Abstract
Background
Percutaneous screw fixation of the posterior pelvic ring is technically demanding and can result in cortical breach. The purpose of this study was to examine risk factors for screw breach and iatrogenic nerve injury.
Methods
A retrospective review at a single level-one trauma center identified 245 patients treated with 249 screws for pelvic ring injuries with postoperative computed tomography (CT) scans. Cortical screw breach, iatrogenic nerve injury, and associated risk factors were evaluated.
Results
There were 86 (35%) breached screws. The breach rate was similar between screw types (33% S1-iliosacral (S1-IS), 44% S1-transsacral (S1-TS), 31% S2-IS, and 30% S2-TS) and was not associated with patient characteristics, Tile C injuries, or corridor size or angle. The overall rate of screw revision for screw malpositioning was 1.2% (3/249). Iatrogenic nerve injuries occurred in 8 (3.2%) of the 249 screws. Screws that caused iatrogenic nerve injuries had greater screw breach distances (5.4 vs. 0 mm, MD 5, CI 2.3 to 8.7, p < 0.0001), were more likely to be S1-IS screws (88% vs. 47%, PD 40%, CI 7 to 58%, p = 0.006), more likely to be placed in Tile C injuries (75% vs. 44%, PD 31%, CI -3 to 55%, p = 0.04), and there was a trend for having a screw corridor size <10 mm (75% vs. 47%, PD 28, CI -6 to 52%, p = 0.06). Of the 7 iatrogenic nerve injuries adjacent to screw breaches, two nerve injuries recovered after screw removal, three recovered with screw retention, and two did not recover with screw retention.
Conclusion
Screw breaches were common and iatrogenic nerve injuries were more likely with S1-IS screws. Surgeons should maintain a high degree of caution when placing these screws and consider removal of any breached screw associated with nerve injury.
Keywords: Pelvic ring injury, Posterior percutaneous screw fixation, Breach, Iatrogenic nerve injury, Sacroiliac, Transsacral
1. Introduction
Percutaneous posterior pelvic ring fixation is technically difficult, with a reported angular tolerance of only one to four degrees.1,2 Several studies have documented the rate of iatrogenic nerve injury, misplaced screws and the revision rate of screws.1,3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 Despite the relatively high rate of screw breach in the published literature (range, 0–59%), the rate of reported iatrogenic neurologic injury (range, 0–3.2%) and screw revision (range, 0–9.9%) remains low.1,3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14
The published literature on screw breaches in percutaneous posterior pelvic ring fixation has several limitations. Most studies report a qualitative account of screw misplacement and do not draw any contrast between screws that have just barely breached the cortex versus screws that are completely out of the intended osseous pathway.1,3, 4, 5, 6, 7,10,14 Additionally, several of the most commonly cited studies report on a single surgeon's experience only, limiting their generalizability.3,7,10,14 Furthermore, many of the published studies focus solely on iliosacral (IS) screws and there is little literature on transsacral (TS) screws, which have a different trajectory and length, giving them a potentially different risk profile.1,3, 4, 5, 6, 7, 8, 9,11,12 Finally, risk factors of screw breach and iatrogenic nerve injury have not been thoroughly evaluated.4,8,11,12
The purpose of this study was to identify risk factors for screw breach and subsequent iatrogenic nerve injury in large number of patients treated with percutaneous screw fixation of the posterior pelvic ring by multiple orthopaedic trauma surgeons over a span of multiple years.
2. Methods
Following institutional review board approval (#19–2483), a retrospective review was completed at a single urban level one trauma center. Patients with pelvic ring injuries undergoing operative fixation were identified. Inclusion criteria included age ≥18. Exclusion criteria included missing or inadequate postoperative computed tomography (CT) scans.
