Abstract
Septoplasty and inferior turbinate reduction is a common operation performed by ear, nose and throat surgeons for obstructive nasal symptoms. We present a case of complete unilateral scarring of the Eustachian tube orifice, a previously unreported complication, following septoplasty and inferior turbinate reduction for nasal obstruction. It is important to consider this differential diagnosis in patients presenting with unilateral middle ear effusion postoperatively.
Keywords: Eustachian tube, Scarring, Septoplasty, Inferior turbinate
Case history
A 31-year-old female presented with a longstanding history of nasal obstruction. She simultaneously underwent a septoplasty and reduction of inferior turbinates in Italy in October 2016.
Two weeks post-procedure, she developed persistent, non-pulsatile tinnitus in her left ear. She described this as intrusive and debilitating, having a significant effect on her quality of life. At the same time, she developed glue ear and had a grommet inserted into her left ear in the same year. There was mild improvement in her symptoms of left-sided hearing loss. However, the grommet self-extruded in April 2018 and her left-sided hearing loss subsequently returned.
She had no significant medical or family history, including no history of granulomatous disease nor any previous radiation exposure. She had no history of smoking or alcohol consumption.
The patient presented to our ear, nose and throat (ENT) department in June 2018, two years following her initial operation. She described a sensation of fullness and pressure disequilibrium of the left ear. The left-sided tinnitus and hearing loss remained persistent. Otoscopy of the left ear demonstrated an injected tympanic membrane with a fluid level – in keeping with chronic left-sided glue ear.
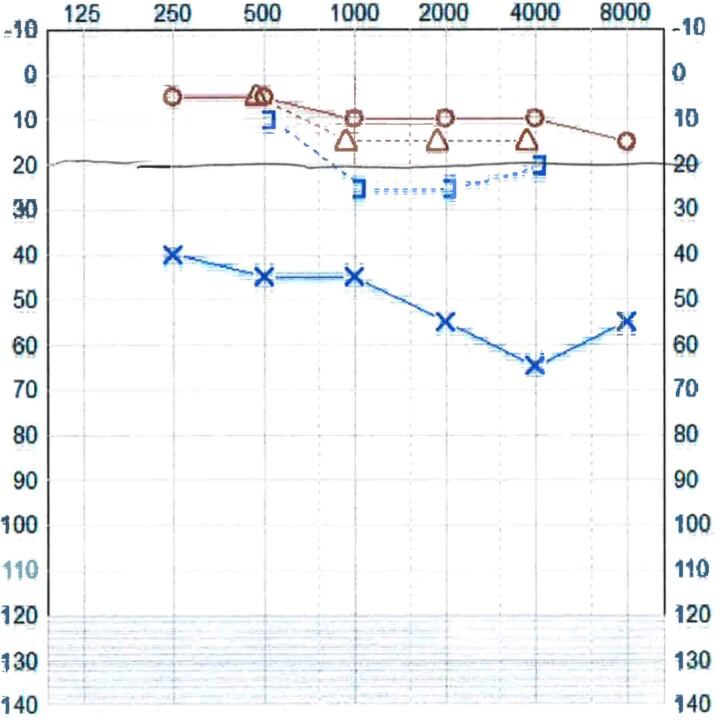
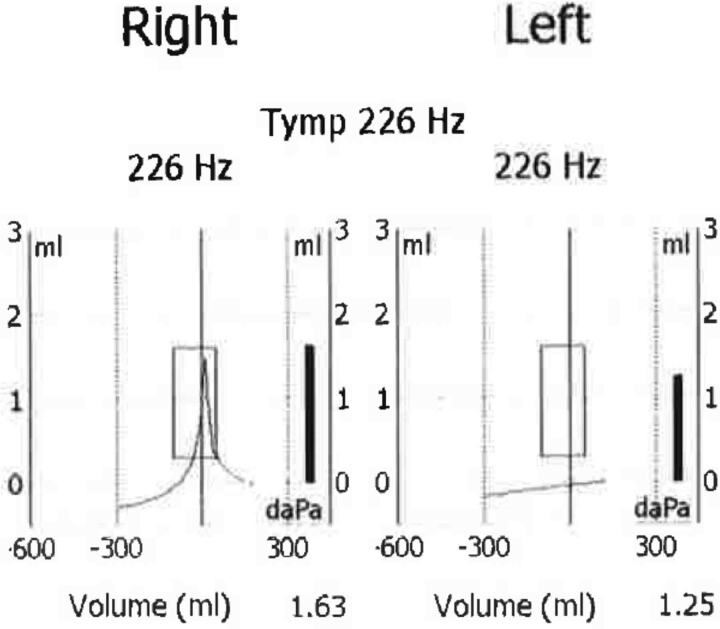
An audiogram in November 2018 demonstrated normal hearing in the right ear and moderate mixed-hearing loss on the left ranging from 40 to 65 decibels. Tympanometry was normal on the right, whereas on the left there was a flat type B trace, in keeping with a left-sided middle ear effusion (Figures 1 and 2).
