Abstract
Background and aim of the work:
Tibial tubercle avulsion fractures (TTAF) are uncommon condition in children and adolescents. These lesions may be misdiagnosed and consequently not properly treated. Reduction and fixation is indicated if displacement is higher than 2mm or if the extensor apparatus is damaged. Authors present a case of a TTAF associated with a complete lateral patellar retinaculum lesion in a 13-year-old male adolescent non-professional basketball player.
Methods:
Surgery consisted of reduction and fixation with 2 half threaded cancellous and washers; TTA was then basted and reinforced with a non absorbable suture according to Krachow technique and finally the patellar lateral retinaculum through a direct repair with absorbable material.
Results:
Clinical evaluation after 3 years showed bone healing, a complete resolution of pain, complete range of motion, good strength and complete functionality of the operated limb.
Conclusions:
Misdiagnosis or delayed treatment of TTAF can often result in nonunion, functional impairment, and persistent pain. For these reasons, authors believe that a stable and quick fixation associated to specialized rehabilitation are crucial for recovery. (www.actabiomedica.it)
Keywords: adolescent, tibial tubercle avulsion, synthesis, patellar retinaculum, childhood
Introduction
Tibial tubercle avulsion fracture (TTAF) is an uncommon condition in children and adolescents counting just 0,4 % to 2,7% of pediatrics fractures and less than 1% of all epiphyseal injuries with a higher risk for male than female, with a 10:1 ratio (1-3).
Males are commonly affected than females because of their higher participation in sports activities (4). Furthermore males tend to have more powerful quadriceps strength than females and it loads more stress during the muscle’s contraction on the carti-lage(5), whose closure occurs later than in females (4).
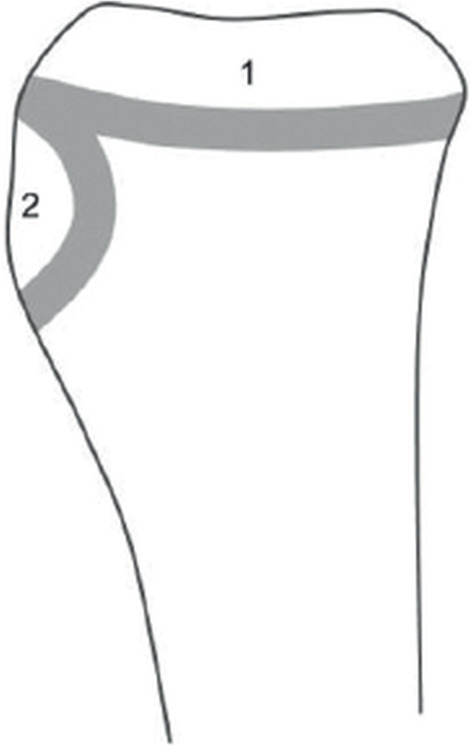
The proximal tibia has two ossification centers: one at the level of proximal tibial epiphysis and a second at the tibial tubercle or apophysis (Fig.1). They fuse together from posterior to anterior and proximal to distal; as consequence, the tibial tubercle is the last part to merge (5).
Figure 1. Ossification centers of proximal tibia.
The two proposed mechanisms of injury are a strong quadriceps contraction during knee extension while jumping and rapid passive flexion of the knee against the contracting quadriceps while landing; basketball is the sport more frequently implicated (10).
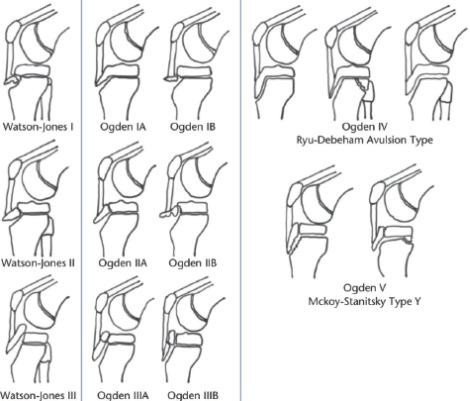
Different classification has been proposed and the one of Ogden (2,9) is the most complete and utilized (Tab. 1).
