Abstract
BACKGROUND
A three-column osteotomy results in dural buckling, which may appear concerning upon intraoperative visualization because it may appear that the neural elements may also be buckled. The authors presented an intraoperative view after intentional durotomy of the neural elements and the relaxed state of the dura after three-column osteotomy.
OBSERVATIONS
A 52-year-old woman with adult tethered cord syndrome and previous untethering presented with worsening leg pain and stiffness, urinary incontinence, and unbalanced gait. Magnetic resonance imaging demonstrated an arachnoid web at T6 and spinal cord tethering. Spinal column shortening via three-column osteotomy was performed with concomitant intradural excision of the arachnoid web. Dural buckling was observed intraoperatively after spinal column shortening. After the durotomy, the spinal cord was visualized without kinking or buckling.
LESSONS
Dural buckling after spinal column shortening of 15 mm via three-column osteotomy at T6 did not result in concomitant buckling of the underlying neural elements.
Keywords: tethered cord syndrome, spinal column shortening, dural buckling
ABBREVIATIONS : CSF = cerebrospinal fluid, CT = computed tomography, MRI = magnetic resonance imaging, TCS = tethered cord syndrome
Tethered cord syndrome (TCS) refers to a constellation of signs and symptoms of motor and sensory dysfunction in the lower extremities and bowel and bladder dysfunction.1–4 The pathology is believed to result from increased tension on the spinal cord due to caudal traction.5 Common etiologies include thickened filum terminale, spinal cord lipoma, lipomyelomeningocele, scoliosis, and injury.5 The current gold standard to treat TCS is untethering surgery in both children and adults.6 Although it has reported success, especially in pain relief, an untethering procedure carries risks of cerebrospinal fluid (CSF) leaks and wound infection in up to 15% of patients.1,7,8 Furthermore, complete untethering may not always be feasible; symptomatic retethering has been reported in up to 50% of patients.9
Spinal column shortening represents an alternative approach to manage TCS, especially in cases of retethering. First reported by Kokubun et al. in 1995, spinal column shortening has been demonstrated to be a safe and effective treatment for TCS.9–14 This approach indirectly relieves the longitudinal tension of tethered neural elements. However, the dural buckling that can ensue after spinal column shortening can appear concerning intraoperatively, and it is unclear if the underlying neural elements are also kinked. Hitherto, previous reports have not shown an intradural view of the spinal cord after shortening.9,11,13,15 Because of the need to concomitantly excise an arachnoid web in this case, the dura was opened. An intraoperative view of the spinal cord and open dura is presented.
Illustrative Case
Patient History
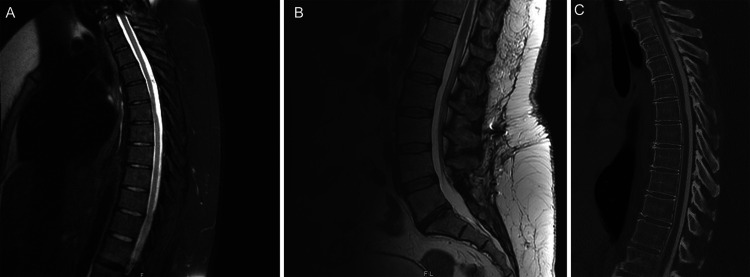
A 52-year-old woman with a history of adult TCS presented with worsening leg pain and stiffness, urinary incontinence, and gait disturbance. She had initially developed these symptoms 11 years ago and at that time received L5-S1 tethered cord release, which improved her right leg spasms. However, her vesicorectal dysfunction persisted, and muscle spasms recurred over the past year. The patient could only walk a half mile before her legs stiffened. Magnetic resonance imaging (MRI) of the thoracic spine demonstrated focal ventral displacement of the spinal cord and a possibly compressive arachnoid web causing cord signal abnormality at T6. A lumbar spine MRI showed the previous detethering site at L5-S1, and the conus medullaris was at L1-L2. Computed tomography (CT) myelogram demonstrated homogenous contrast density without myelographic block at the level of T6, suggesting an arachnoid web (Fig. 1). Because of progressive decline in neurological status, the patient elected to receive spinal column shortening and resection of arachnoid web at the same surgical setting to treat both pathologies.
