Abstract
Background
The type of pre-existing disorder might determine changes in mental health symptoms (i.e., anxiety, depression) during the COVID-19 pandemic and influence the effect of psychological factors (e.g., social support, resilience, stress) on such symptoms.
Methods
Longitudinal data from two assessments (June-2020 and February/March-2021) collected through telephone interviews (Spanish general population) were analysed. Outcome variables included anxiety (GAD-7) and depressive symptoms (PHQ-8). Psychological factors included COVID-perceived stress (adapted COVID-perceived risk scale), social support (OSSS-3), and resilience (CD-RISC). Pre-existing mental conditions (3 groups: mood, anxiety, and comorbid depression+anxiety) were assessed using the CIDI checklist. Changes in anxiety and depressive symptoms between baseline and follow-up were assessed with the paired samples Wilcoxon test. Tobit regression and interaction models were conducted to test associations between psychological factors and these symptoms in follow-up.
Results
Final sample included 1942 participants (mean age 49.6 yrs., ±16.7; 51.7 % females). Anxiety symptoms increased in all groups except for those with pre-existing mood conditions. Depressive symptoms only increased in those without pre-existing mental disorders and in those with pre-existing anxiety. Higher baseline resilience, increases in social support, and decreases in COVID-perceived stress were associated with lower anxiety and depressive symptoms. The type of pre-existing mental disorder did not modify these associations.
Limitations
Lack of pre-pandemic data and the limited number of pre-existing mental conditions.
Conclusions
Having pre-pandemic mental disorders is associated with different patterns of anxiety and depressive symptoms during the pandemic. COVID-related stress, social support, and resilience are key factors in improving mental health regardless of the mental diagnosis.
Keywords: Affective disorders, SARS-CoV-2, Social support, Resilience, Stress
1. Introduction
In addition to being a public health emergency, COVID-19 has also had a detrimental impact on global mental health (González-Sanguino et al., 2020; Vindegaard and Benros, 2020; Wang et al., 2020; Wu et al., 2021). In general, the evidence indicates that compared to pre-pandemic data, a notable increase in the prevalence of mental health symptoms was observed during the early phase of the global pandemic (March–July 2020) (Cénat et al., 2021; Schafer et al., 2022; Wu et al., 2021). Nonetheless, according to a recent meta-analysis of longitudinal cohort studies (n = 65 studies), this increase was short-lived and by mid-2020 mental distress decreased to pre-pandemic levels for most symptom types (anxiety symptoms and general mental health, but not for depressive symptoms) (Robinson et al., 2022).
People with pre-existing mental disorders are not only at increased risk for COVID-19 infection (Taquet et al., 2021), but are also particularly vulnerable to the mental health threat of the pandemic (Moreno et al., 2020). Indeed, several studies conducted during the COVID-19 pandemic outbreak stated that having a pre-existing mental disorder was a risk factor for increased levels of anxiety and depression (Fancourt et al., 2021; Vindegaard and Benros, 2020; Xiong et al., 2020) and that there might be a differential mental health impact across types of pre-existing mental problems (Tamsyn et al., 2020). In addition, there is some longitudinal evidence suggesting that the type of pre-existing mental disorder could predict different levels or changes of anxiety and depressive symptoms over the course of the pandemic. For instance, a study conducted in Germany in March–June 2020 (n = 2376) found that depressive and anxiety symptoms were greater in individuals with comorbid depression and anxiety (D + A) than in individuals with pure anxiety or depression (Bendau et al., 2021). However, most of the evidence is based on the first phase of the pandemic, and longer longitudinal studies are needed to determine the middle-term implications of the COVID-19 pandemic on the population's mental health and, particularly, on those with pre-existing mental health conditions.
Previous studies have identified a variety of psychological factors that may be key determinants for maintaining psychological health during the COVID-19 pandemic such as lower levels of COVID-19 stressors (Abdalla et al., 2021), and greater social support and resilience (Chen et al., 2021; Guo et al., 2021; Liu et al., 2020). Nevertheless, while the significance of these psychological factors during the COVID-19 pandemic is well established for the general population (Serafini et al., 2020), relatively little is known about their clinical significance in patients with pre-existing disorders, and how these may differ according to psychiatric diagnosis. For instance, one study reported that people with pre-existing anxiety-related disorders had higher COVID-related stress than those with mood disorders and no mental disorders during the COVID-19 outbreak (Asmundson et al., 2020). However, it is not well understood whether the type of pre-existing disorder may influence the association between psychological factors and mental health outcomes (i.e., anxiety and depressive symptoms). These are important research gaps, since the identification of these factors is essential to the design of transdiagnostic or disorder-specific intervention strategies.
