Regular bowel screening and aspirin reduce colorectal cancer among patients with LS but extracolonic cancers are difficult to detect and manage. This study suggests that RS reduces morbidity associated with extracolonic cancers.
Abstract
Abstract
The CAPP2 trial investigated the long-term effects of aspirin and resistant starch on cancer incidence in patients with Lynch syndrome (LS). Participants with LS were randomized double-blind to 30 g resistant starch (RS) daily or placebo for up to 4 years. We present long-term cancer outcomes based on the planned 10-year follow-up from recruitment, supplemented by National Cancer Registry data to 20 years in England, Wales, and Finland. Overall, 463 participants received RS and 455 participants received placebo. After up to 20 years follow-up, there was no difference in colorectal cancer incidence (n = 52 diagnosed with colorectal cancer among those randomized to RS against n = 53 on placebo) but fewer participants had non-colorectal LS cancers in those randomized to RS (n = 27) compared with placebo (n = 48); intention-to-treat (ITT) analysis [HR, 0.54; 95% confidence interval (CI), 0.33–0.86; P = 0.010]. In ITT analysis, allowing for multiple primary cancer diagnoses among participants by calculating incidence rate ratios (IRR) confirmed the protective effect of RS against non–colorectal cancer LS cancers (IRR, 0.52; 95% CI, 0.32–0.84; P = 0.0075). These effects are particularly pronounced for cancers of the upper GI tract; 5 diagnoses in those on RS versus 21 diagnoses on placebo. The reduction in non–colorectal cancer LS cancers was detectable in the first 10 years and continued in the next decade. For colorectal cancer, ITT analysis showed no effect of RS on colorectal cancer risk (HR, 0.92; 95% CI, 0.62–1.34; P = 0.63). There was no interaction between aspirin and RS treatments. In conclusion, 30 g daily RS appears to have a substantial protective effect against non–colorectal cancer cancers for patients with LS.
Prevention Relevance:
Regular bowel screening and aspirin reduce colorectal cancer among patients with LS but extracolonic cancers are difficult to detect and manage. This study suggests that RS reduces morbidity associated with extracolonic cancers.
Introduction
Lynch syndrome (LS) is due to germline pathogenic variants in one of the DNA mismatch repair (MMR) genes that increase the risk of many types of cancer, particularly cancers of the colorectum (colorectal cancer) but also of the endometrium, ovary, stomach, small intestine, pancreas, bile duct, urinary tract, brain, and skin (1). The National Institute for Health and Care Excellence (NICE) in the United Kingdom has recommended, primarily based on the outcome of the aspirin limb of the CAPP2 trial (discussed below in more detail), “Consider daily aspirin, to be taken for more than 2 years, to prevent colorectal cancer in people with Lynch syndrome” (2).
In contrast, the only intervention proven to reduce the risk of extracolonic LS-related cancers is prophylactic surgery, where feasible. As a result of their incidence and challenging presentations, extracolonic cancers contribute more cancer deaths than does colorectal cancer to overall mortality among LS patients with cancers of the upper gastrointestinal (GI) tract and brain being substantially more likely to be lethal than are colorectal malignancies (3).
Fifty years ago, Burkitt proposed that higher dietary fiber (DF) intake may protect against colorectal cancer and other bowel disorders (4). An analysis of pooled data from 13 prospective cohort studies showed that higher DF intake was associated inversely with risk of colorectal cancer in age-adjusted analyses, but this protection disappeared after accounting for other dietary risk factors (5). Recent meta-analysis of data from prospective cohort studies shows lower risk of all-cause mortality with higher DF intake (6). This health benefit of higher DF intake was reflected in lower incidence of cardiometabolic disease and of colorectal cancer and lower cancer mortality (6). There is strong evidence that higher intakes of foods containing DF, including wholegrain foods, lower risk of colorectal cancer (7) and may lower risk of hepatocellular carcinoma (8). DF encompasses a heterogeneous mixture of food-derived carbohydrates which escape small-bowel digestion and are fermented to differing extents in the large bowel. The resultant production of short-chain fatty acids (SCFA), including the antineoplastic butyrate (9), and other metabolites, and changes in the gut microbiota, may be important mechanisms through which DF protects against colorectal cancer (10, 11, 12).
From 1999, the CAPP2 study recruited people with LS, formerly known as hereditary non-polyposis colon cancer (13). In a 2 × 2 factorial design, participants received (i) 600 mg enteric-coated aspirin or placebo, and (ii) 30 grams of resistant starch (RS) or placebo, daily. RS is a component of DF found in foods such as bananas, potatoes, grains, pulses, and seeds (14).
In total, 937 patients with LS, mean age 45 years, were recruited to the CAPP2 study. At the end of the intervention period (2.5 years), there was no significant impact of either agent on “neoplasia”, which combined colorectal adenoma and carcinoma formation (13). However, because epidemiologic studies suggest a delayed effect of aspirin on colorectal cancer incidence (15), the protocol provided for follow-up to 10 years. When the first recruits reached 10-year follow-up (mean follow-up 4.5 years), an interim analysis revealed no detectable effect of RS on cancer development (16).
The CAPP2 study had two primary hypotheses that examined evidence, separately, for long-term effects of aspirin and of RS. The primary hypothesis was that each intervention, aspirin and RS, would separately prevent colorectal cancer. A secondary outcome was the effect of each intervention on non–colorectal cancer LS cancers. The design involved consent to follow up for 10 years with the explicit aim of investigating long-term effects of aspirin and of RS treatment on cancer incidence. We have reported the long-term impact of aspirin (17) and we now report the impact of RS censored to 10 years from recruitment. We have complemented this planned analysis with available national cancer registry data through the second decade for three countries where there are formal policies to allow all cancers to be recorded; England, Wales (18) and Finland, the latter via the Finnish Lynch Syndrome Registry (19).
Materials and Methods
Trial design and participant recruitment
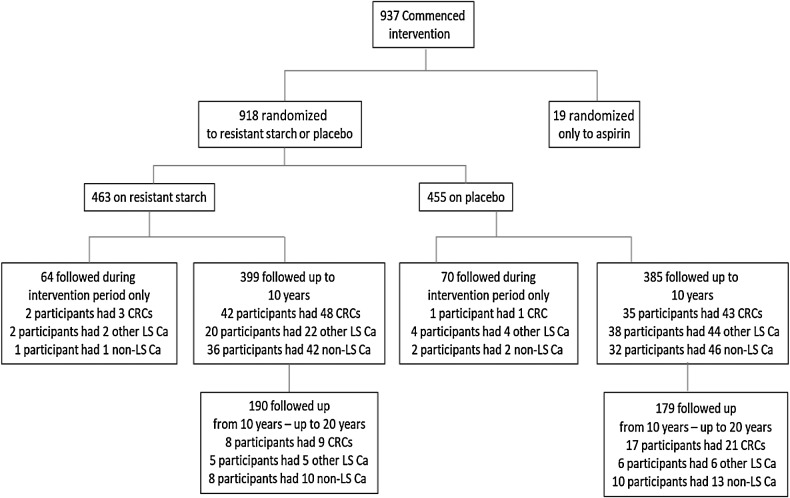
The methods have been described (13, 17). In brief, 937 LS carriers were randomized to RS and/or aspirin in a factorial design such that, if willing to take both interventions, they were randomized with equal probability to one of four groups: aspirin + RS, aspirin placebo tablets + RS, aspirin + placebo (cornstarch), or aspirin placebo tablets + placebo (cornstarch). There was an option to be randomized to a single limb [aspirin/placebo, RS/placebo (cornstarch)] if medically dictated. Intervention took place between 1999 and 2007 (Fig. 1). Of the 937 participants, 463 were assigned to RS and 455 to cornstarch placebo (henceforth called placebo; ref. 16): 19 participants chose not to be randomized in the RS arm of the study. Participants and investigators were blinded to randomized intervention. Daily interventions were 30 g of RS (1:1 blend of Novelose 240 and Novelose 330) or placebo [waxy starch (Amioca)]. Intervention lasted 2 years with an option to continue for a further 2 years. Written informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki and was approved by the relevant ethics committee in each country (13). Consent included health record follow-up for 10 years and was refreshed in the later stages of the study. Participants and their clinicians were informed of randomization category no sooner than the 10-year review, or if and when, later contact was achieved.