FIG. 1.
Preoperative thoracic spine MRI (A), lumbar spine MRI (B), and CT myelogram (C) demonstrating arachnoid web at T6.
Operative Description
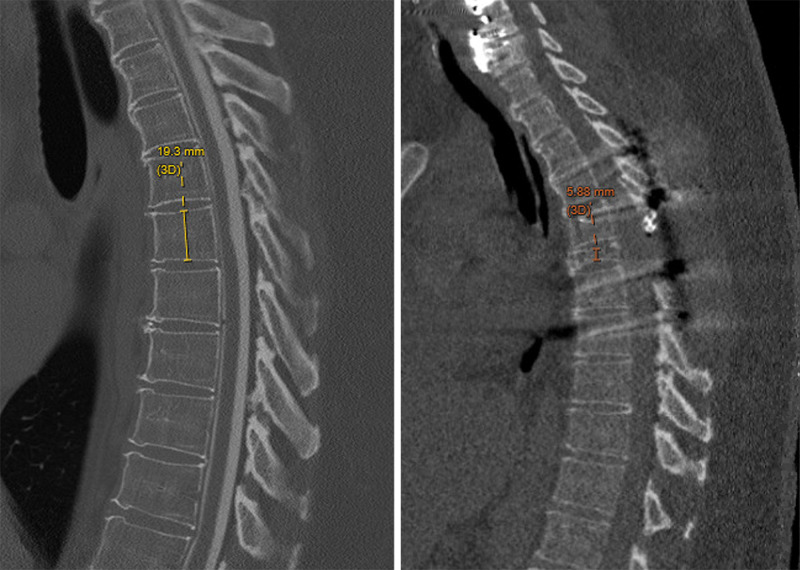
After general anesthesia and prone positioning, the posterior thoracic spine was exposed in the usual standard fashion. Pedicle screws were placed into the pedicles of T4, T5, T7, and T8, and laminectomies at T5 to T7 were performed. Subsequently, a three-column osteotomy of T6 was performed by removing the pedicles, the cancellous bone, the lateral cortical walls, and the posterior cortical wall. A temporary rod was placed at this point to prevent collapse. The ventral vertebral body wall was thinned with a high-speed bur but not excised. The posterior longitudinal ligament was removed, and the spinal column was gently compressed to shorten it by approximately 1.5 cm (Fig. 2). Permanent rods and set screws were then placed and secured.
FIG. 2.
Preoperative (left) and postoperative (right) lateral radiograph demonstrating reduction of T6 vertebral column from 19.3 mm to 5.9 mm.
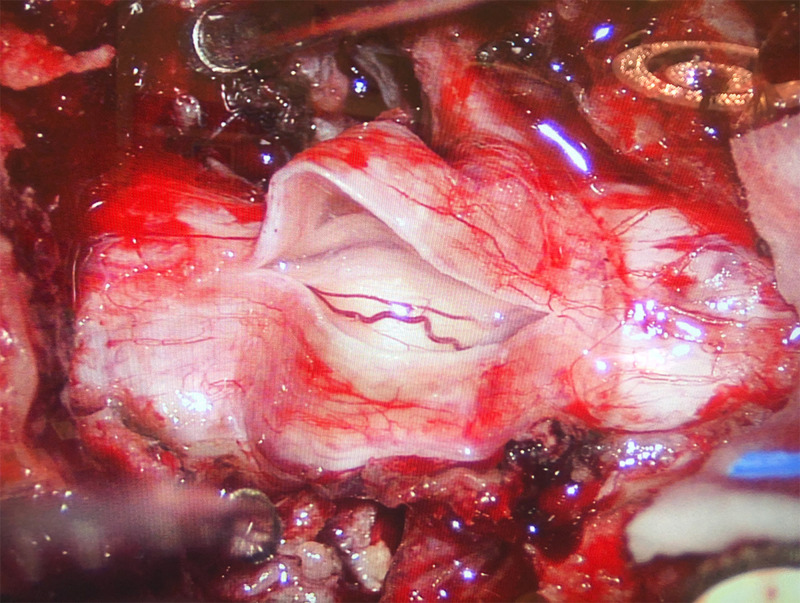
At that point, the intraoperative microscope was brought in. We could see dural buckling, and the dura was subsequently opened via a midline incision (Fig. 3). Motor evoked potentials were stable during the entire operation. The arachnoid web was identified, dissected, and excised. The intraoperative view of the spinal cord demonstrated no buckling or kinking of the spinal cord itself despite the dural buckling. The dura was then closed with a 6-0 Prolene (Ethicon) suture and fibrin glue, and the wound was closed in layers after arthrodesis.
