Abstract
The fascinating scientific history of phage therapy has been documented in numerous publications. In this study, however, we focus on an angle of the story that hitherto has remained relatively neglected, namely, phage therapy treatments, and the protagonists that conducted these in Mandatory-Palestine and subsequently the state of Israel, as part of a global trend. We complete the story by describing efforts in the new era of phage therapy in present-day Israel.
Keywords: phage therapy, Mandatory-Palestine, phage history, Israel phage bank
Introduction
The use of bacteriophages as antibacterial therapeutics is a unique scientific and historical story, with ups and downs spanning more than a century. This story can be divided into several chapters, the early golden age of the discovery and clinical use of phages (“Phage Therapy I”: 1919 to ∼1950), the neglect of phage as antimicrobials in most parts of the world (“The Middle Ages”: ∼1950 to ∼2005), and the recent reintroduction of phage in modern medicine (Phage Therapy II: 2005–the present).
With regard to Israel, ∼90 years separate the first documented clinical application of phage in Mandatory-Palestine (the land of Israel under the rule of the British Empire between 1917 and 1948), in 19291 and 2018, during the “Phage Therapy II” era, when phages were clinically administered for the first time in Israel.2
In this review, we aim to tell the forgotten story of the first phage therapy attempts in Mandatory-Palestine, the few applications that were developed in subsequent years, and the current re-emergence and status of phage therapy in Israel.
Global “Phage therapy I” (1919–1950)
Pieces of evidence relating to phage activity were described as early as 1896, when Hankin observed bactericidal action in the Ganges and Jumna rivers of India.3 However, the discovery of phage is attributed to the British microbiologist Frederick William Twort (1915) and independently to the French Canadian microbiologist Felix d'Hérelle in 1917.4,5 In 1919, d'Hérelle successfully administered phage for the first time as antibacterial therapeutics,4 and soon thereafter, during the first decades of the 20th century, the use of phage as therapeutic agents spreads worldwide.
In 1923, the first phage-therapy institute was established in Tbilisi, Georgia, by d'Hérelle and George Eliava, later named “the Eliava Institute of Bacteriophage, Microbiology & Virology.” For ∼80 years, this institute remained the largest facility in the world for therapeutic-phage preparations and treatments, supplying a major proportion of the clinical phages in the USSR,4 wherein among other uses, they were applied for the treatment of purulent infections and gangrene4 and against cholera.5
In 1927, d'Herelle applied phage for the treatment of patients suffering from cholera in India's Punjab region, thereby reducing mortality rates,5 and in the early 1930s, phages were applied in the United States for a wide range of indications, including dermal and ophthalmological cases.6,7 Simultaneously, commercial companies and research institutes commenced the mass production of phage preparations.7 In Germany, the bacteriophage society began selling tablets of dried phage, and the company Antipiol produced a preparation named Enterofagos.8
Medicine and Biological Research in Mandatory-Palestine and the Young State of Israel
In 1917, during the latter stages of World War I, the British Empire seized the territories of so-called Palestine–Israel from the Ottoman Empire. The League of Nations mandated the British administration with the “Mandate for Palestine and Transjordan areas,” which continued until 1947 when the UN General Assembly voted on Resolution 181, leading to the mandate termination and the establishment of the state of Israel in May 1948.
Several factors documented in the history of medicine in British-ruled Mandatory-Palestine, particularly phage therapy, make interesting reading. First, the high percentage of Jewish immigrants and settlers (also known in Hebrew as “Ha-Yishuv”) in prestate Israel were scholars from different countries specializing in diverse fields. Second, the prioritization of advancements in science and technology by the “Ha-Yishuv” leadership, despite the constant existential threat and resource shortages. And, third, the transition from an Eastern European-oriented society to one more conspicuously pro-Western.
During the onset of Mandatory-Palestine in 1917, the number of Jewish physicians who practiced medicine in the country was 63. In 1918, the Women's Zionist Organization of America “Hadassah,” founded in 1912 in New York by Henrietta Szold with the aim of promoting medicine in Israel,9 established the American Zionist Medical Unit (AZMU). The impact of AZMU organization was remarkable and reflected the “importation” of American medical–scientific knowledge to Mandatory-Palestine9–11 coinciding with a flourishing of medical services offered by Hadassah and also by other health care providers.12,13
In parallel, immediately after establishing the British Mandate in 1918, the cornerstone of the Hebrew University, the second academic institute to be established in the land of Israel (the first being the Technion established in Haifa in 1912), was laid in Jerusalem, and in 1925, supported by Albert Einstein, the Hebrew University was formally established with two institutes, namely Jewish and Chemistry Studies and the Department of Hygiene and Bacteriology, headed by Kligler (described in “Phage Therapy I in Mandatory-Palestine and the Young State of Israel [1929–1950]” section). During the initial years of its existence, this department focused primarily on malaria, the environmental and nutritional aspects of infections, and the etiology and epidemiology of leishmaniasis, dengue fever, and intestinal infections.14
In 1934, the Hebrew University and Hadassah, in a collaboration that endures to this day, established the University Medical Center in Mount Scopus, Jerusalem, which since 1945 has held the Medical School of the Hebrew University. This school, which in 1960 moved to Ein Kerem Campus in Jerusalem, has become one of Israel's leading medical centers and schools. Notably, the center is credited with both the early development of phage-based therapy at the beginning of the 20th century and the current initiatives taking place almost a century later (described in “Clinical Applications of Phage Therapy in Israel [2018–2022]” section).