Table 1. Modified Ogden classification of tibial tubercle avulsion fracture.
| Type | Description | Treatment |
|---|---|---|
| IA | Fracture distal to junction | Conservative, if provided |
| of ossifcation centre of | that the extensor | |
| proximal tibial epiphysis | mechanism is intact and | |
| and tubercle | there is adequate anatomic reduction. If not, surgical. | |
| IB | Same as type IA but with | Conservative, if provided |
| comminution of fracture | that the extensor | |
| fragment | mechanism is intact and there is adequate anatomic reduction. If not, surgical. | |
| IIA | Fracture extension to | Conservative, if provided |
| junction of proximal tibial | that the extensor | |
| physis | mechanism is intact and there is adequate anatomic reduction. If not, surgical. | |
| IIB | Same as type IIA but with comminution of fracture fragment | Surgical |
| IIIA | Fracture extends into joint through proximaltibial epiphysis with displacement of fracture fragment | Surgical |
| IIIB | Same as type IIIA with comminution of fracture fragment. | Surgical |
| IV | Tibial physis with displacement of fracture fragment | Surgical |
| V | Type III associated with Type IV | Surgical |
Associated injuries such as meniscal tears, cruciate ligament laxity, patellar or quadriceps tendon avulsions, and compartment syndrome have been reported with tibial tubercle fractures (11).
Diagnosis is obtained by a combination of physical examination (tenderness at the palpation of tibi- al tubercle and functional impairment of the injured limb) and imaging. The first level exam is X-Ray; CT scan may be necessary for pre-operative planning or when the X-Rays do not clearly show the lesion (1, 2).
In the suspicion of associated soft tissue lesions, an MRI is indicated (2, 7).
The treatment of TAAF could be either conservative or surgical.
Management of these fractures is primarily based on the injury severity and fracture pattern, with the goal of restoring the extensor mechanism, and the articular cartilage surface. (11).
It is generally recommended to treat conservatively the fractures that are undisplaced and that preserve the active extension of the knee, such as fractures types IA, IB, and IIA according to Ogden. Surgical treatment should be applied in displaced, comminuted or intra-ar-ticular fractures or when there is loss of extension capacity such as fractures types IIB, III and IV (11,13).
Conservative treatment is usually performed with a tubular cast at 10° of flexion of the knee for at least 4-5 weeks. Surgical approach is usually performed also in case of unsatisfactory conservative treatment (11-13).
Several fixation methods have been described; even though cannulated screws are the most widespread treatment, different surgical therapeutic alternatives have been proposed, such as reduction with fixation from Kirschner wires to compression plates, suture anchors, tension bands, and combinations of these (11, 13).
Authors present a case of a TTAF associated with a complete lateral patellar retinaculum lesion in a 13 year-old male adolescent non-professional basketball player who was surgically treated.
Case report
A 13-year-old male adolescent non-professional basketball player injured during physical education. Injury occurred as a result of an accidental fall with his right in extension. Patient’s parents provided written informed consent about the treatment he was submitted, the processing of his personal data and to participate scientific study. At the emergency department the patient complained of almost complete functional impairment in the right lower limb; both flexion and extension of the knee were impossible. The patient also complained of severe pain during the compression of the tibial tuberosity (TT); swelling and intraarticular effusion were also remarkable.
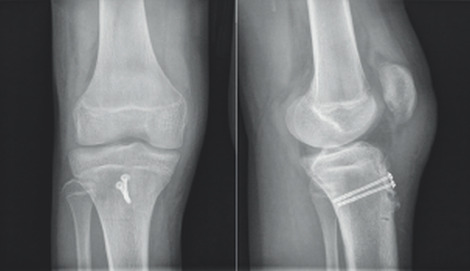
X-rays of the knees were performed showing tib-ial tubercle avulsion fracture (Fig.2).
Figure 2. AP and LL radiographs of the right knee with TT avulsion and displacement >2mm (arrow).
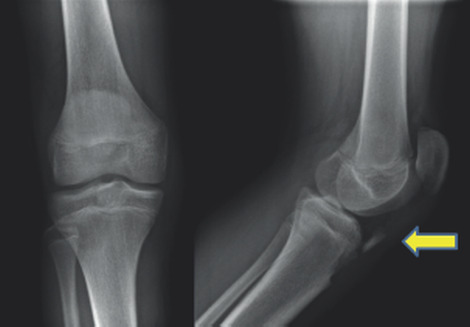
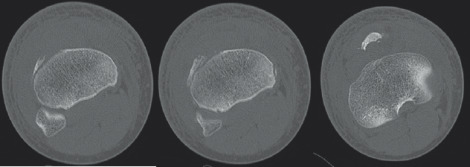
A CT study confirmed the fracture-avulsion and demonstrated a lateral displacement of the patella with suspected injury of the lateral retinacular ligaments (Figs. 3, 4).