FIG. 3.
Intradural view of the spinal cord and dural buckling after spinal column shortening.
Discussion
Observations
Revision TCS surgery can be morbid at the index site of tethering because dissecting the spinal cord off the dura can be morbid, risking iatrogenic neurological worsening.16,17 Revision untethering also carries risks of CSF leak, pseudomeningocele, infection, and wound complications.6,18 In light of these issues, spinal column shortening is an alternative because there is no direct revision detethering, thus decreasing the likelihood of neurological injury. In addition, it mitigates the risk of CSF leak and wound complications by avoiding a previously opened dura and often abnormal, scarred posterior soft tissue.
The rationale for spinal column shortening originates from the cadaveric study by Grande et al., which demonstrated that a shortening of the spinal column by 20 to 25 mm at the thoracolumbar junction resulted in significant reduction tension of the spinal cord, the lumbosacral nerve roots, and the filum terminale.19 In a recent cadaveric experiment by Safain et al., vertebral column resection demonstrated 87.2% of maximal reduction in spinal cord tension from baseline with 10 mm of closure.20 The authors demonstrated an optimal vertebral column resection of 12 to 16 mm to maximize tension reduction while minimizing dural buckling. This closure magnitude is lower than that previously reported by Grande et al. and is more like our operative experience. In our present case, a shortening of 15 mm achieved desirable tension reduction of the spinal cord, evidenced by dural buckling.
Spinal column shortening has been reported to have favorable outcomes for recurrent TCS. Hsieh et al. reviewed 18 cases of spinal column shortening and showed that 86% of patients recovered complete motor function, 75% were relieved of debilitating back or lower-extremity pain, and 28% exhibited improved urological symptoms.9 Several other small case series had similar findings and concluded that spinal column shortening is a safe and efficacious treatment option for recurrent TCS in both children and adults.11,13,15 A meta-analysis conducted by Lin et al. identified six studies with a total of 57 patients.21 They found that spinal column shortening resulted in significant improvement in neurological deficit, motor function, sensory symptoms, and bowel and bladder function. McVeigh et al. reported 41 patients undergoing spinal column shortening and demonstrated improved bowel and bladder function, pain and sensory scores, and motor function.12 Zhang et al. and Safaee et al. also reported similar findings in patients who received previous detethering procedures.22,23
One consideration in this case is that a spinal column shortening may be considered an aggressive procedure over an arachnoid cyst resection or revision detethering. We had discussed the options of cyst excision, revision detethering, and spinal column shortening with our patient, and her case was reviewed at multidisciplinary spine conference. At conference, the cyst itself was not felt to be causing severe cord compression, and the patient had been seen by neurologists, who felt that her symptoms localized to her spinal cord. The totality of the clinical picture was presented to the patient, and because she lived in another state, she wished to receive the most aggressive procedure to give her the best chance of halting neurological progression. Thus, the patient chose to have cyst excision, spinal column shortening, and fusion over the kyphotic apex.
Our current case is unique because the patient concurrently had an arachnoid web at the osteotomy level, affording the rare indication to intentionally open the dura and directly visualize the spinal cord after spinal column shortening. Previous anatomical studies have shown that the optimal decrease in tension in the filum and neural elements is within the range of a 12- to 16-mm vertebral column resection.19,20 In our case, we achieved an approximate 15-mm reduction in length, and dural buckling was noted. Intradural visualization of the cord and neural elements after the osteotomy and shortening revealed that although dural buckling was present, there did not appear to be buckling or kinking of the underlying neural elements themselves.
