks, preferably N95 masks or similarly effective masks,29, 30 to workers in essential sectors and improved ventilation in workplace settings.31
We acknowledge the limitations of the study. For example, there was possible misclassification of occupation on death certificates by next of kin or the text-to-code system and assignment of occupation codes to sectors was challenging in some cases. An individual classified as having occupation code 5520 (dispatchers) could have been classified as working in emergency services or transportation or logistics sectors. In early work,1 we attempted to refine our assignment of occupation codes, allowing individuals with the same occupation code to be assigned to different sectors; we found that this had no discernible impact on the study findings and ultimately abandoned this approach under the principle of methodological parsimony. There were also limitations to our use of the ACS's estimates of population size. The ACS defines residence as current residence rather than usual residence, meaning that migrant workers are included if they are residents at the time of the survey.32 We also acknowledge that the disparities in COVID-19 mortality in our analysis are not necessarily entirely due to on-the-job risk. However, given the time workers spend in workplaces and the documented weaknesses in COVID-19 protections and various outbreaks in workplaces, these disparities were probably a major contributing factor. Other factors are certainly relevant in understanding the disparities identified in this study. These factors include sex, race, ethnicity (and racism), education, comorbidities, crowded housing, use of public transportation, and health-care access. Our sensitivity analysis stratified by sex showed a larger per-capita COVID-19 mortality among male individuals than among female individuals. This disparity was particularly high among essential sectors and might reflect sex-based sorting of occupation and heterogeneity within sectors. Similarly, Black and Latino people are over-represented among low-wage workers,33 and low-wage workers also have a higher prevalence of comorbidities than other workers,34 which are well documented to increase the risk of adverse COVID-19 outcomes.35 Furthermore, low-wage workers are more likely to live in crowded housing36 and might be reluctant to take sick leave. Although these factors are important, disparities across occupational sectors persisted in previous work, in which we stratified by race and ethnicity;1 similarly, in the present study, we continued to observe such disparities in our stratifications by sex and age. Many possible interventions for protecting workers in essential sectors can be pragmatically applied by targeting workers in essential sectors. For example, a worker in an essential sector who becomes infected with SARS-CoV-2 outside of the workplace can be protected via paid sick leave, since this policy can afford the worker time to rest and seek treatment (and, of course, can help prevent workplace transmission). Finally, we acknowledge natural differences across regions with low or high vaccine uptake. These differences include urbanicity, sex, race and ethnicity, educational attainment, and occupation (even within sector). For example, according to the ACS, White individuals make up 65·5% of the population in counties with low vaccine uptake and 57·3% of the population in counties with high vaccine uptake.37 Such variation might contribute to differences observed in the region-stratified analyses.
More than 1 year after we first reported disparities in COVID-19 mortality across occupational sectors,1 and even after widespread availability of vaccination, these disparities continue to occur. The patterns are clear: although there have been a large number of COVID-19 deaths among workers in non-essential sectors, workers in essential sectors continue to have the most COVID-19 deaths. However, not all workers in essential sectors have the same increased risk. Health sector workers had lower risk of COVID-19 mortality and excess mortality than workers in several non-health sectors (agriculture, emergency, facilities, manufacturing, and transportation and logistics) both before and after vaccine availability, despite frequent contact with others in many cases. These differences suggest that increased occupational risk of COVID-19 death might not only depend on social contact, but also on workplace safety, worker protections, and worker empowerment (ie, power to negotiate). Furthermore, even in counties with high vaccination rates, essential sectors have increased risks of COVID-19 mortality and excess mortality, suggesting that vaccine uptake alone has been insufficient to erase documented disparities in COVID-19 mortality. We urge for decisive and collaborative action, using a diverse toolkit—including employer mandates for vaccination, paid sick leave, and improved ventilation in workplace settings—to reduce and eliminate disparities across occupational groups.
Data sharing
The data are available via application to the California Department of Public Health.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
RC was supported by the US National Institute on Aging (4K00AG068431–02). HEA was supported by an early postdoctoral mobility fellowship by the Swiss National Science Foundation. MVK was supported by the US National Institute on Drug Abuse (R00DA051534).
