Ample evidence suggests that gender affects the incidence, susceptibility, presentation, diagnosis and severity of many psychiatric disorders. Schizophrenia is one of the most prevalent severe mental disorders, with an incidence of 0.7%–1% among the total population, which causes suffering and pecuniary losses.1 2 It has long been known that the age of schizophrenia onset differs in women compared with men. Some life events, such as pregnancy, fertility and menopause, are unique to women and can affect the onset and course of mental disorders. However, the role of gender in this association has received little attention. The female sex and reproductive transitions impact various aspects of brain biology and pathobiology. These biologic differences can impact differential gene expression or organ development. Evaluating gender-related differences is the first step in moving towards precision psychiatry. This article provides a brief overview of gender differences in the epidemiology, disease presentation, risk factors and management of schizophrenia.
Epidemiology
The incidence of schizophrenia is higher among men than women, with a ratio of nearly 1.4:1, although several reviews did not find sex differences in the lifetime prevalence of the illness.3 The onset of schizophrenia in males is 3.2–4.1 years earlier than in females.4 Males and females have shown different susceptibilities to schizophrenia in different life stages. The prevalence of schizophrenia was higher among men aged <40 years, with the peak incidence between 20 and 29 years.5 6 The sex gradient was the opposite for females with schizophrenia; a higher prevalence was found for those >40 years of age, with two incidence peaks—the first at the age of 20–39 years and the second at the perimenopause period.7 The prevalence of the illness increases significantly after 40 years of age in women, which may be related to decreased oestrogen levels after menopause. In addition, numerous psychosocial factors may contribute to the development of psychosis, including loneliness, adverse life events and the lack of family/social support, all of which may frequently be found in menopausal and postmenopausal women.8 9
Disease presentation
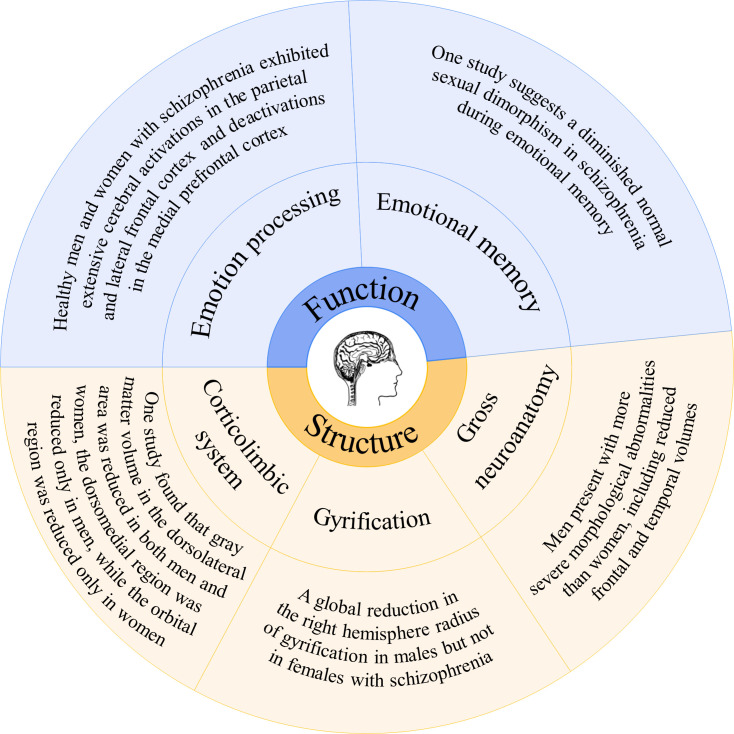
Among patients with schizophrenia, males have a greater risk of experiencing prominent negative symptoms, while females display more affective symptoms, including depression, impulsivity, emotional instability, sexual misconduct and sexual delusions.10 Regarding cognitive dysfunction, female patients performed better on measures of executive function, verbal memory and information processing speed than male patients (figure 1).11 Previous studies have also found that male patients outperformed females regarding visual memory and attention.12 However, male patients also reported worse premorbid functioning. The underlying biological mechanisms might be due to the sex differences in brain morphology, genetic risk factors and neuroprotective functions of oestrogen effects facilitated by gonadal and adrenal hormones and therefore depend on the gender of the individual.13 It should be noted that similar symptoms can be interpreted differently for male and female patients. For example, isolation, withdrawal and avoidance of the outside world may indicate a depressive syndrome in female patients with schizophrenia but may indicate negative symptoms in male patients.
Figure 1.
Main structural and functional differences of brain between males and females among schizophrenia patients.
