Abstract
Background
Although laparoscopic hepatectomy (LH) is associated with improved short-term outcomes compared to open hepatectomy (OH), it is unknown whether frail patients also benefit from LH. The aim of this study was to evaluate the impact of frailty on post-operative outcomes after LH and OH.
Patients and methods
Consecutive patients who underwent LH and OH between January 2011 and December 2018 were identified from a prospective database. Frailty was assessed using the modified Frailty Index (mFI), with patients scoring mFI ≥ 1 deemed to be frail.
Results
Of 1826 patients, 34.7% (N = 634) were frail and 18.6% (N = 340) were elderly (≥ 75 years). Frail patients had significantly higher 90-day mortality (6.6% vs. 2.9%, p < 0.001) and post-operative complications (36.3% vs. 26.1%, p < 0.001) than those who were not frail, effects that were independent of patient age on multivariate analysis. For those undergoing minor resections, the benefits of LH vs. OH were similar for frail and non-frail patients. Length of hospital stay was 53% longer in OH (vs. LH) in frail patients, compared to 58% longer in the subgroup of non-frail patients.
Conclusions
Frailty is independently associated with inferior post-operative outcomes in patients undergoing hepatectomy. However, the benefits of laparoscopic (compared to open) hepatectomy are similar for frail and non-frail patients. Frailty should not be a contraindication to laparoscopic minor hepatectomy in carefully selected patients.
Introduction
Hepatectomy is a potentially curative treatment for patients with primary and secondary hepatic malignancies, and a laparoscopic approach, when feasible, is associated with less morbidity, lower mortality and faster recovery than open surgery [1, 2]. In an increasingly ageing population [3], there is a growing number of frail and elderly patients with comorbidity who are being considered for major surgery, including hepatectomy [4]. Although the risks of surgery are known to increase with advancing age, the short-term advantages of laparoscopic hepatectomy (LH) compared to open hepatectomy (OH) appear to be retained, at least in selected patients undergoing minor hepatectomy [5, 6]. However, the benefits of LH appear to diminish with increasing age amongst elderly cohorts [7], and it is not known whether similar benefits of LH are observed in frail patients.
Frailty is a condition that is characterised by reduced physiological reserve and is associated with an increased risk of post-operative complications, prolonged hospitalization, increased readmission rates and loss of independence following general surgical procedures [8]. Frailty is also common in patients undergoing hepatectomy, with a reported incidence of 14–29% in recently published studies [9, 10], although there is currently limited data to support an association with worse post-operative outcomes [10]. Available data on the impact of frailty in minimally invasive surgery is also limited and conflicting. In two recent studies of the ACS-NSQIP database, Kothari et al. demonstrated that the benefits of laparoscopic colectomy over open colectomy were preserved in frail patients [11], whilst Lo et al. reported possible worse outcomes after robotic compared to open colectomy [12]. The effects of frailty on the short-term outcomes of LH are unknown, and it is unclear whether frail patients should preferentially undergo LH or OH.
Various clinical scores have been developed and validated to measure frailty in surgical patients, and typically include an assessment of functional status combined with the presence and severity of comorbidity, such as diabetes mellitus, hypertension and cardiovascular disease [13]. The modified Frailty Index (mFI) [14] consists of 11 variables that were adapted from the original 70-item Frailty Index [15] and has been shown to be significantly associated with poor surgical outcomes, including after hepatectomy [8].
The primary aim of this study was to evaluate the effects of age and frailty on short-term post-operative outcomes after hepatectomy. The secondary aim was to evaluate the relationship between age, frailty and post-operative outcomes in patients undergoing laparoscopic and open hepatectomy.
Methods
Consecutive patients who underwent laparoscopic or open hepatectomy at a single centre between 2011 and 2018 were identified from a prospectively maintained database. Repeat hepatectomy (N = 152) and emergency hepatectomy for trauma (N = 4) patients were excluded. The type of hepatectomy was defined as minor, major or extra major according to the Tokyo 2020 terminology of liver anatomy and resections which is an update of the Brisbane 2000 system [16]. Frailty was defined as a modified Frailty Index (mFI) ≥ 1 and was calculated for all patients. Patients aged 75 years and over were considered elderly, and the effects of both frailty and age on hepatectomy outcomes were compared. Data were collected regarding comorbidity, indications for surgery, post-operative complications, length of hospital (LOS) and 90-day mortality. Post-operative complications were graded according to the Clavien–Dindo classification [17].
Statistical analysis
Continuous variables were reported as median (interquartile range; IQR), and associations with age and mFI were assessed using Mann–Whitney U tests. Ordinal variables were analysed using the same approach, whilst nominal variables were assessed using Fisher’s exact tests. To assess the interplay between age and frailty with respect to dichotomous patient outcomes, binary logistic regression models were produced with age, frailty and the age*frailty interaction as independent variables. These models were then evaluated to produce odds ratios for frail vs. non-frail patients within each age subgroup, with the p-value of the interaction term representing the comparison between these two odds ratios. Length of stay was then analysed using a similar approach, but using an ANOVA model. Lengths of stay were log10-transformed, prior to this analysis, in order to normalise the distribution; hence were summarised using geometric means, with differences between groups reported as percentages. Multivariable models were then produced, to assess whether age and frailty were independent predictors of the primary outcomes. This used binary logistic regression models for 90-day mortality and complication rates, with a general linear model used for length of stay, which was log10-transformed for analysis. Age and frailty were entered into the models as continuous covariates, and a backwards stepwise approach was used to select other potentially confounding factors for inclusion in the models. Analyses were then performed to compare the effect of operative approach (open vs. laparoscopic) between subgroups of age and frailty, which used a similar approach to that previously described. All analyses were performed using IBM SPSS 24 (IBM Corp. Armonk, NY), with p < 0.05 deemed to be indicative of statistical significance throughout.