Acknowledgments
Contributors
ARR and Y-HC did the literature search. Y-HC, ARR, KAD, ACS, MMG, and KB-D designed the study. Y-HC analysed data, created the figures, and wrote the original draft. All authors contributed to interpretation, investigation, and writing (review and editing). Y-HC and RC accessed and verified the underlying data used in the study.
Supplementary Material
References
- 1.Chen Y-H, Glymour M, Riley A, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through November 2020. PLoS One. 2021;16 doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mutambudzi M, Niedwiedz C, Macdonald EB, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med. 2020;78:307–314. doi: 10.1136/oemed-2020-106731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porto ED, Naticchioni P, Scrutinio V. Lockdown, essential sectors, and COVID-19: lessons from Italy. J Health Econ. 2022;81 doi: 10.1016/j.jhealeco.2021.102572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao A, Ma H, Moloney G, et al. A disproportionate epidemic: COVID-19 cases and deaths among essential workers in Toronto, Canada. Ann Epidemiol. 2021;63:63–67. doi: 10.1016/j.annepidem.2021.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller S, Wherry LR, Mazumder B. Estimated mortality increases during the COVID-19 pandemic by socioeconomic status, race, and ethnicity. Health Aff (Millwood) 2021;40:1252–1260. doi: 10.1377/hlthaff.2021.00414. [DOI] [PubMed] [Google Scholar]
- 6.Nafilyan V, Pawelek P, Ayoubkhani D, et al. Occupation and COVID-19 mortality in England: a national linked data study of 14.3 million adults. Occup Environ Med. 2022;79:433–441. doi: 10.1136/oemed-2021-107818. [DOI] [PubMed] [Google Scholar]
- 7.Elimian KO, Ochu CL, Ebhodaghe B, et al. Patient characteristics associated with COVID-19 positivity and fatality in Nigeria: retrospective cohort study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-044079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stokes AC, Lundberg DJ, Bor J, Bibbins-Domingo K. Excess deaths during the COVID-19 pandemic: implications for US death investigation systems. Am J Public Health. 2021;111:S53–S54. doi: 10.2105/AJPH.2021.306331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.State of California Essential workforce. https://covid19.ca.gov/essential-workforce/
- 10.Wigglesworth A, King L, Megerian CLA. L.A. County teachers, some essential workers eligible for vaccine starting Monday. Feb 28, 2021. https://www.latimes.com/california/story/2021-02-28/essential-workers-teachers-and-others-will-be-eligible-for-vaccine-beginning-monday
- 11.US Centers for Disease Control and Prevention COVID-19 vaccinations in the United States, county. https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-County/8xkx-amqh
- 12.Hyndman RJ, Athanasopoulos G. 2nd edn. OTexts; Melbourne, VIC: 2018. Forecasting: principles and practice. [Google Scholar]
- 13.Rector K, Winton R, Smith D, Welsh B. Many LA cops and firefighters aren't vaccinated against COVID-19. Is this a public safety threat? June 19, 2021. https://www.latimes.com/california/story/2021-06-19/vaccination-rates-lag-among-california-public-safety-workers-drawing-concern
- 14.Ostrov BF. California first in nation to mandate vaccinations for health care workers. CalMatters. Aug 5, 2021. https://calmatters.org/health/coronavirus/2021/08/california-healthcare-vaccinations-mandate/
- 15.Hirsch L, Corkery M. How Tyson Foods got 60,500 workers to get the coronavirus vaccine quickly. Nov 4, 2021. https://www.nytimes.com/2021/11/04/business/tyson-vaccine-mandate.html
- 16.Korte L. Vaccine mandates are working in California. Here's what the numbers show. Oct 3, 2021. https://www.sacbee.com/news/politics-government/capitol-alert/article254645122.html
- 17.Abbasi J, Rubin R, Suran M. How the Supreme Court's COVID-19 vaccine mandate rulings could shape the pandemic's next phase. JAMA. 2022;327:706–708. doi: 10.1001/jama.2022.0791. [DOI] [PubMed] [Google Scholar]
- 18.Gostin LO, Parmet WE, Rosenbaum S. The US Supreme Court's rulings on large business and health care worker vaccine mandates. JAMA. 2022;327:713–714. doi: 10.1001/jama.2022.0852. [DOI] [PubMed] [Google Scholar]
