Abstract
BACKGROUND
Spinal cord stimulation (SCS) uses unique electric stimulation parameters to selectively treat specific regions of chronic or refractory back pain. Changing these parameters can lead to spreading paresthesia and/or pain beyond the desired region.
OBSERVATIONS
A patient with a history of stable, successful SCS treatment presented with acute development of paresthesias that were relieved by reduction of stimulation parameters. The patient required paradoxically lower SCS settings for control of chronic back pain. This presentation prompted further investigation, which revealed a new disc protrusion and cord compression at the level of the paddle lead.
LESSONS
In patients with SCS, a new onset of back pain accompanied by acute paresthesia that is reversible by reducing the SCS amplitude warrants investigation for new spine pathology.
Keywords: spinal cord stimulation, spine pathology, back pain, acute disc herniation
ABBREVIATIONS : CT = computed tomography, SCS = spinal cord stimulation
Spinal cord stimulation (SCS) has been successfully used as a treatment option for refractory back, radicular, and neuropathic pain.1 The most common indication has been for refractory neuropathic pain after spine surgery (i.e., postlaminectomy syndrome). Patient selection, operative procedure and technique, and complications and risk profile of SCS placement have been well described in the literature.2–4 Two major types of SCS electrodes include percutaneously placed cylindrical leads and surgically placed paddle leads via laminotomy.
The traditional tonic SCS uses parameters such as frequency, pulse width, and amplitude to stimulate the dorsal columns, generating paresthesias in the regions of pain, thereby “blocking” the pain signal traveling within the spinal cord. Parameters are chosen to selectively treat specific regions of pain. Increasing the amplitude or pulse width can lead to spreading paresthesia beyond the desired region.5,6
In this report, we present a patient with a history of stable, successful SCS treatment with a paddle lead who presented with acute development of paresthesias that were relieved by reduction of stimulation parameters. This presentation prompted further investigation, which revealed a new disc herniation and cord compression at the level of the paddle lead.
Illustrative Case
A 66-year-old woman with a history of multiple spine surgeries, including an SCS system with thoracic 1 × 4 paddle lead placed in 2009, presented to the clinic with rapidly worsening symptoms of lower extremity pain and paresthesias, which were noted to be different in quality from her baseline chronic back pain. She denied any recent trauma, although the pain occurred while she was cooking. SCS had previously been able to provide satisfactory and stable control of her chronic pain symptoms. Given her new symptoms, her SCS programming was readjusted, but she reported improvement only with reduction in the amplitude. Once the implantable pulse generator was completely powered off, she reported immediate relief of her new lower extremity pain. This paradoxical finding raised concern for a potential new pathology or migration of SCS leads. A computed tomography (CT) myelogram revealed a thoracic disc herniation at the level of the paddle lead, deforming the cord (Fig. 1). The patient received a successful thoracic laminectomy, partial corpectomy, and discectomy without modifications to the SCS paddle position (Fig. 2). Postoperatively, the patient reported resolution of her lower extremity pain and paresthesias and was able to resume use of SCS to manage her chronic pain.
FIG. 1.
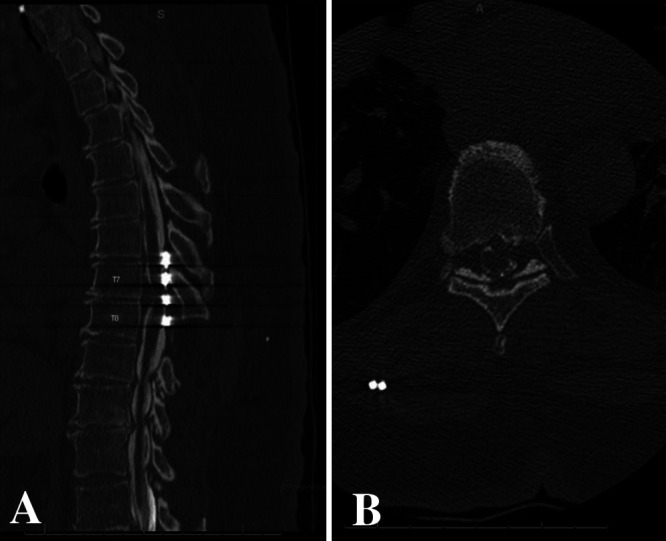
CT myelogram. Sagittal (A) and axial (B) views of the thoracic spine showing intravertebral disc herniation and compression of the spinal cord against the SCS paddle at the level of T7-T8.
FIG. 2.