Results
Cohort characteristics
Data were available for a total of N = 1826 patients (56.6% male), with a median age of 65.3 years (IQR: 56.0–73.1). The most common indication for surgery was colorectal liver metastases (58.8%), with the majority of patients undergoing open surgery (86.0%). The extent of resection was minor in 53.1% of cases, with 33.3% major and 13.6% extra-major resections. Major (Clavien–Dindo grade III-V) complications developed in 10.7% of patients, and patients surviving to discharge had a median length of stay of 6 days (IQR: 5–8). In-hospital, 30-day and 90-day mortality rates were 2.2% (N = 40), 1.9% (N = 35) and 4.2% (N = 76), respectively.
Age and frailty of the cohort
The majority of patients scored 0 on the mFI (65.3%), with 25.9%, 8.5%, and 0.3% scoring 1, 2 and 3 points, respectively. The hypertension and diabetes mellitus components were the main contributors to the mFI scores, being present in 26.1% and 13.3% of patients, respectively. Only 0.3% (N = 5) of patients were non-independent with their activities of daily living. A significant correlation between age and mFI was observed (rho: 0.304, p < 0.001), with the median age increasing from 62.1 (IQR: 52.2–70.9) to 71.7 (64.4–76.7) years, for those with an mFI of 0 vs. 2–3. This was largely as a result of the comorbidity components of the mFI, with rates of hypertension, diabetes mellitus and COPD/pneumonia all increasing significantly with age (all p < 0.001).
Characteristics and outcomes by age and frailty
For the initial analyses, both age and mFI were dichotomised, with age ≥ 75 years classified as “elderly” (18.6%; N = 340), and mFI ≥ 1 classified as “frail” (34.7%; N = 634). Of the demographic factors considered (Table 1), both elderly and frail patients were found to be significantly more likely to be male, and to have malignant tumours. Elderly patients were additionally found to have significantly less extensive resections, compared to the non-elderly (p = 0.042; minor resections: 57.6% vs. 52.1%), with a corresponding reduction in the average operative duration (median: 4.2 vs. 4.6 h; p < 0.001); no such significant differences were observed for the analysis of frailty (p = 0.200, p = 0.451, respectively). Rates of open (vs. laparoscopic) surgery were not found to differ significantly by age (p = 0.260) or frailty (p = 0.229). Univariable analysis of post-operative outcomes found overall complication rates to be significantly higher in both elderly (34.1% vs. 28.6%, p = 0.048) and frail (36.3% vs. 26.1%, p < 0.001) patients (Table 2). Further assessment of complication types found that this was largely a result of higher rates of medical complications (p < 0.001 for both), with surgical complication rates not found to be significantly higher in either elderly (p = 0.270) or frail (p = 0.061) patients. Elderly patients also had significantly longer lengths of stay (median: 7 vs. 6 days, p < 0.001), with no such difference observed for frail patients (median: 6 vs. 6 days, p = 0.060). Mortality rates were also significantly higher in the elderly and the frail, with 90-day mortality of 6.8% vs. 3.6% (p = 0.015) for elderly vs. non-elderly, and 6.6% vs. 2.9% (p < 0.001) for frail vs. non-frail.
Table 1.
Cohort characteristics by age and frailty
| N | Age at surgery | mFI Score | |||||
|---|---|---|---|---|---|---|---|
| < 75 years | ≥ 75 years | p-value | mFI = 0 | mFI ≥ 1 | p-value | ||
| Age at surgery (years) | 1826 | 62.2 (53.4–68.7) | 78.6 (76.6–80.8) | N/A | 62.1 (52.2–70.9) | 69.7 (63.2–75.6) | < 0.001 |
| Gender (% male) | 1826 | 812 (54.6%) | 222 (65.3%) | < 0.001 | 615 (51.6%) | 419 (66.1%) | < 0.001 |
| BMI (kg/m2) | 1825 | 27.1 (24.3–30.9) | 27.2 (24.7–30.0) | 0.840 | 26.6 (23.9–29.8) | 28.4 (25.5–31.8) | < 0.001 |
| ASA grade (% > 2) | 1826 | 421 (28.3%) | 103 (30.3%) | 0.466 | 345 (28.9%) | 179 (28.2%) | 0.786 |
| Hypertension | 1826 | 333 (22.4%) | 144 (42.4%) | < 0.001 | 0 (0.0%) | 477 (75.2%) | N/A |
| Diabetes mellitus | 1826 | 177 (11.9%) | 65 (19.1%) | < 0.001 | 0 (0.0%) | 242 (38.2%) | N/A |
| Congestive heart failure | 1826 | 2 (0.1%) | 0 (0.0%) | 1.000 | 0 (0.0%) | 2 (0.3%) | N/A |
| COPD/pneumonia | 1826 | 52 (3.5%) | 22 (6.5%) | 0.021 | 0 (0.0%) | 74 (11.7%) | N/A |