Figure 3. CT scan sagittal views showing TTA fracture and displacement > 2mm (arrow).

Figure 4. CT scan axial views showing TTA fracture.
This lesion was classified as Type IB, according to Ogden (2).
The patient underwent fixation 10 days after the trauma.
Anterior approach was performed; incision was centred on the TTA. A complete displaced fracture with TTA avulsion was found associated with a lateral patellar retinaculum lesion.
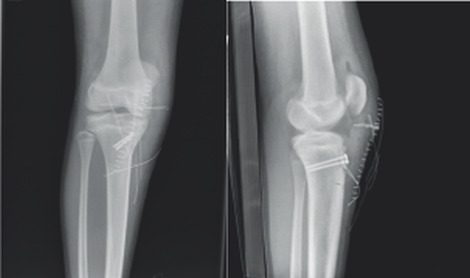
Under fluoroscopic control, the tibial tubercle was first reduced then stabilized with K-wires 1,8 mm diameter and then definitively fixed with 2 half-threaded cancellous screws with washers (Fig.5); the fragment was also basted with an absorbable suture according to Kracow’s technique. The patellar lateral retinaculum was sutured with an absorbable suture.
Figure 5. LL and AP post-op X-Rays.
Finally, an orthopedic brace locked at 10° of flexion was applied and weight bearing was prohibited.
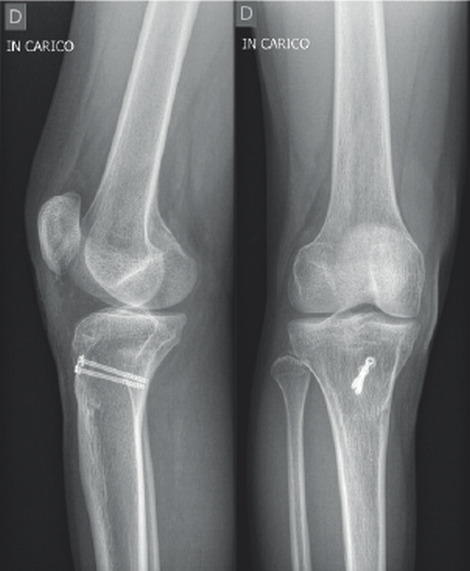
After 40 days the patient underwent a control X-ray which showed healing of the fracture and satisfactory patellar alignment (Fig. 6).
Figure 6. AP and LL X-Rays 40 days after surgery.
Afterwards, the patient started physiotherapy in order to recover joint mobility. In a second phase, strength recovery exercises were introduced.
At 3 months follow-up, no clinical pain or limping and no tenderness to palpation over tibial tubercle was remarkable. The patient was then encouraged to return to his normal activities and sports, including basketball.
Results
At final follow-up, after 3 years, the patient showed a complete recovery. Range of motion was complete.
The patient had no longer limping and no longer referred pain nor at rest, nor during walking or doing sports activities (Fig. 7). X-Rays showed a complete healing of the fracture (Fig. 8); he had no clinical pain, no tenderness over tibial tubercle, no limping or any skeletal anomaly, no lack of strength.
Figure 7. Clinical follow-up after 3 years.

Figure 8. Radiological follow-up after 3 years.
Discussion
The case that the authors described is remarkable for its rarity. TTAF is an uncommon condition in children and adolescents counting just 0,4 % to 2,7% of pediatrics fractures and less than 1% of all epiphyseal injuries (1, 2, 11)
TTAF mainly occur during sport activities. Two kind of mechanism were described in literature: a forced quadriceps contraction during knee extension, or a passive flexion of the knee with a quadricep contraction while landing after a jump. The prototypical sport is basketball, for example during lay-up or dunk (10, 11).
Several classifications were proposed for these lesions.
The first classification of tibial tubercle avulsion fractures introduced by Watson-Jones in 1955, who divided injuries into 3 types:
• Type I: an avulsion of the distal part of the tibial tubercle, which does not reach the proximal tibial epiphysis.
