Abstract
Purpose of Review
The goal of this paper is to provide a comparative review of using phone (audio-only) or video for mental health treatments. Our review includes evidence of phone and video’s effectiveness in terms of reduced symptomology, retention, satisfaction, therapeutic alliance, and other outcomes of interest. This review also discusses how patients and providers’ experiences and attitudes differ between these two modalities. Finally, we present information on different usage rates of phone and video across patient populations and mental health provider types, and different implementation strategies.
Recent Findings
Treatments through phone and video are both able to reduce symptoms related to mental health conditions and have both been found to be non-inferior to in-person care. Both phone and video are more convenient to patients. Video offers important visual information that can be important to diagnosing mental health conditions. Phone, however, is more broadly accessible and may come with fewer technological issues.
Summary
In the context of mental health care, where non-verbal cues are tied to symptomology and diagnosing, and a strong relationship between patient and provider can enhance treatment, we encourage the use of video, especially for psychotherapeutic services. However, as phone is more accessible, we ultimately recommend an accommodating approach, one that flexibly makes use of both phone and video. Future studies on telehealth should focus on direct, head-to-head comparisons between phone and video and conduct more rigorous testing on whether clinical differences exist.
Keywords: Telehealth, Phone, Video, Mental health
Introduction
The ability to receive mental health care remotely—through either video or phone—has been available since 1960 [1, 2]. However, until recently, several barriers stymied widespread adoption of telehealth. Reimbursement policies either refused to cover telehealth visits or allowed reimbursement in only limited circumstances [3, 4]. Furthermore, many providers felt that telehealth offered lower quality care [5, 6].
All of this changed in early 2020. Stay-at-home orders during the COVID-19 pandemic that limit in-person care brought video and phone modalities to the forefront as patients and providers sought to continue care while limiting exposure. Emergency allowances for full reimbursement, whether using phone or video, now allowed providers to deliver care through either modality, and the use of video and phone to deliver mental health care reached new heights [7•, 8, 9].
But the use of phone and video did not increase in equivalent proportions. Across different health systems, the use of phone outpaced video. For example, within the Veterans Health Administration, from April through June 2020, of all mental health encounters, 63% occurred over phone, 21% over video, and 14% were in-person [10]. In a survey of Medicare beneficiaries’ telehealth usage in the Fall of 2020, 56% of visits were phone only, compared to 28% through video only, and 16% a combination of phone and video [11]. Given these trends, the question of whether to use phone or video to connect with patients has taken on a new salience.
The goal of this paper is to provide a comparative review of using phone or video for mental health treatments. The first section is organized by mental health conditions and focuses on the effectiveness of video compared to phone on a variety of outcomes (symptom reduction, retention, adherence, etc.). While an earlier meta-analysis computing weighted average effect sizes using results from previous studies attempted to understand whether phone or video resulted in greater reduction of symptoms across different mental health conditions [12•], we include a wider range of study designs and present findings on a greater range of effectiveness outcomes. This review also provides a more expansive survey of the telehealth landscape. The second section examines other issues relevant to the provision of video and phone, including patient and provider perspectives, implementation, and usage across different provider types, services, and patient groups.
Methods
We define telehealth as the use of phone (audio-only) or videoconferencing to deliver synchronized, real-time care to patients, and include articles on using either of these modalities for mental health treatments. Studies that brought patients into a clinic and then connected them to a remotely located provider [13–15] are also included and treated as video studies. Studies on internet-based treatments, mobile apps, email, or instant messaging were not included. Our review includes randomized control trials, pilot and uncontrolled studies, qualitative methods, retrospective chart reviews, survey analysis, and clinical demonstrations.
Literature was drawn from an ongoing record of recent publications on video-telehealth, managed by our co-authors’ (A.E and G.D.). We supplemented this with a dedicated search through the PubMed database for studies on phone for tele-mental health. We also conducted backwards search using citations of review articles [16, 17] and research reports [18]. We include studies published from 2002 to 2022 to ensure a comprehensive review of original studies and to ensure a balanced compilation of phone and video studies.
Effectiveness of Video vs Phone Across Different Mental Health Conditions
This section reviews findings on the use of phone or video to deliver treatment for anxiety and depression, PTSD, substance use, bipolar disorder and schizophrenia, eating disorders, obsessive compulsive and tic disorders, and smoking cessation. With the exception of bipolar disorder and schizophrenia, each section conducts a comparative review of phone and video treatments as they relate to effectiveness (symptom reduction). Table 1 provides a summary of the outcomes of interests across the different mental health conditions reviewed, and findings as they relate to phone or video.
Table 1.
Comparison of phone vs video on outcomes of interest across mental health disorders
| Effectiveness | Sustained effectiveness | Retention | Satisfaction | Cost-effectiveness | Medication adherence | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phone | Video | Phone | Video | Phone | Video | Phone | Video | Phone | Video | Phone | Video | |
| Anxiety and depression | Yes | Yes | Inconclusive | Yes | Yes | Yes | ||||||
| PTSD | Yes | Yes | Inconclusive | No | Inconclusive | |||||||
| Substance abuse disorders | Yes | Yes | Yes | Yes | ||||||||
| Smoking cessation | Yes | Yes | No | Yes | No | Yes | ||||||
| Bipolar and schizophrenia | Yes | Yes | ||||||||||
| Eating disorders | Yes | Yes | Yes | Yes | ||||||||
| Obsessive compulsive and tic | Yes | Yes | Yes | |||||||||
All modality outcomes are in comparison to in-person care and treatment as usual, or are from uncontrolled studies, with the exception of smoking cessation. Smoking cessation outcomes drawn from randomized control trials directly comparing phone and video modalities
Across almost all mental health conditions (with the exception of those in Smoking Cessation), randomized control trials compared telehealth treatment to in-person care or treatment as usual/standard care (i.e., no active treatment intervention).
Anxiety and Depression
Video telehealth may be particularly valuable for treating mood disorders, as patients who are diagnosed with a mood disorder are more likely to attend video appointments compared to patients with other diagnoses [19]. Both video and phone have been shown to be effective for reducing symptoms related to mood disorders. Phone therapy for depression is more effective than no-treatment or treatment-as-usual [20–23], and anxiety treatments delivered over phone are at least moderately effective for reducing symptoms relative to no treatment and treatment as usual [24]. An earlier review of controlled studies comparing video and in-person care showed that there is no difference in effectiveness between these two modalities for mood disorders [17].
