Abstract
Introduction
Syria’s protracted conflict has devastated the health system reversing progress made on maternal health preconflict. Our aim is to understand the state of maternal health in Syria focused on underage pregnancy and caesarean sections using a scoping review and quantitative analysis; the latter draws on data from the Syrian American Medical Society’s (SAMS) maternal health facilities in northwest Syria.
Methods
We performed a scoping review of academic and grey literature on the state of maternal health across Syria since the onset of conflict (taken as March 2011). Identified articles were screened using pre-established criteria and themes identified. We also performed a retrospective quantitative analysis of maternal health data from SAMS’ facilities in a microcontext in north-west Syria between March 2017 and July 2020, analysing the trends in the proportion of births by caesarean section and age at pregnancy.
Results
Scoping review: of 2824 articles, 21 remained after screening. Main themes related to maternal mortality rates, caesarean sections, maternal age and perinatal care. 12 studies reported caesarean section rates; these varied from 16% to 64% of all births: northern Syria (19%–45%,) Damascus (16%–54%,) Lattakia (64%) and Tartous (59%.) Quantitative analysis: Of 77 746 births across 17 facilities, trend data for caesarean sections showed a decrease from 35% in March 2017 to 23% in July 2020 across SAMS facilities. Girls under 18 years accounted for 10% of births and had a lower proportion of caesarean section births. There was notable geographical and interfacility variation in the findings.
Conclusion
The quality of available literature was poor with country-level generalisations. Research which explores microcontexts in Syria is important given the different effects of conflict across the country and the fragmented health system. Our quantitative analysis provides some evidence around the changes to caesarean section rates in northwest Syria. Despite limitations, this study adds to sparse literature on this important topic.
Keywords: Maternal health, Obstetrics, Public Health, Surgery
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Armed conflict adversely affects maternal health through direct effects on women but also through its effects on healthcare access.
Syria’s protracted conflict has caused widespread destruction to the healthcare system and adversely affected access to maternal health services.
During Syria’s conflict, higher proportions of caesarean sections were reported than preconflict with a greater proportion of underage pregnancies (under 18 years of age)
Conflict adversely affects access to and quality of maternal health services.
WHAT THIS STUDY ADDS
From the scoping review, we report a dearth of literature, particularly that which is localised around important indicators of maternal health.
Our quantitative analysis of 77 746 pregnancies from 17 facilities in northwest Syria (March 2017–July 2020) showed a general downward trend of the proportion of births by caesarean section.
A spike in the proportion of births by caesarean section occurred in March 2020 to 33.2% after an escalation of violence between December 2019 and February 2020 caused widespread displacement.
Deliveries among girls under 18 years of age accounted for 7946 (10.2%) of births in Syrian American Medical Society’s facilities and the proportion delivered by caesarean section was lower than in those aged 18 years and over.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Further research which examines the impact of conflict on maternal health and the proportion of births by caesarean section across geopolitical regions in Syria is required.
Maternal health programmes which address the causes of underage pregnancies and their impacts are required given the sociological impacts which have resulted from the conflict in Syria.
Introduction
Protracted conflict adversely affects health systems, with particular impacts on reproductive, maternal, newborn and child health (RMNCH) services and outcomes. Attacks on healthcare facilities and sociopolitical instability can reduce access and widen existing inequalities with long-term consequences for mother and child.1 Subsequent social changes may contribute to early or forced marriage and the associated potential consequences, including gender-based violence, domestic abuse and birth complications, which may have lasting effects on women, children and their communities.2
The impact of conflict can be both direct and indirect3 with immediate and longer-term consequences to RMNCH. Direct consequences include attacks on healthcare services which can in turn affect healthcare utilisation.4 Indirect consequences include socioeconomic and sociopolitical effects of conflict, ranging from changing roles of women in the community, early or forced marriages, inadequate food or shelter and insecurity.1 3 Quality of services can also be affected by the forced displacement of trained healthcare workers5 and interruptions in supply chains and in the range of services required for RMNCH. Data from such settings may be incomplete or unavailable, but increasing reports from local surveys or surveillance provide evidence around the impacts of conflict with reported indicators on under 5 mortality, maternal mortality rates (MMR) and vaccination rates providing some indication of the state of RMNCH in armed conflict.6
In Syria, the protracted conflict began with peaceful uprisings in March 2011 but rapidly escalated to armed conflict by the middle of 2012 with devastating impacts, particularly on women and children. The conflict has displaced more than half its preconflict population of 22 million and resulted in at least 585 000 deaths.7 Syria has experienced among the worst impacts of attacks on healthcare globally8 with more than 600 attacks on health facilities, including those for maternal or child health, leaving more than 50% of facilities not functioning.9 Areas outside of the control of the Syrian government have been most affected; these include the northeast and northwest of the country where large numbers of internally displaced people shelter, most of whom are women and children.10 The recent COVID-19 pandemic and economic collapse in 2020 have exacerbated existing vulnerabilities, leaving more than 80% of the Syrian population living in poverty (less than US$2 a day) and more than 9 million living with food insecurity.11 Almost 6 million women and at least 2.5 million girls are in need of humanitarian aid with around one quarter of the population of reproductive age.12 Despite the extensive impacts on RMNCH, there remains little data with which to inform activities supporting RMNCH both now and in the longer term.
