Abstract
Sleep paralysis is a period of paralysis at either sleep onset or upon awakening and is often accompanied by terrifying hallucinations. We report a case of a 32-year-old healthy men with a history of mild positional obstructive sleep apnea and sleep paralysis. The positional sleep apnea was successfully treated with the Sleep Position Trainer. Remarkably, he did no longer experience episodes of sleep paralysis since using the Sleep Position Trainer. This case highlights a possible elegant noninvasive long-term solution for the treatment of sleep paralysis.
Citation:
Cui N, van Looij MA, Kasius KM. Successful treatment of sleep paralysis with the Sleep Position Trainer: a case report. J Clin Sleep Med. 2022;18(9):2317–2319.
Keywords: sleep paralysis, SP, obstructive sleep apnea, OSA, position-dependent OSA, POSA, sleep position trainer, SPT, rapid eye movement, REM, REM-sleep
INTRODUCTION
Sleep paralysis (SP) is a state at either sleep onset or upon awakening from sleep, where the ability to perform voluntary motor activities is inhibited.1 During episodes of (conscious) SP, individuals often experience dream activity that is vivid, multisensorial, and accompanied by terrifying visual (hypnopompic) hallucinations. The combination of immobility and waking nightmares make SP a very unpleasant and often frightening experience for most individuals. Surprisingly, 7.6% of the general population have experienced at least 1 SP episode over the course of their lifetime.2 Two studies investigated clinical impacts of SP in a clinical sample and student sample and found that 43.6% and 15.4% met the clinically significant distress/impairment criterion, respectively.3,4
The episodes of SP typically manifest during the rapid eye movement (REM) sleep phase. During REM sleep, muscle atonia is established by the pons and ventromedial medulla suppression of the skeletal muscle tone.5 The current known pathophysiological pathway of SP is considered to be associated with flaws in the brain stem structures. For example, intruder and incubus hallucinations that are characteristic of SP are consistent with activation of threat-induced vigilance systems that typically involve the amygdala.6
A large number of comorbidities are associated with SP ranging from physical and psychiatric illness to obstructive sleep apnea (OSA). Moreover, SP appears to be particularly prevalent in people with posttraumatic stress disorder.7
Previous research has suggested an association between sleeping body position and SP.8 A greater number of patients reported SP in supine position than all other positions combined. It is suggested that the supine position might permit the greatest relaxation and thus potentiate SP.8
Body position may also be a causative factor in sleep apnea. More than half of the patients with OSA have position-dependent OSA (POSA). POSA is defined as supine apnea-hypopnea index (AHI) twice or more compared to the AHI in other positions.9 One of the methods to avoid the supine sleeping position is the Sleep Position Trainer (SPT), a vibrating medical device that has been found to effectively treat POSAs of mild to moderate severity both during short-term and long-term follow up.10,11
REPORT OF CASE
A 32-year-old man presented with a history of self-reported daytime sleepiness, insomnia, and snoring. He had no significant past medical history, nor did he take any medication. He was an entrepreneur, working daily from 1 pm until 11 pm and sleeping from 3 am till 12 pm. His sleep was interrupted by frequent awakenings and possible apneas. His Epworth Sleepiness Scale score was 6. Additionally, he reported frequently experiencing a vivid “dream-like” state and inability to move his body voluntarily upon wakening for the past year. This exclusively happened while he was in the supine position. These episodes were accompanied by the intruder phenomenon, where he reported sensing black forms and spiders.12 After these episodes of sleep paralysis, fear prohibited him from going back to sleep. He also denied having episodes of cataplexy. To evaluate for suspected OSA, polysomnography (PSG) was performed. The PSG showed a sleep onset latency of 18 minutes and REM sleep latency of 122 minutes. The AHI was 7.1 events/h, which consisted of supine AHI 13.8 events/h (45.2% of total sleep time) and nonsupine AHI 1.9 (54.8% of total sleep time) (Table 1 and Figure 1). No SP was reported on the night of the PSG. A diagnosis of mild POSA was made and he was treated with the SPT. In addition, we referred him to a sleep psychologist for cognitive behavioral therapy for insomnia.
Table 1.