All surgeries were completed by fellowship-trained orthopaedic trauma surgeons (n = 6) utilizing a radiolucent operating room table, fluoroscopy, and 6.5/7.3 mm cannulated screws per surgeon discretion through standard percutaneous techniques.3 Preoperative and postoperative CT scans were reviewed by three orthopaedic surgeons. The S1 and S2 TS corridor width was measured on preoperative CT axial reformatted images (parallel with the S1 body) and coronal reformatted images (perpendicular to the S1 body) as the distance between two parallel lines marking the maximum TS corridor possible (Fig. 1). If a corridor less than 10 mm was identified, the IS corridor was measured instead in the same manner. If either the axial or coronal TS corridor width of S1 or S2 was less than 10 mm then the TS corridor was considered to be narrow.15
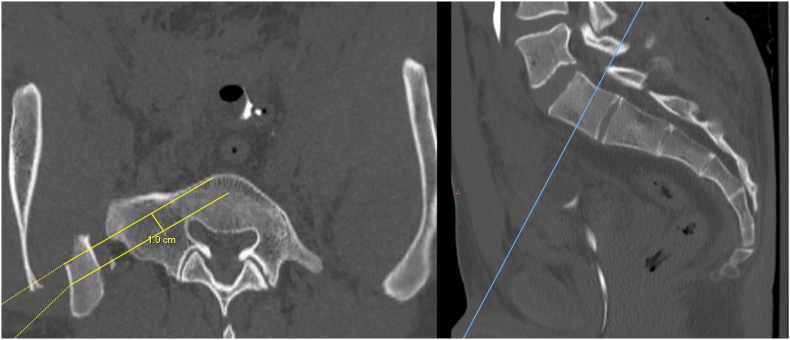
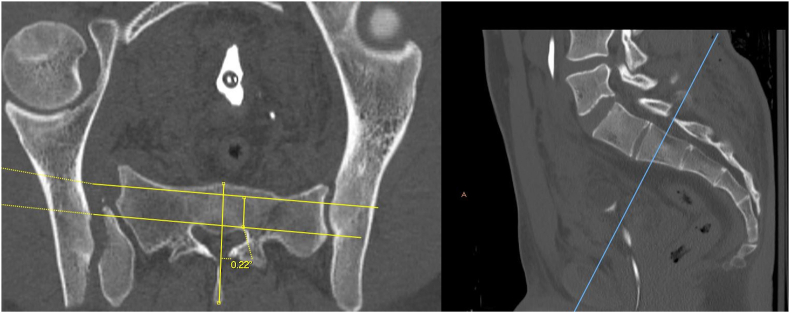
Fig. 1.
(a) Axial reformatted computed tomography (CT) scan showing the measurement of an oblique S1 sacral corridor, (b) axial reformatted CT scan showing the measurement of a transsacral S2 corridor, and (c) coronal reformatted CT scan showing the measurement of both the oblique S1 and transsacral S2 corridors.
The cobb angle tool was used to measure the angle between a line bisecting the sacrum and a line perpendicular to the measured corridor of S1 and S2 on the axial and coronal reformatted images as described by Kaiser et al.15 (Fig. 2). The true S1 alar angle was calculated by inputting the axial and coronal angles into the Pythagorean theorem as originally described by Dror Paley for calculating true angular deformity of malunions.16