Figure 1.
Trial profile showing distribution of participants by randomisation group and length of follow-up together with counted outcomes of cancer diagnoses among participants; CRC, colorectal cancer; LS Ca, Lynch syndrome associated cancers (other than colorectal cancer).
Recruitment to CAPP2 was through specialist centers worldwide which also organized and monitored regular bowel screening as part of routine clinical care of patients with LS. LS cancers can occur at multiple anatomic sites making it more challenging for some specialist centers to record extracolonic cancers. The accession of information from the English, Finnish, and Welsh national records (described below) alleviated such concerns and ensured complete cancer follow-up of participants in these locations.
Data on clinical outcomes from participating centers were sent to the CAPP2 Offices, Newcastle University, United Kingdom, and entered into a TrakGene database (https://www.trakgene.com/). These data were linked to study number, anonymized and sent to the University of Leeds for statistical analysis.
Patient and Public Involvement
This trial was set up in the late 1990s. As was usual at the time, there was no formal Patient and Public Involvement.
Role of the funding source
Neither the funders nor the sponsors of the study had any role in study design, data collection, analysis, or interpretation, or writing of the report. The corresponding authors had full access to all study data and had final responsibility for the decision to publish.
Trial registration
The trial is registered at ISRCTN59521990 (20).
The current analysis includes 10-year data across all centers plus up to a further decade of registry follow-up for participants resident in England, Wales, and Finland. For England and Wales, cancer history was assessed using National Cancer Registration information from Public Health England (PHE) and Welsh counterparts (see below). Similarly, because LS carriers in Finland are monitored centrally, long-term (up to 20 years) cancer data for these participants were obtained from the Finnish national registry.
Long-term data from England and Wales
The National Cancer Registration and Analysis Service (NCRAS) provided information on all diagnoses of cancer among the CAPP2 participants resident in England (from Public Health England (PHE) and Wales [from Public Health Wales (PHW)]. Note that this service is now known as the National Disease Registration Service (NDRS) and is provided by NHS Digital (18). This included ICD-coded information on specific diagnoses and dates of registration. For inclusion in the life-table analyses, we confirmed that participants had remained resident in England or Wales throughout this time period (whether or not they had a cancer diagnosis) by identification of current general practitioner. This provided complete cancer information for these participants through to the last date at which the registry was considered complete. For those participants known to have died or emigrated, follow-up was censored at death or at estimated date of emigration.
Long-term data from Finland
Data were obtained from the Lynch Syndrome Registry of Finland (LSRFi) maintained by the Department of Surgery, Jyväskylä, Finland, which operates as a national research database of MMR pathogenic variant carriers and their high-risk family members. Historically, families were included in the registry based on clustered LS-associated cancers within the families. Because genetic testing became available, pathogenic variants only are recorded in the registry and families are identified by universal MMR testing of LS-related cancers or by clinical phenotype.
Most centers report their clinical findings to the LSRFi office routinely. In addition, the LSRFi office monitors scheduled surveillance for each carrier and requests the clinical reports from the treating institutions. Finally, the nationally operated Finnish Cancer Registry is queried for the carriers of pathological variants known to the LSRFi office. The administration and the ethical board of the Central Finland health care district approved the study.
Outcomes
We have reported details of adenoma recurrence, adverse events, and compliance (i.e., proportion of scheduled starch sachets taken during the intervention; ref. 13).
The primary outcomes of the CAPP2 study were the number, size, and histologic stage of colorectal carcinomas after a minimum of two years’ intervention through to the end of follow-up. Secondary outcomes were size and number of adenomas and numbers of LS-related extracolonic cancers.
This analysis focused on the 918 CAPP2 study participants randomly assigned to RS (n = 463) or placebo (n = 455) from the date of entry until the latest date of information on cancer status. For recruits in England, Finland, and Wales, this was supplemented with passive recording of cancer registration. The analysis included all LS cancer diagnoses, during the intervention phase and during long-term follow-up. Designation of a reported diagnosis as being within the LS cancer spectrum (i.e., endometrial, ovarian, pancreatic, small bowel, gall bladder, ureter, stomach, and kidney cancers and cancer of the brain) was a clinical assessment, masked to intervention (1). Our initial plan was document cancer diagnoses for up to 10 years since starting the intervention. However, the staggered start across countries and the availability of national clinical records for England, Finland, and Wales meant that longer follow-up (up to 20 years) was available for these countries. Consequently, we report here the results for the follow-up up to 20 years to provide the most detailed assessment of impact. Analysis when follow-up is restricted to 10 years is included in Supplementary Tables S1 and S2.
During the intervention phase, adverse events were similar for RS and placebo groups (13). For at least 80% of the time, 77% of the participants complied with the use of RS or placebo. A subgroup of 100 participants from the United Kingdom completed a 4-day dietary assessment and provided a urine sample; the compliance biomarker 4-aminobenzoic acid was detected in 93% of these participants (13).
Analysis
Intention-to-treat (ITT) analyses were conducted according to randomization, RS, or placebo to provide marginal results that are independent of assignment to aspirin/aspirin placebo. Participants were provided with two starch sachets daily and, at clinic visits during intervention, participants were asked to show the sachets remaining; this number was used to estimate the number taken. We also conducted per protocol (PP) analysis restricted to those who took at least 1,400 sachets (equivalent to 2 years’ provision of the treatment).
We used two analytical approaches: (1) we examined time to first occurrence of colorectal cancer (primary endpoint) and non-colorectal cancer LS cancers using life-table methods and Cox proportional hazards, and (ii) we investigated multiple primary cancers at the same, or multiple, anatomic sites using negative binomial regression (NBR), which considers the complete LS cancer history since randomization. In an earlier study, we used Poisson regression modeling (16) but analysis of this extended dataset indicated overdispersion.
For life-table analysis and Cox proportional hazards analysis, end of follow-up was the time to first diagnosis of colorectal cancer (or other LS cancer, as appropriate), or the last recorded date at which clinical status was known. The date of the last clinical follow-up was provided by the local recruiting center for each participant except for those in England and Wales. For the English and Welsh centers, the data from NCRAS was the December 31, 2016, version of complete cancer registration, so participants without a diagnosis were censored at that date. For participants who had died or emigrated, follow-up was censored at the date of death or the date of embarkation, respectively.
For the NBR analysis, exposure time was calculated from randomization until the date of last known clinical status, or 10 years if this came earlier for the whole CAPP2 study cohort and up to 20 years for participants in England, Finland, and Wales.
Sex- and age-adjusted hazard ratio (HR) estimates and 95% confidence intervals (CI) were calculated using Cox proportional hazard models, and cumulative incidence curves were used to assess nonparametrically outcome differences between groups. We made these adjustments because of the variation in cancer risk with age and the sex differences in cancer spectrum. The assumption of proportional hazard was tested using Schoenfeld residuals. Sex- and age-adjusted incidence rate ratios (IRR) were calculated using NBR to estimate the effect of RS from log-linear models for the number of primary cancers diagnosed after randomization until last follow-up.