In this context, the aim of this study was to examine whether the type of pre-existing mental disorder moderated changes and levels of anxiety and depressive symptoms from June 2020 (baseline) to February–March 2021 (follow-up). In addition, we aimed to determine whether the type of pre-existing mental disorder influenced the associations between the aforementioned psychological factors (COVID-related stress, social support, resilience), and anxiety and depression at follow-up.
2. Methods
2.1. Study design and population
The MINDCOVID research project includes a population-based survey of adults residing in Spain; it aims to study the impact of the COVID-19 pandemic on mental health (“MINDCOVID project”, 2020). The current analysis was based on two consecutive assessments: baseline (June 1–30, 2020) and follow-up (February 18–March 12, 2021). The first assessment took place at the end of lockdown in Spain, when COVID-19 infection and mortality rates were low and most of the restrictions had been lifted. Conversely, the second assessment took place at the end of the third wave of infection in Spain. In that period, people had experienced two waves of high infection and mortality rates, tight restrictions were still on (e.g., curfew and limited geographical mobility), and the vaccination campaign had started. Full details of the surveys and their sampling procedure have been described elsewhere (Domènech-Abella et al., 2021; Mortier et al., 2021). In brief, the eligible sample consisted of non-institutionalized adults aged ≥18 that had no language barriers to Spanish and had access to a mobile phone or landline telephone. Baseline assessment and follow-up were conducted by professional interviewers via computer-assisted telephone. For baseline, the sample was drawn using dual-frame random digit dialling including mobile and landline. The sample distribution was planned according to quotas proportional to the Spanish population in terms of age group, gender, and region of residence, with all regions represented (National Institute of Statistics in Spain, July 2019). The cooperation rate (i.e., the proportion of individuals interviewed among all eligible callers) was 16.5 %. Of those who took part at baseline (n = 3500), 57 % completed the follow-up survey (n = 2000). Ethical approval was obtained from corresponding research committees, and oral consent was obtained from all participants.
2.2. Depressive and anxiety symptoms (outcome variables)
The Spanish version of the 7-item Generalized Anxiety Disorder Scale (GAD-7) (García-Campayo et al., 2010; Spitzer et al., 2006) was employed to screen for anxiety. GAD-7 scores range from 0 to 21, with higher scores indicating higher levels of anxiety symptoms. The Spanish version of the Patient Health Questionnaire Depression Scale (PHQ-8) (Kroenke et al., 2009; Muñoz-Navarro et al., 2017) was used to assess depressive symptoms, with higher scores indicating greater depressive symptoms (range 0–24). Anxiety and depressive symptoms were measured both at baseline and in follow-up.
2.3. Pre-existing mental health conditions
The presence of pre-existing mental disorders was assessed using a checklist based on the Composite International Diagnostic Interview (CIDI) (Kessler and Üstün, 2004), which screens for self-reported lifetime depressive disorder, bipolar disorder, anxiety disorders, panic attacks, alcohol and drug use disorders, and other mental disorders. A 4-level variable was created for the type of pre-existing disorder: no disorder, only mood disorders (depressive and/or bipolar disorders), only anxiety disorders (including crisis and/or panic attacks), and comorbid D + A (depressive and anxiety disorders). Those with pre-existing substance abuse disorders, comorbid bipolar and anxiety disorders, and other mental disorders were excluded from the current study due to the small sample size (n = 36, n = 8 and n = 14, respectively).
2.4. Psychological factors and covariates
COVID-perceived stress was assessed at baseline and in follow-up using an adapted version of the COVID-19 perceived risk scale (Wu et al., 2009), which included 4 items related to concerns about being infected, infecting loved ones, dying due to COVID-19, and loved ones' concerns about infecting them. Each item was rated on a 5-level scale ranging from very intense to no stress. The total score was obtained by adding all responses (0–16), with higher scores reflecting greater levels of COVID-perceived stress. Social support was also assessed both at baseline and in follow-up, using the 3-item Oslo Social Support Scale (OSSS-3) (Kocalevent et al., 2018) (range 0—11), with higher scores representing higher levels of social support. Lastly, resilience was evaluated only at baseline using the 10-item Connor-Davidson Resilience Scale (CD-RISC), in which higher scores represent greater resilience (range 0–40). The authors describe resilience as personal qualities that enable a person to thrive in the face of adversity (Connor and Davidson, 2003).
To account for changes in the COVID-perceived stress and the social support between the two time points, the variables “change in COVID-perceived stress” and “change in social support” were calculated as the difference between the levels of COVID-perceived stress in follow-up and at baseline, and the levels of social support in follow-up and at baseline, respectively. Thus, positive values for these variables indicate increases in COVID-perceived stress and social support, respectively. The included covariates were age at baseline and gender.
