China faces a substantial burdensome pandemic of obesity. Recent data from the Chinese Centre for Disease Control and Prevention suggested that over an estimated 8.1% of Chinese adults (85 million Chinese adults) had obesity in 2018, which was three times the level in 2004.[1]
To understand the trends of overweight and obesity in China, we accessed the country/territory-level year-specific data of age-standardized summary exposure value (SEV, standing for the pooled proportion among the population), deaths, and disability-adjusted life of years (DALYs) for high body mass index (BMI, high BMI was defined as the BMI level higher than theoretical minimum risk exposure level [25 kg/m2]) and its associated diseases for 204 countries/territories between 1990 and 2019 using data from the Global Burden of Disease Collaborative Network.[2] Previous literature described detailed methods for the data synthesis.[3,4] Using the country/territory-level data by year, we calculated the estimated annual percentage changes (EAPCs) with 95% uncertainty intervals (UI) to estimate the annual changing patterns of age-standardized SEV, death, and DALY rates among 204 countries/territories. To compare statistics from China and other regions, we calculated the corresponding estimates from regions including global, North Africa and Middle East, Sub-Saharan Africa, Western Pacific Region, European Union, Latin America and Caribbean, and South Asia.
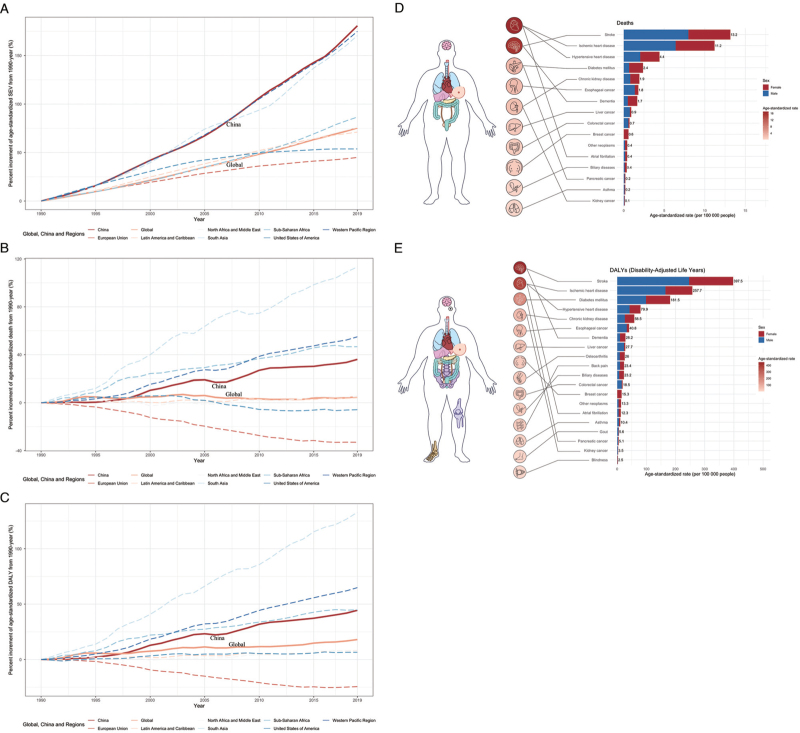
As shown in Figure 1A, China was among the countries with the highest speed of age-standardized SEV increase worldwide and ranked at 18th place among 204 countries/ territories. Compared to data in 1990, the age-standardized SEV in China doubled in 2009 and almost tripled in 2019. The increasing rate of age-standardized SEV of high BMI in China was over two folds the global average level after 2010. The increments of deaths and DALYs attributable to high BMI in China ranked 59th and 52nd among 204 countries/territories worldwide in the past 30 years [Figures 1B and 1C]. The increasing rates of both deaths and DALYs remained on the rise and neither prevalence nor burden of obesity reached a peak in China by 2019.
Figure 1.