Secondary analysis examined the incidence of non–colorectal cancer LS cancers and, finally, the total burden of LS-related cancers. In keeping with the original sample size calculations, all P values were two-sided. Analyses were carried out in Stata v14 (Stata Corp).
As is standard practice in reporting factorial design clinical trials, in the main tables and text, we document the marginal effects of RS on cancer risk. We report in Supplementary Table S3 analyses after adjusting for the randomization within the aspirin arm. In addition, we report the outcomes and analyses for two subsets of the complete follow-up: (i) for all CAPP2 study participants restricted to 10 years follow-up (Supplementary Table S1) and (ii) for the cohort of participants from England, Finland, and Wales for whom up to 20 years of follow-up are available (Supplementary Table S4).
Data availability
Data were generated by the authors and requests for access to data should be made to the corresponding author (J.C. Mathers).
Results
Follow-up and outcomes
We present analyses of the whole CAPP2 cohort at 10 years plus England, Finland, and Wales to 20 years as the main analysis. The characteristics of participants randomized to RS (n = 463) and placebo (n = 455) were similar with approximately 25 months of intervention and ≈10 years of follow-up in each group (Table 1; Supplementary Table S5). Supplementary Figure S1 shows cumulative incidence curves for cancer incidence for the whole cohort over the total study.
Table 1.
The whole CAPP2 cohort at 10 years plus England, Finland, and Wales registry data to 20 years.
| Resistant starch (n = 463) | Placebo (n = 455) | All participants (n = 918) | |
|---|---|---|---|
| Time in CAPP2 intervention study (months) a | 24.6 (13.8, 0.8–74.4) | 25.3 (13.2, 1.1–60.6) | 25.0 (13.5, 0.8–74.4) |
| Months between study entry and last known follow-up date a | 119.7 (37.9, 1.6–238.7) | 114.5 (63.0, 1.1–238.9) | 117.1 (62.8, 1.1–238.9) |
| Years between study entry and last known follow-up date (categorized; n) | |||
| ≤2 | 41 (9%) | 45 (10%) | 86 (9%) |
| >2 and ≤6 | 83 (18%) | 90 (20%) | 173 (19%) |
| >6 and ≤10 | 157 (34%) | 155 (34%) | 312 (34%) |
| >10 and ≤14 | 48 (10%) | 54 (12%) | 102 (11%) |
| >14 and ≤18 | 115 (25%) | 92 (20%) | 207 (23%) |
| >18 and ≤20 | 19 (4%) | 19 (4%) | 38 (4%) |
| Participants with first colorectal cancer (n) | |||
| Since randomization | 52 (11%) | 53 (12%) | 105 (11%) |
| Within 2 years of randomization | 10 (2%) | 10 (2%) | 20 (2%) |
| More than 2 years from randomization | 42 (9%) | 43 (9%) | 85 (9%) |
| Participants with extracolonic LS cancers (n) | |||
| Since randomization | 27 (6%) | 48 (11%) | 75 (8%) |
| Within 2 years of randomization | 7 (2%) | 11 (2%) | 19 (2%) |
| More than 2 years from randomization | 20 (4%) | 37 (8%) | 57 (6%) |
| Participants with one or more LS cancer (including colorectal; n) | |||
| Since randomization | 78 (17%) | 96 (21%) | 174 (19%) |
| Within 2 years of randomization | 17 (4%) | 21 (5%) | 38 (4%) |
| More than 2 years from randomization | 61 (13%) | 75 (16%) | 136 (15%) |
| Participants with non-LS cancers (n) | |||
| Since randomization | 45 (10%) | 44 (10%) | 89 (10%) |
| Within 2 years of randomization | 3 (<1%) | 6 (1%) | 9 (1%) |
| More than 2 years from randomization | 42 (9%) | 38 (8%) | 80 (9%) |
| Types of extra-colonic LS cancers b (n) | |||
| Brain | 2 (<1%) | 3 (<1%) | 5 (1%) |
| Upper GI | |||
| Stomach | 1 (<1%) | 3 (<1%) | 4 (<1%) |
| Duodenum | 1 (<1%) | 7 (2%) | 8 (1%) |
| Bile duct | 0 (<1%) | 3 (<1%) | 3 (<1%) |
| Pancreas | 3 (<1%) | 8 (2%) | 11 (1%) |
| Total of upper GI diagnoses | 5 | 21 | 26 |
| Urinaryc | 5 (1%) | 10 (2%) | 15 (2%) |
| Ovarian | 2 (<1%) | 5 (1%) | 7 (1%) |
| Endometrium | 15 (3%) | 16 (4%) | 31 (3%) |
| Total of non-colorectal cancer LS diagnoses | 29 | 55 | 84 |
Abbreviations: GI, gastrointestinal tract; LS, Lynch syndrome.
aData are mean (SD; range) or n (%).
bTwo participants in RS and 5 participants in placebo had more than one extra-colonic LS cancer.
cUrinary cancers include ureter and kidney cancers.
For all cancers, information obtained from the CAPP2 centers was compared with cancer diagnosis data obtained from national cancer or clinical registries where available (Table 2). For colorectal cancer, there was 1 extra diagnosis in the English and Welsh records and 3 extra diagnoses in the Finnish records. For extracolonic LS cancers, there were 3 extra diagnoses in English and Welsh records, in addition to the 9 concordant diagnoses; Finnish records identified 5 extra diagnoses, in addition to the 6 concordant results. Table 1 also shows the numbers of cancers diagnosed during the total follow-up of the cohort while numbers for the whole CAPP2 cohort at 10 years are shown in Supplementary Table S2 and Supplementary Fig. S2 and the follow-up based registry data (England, Finland, and Wales) for up to 20 years is shown in Supplementary Table S3 and Supplementary Fig. S3.
Table 2.
Comparison of cancer diagnoses identified from the CAPP2 database with those identified from the National Cancer Registry and Analysis System (NCRAS) for England plus its Welsh counterpart and the corresponding national records in Finland.
| A. English and Welsh Records for participants randomised to Starch arm | Colorectal cancer | Extra-colonic LS cancer | Non-LS cancer |
|---|---|---|---|
| Consistent between CAPP2 Study database and PHE | 31 | 9 | 13 |
| Reported by CAPP2 Study database; record not found by PHE in NCRAS system | 1 | 0 | 4 |
| Identified by PHE only between study entry and last follow-up date known to CAPP2 study | 1 | 3 | 3 |
| Identified by PHE after last follow-up date known to CAPP2 study | 19 | 13 | 27 |
| Total | 52 | 25 | 47 |
| % Concordance | 31/33 = 94% | 9/12 = 75% | 13/20 = 65% |
| B. Finnish Records for participants randomised to Starch arm | Colorectal cancer | Extra-colonic LS cancer | Non-LS cancer |
|---|---|---|---|
| Consistent between CAPP2 Study database and Finnish records | 15 | 6 | 5 |
| Reported by CAPP2 Study database; record not found in Finnish clinical records | 0 | 0 | 0 |
| Identified by Finnish records only between study entry and last follow-up date known to CAPP2 study | 3 | 5 | 4 |
| Identified by Finnish records after last follow-up date known to CAPP2 study | 11 | 6 | 1 |
| Total | 29 | 17 | 10 |
| % Concordance | 15/18 = 83% | 6/11 = 55% | 5/9 = 56% |
Follow-up information CAPP2 Study participants resident in England and Wales were collected by the CAPP2 Study TrakGene database and obtained from the National Cancer Registry and Analysis System (NCRAS) for England plus its Welsh counterpart and made available for analysis by Public Health England (PHE). The concordance between the CAPP2 database and PHE (in participants randomised to Starch) for England/Wales is shown in part A with corresponding information for Finland in part B. Part A shows the diagnoses that were consistent between the CAPP2 database and the PHE records (except for modest differences in dates of diagnosis), those which were known to the CAPP2 database but were not found in NCRAS system and those that were found in the NCRAS system but were not known to the CAPP2 database. The final row (“Identified by PHE after last follow-up…”) reflects diagnoses made after the last active follow-up for the CAPP2 database. Similar information is available for Finland (part B).