The aim of our research is to explore the impact of conflict on maternal healthcare in Syria in general with a focus on understanding the reporting of underage pregnancies and caesarean sections during the conflict. We do this by performing a scoping review of available academic and grey literature on maternal health across Syria, coupled with a quantitative analysis of available data on the utilisation of maternal services, age at pregnancy and caesarean section rates from the Syrian American Medical Society (SAMS) a humanitarian organisation which has provided healthcare in Syria since the onset of the conflict. The latter describes data from a microcontext in northwest Syria and provides an opportunity to compare findings in the scoping review from across the whole country.
Methods
We performed (1) a scoping literature review of academic and grey literature sources on maternal health in Syria since the onset of the conflict (taken as March 2011) and (2) a quantitative analysis of routinely collected clinical data on maternal health from a humanitarian organisation operating in northwest Syria between March 2017 and July 2020.
Scoping literature review
To identify available peer-reviewed studies, we searched electronic bibliographic databases including Medline, Embase and Google Scholar for articles relating to maternal health inside Syria during the crisis. We used Medical Subject Heading terms and keywords including ‘maternal health,’ ‘Syria,’ ‘maternal mortality,’ ‘maternal morbidity,’ ‘caesarean section,’ ‘conflict,’ ‘antenatal,’ ‘postnatal’ and ‘perinatal’ in various combinations to keep the search as broad as possible. We excluded manuscripts published before 2011 and those describing issues related to Syrian refugees rather than the situation inside Syria.
For grey literature, we searched OpenAire as well as individual relevant websites such as Maternal Health Task Force, Department For International Development), SAMS, Medecins Sans Frontieres, Save the Children, United Nations Population Fund (UNFPA), US Agency for International Development, the WHO reports and UNICEF.
The full search strategy (online supplemental table 1 appendix) and details of included studies (online supplemental table 2 appendix) are included in online supplemental appendix. Results were imported into excel and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used to document study inclusion based on the selection criteria shown in table 1. Title and abstract screening was conducted by two authors following full text analysis by three authors to agree the final included articles. Following this, all articles had references and citations screened for additional relevant articles.
Table 1.
This table shows the inclusion and exclusion criteria for the scoping literature review
| Feature | Inclusion | Exclusion |
| Population of interest | Syrian women inside Syria who are pregnant or have given birth including internally displaced persons | Syrian women who are pregnant or have given birth outside Syria including refugees |
| Intervention | Maternal health services | Sexual and reproductive health services |
| Outcomes | Maternal health Maternal morbidity and mortality Obstetric care (Antenatal, perinatal and postnatal) Availability of health services Utilisation of health services Maternal variables (age of mother) Birth statistics (caesarean section compared with vaginal birth) Abortion statistics |
Gender based violence Neonatal health |
| Study design | Review articles, epidemiological studies, retrospective analysis, cross-sectional studies | Case reports and newspaper articles. |
| Study period | Study period after the start of the conflict in March 2011. | Study period before the start of the conflict in March 2011. |
| Language | Full paper available in English or Arabic. | Full paper not available in English or Arabic. |
bmjgh-2021-008001supp001.pdf (336.8KB, pdf)
Quantitative analysis
We performed a retrospective analysis of clinical data on maternal health from SAMS’ facilities in northwest Syria using data obtained from March 2017 to June 2020. This included routinely collected data from healthcare facilities which were reported monthly to the country office of SAMS in Gaziantep in Turkey. This is inputted into SAMS’ health information system (HIS) based on International Clasification of Disease (ICD)-10 coding.
Setting
Northwest Syria is an area of almost 36 000 km2 encompassing the governorates of Aleppo, Hama, Idlib and Latakia; it contains 4.17 million Syrians of whom more than 2 million are internally displaced.13 A further escalation of violence between December 2019 and March 2020 displaced one million people, mostly from southern to northern parts of Idlib governorate; 80% of these are women and children. Widespread displacement and attacks on and around health facilities have strained regional health and humanitarian services. 1.4 million displaced Syrians live in tented settlements, while others may reside in rented accommodation, unfinished buildings or communal shelters, for example, schools or mosques facing numerous obstacles to healthcare access and essential humanitarian support.13
SAMS
SAMS is a humanitarian organisation which, as of the end of 2020, is mainly operating in northwest Syria (with some projects in northeast Syria) though it had previously provided healthcare in Dara’a in Southern Syria and in Eastern Ghouta in Damascus’ suburbs. Its programmes focus on populations with the highest needs which are currently in northwest and northeast Syria.
Data
Data from all 17 of SAMS’ facilities which provided maternal healthcare in northwest Syria were included. Anonymised, aggregated data on consultations relating to maternal health and the total number of monthly consultations were provided from SAMS’ HIS. These are classified by local data collectors as per ICD-10 coding on electronic databases and then sent electronically to the SAMS HIS team based in Turkey; this is then aggregated and processed. Monthly aggregates, collected from March 2017 to July 2020, provided the dataset examined in this study; no patient identifiable data were provided to the research team. All data relevant to maternal health as per ICD-10 classification were included. We do not have this disaggregated by antenatal or postnatal visits. Variables included number of maternal consultations, total number of consultations, age of mother (under or over 18), provided as a total as well as by facility, number of vaginal births, number of caesarean sections and facility type.