During the 1930s, a wave of Jewish refugees fleeing from Nazi persecution in Germany and other central European countries emigrated to Mandatory-Palestine, many of whom were qualified physicians, lawyers, engineers, and teachers. Consequently, by 1935, the orientation of medical disciplines had undergone a transition from an eastern European (Russian and Polish) to German perspective.15,16
Phage Therapy I in Mandatory-Palestine and the Young State of Israel (1929–1950)
As part of the burgeoning global interest in phage in the 1930s to 1950s, research in Mandatory-Palestine was led by two prominent researchers, Kligler and Olitzki, who were based at the Hadassah-Hebrew University Medical Center.1,17
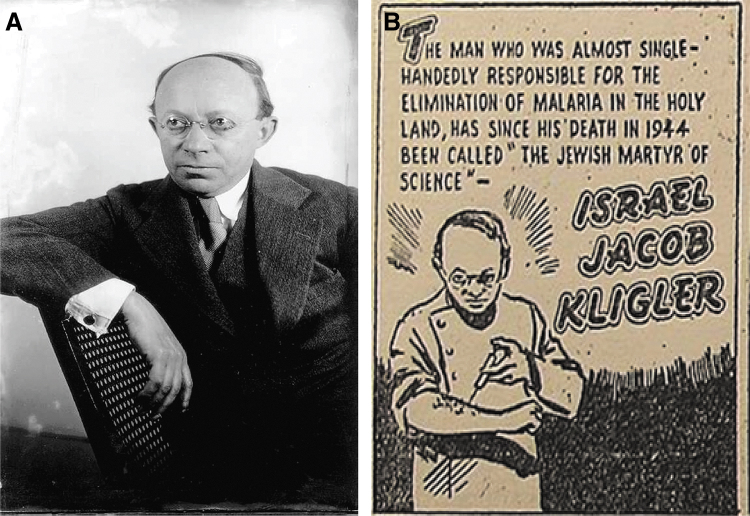
Kligler (Fig. 1A), born in the Austro–Hungarian Empire, was educated in the United States and emigrated to Israel as part of the AZMU initiative. He subsequently spent most of his career as a microbiologist in Mandatory-Palestine, as one of the first four professors of the Hebrew University and founder of the aforementioned department of hygiene and bacteriology, which he headed until his death in 1944.17 As one of the pioneers of modern medical research in Mandatory-Palestine, Kligler focused specifically on the many aspects of infectious diseases, including malaria and sandfly fever, and epidemiology. Among his achievements is the well-known Kligler iron medium, which is still routinely used to differentiate between enterobacteria.18
FIG. 1.
(A) Israel-Jacob Kligler (1925–1944) was the founder and head of the department of hygiene and bacteriology, and among the first four professors of the Hebrew University. Kligler was one of the pioneers of modern medical research in Mandatory-Palestine and the state of Israel. (Courtesy of the Central Zionist Archive). (B) A caricature published in the American Jewish journal The Southern Jewish Weekly, published on October 31, 1947, (from Wikipedia) depicting Kligler injecting himself with medicine against malaria. This picture reflects the main focus of Kligler's work in striving to eradicate malaria and other infections from Israel.
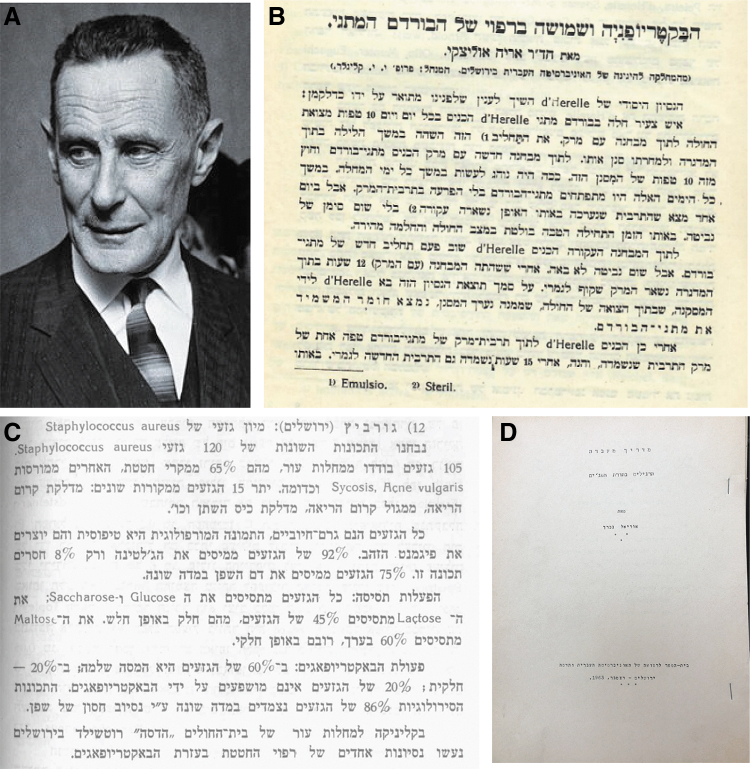
Olitzki (Fig. 2A), born in eastern Prussia in 1898, studied medicine in Braslau and Berlin, before immigrating to Mandatory-Palestine in 1924. Initially, he worked for 2 years as a researcher in the Hadassah Hospital in Jerusalem, after which he spent 2 years at Safed in northern Israel, subsequently returning to the Hebrew University in Jerusalem.19 Here, Olitzki established himself as one of the pioneers of bacteriology and epidemiology in pre-State Israel, and in 1967 was awarded the Israel Prize in Medicine for both fields.20,21
FIG. 2.
(A) Aryeh Leo Olitzki, a professor of microbiology at the Hebrew University of Jerusalem, was awarded the Prize of Israel for Medical Research in 1969. (Photograph by David Harris, Credit: The Wellcome Collection). (B) Olitzki's 1929 article, published in “Harefua,” the Journal of the Israeli Medical Association, in which he describes a phage-based treatment for dysentery conducted in Mandatory-Palestine.1 (C) Abstract number 12 from the second Microbiological Conference in Mandatory-Palestine, in which Gurevich from the Hadassah Hospital in Jerusalem describes using phages for bacterial typing and clinical use against acne vulgaris.41 This abstract states in Hebrew that “The bacteriophage activity against 120 strains of S. aureus resulted in a complete lysis in 60% of the strains, partial lysis in 20%, and no effect in 20%,” and that “Several attempts of treating acne vulgaris with bacteriophages were performed in Hadassah Rothschild Hospital in Jerusalem.”41 (D) A laboratory manual for students, titled (in Hebrew) “Exercise in Phage Studies,” from the Hebrew University and Hadassah Medical School, 1963, written by Uriel Bachrach.
In 1929, Olitzki published an article1 containing the first reference we found of phage therapy in Mandatory-Palestine (Fig. 2B). This article was published in Hebrew in “HaRefua” (Hebrew: “The medicine”), a local journal that continues to be published today as the Journal of the Israeli Medical Association (https://www.ima.org.il/ENG/). In this article, Olitzki presents an updated account of the findings and controversies regarding the phage therapy treatments conducted by d'Hérelle.1
Interestingly, although only as a side note, he also briefly describes the historical first phage therapy in Mandatory-Palestine for the treatment for dysentery that took place in Tel Aviv, although without providing details of patient numbers or the origin of the phages used. Nevertheless, despite a remarkable clinical improvement after phage administration in at least 12 pediatric patients, Olitzki states that, as both treated and untreated groups showed rapid improvement, it was not possible to conclude whether the patients had benefited from the phage-based treatment, writing the (from Hebrew): “…The results achieved last summer in Tel Aviv in the treatment of dysentery using the bacteriophage were not clear enough to justify any support in favor of this method…”.1
Today this skepticism might be considered rather conservative, given that it was written before the introduction of antibiotics and the fact that at that time, phage probably represented the best available option for treating severe infections. Nevertheless, Olitzki concluded the article with a recommendation for controlled trials to further assess the efficacy of phage therapy.
