SARS-CoV-2 has had a massive impact on nursing homes (1). Mortality based on hospital cases is well described for the overall population in Germany (2); however, there is an urgent need to study mortality among inpatient nursing home residents (NHRs) hospitalized with COVID-19—not least in comparison to NHRs in hospital without COVID-19—and to analyze risk factors associated with an increased risk of mortality.
Acknowledgments
Translated from the original German by Christine Rye.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interests exists.
Methods
The COVID-Heim (“COVID Home”) project analyzed the routine data of all NHRs insured with the German General Local Health Insurance Fund (Allgemeine Ortskrankenkasse, AOK) and aged over 60 years of age (N = 531,533); the 90-day mortality of all NHRs that had undergone an inpatient hospital stay for COVID-19 (confirmed COVID-19 diagnosis [ICD U07.1] and COVID-19-relevant main diagnosis [2]) and that had been admitted between 1 January 2020 and a date of death or discharge up to and including 30 June 2021 was investigated. The 13 899 COVID-19-related hospital cases in the sample equate to 63.9% of the total number of hospitalized COVID-19 cases from homes under Section 36 of the German Infection Protection Act (nursing homes, etc.) reported to the Robert Koch Institute (3). Data on mortality were available as weekly aggregated data. COVID-19-relevant comorbidities according to Rößler et al. (4) were operationalized on the basis of data from 2018 up to the quarter in which hospital admission took place.
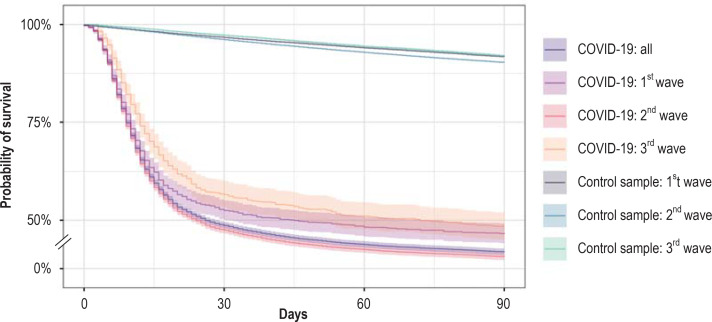
In a first step, the Kaplan-Maier curve of NHRs with COVID-19-relevant hospitalization is compared—per wave of the pandemic—with 33 groups of weighted random samples of NHRs without COVID-19-related hospitalization. Operationalization of the waves was carried out according to Tolksdorf et al. (5). Weighting of the random samples, for which a random inclusion date was generated, was based on sex, age category, level of care, and comorbidities, yielding adequate control samples. Individual implausibly generated inclusion data were excluded, thereby resulting in a slight reduction in case numbers. The random samples from the respective waves were pooled, meaning that adequate distribution of the generated inclusion date was achieved.
In a second step, a multivariate time-to-event analysis (Cox proportional hazard model) by deceased/nondeceased was performed for the group of NHRs hospitalized with a COVID-19 diagnosis and jointly analyzed for risk factors across all three COVID-19 waves.
Results
Univariate time-to-event analysis shows significant differences between the two comparison groups. The group of NHRs that underwent inpatient hospitalization for COVID-19 had a 58.1% risk of death in the 90 days after their stay. There was a significant difference between waves, with the highest risk of mortality being seen in the 2nd wave at 59.3%, whereas the risk was lower in the 1st and 3rd waves at 53.3% and 51.6 %, respectively. Furthermore, mortality rates are significantly higher compared to the control samples of NHRs with simulated hospital cases pooled by wave (1st wave: 8.2%; 2nd wave: 9.7%; 3rd wave: 8.1%) (figure).
Figure.
The Kaplan-Meier curves clearly show higher mortality rates among nursing home residents hospitalized for COVID-19 compared to control samples with simulated hospitalization.
Multivariate time-to-event analysis (table) of NHRs with COVID-19-related hospitalization also shows that those who were hospitalized during the 2nd wave of the COVID-19 pandemic had the highest risk of mortality. Males had a higher risk of mortality compared to females. In contrast to 80- to 84-year-olds, younger residents had lower risk, while older NHRs had higher risk. Compared to care level 3, NHRs with lower levels of care had lower risk and those with higher levels of care higher risk. Of the 35 COVID-19-related comorbidities, chronic renal failure, dementia, hemato-oncologic diseases with treatment (hazard ratio [HR]: 1.62), immunosuppressive therapy (HR: 1.20) and post-organ transplantation status (HR: 1.57) showed a statistically significantly increased risk of death. COPD and other severe lung diseases (HR: 0.93), depression (HR: 0.92), dialysis (HR: 0.79), and immunocompromising diseases (HR: 0.90) were associated with a statistically significantly lower mortality risk. With the exception of chronic renal failure (HR: 0.99), as well as COPD and other severe lung diseases (HR: 1.17) in the 3rd wave, the trends in associations in the wave-specific subgroup analyses remain unchanged.