Facilities
Data from facilities containing records of vaginal births, caesarean sections and assisted births during at least one of the months in question were extracted. Following extraction, facilities were either categorised as offering basic emergency obstetric care (BEmOC) or comprehensive obstetric care (CEmOC), and as being referral or non-referral facilities for maternal and obstetric care. For the purposes of this study, BEmOC facilities were defined according to UNFPA guidance14 as those expected to be capable of administering medications used in obstetric care, performing assisted vaginal births and basic neonatal resuscitation, and removing the placenta and/or other retained products of conception. In addition to these basic procedures, CEmOC facilities are equipped and expected to safely perform surgery and blood transfusions. In the SAMS’ health system, BEmOC facilities are typically primary healthcare centres (PHCs) staffed and equipped with basic equipment including an emergency bag (contains supplies for obstetric and newborn complications as well as newborn resuscitation), ultrasound, fetoscope, labour table and a hospital bed.
Statistical analysis
All available data were obtained; as such, size calculations were not made. The outcomes of interest are the trends in the proportion of births by caesarean sections and underage pregnancies over time. Data were analysed using the R statistical programming language. Relevant summary data frames were generated using the dplyr package from which trends in the proportion of caesarean sections and vaginal births over time were produced for each facility using a combination of base R graphical features and the ggplot2 package. Analysis was restricted to basic summary and descriptive statistics, with no statistical techniques employed to quantify any apparent relationships between variables due to limitations of the data. As such, inferences were primarily made based on a visual and contextual analysis of the graphics that were generated. Line graphs and scatterplots were used to draw conclusions on descriptive data.
Bias
Data were provided from SAMS’ facilities only; this accounted for a varying proportion of the total number of facilities providing maternal healthcare in northwest Syria throughout the study period. Experiences may differ in other regional facilities supported by other organisations. These data were collected during active conflict; as such, there may be inaccuracy in recording, missing data or misdiagnosis due to inadequate resources or experienced staff. Also, the data do not include patients who may not have presented due to difficulties with access, checkpoints or conflict.
We included papers from the whole of Syria on maternal health to be comprehensive and to inform the findings from the microcontext in northwest Syria for which a quantitative analysis was performed. This allows comparison of caesarean section and underage pregnancies across Syria and the microcontext in northwest Syria.
Patient and public involvement
Patients were not involved in setting the research questions, deciding outcomes measured or in the design of this study. The study made use of routinely collected data and so there was no participation burden to patients at the facilities included. This work will directly impact SAMS’ maternal health programmes in Syria. Relevant data will be shared with the public and with healthcare workers working in these areas as well as the health cluster in Gaziantep which is involved with planning of services in northwest Syria.
Results
Of 2873 articles identified in the literature search, 2657 were excluded through title screening. The remaining texts were imported to excel and duplicates removed leaving 201 papers for abstract analysis; excluding another 158 titles. The remaining 43 publications were analysed in full and a final 21 papers deemed appropriate for inclusion in the review.
Scoping literature review
Of the 21 included articles, 13 were peer-reviewed studies15–27 and 8 grey literature reports.28–35 Of the 13 peer-reviewed studies, 6 were secondary data analysis,15–19 27 3 were cross-sectional studies,21 25 28 1 clinical audit,23 1 literature review,22 1 case study,24 1 prospective data registry study26 and 1 mixed-method study that included a literature review and country-level data reporting.20 From the grey literature reports, four were country-level data reporting,28–30 35 two were activity reports,33 34 one was secondary data analysis32 and one was a qualitative study.31 See figure 1 for the PRISMA flow chart. Included articles all reported results from inside Syria, however, the geographical areas described varied; 12 studies described results relating to Syria as a whole, 4 described results specific to Damascus and rural Damascus, 1 focused on northeast Syria (Hassaka, Ar-Raqqa) and 4 reported on northwest Syria (Aleppo, Idlib, Atmeh, Hama).
Figure 1.
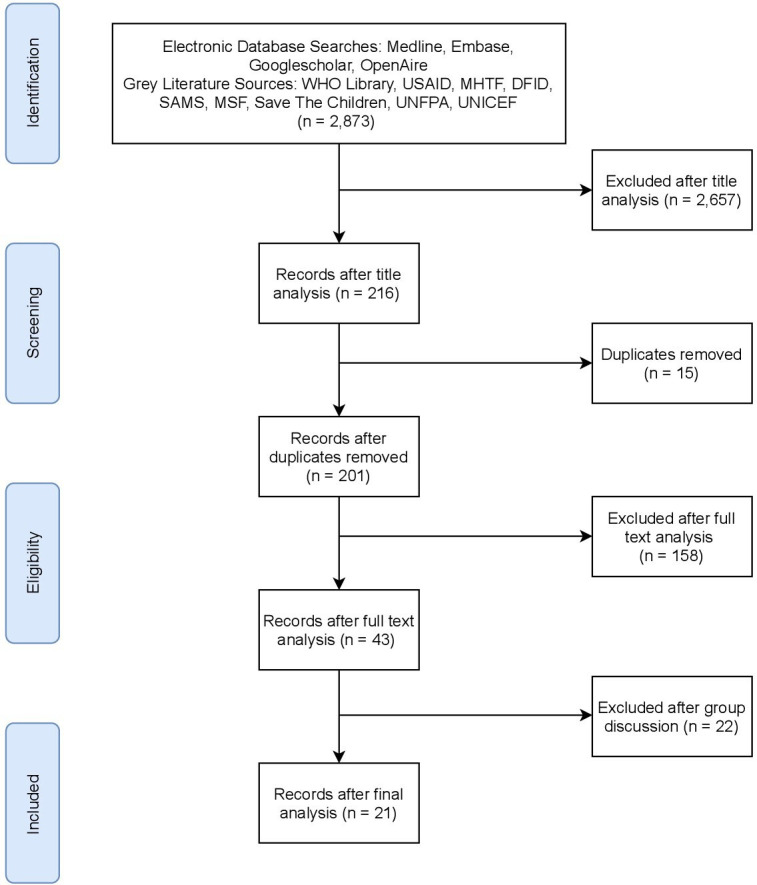
PRISMA flow chart for included and excluded academic and grey literature papers. DFID, Department For International Development; MHTF, Maternal Health Task Force; MSF, Medecins Sans Frontieres; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SAMS, Syrian American Medical Society’s; UNICEF, United Nations Population Fund; USAID, US Agency for International Development.