Lessons
Our case provides a rare opportunity to visualize the spinal cord after spinal column shortening via three-column osteotomy. This report illustrates that although the dura may be significantly buckled, the underlying neural elements are neither buckled nor kinked after a three-column osteotomy and a 15-mm spinal column shortening at T6.
Disclosures
Dr. Agarwal reported royalties from Thieme Medical Publishers and Springer International Publishing outside the submitted work. Dr. Mummaneni reported personal fees from Depuy Synthes, Stryker, Globus, Springer International Publishing, and Thieme Publishers outside the submitted work and grants from Neurosurgery Research & Education Foundation (NREF), AO Spine, International Spine Study Group (ISSG), and the National Institutes of Health. Dr. Chou reported personal fees from Globus and Orthofix outside the submitted work.
Author Contributions
Conception and design: Zhao, Shabani, Chou. Acquisition of data: Agarwal, Chou. Analysis and interpretation of data: Shabani, Agarwal, Chou. Drafting the article: Zhao, Shabani. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Zhao. Administrative/technical/material support: Shabani. Study supervision: Chou.
References
- 1. Lee GY, Paradiso G, Tator CH, Gentili F, Massicotte EM, Fehlings MG. Surgical management of tethered cord syndrome in adults: indications, techniques, and long-term outcomes in 60 patients. J Neurosurg Spine. 2006;4(2):123–131. doi: 10.3171/spi.2006.4.2.123. [DOI] [PubMed] [Google Scholar]
- 2. Lapsiwala SB, Iskandar BJ. The tethered cord syndrome in adults with spina bifida occulta. Neurol Res. 2004;26(7):735–740. doi: 10.1179/016164104225017956. [DOI] [PubMed] [Google Scholar]
- 3. Pang D, Wilberger JE., Jr Tethered cord syndrome in adults. J Neurosurg. 1982;57(1):32–47. doi: 10.3171/jns.1982.57.1.0032. [DOI] [PubMed] [Google Scholar]
- 4. Phuong LK, Schoeberl KA, Raffel C. Natural history of tethered cord in patients with meningomyelocele. Neurosurgery. 2002;50(5):989–995. doi: 10.1097/00006123-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 5. Steinbok P, MacNeily AE. Section of the terminal filum for occult tethered cord syndrome: toward a scientific answer. Neurosurg Focus. 2007;23(2):E5. doi: 10.3171/FOC-07/08/E5. [DOI] [PubMed] [Google Scholar]
- 6. Lew SM, Kothbauer KF. Tethered cord syndrome: an updated review. Pediatr Neurosurg. 2007;43(3):236–248. doi: 10.1159/000098836. [DOI] [PubMed] [Google Scholar]
- 7. Mehta VA, Bettegowda C, Ahmadi SA, et al. Spinal cord tethering following myelomeningocele repair. J Neurosurg Pediatr. 2010;6(5):498–505. doi: 10.3171/2010.8.PEDS09491. [DOI] [PubMed] [Google Scholar]
- 8. Thuy M, Chaseling R, Fowler A. Spinal cord detethering procedures in children: a 5 year retrospective cohort study of the early post-operative course. J Clin Neurosci. 2015;22(5):838–842. doi: 10.1016/j.jocn.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 9. Hsieh PC, Stapleton CJ, Moldavskiy P, et al. Posterior vertebral column subtraction osteotomy for the treatment of tethered cord syndrome: review of the literature and clinical outcomes of all cases reported to date. Neurosurg Focus. 2010;29(1):E6. doi: 10.3171/2010.4.FOCUS1070. [DOI] [PubMed] [Google Scholar]
- 10. Kokubun S. Shortening spinal osteotomy for tethered cord syndrome in adults. Spine Spinal Cord. 1995;8(12 suppl):5. [Google Scholar]