| Non-independent in ADL | 1826 | 4 (0.3%) | 1 (0.3%) | 1.000 | 0 (0.0%) | 5 (0.8%) | N/A |
| mFI (% ≥ 1) | 1826 | 456 (30.7%) | 178 (52.4%) | < 0.001 | – | – | – |
| Indication for surgery | 1826 | < 0.001 | < 0.001 | ||||
| Colorectal liver metastases | 848 (57.1%) | 226 (66.5%) | 705 (59.1%) | 369 (58.2%) | |||
| Hepatocellular carcinoma | 115 (7.7%) | 49 (14.4%) | 75 (6.3%) | 89 (14.0%) | |||
| Gallbladder cancer/cholangiocarcinoma | 149 (10.0%) | 31 (9.1%) | 102 (8.6%) | 78 (12.3%) | |||
| Other malignant | 145 (9.8%) | 18 (5.3%) | 123 (10.3%) | 40 (6.3%) | |||
| Benign | 229 (15.4%) | 16 (4.7%) | 187 (15.7%) | 58 (9.1%) | |||
| Extent of resection | 1826 | 0.042** | 0.200** | ||||
| Minor | 774 (52.1%) | 196 (57.6%) | 623 (52.3%) | 347 (54.7%) | |||
| Major | 501 (33.7%) | 107 (31.5%) | 397 (33.3%) | 211 (33.3%) | |||
| Extra-major | 211 (14.2%) | 37 (10.9%) | 172 (14.4%) | 76 (12.0%) | |||
| Operative approach (% open) | 1826 | 1285 (86.5%) | 286 (84.1%) | 0.260 | 1034 (86.7%) | 537 (84.7%) | 0.229 |
| Operative duration (hours) | 1790 | 4.6 (3.6–5.8) | 4.2 (3.4–5.2) | < 0.001 | 4.5 (3.5–5.7) | 4.4 (3.5–5.6) | 0.451 |
| Blood transfusion* | 1826 | 147 (9.9%) | 43 (12.6%) | 0.140 | 119 (10.0%) | 71 (11.2%) | 0.422 |
Continuous variables are reported as median (interquartile range), with p-values from Mann–Whitney U tests. Categorical variables are reported as N (column %), with p-values from Fisher’s exact tests, unless stated otherwise. Bold p-values are significant at p < 0.05. *Within 24 h post-operatively. **p-Value from Mann–Whitney U test, as the factor is ordinal. ADL activities of daily living; BMI body mass index; COPD Chronic obstructive pulmonary disease; mFI modified frailty index
Table 2.
Post-operative complications by patient age and modified Frailty Index
| Age at surgery | mFI Score | |||||
|---|---|---|---|---|---|---|
| < 75 years | ≥ 75 years | p-value | mFI = 0 | mFI ≥ 1 | p-value | |
| Any complications | 425 (28.6%) | 116 (34.1%) | 0.048 | 311 (26.1%) | 230 (36.3%) | < 0.001 |
| Highest Clavien–Dindo grade | 0.032** | < 0.001** | ||||
| No complication | 1061 (71.4%) | 224 (65.9%) | 881 (73.9%) | 404 (63.7%) | ||
| Grade I–II | 270 (18.2%) | 75 (22.1%) | 201 (16.9%) | 144 (22.7%) | ||
| Grade III–V | 155 (10.4%) | 41 (12.1%) | 110 (9.2%) | 86 (13.6%) | ||
| Length of stay (days)* | 6 (5–8) | 7 (5–9) | < 0.001 | 6 (5–8) | 6 (5–9) | 0.060 |
| 30-day mortality | 22 (1.5%) | 13 (3.8%) | 0.008 | 14 (1.2%) | 21 (3.3%) | 0.002 |
| 90-day mortality | 53 (3.6%) | 23 (6.8%) | 0.015 | 34 (2.9%) | 42 (6.6%) | < 0.001 |
| In-hospital mortality | 25 (1.7%) | 15 (4.4%) | 0.006 | 17 (1.4%) | 23 (3.6%) | 0.004 |
| Details of surgical complications | ||||||
| PHLF | 45 (3.0%) | 7 (2.1%) | 0.468 | 28 (2.3%) | 24 (3.8%) | 0.103 |
| PHLF Grade | 0.335** | 0.079** | ||||
| No PHLF | 1441 (97.0%) | 333 (97.9%) | 1164 (97.7%) | 610 (96.2%) | ||
| Grade A | 24 (1.6%) | 3 (0.9%) | 14 (1.2%) | 13 (2.1%) | ||
| Grade B | 8 (0.5%) | 2 (0.6%) | 7 (0.6%) | 3 (0.5%) | ||
| Grade C | 13 (0.9%) | 2 (0.6%) | 7 (0.6%) | 8 (1.3%) | ||
| Bile leak | 65 (4.4%) | 9 (2.6%) | 0.170 | 41 (3.4%) | 33 (5.2%) | 0.081 |
| Post-operative haemorrhage | 25 (1.7%) | 8 (2.4%) | 0.372 | 23 (1.9%) | 10 (1.6%) | 0.713 |
| Wound infection | 45 (3.0%) | 10 (2.9%) | 1.000 | 37 (3.1%) | 18 (2.8%) | 0.886 |
| Re-operation for bleeding | 10 (0.7%) | 5 (1.5%) | 0.175 | 11 (0.9%) | 4 (0.6%) | 0.597 |
| Radiological drainage of collection | 42 (2.8%) | 6 (1.8%) | 0.348 | 28 (2.3%) | 20 (3.2%) | 0.357 |
| Other surgical complication | 32 (2.2%) | 5 (1.5%) | 0.526 | 20 (1.7%) | 17 (2.7%) | 0.164 |
| Any of the above | 226 (15.2%) | 43 (12.6%) | 0.270 | 162 (13.6%) | 107 (16.9%) | 0.061 |
| Details of medical complications | ||||||
| Pneumonia | 85 (5.7%) | 20 (5.9%) | 0.897 | 62 (5.2%) | 43 (6.8%) | 0.171 |
| AKI (requiring RRT) | 4 (0.3%) | 2 (0.6%) | 0.311 | 3 (0.3%) | 3 (0.5%) | 0.424 |
| Respiratory failure (requiring vent.) | 12 (0.8%) | 5 (1.5%) | 0.342 | 10 (0.8%) | 7 (1.1%) | 0.613 |
| Myocardial infarction | 5 (0.3%) | 3 (0.9%) | 0.173 | 6 (0.5%) | 2 (0.3%) | 0.722 |
| Dysrhythmia | 35 (2.4%) | 20 (5.9%) | 0.001 | 30 (2.5%) | 25 (3.9%) | 0.113 |