2.5. Statistical analysis
To compensate for potential survey non-response bias in follow-up and ensure sample representativeness, data were weighted with inverse probability weights (IPW) (Seaman and White, 2013), obtained as the inverse of the probability of completing the follow-up survey on observed related baseline covariates, estimated using a logistic regression model, and with post-stratification weights to restore the distribution of the adult general population of Spain according to age groups, sex and geographic area. Missing item-level data were minimal (6.5 %) and were addressed using multivariate fully conditional specification methods, where imputations for each variable were created by drawing from iterated conditional models (van Buuren, 2018). No significant differences in demographic characteristics were observed between participants with complete data and those excluded because of missing data.
Descriptive analyses were conducted to characterize the study sample. These analyses included unweighted frequencies, weighted proportions, and weighted mean age and standard deviation. The paired samples Wilcoxon test was used to determine whether there were significant differences in anxiety, depressive, COVID-perceived stress, and social support levels between the two waves of data collection.
Tobit models are suitable to test for dependent variables which are not normally distributed, and a large number of responses are piled up at the lowest or highest values due to insufficient range of measurement of the given instrument (McBee, 2010). The model yields theoretically continuous values normally distributed through maximum likelihood estimates for censored values while using a standard linear model for the remaining values (Long, 1997). In our case, the Tobit approach assumes that several responses are censored at the lowest value because the measured categories are not sufficiently detailed to detect latent values in anxiety and depression scales. Approximately 17.2 % of our sample accumulated at the lowest score of anxiety or depression (0), and around 41.8 % among the three lowest values (0, 1 and 2). The rest of the sample was distributed among the remaining values, and the frequencies gradually decreased towards the highest values (21 for GAD-7 and 24 for PHQ-8).
First, univariate Tobit regression models were performed to analyse the unadjusted associations between the two outcomes (anxiety and depressive symptoms at follow-up) and the following variables: age, gender, type of pre-existing mental disorder, change in COVID-perceived stress, and change in social support and resilience (all of them adjusted by outcomes at baseline). Then, to analyse the influence of the type of pre-existing mental disorder on the outcomes, multivariate Tobit regression models were run adjusting for age, gender, and baseline levels of anxiety and depressive symptoms.
Finally, to determine whether the type of pre-existing mental disorder modified the association between the psychological factors and anxiety and depressive symptoms in follow-up, several interactional models were run for depressive and anxiety symptoms separately, as follows: resilience*pre-existing mental disorder, change in social support*pre-existing mental disorder, and change in COVID-perceived stress*pre-existing mental disorder. Models for change in COVID-perceived stress and change in social support were also adjusted for baseline COVID-perceived stress and baseline social support, respectively. Results from Tobit regression models are presented as unstandardized coefficients and standard errors (SE).
The level of statistical significance was set at p < 0.05. Statistical analyses were performed with Stata 14.1 (Stata Corp LP, College Station, Texas) and R (version 4.1.0).
3. Results
The final sample included 1942 participants who completed both assessments. The socio-demographic characteristics of the study sample are shown in Table 1 . 67 % of individuals reported no pre-existing mental disorders, 3.6 % reported having pre-existing mood disorders, 20.4 % pre-existing anxiety, and 9 % comorbid D + A. Mean age was 49.6 years (SD: 16.7), and 51.7 % were female.
Table 1.
Characteristics of study population.
| Overall (n = 1942) |
No disorder (n = 1303) |
Pre-existing anxiety (n = 397) |
Pre-existing mood disorders (n = 70) |
Pre-existing D + A (n = 172) |
||
|---|---|---|---|---|---|---|
| Age, mean (SD) | 49.5 (16.70) | 50.78 (16.85) | 43.67 (15.83) | 56.33 (13.98) | 51.05 (15.28) | |
| Gender, n (%) | Male | 861 (48.30) | 629 (48.27) | 149 (42.47) | 30 (47.19) | 53 (33.96) |
| Female | 1081 (51.70) | 674 (51.72) | 248 (57.53) | 40 (52.81) | 119 (66.04) | |
| COVID-perceived stress, mean (SD) | Baseline | 5.02 (3.64) | 4.8 (3.63) 4.28 (3.39)*** |
5.7 (3.57) | 4.49 (3.62) | 5.37 (3.60) |
| Follow-up | 4.52 (3.47)*** | 5.16 (3.51)* | 4.29 (3.6) | 4.94 (3.73) | ||
| Social support, mean (SD) | Baseline | 8.13 (1.86) | 8.28 (1.76) 8.12 (1.90)*** |
7.93 (1.99) | 7.92 (1.77) | 7.58 (2.12) |
| Follow-up | 7.97 (1.96)*** | 7.85 (1.84) | 7.61 (2.33) | 7.28 (2.31) | ||
| Resilience, mean (SD) | Baseline | 33 (6.00) | 33.79 (5.72) | 31.91 (5.66) | 32.32 (5.80) | 29.95 (7.33) |
| Outcomes | ||||||
| Anxiety symptoms, mean (SD) | Baseline | 3.45 (4.07) | 2.62 (3.44) 3.33 (3.96)*** |
4.76 (4.20) | 4.24 (4.40) | 6.38 (5.52) |
| Follow-up | 4.12 (4.46)*** | 5.27 (4.60)* | 4.78 (4.99) | 7.15 (5.50)* | ||
| Depressive symptoms, mean (SD) | Baseline | 3.79 (4.44) | 2.86 (3.79) 3.47 (4.21)*** |
4.94 (4.20) | 5.18 (4.91) | 7.59 (6.24) |
| Follow-up | 4.34 (4.71)*** | 5.44 (4.72)* | 5.84 (4.95) | 7.64 (5.86) |
Unweighted frequencies and weighted proportions are displayed for categorical variables. Weighted mean and standard deviation (SD) are shown for continuous variables. Differences between baseline and follow-up variables (p values) were obtained with the paired samples Wilcoxon test. D + A: Depression and anxiety.