The main emerging areas from the literature can be grouped into those relating to (1) maternal mortality estimates; (2) caesarean sections; (3) underage pregnancies and (4) perinatal care (PNC).
Maternal mortality estimates
The MMR reports the number of maternal deaths per 100 000 live births and is a recognised indicator of maternal health globally, however, estimates can vary widely. Of the 21 articles identified, 7 described MMR in Syria.17–20 22 29 30 MMR estimates ranged from between 27 and 49 per 100 000 in 2010 to between 54.1 and 68 per 100 000 in 2015. All data were country-level estimates with results available between 1990 and 2017. The papers which mention MMR draw on similar data sources including the Global Burden of Disease17 19 or secondary analyses from the UN MMEIG (United Nations Maternal Mortality Estimation Inter-agency Group).18 30 36 Data reported by some authors as World Bank estimates use data from the UN MMEIG. All studies present a similar trend with an initial decline in MMR between 1990 and 2010, preconflict, followed by an overall increase in MMR during the years of the conflict until 2017. This is reported by UN MMEIG as increasing from 16 per 100 000 in 2000 to 27 per 100 000 in 2010 and 31 per 100 000 in 201736
Types of birth
Twelve studies describe caesarean sections compared with vaginal births.15 21–23 25–27 31–35 Of these, 1115 21–23 25–27 31–33 35 reported facility level, caesarean section rates higher than the population-level WHO recommended 10%–15%, with the remaining study34 reporting no births in its Syrian facilities during the included study period. These studies are summarised in table 2. In terms of geographical area, six studies26 31–35 reported caesarean section rates from northern Syria, including Hassakeh, Ar-Raqqa, Atmeh, Aleppo and Deir-ez-zour ranging between 0%35 and 44.6%.32 Seven studies21–23 25 27 32 35 reported caesarean section rates from Southern Syria including Damascus, Hama, Homs, Dar’a, As-Sweida, Quneitra and East Ghouta, ranging between 16.3%25 and 53.9%.21 One study reported very high caesarean section rates in facilities in Lattakia (63.7%) and Tartous (58.7%), which was attributed to cultural preferences rather than the effect of the conflict.35
Table 2.
This table summarises findings from studies which report caesarean section rates including location and date
| Author | Study period | Location | No of facilities | Type of facilities | Vaginal births | Caesarean sections | Caesarean section rate (%) |
| Al-Hammami23 | 2011–2017 | Damascus, Syria | 1 | University Hospital | 45 649 | 32 466 | 41.6 |
| 2011 | Not stated | Not stated | 32 | ||||
| 2012 | Not stated | Not stated | 33 | ||||
| 2013 | Not stated | Not stated | 43.5 | ||||
| 2017 | Not stated | Not stated | 51 | ||||
| WHO | December 2015 | Ar-Raqqa | 4 | Public Hospitals | 1702 | 386 | 18.5 |
| Hama | 6 | 659 | 611 | 48.1 | |||
| Homs | 6 | 240 | 217 | 47.5 | |||
| Dara’a | 4 | 85 | 28 | 24.8 | |||
| Aleppo | 13 | 226 | 180 | 44.3 | |||
| Deir-ez-zour | 4 | 35 | 0 | 0 | |||
| Al Hassakeh | 4 | 717 | 115 | 13.8 | |||
| As-Sweida | 3 | 280 | 165 | 37.1 | |||
| Quneitra | 1 | 70 | 40 | 36.4 | |||
| Damascus | 15 | 958 | 572 | 37.4 | |||
| Rural Damascus | 9 | 325 | 291 | 47.2 | |||
| Lattakia | 8 | 272 | 478 | 63.7 | |||
| Tartous | 6 | 311 | 442 | 58.7 | |||
| Terkawi26 | October–December 2017 | Atmeh District, Syria | 1 | Women and Children’s Health Centre | 1440 | 617 | 30.0 |
| Human Appeal31 | January–August 2019 | Aleppo, Syria | 1 | NGO hospital | 1367 | 385 | 22.0 |
| UNFPA33 | 2016 | North Syria | Not Specified | Not specified | 1296 | 431 | 25.0 |
| Southern Syria | 1096 | 574 | 34.4 | ||||
| MSF34 | 2015 | Hassakeh, Syria | 1 | Maternity hospital | 1166 | 393 | 25.2 |
| Kabakian-Khasholian25 | November 2014–April 2015 | Damascus, Syria | 1 | Public teaching hospital | 1009 | 197 | 16.3 |
| Alsharif27 | 2018–2020 | Damascus, Syria | Not Specified | Not specified | 734 | 787 | 51.7 |
| Roumieh21 | January–December 2017 | Damascus, Syria | 8 | Largest primary care facilities | 509 | 596 | 53.9 |
| Cuesta15 | 2008–2015 | MSF Facilities, Syria | 1 | General hospital | 0 | 0 | 0 |
| DeJong22 | 2014 | Damascus, Syria | 1 | Public maternity hospital | Not stated | Not stated | 46 |
| Syrian American Medical Society47 | September 2017–February 2018 | North Syria | 3 | Major reproductive health facilities | Not stated | Not stated | 44.6 |
| Southern Syria | 3 | Not stated | Not stated | 39.3 | |||
| East Ghouta, Syria | 1 | Not stated | Not stated | 41.1 |
MSF, Medecins Sans Frontieres; NGO, Non-governmental organisation; UNFPA, United Nations Population Fund.