In this article, Olitzki also proposes a hypothesis that remains valid to this day, namely, that the efficacy of phage-based therapy might be mediated through an induction of a patient's immune response. However, Olitzki's interest in phages did not end there, as is evident from the fact that between 1931 and 1934, he published a series of articles focusing on phage research,22–25 in one of which, he discusses methods for phage purification,26 which was subsequently cited by Sandholzer et al. in an article published in Science in 1937.27
Olitzki's abiding interest in phages is reflected in a document discovered in the Hebrew University archives, describing a course with a series of seminars held in the department of hygiene and bacteriology. In this course, a talk titled (translated from Hebrew) “New methods in bacteriophages and viruses growth” (Supplementary Fig. S1) was presented by a young female graduate student, Genia Goldwasser, a Polish immigrant who may at that time have gained experience of phage therapy in Poland.28
It seems probable that Goldwasser and the other researcher were inspired by the works of the prominent Jewish Polish microbiologist Bronisława Fejgin, one of the pioneers in phage research, whose life story has only recently come to light.28–30 Fejgin, who was in correspondence with d'Hérelle, contributed significantly to our understanding of phages, including her observation that bacteria in the genus Proteus possess lysogens31 and that the efficacy of phages can be enhanced by “training” these to attack their target,28 a technique still employed today.32,33 It has even been suggested that the discovery of phage by Twort and d'Hérelle was perhaps influenced by Fejgin's preliminary research describing a lytic agent.30
Unfortunately, as a Jew, Fejgin was deported to the Warsaw ghetto by the Nazis, wherein she became head of the bacteriology department of the Ghetto's Chemical-Bacteriological Institute and struggled against a terrible typhus epidemic that raged through the Ghetto during this time. Regrettably, in 1943, she was murdered in the Ghetto during a spate of mass deportations.
In 1934, Olitzki published a study in the Journal of Experimental Pathology on the properties of viral proteins, in which he describes how the reactions of purified protein-free phage (seemingly phage DNA) differed from those of wild-type phage under several different conditions, including different electrical polarities.22 Notably, the coauthor of this article was the aforementioned second phage research pioneer in prestate Israel, Kligler, who in his research at this time established methods for inhibiting phage activity, thereby facilitating bacterial growth.34–36
Subsequently, in 1943, Kligler coauthored two additional articles describing the clinical isolation of phages and associated laboratory research,35,36 whereas in 1948, Olitzki et al. described the use of phages in bacterial typing.37 In the same year, in an article on mucins, Olitzki also mentions a list of modalities for the treatment of pathogenic bacteria: “chemotherapeutic agents, antibiotics, and bacteriophages,” an indication of the therapeutic potential he envisaged for bacteriophages.38
Apart from Olitzki and Kligler, there were a number of other clinicians and microbiologists in the prestate of Israel with a clear interest in phage therapy, among whom was Rokach,39 a physician who served as chairman of the Jerusalem Medical Association for >17 years. In 1931, Rokach published a review summarizing an article by Sonnenschein and Koch from 1930, in which they describe using phage therapy in the treatment of paratyphoid fever.40
Furthermore, in 1937, as a contributor to the second Microbiological Conference of Mandatory-Palestine, a clinician named Gurevich who was a member of the microbiology department of Hadassah Hospital in Jerusalem, published an abstract “HaRefua” describing phage therapy in the treatment of acne vulgaris (Fig. 2C).41 This study established that the susceptibility of 60% of the isolates to phages was high, whereas 20% was intermediate, and remaining 20% were resistant. Interestingly these numbers are consistent with those reported more recently,42,43 including our observations in Israel,44 indicating an ∼80% susceptibility of Cutibacterium acnes to phages.
However, despite the aforementioned interest in phage, and although the current review is primarily concerned with phage therapy, it should be noted that the main focus of research performed in prestate Israel by Olitzki, Kligler, Rokach, Gurevich, and others was not associated with phage therapy, but primarily linked to malaria, which was viewed at the time as the “enemy of the Zionist enterprise”.9,45,46 This notion is evident from the numerous articles on malaria published by these researchers and also the assignment of Kligler as the deputy of Malaria affairs in Mandatory-Palestine (Fig. 1B).
The “Middle Ages” of Global Phage Therapy (1950–2005)
In Western countries, the “golden era” of phage therapy research came to an end during the 1940s and 1950s in the aftermath of the World War II. In retrospect, this wane in interest was perhaps an inevitable consequence of the combination of negative results and controversies regarding the antibacterial efficacy of phage therapy, mainly associated with inefficient purification and preservation, failure in matching techniques and clinical procedure, and the unavailability of genome sequencing methods at that time.5,28,47 A further contributor to this decline was undoubtedly the phenomenal success and numerous advantages of the newly discovered antibiotics,48 as simple nonmultiplying highly efficient molecules with a wide range of activities.
In contrast, phages are complex multiplying entities with comparatively narrow host ranges that are generally difficult to predict. Moreover, phage therapy was not only abandoned by Western clinicians, it was even prohibited and denounced as a nonserious “pseudo-science of the Bolsheviks”,49 similar to several other scientific discoveries made in Eastern Europe at that time.50
Nevertheless, whereas phage-based therapy was largely ignored in the West, researchers worldwide continued to conduct extensive basic scientific studies of phages, which led to numerous significant findings that contributed to establishing the basis of molecular biology as we know it today,51 and indeed is reflected in the multiple Nobel Prizes awarded for phage-related research.
Some notable examples in the latter regard include the study of Jacob, Monod, and Lwoff, who received the Nobel Prize in 1965 for the genetic control of enzyme and virus synthesis52; Delbrück, Hershey, and Luria, who were awarded the Nobel Prize in 1969 for the discovery of replication mechanisms and the genetic structure of viruses; Arber, Nathans, and Smith, who won the prize in 1978 for the discovery of restriction enzymes and their application to problems of molecular genetics; and Smith and Winter, who received the prize in 2018 for the discovery of phage display of peptides and antibodies, the findings of each of which revolutionized scientific knowledge and led to the development of novel molecular biology technologies.53
This trend has continued to the present day, with Charpentier and Doudna being awarded the 2020 Nobel Prize for Chemistry for development of a method for genome editing using the CRISPR/Cas systems, which is a component of a bacterial immune system induced in response to phage infection.51
In contrast to the West, throughout the postwar period, researchers in phage therapy centers in Eastern Europe, mainly Georgia, Poland, and Russia, continued to work tirelessly despite the difficulties presented by the subsequent advent of the Cold War, fall of the Soviet Union, and numerous national and political crises, compounded by a general disregard from the West.