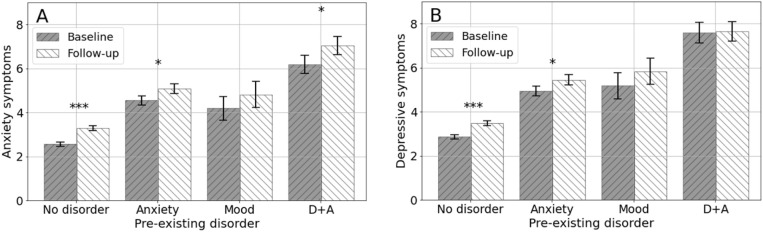
Anxiety and depressive symptoms significantly increased from baseline to follow-up. Nevertheless, as illustrated in Fig. 1 , after stratifying for each type of pre-existing mental disorder we observed that not all the subgroups experienced an increase in symptoms. A statistically significant increase in anxiety levels was observed for those with anxiety disorders, comorbid D + A, and no pre-existing mental disorder, but not for those with mood disorders. Regarding depressive symptoms, only those with no pre-existing disorder and pre-existing anxiety experienced a significant increase in symptomatology. Median difference of anxiety and depressive symptoms between baseline and follow-up for each type of pre-existing disorder is also represented in Supplementary Fig. 1.
Fig. 1.
Mean anxiety symptoms (A) and mean depressive symptoms (B) in the two waves of data collection by type of pre-existing mental disorder. Error bars show standard errors of the means. P-values were obtained with the paired samples Wilcoxon test, *p < 0.05, **p < 0.01, ***p < 0.001. Anxiety symptoms were measured with GAD-7; depressive symptoms were measured with PHQ-8. D + A: depression and anxiety.
Results of univariate analysis are presented in Supplementary table 1. Table 2 presents multivariate models of the associations between type of pre-existing mental disorder, and anxiety and depressive symptoms at follow-up, adjusting for covariates. Compared to those with no pre-existing mental conditions, having pre-existing anxiety disorders and pre-existing comorbid D + A were factors significantly associated with higher levels of anxiety symptoms. Having a pre-existing mood disorder was not significantly associated with anxiety. Furthermore, all types of pre-existing mental disorders were significantly associated with higher levels of depressive symptoms, compared to those with no pre-existing mental disorder. For both outcomes, those with comorbid D + A were the group with the strongest associations.
Table 2.
Adjusted Tobit regression models of the associations between type of pre-existing mental disorder, and anxiety and depressive symptoms.
| Anxiety symptoms Coef (SE) |
p-Value | Depressive symptoms Coef (SE) |
p-Value | |
|---|---|---|---|---|
| Type of pre-existing mental disorder | ||||
| No disorder | Ref | Ref | ||
| Anxiety | 0.70 (0.27) | 0.009 | 0.94 (0.28) | 0.001 |
| Mood disorders | 1.01 (0.55) | 0.067 | 1.60 (0.59) | 0.007 |
| Comorbid D + A | 2.00 (0.37) | <0.001 | 1.89 (0.40) | <0.001 |
Unstandardized coefficients with the Standard Errors (SE) are displayed. Analyses were adjusted for age, gender, and baseline levels of anxiety and depression, respectively. D + A: Depression and anxiety.
The multivariate models including the psychological factors are presented in Table 3 . We found that increases in COVID-perceived stress (from baseline to follow-up) (model A) were associated with higher anxiety and depressive symptoms at follow-up. Similarly, decreases in social support between baseline and follow-up (model B) were associated with higher anxiety and depressive symptoms at follow-up. The interactions between these factors and the type of pre-existing mental disorders for anxiety and depressive symptoms were not significant (Supplementary table 2). Furthermore, we found that greater resilience (at baseline) was negatively associated with higher anxiety and depressive symptoms at follow-up (model C). An interaction tendency was found towards a different effect of resilience in anxiety symptoms for those with pre-existing mood disorders (Supplementary table 2). No significant interactions were found between resilience and the type of pre-existing mental disorders for depressive symptoms.