Figure 1 .
Audiogram in November 2018
Figure 2 .
Tympanogram in November 2018
Flexible nasoendoscopy was performed, demonstrating unilateral left-sided scarring and complete occlusion of the Eustachian tube orifice. There were no other lesions in the post-nasal space (Figures 3–5).
Figure 3 .
Endoscopic image of left post-nasal space demonstrating Eustachian tube scarring
Figure 5 .
Endoscopic image of right post-nasal space showing a normal Eustachian tube opening
Figure 4 .
Second endoscopic image of left post-nasal space demonstrating Eustachian tube scarring
T2-weighted magnetic resonance imaging (MRI) of bilateral internal acoustic meatuses in November 2019 demonstrated no evidence of acoustic neuroma bilaterally, or mass lesions. However, there was opacification of the mastoid air cells on the left, extending into the left middle ear.
A diffusion-weighted MRI was subsequently performed in January 2020 of bilateral internal acoustic meatuses, confirming fluid signal in the left mastoid bone reflective of non-specific debris with middle ear effusion. There was no gross abnormality visualised in the nasopharynx to cause Eustachian tube obstruction.
The patient was reviewed regularly by the local ENT team and initially treated with a left-sided hearing aid in November 2018 for her moderate hearing loss. She underwent tinnitus re-training therapy and completed a course of xylometazoline and fluticasone nasal sprays.
The patient was offered T-tube insertion for her left ear, but this was postponed as she was pregnant. She subsequently underwent this procedure in January 2020. Balloon dilation was not offered because the presence of scarring prevented placement of the introducer into the Eustachian tube orifice.
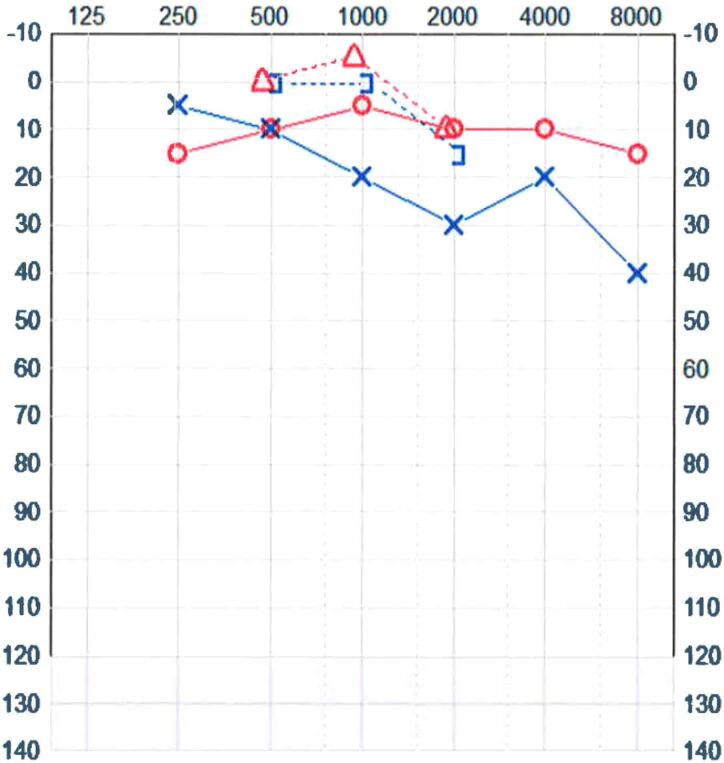
Insertion of a left-sided T-tube resulted in complete resolution of her symptoms of tinnitus, hearing loss, aural fullness and chronic glue ear. A repeat audiogram in November 2020 demonstrated improved hearing in the left ear (Figure 6).