Israeli Phage Therapy During the “Middle Ages”
During the 1950s, on more than one occasion, phage therapy was discussed in the Israeli media. In 1950, the journalist Segal published two reviews in “Herut,” a magazine of the rightwing political movement Herut, in which he described phages and detailed the therapeutic studies of d'Herelle.54,55
In 1958, Olitzki published a similar article titled “Healing by Bacteriophages,” this time, in the leftwing socialist daily newspaper “Davar,” in which he highlighted the problematic emergence of antibiotic-resistant strains and the need for effective alternatives to antibiotics. This article described the isolation of phages from sewage collected from a site adjacent to Hadassah Hospital in Tel-Aviv56 and their use in eliminating the causal bacteria of typhoid fever. Also mentioned is an unsuccessful attempt to cure an outbreak of dysentery among German prisoners of war during World War II in North Africa.56
Furthermore, he raised an interesting point, still relevant today, that compared with living tissue, phages might behave quite differently in a laboratory setting, on the basis of which he emphasized the need to develop precise matching of phages to bacterial targets, a concept encompassed today in the discipline of “clinical phage microbiology.”57
These few examples notwithstanding, during these years, along with much of the Western world, a declining interest in phage therapy was also clearly apparent in the state of Israel, mainly associated with the increasing prominence of antibiotics, previously introduced to Mandatory-Palestine by the British army and authorities.
A further factor contributing to the neglect of phage therapy in Israel was a general shift from the ideological, cultural, technological, and scientific perspectives of the Eastern Bloc to a more pro-Western outlook during the 1950s and 1960s. This process was completed in 1967 after the Six-Day War, when all the Eastern Bloc countries, with the exception of Romania, proceeded to break their diplomatic ties with Israel.
In 1963, phage biology was taught in Israel for the first time in a dedicated course run by Uriel Bachrach at the Microbiology Institute of the Hebrew University of Jerusalem (Fig. 2D), and throughout the 1960s and thereafter, research on phages was conducted in the Israel Institute for Biological Research (IIBR), led by Renana Leshem-Ben Gurion, the daughter of David Ben Gurion, who at this time focused mainly on the induction of lysogens.58,59 Given the nature of the study undertaken at the IIBR, it seems probable that her team also conducted studies related to phage therapy.
Throughout the period spanning the 1970s to 1990s, as in most Western countries, phage therapy appears to have been almost completely abandoned in Israel, and indeed, we were unable to find any references to phage therapy during these years. Most of the Israeli phage-related scientific publications and newspaper articles from this time tended to focus on the findings and breakthroughs that were achieved using phages,60 many of which describe studies on phage elements61–63 that were subsequently used as essential tools in developing the field of molecular biology.64 In contrast, little or no consideration was given to the application of phage as viable therapeutic alternatives to antimicrobial agents.
Moreover, even Amos Oppenheim (1934–2006), a leading Israeli phage researcher from the Hebrew University, whose significant discoveries regarding Lambda phage contributed to its subsequent adoption as a model organism in molecular biology,65–68 was seemingly uninvolved in phage therapy. Nonetheless, a notable exception during this period was the biotechnology company Biolum, established in the 1980s by Jonathan Kuhn and Shimon Ulitzur, two researchers from the Technion Faculty of Biology, which applied phages as a means of diagnosing bacteria such as Salmonella in different food sources.69
Global Phage Therapy II (2005–Present Day)
Over the past 50 years, bacterial antibiotic resistance has emerged as a pervasive major medical threat, exacerbated in recent years by the excessive use of these agents.70–72 Given this situation and the necessity to develop a more diverse arsenal of antimicrobial tools, phage therapy has been regaining interest in the West since the beginning of the 21st century, as among the potentially most promising solutions to avert this crisis. This trend is reflected in the establishment of phage therapy centers in several countries, including the Queen Astrid Military Hospital in Brussels, Belgium,73 the University of Sydney, Australia,74 IPATH in San Diego,75 and the CRIOAc center in Lyon, France.76
In addition, pioneering modern clinical trials utilizing phage therapy are being actively conducted. Among these were the PhagoBurn trial (2013–2017), in which the efficacy of topical application of phage for the treatment of infected burn wounds was examined,77 and trials assessing oral phage therapy for acute bacterial diarrhea conducted by Nestlé Research Centre and the International Centre for Diarrheal Diseases Research in Bangladesh,78 and others.79,80
In the United States in 2016, ∼90 years after the last therapeutic use of phage in the country, a significant breakthrough in phage therapy was achieved, in which the life of Tom Patterson was saved upon treatment with systemic phages against Acinetobacter baumannii, which was deemed resistant to all assessed antibiotics.81 This treatment, performed at the University of California in San Diego, paved the way for the establishment IPATH, the first phage therapy center in North America.75
This seminal episode is fascinatingly recounted in the book The Perfect Predator: A Scientist's Race to Save Her Husband from a Deadly Superbug: A Memoir, penned by his wife Steffanie Strathdee, who herself subsequently became profoundly involved in phage therapy. Since that time, the interest in phage therapy has risen markedly worldwide, as evidenced by the burgeoning number of phage therapy-related publications, dedicated conferences, compassionate treatments, clinical trials, phage therapy centers and clinics, and phage-based companies.
Israeli Phage Therapy II
During the first years of the 21st century, phage therapy also regained considerable attention in Israel, which likewise faces a worrying increase in cases involving antibiotic-resistant pathogens.82 In 2013, Israel's State Comptroller published a report indicating that ∼5000 patients die annually in Israel from infections associated with bacterial resistance,83 and their numbers are on the rise, as reflected by the fact that with each passing year, an even greater number of bacteria are being defined as problematic.