• Type II: the fracture extends through the epiphysis without involving the knee joint.
• Type III: TTA avulsion continuing proximal to the epiphysis involving the knee joint.
In 1980, this classification was modified by Og-den et al. who described a type IV in which the fracture extend posteriorly through the physis and a type V, also called the “Y” fracture, that couples type IIIB with type IV to form a “Y” shape (1, 9, 12) (Fig. 9).
Figure 9. Graphic representation of Ogden classification.
The diagnostic pathway is a combination of clinic and imaging.
Clinically, the patient usually complains of acupressure pain at TTA and there may also be functional impairment of the extensor apparatus.
The first level imaging exam are X-rays, both frontal and latero-lateral view.
CT could be useful for a better preoperative evaluation.
MRI could have a role if meniscal or ligamentous injuries or undisplaced fractures are suspected (18) even if low rates associated injuries such as meniscal tears, cruciate ligament laxity, patellar or quadriceps tendon avulsions, and compartment syndrome have been reported with tibial tubercle fractures (11).
The main objective of treatment is to restore the anatomy and, consequently, the function of the knee.
Conservative treatment is generally performed for undisplaced (< 2 mm) fractures who do not interest extensors capacity of the knee such as fractures types IA, IB, and IIA .
It is generally recommended to treat conservatively the fractures that are undisplaced and that preserve the active extension of the knee, such as fractures types IA, IB, and IIA according to Ogden (11-13).
Surgical treatment should be applied in displaced (> 2mm), comminuted or intra-articular fractures or when there is loss of extension capacity such as fractures types IIB, III and IV and in those cases of unsatisfactory conservative treatment (13).
Several fixation methods for these fractures have been described. Even though cannulated screws are the most widespread treatment, different surgical therapeutic alternatives have been proposed, such as fixation with Kirschner wires, compression plates, suture anchors, tension bands, and combinations of these.
Absorbable pins are usually used in children under 3 years of age (11). In case of small fragments or comminuted fractures tension banding with a cerclage wire and K-wires, which provide rotational stability, is a good alternative to cancellous screws (14).
A possible complication of this type of injury is the compartment syndrome; it could be due to rupture of the recurrent branch of the anterior tibial artery that runs along the lateral border of the tibial tuberosity. Even if the incidence of preoperative compartment syndrome is very low (up to 4% ) it can be devastating if not detected (11, 18).
The most common postoperative complications are bursitis, tenderness or prominence on the tibial tubercle and irritation due to hardware. A second surgical intervention for implant removal may be necessary in these cases (5). Low rates of refractures and wound infections have also been reported. In patients younger than 13 years, other complications that have been reported are genu recurvatum and limb length discrepancy. These events are rare and probably related to a partial growth arrest of the proximal tibial physis (11).
In conclusion, TTAF is an uncommon type of injury in young patients. It could be treated both conservatively and surgically thus depending of with the aim of anatomic and functional complete recovery. The authors proposed a rare case of Ogden IB displaced fracture that was associated with a complete tear of lateral reti-naculum of the patella. Senior author decided for a surgical treatment with two cancellous half-threaded screws, with washers, and with a reparation of lateral retinaculum of the patella. After 3 years fully recovery in anatomy and function was finally achieved.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- Zaizi A, El Yaacoubi T, Chafry B, Boussouga M. Tibial tubercle avulsion fractures in school sports injury: A case report. International Journal of Surgery Case Reports. 2019;58:30–32. doi: 10.1016/j.ijscr.2019.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole WW, Brown SM, Vopat B, Heard WMR, Mulcahey MK. Epidemiology, Diagnosis, and Management of Tibial Tubercle Avulsion Fractures in Adolescents. JBJS Reviews. 2020;8(4):e0186. doi: 10.2106/JBJS.RVW.19.00186. [DOI] [PubMed] [Google Scholar]