Underage pregnancies
From the articles reviewed, four22 31–33 commented on maternal age, three of which reported primary data31–33 and one secondary data.22 Human Appeal reported that 25% of patients seen at Al Imaan Hospital in Idlib were under 18 years old.31 SAMS reported that in one of their facilities in Southern Syria, 12.2% of pregnancies were in girls under the age of 18 between September 2017 and February 2018 and in another in East Ghouta the proportion was 12.7% in the same time period.32 UNFPA reported the number of pregnant women under 18 in its northern facilities (129) and in its Southern facilities (506).33 DeJong et al report secondary data from the 2006 UN Population Division estimates on the adolescent birth rate per 1000 adolescent women preconflict, in 2009, to be 69 per 1000 compared with 70 per 1000 in 2013.22 None of the four articles commented on the parity or gravidity of the women discussed. Not all reports gave the denominator of their studies or explored relevant indicators including birth outcomes.
Perinatal care
Of the included articles, seven discuss the provision of antenatal care (ANC) in Syria since 2011,21 22 25 26 28 33 34 three commented on PNC23 27 33 and three articles comment on the presence of skilled birth attendants during labour all of which report figures for Syria as a whole.22 28 31
Two of the studies comment on ANC coverage in Syria generally17 23; Abdelgawad et al report 88% ANC coverage between the years 2009 and 2013, DeJong et al report the proportion of women attending at least one ANC visit preconflict was 87.7% compared with 62% during the conflict. Three studies reported the proportion of antenatal visits at specific hospitals, two in Damascus in 2015 and 201722 26 and one in Atmeh in 2017.27 Kabakian-Khasholian et al interviewed 1200 women using public services in a teaching hospital in Damascus between November 2014 and April 2015 and found that 32.5% attended less than four ANC visits while 67.5% attended four or more ANC visits. Roumieh et al interviewed 1105 women from the 8 largest primary care facilities in Damascus between January and December 2017 and found that 79% had 5 or more ANC visits. The Atmeh study27 reviewed records of 730 women at the Syrian Expatriate Medical Association (SEMA) women’s and children’s health centre between October and December 2017. Of these women 39% received no ANC visits, 14% met the minimum requirements for the WHO four ANC visits (1 first trimester, 1 s trimester, 2 third trimester) and only 4% met the minimum requirements for the WHO ideal 8 visits (1 first trimester, 2 s trimester, 5 third trimester).
Quantitative analysis
Data were available for 24 facilities of which 7 were excluded leaving 17. Five were excluded because they did not routinely provide obstetric or newborn care but had performed one or two births under extenuating circumstances. Two other facilities were excluded after examination revealed that births performed at larger nearby hospitals were misattributed to them.
Descriptive analysis
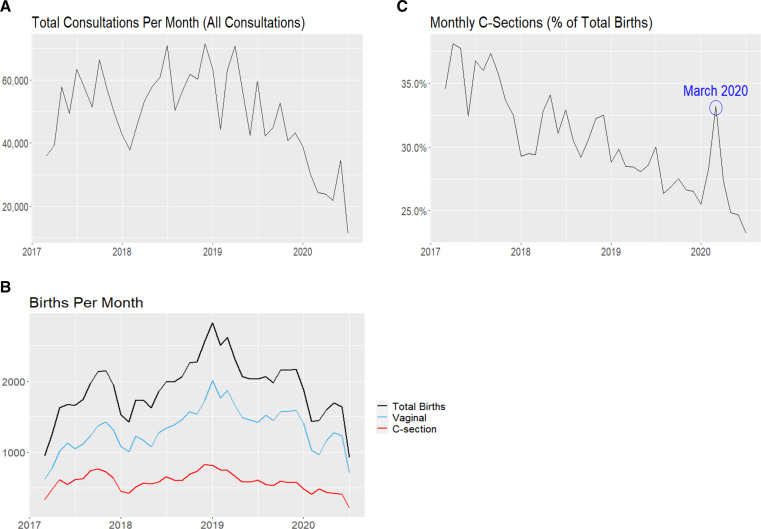
There were a total of 2 007 748 consultations (for all conditions) in SAMS’ facilities during the study period with a median of 50 398 (IQR: 40 820–59 637) consultations per month. There were 77 746 births with a median of 129 births per facility per month. Figure 2A shows the total consultations per month (for all presentations) of the study period and figure 2B shows the number of births by caesarean section and vaginal births.