The new dawn of phage therapy in Israel appeared as early as the second decade of the 21st century when Eugene Rosenberg, a microbiologist at the Faculty of Life Sciences at Tel Aviv University, used phage to treat coral infections. He focused on the two coral pathogens Vibrio coralliilyticus and Thalassomonas loyana, which are known to cause disease outbreaks worldwide, which were treated with phages isolated from coral reefs in the Red Sea or the Great Barrier Reef in Australia. Notably, these experiments were conducted both in the laboratory and in natural settings in the sea, the results of which indicated that the application phages offered significant protection to corals from bacterial infection, whereas 61% of untreated corals were infected and only 5% were infected when phages were applied by dispersing near a reef.84,85
In 2000, Asher Wilf and Sergey Bujanover established the phage biotech company “Phage-Biotech,” with a specific focus on tailored phage applications in health, food safety, veterinary medicine, agriculture, aquaculture, and fermentation, and in 2018, they introduced AgriPhage™, a registered biopesticide that prevents and controls phytopathogenic bacteria infecting tomato and pepper plants.
The IIBR has also recently begun to explore the realms of phage therapy, describing the application of phages for the clinical treatment and rapid detection of Yersinia pestis.86–88
In addition, several phage-related companies have been established during the past 5 years, including “BIOMX” that trades on Nasdaq and aims to employ phage in the treatment of several medical conditions, including cystic fibrosis (CF) and inflammatory bowel disease; “EcoPhage,” which is exploring phage-based solutions for agriculture infections; and “Trobix Bio,” which has developed several phages-based applications and antimicrobials.
Clinical Applications of Phage Therapy in Israel (2018–2022)
Less than 2 years after Patterson's revolutionary treatment in San Diego, Israel joined the exclusive club of countries treating patients with phages, when our team from the Hebrew University of Jerusalem and Hadassah Medical Center performed the first new-era treatments in the country.2 Our first patient, treated in June 2018, had contracted a trauma-related left tibial polymicrobial infection caused by extensively drug-resistant A. baumannii and multiple drug resistance Klebsiella pneumoniae, which had persisted for >14 weeks, on account of unsuccessful antibiotic regimens.2
On the basis of thorough in vitro simulations of the complex polymicrobial environment, we selected a combined treatment comprising phages and antibiotics. The treatment, performed at Hadassah Medical Center, entailed the administration of IV doses of two phages (one for each pathogen) applied generously through adaptive phage therapy, combined with the prolonged administration of IV antibiotics. Therapy was continued for 11 days, at the end of which, tissues had begun to heal concomitant with a rapid eradication of the causal pathogens.2
Our second patient had suffered an injury 27 years earlier during his military service, the subsequent infection of which had yet to completely heal, until successfully treated in our institute. On the basis of a search for phage that could be applied to target the Pseudomonas aeruginosa isolated from cultures obtained from this patient, we identified PASA16, a highly efficient phage that has been used in several other treatments reported in Israel and globally.89,90
The successful outcomes of these cases prompted us to establish in 2022 the Israeli Phage Therapy Center (IPTC) of the Hebrew University and Hadassa Medical Center in Jerusalem, with the aim of providing comprehensive phage services. To date, in Israel, we have treated several patients with infections attributable to various pathogens, including device-associated bacteremia, osteomyelitis, mastoiditis, and soft tissue infections. In addition, the IPTC is currently participating in an ongoing clinical trial (data not published yet). One important facility of the IPTC is the Israeli Phage Bank (IPB), which at present contains a collection of >500 phages, a majority of which are fully characterized with sequenced genomes that have been established to be virulent against dozens of bacteria.91
The IPB constantly broadening its scope by scanning samples for phages using a range of isolation techniques, “training,” and engineering. Moreover, a number medical and research centers worldwide have benefitted from the IPB phage collection, including the anti-P. aeruginosa phage PASA16, sent to Australia for treatment of an extensive chronic osteoarticular infection89; anti-Enterococcus faecium phages sent to Germany for treatment of a critically ill 1-year-old child suffering from an abdominal infection92; and to Finland for a patient suffering from a K. pneumoniae infection, resistant to all evaluated antibiotic agents and other phages available at the time.93
We have also isolated phages against the Burkholderia isolate from the CF patient Mallory Smith, whose story and treatments with phages have been published globally in the media and the book Salt in my soul.94 Unfortunately, we received the bacterial strain only after she had already passed away.
Future Perspectives
Despite the current consolidation of “Phage Therapy II” initiatives worldwide, including in Israel, the future of phage-based therapy is still unclear. There remain multiple scientific, clinical, and regulatory obstacles that need to be overcome. Both global and Israeli medicine have made significant strides since the “Phage Therapy I” era regarding our knowledge in microbiology and infectious diseases, and since that time, we have seen the development of numerous groundbreaking technologies, including full-genome sequencing, microscopy techniques, and delivery methods. Consequently, the factors that contributed to the abandonment of phage-based therapeutics during the “Phage Therapy I” era, including in Mandatory-Palestine as described here, can be overcome.
We believe that an absence of matching or inaccurate matching may be a significant cause in many of the failures encountered in the past. Consequently, if phage-based therapy is to become a well-established and accepted clinical option, we need to adopt a more prudent approach, such that “Phage Therapy II” does not suffer the same fate as “Phage Therapy I.” In our view, one of the critical aspects of successful phage therapy is the application of rapid and highly accurate clinical phage microbiological techniques57 based on a personalized approach. Furthermore, despite some of the drawbacks of antimicrobials, we are of the opinion that phages should not replace antibiotic treatment, but instead complement it, and if this is to be achieved, clinical phage microbiology needs to incorporate antibiotics as well as immune system matching.
Finally, in our view, the main lesson to be drawn from the stories of phage therapy, both on global scale and in Israel, is the importance of international collaborations. In this regard, the fact that phage therapy was conducted in eastern Europe for decades, during which time it was all but ignored in western Europe, can be attributed to the Iron Curtain and the associated disconnection between western and eastern blocks. From an Israeli perspective, perhaps the key factor contributing to the relative success of Israeli medicine during its infantry was the multidiscipline collaboration of scientists and clinicians who had emigrated to the country from destinations worldwide.
Accordingly, we believe that the key to succeeding in the present-day battle against antibiotic resistance lies in bolstering international collaborative efforts, as has been admirably demonstrated during the recent COVID-19 pandemic.
Indeed, phage therapy researchers and clinicians have already started to pave the road for forging international ties, creating global phage therapy networks such as Phage Directory (https://phage.directory), attending conferences, and sharing registries. Nowadays, it is not exceptional for phages to be isolated in one country, prepared for treatment in a second, and used for treatment in a third. However, concerted efforts should be made to maintain these trends, even in the face of potential disconnections and boycotts due to precipitous events, such as the current invasion of Ukraine.