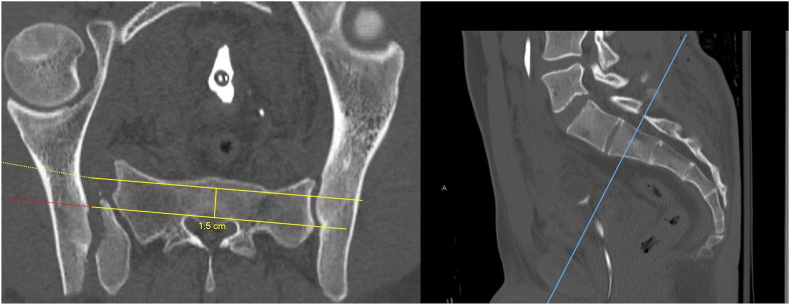
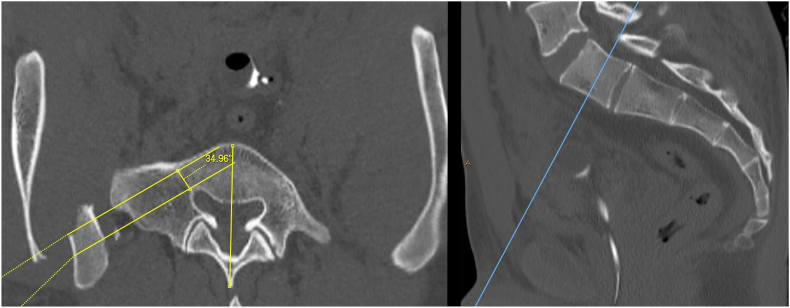
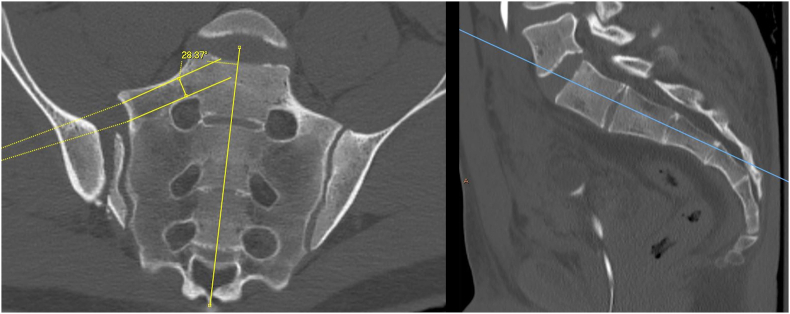
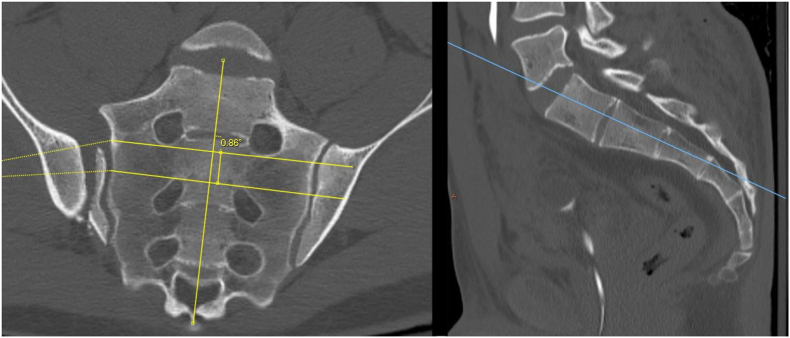
Fig. 2.
(a) Axial reformatted computed tomography (CT) scan showing the angle between the oblique S1 corridor and the sagittal plane, (b) axial reformatted CT scan showing the angle between the transsacral S2 corridor and the sagittal plane, (c) coronal reformatted CT scan showing the angle between the oblique S1 corridor and the sagittal plane, and (d) coronal reformatted CT scan showing the angle between the transsacral S2 corridor and the sagittal plane.
The screw breach distance was measured on sagittal CT images reformatted to be perpendicular to the screw axis (Fig. 3). The maximum distance of screw breach, perpendicular to the breached cortex, was measured. In the event of metal artifact obscuring the border of the screw at the area of measurement, the screw border was extrapolated by matching a circle with the same radius of curvature as a visible part of the screw border elsewhere around the diameter. If the screw was breached in multiple areas, the largest breach was recorded. The direction of screw breach, corridor (S1 vs. S2), screw size, and screw type (IS vs. TS) were recorded.
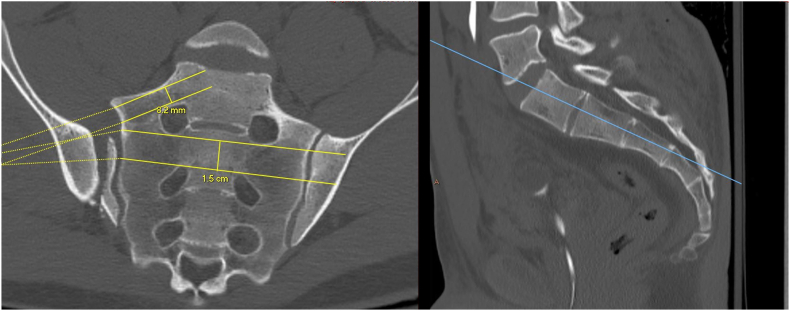
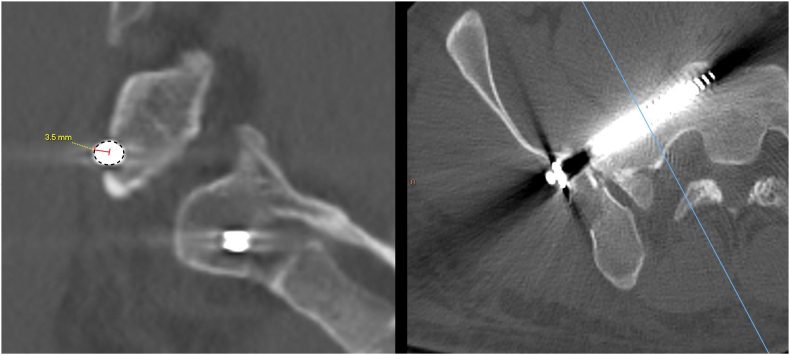
Fig. 3.
Sagittal reformatted CT scan perpendicular to the screw trajectory with an outline around the periphery of the screw and a measurement from the cortex to the most breached aspect of the screw to assess breach distance.