Figure 2.
(A) This figure shows the total number of consultations (all presentations) per month between March 2017 and July 2020. (B) This figure shows the number of births per month delivered by caesarean sections or vaginal birth. In boxes are two time periods in which there are declines in the numbers of births. (C) This figure shows the caesarean section rates as a percentage of the total births across all SAMS’ health facilities per month between March 2017 and July 2020. SAMS, Syrian American Medical Society’s.
In figure 2A and a steep drop in the number of consultations is apparent starting in late 2017, as is a decline in the number of total monthly consultations from the end of 2019 and the beginning of 2020. Figure 2B shows that, in both time periods noted in figure 2A, there is a decline in total overall births. In the first time period at the end of 2017, the fall in the number of vaginal and caesarean section births was similar, however, given the overall lower numbers of caesarean section births, this resulted in a proportionately greater decrease in caesarean sections compared with the total number of births (corresponding to the dip in caesarean section rate seen in figure 2C). In the second time period in early 2020, figure 2B shows a sharper decrease in the number of vaginal births relative to caesarean sections, which only decreased slightly in accordance with the established trend causing the spike in caesarean section rates in March 2020 in figure 2C.
Types of births
The percentage of births by caesarean section varied throughout the study period. Figure 2C shows a general decline in the percentage caesarean section rate from around 37% in early 2017 towards less than 25% in the middle of 2020; with a sharp drop in the percentage of caesarean sections in late 2017 and peak in March 2020.
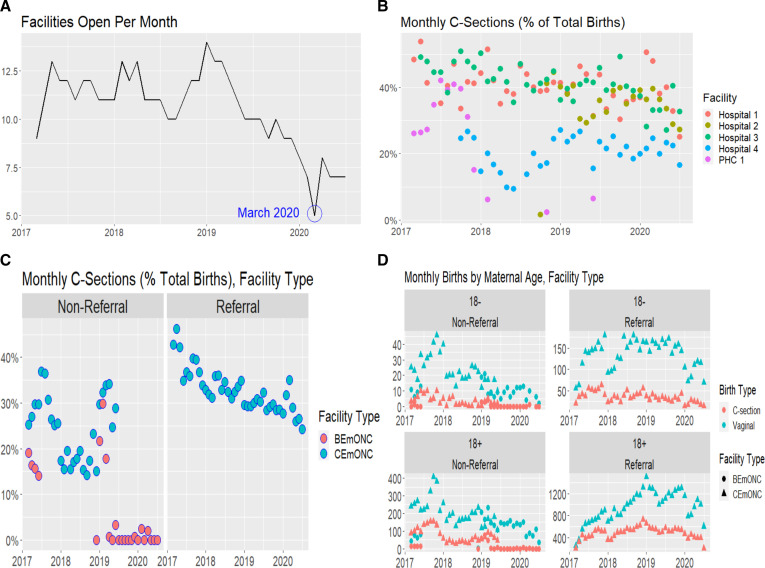
To explore whether the changes to the number of births related to a change in the number of open facilities, we plotted the number of open facilities each month, shown in figure 3A. A decline throughout 2019 is noted from a peak of 14 facilities in January 2019 to a low of 5 facilities in March 2020. The decreases in consultations seen in figure 2A in late 2017 and early 2020 correspond to reductions in functioning facilities in the same periods in figure 3A.
Figure 3.
(A) This figure shows the number of facilities open each month from March 2017 to July 2020. (B) This figure shows the monthly caesarean section proportions as a percentage of total births, for each of the five facilities which remained open in March 2020 and were functioning between March 2017 and July 2020. (C) This figure shows the percentage of births by caesarean section on a monthly basis in referral and non-referral hospitals and in BemONC and CEmONC facilities. (D) This figure shows the number of vaginal and caesarean section births in referral and non-referral facilities divided by age group, under 18 and 18 years and over. BemONC, basic emergency obstetric care; CEmONC, comprehensive obstetric care; PHC, primary healthcare centre.
To further investigate the peak in the proportion of caesarean sections in March 2020, we plotted the percentage of caesarean sections for the five facilities which remained open that month, see figure 3B. Hospital 1 and hospital 3 follow the same overall trend of all facilities with an overall decrease in caesarean section rate. However, their proportions were consistently higher than average, starting at 48.3% in hospital 1 and 48.9% in hospital 3 in March 2017 and ending at 25% in Hospital 1 and 32.6% in hospital 3 in July 2020. Hospital 2 also had a generally higher than average caesarean section proportion, although not as high as the previously mentioned hospitals. Hospital 4 maintained a steady, although lower, proportion of caesarean sections relative to the other facilities, except for a notable drop in mid 2018. Online supplemental table 4 appendix shows the catchment, total births in the time-period and mean monthly births for these five facilities.