Colorectal cancer outcomes
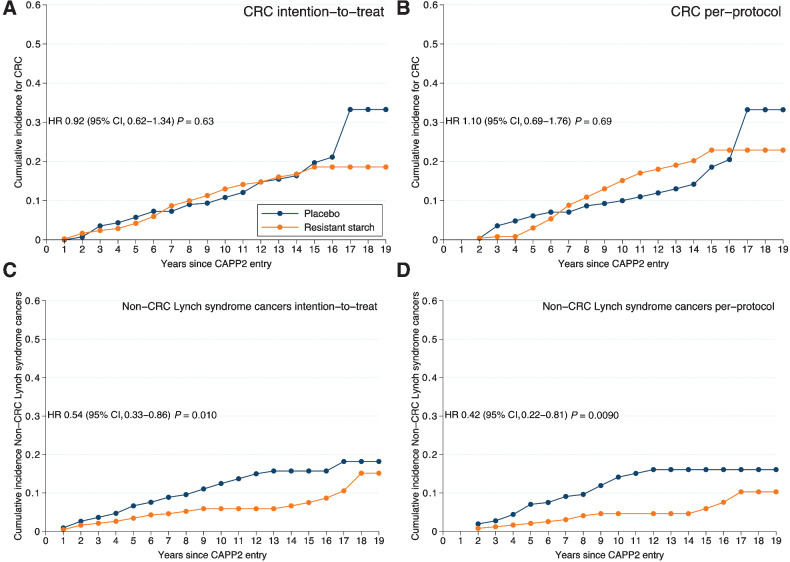
Since randomization, 52 and 53 participants developed colorectal cancer in RS and placebo groups, respectively. ITT analysis indicated no effect of RS on colorectal cancer incidence (HR, 0.92; 95% CI, 0.62–1.34; P = 0.63; Table 3; Fig. 2A). Similarly, PP analysis restricted to participants on treatment for ≥2 years showed no effect of RS on colorectal cancer incidence (HR, 1.10; 95% CI, 0.69–1.76; P = 0.69; Table 3; Fig. 2B). Because participants could be diagnosed with multiple primary cancers, we calculated IRR using NBR and confirmed no effect of RS on colorectal cancer in both ITT and PP analyses (Table 3). There was no evidence of any interaction between aspirin and RS treatments; Supplementary Table S4 shows the marginal results for RS treatment both without adjustment for aspirin as well as after adjustment for the aspirin arm to which the participant was randomized.
Table 3.
Cox proportional hazards and negative binomial regression analyses of cancer incidencea.
| Hazard ratiob (95% CI) | P value | Incidence rate ratioc (95% CI) | P value | |
|---|---|---|---|---|
| Colorectal Cancer | ||||
| Intention-to-treat analysis (N = 918, 105 events) | ||||
| Resistant Starch (RS) versus placebo | 0.92 (0.62–1.34) | 0.63 | 0.85 (0.58–1.25) | 0.41 |
| Per-Protocol Analysisd (N = 521, 71 events) | ||||
| ≥2 years' placebo | 1.0 | — | 1.0 | — |
| ≥2 years' Resistant Starch | 1.10 (0.69–1.76) | 0.69 | 0.96 (0.60–1.53) | 0.86 |
| Cumulative RS dosee (N = 918, 105 events) | ||||
| Units of 100 Resistant Starch | 1.00 (0.98–1.02) | 0.73 | 1.00 (0.98–1.02) | 0.91 |
| Non-colorectal LS cancers | ||||
| Intention-to-treat analysis (N = 918, 75 events) | ||||
| Resistant Starch versus placebo | 0.54 (0.33–0.86) | 0.010 | 0.52 (0.32–0.84) | 0.0075 |
| Per-Protocol Analysisd (N = 521, 44 events) | ||||
| ≥2 years' placebo | 1.0 | — | 1.0 | — |
| ≥2 years' Resistant Starch | 0.42 (0.22–0.81) | 0.0090 | 0.37 (0.19–0.73) | 0.0040 |
| Cumulative RS dosee (N = 918, 75 events) | ||||
| Units of 100 Resistant Starch | 0.96 (0.93–0.98) | 0.0025 | 0.95 (0.92–0.98) | 0.0018 |
| All LS cancers | ||||
| Intention-to-treat analysis (N = 918, 174 events) | ||||
| Resistant Starch versus placebo | 0.76 (0.56–1.02) | 0.066 | 0.69 (0.52–0.93) | 0.014 |
| Per-Protocol Analysisd (N = 521, 110 events) | ||||
| ≥2 years' placebo | 1.0 | — | 1.0 | — |
| ≥2 years' Resistant Starch | 0.80 (0.55–1.16) | 0.24 | 0.68 (0.47–0.99) | 0.044 |
| Cumulative RS dosee (N = 918, 174 events) | ||||
| Units of 100 Resistant Starch | 0.99 (0.97–1.00) | 0.082 | 0.98 (0.97–1.00) | 0.031 |
| All non-LS cancers f | ||||
| Intention-to-treat analysis (N = 918, 89 events) | ||||
| Resistant Starch versus placebo | 0.97 (0.64–1.47) | 0.88 | 0.88 (0.56–1.40) | 0.60 |
| Per-Protocol Analysisd (N = 521, 54 events) | ||||
| ≥2 years' placebo | 1.0 | — | 1.0 | — |
| ≥2 years' Resistant Starch | 0.96 (0.56–1.64) | 0.89 | 0.97 (0.54–1.73) | 0.92 |
| Cumulative RS dosee (N = 918, 89 events) | ||||
| Units of 100 Resistant Starch | 1.00 (0.97–1.02) | 0.69 | 1.00 (0.97–1.02) | 0.72 |
aAdjusted for age and gender in all participants up to 10 years and up to 20 years in England, Finland, and Wales, randomly assigned to Resistant Starch (RS) or placebo.
badjusted for age at consent and gender.
cIncidence rate ratio from negative binomial regression adjusted for age at consent and gender.
dThe threshold for 2 years’ intervention was consumption of more than 1,400 starch sachets; rounded from a 2-year total of 1,461 to allow for early scheduling of the exit colonoscopy or occasional missed dosage.
eUnits of 100 starch = total number of starch sachets taken divided by 100.
fFor details of non-LS cancers, see Supplementary Table S9.
Figure 2.
Time to first colorectal cancer and time to first non-colorectal cancer Lynch syndrome cancer in all CAPP2 study participants followed up for 10 years and for 20 years in England, Finland, and Wales. Cox proportional hazards (HRs and 95% CIs) comparing those on Resistant Starch vs. those on placebo and depicted by Cumulative incidence curves (n = 918). A, Intention-to-treat analysis (n = 463 Resistant Starch, 455 placebo) by randomisation group. B, Per-protocol analysis of all those achieving 2 years Resistant Starch or placebo (n = 521). C, Intention-to-treat analysis for non-colorectal cancer Lynch syndrome cancers. D, Per-protocol analysis for non-colorectal cancer Lynch syndrome cancers.