| Other medical complication | 120 (8.1%) | 40 (11.8%) | 0.034 | 84 (7.0%) | 76 (12.0%) | < 0.001 |
| Any of the above | 247 (16.6%) | 84 (24.7%) | < 0.001 | 182 (15.3%) | 149 (23.5%) | < 0.001 |
Continuous variables are reported as median (interquartile range), with p-values from Mann–Whitney U tests. Categorical variables are reported as N (column %), with p-values from Fisher’s exact tests, unless stated otherwise. Bold p-values are significant at p < 0.05. *Excludes patients that died in hospital prior to discharge. **p-Value from Mann–Whitney U test, as the factor is ordinal. AKI acute kidney injury; mFI modified frailty index; PHLF Post hepatectomy liver failure; RRT renal replacement therapy; Vent. ventilation
Interplay between age and frailty
Comparisons of outcomes between frail and non-frail patients were then performed within the elderly and non-elderly patient subgroups. Analysis of mortality, complication rates and length of stay found the effect of frailty to be similar in non-elderly and elderly patients (Table 3). For example, for non-elderly patients, frailty (vs. non-frailty) was associated with odds ratio for 90-day mortality of 2.25 (5.7% vs. 2.6%), which was similar to the 2.19 (9.0% vs. 4.3%) observed in elderly patients (p = 0.961).
Table 3.
Interplay between age and frailty
| Age: < 75 years | Age: ≥ 75 years | Interaction term p-value | |||||
|---|---|---|---|---|---|---|---|
| mFI = 0 (N = 1030) | mFI ≥ 1 (N = 456) | Odds ratio (95% CI) | mFI = 0 (N = 162) | mFI ≥ 1 (N = 178) | Odds ratio (95% CI) | ||
| Any complications | 265 (25.7%) | 160 (35.1%) | 1.56 (1.23–1.98) | 46 (28.4%) | 70 (39.3%) | 1.63 (1.04–2.58) | 0.860 |
| Any surgical complication | 143 (13.9%) | 83 (18.2%) | 1.38 (1.03–1.86) | 19 (11.7%) | 24 (13.5%) | 1.17 (0.62–2.23) | 0.652 |
| Any medical complication | 151 (14.7%) | 96 (21.1%) | 1.55 (1.17–2.06) | 31 (19.1%) | 53 (29.8%) | 1.79 (1.08–2.97) | 0.628 |
| Length of stay (days)* | 6.3 (6.1, 6.5)* | 6.5 (6.2, 6.9)* | 4% (− 3%, 10%) | 6.9 (6.3, 7.6)* | 7.8 (7.0, 8.6)* | 12% (− 2%, 28%)* | 0.276* |
| In-hospital mortality | 13 (1.3%) | 12 (2.6%) | 2.11 (0.96–4.67) | 4 (2.5%) | 11 (6.2%) | 2.60 (0.81–8.34) | 0.773 |
| 30-day mortality | 10 (1.0%) | 12 (2.6%) | 2.76 (1.18–6.43) | 4 (2.5%) | 9 (5.1%) | 2.10 (0.64–6.97) | 0.718 |
| 90-day mortality | 27 (2.6%) | 26 (5.7%) | 2.25 (1.30–3.89) | 7 (4.3%) | 16 (9.0%) | 2.19 (0.88–5.46) | 0.961 |
For binary outcomes, odds ratios are from binary logistic regression models within each age subgroup, with mFI (≥ 1 vs. 0) as the independent variable. The p-values relate to the interaction terms of binary logistic regression models with age, frailty and the age*frailty interaction as independent variables, hence represent a comparison between the reported odds ratio for each subgroup. *Analysis of length of stay excluded those patients who died in hospital prior to discharge. For the remainder, the average lengths of stay are reported as geometric mean (95% CI). Lengths of stay were then log10-transformed, and analysed using an ANOVA model, parameterised as previously described, with the comparisons between groups reported as percentage differences. CI confidence interval; mFI modified frailty index
Associations with primary outcomes
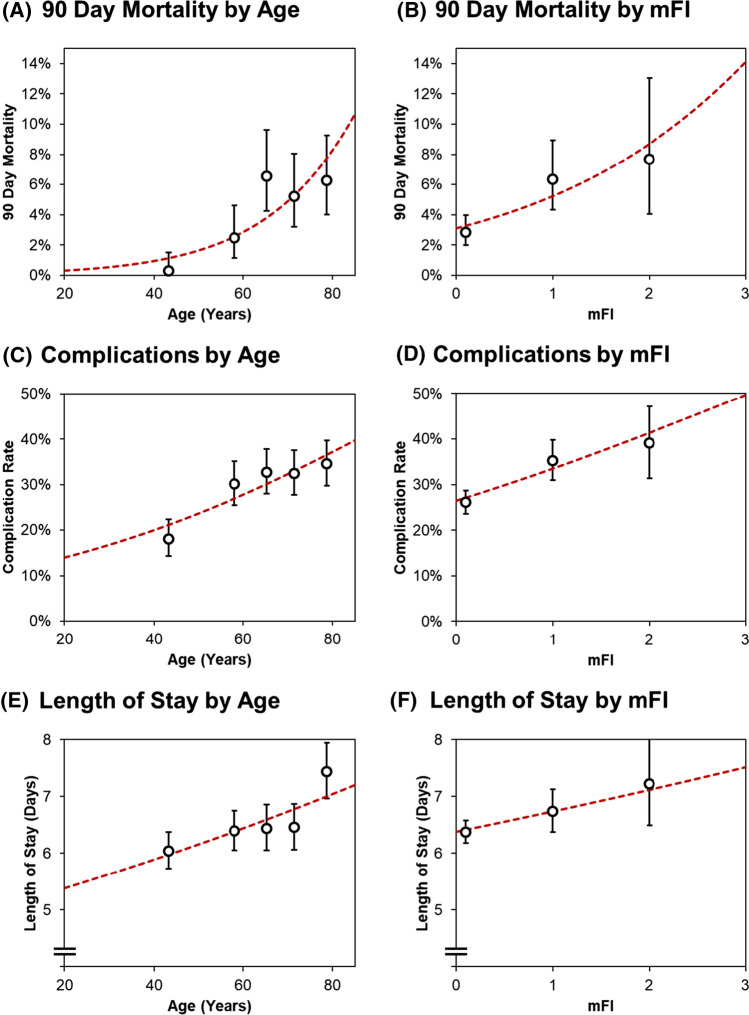
The associations between both age and frailty, and the primary outcomes of 90-day mortality, post-operative complications and length of stay were then assessed in further detail. Age and mFI were treated as continuous covariates in these analyses and were found to be significantly associated with all three outcomes on univariable analysis (Fig. 1). On multivariable analysis, both age and mFI were found to be significant independent predictors of 90-day mortality, with odds ratios of 1.71 (95% CI: 1.32–2.22, p < 0.001) per decade of age and 1.45 (1.04–2.03, p = 0.029) per point on the mFI (Table 4). Age and mFI were found to be significant independent predictors of post-operative complications (p < 0.001, p = 0.002, respectively). Whilst age was found to be significantly associated with length of stay (p < 0.001), mFI narrowly missed statistical significance in this analysis (p = 0.056).
Fig. 1.