Figure 3C compared caesarean section rates in facilities that received external referrals and those that did not. Caesarean section rates in referral facilities follow the same trend generally seen across all facilities with a steady decrease during the study period except for a peak seen in March 2020. However, in non-referral facilities there is no linear trend in caesarean section rates throughout the study period, although an overall decrease is nonetheless present. In non-referral hospitals, the percentage of births by caesarean section fell to zero in BEmONC facilities.
Underage pregnancies
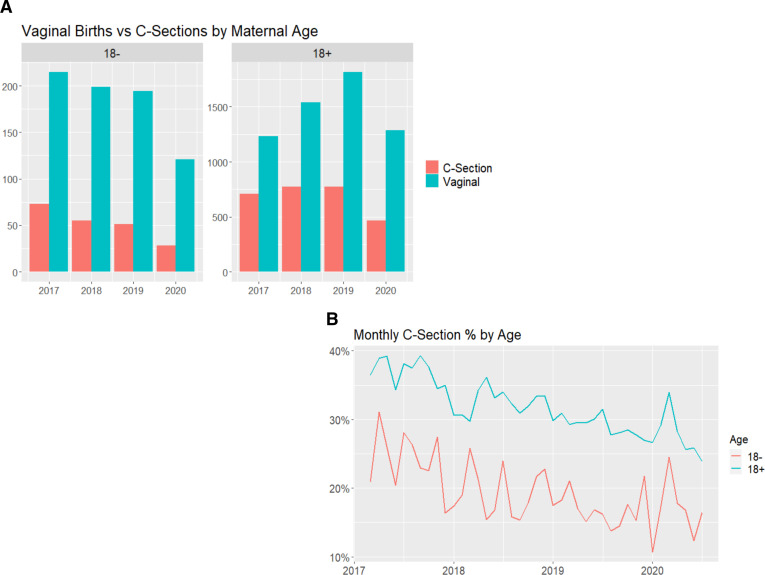
Of 77 746 births, 7946 (10.2%) were in girls under 18 years of age.
Figure 3D shows caesarean section rates in referral and non-referral facilities divided into pregnancies in those under 18 and those 18 years and over. In these figures, we can note that the referral facilities follow the same trends as seen in figure 2B. Though the non-referral facilities have less uniform trends, overall we can see that the number of births decreased throughout the study period. Trends in births by caesarean section in referral and non-referral facilities were similar in both age groups.
Figure 4A shows the number of caesarean section and vaginal births by maternal age; there is a decline in the number of vaginal and caesarean section births over the time period in the under 18 age group that is not evident among those 18 and over. Figure 4B compares the proportions of caesarean section births by maternal age. Here, it is evident that the proportion of caesarean section births in women under the age of 18 were consistently lower than in those over 18. While the trend in the proportion of caesarean sections in girls under 18 is more volatile due to the smaller number of births vs those over 18, the previously noted dip in late 2017 and peak in March 2020 are both still visible.
Figure 4.
(A) This figure shows the number of births by caesarean section or vaginal birth divided into those aged under 18 years or 18 years and over. (B) This figure shows the percentage of caesarean section births each month in women under 18 compared with women aged 18 years of age or over.
Discussion
The scoping literature review revealed limited information regarding maternal health in Syria after the onset of the conflict; of 21 including reports, most reported on single centres or made country-level generalisations with limited discussion of geographical disparities. Four main themes around maternal health in Syria were noted: maternal mortality, caesarean sections rates, underage pregnancies and PNC.
Key findings from the quantitative analysis of data of 77 746 births between March 2017 and July 2020 from SAMS’ facilities in northwest Syria show that the proportion of caesarean sections over time trended downward from 38% in April 2017 to 23% in July 2020. In addition, we highlight two prominent changes to the proportion of caesarean section births during the study period; one in late 2017 when the percentage of births by caesarean section dropped to 29.3% and the other in March 2020 when there was a steep peak in the percentage of caesarean section births from 26.5% to 33.2%. We also highlight of 77 746 births in SAMS facilities that 7946 (10.2%) were in girls under 18 years of age and that the proportion of caesarean section births in this age group was lower than in those aged 18 years and over throughout the time period.
Maternal mortality
MMR estimates varied widely in the literature from between 27 and 49 per 100 000 in 2010 to between 54.1 and 68 per 100 000 in 2015. Only country-level estimates were available. Besides potential inaccuracies in the recording of maternal deaths during conflict, we also highlight the need for more decentralised reporting of MMR given that the conflict has disparate effects on the different regions in Syria. Government controlled areas throughout the conflict may have been less affected by attacks on healthcare37 though services may have been degraded by insufficient resources, insufficient numbers of healthcare workers and now the impacts of the COVID-19 pandemic.38 Discrepancies in reporting on MMR and other indicators are noted internationally even in countries not facing conflict.39 However, given the weaknesses of international reporting systems on MMR, we call for improved reporting on maternal deaths, perhaps through MDSR (Maternal Death Surveillance and Response) systems; these did not exist robustly pre or post conflict onset40 but are key to accurate reporting and action regarding maternal mortality.