Polysomnogram data of 1 night of sleep of patient before treatment.
| AHI, events/h | 7.1 |
| Apnea index, events/h | 5.7 |
| Hypopnea, events/h | 1.4 |
| Obstructive apnea, events/h | 4.1 |
| Central apnea, events/h | 0.2 |
| Mixed apnea, events/h | 1.4 |
| RERA, events/h | 4.3 |
| RDI, events/h | 11.4 |
| Nonsupine, %TST | 54.8 |
| AHI nonsupine, events/h | 1.9 |
| Supine, %TST | 45.2 |
| AHI supine, events/h | 13.3 |
| REM, %TST | 21.4 |
| AHI REM, events/h | 12.7 |
| Sleep latency, min | 17.7 |
| Sleep efficiency, % | 90.3 |
| Hypnogram | Fragmented |
| Sleep cycles | 5 |
| Periods of REM sleep | 5 |
| Deep sleep, % | 14.1 |
| Arousal index | 15.7 |
| Awakenings | 13 |
| REM latency, hours | 02:12:00 |
| Average O2, % | 96 |
| O2 (min), % | 92 |
| O2 desaturation index 3%, events/h | 5.6 |
| O2 desaturation index 4%, events/h | 0.7 |
| Snoring | heavily |
| PLMS | none |
AHI = apnea-hypopnea index, RDI = respiratory disturbance Index, REM = rapid eye movement, RERA = respiratory effort related arousal, PLMS = periodic limb movements, TST = total sleep time.
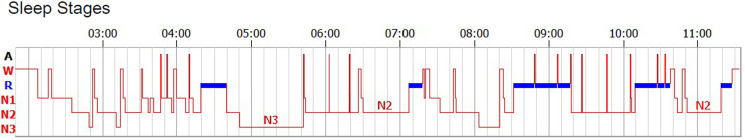
Figure 1. Hypnogram of 1 night of sleep of patient before treatment.
Fragmented sleep pattern with 14.1% deep sleep of total sleeping time. A= artifact, N1 = NREM1, N2 = NREM2, N3 = NREM3, R = rapid eye movement sleep, W = wake.
At follow up, the patient reported that with the use of the SPT and after cognitive behavioral therapy for insomnia, his sleepiness and snoring complaints were relieved. Remarkably, since using the SPT, he was no longer experiencing episodes of sleep paralysis. Hence, he was motivated to continue the use of the SPT. Nowadays he sleeps calmly without interruptions and reports feeling restored in the morning. According to national guidelines, PSG was in his case not repeated posttreatment due to mild OSA and self-resolved complaints.13
DISCUSSION
This present report illustrates a beneficial effect of SPT where not only OSA was treated, but the patient was also relieved from his SP. Taking into account the association between body position and SP, we believe that this may be the direct result of the use of the SPT.
The relationship between SP and OSA is not well understood. Nevertheless, there is a well-known association between the body position and OSA in the majority of patients. The gravitational effects on soft upper airways tissues in the supine position increase the propensity and frequency of upper airway collapse and result in apneas.14 Furthermore, Vernet et al15 reported increased sleep paralysis in patients with OSA with residual excess sleepiness compared to controls, 20% vs 5%, respectively. Cheyne et al8 suggested that the relation between apnea induced REM microarousals and SP increased sympathetic tone during REM sleep caused by OSA could induce sleep paralysis. However, a recent study by Kliková et al,16 despite finding higher cortical activity, did not demonstrate an increased REM sleep fragmentation in a series of recurrent isolated patients with SP. Taking the above into consideration, the reduction of the OSA in the present case may have also been a beneficial factor in relieving the number of SP episodes.
A recent review of Denis et al7 addressed the relationship between SP and sleep quality. It was concluded that objective predictors are limited; however, sleep latency and sudden-onset REM may be predictors of SP. Both of these predictors were within the normal range in our patient. Patient-reported lower sleep quality and stress seem to be associated with an increased risk of SP, therefore we cannot exclude a beneficial effect of the cognitive behavioral therapy for insomnia on the incidence of SP in our patient.7 Although there seems to be an association between narcolepsy and SP, the relationship between insomnia disorder and SP remains unclear.
There is currently no “gold standard” therapy for SP. A review of Sharpless et al17 concluded that, although there are several promising psychopharmacological and psychotherapeutic approaches to treatment for sleep paralysis, no empirically supported treatment recommendations can be made since not a single randomized controlled trial has been conducted for SP. However, we believe that the SPT may provide an elegant noninvasive and nonpharmacological long-term solution for treatment of SP.