Subset analyses of time to first colorectal cancer among participants are shown for (i) the first 10 years for all centers in Supplementary Table S5 and 20-year follow-up for England, Finland, and Wales in Supplementary Table S6. Supplementary Table S7 shows the distribution in Dukes stage at presentation (where known) with no apparent stage differences between those randomized to RS and those randomized to placebo.
Non–colorectal cancer LS cancer outcomes
There were extracolonic LS cancers among 27 participants in the RS group (and 29 cancers overall) compared with 48 participants in the placebo group (and 53 cancers overall; Table 1). This protective effect was apparent in ITT analysis (HR, 0.54; 95% CI, 0.33–0.86; P = 0.010; Fig. 2C) and the effect was greater in PP analysis (HR, 0.42; 95% CI, 0.22–0.81; P = 0.0090; Table 3; Fig. 2D). When accounting for multiple primary cancers using IRR analysis, the protective effect of RS against non–colorectal cancer LS cancers was evident for both ITT (IRR, 0.52; 95% CI, 0.32–0.84; P = 0.0075) and PP (IRR, 0.37; 95% CI, 0.19–0.73; P = 0.0040) analyses (Table 3). These effects appeared to be particularly pronounced for cancers of the upper gastrointestinal (GI) tract (stomach, duodenal, bile duct, and pancreatic cancers; Supplementary Fig. S4), which totaled 5 cancers in 5 participants in those randomized to RS versus 21 cancers in 17 participants in the placebo group. Findings were similar when analyses were restricted to all CAPP2 study participants at up to 10 years follow-up (Supplementary Table S5; ITT analysis; HR, 0.51; 95% CI, 0.30–0.85; P = 0.011); PP analysis (HR, 0.35; 95% CI, 0.17–0.72; P = 0.0044) or to participants in England, Finland, and Wales with up to 20 years follow-up whose information on cancer diagnoses was supplemented by national records (Supplementary Table S6; ITT analysis (HR, 0.40; 95% CI, 0.20–0.78; P = 0.0077); PP analysis (HR, 0.31; 95% CI, 0.12–0.77; P = 0.012). Importantly, there was no interaction between aspirin and RS treatments (Supplementary Table S4 shows the results for RS treatment with and without adjustment for aspirin).
All LS cancer outcomes
The HRs for all LS cancers were HR 0.76 (95% CI, 0.56–1.02; P = 0.066) and HR 0.80 (95% CI, 0.55–1.16; P = 0.24) for ITT and PP analyses, respectively (Table 3). However, the IRR was lower in those randomized to RS compared with placebo for both ITT (IRR, 0.69; 95% CI, 0.52–0.93; P = 0.014) and PP (IRR, 0.68; 95% CI, 0.47–0.99; P = 0.044) analyses (Table 3). Findings were less pronounced when analyses were restricted to all CAPP2 participants up to 10 years follow-up (Supplementary Table S5) but were stronger when restricted to participants in England, Finland, and Wales with up to 20 years follow-up (Supplementary Table S6). Details of the timing of the first LS cancer post study entry by years since randomization among participants are presented in Supplementary Table S8 and time to first LS cancer type is summarized in Supplementary Fig. S3. There was no interaction between aspirin and RS treatments; Supplementary Table S4 shows results for RS treatment with and without adjustment for aspirin.
Non-LS cancer outcomes
During follow-up, 45 and 44 non-LS cancers were diagnosed in participants randomized to RS and placebo, respectively (Table 1). There was no effect of RS on the risk of non-LS cancers in ITT (HR, 0.97; 95% CI, 0.64–1.47; P = 0.88), PP (HR, 0.96; 95% CI, 0.56–1.64; P = 0.89) or IRRs; ITT (IRR, 0.88; 95% CI, 0.56–1.40; P = 0.60) and PP (IRR, 0.97; 95% CI, 0.54–1.73; P = 0.92; Table 3). There was no interaction between aspirin and RS treatments (Supplementary Table S4 shows the marginal results for RS treatment with and without adjustment for aspirin). Further details of non-LS cancers occurring in the overall cohort are summarized by time since start of randomization in Supplementary Table S9.
Discussion
Randomization to RS for a mean of 25 months had no effect on colorectal cancer risk in patients with LS after long-term follow-up of the CAPP2 study in the test of our primary hypothesis. Our findings of no effect of RS on colorectal cancer risk in this long-term follow-up study are consistent with our findings of the interim follow-up at mean 53 months, which showed that RS had no detectable effect on colorectal cancer development in patients with LS (16). Dietary supplementation with RS for this limited time period does not emulate the apparently protective effect of diets rich in DF against colorectal cancer in the general population (16).
In contrast, those randomized to RS had significantly lower risk of diagnosis with non-colorectal LS cancers, our secondary hypothesis. This protective effect of RS was robust to both ITT and PP analyses and was evident in participants resident in England, Finland, and Wales for whom we had national registry follow-up for up to 20 years as well as in the whole CAPP2 study cohort with 10-year follow-up. There was no evidence of an effect of RS on endometrial cancer incidence (15 diagnoses in RS group, 16 in placebo group), the most common extracolonic site but, for all other anatomic sites, limited numbers precluded conclusions. However, an effect appeared particularly evident for upper GI cancers (including pancreatic, bile duct, stomach, and duodenal cancers) where we found 5 cancers in 5 participants in those on RS compared with 21 cancers in 17 controls.
Given their lower incidence, it is unsurprising that there is much less evidence from epidemiologic studies of associations between DF intake and risk of upper GI cancers than for colorectal cancer (7). However, findings from meta-analyses of data from case–control and prospective cohort studies suggest higher DF intake may lower risk of both stomach (21) and pancreatic (22) cancers. In a Japanese prospective cohort study, higher DF intake was associated with lower extrahepatic bile duct cancer (23) whereas in the EPIC study, higher DF was associated with reduced intrahepatic bile duct cancer but not with biliary tract cancer incidence (24).
Our unexpected finding has important implications for the management for patients with LS because surveillance for such cancers is challenging and survival after upper GI cancer diagnosis is much lower than for other LS cancers. For patients with LS diagnosed under 65 years, 5-year survival is 0%, 29%, 61%, and 67% for pancreatic, bile duct & gall bladder, stomach, and duodenal cancers, respectively, compared with 88% and 93% for colon and endometrial cancers, respectively (3). Overall, in a Finnish study, deaths due to upper GI cancers accounted for about 30% of non–colorectal cancer deaths in patients with LS (3).
RS is a component of DF (14) and prospective cohort studies provide strong evidence that higher DF intake is associated with lower colorectal cancer risk (6, 7). However, few intervention studies have tested the effects of higher DF intake on colorectal cancer risk. A recent meta-analysis of outcomes from 5 studies that tested the effect of DF on colorectal adenomatous polyps recurrence found no difference in the number of people with ≥1 adenoma (RR, 1.04; 95% CI, 0.95–1.13), >1 adenoma (RR, 1.06; 95% CI, 0.94–1.20), or ≥1 adenoma ≥1 cm (RR, 0.99; 95% CI, 0.82–1.20; ref. 25). The authors concluded that there is a lack of evidence from RCTs that increased DF reduces polyp recurrence but that the findings should be interpreted cautiously because of the relatively high rate of loss to follow-up and because polyp recurrence was used as a surrogate for colorectal cancer.