Supplementary Material
Acknowledgments
We sincerely thank Uriel Bachrach, emeritus professor of the Hebrew University, for fruitful discussions regarding the fundamentals of biological research in Israel. We also thank Professor Yehuda Shoenfeld, chief editor of the “Harefua” journal, for approving the use of figures from the original journal, and staff at the Berman Medical Library of The Library Authority at the Hebrew University of Jerusalem for their assistance. We likewise wish to thank personnel of the Hebrew-University-Archive and the Central-Zionist-Archive for collecting documents and figures for us regarding the study of Kligler and Olytzki and approving their publication.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The authors are supported by the:
1) Israel Science Foundation IPMP Grant #ISF1349/20.
2) Rosetrees Trust Grant A2232.
3) Milgrom Family Support Program.
Supplementary Material
References
- 1. Olitzki AL. Bacteriophages and its use as therapy for rod Bohrdom. Harefuah. 1929;3(2):7–9. [Google Scholar]
- 2. Nir-Paz R, Gelman D, Khouri A, et al. Successful treatment of antibiotic-resistant, poly-microbial bone infection with bacteriophages and antibiotics combination. Clin Infect Dis. 2019;69(11):2015–2018. [DOI] [PubMed] [Google Scholar]
- 3. Abedon ST, Thomas-Abedon C, Thomas A, et al. Bacteriophage prehistory: Is or is not Hankin, 1896, a phage reference? Bacteriophage. 2011;1(3):174–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. D'Herelle F. On an invisible microbe antagonistic toward dysenteric bacilli: Brief note by Mr. F. D'Herelle, presented by Mr. Roux. 1917. Res Microbiol. 2007;158(7):553–554. [DOI] [PubMed] [Google Scholar]
- 5. Chanishvili N. Phage therapy-history from Twort and d'Herelle through Soviet experience to current approaches. In: Łobocka M, Szybalski W, eds. Advances in Virus Research, vol. 83. US: Academic Press Inc., 2012:3–40. [DOI] [PubMed] [Google Scholar]
- 6. Cipollaro AC, Sheplar AE. Therapeutic uses of bacteriophage in the pyodermias. Arch Derm Syphilol. 1932;25(2):280–293. [Google Scholar]
- 7. Town AE, Frisbee FC. Bacteriophage in ophthalmology: A preliminary report. Arch Ophthalmol. 1932;8(5):683–689. [Google Scholar]
- 8. Kutateladze M, Adamia R. Phage therapy experience at the Eliava Institute. Médecine Mal Infect. 2008;38(8):426–430. [DOI] [PubMed] [Google Scholar]
- 9. Nissim Levy YL. On Title Page Verso: Physicians of the Holy Land, 1799–1948. Israel: Itay Bahur Publishing, 2017. [Google Scholar]
- 10. Katvan E. ‘That was the beginning’: The professionalization and Americanization of dentistry in pre-state Israel. J Hist Dent. 2010;58(3):147–156. [PubMed] [Google Scholar]
- 11. Shvarts S, Falchuk N, Mor-Yosef S, et al. Hadassah for the Health of the People: The Health Education Mission of Hadassah: The Ameican Zionist Women in the Holy Land. Dekel Academic Press, 2012. [Google Scholar]
- 12. Shvarts S, Brown TM, Holim K. Dr. Isaac Max Rubinow, and the American Zionist Medical Unit's experiment to establish health care services in Palestine, 1918–1923. Bull Hist Med. 1998;72(1):28–46. [DOI] [PubMed] [Google Scholar]
- 13. Anson O, Soval YT. The main thing is health: social structure and health in Israel. Jerusalem: Magnes Press of the Hebrew University, 2000. [Google Scholar]
- 14. Kligler IJ. Memorandum on the Activities of the Department of Hygiene of the 1926–1928. The Hebrew University Archive, 1928. [Google Scholar]
- 15. Niderland D. The Influence of German-Immigrant Physicians on the Development of Medicine in Israel (1933–1948). An M.Sc thesis of Doron Niderland with the instruction of Moshe Zimmermann from the Hebrew University, Jerusalem, Israel, 1983. [Google Scholar]
- 16. Kirsch DN. Hebrew researchers dream in German: Scientists from Germany at the Hebrew University during the Yishuv period. Galileo 2008;117(1):17–20. [Google Scholar]
- 17. Greenberg Z, Alexander A. Israel Jacob Kligler: The story of “A little big man.” Korot. 2011;21:2011–2012. [Google Scholar]
- 18. Hajna AA. Triple-sugar iron agar medium for the identification of the intestinal group of bacteria. J Bacteriol. 1945;49(5):516–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Levy N, Levy Y. Rofeha shel Erets-Yisrael 1948–1799 = Physicians of the Holy Land, 1799–1948. Israel: Itay Bahur Publishing, 2012. [Google Scholar]
- 20. Grossowicz N. To Prof. AL Olitzky on His 60th Birthday. Harefuah. 1958;54(11):296–301. [PubMed] [Google Scholar]
- 21. Olitzki L. Contribution of bacteriologists for the control of infectious diseases in Palestine. Harofe Haivri Heb Med J. 1947;2:174–180. [PubMed] [Google Scholar]
- 22. Kligler IJ, Olitzki L. Studies on protein-free suspensions of viruses. V: Further observations on the nature and antigenic properties of a highly purified phage. Br J Exp Pathol. 1934;15(1):14. [Google Scholar]
- 23. Kligler IJ, Olitzki L. Studies on protein-free suspensions of viruses. III.—The resistance to heat and disinfectants of protein-free eluates of a bacteriophage and Fowl-pox virus. Br J Exp Pathol. 1931;12(6):393. [Google Scholar]
- 24. Kligler IJ, Olitzki L, Aschner M. Studies on protein-free suspensions of viruses. II.—Cataphoresis experiments with protein-free suspensions of a bacteriophage and Fowl-pox virus. Br J Exp Pathol. 1931;12(3):178. [Google Scholar]
- 25. Kligler IJ, Olitzki L. Studies on protein-free suspensions of viruses. I.—The adsorption and elution of bacteriophage and Fowl-pox virus. Br J Exp Pathol. 1931;12(3):172. [Google Scholar]
- 26. Kligler IJ, Olitzki L. Purification of phage by adsorption and elution. Proc Soc Exp Biol Med. 1933;30(9):1365–1367. [Google Scholar]
- 27. Sandholzer LA, Mann MM, Berry GP. Determination of ultra-violet light absorption by certain bacteriophages. Science (80−.). 1937;86(2222):104–105. [DOI] [PubMed] [Google Scholar]