- Arkader A, Schur M, Refakis C, Capraro A, Woon R, Choi P. Unicortical Fixation is Sufficient for Surgical Treatment of Tibial Tubercle Avulsion Fractures in Children. Journal of Pediatric Orthopaedics. 2019;39(1):e18–e22. doi: 10.1097/BPO.0000000000001269. [DOI] [PubMed] [Google Scholar]
- Shin YW, Kim DW, Park KB. Tibial tubercle avulsion fracture according to different mechanisms of injury in adolescents. Medicine. 2019;98(32):e16700. doi: 10.1097/MD.0000000000016700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz P, Luderowski E, Tuca M. Tibial tubercle avulsion fractures in children. Current Opinion in Pediatrics. 2020;32(1):86–92. doi: 10.1097/MOP.0000000000000870. [DOI] [PubMed] [Google Scholar]
- Makram Z, Hedi A, Taoufik A, Mohsen T, Mondher M, Habib BH. Acute tibial tubercle avulsion fractures in the sporting adolescent. Arch Orthop Trauma Surg. 2008;128(12):1437–42. doi: 10.1007/s00402-008-0628-4. [DOI] [PubMed] [Google Scholar]
- McKoy BE, Stanitski CL. Acute tibial tubercle avulsion fractures. Orthop Clin North Am. 2003 Jul;34(3):397–403. doi: 10.1016/s0030-5898(02)00061-5. [DOI] [PubMed] [Google Scholar]
- Mosier SM, Stanitski CL. Acute Tibial Tubercle Avulsion Fractures. Journal of Pediatric Orthopaedics. 2004;24(2):181–4. doi: 10.1097/00004694-200403000-00009. [DOI] [PubMed] [Google Scholar]
- Ogden JA, Tross RB, Murphy MJ. Fractures of the tibial tuberosity in adolescents. J Bone Joint Surg Am. 1980 Jul;34(3):397–403. [PubMed] [Google Scholar]
- Mubarak SJ, Kim JR, Edmonds EW, Pring ME, Bastrom TP. Classification of proximal tibial fractures in children. J Child Orthop. 2009 Jun;3(3):191–7. doi: 10.1007/s11832-009-0167-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pretell-Mazzini J, Kelly DM>, Sawyer JR, et al. Outcomes and Complications of Tibial Tubercle Fractures in Pediatric Patients: A Systematic Review of the Literature. Journal of Pediatric Orthopaedics. 2016;36(5):440–6. doi: 10.1097/BPO.0000000000000488. [DOI] [PubMed] [Google Scholar]
- Kushner RL, Massey P. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2021 Jun 5. Tibial Tubercle Avulsion. [PubMed] [Google Scholar]
- Checa Betegón P, Arvinius C, Cabadas González MI, et al. Management of pediatric tibial tubercle fractures: Is surgical treatment really necessary? European Journal of Orthopaedic Surgery & Traumatology. 2019; Jul;29(5):1073–9. doi: 10.1007/s00590-019-02390-x. [DOI] [PubMed] [Google Scholar]
- Abalo A, Akakpo-numado KG, Dossim A, Walla A, Gnassingbe K, Tekou AH. Avulsion fractures of the tibial tubercle. J Orthop Surg (Hong Kong) 2008 Dec;16(3):308–11. doi: 10.1177/230949900801600308. [DOI] [PubMed] [Google Scholar]
- Yue I, Hurst N, Peterson JB, Kanegaye JT, Auten JD. Bilateral tibial tubercle avulsion fractures: A pediatric orthopedic injury at high risk for compartment syndrome. The American Journal of Emergency Medicine. 2019 doi: 10.1016/j.ajem.2019.05.033. S0735675719303444. [DOI] [PubMed] [Google Scholar]
- Pape JM, Goulet JA, Hensinger RN. Compartment syndrome complicating tibial tubercle avulsion. Clin Orthop Relat Res. 1993 Oct;;295:201–4. [PubMed] [Google Scholar]
- Brey JM, Conoley J, Canale ST, et al. Tibial tuberosity fractures in adolescents: is a posterior metaphyseal fracture component a predictor of complications? J Pediatr Orthop. 2012 Sep;32(6):561–6. doi: 10.1097/BPO.0b013e318263a370. [DOI] [PubMed] [Google Scholar]
- Rodriguez I, Sepulveda M, Birrer E, Tuca MJ. Fracture of the anterior tibial tuberosity in children. EFORT Open Rev. 2020 May 5;5(5):260–7. doi: 10.1302/2058-5241.5.190026. [DOI] [PMC free article] [PubMed] [Google Scholar]