A chart review was completed to record the rate of neurologic complication, neurologic recovery and revision surgery. Demographic details were also collected including age, gender and body mass index (BMI).
Statistical analysis was done in accordance to the guidelines of Strage et al.17 All continuous variables were determined to be nonparametric based on the Shapiro-wilk test and are therefore presented as a median value with interquartile range (IQR). The Wilcoxon test was used to compare nonparametric continuous variables between groups. The median difference (MD) along with 95% confidence interval (CI) was calculated using the Hodges-Lehmann estimator.18 Fisher exact test and Chi-square test were used to compare nominal variables between groups. Adjusted Wald test was used to calculate 95% CI of the proportional difference (PD).19 A p-value less than 0.05 was considered statistically significant. JMP Pro 14 (SAS, Cary, NC) was used for all statistical analysis.
3. Results
249 screws in 245 patients were included in the analysis. There were 121 S1-IS screws, 55 SI-TS screws, 16 S2-IS screws and 57 S2-TS screws. All screw type groups were similar with regard to age, gender, BMI, and rate of Tile C injury (Table 1). Due to the small number of S2-IS screws, all of the S2 screws were combined to analyze variables associated with screw breach (n = 73).
Table 1.
Comparison of screws by type.
| N = 249 screws | S1-IS (n = 121) | S1-TS (n = 55) | S2-IS (n = 16) | S2-TS (n = 57) | P-value |
|---|---|---|---|---|---|
| Age | 41 (27–54) | 44 (26–58) | 33 (22–41) | 35 (25–49) | 0.1 |
| Female gender | 41 (34%) | 18 (33%) | 8 (50%) | 18 (32%) | 0.5 |
| BMI | 26 (22–29) | 25 (22–28) | 26 (22–29) | 26 (22–29) | 0.9 |
| Tile C injury | 57 (47%) | 26 (47%) | 6 (37%) | 24 (42%) | 0.9 |
| Screw breach | 40 (33%) | 24 (44%) | 5 (31%) | 17 (30%) | 0.4 |
| Screw breach distance (mm) | 2.6 (1.6–6.8) | 2.9 (1.3–4.7) | 2.4 (1.6–3.8) | 2.1 (1.5–2.9) | 0.4 |
| Nerve injury | 7 (5.8%) | 0 (0%) | 1 (6%) | 0 (0%) | 0.07 |
Continuous variables are presented as median (interquartile interval).
(IS – Iliosacral, TS – transsacral).
Screw breaches occurred in 86 (35%) of the 249 screws. There was no observed difference in the rate of screw breach based on screw type: 33% S1-IS, 44% S1-TS, 31% S2-IS and 30% S2-TS (Table 1). The severity of screw breach, in terms of distance, did not differ between screw types.
When analyzing S1-IS, S1-TS, and S2 screw breaches separately, there were no associations with age, gender, BMI, Tile C injury, axial or coronal corridor width, or sacral alar angulation (Table 2, Table 3, Table 4). Two screws in a single corridor were associated with S2 breaches (18% vs. 0%) but not S1-IS or S1-TS breaches.
Table 2.
Associations with S1 iliosacral screw breach.
| n = 121 screws | Breach (n = 40) | No breach, (n = 79) | Difference, 95% Confidence Interval | P-value |
|---|---|---|---|---|
| Age | 41 (28–53) | 42 (27–54) | −1, −7 to 5 | 0.7 |
| Female gender | 14 (33%) | 28 (35%) | −2%, −19 to 16% | 0.8 |
| BMI | 26 (22–29) | 26 (22–29) | −0.2, −2 to 2 | 0.8 |
| Tile C injury | 24 (57%) | 33 (42%) | 15%, −3 to 33% | 0.1 |
| S1-IS axial corridor width (mm) | 15 (14–17) | 16 (14–18) | −1, −2 to 1 | 0.3 |
| S1-IS coronal corridor width (mm) | 14 (13–15) | 14 (13–15) | 0, −1 to 1 | 0.5 |
| Axial or coronal S1-TS corridor < 10 mm | 24 (60%) | 41 (51%) | 9%, −8 to 24% | 0.1 |
| True S1 alar angle (degree) | 29 (1–44) | 28 (0–36) | 1, −0.6 to 5 | 0.1 |
| 2 screws in same corridor | 17 (43%) | 23 (28%) | 14%, −3 to 32% | 0.1 |
Continuous variables are presented as median (interquartile interval).
(IS – Iliosacral, TS – transsacral).
Table 3.