Figure 6 .
Audiogram in November 2020
Discussion
Nasal obstruction, a blocked nose sensation, affects up to 33% of the population.1 Severity is variable and there can be considerable impact on activities of daily living.2 Obstruction is classified into two main categories: structural or inflammatory. Structural causes include deviation of the nasal septum, nasal trauma, adenoid or inferior turbinate hypertrophy. Inflammatory causes are secondary to rhinosinusitis.
Septal deviation is the most common structural abnormality identified in those with obstructive nasal symptoms. It is in these patients that septoplasty may be indicated to improve the nasal airway. Reduction of the inferior turbinate may be performed simultaneously to further aid this.
Recognised complications of septoplasties include: pain, bleeding, cerebrospinal fluid rhinorrhoea, ocular complications, infection, septal perforation and altered cosmesis. Less common complications include empty nose syndrome, anosmia and dental anaesthesia.3
Reported complications following inferior turbinate reduction include: bleeding, nasal dryness and crusting, atrophic rhinitis and empty nose syndrome.2
To the best of our knowledge, complete unilateral scarring of the Eustachian tube orifice following septoplasty and inferior turbinate reduction has not been reported previously. In this case, the patient’s clinical presentation was highly suspicious of iatrogenic injury following an overzealous attempt at inferior turbinate reduction. The surgical technique employed in this case is not detailed in the operation notes. Generally, these can be classified as mucosal preserving or non-mucosal preserving. Mucosal sparing, by means of microdebrider turbinoplasty, is most commonly utilised.4 Non-mucosal preserving techniques are associated with increased side effects including the formation of scar tissue and nasal synechiae.4 In this case, significant mucosal disruption may have resulted in the formation of scar tissue at the Eustachian tube orifice. This is also a risk with mucosal-preserving techniques but can be limited by cautious use of the microdebrider; a point emphasised by this case.4
The management of Eustachian tube dysfunction can be challenging and is guided by the underlying cause of dysfunction. Here, we discuss symptomatic management of Eustachian tube dysfunction, not physical obstruction of the tube orifice. Nonoperative methods include intranasal corticosteroids and regular performance of the Valsalva manoeuvre.5 Surgical options include pressure-equalisation devices (such as T-tubes), Eustachian tuboplasty and tubal dilation with the Bielefeld balloon catheter.1 Single trials have found two pressure-equalisation devices to be associated with significant short-term improvements in symptoms, middle ear function and hearing.1 Furthermore, multiple case series have found Eustachian tuboplasty and balloon dilation to be associated with improved patient outcomes.1
In this case, the local ENT team determined use of surgical pressure-equalisation device (T-tube) as the most appropriate option for her symptom control.
Conclusions
This paper describes Eustachian tube dysfunction as a previously unreported complication of septoplasty and inferior turbinate reduction. It is important to consider Eustachian tube scarring as a differential diagnosis in patients presenting with unilateral middle ear effusion postoperatively.
References
- 1.Llewellyn A, Norman G, Harden Met al. Interventions for adult Eustachian tube dysfunction: a systematic review. Health Technol Access 2014; 18: 1–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jourdy D. Inferior turbinate reduction. Oper Tech Otolaryngol 2014; 25: 160–170. [Google Scholar]
- 3.Ketcham AS, Han JK. Complications and management of septoplasty. Otolaryngol Clin North Am 2010; 43: 897–904. [DOI] [PubMed] [Google Scholar]
- 4.Abdullah B, Singh S. Surgical interventions for inferior turbinate hypertrophy: A comprehensive review of current techniques and technologies. Int J Environ Res Public Health 2021; 18: 3441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schroeder S, Ebmeyer J. Diagnosis and treatment of eustachian tube dysfunction. HNO 2018; 66: 155. [DOI] [PubMed] [Google Scholar]