Risk factors
Important psychosocial factors, including education, occupation, pregnancy and marriage, are closely related to schizophrenia’s occurrence, treatment response and recurrence. However, similar life events may have different effects on men and women. Previous findings suggested that childhood abuse may be more strongly associated with a risk for the development of schizophrenia and an earlier onset of the illness in women than in men.14 In addition, childhood adversity has been linked to the severity of different symptom dimensions in men and women.15 However, due to a later onset of schizophrenia and relatively normal social function, females tend to receive more years of education than men; this contributes to the lower risk of the illness for females.16 17 Stratified analyses found that urbanisation rates, divorce rates and socioeconomic conditions for female adults were positively associated with increased risk for schizophrenia.17 However, for male adults, low socioeconomic conditions were related to decreased risk of schizophrenia, and there was no significant association between rates of divorce and risks for schizophrenia.14–17 A frequent topic discussed by young female patients with schizophrenia during routine psychiatric clinic visits is the presence or absence of a desire for pregnancy. Those who become pregnant are concerned about controlling their illness symptoms during the antenatal and postnatal periods and express fear of losing their marriage, congenital malformation of the fetus and stigma.
Disease management
In therapeutic strategies used to treat schizophrenia, classic symptomatic diagnoses often describe male presentations of the illness. Thus, an important area needing improvement is the early detection of gender-specific signs of first-episode schizophrenia to shorten the duration of untreated schizophrenia for females. Due to the different physical structures of males and females, the pharmacodynamics and pharmacokinetics of antipsychotics may also be affected by gender. Previous studies have shown that the serum concentrations of most antipsychotics in premenopausal women are higher than in men, or if the serum concentrations are the same, the share of the dopamine receptors is higher in women than in men.18–21 However, there are no gender-specific dosing recommendations in clinical practice, leading to unavoidable risks of overmedicating. A more comprehensive appreciation of the role of gender in the molecular basis of schizophrenia will encourage the development of novel and more effective pharmacotherapies. Considering the hormonal phases women commonly experience during their lives, ongoing management of the hormonal fluctuations of women being treated for schizophrenia is especially vital as they undergo events that trigger hormonal changes: pregnancy, childbirth, lactation and menopause. Moreover, societal prejudices against those with mental illness may more significantly impact female patients with schizophrenia. Thus, female patients require drugs with fewer adverse reactions, more comprehensive control of symptoms and greater restoration of social function. Closer cooperation with gynaecologists and obstetricians is also needed.
Conclusion
Although gender differences are innate, the diverse outcomes of these differences in disease have been emphasised in recent years. Classical symptom recognition in medicine is often based on male presentations, an insufficiency in this present era of precision medicine. The most notable medical example is heart disease, in which men and women manifest different symptoms. For instance, when myocardial infarction occurs, men present with typical chest pain, while women present with pain between the shoulder blades, nausea or vomiting, resulting in an extension of 30–45 min for cardiac resuscitation.22 At present, researchers studying gender differences in schizophrenia often focus on clinical symptoms but lack large-scale, high-quality clinical cohort studies, leading to various controversial conclusions. Meanwhile, more targeted treatment strategies are lacking. Sex differences in schizophrenia are well-recognised yet poorly understood clinical phenomena. Only by receiving gender-specific care will men and women with schizophrenia have optimal chances to fare well.
Biography
Xin Li obtained a bachelor's degree in clinical medicine from Fudan University, Shanghai, China in 2021. Currently, he is a second-year doctoral student at the Department of Psychiatry, Huashan Hospital, Fudan University, in Shanghai, China. His main research interests include evidence-based medicine and the early identification and optimized treatment of affective disorders.

Footnotes
Contributors: Design and conceptualisation of the study: XL. Data collection: XL, WZ. Drafted and revising the manuscript for intellectual content: XL, WZ, ZY.