Associations between age/mFI and the primary outcomes. Points represent the observed mortality/complication rates, or the geometric mean lengths of stay, with whiskers representing 95% confidence intervals. For age, each point corresponds to a quintile of the age distribution, and is plotted at the mean of the interval, whilst points for mFI correspond to values of 0, 1 and 2; mFI = 3 was not plotted, due to the small sample size (N = 5). Trend lines are from univariable binary logistic regression models for the dichotomous outcomes, with a univariable log-linear regression model used for length of stay, as per Table 4
Table 4.
Associations between age/frailty and primary outcomes
| Univariable analysis | Multivariable analysis | |||
|---|---|---|---|---|
| Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | |
| 90-day mortality | ||||
| Age at surgery (per decade) | 1.75 (1.39–2.22) | < 0.001 | 1.71 (1.32–2.22) | < 0.001 |
| mFI (per point) | 1.72 (1.28–2.32) | < 0.001 | 1.45 (1.04–2.03) | 0.029 |
| Any post-operative complications | ||||
| Age at surgery (per decade) | 1.24 (1.14–1.35) | < 0.001 | 1.26 (1.14–1.39) | < 0.001 |
| mFI (per point) | 1.40 (1.21–1.62) | < 0.001 | 1.30 (1.10–1.53) | 0.002 |
| Length of stay | ||||
| Age at surgery (per decade) | 4.5% (2.4%, 6.7%) | < 0.001 | 5.9% (3.7%, 8.1%) | < 0.001 |
| mFI (per point) | 5.5% (1.4%, 9.9%) | 0.009 | 3.8% (− 0.1%, 8.0%) | 0.056 |
Analyses of 90-day mortality and complications were performed using binary logistic regression models, with coefficients representing odds ratios. Analysis of length of stay was performed using general linear models, with the log10[length of stay] as the dependent variable; coefficients represent percentage differences. For all outcomes, age and mFI were initially treated as continuous covariates in separate univariable models, with coefficients representing the change in the outcome per decade or per point, respectively. Multivariable models were then produced, which considered gender, BMI, ASA grade, indication for surgery, extent of resection, operative approach and duration of surgery for inclusion, with a backwards stepwise approach to variable selection. The full models are reported in Supplementary Table 1–3. Bold p-values are significant at p < 0.05. CI confidence interval; mFI modified frailty index; OR odds ratio
Effect of operative approach by age and frailty in minor resections
The operative approach was found to vary significantly by the extent of the resection (p < 0.001), with 22.3% of minor resections being laparoscopic, compared to 6.1% of major and 0.8% of extra-major resections. As such, to negate the confounding effect of the extent of resection, only the subgroup of minor resections were considered in the analysis (N = 970). Within this subgroup, neither complication nor mortality rates were found to differ significantly by the operative approach (Table 5). However, open surgery was associated with a significantly longer operative duration (median: 4.1 vs. 3.6 h, p < 0.001) and length of stay (median 6 vs. 4 days, p < 0.001), compared to laparoscopic surgery. The effects of operative approach were then compared between elderly vs. non-elderly and frail vs. non-frail patients (Table 6). We found no evidence to suggest that the effect of operative approach varied significantly by age or frailty for any of the outcomes considered. For example, open (vs. laparoscopic) surgery was associated with a 53% (geometric mean: 6.5 vs. 4.2 days) longer length of stay in frail patients, which was similar to the 58% (6.1 vs. 3.8 days) longer length of stay after open (vs. laparoscopic) surgery in non-frail patients (p = 0.699). As such, the relative benefits of laparoscopic vs. open surgery appeared to be similar, regardless of the age or frailty of the patient. However, these analyses were limited by the small number of outcomes occurring within some subgroups of patients, with no events being observed for some of the outcomes considered. This will have resulted in very low statistical power, meaning that only large differences will have been detectable. As such, this analysis will be subject to an inflated false-negative rate, and the results must be interpreted with this in mind.