Our earlier randomized controlled trial (RCT) of colorectal cancer patients given RS, showed reduction of cell proliferation in the upper part of colonic crypts and changes in gene expression that were consistent with antineoplastic effects (26) Meta-analysis of findings from two studies that reported colorectal cancer outcomes at ≤4 years of intervention (27, 28) showed higher colorectal cancer risk in those randomized to DF (RR, 2.7; 95% CI, 1.07–6.85; ref. 25). However, there were few colorectal cancer events (23 among 2,794 participants) and the evidence was graded as low quality (25).
RS is fermented by multiple human colonic bacteria including members of the Ruminococcaceae, Lachnospiraceae, Erysipelotrichaceae, and Clostridiaceae families that are butyrate producers (29) and involves synergy between primary RS degraders and secondary starch scavengers (30). Butyrate suppresses cancer cell proliferation and may enhance apoptosis (31). In addition, cells defective in MMR may be more susceptible to the antineoplastic effects of butyrate (32). In the CAPP1 trial, we randomized 227 participants with familial adenomatous polyposis to RS or placebo for median 17 months (33). RS had no effect on polyp number or size but colorectal mucosal crypt length diminished in those randomized to RS (33). There is evidence from short-term mechanistic studies that RS and/ or its fermentation end products is antineoplastic; for example, in a well-controlled human intervention study in which healthy adults consumed high intakes of red meat (a risk factor for bowel cancer) for 4 weeks, supplementation with RS reduced multiple biomarkers of cancer risk, including the pattern of expression of oncogenic microRNAs and reduction of red-meat induced O6-methyl-2-deoxyguanosine adducts (34).
An indirect effect of RS on the immune response to a highly immunogenic tumor could explain the effect on the wide spectrum of non–colorectal cancer cancers although this does not account for the lack of an effect in the colon or endometrium. The mechanisms through which RS appears to have a protective effect on upper GI tumors are not apparent. In a xenograft pancreatic cancer mouse model, RS reduced tumor growth and expression of the cell proliferation marker Ki67 in tumors (35). Very recent studies in mice have revealed a central role for butyrate (a fermentation product derived from RS) in reversing the progression of necrotizing pancreatitis (36). Although the causal links remain unclear, pancreatitis appears to increase risk of pancreatic cancer (37). There is, although, no suggestion that pancreatitis is a feature of LS.
One possible explanation for our findings could be an effect of RS on total and, especially, unconjugated secondary bile acids. Bile salts exiting the terminal ileum into the colon are exposed to bile salt hydrolases (expressed by multiple intestinal bacteria) and metabolized to secondary bile acids (38); these can promote carcinogenesis (39) by inducing cancer stem cells (40). Intervention studies in both healthy volunteers (41) and participants with recent colorectal adenomas, showed that RS reduced fecal concentrations of total and secondary bile acids (42). Lower secondary bile acids may result from RS-induced changes in bile acid metabolism by the gut microbiota but RS can also change bile acid patterns through pathways independent of the microbiome (43).
There is growing evidence that pancreatic cancer is associated with distinctive changes in the gut microbiome (38), but to date, it is unclear whether those changes are causes or consequences of the disease. If they are causal, then manipulation of the microbiome via RS (44) may offer potential for reduced risk of this difficult cancer.
Antineoplastic effects may also be mediated via microbial modulation of immune homeostasis (45). This was demonstrated in experimental studies showing differential stimulation of Toll-like receptors and attenuation of proinflammatory cytokines in dendritic cells (46). Although the mechanisms through which RS reduces risk of upper GI cancer remain to be discovered, it is likely that they involve the gut microbiota since, by definition, RS is not digested in the small bowel but is fermented to SCFA by the commensal bacteria in the large bowel (14).
The consensus statement from the International Cancer Microbiome Consortium (ICMC) concluded that, despite mechanistic and supporting evidence from animal and human studies, there is currently no direct evidence that the human commensal microbiome is a key determinant in the etiopathogenesis of cancer (47). However, the recent discovery that some colorectal cancer cases may be due to exposure to bacteria carrying the colibactin-producing pks pathogenicity island (48), which induces chromosomal instability and DNA damage (49), indicates a novel mechanism through which dietary factors may influence colorectal cancer risk. The ICMC concluded that the microbiome represents one apex of a tripartite, multidirectional interactome [the other apices are environmental factors (including diet) and host epigenetic/genetic vulnerability] that drives carcinogenesis (47). Our finding that a RS supplement reduced upper GI cancers in patients with LS, who are at higher genetic susceptibility, should prompt further mechanistic investigation.
A recent analysis of the NHANES 2015 to 2016 survey suggested that American adults eat, on average, 4.0 g RS/day (50) The supplement used in CAPP2 delivered a daily dose of RS equivalent to eating a green tipped banana. Thus, the potential health benefits observed in this intervention study might be achievable in the wider population of LS gene carriers with a modest dietary change.
A major strength of this study was that blinded follow up was sustained to the planned 10-year follow-up from recruitment, supplemented by reliable national registry data in England, Wales, and Finland. We found strong evidence of lack of effect of RS on colorectal cancer risk and a clearly significant reduction in other LS cancers. Possible mechanisms are explored but these could not be investigated in this study in the absence of a suitable biobank.
A weakness of these results is that our original hypothesis focused on colorectal cancer where no effect was found. Detection of an effect on other LS cancers so long after a relatively brief intervention is surprising but not impossible; mutagens can damage stem cells and lead to malignancy many years later, especially where DNA repair mechanisms are impaired.
In conclusion, we found no evidence that RS alters colorectal cancer risk in LS but those randomized to RS have significantly lower risk of non–colorectal cancer LS cancers, especially upper GI cancers. Given that diagnosis and management of these cancers is difficult, this finding has substantial potential benefits for patients with LS. Furthermore, the possibility that RS, and by analogy other forms of DF, may reduce upper GI cancers in the wider population should be investigated in large-scale prospective cohort studies.
Supplementary Material
Acknowledgments
J. Burn, D.T. Bishop, and J.C. Mathers received grants from Cancer Research UK, European Commission, Medical Research Council, and National Institute for Health Research.