Sustained effectiveness (effectiveness at n-month follow-up) of treatments for depressive symptoms through phone has produced mixed findings. In one study, patients completing phone treatment reported fewer depressive symptoms at 4- and 8-month follow-up, in comparison to a standard care control group [25]. However, in another study, there were no significant differences between phone and standard care at follow-up [22], and another study showed that phone treatments resulted in fewer sustained effects compared to in-person care [26]. Offering treatment through video may be better at sustaining effects: improvements in depression severity were sustained at two-month follow-up [27] in a study of home-bound older adults receiving video-based problem-solving therapy.
For patients with mood disorders, both video and phone are more likely to keep patients in care compared to in-person treatment. Receiving care for depression through phone [23, 26] or video [28] leads to higher completion rates and fewer dropouts compared to in person care: in one study, 73% of video patients completed the study, compared to 63% of their in-person counterparts [28]; in another, phone patients tended to participate in one more session compared to in-person patients [23].
Post-Traumatic Stress Disorder (PTSD)
Effectiveness of video-based treatment for PTSD are generally comparable to in-person care [16, 29, 30] and result in symptom improvement [13]. For phone-based treatments, patients receiving care through phone reported decreased PTSD symptoms in comparison to an assessment-only group [31].
Whether remote care can provide sustained effects for PTSD is inconclusive. A pre-post comparison of patients receiving care through video (with no modality comparison group), showed large effect size between PTSD symptoms at three-month follow-up [32]. However, another study that compared video and in-person care found that patients and providers disagreed on whether treatments had lasting effects: provider-assessments found continuing reduction in symptoms only for in person groups, but patient-reports on symptom reduction at follow-up were comparable across both video and in person [30]. No studies on the sustained effectiveness of phone-based PTSD treatment were found.
Patients receiving care through video for PTSD have been found to appreciate its convenience and confidentiality, and have found that it provides timely access to care [33]. However, in head-to-head comparison video and in-person care for PTSD, video patients were less satisfied than their phone counterparts [34], and treatments through video had higher rates of dropout compared to in-person care [13]. We did not find studies on patient satisfaction for PTSD treatments over phone.
Substance Use Disorders (SUD)
For SUD treatments, there are no significant differences in effectiveness when patients receive treatment over video or phone, compared to in-person care [35–38]. Patients receiving group therapy in person or by video had comparable rates of positive urine screening, similar duration of sustained abstinence from opioids, and similar amounts of time spent in intensive counseling [35, 36].
Patients also reported similar levels of satisfaction with receiving substance SUD treatment through video as those receiving in person care [35, 36]. Convenience and increased confidentiality bolstered satisfaction with video, while providers report that technology was easy to learn and did not interfere with therapy [35].
Patients who received care through video had higher attendance and retention compared to those in-person care [35–37]. Asking patients to choose whether they would prefer in-person or video appears to have notable influence on retention, as patients who were given this flexibility had much lower drop-out rates compared to those who were restricted to in-person care [37].
Smoking Cessation
Studies on remotely delivered treatments for smoking cessation stand out in that they include head-to-head comparisons of phone versus video modalities for treatment. No difference in effectiveness of treatment was found between phone and video arms, with rates of abstinence, cigarettes per day, and quit attempts similar across both video and phone [14].Compared to those using phone, participants using video were more likely to maintain smoking abstinence over a 6-month follow-up period [39••]. Taken all together, smoking cessation therapies can be effectively delivered using phone or video, but treatments over video may have more lasting effects.
While clinical outcomes appear comparable for phone or video, feasibility (assessed through patients’ ability to enroll, rates of access to video equipment, and retention rates) is not. Older patients, economically disadvantaged, or those living in regions with limited to no access to video-enabled equipment, have found treatment through video 30% less feasible than phone. However, those who were able to connect over video were more likely to complete the study compared to those who received treatment over phone, indicating that video may influence retention rate [39].
There are some significant limitations with one of the randomized trials reviewed here [14, 15]. Fewer sessions were offered for participants in the video arm compared to the phone arm. Additionally, video sessions were delivered at a clinic (the participant would receive treatment on video at a clinic from a remotely located provider); while the telephone sessions were received in participants’ homse. Differences in the number of sessions and the setting of treatment likely impacted results of these studies.
Bipolar Disorder and Schizophrenia
Compared to patients with other mental health conditions, patients with bipolar disorder and schizophrenia are more likely to use in-person services, rather than either phone or video [40••]. Remote delivery of care for patients with bipolar disease or schizophrenia has focused on two main outcomes: quality of life and medication adherence.
A study on treatment through phone involved brief sessions with a nurse or social worker that asked patients about topics of everyday life that the patient identified as important to their condition [41]. A study on treatment through video connected patients to psychiatrists, case managers, and nurses to provide an integrated package of treatment, practical and social support, and vocational rehabilitation [42]. Neither phone [41] nor video [42] treatments resulted in improved quality of life compared to treatment as usual and in person groups. Patients in the video study expressed a higher degree of satisfaction compared to in-person counterparts [42].
While neither phone nor video treatments resulted in improvements for quality of life for this condition, phone is extremely effective in supporting medication adherence for patients with severe mental illnesses. Patients receiving care through phone were much more likely to be adherent after 6 months compared to those receiving treatment as usual [43••].
Eating Disorders
Treatments delivered over phone or video for eating disorders have both been effective. A telephone-delivered treatment for eating disorders resulted in reduced symptoms of binge eating, emotional eating, and depression [44]. In two separate studies, video groups’ rates of abstinence from binging and purging were comparable to in-person groups [45, 46], even though video patients had a slower response to treatment [45]. Improvement in binge eating rates among those receiving care through video has been sustained at 3-month and 12-month follow-up [45]. Video is also more cost-effective with a lower cost per abstinent subject than in-person care [46]. Unfortunately, few studies on using telephone-delivered treatment for eating disorders exist, and studies on video-delivered care for eating disorders are more prominent.
Obsessive Compulsive and Tic Disorders (OCD)
Both phone and video are viable modalities for care for treating OCD and tic disorders. In two separate randomized control trials comparing phone and in-person delivery of OCD treatments, phone was clinically non-inferior to in-person treatment. Reduction in symptoms persisted 6 months after treatment among patients receiving treatment over phone [47, 48]. Video also appears to be a viable option for delivering treatments related to OCD and tic disorders. Studies using video treatments show improvement in symptoms [49, 50•], and comparable effectiveness to in-person care [51].