Future studies are therefore recommended to validate the use of SPT for treatment of SP of patients who meet the clinically significant impairment criterion.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. Work for this study was performed at Amsterdam Sleep and Apnea Centre, OLVG West, Jan Tooropstraat 164, 1061AE, Amsterdam. The authors report no conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- OSA
obstructive sleep apnea
- POSA
position-dependent obstructive sleep apnea
- PSG
polysomnography
- REM
rapid eye movement
- SP
sleep paralysis
- SPT
Sleep Position Trainer
REFERENCES
- 1. American Academy of Sleep Medicine . International Classification of Sleep Disorders. 3rd ed. Darien, IL: : American Academy of Sleep Medicine; ; 2014. . [Google Scholar]
- 2. Sharpless BA , Barber JP . Lifetime prevalence rates of sleep paralysis: A systematic review . Sleep Med Rev. 2011. ; 15 ( 5 ): 311 – 315 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sharpless BA , Grom JL . Isolated sleep paralysis: Fear, prevention, and disruption . Behav Sleep Med. 2016. ; 14 ( 2 ): 134 – 139 . [DOI] [PubMed] [Google Scholar]
- 4. Sharpless BA , McCarthy KS , Chambless DL , Milrod BL , Khalsa SR , Barber JP . Isolated sleep paralysis and fearful isolated sleep paralysis in outpatients with panic attacks . J Clin Psychol. 2010. ; 66 ( 12 ): 1292 – 1306 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Peever J , Fuller PM . The biology of REM sleep . Curr Biol. 2017. ; 27 ( 22 ): R1237 – R1248 . [DOI] [PubMed] [Google Scholar]
- 6. JA C . Sleep paralysis: State transition disruption and narcolepsy . In: Basetti C , Billiard M , Mignot E , eds. Narcolepsy and Hypersomnia. New York: : Taylor and Francis Group; ; 2006. : 109–118. [Google Scholar]
- 7. Denis D , French CC , Gregory AM . A systematic review of variables associated with sleep paralysis . Sleep Med Rev. 2018. ; 38 : 141 – 157 . [DOI] [PubMed] [Google Scholar]
- 8. Cheyne JA . Situational factors affecting sleep paralysis and associated hallucinations: Position and timing effects . J Sleep Res. 2002. ; 11 ( 2 ): 169 – 177 . [DOI] [PubMed] [Google Scholar]
- 9. Oksenberg A , Arons E , Greenberg-Dotan S , Nasser K , Radwan H . [The significance of body posture on breathing abnormalities during sleep: Data analysis of 2077 obstructive sleep apnea patients] . Harefuah. 2009. ; 148 ( 5 ): 304 – 309, 351, 350 . [PubMed] [Google Scholar]
- 10. van Maanen JP , Meester KAW , Dun LN , et al . The sleep position trainer: A new treatment for positional obstructive sleep apnoea . Sleep Breath. 2013. ; 17 ( 2 ): 771 – 779 . [DOI] [PubMed] [Google Scholar]
- 11. van Maanen JP , de Vries N . Long-term effectiveness and compliance of positional therapy with the sleep position trainer in the treatment of positional obstructive sleep apnea syndrome . Sleep. 2014. ; 37 ( 7 ): 1209 – 1215 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jalal B , Ramachandran VS . Sleep paralysis, “The ghostly bedroom intruder” and out-of-body experiences: The role of mirror neurons . Front Hum Neurosci. 2017. ; 11 : 92 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. NVALT/NVKNO . Obstructief slaapapneu (OSA) bij volwassenen. Richtlijnendatabase; . https://richtlijnendatabase.nl/richtlijn/osa_bij_volwassenen/startpagina_-_obstructief_slaapapneu_osa.html . Published 2018. Accessed May 16, 2022. [Google Scholar]
- 14. Cartwright RD . Effect of sleep position on sleep apnea severity . Sleep. 1984. ; 7 ( 2 ): 110 – 114 . [DOI] [PubMed] [Google Scholar]
- 15. Vernet C , Redolfi S , Attali V , et al . Residual sleepiness in obstructive sleep apnoea: Phenotype and related symptoms . Eur Respir J. 2011. ; 38 ( 1 ): 98 – 105 . [DOI] [PubMed] [Google Scholar]
- 16. Kliková M , Piorecký M , Miletínová E , Jank ů K , Dudysová D , Bušková J . Objective rapid eye movement sleep characteristics of recurrent isolated sleep paralysis: A case-control study . Sleep. 2021. ; 44 ( 11 ): zsab153 . [DOI] [PubMed] [Google Scholar]
- 17. Sharpless BA . A clinician’s guide to recurrent isolated sleep paralysis . Neuropsychiatr Dis Treat. 2016. ; 12 : 1761 – 1767 . [DOI] [PMC free article] [PubMed] [Google Scholar]