Table 3.
Adjusted Tobit regression models for each psychological factor between these factors and the type of pre-existing disorder for anxiety and depressive symptoms.
| Anxiety symptoms Coef (SE) |
p value | Depressive symptoms Coef (SE) |
p value | ||
|---|---|---|---|---|---|
| Model A | |||||
| Change in COVID-perceived stress | 0.43 (0.03) | <0.001 | 0.37 (0.03) | <0.001 | |
| Pre-existing mental disorder | No disorder | Ref | Ref | ||
| Anxiety | 0.61 (0.25) | 0.015 | 0.81 (0.27) | 0.003 | |
| Mood disorders | 1.12 (0.52) | 0.033 | 1.69 (0.57) | 0.003 | |
| Comorbid D + A | 2.07 (0.35) | <0.001 | 1.92 (0.39) | <0.001 | |
| Model B | |||||
| Change in social support | −0.20 (0.07) | 0.002 | −0.24 (0.07) | 0.001 | |
| Pre-existing mental disorder | No disorder | Ref | Ref | ||
| Anxiety | 0.65 (0.26) | 0.015 | 0.92 (0.28) | 0.001 | |
| Mood disorders | 0.89 (0.55) | 0.106 | 1.53 (0.59) | 0.010 | |
| Comorbid D + A | 1.83 (0.37) | <0.001 | 1.79 (0.40) | <0.001 | |
| Model C | |||||
| Resilience | −0.07 (0.02) | <0.001 | −0.11 (0.02) | <0.001 | |
| Pre-existing mental disorder | No disorder | Ref | Ref | ||
| Anxiety | −0.27 (1.49) | 0.854 | 0.85 (1.59) | 0.594 | |
| Mood disorders | −5.41 (3.17) | 0.088 | −3.13 (3.32) | 0.346 | |
| Comorbid D + A | −0.92 (1.60) | 0.565 | −1.35 (1.71) | 0.430 |
Unstandardized coefficients with Standard Errors (SE) and p-values are displayed. Analyses were made separately for each psychological factor and adjusted for age, gender, type of disorder, and baseline anxiety or depressive symptoms. COVID-perceived stress and change in social support regression models were also adjusted for baseline COVID-perceived stress and baseline social support, respectively. D + A: depression and anxiety.
4. Discussion
This longitudinal study expands upon previous evidence by assessing levels of and changes in current anxiety and depressive symptoms according to the type of pre-existing mental disorder, a year after the COVID-19 outbreak in Spain. Furthermore, we provided evidence regarding the role of COVID-perceived stress, social support, and resilience on anxiety and depressive symptoms, according to the type of pre-existing mental disorder.
4.1. Changes in anxiety and depressive symptoms by type of pre-existing mental condition
Our results show that levels of anxiety and depressive symptoms significantly increased from baseline (June 2020) to follow-up (February–March 2021) for the overall sample. After stratifying by type of pre-existing mental disorder, all groups showed increased levels of anxiety and depressive symptoms, but the increases did not reach statistical significance for all groups. Those with no pre-existing mental disorders and those with pre-existing anxiety showed significant increases in both anxiety and depressive symptoms. Those with pre-existing comorbid D + A had significantly increased anxiety symptoms only, while those with pre-existing mood disorders did not show significant increases either in anxiety or depressive symptoms.
These results contradict the findings of prior studies reporting a progressive decrease in mental health symptoms over the course of the pandemic in people with pre-existing affective disorders (Bartels et al., 2022, Bendau et al., 2021). One way to explain these divergent findings is related to the timing of data collection points and the associated evolution of the pandemic. Some authors have suggested that mental health symptoms might fluctuate following the COVID-19 pandemic waves (i.e., infection and mortality rates) (Santomauro et al., 2021), and associations between periods of tighter containment measures and worsening of mental health symptoms have been reported (Pedersen et al., 2022). In this study, baseline data collection occurred after the devastating first wave of infection, at the end of the lockdown in Spain. During this period, infection and mortality rates were much lower compared to the outbreak (140 vs 5300 mean weekly confirmed deaths) (Spain - WHO Coronavirus (COVID-19) Dashboard, 2022), an easing of restrictive control measures was occurring, and there was a general optimistic thinking concerning the pandemic. Follow-up data were collected at the end of the third COVID-19 wave in Spain. In this period people had experienced two waves of high infection and mortality rates, which were still quite high at the time of data collection (1260 mean weekly confirmed deaths) (Spain - WHO Coronavirus (COVID-19) Dashboard, 2022). Furthermore, tight restrictions were still on (e.g., curfew and limited geographical mobility), and the vaccination campaign had started. Therefore, the observed increase in mental health symptoms in most groups might be explained by the worsening of the epidemiological situation that occurred during the specific data collection periods.