Those receiving OCD treatment through phone reported high satisfaction with their treatment compared to in-person patients [47]. Video, too, garnered patients’ favor with high ratings of acceptability compared to in-person [51]. Phone has also proven to be a cost-effective means for delivering treatment to patients with OCD. Especially for those who may be less willing to pay for treatment, using phone to receive treatment was found to be even more cost-effective than in-person care, likely due to the reduction in expenses related to travel and time [52]. Unfortunately, no studies on treating these disorders through video provided information on cost-effectiveness.
Using video to conduct exposure treatments has expanded treatment possibilities in ways that neither phone nor in person modalities can: providers were able to view patients’ home environments to better understand patients’ symptoms and could teach patients how to do exposure treatment in their home environment [50]. Because of the unique aspects of treatments related to OCD and tic disorders, video may be preferable to phone, as it allows providers to collect collateral information from patients and tailor exposure protocols to patients’ homes. This is one clear advantage of video that is not available through phone (or in-person).
Summary
Across a range of mental health conditions, with the exception of bipolar and schizophrenia, both phone and video appear as effective as in-person care for reducing symptoms. However, we cannot definitively determine whether video or phone is more effective. An earlier meta-analysis similarly concluded that phone and video are as effective as in-person care [12], but found no strong differences in effect sizes when comparing phone to video. And in one randomized control trial that compared all three modalities for general mental health treatment [53••], the authors note that “similarities among the three treatment groups… came through more strongly than differences” [53]. Ultimately, more studies directly comparing phone and video are needed.
There is also some evidence that receiving care through video may be tied to sustained effectiveness, as studies on using video to treat mood disorders and eating disorders all maintained a reduction in symptoms, but no direct comparisons to phone were made. Direct comparisons conducted for smoking cessation treatments did find that video demonstrated lasting effects compared to phone.
Finally, there is limited evidence that, compared to in-person care, both video and phone increase retention. The link between video and retention, however, does not appear to hold for PTSD treatments. Substance use patients appear to stay more engaged over video (although no parallel phone data exists). Treatments for smoking cessation show that video patients were more likely than phone patients to stay engaged.
Video vs Phone: Implementation and Experience
The success (or failure) of telehealth, whether by phone or video, is deeply intertwined with interpersonal, organizational, administrative, and social-structural circumstances. In this section, we discuss issues that cut across mental health disorders and are particularly salient to remote care, with a continued focus on how video and phone compare across different topics. Table 2 highlights key findings and contributions from studies in this and the previous section.
Table 2.
Key literature and contributions
| First author Year |
Telehealth modality | Comparator | Topic | Study design | |
|---|---|---|---|---|---|
|
Karimi et al. 2022 [83••] |
Video vs phone | Access | Survey | Compared to phone, rates of video use are lower among under-served populations, including those with lower income, without a high school degree, Black, Latino, and Asian respondents, and those without insurance | |
|
Connolly 2021 [40••] |
Video, phone | In-person | Services and treatment | Retrospective comparative analysis | Psychiatrists and other medical providers are less likely to use video. Psychologists are more likely to use video |
|
Day and Schneider 2002 [53••] |
Video, phone | In-person | Effectiveness | Controlled comparison | No significant differences in effectiveness of treatment across phone, video, or in-person. But participation is higher among video and phone users |
|
Kim et al. 2018 [39••] |
Video vs phone | Effectiveness | Randomized control trial | Video visits were less feasible than phone for those in 50 s and 60 s, lower SES, women in regions without access to video equipment. However, when able to use video, patients were more likely to complete the study and were more likely to experience sustained effects | |
|
Schifeling et al. 2020 [75••] |
Video vs phone | Services and treatments, access | Retrospective comparative analysis | Video visits are longer than phone; video visits result in more diagnoses than phone; cognitive, visual, and hearing impairments of older patients did not result in less video visits | |
|
Payán et al. 2022 [69••] |
Video vs phone | Preferences and experiences, implementation | Qualitative, interviews | Providers say use of phone or video will depend on federal and state reimbursement policies | |
|
Molfenter et al. 2021 [65••] |
Video vs phone | Services and treatment | Survey | Phone is more commonly used for case management | |
|
Schulze et al. 2019 [43••] |
Phone | Usual care | Effectiveness, services and treatment | Randomized control trial | Phone offers low threshold support sufficient for medication management |
|
Fletcher et al. 2021 [50•] |
Video | None | Effectiveness | Mixed methods | Video offers unique benefits including ability for providers to access collateral information and provide exposure protocols in patients’ homes |
|
Slightam et al. 2020 [68••] |
Video | None | Preferences and experience | Mixed methods | Many patients feel video is similar to in person care; technological difficulties are a common challenge for video |
|
Rushton et al. 2020 [60••] |
Phone | None | Rapport and alliance, implementation | Qualitative, interviews | Patients feel phone is acceptable and benefit from treatment through phone. Communication challenges—such as lack of visual feedback—can be overcome through provider training and skill, as well as increased familiarity between patient and providers |
|
Lindsay et al. 2019 [72••] |
Video | None | Implementation | Clinical demonstration | Flexibility, engagement with leadership, attention to regional culture, and a telehealth “champion” are key strategies needed to support implementation of video telehealth within clinics |
Rapport and Alliance
Patient perception of therapist empathy and helpfulness was equivalent between telephone and in-person groups [23, 54, 55]. Similarly, patient satisfaction and ratings on the quality of relationships were comparable for video and in-person care [56–58]. In the few randomized control trials comparing phone and video directly, both phone and video were equally acceptable to patients [39]; and there were no differences in working alliance [15]. One qualitative study with patients who used video telehealth found a majority of patients felt visual information afforded through video was very important to their care experience, and that non-verbal communication was essential to building relationship with their provider [59•]. However, other patients receiving care through phone felt that the lack of visual feedback could be overcome through provider training and skill, as well as increased familiarity over time [60••].
Insofar as rapport and its relationship to telehealth, perhaps a more interesting comparison is not between modalities, but rather between patient and providers. Even when video and in-person patients show no significant difference in therapeutic alliance, providers themselves felt a loss in rapport and reported lower satisfaction and therapeutic alliance with their video patients [5, 6, 61•, 62].
Preferences and Experiences
Prior to the recent COVID-19 pandemic, providers had markedly negative preconceptions about phone use [63]. Once more providers were forced to use phone; however, they reported more positive experiences [64]. Some providers prefer video over phone [65••], while others are equally likely to recommend phone or video, finding both equally effective [66]. And others still consider in-person the gold-standard, with remote technologies a “necessary evil” required to confront the national workforce shortage of in-person providers and expand access [67••].