The epidemiology trend and burden of high BMI in China. (A) The estimated percentage changes of age-standardized summary exposure value of high BMI in China and other regions over the world from 1990 to 2019. (B) The estimated percentage changes of age-standardized death of high BMI in China and other regions over the world from 1990 to 2019. (C) The estimated percentage changes of age-standardized DALY of high BMI in China and other regions over the world from 1990 to 2019. (D) The specific causes of death attributable to high BMI in China, 2019. (E) The specific causes of DALY attributable to high BMI in China, 2019. Colors of the organs represent the age-standardized rate of deaths in Panel D and DALYs in Panel E, with darker color represents higher burden. BMI: Body mass index; DALY: Disability-adjusted life of years; SEV: Summary exposure value.
Specific diseases attributable to overweight and obesity have also shown unique patterns in China. As shown in Figures 1D and 1E, the top five diseases that contributed to the majority of the age-standardized deaths and DALYs in 2019 included cardiovascular diseases (i.e., stroke, ischemic heart disease and hypertensive heart disease), diabetes mellitus, and chronic kidney disease. High BMI caused a heavy disease burden of malignancies in the esophagus, liver, breast, pancreas, kidney, thyroid, female reproduction system and hematological system. Dementia and pain (mainly in the knee and back) attributable to high BMI also impaired people's health and reduced healthy life years.
The current strikingly increasing trend heavily challenges the healthcare and economic systems in China now and expectedly in the following decades. Although several actions are on their way, China cannot wait for more to rescue the country from the potential crisis.
For people who have overweight or obesity and possibly associated complications, there is no one-pill-fit-all strategy in practice. The individualized desire regarding body shape varies across different populations.[5] Most adults with obesity in China consider weight loss rather a cosmetic issue than a life-threatening problem. It delays the behavior of seeking medical care until major obesity-related diseases occur. Before giving advice, clinicians should make an essential assessment to identify potential diseases and complications associated with obesity and communicate with the patient regarding his/her motivation and target in weight control. Health motivation and target of weight control are critical and may need education from the clinicians. Both clinicians and patients with weight control need to be aware that his/her target is to improve health conditions and ultimately to decrease obesity-related disease burden rather than the specific number of surrogate parameters such as body weight.
Although novel approaches come forth, clinicians have limited choice in managing obesity. Lifestyle modifications, including dietary and exercise advice, are always the first action. For severe obesity, bariatric surgery adding to lifestyle modification is one of the limited options to improve long-term survival with solid evidence.[6] If lifestyle modifications fail and bariatric surgery is not clinically indicated or practical, clinicians may consider weight-lowering drugs and some special dietary treatments such as ketogenic diet and intermediate fasting.[7–10] Orlistat remains the only approved drug for bodyweight loss in China. However, anti-diabetic drugs including metformin and glucagon-like peptide-1 (GLP-1) receptor agonists are widely used in adults with obesity but not diabetes in China. Nevertheless, the latest network meta-analysis demonstrates clinically meaningful bodyweight reduction of GLP-1 receptor agonist but not that of metformin in adults with overweight or obesity regardless of the presence of diabetes.[7] The non-evidence-supportive clinical behavior calls for high-quality clinical practice guidelines for the management of obesity in China.
Given the complicity of the clinical management of overweight and obesity at the individual level, the ultimate solution also relies on addressing the determinants at the population level, which include systemic forces, environmental drivers, and individual risk factors.[11] Economic growth with adequate food supply before ecological adaption of our body is among one of them but never the one that we should blame. Rather, intemperate eating, physical inactivity and sedentariness are the culprits that need nationwide health education. Close collaboration between the government and academic society may facilitate environmental improvement including food and beverage, healthcare, physical activity, marketing, children care and schooling.[12] Although successful experiences for obesity control are accumulating, policymakers and public health practitioners in China need to adapt them to the Chinese local conditions.
Substantial opportunities company with the challenges, calling for innovative actions from policymakers, health providers and industry before the prevalence and burdens attributable to overweight and obesity reach the peak in China. As shown in Figures 1A, 1B and 1C, the age-standardized SEV of high BMI in the European Union and the US already fell below the global average level and the deaths and QALYs attributable to high BMI decreased by 33% and 24.5% in European Union from 1990 to 2019. These changes are inspiring, and China may emulate these regions with its commitments after proper tailoring and localization to the Healthy China vision. Health care providers call for trustworthy and transparent evidence-based clinical practice guidelines to facilitate their practice of bodyweight control. The health industry may consider novel biological or informatic approaches with evidence-based approval for long-term health net benefits in the following years.