Beyond potential explanations linked to data collection points, those with pre-existing anxiety might experience increased mental health symptoms (i.e., anxiety and depressive symptoms) for several reasons. First, their elevated tendency to overestimate threat (Abramowitz and Blakey, 2020) and their lower tolerance of uncertainty (Carleton et al., 2012, Gu et al., 2020) could be key contributing factors in explaining increases in their symptomatology during periods of high COVID-19 incidence and restrictive measures (i.e. follow-up). Related to this, one study conducted at the beginning of the pandemic suggested that those with pre-existing anxiety were more likely to make efforts to cope with the COVID-19 stressors (Asmundson et al., 2020). However, it is possible that these efforts were directed towards maladaptive coping strategies (Penley et al., 2020), or that, due to pandemic stressors becoming chronic over time, coping mechanisms that were effective at baseline were no longer effective in follow-up, which may ultimately have led to a worsening of mental distress symptoms.
We found that those with pre-existing mood disorders did not show significantly increased mental health symptoms. This is seemingly the result of the limited sample size of this group (n = 70) as similar increases in both anxiety and depressive symptoms between baseline and follow-up were statistically significant for those with no disorder and the group with pre-existing anxiety.
Finally, those with pre-existing comorbid D + A showed increases in anxiety symptoms, but depressive symptoms remained high and stable. When depression and anxiety symptoms occur together, the severity and the chronicity of each disorder increases, recovery slows, and the likelihood of recurrence increases (Choi et al., 2020, Hirschfeld, 2001). This suggests that people with pre-existing comorbid D + A are at a greater risk of suffering the mental health impact of the pandemic. Their increased vulnerability, together with a worse response to psychosocial and pharmacological treatments (Coplan et al., 2015), greater utilization of medical services, and higher treatment costs (McLaughlin et al., 2006), all suggest that people with comorbid D + A require special attention during a prolonged stressful situation such as a pandemic.
While our results provide evidence regarding the middle-term impact of the COVID-19 pandemic on those with pre-existing mental disorders, further research is needed to elucidate the complete courses of mental health symptoms during the entire duration of the COVID-19 pandemic in relation to pre-existing mental conditions.
4.2. Psychological factors related to changes in mental health over time
As for psychological factors, we observed that after adjusting for confounders and type of pre-existing disorder, COVID-perceived stress predicted higher levels of anxiety and depressive symptoms, while resilience and social support were protective factors. This is in line with previous evidence from studies of the general population (Coiro et al., 2021, Grey et al., 2020, Haliwa et al., 2021, Ran et al., 2020), and it suggests that clinical interventions aimed at reducing pandemic-related stress and boosting social support and resilience could be effective in reducing mental health symptoms. Indeed, one randomized controlled trial reported the effectiveness of an online intervention aimed at reducing mental health symptoms in a sample of distressed adults that included strategies for the management of pandemic-related worries and for accessing social support during lockdown (Bryant et al., 2022). Furthermore, the finding that the type of pre-existing mental disorder did not moderate the relationships between psychological factors and mental health outcomes suggests that these psychological variables are risk and protective factors independently of the type of pre-existing disorder and can be considered in transdiagnostic approaches.
4.3. Limitations
This study should be considered in light of several limitations. First, while this study included two waves of data, future longitudinal evidence assessing multiple time points is warranted to better understand the mental impact dynamics of the COVID-19 pandemic. In addition, other factors not assessed in the current study may be also important to understand the impact of the pandemic on people with pre-existing mental disorders (e.g., whether participants were receiving mental health treatment, etc.…). Second, since we lacked pre-pandemic data, assessment of the pre-existing mental conditions was based on a CIDI checklist, which includes lifetime-based items. Moreover, current mental health symptoms were based on self-reported screening scales, which are inferior to face-to-face clinical diagnostic interviews. Third, while the sample is representative of the general population, present findings cannot be generalized to other institutionalized populations or other hard-to-reach groups. Fourth, the loss of follow-up was considerable (43 %), which might reduce the generalizability and comparability of the results. However, no significant differences in demographic characteristics were observed between participants with complete data and those excluded because of missing data, and weights were used to restore representativeness. Finally, the sample size for the group of people with pre-existing mood disorders was limited (n = 70), so the results obtained in this group might be underpowered.
5. Conclusions
Notwithstanding the above limitations, current findings suggest that people with distinct pre-existing mental disorders have experienced different patterns of anxiety and depressive symptoms during the middle phase of the COVID-19 pandemic in Spain. Furthermore, we found COVID-perceived stress to be a risk factor for increased anxiety and depressive symptoms, while resilience and social support were protective factors. Thus, efforts should be made to implement interventions focused on reducing pandemic-related stress and increasing social support and resilience. Such efforts could be effective transdiagnostic approaches regardless of the pre-existing mental diagnosis.