For patients, both video and phone share a key advantage: convenience. Patients consistently discuss the convenience of telehealth—being able to avoid time in traffic, parking, and scheduling difficulties—as one of the greatest advantages [33, 60, 68]. For patients who struggle with anxiety or have physical limitations, being able to connect with providers over phone or video, rather than having to encounter physically or emotionally stressful clinical spaces, is also an important benefit of remote care [68••].
Among the 31 patients interviewed by co-authors (A.H. and P.C.) during 2020–2021, 52% (16/31) said they preferred using a video platform, 17% (5/31) preferred phone, and 29% preferred in-person. Those who preferred video often mentioned how important it was to have “eyes-on,” being able to see and be seen by their providers:
To me that’s important because your facial expressions and the way you’re presenting yourself, they’re very keen in seeing that there is a problem with me. They notice a change in me and ask why that’s happening. So that helps because you’re talking to someone directly, you’re not just talking to someone on the phone. (White, Male, 69 Years Old)
Frustrations with technological issues, which are often avoided during phone sessions, continue to be a well-documented problem for patients and providers using video telehealth. Providers have often reported having to spend limited appointment time on trouble shooting rather than on the therapeutic content of their sessions. Phone has often been used after failed attempts to use video or when patients were not equipped to use video devices [45, 59•, 68••, 69••].
Implementation Factors
At the clinic level, remote delivery of care requires a “telehealth infrastructure”: coordination, provider training, equipment, modifications in scheduling systems and flow—in order to support both initial adoption of telehealth and its sustained usage [70, 71]. Implementation experts for video telehealth encourage flexibility, engagement with leadership, attention to regional culture, and the importance of a facility telehealth “champion” to provide additional support and coordination, particularly to encourage adoption of video telehealth [70, 72••, 73]. Successfully using phone to deliver mental health care also requires additional training on telephone and communication skills for providers [
Services and Treatments
The use of phone and video is also linked to provider and service type. Psychiatrists are more likely to use phone compared to psychologists, likely due to the type of treatment and nature of services that psychiatrists provide [40]. Compared to video, phone is more commonly used for case management [65] and has been deemed acceptable for follow-up assessments [66]. Phone also provides sufficient and “low threshold” support for medication adherence [43].
Providers appear to use video or phone in equal proportion for diagnostic assessment [65]. Video is considered acceptable by providers for prescribing medication—although in person is preferred. Video visits tend to be longer compared to phone and come with more visit diagnoses [75••]. For diagnosing and medication initiation, prior studies, current practice, and clinical rigor appear to point toward video as the better option due to the complex information gathering involved in these early stages of care.
Access
Advocates of telehealth have shown that both phone and video can be used to reach historically underserved populations, opening a pathway to treatment with specialists and interventions that may not be available at local levels [24, 27, 76–78]. However, as telehealth has become more widespread, social-structural conditions that present as patient-level factors have reproduced inequities in terms of what patient populations are using which modality.
Race-ethnic minorities (typically Black and Hispanic), those using English as a second-language, those with low-broadband access (often those in rural areas), lower SES, and older patients all have higher phone usage compared to video [(75••, 79–83••, 84]*. Salient barriers to video that patients in these groups typically face include: limited access to video-enabled devices, more tech issues (related to low broadband), and limited digital literacy. Given these barriers, providing services through phone increases access as phone represents more readily available equipment, lower connection costs, and fewer technological challenges compared to video (74, 85).
Compared to in-person care, video telehealth does increase access for patients, reducing travel costs, allowing more flexible scheduling, and giving those with mobility issues a way to connect from home [86]. But when compared to phone, video requires greater resources on the part of patients. Such resources include purchasing power for a video-enabled device and broadband service for connectivity, as well as available social support to assist with setup and trouble shooting [69]. The visual summary below compares the benefits of video, phone, and in-person care Fig. 1.
Fig. 1.
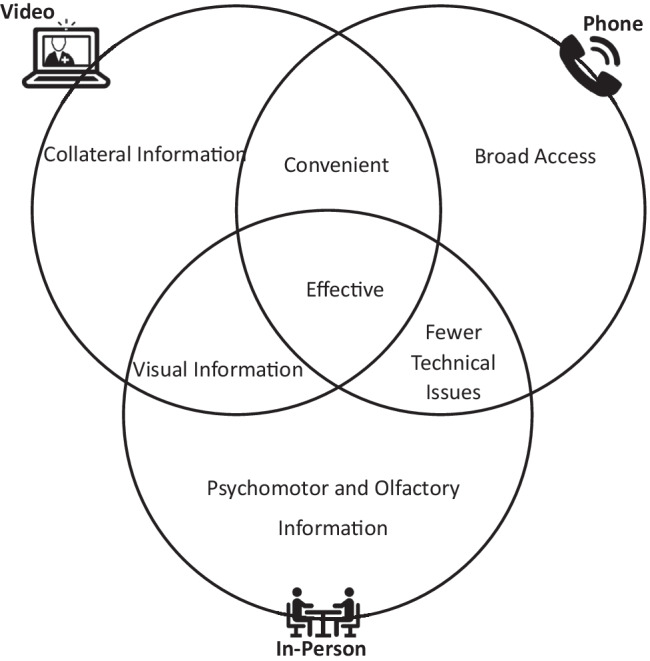
Video vs Phone vs In-Person: Benefits Across Modalities
While phone, video, and in-person care are all effective modes of care, phone and video are more convenient to patients. Video offers important visual information and can give providers a unique window into patients’ homes, as appropriate. Phone, however, is more broadly accessible and may come with fewer technological issues.
Conclusion
In the context of mental health care, where nonverbal cues can be tied to symptomology and diagnosing, and a strong relationship between patient and provider is interwoven with effective treatment, we encourage the use of video, especially for psychotherapeutic services.
Even so, the relationship between mental health outcomes and modality may very well be moot if patients’ ability to access and afford devices and broadband services supersede clinical considerations. Due to the greater availability of phone for those who are so often at the margins of receiving mental health care, we ultimately recommend an accommodating approach above all, one that flexibly makes use of both phone and video.
In circumstances where a patient may have the option to use either phone or video, and prefers phone, we advise providers to first and foremost consider the clinical safety of the patient. Rather than patient preference, factors such as the type of service being offered (psychotherapy, medication management, case management), the specific mental health issues and medical circumstances of the patient (including practice standards associated with prescription of certain medications, such as opioids or benzodiazepines), and other state-specific standards of practice, should all inform a provider’s decision on whether to use phone or video. If a provider determines that video modality best supports their patient’s safety during treatment, a collaborative discussion with the patient to identify reasons behind their reluctance and to explain the provider’s rationale for using video is warranted. In cases where a patient continues to refuse the use of video, providers should document that the patient was informed of the risks and limitations of phone, and why phone was used for the encounter.