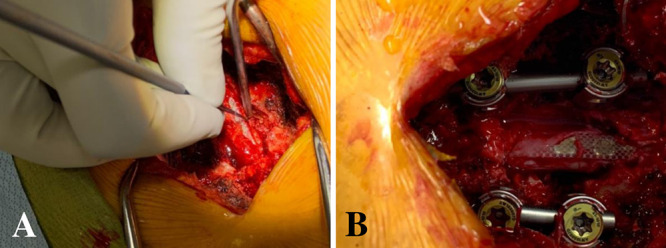
Intraoperative image of the thoracic SCS device before (A) and after (B) discectomy.
Discussion
Observations
In patients who have a SCS device, a new onset of back pain accompanied by acute paresthesia that is reversible by reducing SCS amplitude warrants investigation for new spine pathology. This is particularly true in the setting of a paddle lead, which has extremely low risk of migration and occupies more space within the spinal canal than cylindrical leads.7,8 Previous studies have shown that the gradual reduction of spinal canal space and therefore smaller distance between the SCS device and the spinal cord causes changes in neurological symptoms. These changes, although common, are subtle and require manipulation in amplitude for pain control.6 Therefore, it is thought that a closer interaction of the SCS paddle with the spinal cord can be clinically equivocal to an increase in the SCS amplitude parameter.
In this patient, both the need for a lower SCS amplitude setting for control of chronic back pain and the reversal of the new paresthesias with reduction in SCS amplitude were suspicious for an acute pathology that caused a closer interaction between the SCS paddle and the spinal cord. This pathophysiology was well explainable with a potential thoracic disc herniation, and a follow-up CT myelogram confirmed this diagnosis. The patient was treated with a discectomy without the removal of the SCS paddle.
Lessons
Patients with an SCS paddle who present with new acute symptoms of lower extremity pain and paresthesias that are different in quality than their chronic pain should receive an examination if the index of suspicion is high, with consideration for proper understanding of the dynamics of SCS and its modulation of the spinal cord.
Disclosures
Dr. Abdulhak is a teaching consultant with SeaSpine and a teaching consultant with Ulrich Medical USA.
Author Contributions
Conception and design: Air, Behzadi, Mansour, Zervos, Abdulhak. Acquisition of data: Air, Behzadi, Zervos. Analysis and interpretation of data: Air, Behzadi, Zervos. Drafting the article: Behzadi, Telemi, Mansour. Critically revising the article: Air, Behzadi, Telemi, Mansour. Reviewed submitted version of manuscript: Behzadi, Mansour, Zervos, Abdulhak. Approved the final version of the manuscript on behalf of all authors: Air. Administrative/technical/material support: Zervos. Study supervision: Air, Zervos.
References
- 1. Kumar K, Rizvi S. Cost-effectiveness of spinal cord stimulation therapy in management of chronic pain. Pain Med. 2013;14(11):1631–1649. doi: 10.1111/pme.12146. [DOI] [PubMed] [Google Scholar]
- 2.Barolat G. Spinal Cord Stimulation for Chronic Pain Management Implantation Techniques. Interventional Spine; 2008. pp. 341–350. [Google Scholar]
- 3. Henderson JM, Levy RM, Bedder MD, et al. Nans training requirements for spinal cord stimulation devices: selection, implantation, and follow-up. Neuromodulation. 2009;12(3):171–174. doi: 10.1111/j.1525-1403.2009.00211.x. [DOI] [PubMed] [Google Scholar]
- 4. Kumar K, Taylor RS, Jacques L, et al. The effects of spinal cord stimulation in neuropathic pain are sustained: a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord stimulation. Neurosurgery. 2008;63(4):762–770. doi: 10.1227/01.NEU.0000325731.46702.D9. [DOI] [PubMed] [Google Scholar]
- 5. Hussaini SMQ, Murphy KR, Han JL, et al. Specialty-based variations in spinal cord stimulation success rates for treatment of chronic pain. Neuromodulation. 2017;20(4):340–347. doi: 10.1111/ner.12582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shamji MF, Westwick HJ, Heary RF. Complications related to the use of spinal cord stimulation for managing persistent postoperative neuropathic pain after lumbar spinal surgery. Neurosurg Focus. 2015;39(4):E15. doi: 10.3171/2015.7.FOCUS15260. [DOI] [PubMed] [Google Scholar]
- 7. Babu R, Hazzard MA, Huang KT, et al. Outcomes of percutaneous and paddle lead implantation for spinal cord stimulation: a comparative analysis of complications, reoperation rates, and health-care costs. Neuromodulation. 2013;16(5):418–427. doi: 10.1111/ner.12065. [DOI] [PubMed] [Google Scholar]
- 8. Pahapill PA. Incidence of revision surgery in a large cohort of patients with thoracic surgical three-column paddle leads: a retrospective case review. Neuromodulation. 2015;18(5):367–375. doi: 10.1111/ner.12239. [DOI] [PubMed] [Google Scholar]