We dedicate this work to the memory of our late friends and colleagues Henry Lynch, Doug Altman, and Lynn Faulds Wood. They made major contributions respectively to the design, analysis, and conduct of this study. The CAPP2 trial was made possible by the dedicated efforts of Pam Chapman and Gail Barker together with the commitment of the participants and the Research Staff at all of the CAPP2 UK and international sites, with special thanks to Pascale Ives (retired). We thank the other CAPP2 Investigators including:
Prof. Alex Boussioutas MD, University of Melbourne, Peter MacCallum Cancer Centre, Royal Melbourne Hospitals, Melbourne, Australia; Dr Carole Brewer MD, Royal Devon and Exeter NHS Foundation Trust, Exeter, UK; Dr Jackie Cook, MD Sheffield Children's Hospital, Sheffield Children's NHS Foundation Trust, Sheffield, UK; Prof Diana Eccles MD, Faculty of Medicine, University of Southampton, Southampton, UK; Dr Anthony Ellis MD, Department of Medicine, University of Liverpool & Department of Gastroenterology, Royal Liverpool University Hospital, Liverpool, UK; Prof Shirley V Hodgson MD, Emeritus, St Georges, London, UK; Prof Jan Lubinski MD, Department of Genetics and Pathology, Pomeranian Medical University, Szczecin, Poland; Prof Eamonn R Maher MD, University of Cambridge, NIHR Cambridge Biomedical Research Centre, Cancer Research UK Cambridge Biomedical Campus, Cambridge, UK; Dr Mary EM Porteous MD, University of Edinburgh, SE Scotland Genetics Service, Edinburgh, UK; Prof Julian Sampson MD, Division of Cancer and Genetics, School of Medicine, Cardiff University, Cardiff, UK; Prof Rodney J Scott PhD, Discipline of Medical Genetics, University of Newcastle, NSW, Australia & Hunter Medical Research Institute & Division of Molecular Medicine, NSW Health Pathology North, John Hunter Hospital, NSW, Australia; Dr Lucy Side MD, Wessex Clinical Genetics Service, University Hospitals Southampton, UK. Our thanks to the following investigators: Dr Marie Luise Bisgaard, Dr Carol Chu, Dr Paulo Fidalgo, Prof Steven Gallinger, Dr Tessa Homfray, Dr Pierre Hutter, Prof Julio Leite, Dr James MacKay, Prof Christopher G Marks, Mr Anthony Miles, Dr Vicky Murday, Dr Cristina Oliani, Dr Sylviane Olschwang, Dr Pedro Perez Segura, Dr Gabriella Pichert, Prof Andre-Pascale Sappino, Dr Alfonso Tempesta, Prof Hans FA Vasen, Dr Ian Walpole. We acknowledge the contribution of the late Caroline Langman. Our thanks to Dr Brian Shand and Andrew Bacon, Public Health England, UK for their expertise in developing the pseudonymisation code. We acknowledge support from Bayer Pharma Ag, the National Starch & Chemical Company and the Barbour Foundation. We also acknowledge the contribution of TrakGene Genetics Information Management Solutions (www.trakgene.com) for providing the database software supporting this trial.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
Footnotes
Note: Supplementary data for this article are available at Cancer Prevention Research Online (http://cancerprevres.aacrjournals.org/).
Authors' Disclosures
J.C. Mathers reports grants from Medical Research Council and Cancer Research UK and nonfinancial support from National Stach and Bayer during the conduct of the study. F. Macrae reports grants from Cancer Council of Victoria, NSW Cancer Council, SA Cancer Council, and Queensland Cancer Fund, and nonfinancial support from Bayer during the conduct of the study. T.T. Seppälä reports personal fees from Boehringer Ingelheim Finland and Amgen Finland, grants from Jane and Aatos Erkko Foundation, Sigrid Juselius Foundation, Emil Aaltonen Foundation, Relander Foundation, Academy of Finland, Cancer Society Finland, Finnish Medical Foundation, Instrumentarium Science Foundation, and iCAN Precision Medicine Flagship of the Academy of Finland outside the submitted work and is the CEO and co-owner of Healthfund Finland. No disclosures were reported by the other authors.
Authors' Contributions
J.C. Mathers: Writing–review and editing. F. Elliott: Formal analysis. F. Macrae: Principal investigator. J.-P. Mecklin: Principal investigator. G. Möslein: Principal investigator. F.E. McRonald: Formal analysis. L. Bertario: Principal investigator. D.G. Evans: Principal investigator. A. Gerdes: Principal investigator. J.W. Ho: Principal investigator. A. Lindblom: Principal investigator. P.J. Morrison: Principal investigator. J. Rashbass: Formal analysis. R.S. Ramesar: Principal investigator. T.T. Seppälä: Principal investigator. H.J. Thomas: Principal investigator. H.J. Sheth: Data analysis. K. Pylvänäinen: Project administration. L. Reed: Project administration. G.M. Borthwick: Writing–review and editing. D.T. Bishop: Formal analysis. J. Burn: Conceptualization, funding acquisition, writing–review and editing.
References
- 1. Vasen HF, Moslein G, Alonso A, Bernstein I, Bertario L, Blanco I, et al. Guidelines for the clinical management of Lynch syndrome (hereditary non-polyposis cancer). J Med Genet 2007;44:353–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Colorectal cancer NICE guideline [NG151] Published: 29 January 2020. [cited 2022 June 22]. Available from: https://www.nice.org.uk/guidance/NG151.
- 3. Moller P, Seppala TT, Bernstein I, Holinski-Feder E, Sala P, Gareth Evans D, et al. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the prospective lynch syndrome database. Gut 2018;67:1306–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Burkitt DP, Walker AR, Painter NS. Effect of dietary fibre on stools and the transit-times, and its role in the causation of disease. Lancet 1972;2:1408–12. [DOI] [PubMed] [Google Scholar]
- 5. Park Y, Hunter DJ, Spiegelman D, Bergkvist L, Berrino F, van den Brandt PA, et al. Dietary fiber intake and risk of colorectal cancera pooled analysis of prospective cohort studies. JAMA 2005;294:2849–57. [DOI] [PubMed] [Google Scholar]
- 6. Reynolds A, Mann J, Cummings J, Winter N, Mete E., Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet North Am Ed 2019;393:434–45. [DOI] [PubMed] [Google Scholar]
- 7. WCRF/AICR. Diet Nutrition, Physical Activity and Cancer: a global perspective. The Third Expert Report. Continuous Update Project. World Cancer Research Fund /American Institute for Cancer Research;2018.
- 8. Yang W, Ma Y, Liu Y, Smith-Warner SA, Simon TG, Chong DQ, et al. Association of intake of whole grains and dietary fiber with risk of hepatocellular carcinoma in US adults. JAMA Oncol 2019;5:879–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williams EA, Coxhead JM, Mathers JC. Anti-cancer effects of butyrate: use of micro-array technology to investigate mechanisms. Proc Nutr Soc 2003;62:107–15. [DOI] [PubMed] [Google Scholar]
- 10. O'Keefe SJD, Kidd M, Espitalier-Noel G, Owira P. Rarity of colon cancer in africans is associated with low animal product consumption, not fiber. Am J Gastroenterol 1999;94:1373–80. [DOI] [PubMed] [Google Scholar]
- 11. Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. BMJ 2018;361:k2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med 2016;375:2369–79. [DOI] [PubMed] [Google Scholar]
- 13. Burn J, Bishop DT, Mecklin JP, Macrae F, Moslein G, Olschwang S, et al. Effect of aspirin or resistant starch on colorectal neoplasia in the Lynch syndrome. N Engl J Med 2008;359:2567–78. [DOI] [PubMed] [Google Scholar]
- 14. DeMartino P, Cockburn DW. Resistant starch: impact on the gut microbiome and health. Curr Opin Biotechnol 2020;61:66–71. [DOI] [PubMed] [Google Scholar]
- 15. Rothwell PM, Wilson M, Price JF, Belch JF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet 2012;379:1591–601. [DOI] [PubMed] [Google Scholar]
- 16. Mathers JC, Movahedi M, Macrae F, Mecklin J-P, Moeslein G, Olschwang S, et al. Long-term effect of resistant starch on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet Oncol 2012;13:1242–9. [DOI] [PubMed] [Google Scholar]
- 17. Burn J, Sheth H, Elliott F, Reed L, Macrae F, Mecklin J-P, et al. Cancer prevention with aspirin in hereditary colorectal cancer (Lynch syndrome), 10-year follow-up and registry-based 20-year data in the CAPP2 study: a double-blind, randomised, placebo-controlled trial. Lancet North Am Ed 2020;395:1855–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. NHS Digital National Disease Registration Service (NDRS) [cited 2022 June 22]. Available from: https://digital.nhs.uk/services/national-disease-registration-service.
- 19. Lunkka P, Malila N, Ryynanen H, Heikkinen S, Sallinen V, Koskenvuo L. Accuracy of finnish cancer registry colorectal cancer data: a comparison between registry data and clinical records. Scand J Gastroenterol 2021;56:247–51. [DOI] [PubMed] [Google Scholar]
- 20. ISRCTN Registry 59521990 A randomised controlled trial of colorectal polyp and cancer prevention using aspirin and resistant starch in carriers of hereditary nonpolyposis colorectal cancer [cited 2022 June 22]. Available from: http://www.isrctn.com/ISRCTN59521990.