Our review provides little consensus on whether phone or video is better for mental health care. We attribute this to a substantive limitation: among the articles we reviewed, only 21 compared video and phone, and only 4 conducted randomized control trials for a head-to-head, controlled comparison between video and phone. All other randomized control trials compared either video or phone to in-person care or treatment as usual (limited to no active intervention). Future studies on telehealth studies should focus on direct comparisons between modalities. We are optimistic that additional research will provide additional impetus to increase access to digital health solutions across broader swathes of society.
Footnotes
This article is part of the Topical Collection on Psychiatry in the Digital Age
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Bashshur R, Shannon GW. History of telemedicine: evolution, context, and transformation: Mary Ann Liebert New Rochelle, NY. 2009.
- 2.Shore J. The evolution and history of telepsychiatry and its impact on psychiatric care: current implications for psychiatrists and psychiatric organizations. Int Rev Psychiatry. 2015;27(6):469–475. doi: 10.3109/09540261.2015.1072086. [DOI] [PubMed] [Google Scholar]
- 3.Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 4.Daschle T, Dorsey ER. The return of the house call. Am Coll Phys. 2015:587–8. [DOI] [PubMed]
- 5.Ertelt TW, Crosby RD, Marino JM, Mitchell JE, Lancaster K, Crow SJ. Therapeutic factors affecting the cognitive behavioral treatment of bulimia nervosa via telemedicine versus face-to-face delivery. Int J Eat Disord. 2011;44(8):687–691. doi: 10.1002/eat.20874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simpson S, Reid C. Telepsychology in Australia: 20/20 vision. Aust J Rural Health. 2014;22(6):306–309. doi: 10.1111/ajr.12103. [DOI] [PubMed] [Google Scholar]
- 7.• Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. New England J Med. 2020;382(18):1679–81. Evidence on the rise of telehealth during the COVID-19 pandemic, published in a major journal. [DOI] [PubMed]
- 8.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States: study examines variation in total US outpatient visits and telemedicine use across patient demographics, specialties, and conditions during the COVID-19 pandemic. Health Aff. 2021;40(2):349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.VHA Support Service Center Capital Assets. (VSSC). [VA Intranet]. Department of Veterans Affairs. Heathc Inform Res 2010;16(1):65–66. Accessed 25 Apr 2022.
- 11.Koma W, Cubanski J, Neuman T. Medicare and telehealth: coverage and use during the COVID-19 pandemic and options for the future. Kaiser Family Foundation. 2021.
- 12.• McClellan MJ, Osbaldiston R, Wu R, Yeager R, Monroe AD, McQueen T, et al. The effectiveness of telepsychology with veterans: A meta-analysis of services delivered by videoconference and phone. Psychol Serv. 2021. A review article that compares effectiveness of video versus phone to by calculating weighted average effect sizes. No signficant difference found through this method. [DOI] [PubMed]
- 13.Morland LA, Mackintosh MA, Glassman LH, Wells SY, Thorp SR, Rauch SAM, et al. Home-based delivery of variable length prolonged exposure therapy: A comparison of clinical efficacy between service modalities. Depress Anxiety. 2020;37(4):346–355. doi: 10.1002/da.22979. [DOI] [PubMed] [Google Scholar]
- 14.Mussulman L, Ellerbeck EF, Cupertino AP, Preacher KJ, Spaulding R, Catley D, et al. Design and participant characteristics of a randomized-controlled trial of telemedicine for smoking cessation among rural smokers. Contemp Clin Trials. 2014;38(2):173–181. doi: 10.1016/j.cct.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liebmann EP, Preacher KJ, Richter KP, Cupertino AP, Catley D. Identifying pathways to quitting smoking via telemedicine-delivered care. Health Psychol. 2019;38(7):638. doi: 10.1037/hea0000740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olthuis JV, Wozney L, Asmundson GJ, Cramm H, Lingley-Pottie P, McGrath PJ. Distance-delivered interventions for PTSD: A systematic review and meta-analysis. J Anxiety Disord. 2016;44:9–26. doi: 10.1016/j.janxdis.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Berryhill MB, Culmer N, Williams N, Halli-Tierney A, Betancourt A, Roberts H, et al. Videoconferencing psychotherapy and depression: a systematic review. Telemedicine and e-Health. 2019;25(6):435–446. doi: 10.1089/tmj.2018.0058. [DOI] [PubMed] [Google Scholar]
- 18.Uscher-Pines LS, L. Rethinking the Impact of Audio-Only Visits on Health Equity. The RAND Blog. 2021.