Associations with S1 transsacral screw breach.
| n = 55 screws | Breach (n = 24) | No breach, (n = 31) | Difference, 95% Confidence Interval | P-value |
|---|---|---|---|---|
| Age | 47 (31–61) | 36 (24–58) | 6, −3 to 19 | 0.1 |
| Female gender | 10 (42%) | 8 (26%) | 16%, −9 to 39% | 0.2 |
| BMI | 24 (22–28) | 25 (23–27) | −0.6, −3 to 2 | 0.7 |
| Tile C injury | 12 (50%) | 14 (45%) | 5%, −21 to 30% | 0.7 |
| S1-TS axial corridor width (mm) | 15 (12–18) | 16 (14–18) | −1, −3 to 1 | 0.2 |
| S1-TS coronal corridor width (mm) | 15 (13–16) | 14 (13–17) | 0, −2 to 2 | 0.9 |
| Axial or coronal S1-TS corridor < 10 mm | 3 (13%) | 3 (10%) | 3%, −14 to 21% | 0.3 |
| 2 screws in same corridor | 8 (33%) | 4 (13%) | 20%, −3 to 41% | 0.1 |
Continuous variables are presented as median (interquartile interval).
(TS – transsacral).
Table 4.
Associations with S2 screw breach.
| n = 73 screws | Breach (n = 22) | No breach (n = 51) | Difference, 95% Confidence Interval | P-value |
|---|---|---|---|---|
| Age | 31 (23–51) | 35 (25–47) | −3, −10 to 5 | 0.4 |
| Female gender | 7 (32%) | 19 (37%) | −5%, −27 to 19% | 0.7 |
| BMI | 26 (21–29) | 27, 22 to 29 | −0.6 | 0.6 |
| Tile C injury | 9 (41%) | 21 (41%) | −0.2%, −24 to 24% | 1.0 |
| S2-TS axial corridor width (mm) | 12 (10 t o14) | 11 (10–13) | 0, −1 to 1 | 0.8 |
| S2-TS coronal corridor width (mm) | 11 (10–13) | 12 (10–13) | −1, −2 to 0 | 0.1 |
| Axial or coronal S2-TS corridor < 10 mm | 6 (27%) | 8 (16%) | 11%, −9 to 33% | 0.3 |
| 2 screws in same corridor | 4 (18%) | 0 (0%) | 18%, 2–35% | 0.007 |
Continuous variables are presented as median (interquartile interval).
(TS – transsacral).
Iatrogenic nerve injuries occurred after placement of 8 (3.2%) of the 249 screws. Screws associated with iatrogenic nerve injuries had greater screw breach distances (5.4 vs. 0 mm, MD 5, CI 2.3 to 8.7, p < 0.0001), were more likely to be S1-IS screws (88% vs. 47%, PD 40%, CI 7 to 58%, p = 0.006), more likely to be placed in Tile C injuries (75% vs. 44%, PD 31%, CI -3 to 55%, p = 0.04), and there was a trend for having a screw corridor size <10 mm (75% vs. 47%, PD 28, CI -6 to 52%, p = 0.06). Patients with iatrogenic nerve injuries did not differ in age (42 vs. 39 years, MD 1, CI -12 to 14, p = 0.7), female gender (38% vs. 34%, PD 3%, CI -25 to 36%, p = 0.3), or BMI (25 vs. 26, MD -1.3, CI −5.7 to 2.2, p = 0.4).
There were 7 iatrogenic nerve injuries adjacent to screw breaches (Table 5). Two nerve injuries recovered after screw removal, three recovered with screw retention, and two did not recover with screw retention.
Table 5.
Details of iatrogenic nerve injuries.
| Screw | Breach distance (mm) | Breach adjacent to nerve? | Nerve | Type | Screw revision? | Nerve Recovery? | Time to nerve recovery (months) | |
|---|---|---|---|---|---|---|---|---|
| #1 | S1-IS | 12 | No | L5 | Motor/Sensory | No | Motor recovery at last follow-up but sensory persisted | 6 |
| #2 | S1-IS | 10 | Yes | L5 | Sensory | No | Yes | 4 |
| #3 | S1-IS | 0 | No (unused guide-wire hole seen adjacent to nerve on CT) | L5 | Motor/Sensory | No | No improvement at 2-month follow-up. Lost to follow-up | |
| #4 | S1-IS | 6 | Yes | S1 | Motor/Sensory | No | No improvement at 19-month follow-up | |
| #5 | S2-IS | 5 | Yes | S1 | Motor/Sensory | Yes, 2 months after primary surgery | Yes, after screw removal | 2.5 months after primary fixation |
| #6 | S1-IS | 2.3 | Yes | S1 | Sensory | No | Yes | 24 |
| #7 | S1-IS | 3.5 | Yes | L5 | Sensory | No | Yes | 2 |
| #8 | S1-IS | 11 | Yes | S1 | Motor/Sensory | Yes | Yes, after screw removal | 2 weeks after primary fixation |
(IS – Iliosacral).