- 11. Aldave G, Hansen D, Hwang SW, Moreno A, Briceño V, Jea A. Spinal column shortening for tethered cord syndrome associated with myelomeningocele, lumbosacral lipoma, and lipomyelomeningocele in children and young adults. J Neurosurg Pediatr. 2017;19(6):703–710. doi: 10.3171/2017.1.PEDS16533. [DOI] [PubMed] [Google Scholar]
- 12. McVeigh LG, Anokwute MC, Belal A, et al. Spinal column shortening for secondary tethered cord syndrome: radiographic, clinical, patient-reported, and urodynamic short-term outcomes. J Neurosurg Pediatr. doi: 10.3171/2020.11.PEDS20847. Published online May 7, 2021. doi: 10.3171/2020.11.PEDS20847. [DOI] [PubMed] [Google Scholar]
- 13. Nakashima H, Imagama S, Matsui H, et al. Comparative study of untethering and spine-shortening surgery for tethered cord syndrome in adults. Global Spine J. 2016;6(6):535–541. doi: 10.1055/s-0035-1569004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hsieh PC, Ondra SL, Grande AW, et al. Posterior vertebral column subtraction osteotomy: a novel surgical approach for the treatment of multiple recurrences of tethered cord syndrome. J Neurosurg Spine. 2009;10(4):278–286. doi: 10.3171/2008.10.SPINE08123. [DOI] [PubMed] [Google Scholar]
- 15. Kokubun S, Ozawa H, Aizawa T, Ly NM, Tanaka Y. Spine-shortening osteotomy for patients with tethered cord syndrome caused by lipomyelomeningocele. J Neurosurg Spine. 2011;15(1):21–27. doi: 10.3171/2011.2.SPINE10114. [DOI] [PubMed] [Google Scholar]
- 16. Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurg Clin N Am. 2007;18(3):531–547. doi: 10.1016/j.nec.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 17. Lagae L, Verpoorten C, Casaer P, Vereecken R, Fabry G, Plets C. Conservative versus neurosurgical treatment of tethered cord patients. Zeitschrift für Kinderchirurgie. 1990;45(suppl 1):16–17. doi: 10.1055/s-2008-1042626. [DOI] [PubMed] [Google Scholar]
- 18. Maher CO, Goumnerova L, Madsen JR, Proctor M, Scott RM. Outcome following multiple repeated spinal cord untethering operations. J Neurosurg. 2007;106(6 suppl):434–438. doi: 10.3171/ped.2007.106.6.434. [DOI] [PubMed] [Google Scholar]
- 19. Grande AW, Maher PC, Morgan CJ, et al. Vertebral column subtraction osteotomy for recurrent tethered cord syndrome in adults: a cadaveric study. J Neurosurg Spine. 2006;4(6):478–484. doi: 10.3171/spi.2006.4.6.478. [DOI] [PubMed] [Google Scholar]
- 20. Safain MG, Burke SM, Riesenburger RI, Zerris V, Hwang SW. The effect of spinal osteotomies on spinal cord tension and dural buckling: a cadaveric study. J Neurosurg Spine. 2015;23(1):120–127. doi: 10.3171/2014.11.SPINE14877. [DOI] [PubMed] [Google Scholar]
- 21. Lin W, Xu H, Duan G, et al. Spine-shortening osteotomy for patients with tethered cord syndrome: a systematic review and meta-analysis. Neurol Res. 2018;40(5):340–363. doi: 10.1080/01616412.2018.1446268. [DOI] [PubMed] [Google Scholar]
- 22. Safaee MM, Winkler EA, Chou D. Mini-open spinal column shortening for the treatment of adult tethered cord syndrome. J Clin Neurosci. 2017;44:315–319. doi: 10.1016/j.jocn.2017.07.037. [DOI] [PubMed] [Google Scholar]
- 23. Zhang C, Chang C-C, Mummaneni PV, et al. Spinal column shortening versus revision detethering for recurrent adult tethered cord syndrome: a preliminary comparison of perioperative and clinical outcomes. J Neurosurg Spine. 2020;32(6):1–7. doi: 10.3171/2019.12.SPINE19659. [DOI] [PubMed] [Google Scholar]