Table. Risk of mortality among nursing home residents hospitalized with COVID-19*1.
| N = 13 899 | Deceased = 8079 | HR [95% CI] |
| 1st Wave of the pandemic | 817 (53.5%)*2 | 0.87 [0.81; 0.93] (p < 0.001) |
| 2nd Wave of the pandemic | 6758 (59.3%) | Reference category |
| 3rd Wave of the pandemic | 415 (51.6%) | 0.78 [0.70; 0.86] (p < 0.001) |
| Other | 89 (49.7%) | 0.76 [0.62; 0.94] (p = 0.010) |
| Female | 4460 (55.0%) | Reference category |
| Male | 3619 (62.4%) | 1.34 [1.28; 1.40] (p < 0.001) |
| 60–79 Years | 1689 (47.6%) | 0.75 [0.70; 0.81] (p < 0.001) |
| 80–84 Years | 1882 (58.2%) | Reference category |
| 85–89 Years | 2274 (60.3%) | 1.09 [1.02; 1.16] (p = 0.006) |
| ≥ 90 Years | 2234 (66.8%) | 1.32 [1.24; 1.41] (p < 0.001) |
| Level of care 1 | 24 (32.0%) | 0.51 [0.34; 0.76] (p = 0.001) |
| Level of care 2 | 1022 (52.4%) | 0.92 [0.85; 0.99] (p = 0.019) |
| Level of care 3 | 2801 (56.3%) | Reference category |
| Level of care 4 | 3077 (61.8%) | 1.13 [1.07; 1.19] (p < 0.001) |
| Level of care 5 | 1155 (60.1%) | 1.11 [1.03; 1.19] (p = 0.006) |
| Morbidity (reference category = no) *3 | ||
| Hypertension | No: 1081 (57.8%) Yes: 6998 (58.2%) |
0.97 [0.90; 1.04] (p = 0.331) |
| Dementia | No: 2584 (52.5%) Yes: 5495 (61.2%) |
1.15 [1.10; 1.21] (p < 0.001) |
| Chronic renal failure | No: 3543 (55.6%) Yes: 4536 (60.3%) |
1.10 [1.05; 1.16] (p < 0.001) |
| Heart failure | No: 3945 (56.9%) Yes: 4134 (59.4%) |
1.05 [0.99; 1.10] (p = 0.080) |
| Cerebrovascular disease | No: 4391 (58.5%) Yes: 3688 (57.7%) |
0.95 [0.91; 1.00] (p = 0.051) |
*1 Multivariate time-to-event analysis of non-specific mortality within 90 days
*2 Percentages show the proportion of deceased nursing home residents per category.
*3 Operationalization according to Rößler et al. (4) based on data from 2018 onwards. The five most frequent existing morbidities are presented; with monitoring of a further 29 morbidities; HIV was excluded from the analysis since none of the nursing home residents with HIV died. For reasons of availability, it was necessary to dispense with data from quarter (Q) 1/2021 for hospital cases in Q2/2021 and resort to data from Q4/2020.
A sensitivity analysis on this fallback resulted in only minor deviations (< 3%).
HR, hazard ratio; 95% CI, 95% confidence interval
Discussion
The present findings confirm the high mortality rate among nursing home residents with COVID-19 treated in hospital. At 58.1%, the analysis shows a significantly higher proportion compared to a previous analysis focusing on the 1st wave (1). This also results from the modified COVID inclusion criteria applied by Günster et. al. (addition of a COVID-19-relevant main diagnosis as a criterion) (2). In the previous study, 42.7% of fully inpatient care-dependent individuals with a COVID-19 diagnosis died while still in hospital, whereas the rate among other NHRs was 25.7% (1). Differing mortality rates between waves should be discussed against the background of differences in hospital admission probabilities across waves, given that only those who were admitted to hospital were included in the analyses. An increased risk was observed across all waves for male sex, age ≥ 90, care level > 3, as well as for chronic renal failure, dementia, hemato-oncologic disease with treatment, immunosuppressive therapy, and post-organ transplant status. This highlights the significance of infection prevention among NHRs with these risks. In addition to individual factors, future research should investigate further care-related risk factors and structural characteristics of nursing homes.
References
- 1.Kohl R, Jürchott K, Hering C, Gangnus A, Kuhlmey A, Schwinger A. Jacobs K, Kuhlmey A, Greß S, Klauber J, Schwinger A, editors. COVID-19-Betroffenheit in der vollstationären Langzeitpflege, Pflege-Report 2021: Sicherstellung der Pflege: Bedarfslagen und Angebotsstrukturen. Berlin, Heidelberg. Springer. 2021:3–20. [Google Scholar]
- 2.Günster C, Busse R, Spoden M, et al. 6-month mortality and readmissions of hospitalized COVID-19 patients: a nationwide cohort study of 8,679 patients in Germany. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255427. e0255427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.RKI. Täglicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19). 30.06.2021. www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Jun_2021/2021-06-30-de.pdf?__blob=publicationFile (last accessed on 18 February 2022) [Google Scholar]
- 4.Rößler M, Jacob J, Risch L, et al. Hierarchisierung von Risikofaktoren für schwere COVID-19-Erkrankungsverläufe im Kontext der COVID-19-Schutzimpfungen. Epid Bull. 2021,;19:3–12. [Google Scholar]
- 5.Tolksdorf K, Buda S, Schilling J. Aktualisierung zur „Retrospektiven Phaseneinteilung der COVID-19-Pandemie in Deutschland“. Epid Bull. 2021;37:13–14. [Google Scholar]