- 19.Valentine LM, Donofry SD, Sexton MB. Demographic and psychiatric predictors of engagement in psychotherapy services conducted via clinical video telehealth. J Telemed Telecare. 2020;26(1–2):113–118. doi: 10.1177/1357633X18801713. [DOI] [PubMed] [Google Scholar]
- 20.Corruble E, Swartz HA, Bottai T, Vaiva G, Bayle F, Llorca P-M, et al. Telephone-administered psychotherapy in combination with antidepressant medication for the acute treatment of major depressive disorder. J Affect Disord. 2016;190:6–11. doi: 10.1016/j.jad.2015.07.052. [DOI] [PubMed] [Google Scholar]
- 21.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292(8):935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 22.Ngai F-W, Wong P W-C, Leung K-Y, Chai P-H, Chung K-F. The effect of telephone-based cognitive-behavioral therapy on postnatal depression: a randomized controlled trial. Psychother Psychosomat. 2015;84(5):294–303. [DOI] [PubMed]
- 23.Fann JR, Bombardier CH, Vannoy S, Dyer J, Ludman E, Dikmen S, et al. Telephone and in-person cognitive behavioral therapy for major depression after traumatic brain injury: a randomized controlled trial. J Neurotrauma. 2015;32(1):45–57. doi: 10.1089/neu.2014.3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coughtrey AE, Pistrang N. The effectiveness of telephone-delivered psychological therapies for depression and anxiety: a systematic review. J Telemed Telecare. 2018;24(2):65–74. doi: 10.1177/1357633X16686547. [DOI] [PubMed] [Google Scholar]
- 25.Heckman TG, Markowitz JC, Heckman BD, Woldu H, Anderson T, Lovejoy TI, et al. A randomized clinical trial showing persisting reductions in depressive symptoms in HIV-infected rural adults following brief telephone-administered interpersonal psychotherapy. Ann Behav Med. 2018;52(4):299–308. doi: 10.1093/abm/kax015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, et al. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA. 2012;307(21):2278–2285. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choi NG, Marti CN, Bruce ML, Hegel MT, Wilson NL, Kunik ME. Six-month postintervention depression and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income homebound older adults. Depress Anxiety. 2014;31(8):653–661. doi: 10.1002/da.22242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zimmerman M, Terrill D, D’Avanzato C, Tirpak JW. Telehealth treatment of patients in an intensive acute care psychiatric setting during the COVID-19 pandemic: comparative safety and effectiveness to in-person treatment. J Clin Psychiatry. 2021;82(2):28542. doi: 10.4088/JCP.20m13815. [DOI] [PubMed] [Google Scholar]
- 29.Acierno R, Knapp R, Tuerk P, Gilmore AK, Lejuez C, Ruggiero K, et al. A non-inferiority trial of Prolonged Exposure for posttraumatic stress disorder: In person versus home-based telehealth. Behav Res Ther. 2017;89:57–65. doi: 10.1016/j.brat.2016.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu L, Thorp SR, Moreno L, Wells SY, Glassman LH, Busch AC, et al. Videoconferencing psychotherapy for veterans with PTSD: Results from a randomized controlled non-inferiority trial. J Telemed Telecare. 2020;26(9):507–519. doi: 10.1177/1357633X19853947. [DOI] [PubMed] [Google Scholar]
- 31.DuHamel KN, Mosher CE, Winkel G, Labay LE, Rini C, Meschian YM, et al. Randomized clinical trial of telephone-administered cognitive-behavioral therapy to reduce post-traumatic stress disorder and distress symptoms after hematopoietic stem-cell transplantation. J Clin Oncol. 2010;28(23):3754. doi: 10.1200/JCO.2009.26.8722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murphy D, Turgoose D. Evaluating an Internet-based video cognitive processing therapy intervention for veterans with PTSD: A pilot study. J Telemed Telecare. 2020;26(9):552–559. doi: 10.1177/1357633X19850393. [DOI] [PubMed] [Google Scholar]
- 33.Whealin JM, King L, Shore P, Spira JL. Diverse veterans' pre- and post-intervention perceptions of home telemental health for posttraumatic stress disorder delivered via tablet. Int J Psychiatry Med. 2017;52(1):3–20. doi: 10.1177/0091217417703291. [DOI] [PubMed] [Google Scholar]
- 34.White CN, Kauffman BY, Acierno R. Factors contributing to veterans’ satisfaction with PTSD treatment delivered in person compared to telehealth. J Telemed Telec. 2021:1357633X20987704. [DOI] [PubMed]
- 35.King VL, Stoller KB, Kidorf M, Kindbom K, Hursh S, Brady T, et al. Assessing the effectiveness of an Internet-based videoconferencing platform for delivering intensified substance abuse counseling. J Subst Abuse Treat. 2009;36(3):331–338. doi: 10.1016/j.jsat.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 36.King VL, Brooner RK, Peirce JM, Kolodner K, Kidorf MS. A randomized trial of Web-based videoconferencing for substance abuse counseling. J Subst Abuse Treat. 2014;46(1):36–42. doi: 10.1016/j.jsat.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tarp K, Bojesen AB, Mejldal A, Nielsen AS. Effectiveness of Optional Videoconferencing-Based Treatment of Alcohol Use Disorders: Randomized Controlled Trial. JMIR Ment Health. 2017;4(3):e38. doi: 10.2196/mental.6713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harder VS, Musau AM, Musyimi CW, Ndetei DM, Mutiso VN. A randomized clinical trial of mobile phone motivational interviewing for alcohol use problems in Kenya. Addiction. 2020;115(6):1050–1060. doi: 10.1111/add.14903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.•• Kim SS, Darwish S, Lee SA, Sprague C, DeMarco RF. A randomized controlled pilot trial of a smoking cessation intervention for US women living with HIV: telephone-based video call vs voice call. Int J Womens Health. 2018;10:545–55. A randomized, control trial comparing video and phone on multiple outcome measures. While no difference in effectiveness were found immediately after treatment, shows evidence that video participants had more sustained effects compared to phone. [DOI] [PMC free article] [PubMed]
- 40.•• Connolly SL, Stolzmann KL, Heyworth L, Sullivan JL, Shimada SL, Weaver KR, et al. Patient and provider predictors of telemental health use prior to and during the COVID-19 pandemic within the Department of Veterans Affairs. Am Psychol. 2021. Comprehensive study that discussed predictors for phone or video use for patients and providers. Shows that psychiatrists and other medical professionals are less likely to use video. Psychologists are more likely to use video. Patients with schizophrenia and biopolar disorders are more likely to use in-person care over phone or video.
