Corresponding Author
Key Words: COVID-19, coronavirus cardiovascular imaging, diagnostic cardiovascular procedure, cardiovascular disease, cardiac testing
Over the last 15 months, every health care delivery system in the world has been affected by the coronavirus disease-2019 (COVID-19) pandemic. Early on, it was clear that high infection rates, hospitalizations, and resources used by both patients and providers were going to dictate how individual health care systems would be able to manage the pandemic (1). Now, with rates of COVID-19 infections declining across most of the world, many systems have transitioned to the next phase of the pandemic and have encouraged a safe increase in cardiovascular services offered to patients. Because we are at this vital transition point, it is important to reflect on the changing practices during the pandemic, not only to learn more about the strategies of crisis management but also to anticipate the impact that these changes may have on the future of patient care.
With the implementation of stay-at-home orders, transition to remote work stations, relocations of hospital staff, and delays in nonurgent procedures, it became obvious that there was going to be a reduction in the rates of cardiovascular and, indeed, almost all non-COVID-related services being offered to patients across the world; but the impact of those changes remains largely unknown (1,2). In this issue of iJACC, Hirshfeld et al. (3) present the results of the INCAPS COVID (International Atomic Energy Agency Non-Invasive Cardiology Protocols Study of COVID-19), a survey of 909 medical facilities in 108 countries. This important study assessed objectively how cardiovascular procedure rates changed during the peak months of the pandemic. By issuing electronic surveys organized by the International Atomic Energy Agency, total numbers and types of non-invasive and invasive cardiovascular procedures were reported according to each institution. The authors were then able to compare procedural types and volumes across a representative number of centers throughout the world from a pre-pandemic time period (March 2019) to time periods in the middle of the pandemic (March 2020 and April 2020). There are numerous interesting findings in this large study, and the results are at once encouraging and reasons for concern.
Encouraging Evidence of Medical Leadership
Early in the pandemic course, there were several expert consensus documents published by the cardiac imaging and procedural societies to help guide facilities through the changing demands for health care services (4, 5, 6). These documents, in near perfect harmony, advocated for the creation of tier and triaging systems to help expedite services that may have significant influences on individual outcomes while delaying lower yield procedures. With secondary aims of offering maximum protection against exposure to COVID-19 to both patients and providers, additional themes of society recommendations included screening patients for symptoms prior to procedures, advocating for greater time for sanitary efforts, and providing appropriate personal protective equipment. As conditions continued to rapidly change throughout the course of the pandemic, however, it was hard to predict how effective those expert consensus documents would be in real time.
The results presented in INCAPS COVID suggest that the expert consensus recommendations were indeed well received by physicians and hospitals throughout various practice settings in the world and likely influenced institutional practices. For example, with recommendations to postpone less urgent cardiovascular procedures, INCAPS COVID showed that there was indeed an appropriate decrease in the number of cardiovascular procedures being completed in the peak month of the pandemic, both in the United States (68% total procedural reduction) and globally (63% reduction). These reductions were highest in regions most affected by the pandemic, greater in outpatient than inpatient facilities, greater for more elective procedures, and seemingly were not affected by regional politics. As a specific example of postponing less urgent procedures, in the United States, there was an overall 94% reduction in the number of computed tomography (CT) coronary calcium scoring procedures in April 2020, likely the most elective of all the procedures studied. Importantly, the overall procedural reductions were found to be similar regardless of the type of facility (teaching status or those affected by staffing issues).
Not only was there a significant reduction in the number of cardiovascular procedures being completed at the peak of the pandemic, but INCAPS COVID provides objective data to suggest that the recommendations for avoiding aerosolizing procedures were being followed. For example, procedures such as stress electrocardiography and stress echocardiography, which are usually completed with an exercise component, saw an 81% and 85% reduction in the United States, respectively. Meanwhile, providers seemed to be appropriately choosing more single-photon emission computed tomography (SPECT) and positron emission tomography (PET) stress tests, which can be performed with pharmacologic stress, which only saw a 75% and 58% reduction, respectively, in the United States. Furthermore, because transesophageal echocardiograms are arguably one of the highest risk procedures for aerosolizing COVID-19 transmission, those procedures had some of the highest case reductions (80% in the United States and 73% in non-US facilities), whereas procedures posing lower risks of aerosolization, such as computed tomography angiography (CTA) and transthoracic echocardiography, had lower reductions. Importantly, each of those practice changes were encouraged and supported by several cardiac imaging leaders. Statistically similar procedural reductions occurred between U.S. and non-U.S. facilities, strongly suggesting that advice provided from expert consensus documents was heeded or that medical decision makers came to very similar common-sense conclusions about wise practices, or both.