Ethical approval
Ethical approval was provided by the Fundació Sant Joan de Déu Ethics Committee, Barcelona, Spain (PIC 86-20) and by the Parc de Salut Mar Clinical Research Ethics Committee (2020/9203/I) and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Oral consent from all participants was obtained prior to proceeding with the interview.
Financial disclosure
This work was supported by the Instituto de Salud Carlos III (ISCIII), Ministerio de Ciencia e Innovación/FEDER, (grant number COV20/00711) and by the Centro de Investigación Biomédica Red de Salud Mental (CIBERSAM), ISCIII, Madrid, Spain. Additional support was received by the European Union's Horizon 2020 Framework Program under grant agreement No 101016127, and the ISCIII, (CD20/00036) (MF-N), (CD18/00049) (PM). The funding bodies had no role in study design, data collection and analysis, interpretation of data, or in writing the manuscript.
CRediT authorship contribution statement
AMM and MFN conceptualized the study. Material preparation and data collection were performed by PM, GV, JA and JMH. Statistical analysis were performed by MVM, EC, MFN and AMM. The first draft of the manuscript was written by AMM, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Availability of data and materials
The de-identified participant data is available as from publication and upon reasonable request from the corresponding author as long as the main objective of the data sharing request is replicating the analysis and findings as reported in this paper (without investigator support), after approval of a proposal, and with a signed data access agreement.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgements
We thank all cohort members for their collaboration in the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.08.127.
Appendix A. Supplementary data
Supplementary material
References
- Abdalla S.M., Ettman C.K., Cohen G.H., Galea S. Mental health consequences of COVID-19: a nationally representative cross-sectional study of pandemic-related stressors and anxiety disorders in the USA. BMJ Open. 2021;11(8) doi: 10.1136/bmjopen-2020-044125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abramowitz J.S., Blakey S.M., American Psychological Association . Clinical handbook of fear and anxiety: Maintenance processes and treatment mechanisms. American Psychological Association; 2020. [Google Scholar]
- Asmundson G.J.G., Paluszek M.M., Landry C.A., Rachor G.S., McKay D., et al. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels C., Hessmann P., Schmidt U., Vogelgsang J., Ruhleder M., et al. Medium-term and peri-lockdown course of psychosocial burden during the ongoing COVID-19 pandemic: a longitudinal study on patients with pre-existing mental disorders. Eur Arch Psychiatry Clin Neurosci. 2022;272(5):757–771. doi: 10.1007/s00406-021-01351-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., et al. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2021;11(2) doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant R.A., Dawson K.S., Keyan D., Azevedo S., Yadav S., et al. Effectiveness of a Videoconferencing-Delivered Psychological Intervention for Mental Health Problems during COVID-19: A Proof-of-Concept Randomized Clinical Trial. Psychother Psychosom. 2022;91(1):63–72. doi: 10.1159/000520283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton N.R., Mulvogue M.K., Thibodeau M.A., McCabe R.E., Antony M.M., et al. Increasingly certain about uncertainty: Intolerance of uncertainty across anxiety and depression. J Anxiety Disord. 2012;26(3):468–479. doi: 10.1016/j.janxdis.2012.01.011. [DOI] [PubMed] [Google Scholar]
- Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Gao J., Dai J., Mao Y., Wang Y., et al. Generalized anxiety disorder and resilience during the COVID-19 pandemic: evidence from China during the early rapid outbreak. BMC Public Health. 2021;21(1) doi: 10.1186/s12889-021-11877-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K.W., Kim Y.K., Jeon H.J. Advances in Experimental Medicine and Biology. Vol. 1191. Springer; 2020. Comorbid anxiety and depression: Clinical and conceptual consideration and transdiagnostic treatment. [DOI] [PubMed] [Google Scholar]
- Coiro M., Asraf K., Tzischinsky O., Hadar-Shoval D., Tannous-Haddad L., et al. Sleep quality and COVID-19-related stress in relation to mental health symptoms among Israeli and U.S. adults. Sleep Health. 2021;7(2):127–133. doi: 10.1016/j.sleh.2021.02.006. [DOI] [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R.T. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC) Depress Anxiety. 2003;18(2) doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Coplan J.D., Aaronson C.J., Panthangi V., Kim Y. Treating comorbid anxiety and depression: Psychosocial and pharmacological approaches. World J Psychiatry. 2015;5 doi: 10.5498/wjp.v5.i4.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domènech-Abella J., Gabarrell-Pascuet A., Faris L.H., Cristóbal-Narváez P., Félez-Nobrega M., et al. The association of detachment with affective disorder symptoms during the COVID-19 lockdown: the role of living situation and social support. J. Affect. Disord. 2021;292 doi: 10.1016/j.jad.2021.05.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. The Lancet Psychiatry. 2021;8(2) doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Campayo J., Zamorano E., Ruiz M.A., Pardo A., Pérez-Páramo M., et al. Cultural adaptation into spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual. Life Outcomes. 