- 41.Stentzel U, van den Berg N, Moon K, Schulze LN, Schulte J, Langosch JM, et al. Telemedical care and quality of life in patients with schizophrenia and bipolar disorder: results of a randomized controlled trial. BMC Psychiatry. 2021;21(1):1–14. doi: 10.1186/s12888-021-03318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hulsbosch AM, Nugter MA, Tamis P, Kroon H. Videoconferencing in a mental health service in the Netherlands: a randomized controlled trial on patient satisfaction and clinical outcomes for outpatients with severe mental illness. J Telemed Telecare. 2017;23(5):513–520. doi: 10.1177/1357633X16650096. [DOI] [PubMed] [Google Scholar]
- 43.•• Schulze LN, Stentzel U, Leipert J, Schulte J, Langosch J, Freyberger HJ, et al. Improving medication adherence with telemedicine for adults with severe mental illness. Psychiat Serv. 2019;70(3):225–8. Shows that phone offers low threshold of suppor sufficient for medication management. [DOI] [PubMed]
- 44.Sockalingam S, Cassin SE, Wnuk S, Du C, Jackson T, Hawa R, et al. A pilot study on telephone cognitive behavioral therapy for patients six-months post-bariatric surgery. Obes Surg. 2017;27(3):670–675. doi: 10.1007/s11695-016-2322-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mitchell JE, Crosby RD, Wonderlich SA, Crow S, Lancaster K, Simonich H, et al. A randomized trial comparing the efficacy of cognitive-behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav Res Ther. 2008;46(5):581–592. doi: 10.1016/j.brat.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crow SJ, Mitchell JE, Crosby RD, Swanson SA, Wonderlich S, Lancanster K. The cost effectiveness of cognitive behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav Res Ther. 2009;47(6):451–453. doi: 10.1016/j.brat.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Turner CM, Mataix-Cols D, Lovell K, Krebs G, Lang K, Byford S, et al. Telephone cognitive-behavioral therapy for adolescents with obsessive-compulsive disorder: a randomized controlled non-inferiority trial. J Am Acad Child Adolesc Psychiat. 2014;53(12):1298–307. e2. [DOI] [PMC free article] [PubMed]
- 48.Nair A, Turner C, Heyman I, Mataix-Cols D, Lovell K, Krebs G, et al. Moderators and predictors of outcomes in telephone delivered compared to face-to-face cognitive behaviour therapy for paediatric obsessive-compulsive disorder: preliminary evidence from a non-inferiority RCT. Cogn Behav Ther. 2019;48(5):353–368. doi: 10.1080/16506073.2018.1513555. [DOI] [PubMed] [Google Scholar]
- 49.Storch EA, Caporino NE, Morgan JR, Lewin AB, Rojas A, Brauer L, et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011;189(3):407–412. doi: 10.1016/j.psychres.2011.05.047. [DOI] [PubMed] [Google Scholar]
- 50.• Fletcher TL, Amspoker AB, Wassef M, Hogan JB, Helm A, Jackson C, et al. Increasing access to care for trauma-exposed rural veterans: A mixed methods outcome evaluation of a web-based skills training program with telehealth-delivered coaching. J Rural Health. 2021. Evidence of a unique benefit of video: providers can access collateral information. Also, providers can provide exposure protocols that patientc can practice in their own home environments. [DOI] [PubMed]
- 51.Himle MB, Freitag M, Walther M, Franklin SA, Ely L, Woods DW. A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behav Res Ther. 2012;50(9):565–570. doi: 10.1016/j.brat.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 52.Tie H, Krebs G, Lang K, Shearer J, Turner C, Mataix-Cols D, et al. Cost-effectiveness analysis of telephone cognitive-behaviour therapy for adolescents with obsessive-compulsive disorder. BJPsych Open. 2019;5(1):e7. doi: 10.1192/bjo.2018.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.•• Day SX, Schneider PL. Psychotherapy using distance technology: A comparison of face-to-face, video, and audio treatment. J Counsel Psychol. 2002;49(4):499. The only randomized trial that directly compares phone, video, and in-person modalities for general mental health treatments. While no significant differences in effectiveness were found, participation is higher among video and phone users.
- 54.Dobkin RD, Mann SL, Gara MA, Interian A, Rodriguez KM, Menza M. Telephone-based cognitive behavioral therapy for depression in Parkinson disease: a randomized controlled trial. Neurology. 2020;94(16):e1764–e1773. doi: 10.1212/WNL.0000000000009292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stiles-Shields C, Kwasny MJ, Cai X, Mohr DC. Therapeutic alliance in face-to-face and telephone-administered cognitive behavioral therapy. J Consult Clin Psychol. 2014;82(2):349–354. doi: 10.1037/a0035554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Egede LE, Acierno R, Knapp RG, Walker RJ, Payne EH, Frueh BC. Psychotherapy for depression in older veterans via telemedicine: effect on quality of life, satisfaction, treatment credibility, and service delivery perception. J Clin Psychiatry. 2016;77(12):16304. doi: 10.4088/JCP.16m10951. [DOI] [PubMed] [Google Scholar]
- 57.Luxton DD, Pruitt LD, Wagner A, Smolenski DJ, Jenkins-Guarnieri MA, Gahm G. Home-based telebehavioral health for US military personnel and veterans with depression: A randomized controlled trial. J Consult Clin Psychol. 2016;84(11):923. doi: 10.1037/ccp0000135. [DOI] [PubMed] [Google Scholar]
- 58.Watts S, Marchand A, Bouchard S, Gosselin P, Langlois F, Belleville G, et al. Telepsychotherapy for generalized anxiety disorder: Impact on the working alliance. J Psychother Integr. 2020;30(2):208. doi: 10.1037/int0000223. [DOI] [Google Scholar]
- 59.• Chen PV, Helm A, Fletcher T, Wassef M, Hogan J, Amspoker A, et al. Seeing the value of video: A qualitative study on patient preference for using video in a veteran affairs telemental health program evaluation. telemed reports. 2021;2(1):156–62. Discusses patient perspective that being able to see a provider through video is important to building and maintaing a strong relationship with their provider. [DOI] [PMC free article] [PubMed]
- 60.•• Rushton K, Ardern K, Hopkin E, Welsh C, Gellatly J, Faija C, et al. ‘I didn’t know what to expect’: Exploring patient perspectives to identify targets for change to improve telephone-delivered psychological interventions. BMC Psychiatry. 2020;20(1):1–13. One of the few articles that provides and in-depth exploration of patients experience with the using phone for mental health care, showing evidence that building rapport is possible through phone with appropriate provider training. [DOI] [PMC free article] [PubMed]
- 61.• Connolly SL, Miller CJ, Lindsay JA, Bauer MS. A systematic review of providers’ attitudes toward telemental health via video conferencing. Clin Psychol: Sci Prac. 2020;27(2):e12311. A study that shows that even while patients are satisfied with receiving mental health treatment through video, providers tend to have lower satisfaction. [DOI] [PMC free article] [PubMed]
- 62.Pierce BS, Perrin PB, McDonald SD. Pre-COVID-19 deterrents to practicing with videoconferencing telepsychology among psychologists who didn't. Psycholog Serv. 2020. [DOI] [PubMed]