Changing Practices
Disruptive forces often spurn and accelerate innovation. In several clear ways, the challenges presented by the COVID-19 pandemic have forced innovative changes in cardiovascular procedures that will likely affect society guidelines moving forward. In nuclear cardiology laboratories, “stress first/stress only” strategies have been advocated for several years as a method of reducing radiation doses (7). With the desire to increase social distancing and to limit time and exposures for both patients and staff members in medical facilities, that strategy has been embraced with new vigor. Also, 2-day nuclear stress test protocols have usually been used to allow higher doses of radioisotope in obese patients or to accommodate physician availability. However, the protocol’s benefit of social distancing outweighs the potential scheduling inconvenience to patients during a pandemic and has likewise been embraced. At Saint Luke’s Mid America Heart Institute, staff have followed suggestions for alternative testing during the pandemic by, for example, frequently substituting CT for transesophageal echocardiography for planning of left atrial appendage occlusion procedures and to clear the left atrial appendage prior to cardioversion (1). If those modified strategies prove to be more efficient and safer for patient care, the innovative efforts brought on by the pandemic may prove beneficial in advancing modern practices (8).
The practice pattern change documented by INCAPS COVID were not only appropriate, they should also be viewed as a clear victory for the scientific community, with an active platform, physicians have the ability to lead hospitals and communities when faced with the challenges related to this pandemic. Moving forward, we have the responsibility to remain active leaders as it will prove to be instrumental with the re-opening efforts as the pandemic continues to progress. These efforts can be seen by multiple societies already issuing re-opening guideline documents (9, 10, 11).
Reason for Concern: Impact on Cardiovascular Care
Although we now have objective evidence for how volumes of cardiovascular procedures have changed during the early phase of the COVID-19 pandemic, there are significant concerns about how those procedural reductions may impact overall cardiovascular outcomes (2). The fear is that we have traded efforts to contain the pandemic for losses in prevention of cardiovascular disease, which is especially concerning given the overall global burden of cardiovascular disease (1). Indeed, the next step in studying the effects of the pandemic will involve research designed to evaluate the consequences of delayed cardiac procedures. From INCAPS COVID, it is not known if after the early pandemic lockdowns large numbers of patients had long delays or never received diagnostic tests, cardiovascular treatments, and preventive therapies, or whether those procedures returned to the previous baseline numbers relatively quickly. If the former is the case, we anticipate seeing a large wave of cardiovascular illness in the coming months and years.
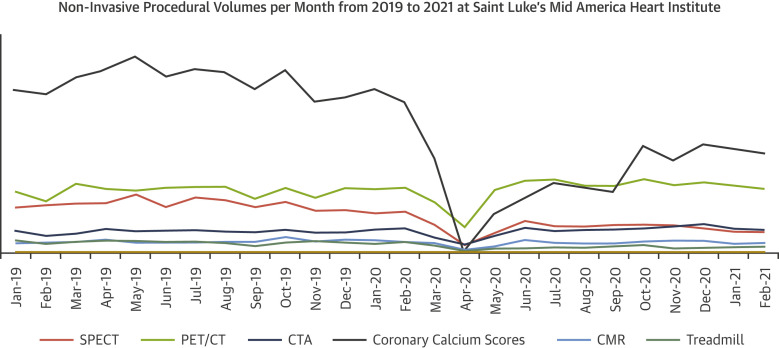
Experience from the present authors’ center shows that, by following society recommendations and guidance to return to practice, there was a dramatic decrease in the number of all non-invasive procedural studies at the peak of the pandemic, similar to that described in INCAPS COVID (Figure 1 ). However, those reductions in procedure volumes at the authors’ center were mostly short lived, with numbers achieving and, in some cases, exceeding pre-pandemic case volumes in just a couple of months. In fact, the authors’ laboratory subsequently experienced an increase in the number of cases per month that underwent PET myocardial perfusion imaging (MPI) compared to baseline, shifting many cases from SPECT MPI as a more accurate test when exercise was being avoided and taking advantage of a more rapid protocol to facilitate social distancing, in compliance with society recommendations (1,9). Also, as coronary calcium scoring is believed to be the most elective cardiovascular procedure, we have accordingly yet to return to pre-pandemic volumes of this test.