The was one nerve injury that was not associated with a breached screw. In this case a breached wire tract was seen directed at the nerve on the postoperative CT scan with no other explanation for the nerve injury. This nerve injury did not recover.
The overall rate of screw revision for screw malpositioning was 1.2% (3/249). Two of these revisions were for breached screws with iatrogenic nerve injuries as described above and one revision was for penetration of the screw head through the outer ilium and into the SI joint.
4. Discussion
This study found that 35% of screws used for posterior pelvic ring fixation were breach with a 3.2% rate of iatrogenic nerve injuries. Screw type, age, sex, BMI, and corridor size were not associated with screw breaches. S1-IS screw placement was responsible for 7 of the 8 nerve injuries despite making up only 48% (121/249) of the screws evaluated in this study.
This study found similar findings as the three largest studies on posterior pelvic ring screw breaches which analyzed a combined total of 462 screws. Screw breach rates reported in each of these studies were 16%, 38%, and 59%, resulting in a combined rate of 35% (160/462), which is interestingly the same percentage reported in the current study.8,9,11 This rate of screw breaches is notably higher than the rate of screw breaches reported by several single surgeon series which have reported rates from 0% to 2.7%, emphasizing the limited generalizability of single surgeon studies.3,7,10
In the current study, the rate of screw breaches and the breach distance did not differ between the different screw types. These findings have not been previously reported as nearly all of the current published literature focuses on IS screws only (Table 6). The rate of screw breach was similar between IS and TS screws, despite the lower angular tolerances of TS screws.1,2
Table 6.
Literature review of percutaneous posterior pelvic ring screw breaches placed with standard fluoroscopic techniques.
| Study | Total Patients | Surgeons | Number of screws examined on postoperative CT | Screw location (S1, S2) | Screw trajectory (IS, TS) | Total malpositioned screws | Neurologic complications associated with screw position | Screw types that caused neurologic injury | Permanent neurologic symptoms | Revision surgeries due to screw placement |
|---|---|---|---|---|---|---|---|---|---|---|
| Routt et al.3 | 177 | 1 | 244 | S1- 240 | IS- 244 | 5 (2%) | 1 (0.4%) | S1 IS- 1 | 0 (0%) | 1 (0.4%) |
| S2- 4 | ||||||||||
| Van den Bosch4 | 88 | NR | 220 | S1- 254 | IS- 220 | 15 (6.8%) | 7 (3.2%) | S1 IS- 1 | 0 (0%) | 8 (3.6%) |
| S2- 31 | S2 IS- 2 | |||||||||
| Osterhoff5 | 38 | NR | 82 | S1- 62 | IS- 82 | 4 (4.9%) | 2 (2.4%) | S1 IS- 1 | 2 (100%) | 3 (3.7%) |
| S2- 21 | S2 IS- 1 | |||||||||
| Schweitzer6 | 71 | NR | 109 | NR | IS- 109 | 3 (2.8%) | 2 (1.8%) | NR | 0 (0%) | 1 (0.9%) |
| Templeman1 | 31 | NR | 57 | S1- 57 | IS- 57 | 9 (15.8%) | 0 (0%) | NA | NA | 0 (0%) |
| Gardner7 | 68 | 1 | 106 | S1- 106 | IS- 106 | 0 (0%) | NA | NA | NA | NA |
| Boudissa8 | 165 | multiple | 194 | NR | IS- 194 | 31 (16%) | 3 (1.5%) | NR | 2 (67%) | 3 (1.5%) |
| Pishnamaz9 | 102 | 3 | 137 | NR | IS- 137 | 52 (38%) | 2 (1.5%) | NR | NR | NR |
| Gardner10 | 56 | 1 | 73 | S1- 38 | TS- 73 | 2 (2.7%) | 0 (0%) | NA | NA | 0 (0%) |
| S2- 35 | ||||||||||
| Zwingmann11 | 87 | 12 | 131 | NR | IS- 131 | 77 (58.8%) | 0 (0%) | NA | NA | 13 (9.9%) |
| Berger-Groch12 | 36 | 4 | 62 | S1- 60 | IS- 62 | 13 (21%) | NR | NR | NR | 3 (4.8%) |
| S2- 2 | ||||||||||
| Matiyahu13 | 58 | multi-center | 95 | NR | IS- 95 | 16 (16.8%) | NR | NR | NR | NR |
| Combined | 977 | 21 | 1510 | S1 - 577 | IS - 1193 | 15.5% | 1.3% | S1-IS – 50% | 33.4% | 2.8% |
| S2 - 93 | TS - 73 | S2-IS – 50% |
(NR-not reported, NA-not applicable, CT – computed tomography scan, TS – transsacral, IS – Iliosacral).