In summary, China is facing a challenge by the obesity pandemic warranting urgent action from policymakers, public health practitioners and clinicians. Historical examples and lessons from high socio-demographic index countries such as European Union and the US may help stakeholders in China to find their own way to respond to the pandemics.
Acknowledgement
The authors thank the contributors of the Global Burden of Disease Collaborative Network.
Funding
This study was supported by a grant from West China Hospital of Sichuan University (1.3.5 Project for Disciplines of Excellence, Nos. ZYGD18022 and 2020HXF011).
Conflicts of interest
None.
Footnotes
How to cite this article: Li J, Shi Q, Gao Q, Pan XF, Zhao L, He Y, Tian H, Zhu Z, Li S. Obesity pandemic in China: epidemiology, burden, challenges, and opportunities. Chin Med J 2022;135:1328–1330. doi: 10.1097/CM9.0000000000002189
References
- 1.Wang L, Zhou B, Zhao Z, Yang L, Zhang M, Jiang Y, et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet 2021; 398:53–63. doi: 10.1016/s0140-6736(21)00798-4. [DOI] [PubMed] [Google Scholar]
- 2.Institute for Health Metrics and Evaluation. Global Health Data Exchange. Available from: http://ghdx.healthdata.org/gbd-results-tool. [Last accessed on February 15, 2022]. [Google Scholar]
- 3.Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396:1223–1249. doi: 10.1016/s0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai H, Alsalhe TA, Chalghaf N, Ricco M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: An analysis of the Global Burden of Disease Study. PLoS Med 2020; 17:e1003198.doi: 10.1371/journal.pmed.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grabe S, Hyde JS. Ethnicity and body dissatisfaction among women in the United States: a meta-analysis. Psychol Bull 2006; 132:622–640. doi: 10.1037/0033-2909.132.4.622. [DOI] [PubMed] [Google Scholar]
- 6.Syn NL, Cummings DE, Wang LZ, Lin DJ, Zhao JJ, Loh M, et al. Association of metabolic-bariatric surgery with long-term survival in adults with and without diabetes: a one-stage meta-analysis of matched cohort and prospective controlled studies with 174 772 participants. Lancet 2021; 397:1830–1841. doi: 10.1016/s0140-6736(21)00591-2. [DOI] [PubMed] [Google Scholar]
- 7.Shi Q, Wang Y, Hao Q, Vandvik PO, Guyatt G, Li J, et al. Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. Lancet 2022; 399:259–269. doi: 10.1016/s0140-6736(21)01640-8. [DOI] [PubMed] [Google Scholar]
- 8.Ge L, Sadeghirad B, Ball GDC, da Costa BR, Hitchcock CL, Svendrovski A, et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ 2020; 369:m696.doi: 10.1136/bmj.m696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Churuangsuk C, Hall J, Reynolds A, Griffin SJ, Combet E, Lean MEJ. Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission. Diabetologia 2022; 65:14–36. doi: 10.1007/s00125-021-05577-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patikorn C, Roubal K, Veettil SK, Chandran V, Pham T, Lee YY, et al. Intermittent Fasting and Obesity-Related Health Outcomes: An Umbrella Review of Meta-analyses of Randomized Clinical Trials. JAMA Netw Open 2021; 4:e2139558.doi: 10.1001/jamanetworkopen.2021.39558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan X-F, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol 2021; 9:373–392. doi: 10.1016/s2213-8587(21)00045-0. [DOI] [PubMed] [Google Scholar]
- 12.Chriqui JF. Obesity Prevention Policies in U.S. States and Localities: Lessons from the Field. Curr Obes Rep 2013; 2:200–210. doi: 10.1007/s13679-013-0063-x. [DOI] [PMC free article] [PubMed] [Google Scholar]