- 19.Smith D. Firefighters sue over city of LA's vaccine mandate. Sept 17, 2021. https://www.latimes.com/california/story/2021-09-17/firefighters-sue-over-city-of-la-vaccine-mandate
- 20.Durbin DA. Biden administration withdraws COVID vaccine-or-test rule for large companies. Jan 25, 2022. https://www.latimes.com/world-nation/story/2022-01-25/biden-administration-officially-withdraws-vaccine-rule
- 21.State of California Employer vaccination toolkit. https://saferatwork.covid19.ca.gov/employer-vaccination-toolkit/
- 22.Carson SL, Casillas A, Castellon-Lopez Y, et al. COVID-19 vaccine decision-making factors in racial and ethnic minority communities in Los Angeles, California. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.27582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kricorian K, Turner K. COVID-19 vaccine acceptance and beliefs among Black and Hispanic Americans. PLoS One. 2021;16 doi: 10.1371/journal.pone.0256122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abdul-Mutakabbir JC, Casey S, Jews V, et al. A three-tiered approach to address barriers to COVID-19 vaccine delivery in the Black community. Lancet Glob Health. 2021;9:e749–e750. doi: 10.1016/S2214-109X(21)00099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59:137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Green T, Venkataramani AS. Trade-offs and policy options—using insights from economics to inform public health policy. N Engl J Med. 2022;386:405–408. doi: 10.1056/NEJMp2104360. [DOI] [PubMed] [Google Scholar]
- 27.Prather KA, Wang CC, Schooley RT. Reducing transmission of SARS-CoV-2. Science. 2020;368:1422–1424. doi: 10.1126/science.abc6197. [DOI] [PubMed] [Google Scholar]
- 28.Wang CC, Prather KA, Sznitman J, et al. Airborne transmission of respiratory viruses. Science. 2021;373 doi: 10.1126/science.abd9149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ueki H, Furusawa Y, Iwatsuki-Horimoto K, et al. Effectiveness of face masks in preventing airborne transmission of SARS-CoV-2. mSphere. 2020;5:e00637. doi: 10.1128/mSphere.00637-20. 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andrejko KL, Pry JM, Myers JF, et al. Effectiveness of face mask or respirator use in indoor public settings for prevention of SARS-CoV-2 infection—California, February–December 2021. MMWR Morb Mortal Wkly Rep. 2022;71:212–216. doi: 10.15585/mmwr.mm7106e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.California Department of Public Health Interim guidance for ventilation, filtration, and air quality in indoor environments. Oct 7, 2021. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/Interim-Guidance-for-Ventilation-Filtration-and-Air-Quality-in-Indoor-Environments.aspx
- 32.US Census Bureau A compass for understanding and using American community survey data: what general data users need to know. October 2008. https://www.census.gov/content/dam/Census/library/publications/2008/acs/ACSGeneralHandbook.pdf
- 33.University of California Berkeley Center for Labor Research and Education Low-wage work in California data explorer. https://laborcenter.berkeley.edu/low-wage-work-in-california
- 34.Harris JR, Huang Y, Hannon PA, Williams B. Low-socioeconomic status workers: their health risks and how to reach them. J Occup Environ Med. 2011;53:132–138. doi: 10.1097/JOM.0b013e3182045f2c. [DOI] [PubMed] [Google Scholar]
- 35.Ejaz H, Alsrhani A, Zafar A, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health. 2020;13:1833–1839. doi: 10.1016/j.jiph.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ortiz-Prado E, Simbaña-Rivera K, Barreno LG, et al. Epidemiological, socio-demographic and clinical features of the early phase of the COVID-19 epidemic in Ecuador. PLoS Negl Trop Dis. 2021;15 doi: 10.1371/journal.pntd.0008958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Census Bureau 2019 American Community Survey single-year estimates. https://www.census.gov/newsroom/press-kits/2020/acs-1year.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are available via application to the California Department of Public Health.