The rate of neurologic injury in this cohort was 3.2% (8/249) which is similar to previously published reports (0–3.2%)(Table 6).1,3, 4, 5, 6, 7, 8, 9, 10,20 The combined overall rate of neurologic injury from these previous studies is 1.3% (17/1,353). All of these reported neurologic injuries were the result of the oblique IS screw trajectories. The current study supports this finding as S1-IS screws were more likely to result in nerve injuries. There is limited evidence in the current literature on this comparison as currently published studies focus almost exclusively on S1-IS screws.
There were three persistent neurologic injuries in this cohort (38%, 3/8). One of these patients was lost to follow at 2 months, so it is unknown if that patient ever had any meaningful neurologic recovery. Additionally, one of these patients had partial return of motor function but persistent sensory changes. The overall rate of permanent neurologic injury in previously published reports was 27% (4/15).3, 4, 5, 6,8 Notably, in all but one of these instances, the screws were removed urgently (14/15).3, 4, 5, 6,8 In contrast, in the current study five patients with breached screws associated with iatrogenic nerve injuries did undergo screw removal. Two of these five patients had persistent neurologic injuries.
There is currently minimal evidence supporting removal of breached screws associated with iatrogenic nerve injuries. Considering that two nerve injuries adjacent to screw breaches in this study recovered postoperatively after screw removal, this practice is likely prudent to maximize the chance for recovery.
The main limitations of this study relate to the retrospective study design, especially in regards to monitoring of nerve injury and its recovery, which would be better assessed in a prospective manner. Additionally, the number of iatrogenic nerve injuries was small, making this study underpowered to look at risk factors and nerve recovery as demonstrated by the wide confidence intervals of the differences seen between groups. This study is also limited in that pelvic ring fracture reduction was not assessed and therefore we cannot comment on the relationship between persistent pelvic ring displacement and breached screws. While it is possible that screw breach was associated with increased pelvic ring displacement, each surgeon in this study routinely reduced pelvic ring displacement prior to screw insertion, therefore this data reflects current practice at a single level one trauma center.
Strengths of this study include a large number of screws, screw types, and patients, the use of a standardized screw breach distance measuring system, and the reporting of breach as a continuous variable which allows for a more granular study of screw breach and the risk of iatrogenic nerve injury.
In conclusion, percutaneous screw fixation of the posterior pelvic ring is a technically demanding procedure with a high cortical breach rate. The rate of neurologic injury is low and more likely to occur with S1-IS screws. Surgeons should maintain a high degree of caution when placing these screws and consider removal of any breached screw associated with an iatrogenic nerve injury.
Declaration of competing interest
The authors have no conflicts of interest to report. This study received no funding.
Footnotes
There was no funding for this project.