2010;8 doi: 10.1186/1477-7525-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87 doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grey I., Arora T., Thomas J., Saneh A., Tomhe P., et al. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y., Gu S., Lei Y., Li H. From uncertainty to anxiety: How uncertainty fuels anxiety in a process mediated by intolerance of uncertainty. Neural Plast. 2020 doi: 10.1155/2020/8866386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo K., Zhang X., Bai S., Minhat H.S., Nazan A.I.N.M., et al. Assessing social support impact on depression, anxiety, and stress among undergraduate students in Shaanxi province during the COVID-19 pandemic of China. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0253891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haliwa I., Wilson J., Lee J., Shook N.J. Predictors of Change in Mental Health during the COVID-19 Pandemic. J Affect Disord. 2021;291:331–337. doi: 10.1016/j.jad.2021.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfeld R.M.A. The comorbidity of major depression and anxiety disorders: Recognition and management in primary care. Prim Care Companion J Clin Psychiatry. 2001;3 doi: 10.4088/pcc.v03n0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Üstün B.B. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13(2):93–117. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocalevent R.D., Berg L., Beutel M.E., Hinz A., Zenger M., et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3) BMC Psychology. 2018;6(1) doi: 10.1186/s40359-018-0249-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Strine T.W., Spitzer R.L., Williams J.B.W., Berry J.T., et al. The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long J.S. Regression Models for Categorical and Limited Dependent Variables. SAGE Publications; 1997. [Google Scholar]
- McBee M. Modeling outcomes with floor or ceiling effects: an introduction to the Tobit model. Gift. Child Q. 2010;54(4) doi: 10.1177/0016986210379095. [DOI] [Google Scholar]
- McLaughlin T.P., Khandker R.K., Kruzikas D.T., Tummala R. Overlap of anxiety and depression in a managed care population: Prevalence and association with resource utilization. J Clin Psychiatry. 2006;67(8):1187–1193. doi: 10.4088/jcp.v67n0803. [DOI] [PubMed] [Google Scholar]
- MINDCOVID project 2020. https://www.mindcovid.org/quienes-somos Available at.
- Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., et al. How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(9) doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortier P., Vilagut G., Ferrer M., Alayo I., Bruffaerts R., et al. Thirty-day suicidal thoughts and behaviors in the spanish adult general population during the first wave of the Spain COVID-19 pandemic. Epidemiol. Psychiatr. Sci. 2021 doi: 10.1017/S2045796021000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Navarro R., Cano-Vindel A., Medrano L.A., Schmitz F., Ruiz-Rodríguez P., et al. Utility of the PHQ-9 to identify major depressive disorder in adult patients in Spanish primary care centres. BMC Psychiatry. 2017;17(1):1–9. doi: 10.1186/s12888-017-1450-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen M.T., Andersen T.O, Clotworthy A., Jensen A.K., Strandberg-Larsen K., et al. Time trends in mental health indicators during the initial 16 months of the COVID-19 pandemic in Denmark. BCM Psychiatry. 2022;22:25. doi: 10.1186/s12888-021-03655-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penley J.A., Tomaka J., Wiebe J.S. The Association of Coping to Physical and Psychological Health Outcomes: A Meta-Analytic Review. J Behav Med. 2020;25:551–603. doi: 10.1023/A:1020641400589. [DOI] [PubMed] [Google Scholar]
- Ran L., Wang W., Ai M., Kong Y., Chen J., et al. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: A study of the general population in China at the peak of its epidemic. Soc Sci Med. 2020;262 doi: 10.1016/j.socscimed.2020.113261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296 doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santomauro D.F., Mantilla Herrera A.M., Shadid J., Zheng P., Ashbaugh C., et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312) doi: 10.1016/s0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer K.M., Lieberman A., Sever A.C., Joiner T. Prevalence rates of anxiety, depressive, and eating pathology symptoms between the pre- and peri-COVID-19 eras: a meta-analysis. J. Affect. Disord. 2022;298 doi: 10.1016/j.jad.2021.10.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., et al. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spain - WHO Coronavirus (COVID-19) Dashboard 2022. https://covid19.who.int/region/euro/country/es Available at.
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tamsyn E.V.R., Denny M., Erica N., Andrea P., Eric J.T., et al. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. J. Affect. Disord. 2020;275:69–77. doi: 10.1016/J.JAD.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S. Flexible Imputation of Missing Data. 2nd. Chapman & Hall; 2018. [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 2009;54(5) doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. In. J. Affect. Disord. 2021;281 doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The de-identified participant data is available as from publication and upon reasonable request from the corresponding author as long as the main objective of the data sharing request is replicating the analysis and findings as reported in this paper (without investigator support), after approval of a proposal, and with a signed data access agreement.