Funding: This work was supported by the Shanghai Science and Technology Innovation Action Plan Natural Science Fund Project (21ZR1455400); Jiangsu Province Science and Technology Plan Project Key R&D Programme (BE2020661).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet 1997;349:1436–42. 10.1016/S0140-6736(96)07495-8 [DOI] [PubMed] [Google Scholar]
- 2.Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull 2004;30:279–93. 10.1093/oxfordjournals.schbul.a007078 [DOI] [PubMed] [Google Scholar]
- 3.Aleman A, Kahn RS, Selten J-P. Sex differences in the risk of schizophrenia: evidence from meta-analysis. Arch Gen Psychiatry 2003;60:565–71. 10.1001/archpsyc.60.6.565 [DOI] [PubMed] [Google Scholar]
- 4.Fernando P, Sommer IEC, Hasan A. Do we need sex-oriented clinical practice guidelines for the treatment of schizophrenia? Curr Opin Psychiatry 2020;33:192–9 10.1097/YCO.0000000000000597 [DOI] [PubMed] [Google Scholar]
- 5.Giordano GM, Bucci P, Mucci A, et al. Gender differences in clinical and psychosocial features among persons with schizophrenia: a mini review. Front Psychiatry 2021;12:789179. 10.3389/fpsyt.2021.789179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corrigan P, Thompson V, Lambert D, et al. Perceptions of discrimination among persons with serious mental illness. Psychiatr Serv 2003;54:1105–10. 10.1176/appi.ps.54.8.1105 [DOI] [PubMed] [Google Scholar]
- 7.McGrath J, Saha S, Welham J, et al. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med 2004;2:13. 10.1186/1741-7015-2-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charlson FJ, Ferrari AJ, Santomauro DF, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull 2018;44:1195–203. 10.1093/schbul/sby058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jauhar S, Johnstone M, McKenna PJ. Schizophrenia. Lancet 2022;399:473–86. 10.1016/S0140-6736(21)01730-X [DOI] [PubMed] [Google Scholar]
- 10.Leger M, Neill JC. A systematic review comparing sex differences in cognitive function in schizophrenia and in rodent models for schizophrenia, implications for improved therapeutic strategies. Neurosci Biobehav Rev 2016;68:979–1000. 10.1016/j.neubiorev.2016.06.029 [DOI] [PubMed] [Google Scholar]
- 11.Mendrek A, Mancini-Marïe A. Sex/gender differences in the brain and cognition in schizophrenia. Neurosci Biobehav Rev 2016;67:57–78. 10.1016/j.neubiorev.2015.10.013 [DOI] [PubMed] [Google Scholar]
- 12.Buck G, Lavigne KM, Makowski C, et al. Sex differences in verbal memory predict functioning through negative symptoms in early psychosis. Schizophr Bull 2020;46:1587–95. 10.1093/schbul/sbaa054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen J-H, Sun Y, Ju P-J, et al. Estrogen augmented visceral pain and colonic neuron modulation in a double-hit model of prenatal and adult stress. World J Gastroenterol 2021;27:5060–75. 10.3748/wjg.v27.i30.5060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia M, Montalvo I, Creus M. Labad sex differences in the effect of childhood trauma on the clinical expression of early psychosis Compr. Psychiatry 2016;68:86–96. [DOI] [PubMed] [Google Scholar]
- 15.Pruessner M, King S, Vracotas N, et al. Gender differences in childhood trauma in first episode psychosis: association with symptom severity over two years. Schizophr Res 2019;205:30–7. 10.1016/j.schres.2018.06.043 [DOI] [PubMed] [Google Scholar]
- 16.Luo Y, Pang L, Zhao Y, et al. Gender difference in the association between education and schizophrenia in Chinese adults. BMC Psychiatry 2020;20:296. 10.1186/s12888-020-02700-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luo Y, Guo C, Zhang L, et al. County-level social factors and schizophrenia: a multilevel study of 1.9 million Chinese adults. Psychiatry Res 2019;271:286–90. 10.1016/j.psychres.2018.08.057 [DOI] [PubMed] [Google Scholar]
- 18.Weng J, Zhang Y, Li H, et al. Study on risk factors of extrapyramidal symptoms induced by antipsychotics and its correlation with symptoms of schizophrenia. Gen Psychiatr 2019;32:e100026. 10.1136/gpsych-2018-100026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brand BA, de Boer JN, Dazzan P, et al. Towards better care for women with schizophrenia-spectrum disorders. Lancet Psychiatry 2022;9:330–6. 10.1016/S2215-0366(21)00383-7 [DOI] [PubMed] [Google Scholar]
- 20.Jönsson AK, Spigset O, Reis M. A compilation of serum concentrations of 12 antipsychotic drugs in a therapeutic drug monitoring setting. Ther Drug Monit 2019;41:348–56. 10.1097/FTD.0000000000000585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seeman MV. Men and women respond differently to antipsychotic drugs. Neuropharmacology 2020;163:10763. 10.1016/j.neuropharm.2019.05.008 [DOI] [PubMed] [Google Scholar]
- 22.Bairey Merz CN, Pepine CJ, Walsh MN, et al. Ischemia and no obstructive coronary artery disease (INOCA): developing evidence-based therapies and research agenda for the next decade. Circulation 2017;135:1075–92. 10.1161/CIRCULATIONAHA.116.024534 [DOI] [PMC free article] [PubMed] [Google Scholar]