- 28. Żaczek M, Weber-Dąbrowska B, Międzybrodzki R, et al. Phage therapy in Poland—A Centennial journey to the first ethically approved treatment facility in Europe. Front Microbiol. 2020;11:1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Weisz GM. Remembering Jewish physicians. Isr Med Assoc J. 2015;17(4):203–205. [PubMed] [Google Scholar]
- 30. Grzybowski A, Żaczek M, Górski A, et al. Bronisława Fejgin (1883–1943): Forgotten important contributor to international microbiology and phage therapy. Antibiotics. 2021;10(11):1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fejgin B. On the sudden variations of Proteus HX19 occurring under the influence of the anti-HX19 lytic agent and their relationship with the strains isolated from guinea pigs infected with the passage virus of exanthematous typhus. CR Soc Biol. 1924;90:1106–1108. [Google Scholar]
- 32. Abdelsattar AS, Dawooud A, Rezk N, et al. How to train your phage: The recent efforts in phage training. Biologics. 2021;1(2):70–88. [Google Scholar]
- 33. Borin JM, Avrani S, Barrick JE, et al. Coevolutionary phage training leads to greater bacterial suppression and delays the evolution of phage resistance. Proc Natl Acad Sci USA. 2021;118(23):e2104592118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Olitzki L. In memoriam of Israel Kligler. Harefuah. 1944;27:185–189. [Google Scholar]
- 35. Kligler IJ, Oleinik E. Inactivation of phage by aldehydes and aldoses and subsequent reactivation. J Immunol. 1943;47(4):325–333. [Google Scholar]
- 36. Kligler IJ, Oleinik E, Czazkes I. Improved technic for isolation of dysentery bacteria from stools by formaldehyde inactivation of bacteriophage. Am J Public Health Nations Health. 1943;33(6):682–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Olitzki AL, Shelubsky M, Strauss W. Typing of typhoid bacteria and its value in epidemiological research in Palestine. Harefuah. 1948;34(9):105–107. [PubMed] [Google Scholar]
- 38. Olitzki L. Mucin as a resistance-lowering substance. Bacteriol Rev. 1948;12(2):149–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rokach YL. Bacteriophage Paratyphus therapy. Harefuah. 1931;5:37. [Google Scholar]
- 40. Sonnenschein C, Koch F El. Bacteriophagebehandlung bei Paratyphus. Dtsch Arch Klin Med. 1930;167:294–301. [Google Scholar]
- 41. Gorevich. Second Israeli Bacteriologist conference. Harefuah. 1937;13:57. [Google Scholar]
- 42. Castillo DE, Nanda S, Keri JE. Propionibacterium (Cutibacterium) acnes bacteriophage therapy in acne: Current evidence and future perspectives. Dermatol Ther (Heidelb). 2019;9(1):19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Brüggemann H, Lood R. Bacteriophages infecting Propionibacterium acnes. Biomed Res Int. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sheffer-Levi S, Rimon A, Lerer V, et al. Antibiotic susceptibility of Cutibacterium acnes strains isolated from Israeli Acne Patients. Acta Derm Venereol. 2020;100(17): adv00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sufian SM. Healing the Land and the Nation: Malaria and the Zionist Project in Mandatory-Palestine, 1920–1947. New York University, 1999. [Google Scholar]
- 46. Sufian S. Colonial malariology, medical borders, and sharing scientific knowledge in Mandatory-Palestine. Sci Context. 2006;19(3):381–400. [DOI] [PubMed] [Google Scholar]
- 47. Eaton MD, Bayne-Jones S. Bacteriophage therapy: Review of the principles and results of the use of bacteriophage in the treatment of infections. J Am Med Assoc. 1934;103(23):1769–1776. [Google Scholar]
- 48. Reardon S. Phage therapy gets revitalized. Nat News. 2014;510(7503):15. [DOI] [PubMed] [Google Scholar]
- 49. Myelnikov D. Creature features: The lively narratives of bacteriophages in Soviet biology and medicine. Notes Rec R Soc J Hist Sci. 2020;74(4):579–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dugatkin LA, Trut L, Trut LN. How to Tame a Fox (and Build a Dog): Visionary Scientists and a Siberian Tale of Jump-Started Evolution. University of Chicago Press, 2017. [Google Scholar]
- 51. Salmond GPC, Fineran PC. A century of the phage: Past, present and future. Nat Rev Microbiol. 2015;13(12):777–786. [DOI] [PubMed] [Google Scholar]
- 52. Jacob F, Monod J. Genetic regulatory mechanisms in the synthesis of proteins. J Mol Biol. 1961;3(3):318–356. [DOI] [PubMed] [Google Scholar]
- 53. McCafferty J, Griffiths AD, Winter G, et al. Phage antibodies: Filamentous phage displaying antibody variable domains. Nature. 1990;348(6301):552–554. [DOI] [PubMed] [Google Scholar]
- 54. Segal E. Invisible Venomous Creatures Destroy the Bacteria. Herut, 1950.
- 55. Segal E. Healing by Infection (Bacteriophages and Their Actions). Herut, 1950.
- 56. Olitzki AL. Healing by Bacteriophages. Davar, 1958.
- 57. Gelman D, Yerushalmy O, Ben-Porat S, et al. Clinical phage microbiology: A suggested framework and recommendations for the in-vitro matching steps of phage therapy. Lancet Microbe. 2021;2(10):e555–e563. [DOI] [PubMed] [Google Scholar]
- 58. Ben-Gurion R. Photoreactivation and cysteine reversion of lysogenic induction. J Mol Biol. 1964;9(3):619–623. [DOI] [PubMed] [Google Scholar]
- 59. Ben-Gurion R. The production of phage in induced lysogenic and in infected sensitive bacteria. Virology. 1963;20(2):288–291. [DOI] [PubMed] [Google Scholar]
- 60. Shemer M. Genetical Mistakes Might Be Beneficial. Davar, the daily news paper of the workers of the Land of Israel, 1969. [Google Scholar]
- 61. Bora A. Hebrew University Scientists in Jerusalem Discovered: Substances That Inhibit the Culture of Bacteria and Viruses. LaMerhav, a Hebrew language daily newspaper published by the Ahdut HaAvoda party, 1969. [Google Scholar]
- 62. Hareuveni M. The Study of the Discovery of the Secret of Life (About Dr. Lurie who won the Nobel Prize); Lamerhav, 1969. [Google Scholar]
- 63. Shomron B. Centropoga (On Centrifuge and Phage Insulation). The Cattle, 1963.