Table 5.
Outcomes by operative approach in minor resections
| Operative approach | |||
|---|---|---|---|
| Laparoscopic (N = 216) | Open (N = 754) | p-value | |
| Operative duration (hours) | 3.6 (3.0–4.4) | 4.1 (3.3–5.2) | < 0.001 |
| Any complications | 37 (17.1%) | 175 (23.2%) | 0.062 |
| Any surgical complication | 13 (6.0%) | 74 (9.8%) | 0.104 |
| Any medical complication | 24 (11.1%) | 110 (14.6%) | 0.219 |
| Length of stay (days)* | 4 (3–5) | 6 (5–7) | < 0.001 |
| In-hospital mortality | 2 (0.9%) | 7 (0.9%) | 1.000 |
| 30-day mortality | 2 (0.9%) | 6 (0.8%) | 1.000 |
| 90-day mortality | 3 (1.4%) | 19 (2.5%) | 0.441 |
Only those patients with minor resections (N = 970) are included in the analysis. Data are reported as N (column %), with p-values from Fisher’s exact tests, or as median (interquartile range), with p-values from Mann–Whitney U tests. Bold p-values are significant at p < 0.05. *Analysis of length of stay excluded those patients who died in hospital prior to discharge
Table 6.
Interplay between operative approach and age/frailty in minor resections
| Age: < 75 years | Age: ≥ 75 years | ||||||
|---|---|---|---|---|---|---|---|
| Laparoscopic (N = 172) | Open (N = 602) | Odds ratio (95% CI) | Laparoscopic (N = 44) | Open (N = 152) | Odds ratio (95% CI) | Interaction term p-value | |
| Operative duration (hours)* | 3.7 (3.5, 3.9)* | 4.2 (4.1, 4.4)* | 15% (8%, 22%)* | 3.8 (3.5, 4.2)* | 3.9 (3.8, 4.1)* | 3% (− 6%, 14%)* | 0.096* |
| Any complications | 29 (16.9%) | 132 (21.9%) | 1.38 (0.89–2.16) | 8 (18.2%) | 43 (28.3%) | 1.78 (0.76–4.13) | 0.610 |
| Any surgical complication | 11 (6.4%) | 60 (10.0%) | 1.62 (0.83–3.16) | 2 (4.5%) | 14 (9.2%) | 2.13 (0.47–9.75) | 0.747 |
| Any medical complication | 18 (10.5%) | 79 (13.1%) | 1.29 (0.75–2.22) | 6 (13.6%) | 31 (20.4%) | 1.62 (0.63–4.18) | 0.683 |
| Length of stay (days)* | 3.9 (3.6, 4.2)* | 6.0 (5.8, 6.3)* | 54% (41%, 67%)* | 4.4 (3.7, 5.1)* | 7.1 (6.5, 7.7)* | 61% (34%, 92%)* | 0.632* |
| In-hospital mortality | 0 (0.0%) | 4 (0.7%) | NC** | 2 (4.5%) | 3 (2.0%) | 0.42 (0.07–2.61) | NC** |
| 30-day mortality | 0 (0.0%) | 3 (0.5%) | NC** | 2 (4.5%) | 3 (2.0%) | 0.42 (0.07–2.61) | NC** |
| 90-day mortality | 1 (0.6%) | 15 (2.5%) | 4.37 (0.57–33.3) | 2 (4.5%) | 4 (2.6%) | 0.57 (0.10–3.21) | 0.134 |
| mFI = 0 | mFI ≥ 1 | ||||||
|---|---|---|---|---|---|---|---|
| Laparoscopic (N = 130) | Open (N = 493) | Odds ratio (95% CI) | Laparoscopic (N = 86) | Open (N = 261) | Odds ratio (95% CI) | Interaction term p-value | |
| Operative duration (hours)* | 3.6 (3.4, 3.8)* | 4.2 (4.1, 4.3)* | 17% (10%, 25%)* | 3.9 (3.6, 4.2)* | 4.1 (4.0, 4.3)* | 6% (− 2%, 15%)* | 0.066* |
| Any complications | 21 (16.2%) | 97 (19.7%) | 1.27 (0.76–2.13) | 16 (18.6%) | 78 (29.9%) | 1.86 (1.02–3.41) | 0.345 |
| Any surgical complication | 8 (6.2%) | 42 (8.5%) | 1.42 (0.65–3.10) | 5 (5.8%) | 32 (12.3%) | 2.26 (0.85–6.01) | 0.465 |
| Any medical complication | 13 (10.0%) | 61 (12.4%) | 1.27 (0.68–2.39) | 11 (12.8%) | 49 (18.8%) | 1.58 (0.78–3.19) | 0.656 |
| Length of stay (days)* | 3.8 (3.5, 4.2)* | 6.1 (5.8, 6.3)* | 58% (43%, 73%)* | 4.2 (3.8, 4.8)* | 6.5 (6.1, 6.9)* | 53% (34%, 74%)* | 0.699* |
| In-hospital mortality | 1 (0.8%) | 3 (0.6%) | 0.79 (0.08–7.66) | 1 (1.2%) | 4 (1.5%) | 1.32 (0.15–12.00) | 0.749 |
| 30-day mortality | 1 (0.8%) | 3 (0.6%) | 0.79 (0.08–7.66) | 1 (1.2%) | 3 (1.1%) | 0.99 (0.10–9.63) | 0.891 |
| 90-day mortality | 1 (0.8%) | 9 (1.8%) | 2.40 (0.30–19.1) | 2 (2.3%) | 10 (3.8%) | 1.67 (0.36–7.79) | 0.785 |
Only those patients with minor resections (N = 970) are included in the analysis, with analysis of length of stay additionally excluding those patients who died in hospital prior to discharge. For the analysis by age, odds ratios are from binary logistic regression models within each age subgroup, with the operative approach (open vs. laparoscopic) as the independent variable. The p-values relate to the interaction terms of binary logistic regression models with age, operative approach and the age*operative approach interaction as independent variables, hence represent a comparison between the reported odds ratio for each subgroup. The analysis was repeated similarly for mFI. *Operative duration and length of stay followed skewed distributions, hence were log10-transformed, and analysed using an ANOVA model, parameterised as previously described; averages are reported as geometric means (95% CI), and comparisons between groups are reported as percentage differences. **Hazard ratios were not calculable, as there were no events in one of the subgroups