Figure 1.
Saint Luke’s Mid America Heart Institute’s experience With Non-Invasive Procedural Volume Over the Course of the Pandemic
CMR = cardiac magnetic resonance; CTA = computed tomography angiogram; PET/CT = positron emission tomography/computed tomography; SPECT = single-photon emission computed tomography.
Although the present data represent only 1 center’s experience, we eagerly await the INCAPS COVID follow-up study planned by the authors. If such trends are consistent across multiple sites, we may see that a recovery back to normal procedural volumes over the course of a few months may mitigate substantial adverse outcomes. Additionally, if the widely implemented triage system worked, patients who truly needed procedures should have found their way to access.
The COVID-19 pandemic continues to be the single greatest challenge faced by global health care systems in the modern medical era. When guidance was needed, cardiovascular society leaders came together to present clear and consistent management recommendations which were widely adopted by physicians and hospitals around the world. Although we are just beginning to understand the impact of the procedural reductions that came as a result of these recommendations, cardiovascular outcomes remain an unknown value during pandemic management. Nevertheless, ongoing studies of cardiovascular outcomes will offer an important parallel perspective to the effects of procedural volume changes and together may tell a more complete story of the cardiovascular health care delivery impacts of COVID-19.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Einstein A.J., Shaw L.J., Hirschfeld C., et al. International impact of COVID-19 on the diagnosis of heart disease. J Am Coll Cardiol. 2021;77:173–185. doi: 10.1016/j.jacc.2020.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rangé G., Hakim R., Motreff P. Where have the ST-segment elevation myocardial infarctions gone during COVID-19 lockdown? Eur Heart J Qual Care Clin Outcomes. 2020;6:223–224. doi: 10.1093/ehjqcco/qcaa034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirschfeld C.B., Shaw L.J., Williams M.C., Lahey R., Villines T.C., Dorbala S., et al. Impact of COVID-19 on cardiovascular testing in the United States versus rest of the world: the INCAPS COVID study. J Am Coll Cardiol Img. 2021;14:1787–1801. doi: 10.1016/j.jcmg.2021.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skali H., Murthy V.L., Al-Mallah M.H., et al. Guidance and best practices for nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: an information statement from ASNC and SNMMI. J Nucl Cardiol. 2020;27:1022–1029. doi: 10.1007/s12350-020-02123-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi A.D., Abbara S., Branch K.R., et al. Society of Cardiovascular Computed Tomography guidance for use of cardiac computed tomography amidst the COVID-19 pandemic endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr. 2020;14:101–104. doi: 10.1016/j.jcct.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak: endorsed by the American College of Cardiology. J Am Coll Cardiol. 2020;75:3078–3084. doi: 10.1016/j.jacc.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorbala S., Anathasubramaniam K., Armstrong I.S., et al. Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol. 2018:1784–1846. doi: 10.1007/s12350-018-1283-y. [DOI] [PubMed] [Google Scholar]
- 8.Skali H. The COVID-19 pandemic and nuclear cardiology: an opportunity to grow stronger? J Nucl Cardiol. 2021;28:336–337. doi: 10.1007/s12350-020-02383-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zoghbi W.A., DiCarli M.F., Blankstein R., et al. Multimodality cardiovascular imaging in the midst of the COVID-19 pandemic: ramping up safely to a new normal. J Am Coll Cardiol Img. 2020;13:1615–1626. doi: 10.1016/j.jcmg.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skali H., Murthy V.L., Paez D., et al. Guidance and best practices for reestablishment of non-emergent care in nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: an information statement from ASNC, IAEA, and SNMMI. J Nucl Med. 2020;61:1534–1539. doi: 10.2967/jnumed.120.251355. [DOI] [PubMed] [Google Scholar]
- 11.Paschali A., Anagnostopoulos C. Nuclear cardiology practice in COVID-19 era. Hell J Nucl Med. 2020;23(Suppl):26–30. [PubMed] [Google Scholar]