- 64. Genetic Therapy Breakthrough. Davar, the daily newspaper of the workers of the Land of Israel, 1971. [Google Scholar]
- 65. Altuvia S, Locker-Giladi H, Koby S, et al. RNase III stimulates the translation of the cIII gene of bacteriophage lambda. Proc Natl Acad Sci USA. 1987;84(18):6511–6515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Oppenheim AB, Kobiler O, Stavans J, et al. Switches in bacteriophage lambda development. Annu Rev Genet. 2005;39:409–429. [DOI] [PubMed] [Google Scholar]
- 67. Rokney A, Kobiler O, Amir A, et al. Host responses influence on the induction of lambda prophage. Mol Microbiol. 2008;68(1):29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Adhya SL, Court DL, Friedman DI, et al. Amos Oppenheim (31 October 1934 to 24 September 2006). Mol Microbiol. 2008;67(4):685–686. [DOI] [PubMed] [Google Scholar]
- 69. Kuhn J, Suissa M, Wyse J, et al. Detection of bacteria using foreign DNA: The development of a bacteriophage reagent for Salmonella. Int J Food Microbiol. 2002;74(3):229–238. [DOI] [PubMed] [Google Scholar]
- 70. Rossolini GM, Arena F, Pecile P, et al. Update on the antibiotic resistance crisis. Curr Opin Pharmacol. 2014;18:56–60. [DOI] [PubMed] [Google Scholar]
- 71. Murray CJL, Ikuta KS, Sharara F, et al. , Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399:629–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Rosini R, Nicchi S, Pizza M, et al. Vaccines against antimicrobial resistance. Front Immunol. 2020;11:1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Djebara S, Maussen C, De Vos D, et al. Processing phage therapy requests in a Brussels military hospital: Lessons identified. Viruses. 2019;11(3):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lin RCY, Sacher JC, Ceyssens P-J, et al. Phage biobank: Present challenges and future perspectives. Curr Opin Biotechnol. 2021;68:221–230. [DOI] [PubMed] [Google Scholar]
- 75. Aslam S, Lampley E, Wooten D, et al. Lessons learned from the first 10 consecutive cases of intravenous bacteriophage therapy to treat multidrug-resistant bacterial infections at a single center in the United States. In: Baddley JW, Spec A, eds. Open Forum Infectious Diseases, vol. 7. Oxford University Press US, 2020:ofaa389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ferry T, Kolenda C, Briot T, et al. Implementation of a complex bone and joint infection phage therapy centre in France: Lessons to be learned after 4 years' experience. Clin Microbiol Infect. 2022;28(1):145–146. [DOI] [PubMed] [Google Scholar]
- 77. Jault P, Leclerc T, Jennes S, et al. efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): A randomised, controlled, double-blind phase 1/2 trial. Lancet Infect Dis. 2019;19(1):35–45. [DOI] [PubMed] [Google Scholar]
- 78. Sarker SA, Sultana S, Reuteler G, et al. Oral phage therapy of acute bacterial diarrhea with two coliphage preparations: A randomized trial in children from Bangladesh. EBioMedicine. 2016;4:124–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Wright A, Hawkins CH, Änggård EE, et al. A controlled clinical trial of a therapeutic bacteriophage preparation in chronic otitis due to antibiotic-resistant Pseudomonas aeruginosa; a preliminary report of efficacy. Clin. Otolaryngol. 2009;34(4):349–357. [DOI] [PubMed] [Google Scholar]
- 80. Furfaro LL, Payne MS, Chang BJ. Bacteriophage therapy: Clinical trials and regulatory hurdles. Front Cell Infect Microbiol. 2018;8:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Schooley RT, Biswas B, Gill JJ, et al. Development and use of personalized bacteriophage-based therapeutic cocktails to treat a patient with a disseminated resistant Acinetobacter baumannii infection. Antimicrob Agents Chemother. 2017;61(10):e00954-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Graif N, Abozaid S, Peretz A. Trends in distribution and antibiotic resistance of bacteria isolated from urine cultures of children in Northern Israel between 2010 and 2017. Microb Drug Resist. 2020;26(11):1342–1349. [DOI] [PubMed] [Google Scholar]
- 83. Shapira JC. State Comptroller's Report. 2013. https://www.mevaker.gov.il/he/Reports/Report_114/8ce78a84-8fc5-4a3e-8ade-f8bbf4c78fdf/7956.pdf.
- 84. Cohen Y, Joseph Pollock F, Rosenberg E, et al. Phage therapy treatment of the coral pathogen Vibrio coralliilyticus. Microbiologyopen. 2013;2(1):64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Atad I, Zvuloni A, Loya Y, et al. Phage therapy of the white plague-like disease of Favia favus in the Red Sea. Coral Reefs. 2012;31(3):665–670. [Google Scholar]
- 86. Moses S, Aftalion M, Mamroud E, et al. Reporter-phage-based detection and antibiotic susceptibility testing of Yersinia pestis for a rapid plague outbreak response. Microorganisms. 2021;9(6):1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Moses S, Vagima Y, Tidhar A, et al. Characterization of Yersinia pestis phage lytic activity in human whole blood for the selection of efficient therapeutic phages. Viruses. 2021;13(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Vagima Y, Gur D, Aftalion M, et al. Phage therapy potentiates second-line antibiotic treatment against pneumonic plague. Viruses. 2022;14(4):688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Khatami A, Lin RCY, Petrovic-Fabijan A, et al. Bacterial lysis, autophagy and innate immune responses during adjunctive phage therapy in a child. EMBO Mol Med. 2021;13(9):e13936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Alkalay-Oren S, Yerushalmy O, Adler K, et al. Complete genome sequence of Pseudomonas aeruginosa bacteriophage PASA16, used in multiple phage therapy treatments globally. Microbiol Resour Announc. 2022;11(4):e00092-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Yerushalmy O, Khalifa L, Gold N, et al. The Israeli phage bank (IPB). Antibiotics. 2020;9(5):269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Paul K, Merabishvili M, Hazan R, et al. Bacteriophage rescue therapy of a vancomycin-resistant Enterococcus faecium infection in a one-year-old child following a third liver transplantation. Viruses. 2021;13(9):1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Yerushalmy O, Coppenhagen-Glazer S, Nir-Paz R, et al. Complete genome sequences of two Klebsiella pneumoniae phages isolated as part of an international effort. Microbiol. Resour. Announc. 2019;8(38):e00843-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Smith M. Salt in My Soul: An Unfinished Life. Random House: New York, NY; 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.