Discussion
Frailty is increasingly recognised as being an important determinant of post-operative outcomes in surgical patients [18], and our data have shown that frailty is an independent predictor of morbidity and mortality after hepatectomy. Over one third of patients in this large cohort were considered frail, and despite acceptable short-term outcomes, were exposed to an increased risk of medical complications, prolonged recovery and post-operative mortality compared to non-frail patients, which is consistent with published data [9, 19, 20]. Importantly, frailty was associated with worse outcomes for both elderly and non-elderly patients undergoing hepatectomy. Data from meta-analyses and randomized trials have shown that laparoscopic hepatectomy is associated with improved short-term outcomes compared to open hepatectomy [2, 21]. Our analysis has indicated that the short-term benefits (e.g. reduced hospital stay) of laparoscopic surgery are retained in frail patients undergoing minor hepatectomy, and suggests that in carefully selected patients, frailty is not a contraindication to laparoscopic minor hepatectomy. This finding is not unexpected, since the benefits of laparoscopic surgery are primarily due to reduced medical complications, which occur as a result of less post-operative pain, improved respiratory function and earlier ambulation. It is unknown whether frail patients undergoing major hepatectomy would also benefit from a laparoscopic approach. A recent patient blinded randomized trial demonstrated a faster recovery in patients undergoing laparoscopic major hepatectomy compared to open [22], but there is currently no data specifically evaluating the outcomes of laparoscopic major hepatectomy in frail patients. Laparoscopic major hepatectomy is a complex procedure associated with significantly longer operating times and longer hepatic inflow occlusion times compared to open surgery, and it is unknown whether these factors may negate the potential benefits of laparoscopic surgery in frail patients. It was not possible to evaluate the effect of laparoscopic approach in frail patients undergoing major hepatectomy in our study due to small numbers in this subgroup (Supplementary Table 4), and it is likely that a multi-centre study would be required.
Detection of frailty prior to major surgery is important, since it may allow risk stratification, facilitates preoperative counselling, and guides perioperative management including choice of post-operative destination (i.e. critical care or surgical high dependency). Frail patients may also benefit from preoperative interventions to address reversible deficits (e.g. aerobic fitness and nutrition) [23], and the concept of prehabilitation is likely to become a central component of perioperative care for patients being considered for hepatectomy in the near future [24, 25]. Post-operative functional recovery following hospital discharge and return to baseline function is an under-researched, patient-centred outcome that may also be influenced by frailty. A recent Japanese study of over 65-year-old patients undergoing hepatectomy found that frailty, advanced age (≥ 76 years) and open hepatectomy were independent risk factors for post-operative loss of independence [9].
This study has several limitations. Due to its retrospective nature, the effect of selection bias on the operative approach may have affected the results, and it was also not possible to ascertain how many patients were deemed unsuitable for hepatectomy due to severe frailty. As discussed above, the small number of laparoscopic major hepatectomy patients precluded analysis of the impact of frailty and outcome in this subgroup.
In conclusion, frailty is a common finding in patients undergoing hepatectomy, and is an independent risk factors for post-operative morbidity and mortality. The short-term benefits of laparoscopic hepatectomy appear to be preserved in frail patients. As such, frailty is not contraindicated in patients being considered for laparoscopic minor hepatectomy. Further study is needed to determine if frail patients would also benefit from laparoscopic major hepatectomy.
Declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
D. Osei-Bordom and L. Hall have contributed equally.
References
- 1.Hallet J, et al. Short and long-term outcomes of laparoscopic compared to open liver resection for colorectal liver metastases. HepatoBiliary Surg Nutr. 2016;5:300–310. doi: 10.21037/hbsn.2016.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fretland ÅA, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 2018;267:199–207. doi: 10.1097/SLA.0000000000002353. [DOI] [PubMed] [Google Scholar]
- 3.Lunenfeld B, Stratton P. The clinical consequences of an ageing world and preventive strategies. Best Pract Res Clin Obstet Gynaecol. 2013;27:643–659. doi: 10.1016/j.bpobgyn.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen K, Pan Y, Maher H, Zhang B, Zheng XY (2018) Laparoscopic hepatectomy for elderly patients major findings based on a systematic review and meta-analysis. Medicine (United States) 97 [DOI] [PMC free article] [PubMed]
- 5.Hildebrand N, et al. Short-term outcomes of laparoscopic versus open hepatectomy in the elderly patient: systematic review and meta-analysis. HPB. 2021;23:984–993. doi: 10.1016/j.hpb.2021.01.016. [DOI] [PubMed] [Google Scholar]
- 6.MohamedAhmed AYY, et al. Laparoscopic versus open hepatectomy for malignant liver tumours in the elderly: systematic review and meta-analysis. Updates Surg. 2021;73:1623–1641. doi: 10.1007/s13304-021-01091-7. [DOI] [PubMed] [Google Scholar]
- 7.Martínez-Cecilia D et al (2017) Laparoscopic versus open liver resection for colorectal metastases in elderly and octogenarian patients: a multicenter propensity score based analysis of short- and long-term outcomes. Ann Surg 265 [DOI] [PubMed]
- 8.Wahl TS, et al. Association of the modified frailty index with 30-day surgical readmission. JAMA Surg. 2017;152:749–757. doi: 10.1001/jamasurg.2017.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanaka S, et al. Preoperative assessment of frailty predicts age-related events after hepatic resection: a prospective multicenter study. J Hepatobiliary Pancreat Sci. 2018;25:377–387. doi: 10.1002/jhbp.568. [DOI] [PubMed] [Google Scholar]
- 10.Serrano PE, Mckechnie T, Bao T, Fabbro M, Ruo L (2021) Frailty as a predictor of postoperative morbidity and mortality following liver resection 87 [DOI] [PubMed]
- 11.Kothari P, Congiusta DV, Merchant AM. Laparoscopic versus open colectomy: the impact of frailty on outcomes. Updates Surg. 2019;71:89–96. doi: 10.1007/s13304-018-0531-7. [DOI] [PubMed] [Google Scholar]
- 12.Lo BD et al Frailer patients undergoing robotic colectomies for colon cancer experience increased complication rates compared with open or laparoscopic approaches. [DOI] [PubMed]
- 13.Koohestani D, Chobrutskiy BI, Janjua H, Velanovich V The accumulating deficits model for postoperative mortality and readmissions: comparison of four methods over multiple calendar year cohorts: brief title: stability of the modified frailty index. 10.1097/SLA.0000000000004421 [DOI] [PubMed]
- 14.Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res. 2013;183:104–110. doi: 10.1016/j.jss.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wakabayashi G, Cherqui D, Geller DA, Abu Hilal M, Berardi G, Ciria R, Abe Y, Aoki T, Asbun HJ, Chan ACY, Chanwat R, Chen K-H, Chen Y, Cheung TT, Fuks D, Gotohda N, Han H-S, Hasegawa K, Hatano E, Yamamoto M. The Tokyo 2020 terminology of liver anatomy and resections: updates of the Brisbane 2000 system. J Hepatobiliary Pancreat Sci. 2022;29(1):6–15. doi: 10.1002/jhbp.1091. [DOI] [PubMed] [Google Scholar]
- 17.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin HS, Watts JN, Peel NM, Hubbard RE (2016) Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr 16 [DOI] [PMC free article] [PubMed]
- 19.Wagner D. Role of frailty and sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg. 2016;8:27. doi: 10.4240/wjgs.v8.i1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gani F, et al. Frailty as a risk predictor of morbidity and mortality following liver surgery. J Gastrointest Surg. 2017;21:822–830. doi: 10.1007/s11605-017-3373-6. [DOI] [PubMed] [Google Scholar]
- 21.Mirnezami R, et al. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB. 2011;13:295–308. doi: 10.1111/j.1477-2574.2011.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong-Lun-Hing EM, et al. Randomized clinical trial of open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery after surgery programme (ORANGE II study) Br J Surg. 2017;104:525–535. doi: 10.1002/bjs.10438. [DOI] [PubMed] [Google Scholar]
- 23.Baimas-George M, et al. Prehabilitation for hepatopancreatobiliary surgical patients: interim analysis demonstrates a protective effect from neoadjuvant chemotherapy and improvement in the frailty phenotype. Am Surg. 2021;87:714–724. doi: 10.1177/0003134820952378. [DOI] [PubMed] [Google Scholar]
- 24.Dunne DFJ, et al. Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg. 2016;103:504–512. doi: 10.1002/bjs.10096. [DOI] [PubMed] [Google Scholar]
- 25.Wang B, et al. Prehabilitation program improves outcomes of patients undergoing elective liver resection. J Surg Res. 2020;251:119–125. doi: 10.1016/j.jss.2020.01.009. [DOI] [PubMed] [Google Scholar]