- 63.Faija CL, Connell J, Welsh C, Ardern K, Hopkin E, Gellatly J, et al. What influences practitioners’ readiness to deliver psychological interventions by telephone? A qualitative study of behaviour change using the Theoretical Domains Framework. BMC Psychiatry. 2020;20(1):1–16. doi: 10.1186/s12888-020-02761-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Korecka N, Rabenstein R, Pieh C, Stippl P, Barke A, Doering B, et al. Psychotherapy by telephone or internet in Austria and Germany Which CBT psychotherapists rate it more comparable to face-to-face psychotherapy in personal contact and have more positive actual experiences compared to previous expectations? Int J Environ Res Public Health. 2020;17(21):7756. doi: 10.3390/ijerph17217756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.•• Molfenter T, Heitkamp T, Murphy AA, Tapscott S, Behlman S, Cody OJ. Use of telehealth in mental health (MH) services during and after COVID-19. Commun Ment Health J. 2021;57(7):1244–51. Phone is commonly used for case management. [DOI] [PMC free article] [PubMed]
- 66.Budhwani S, Fujioka JK, Chu C, Baranek H, Pus L, Wasserman L, et al. Delivering mental health care virtually during the COVID-19 Pandemic: qualitative evaluation of provider experiences in a scaled context. JMIR Formative Research. 2021;5(9):e30280. doi: 10.2196/30280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.• Uscher-Pines L, Raja P, Qureshi N, Huskamp HA, Busch AB, Mehrotra A. Use of tele–mental health in conjunction with in-person care: a qualitative exploration of implementation models. Psychiat Serv. 2020;71(5):419–26. A facility level analysis of the use of telehealth that offers insight on provider perspective that telehealth -- either phone or video-- is a "necessary evil" or Plan B. [DOI] [PMC free article] [PubMed]
- 68.•• Slightam C, Gregory AJ, Hu J, Jacobs J, Gurmessa T, Kimerling R, et al. Patient perceptions of video visits using veterans affairs telehealth tablets: Survey study. J Med Internet Res. 2020;22(4):e15682. Evidence of patient perspective that video is similar to in-person care and also highlights technilogical issues associated with video. [DOI] [PMC free article] [PubMed]
- 69.•• Payán DD, Frehn JL, Garcia L, Tierney AA, Rodriguez HP. Telemedicine implementation and use in community health centers during COVID-19: Clinic personnel and patient perspectives. SSM-Qualitat Res Health. 2022;2:100054. Evidence that providers decisions on whether to use phone or video in the future will largely depend on reimbursement policies. [DOI] [PMC free article] [PubMed]
- 70.Glynn LH, Chen JA, Dawson TC, Gelman H, Zeliadt SB. Bringing chronic-pain care to rural veterans: A telehealth pilot program description. Psychol Serv. 2021;18(3):310–318. doi: 10.1037/ser0000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bennett SD, Au C, Byford S, Chorpita B, Coughtrey AE, Cross JH, et al. Feasibility of telephone-delivered therapy for common mental health difficulties embedded in pediatric epilepsy clinics. Epilepsy Behav. 2021;116:107743. doi: 10.1016/j.yebeh.2020.107743. [DOI] [PubMed] [Google Scholar]
- 72.•• Lindsay JA, Day SC, Amspoker AB, Fletcher TL, Hogan J, Day G, et al. Personalized implementation of video telehealth. Psychiat Clin. 2019;42(4):563–74. Shows that flexibility, engagement with leadership, attention to regional culture, and a telehealth "champion" are key strategies needed to support implementation of video telehealth within clinics. [DOI] [PubMed]
- 73.Day SC, Day G, Keller M, Touchett H, Amspoker AB, Martin L, et al. Personalized implementation of video telehealth for rural veterans (PIVOT-R). Mhealth. 2021;7. [DOI] [PMC free article] [PubMed]
- 74.Brenes GA, Ingram CW, Danhauer SC. Benefits and challenges of conducting psychotherapy by telephone. Prof Psychol Res Pract. 2011;42(6):543. doi: 10.1037/a0026135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.•• Schifeling CH, Shanbhag P, Johnson A, Atwater RC, Koljack C, Parnes BL, et al. Disparities in video and telephone visits among older adults during the COVID-19 pandemic: Cross-sectional analysis. JMIR Aging. 2020;3(2):e23176. Evidence that video visits tend to be londer compared to phone and result in more diagonses. [DOI] [PMC free article] [PubMed]
- 76.Patel SY, Huskamp HA, Busch AB, Mehrotra A. Telemental health and US rural–urban differences in specialty mental health use, 2010–2017. Am J Public Health. 2020;110(9):1308–1314. doi: 10.2105/AJPH.2020.305657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Choi NG, Hegel MT, Marti N, Marinucci ML, Sirrianni L, Bruce ML. Telehealth problem-solving therapy for depressed low-income homebound older adults. Am J Geriatr Psychiatry. 2014;22(3):263–271. doi: 10.1016/j.jagp.2013.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Egede LE, Acierno R, Knapp RG, Lejuez C, Hernandez-Tejada M, Payne EH, et al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. The Lancet Psychiatry. 2015;2(8):693–701. doi: 10.1016/S2215-0366(15)00122-4. [DOI] [PubMed] [Google Scholar]
- 79.Jaklevic MC. Telephone visits surge during the pandemic, but will they last? JAMA. 2020;324(16):1593–1595. doi: 10.1001/jama.2020.17201. [DOI] [PubMed] [Google Scholar]
- 80.Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(1). [DOI] [PMC free article] [PubMed]
- 81.Chen J, Li KY, Andino J, Hill CE, Ng S, Steppe E, et al. Predictors of Audio-Only Versus Video Telehealth Visits During the COVID-19 Pandemic. J Gen Int Med. 2021:1–7. [DOI] [PMC free article] [PubMed]
- 82.Drake C, Lian T, Cameron B, Medynskaya K, Bosworth HB, Shah K. Understanding telemedicine's “new normal”: variations in telemedicine use by specialty line and patient demographics. Telemedicine and e-Health. 2022;28(1):51–59. doi: 10.1089/tmj.2021.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.•• Karimi M, Lee EC, Couture SJ, Gonzales A, Grigorescu V, Smith SR, De Lew N, Sommers BD. National Survey Trends in Telehealth Use in 2021: Disparities in Utilization and Audio vs. Video Services. Off Assist Sec Plann Evaluat. 2022. A nationwide survey on telephone versus phone usage that shows rates of video use are lower among under-served populations, including those with lower income, without a high school degree, Black, Latino, and Asian respondents, and those without insurance.
- 84.Uscher-Pines L, Jones M, Sousa J, Predmore Z, Ober A. The doctor will call me maybe: the uncertain future of audio-only visits and why we need them to address disparities. Health Affairs Blog. 2021.
- 85.Jacobs JC, Blonigen DM, Kimerling R, Slightam C, Gregory AJ, Gurmessa T, et al. Increasing Mental Health Care Access, Continuity, and Efficiency for Veterans Through Telehealth With Video Tablets. Psychiatr Serv. 2019;70(11):976–982. doi: 10.1176/appi.ps.201900104. [DOI] [PubMed] [Google Scholar]
- 86.Jacobs JC, Hu J, Slightam C, Gregory A, Zulman DM. Virtual Savings: Patient-Reported Time and Money Savings from a VA National Telehealth Tablet Initiative. Telemed J E Health. 2020;26(9):1178–1183. doi: 10.1089/tmj.2019.0179. [DOI] [PubMed] [Google Scholar]