- 21. Zhang Z, Xu G, Ma M, Yang J, Liu X. Dietary fiber intake reduces risk for gastric cancer: a meta-analysis. Gastroenterology 2013;145:113–20. [DOI] [PubMed] [Google Scholar]
- 22. Wang C-H, Qiao C, Wang R-C, Zhou W-P. Dietary fiber intake and pancreatic cancer risk: a meta-analysis of epidemiologic studies. Sci Rep 2015;5:10834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Makiuchi T, Sobue T, Kitamura T, Ishihara J, Sawada N, Iwasaki M, et al. The relationship between vegetable/fruit consumption and gallbladder/bile duct cancer: A population-based cohort study in Japan. Int J Cancer 2017;140:1009–19. [DOI] [PubMed] [Google Scholar]
- 24. Fedirko V, Lukanova A, Bamia C, Trichopolou A, Trepo E, Nöthlings U, et al. Glycemic index, glycemic load, dietary carbohydrate, and dietary fiber intake and risk of liver and biliary tract cancers in Western Europeans. Ann Oncol 2013;24:543–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yao Y, Suo T, Andersson R, Cao Y, Wang C, Lu J, et al. Dietary fibre for the prevention of recurrent colorectal adenomas and carcinomas. Cochrane Database Syst Rev 2017;1:Cd003430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dronamraju SS, Coxhead JM, Kelly SB, Burn J, Mathers JC. Cell kinetics and gene expression changes in colorectal cancer patients given resistant starch: a randomised controlled trial. Gut 2009;58:413–20. [DOI] [PubMed] [Google Scholar]
- 27. Alberts DS, Martínez ME, Roe DJ, Guillén-Rodríguez JM, Marshall JR, van Leeuwen JB, et al. Lack of effect of a high-fiber cereal supplement on the recurrence of colorectal adenomas. N Engl J Med 2000;342:1156–62. [DOI] [PubMed] [Google Scholar]
- 28. Schatzkin A, Lanza E, Corle D, Lance P, Iber F, Caan B, et al. Lack of effect of a low-fat, high-fiber diet on the recurrence of colorectal adenomas. N Engl J Med 2000;342:1149–55. [DOI] [PubMed] [Google Scholar]
- 29. Louis P, Flint HJ. Formation of propionate and butyrate by the human colonic microbiota. Environ Microbiol 2017;19:29–41. [DOI] [PubMed] [Google Scholar]
- 30. Cerqueira FM, Photenhauer AL, Pollet RM, Brown HA, Koropatkin NM. Starch digestion by gut bacteria: crowdsourcing for carbs. Trends Microbiol 2020;28:95–108. [DOI] [PubMed] [Google Scholar]
- 31. Bordonaro M, Lazarova DL, Sartorelli AC. Butyrate and Wnt signaling: a possible solution to the puzzle of dietary fiber and colon cancer risk? Cell Cycle 2008;7:1178–83. [DOI] [PubMed] [Google Scholar]
- 32. Dronamraju SS, Coxhead JM, Kelly SB, Mathers JC. Differential antineoplastic effects of butyrate in cells with and without a functioning DNA mismatch repair. Nutr Cancer 2009;62:105–15. [DOI] [PubMed] [Google Scholar]
- 33. Burn J, Bishop DT, Chapman PD, Elliott F, Bertario L, Dunlop MG, et al. A randomized placebo-controlled prevention trial of aspirin and/or resistant starch in young people with familial adenomatous polyposis. Cancer Prev Res 2011;4:655–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Le Leu RK, Winter JM, Christophersen CT, Young GP, Humphreys KJ, Hu Y, et al. Butyrylated starch intake can prevent red meat-induced O6-methyl-2-deoxyguanosine adducts in human rectal tissue: a randomised clinical trial. BrJNutr 2015;114:220–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Panebianco C, Adamberg K, Adamberg S, Saracino C, Jaagura M, Kolk K, et al. Engineered resistant-starch (ERS) diet shapes colon microbiota profile in parallel with the retardation of tumor growth in in vitro and in vivo pancreatic cancer models. Nutrients 2017;9:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. van den Berg FF, van Dalen D, Hyoju SK, van Santvoort HC, Besselink MG, Wiersinga WJ, et al. Western-type diet influences mortality from necrotising pancreatitis and demonstrates a central role for butyrate. Gut 2020:gutjnl–2019–320430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 2013;144:1252–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kartal E, Schmidt TSB, Molina-Montes E, Rodriguez-Perales S, Wirbel J, Maistrenko OM, et al. A faecal microbiota signature with high specificity for pancreatic cancer. Gut 2022;71:1359–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Louis P, Hold GL, Flint HJ. The gut microbiota, bacterial metabolites and colorectal cancer. Nat Rev Microbiol 2014;12:661–72. [DOI] [PubMed] [Google Scholar]
- 40. Farhana L, Nangia-Makker P, Arbit E, Shango K, Sarkar S, Mahmud H, et al. Bile acid: a potential inducer of colon cancer stem cells. Stem Cell Res Ther 2016;7:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hylla S, Gostner A, Dusel G, Anger H, Bartram H-P, Christl SU, et al. Effects of resistant starch on the colon in healthy volunteers: possible implications for cancer prevention. Am J Clin Nutr 1998;67:136–42. [DOI] [PubMed] [Google Scholar]
- 42. Grubben MJAL, CCMvd B, Essenberg M, Olthof M, Tangerman A, Katan MB, et al. Effect of resistant starch on potential biomarkers for colonic cancer risk in patients with colonic adenomas. Dig Dis Sci 2001;46:750–6. [DOI] [PubMed] [Google Scholar]
- 43. Bindels LB, Gomes-Neto JC, Mutemberezi V, Martínez I, Salazar N, et al. Resistant starch can improve insulin sensitivity independently of the gut microbiota. Microbiome 2017;5:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dobranowski PA, Stintzi A. Resistant starch, microbiome, and precision modulation. Gut Microbes 2021;13:1926842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schramm C. Bile acids, the microbiome, immunity, and liver tumors. N Engl J Med 2018;379:888–90. [DOI] [PubMed] [Google Scholar]
- 46. Bermudez-Brito M, Rosch C, Schols HA, Faas MM, de Vos P. Resistant starches differentially stimulate toll-like receptors and attenuate proinflammatory cytokines in dendritic cells by modulation of intestinal epithelial cells. Mol Nutr Food Res 2015;59:1814–26. [DOI] [PubMed] [Google Scholar]
- 47. Scott AJ, Alexander JL, Merrifield CA, Cunningham D, Jobin C, Brown R, et al. International Cancer Microbiome Consortium consensus statement on the role of the human microbiome in carcinogenesis. Gut 2019;68:1624–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pleguezuelos-Manzano C, Puschhof J, Rosendahl Huber A, van Hoeck A, Wood HM, Nomburg J, et al. Mutational signature in colorectal cancer caused by genotoxic pks+ E. coli. Nature 2020;580:269–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Faïs T, Delmas J, Barnich N, Bonnet R, Colibactin DG.: More than a new bacterial toxin. Toxins 2018;10:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Miketinas DC, Shankar K, Maiya M, Patterson MA. Usual dietary intake of resistant starch in US adults from NHANES 2015–2016. J Nutr 2020;150:2738–47. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data were generated by the authors and requests for access to data should be made to the corresponding author (J.C. Mathers).