References
- 1.Templeman D., Schmidt A., Freeze J., Weisman I. Clinical Orthopaedics and Related Research. Springer New York LLC; 1996. Proximity of iliosacral screws to neurovascular structures after internal fixation; pp. 194–198. [DOI] [PubMed] [Google Scholar]
- 2.McLaren D.A., Busel G.A., Parikh H.R., et al. Corridor-diameter-dependent angular tolerance for safe transiliosacral screw placement: an anatomic study of 433 pelves. Eur J Orthop Surg Traumatol. 2021;(3):1–8. doi: 10.1007/s00590-021-02913-5. [DOI] [PubMed] [Google Scholar]
- 3.Routt M.L.C. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997;11(8):584–589. doi: 10.1097/00005131-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 4.van den Bosch E.W., van Zwienen C.M.A., van Vugt A.B. Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma. 2002;53(1):44–48. doi: 10.1097/00005373-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Osterhoff G., Ossendorf C., Wanner G.A., Simmen H.P., Werner C.M.L. Percutaneous iliosacral screw fixation in S1 and S2 for posterior pelvic ring injuries: technique and perioperative complications. Arch Orthop Trauma Surg. 2011;131(6):809–813. doi: 10.1007/s00402-010-1230-0. [DOI] [PubMed] [Google Scholar]
- 6.Schweitzer D., Zylberberg A., Córdova M., Gonzalez J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury. 2008;39(8):869–874. doi: 10.1016/j.injury.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 7.Gardner M.J., Farrell E.D., Nork S.E., Segina D.N., Chip Routt M.L. Percutaneous placement of iliosacral screws without electrodiagnostic monitoring. J Trauma Inj Infect Crit Care. 2009;66(5):1411–1415. doi: 10.1097/TA.0b013e31818080e9. [DOI] [PubMed] [Google Scholar]
- 8.Boudissa M., Roudet A., Fumat V., et al. Part 1: outcome of posterior pelvic ring injuries and associated prognostic factors – a five-year retrospective study of one hundred and sixty five operated cases with closed reduction and percutaneous fixation. Int Orthop. 2020;44(6):1209–1215. doi: 10.1007/s00264-020-04574-1. [DOI] [PubMed] [Google Scholar]
- 9.Pishnamaz M., Dienstknecht T., Hoppe B., et al. Assessment of pelvic injuries treated with ilio-sacral screws: injury severity and accuracy of screw positioning. Int Orthop. 2016;40(7):1495–1501. doi: 10.1007/s00264-015-2933-1. [DOI] [PubMed] [Google Scholar]
- 10.Gardner M.J., Routt M.L.C. Transiliac–transsacral screws for posterior pelvic stabilization. J Orthop Trauma. 2011;25(6):378–384. doi: 10.1097/BOT.0b013e3181e47fad. [DOI] [PubMed] [Google Scholar]
- 11.Zwingmann J., Hauschild O., Bode G., Südkamp N.P., Schmal H. Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2013;133(9):1257–1265. doi: 10.1007/s00402-013-1788-4. [DOI] [PubMed] [Google Scholar]
- 12.Berger-Groch J., Lueers M., Rueger J.M., et al. Accuracy of navigated and conventional iliosacral screw placement in B- and C-type pelvic ring fractures. Eur J Trauma Emerg Surg. 2020;46(1):107–113. doi: 10.1007/s00068-018-0990-z. [DOI] [PubMed] [Google Scholar]
- 13.Matityahu A., Kahler D., Krettek C., et al. Three-dimensional navigation is more accurate than two-dimensional navigation or conventional fluoroscopy for percutaneous sacroiliac screw fixation in the dysmorphic sacrum: a randomized multicenter study. J Orthop Trauma. 2014;28(12):707–710. doi: 10.1097/BOT.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 14.Shaw J., Gary J., Ambrose C., Routt M.C. Multidimensional pelvic fluoroscopy: a new and novel technique for assessing safety and accuracy of percutaneous iliosacral screw fixation. J Orthop Trauma. 2020;34(11):572–577. doi: 10.1097/BOT.0000000000001796. [DOI] [PubMed] [Google Scholar]
- 15.Kaiser S.P., Gardner M.J., Liu J., Routt M.L.C., Morshed S. Anatomic determinants of sacral dysmorphism and implications for safe iliosacral screw placement. J Bone Jt Surg - Am. 2014;96(14) doi: 10.2106/JBJS.M.00895. e120(1) [DOI] [PubMed] [Google Scholar]
- 16.Paley D. Principles of Deformity Correction. first ed. Springer; 2002. Translation and angulation-translation deformities; pp. 195–234. [Google Scholar]
- 17.Strage K., Parry J., Mauffrey C. Standardizing statistics and data reporting in orthopaedic research. Eur J Orthop Surg Traumatol. 2021;31(1) doi: 10.1007/S00590-020-02843-8. [DOI] [PubMed] [Google Scholar]
- 18.Efron B., Tibshirani R. The bootstrap method for assessing statistical accuracy. Behaviormetrika. 1985;12(17):1–35. doi: 10.2333/bhmk.12.17_1. [DOI] [Google Scholar]
- 19.Agresti A., Coull B.A. Approximate is better than “exact” for interval estimation of binomial proportions. Am Statistician. 1998;52(2):119–126. doi: 10.1080/00031305.1998.10480550. [DOI] [Google Scholar]
- 20.Zwingmann J., Konrad G., Mehlhorn A.T., Südkamp N.P., Oberst M. Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (Navigated Vs. Conventional) J Trauma Inj Infect Crit Care. 2010;69(6):1501–1506. doi: 10.1097/TA.0b013e3181d862db. [DOI] [PubMed] [Google Scholar]