Proportion of births by caesarean section
In the literature review, caesarean section rates varied greatly across Syria and were almost all higher than the population level, WHO recommended 10%–15%.41 It is important to note that this recommendation refers to population rather than facility level with recent WHO statements noting the importance of appropriate caesarean section rates at a facility level.41 Of note, preconflict, caesarean section rates of up to 15% were reported in Syria.42 The variation across geographical areas was wide but the average caesarean section rate in northern Syria was 25% compared with 39% in Southern Syria with the highest caesarean section rates found in Lattakia (63.7%) and Tartous (58.7%), both government-controlled areas. This finding is notable considering that most areas in Southern Syria are under government control. There is little consensus on the effect of armed conflict on caesarean section rates; in some settings such as Columbia, caesarean section rates decreased in conflict-affected areas43 due to disruption of services, whereas in the Democratic Republic of Congo, caesarean section rates were higher in areas of armed conflict compared with the national average.44 In a review of obstetric care among refugees in sub-Saharan Africa and Asia, the overall caesarean section rate in the countries was low and it was even lower among those who had been forcibly displaced.45
In cases of protracted conflict, the destruction of health infrastructure reduces rates of institutional births and subsequently reduces the number of caesarean sections performed.46 However, it is possible that in Syria, although access to services has been compromised, the quality of healthcare provided for women who are able to deliver in healthcare facilities allows for higher rates of caesarean sections. One possible reason for this is scheduled caesarean sections that allow women and healthcare staff to decide on when the birth happens. The desire to reduce the amount of time women must be in hospital is a consequence of the targeted attacks on healthcare facilities that have made them unsafe places to reside.31 32 There is an evidence gap regarding the quality of decision making around caesarean sections in conflict and their impact on mortality; an MDSR system would allow better tracking of this.
From the SAMS quantitative analysis, there was also a large variation in caesarean section rates with changing trends over time. In particular, there was a fall in caesarean section rates in late 2017 from 37.3% to 29.3% and peak in March 2020 to 33.2%. The first notable decline seen in figure 2C in late 2017 is matched by a fall in consultations in the same period, as seen in figure 2A. In this time, both caesarean sections and vaginal births decreased by similar proportions; however, given the overall lower numbers of caesarean section births, this resulted in a relative decrease in the proportion of caesarean sections compared with the total number of births. In the same period in which the lowest proportion of caesarean sections were recorded, there was an escalation in violence in East Ghouta with aerial and chemical weapon attacks killing at least 2000 civilians and displacing a further 13 000.47 There was also a large-scale attack on Idlib in northwest Syria between October 2017 and February 2018 destroying six healthcare facilities and five white helmet centres.48 SAMS facilities were functioning in both of these areas during the period of attacks which may be the reason for the considerable drop in consultations and subsequently recorded births and caesarean section proportions during that time.
The peak in the proportion of caesarean sections in March 2020, from 26.5% to 33.2% in late 2019, occurred alongside a sharper decline in vaginal births (and total births) compared with caesarean sections. As such, though the proportion of caesarean sections increased, the total number of caesarean sections performed did not. This time period correlated with a steep reduction in the number of total monthly consultations, seen in figure 2A. The importance of this finding relates to a significant escalation of violence with increasing attacks by the Syrian government and its allies, such as Russia, on northwest Syria where SAMS facilities were located.49 Between December 2019 and February 2020, this escalation of violence forcibly displaced around one million people from their homes.50 51 Many were displaced away from facilities in which SAMS provided maternal healthcare and, as seen in figure 3A, there was a decline in the number of open facilities. Of the five facilities that remained open during March 2020, the majority had historically tended to have above-average caesarean section rates, as seen in figure 3B, contributing to the greater proportion of caesarean sections. Three of the five were larger CEmONC Referral Hospitals which would have received patients requiring caesarean sections sent from smaller facilities or presenting independently. Of the two other facilities, one was a PHC that performed fewer caesarean sections and fewer births overall, and the other was a maternity hospital in a more remote area that consequently received fewer transfers from other facilities.
Throughout the first half of the study period both referral and non-referral facilities, some of which were BEmONC facilities, were carrying out caesarean sections. However, towards the middle of 2019, non-referral CEmONC facilities were either downgraded to BEmONC facilities (as in most cases) or ended all obstetric care (or closed entirely). All remaining BEmONC facilities stopped performing caesarean sections completely. As a result, the caesarean sections proportions fell among non-referral facilities from mid-2019 onwards as seen in figure 3D. This is explained in more detail in online supplemental appendix.
Underage pregnancies
Pregnancy under the age of 19 years is a risk factor for obstetric complications.52 53 There is limited information in the literature regarding underage pregnancies, and it shows heterogeneity in the rates across the different regions of Syria. Our literature review suggested that one quarter of pregnant patients seen in a hospital in Idlib were under the age of 18.31 Armed conflict can increase the risk of violence against women who suffer due to the breakdown of social norms, destruction of health services and increased economic pressures. This puts women and girls at risk of rape, known to be used as a weapon in war,54 forced early marriage and sexual exploitation.55
From SAMS data, we note that 7946 (10.2%) of 77 748 total births were in girls aged under 18 years. Of note, the proportion of births by caesarean sections in girls under 18 was lower than those aged 18 years and over, and the trends in the two age groups broadly mirrored each other. Reasons for this could be that older patients may have had prior caesarean sections increasing their risk of a subsequent caesarean section. These findings mirror some studies56 but not others.57 A study from Ghana noted a higher risk of caesarean section and complications in girls aged 19 years and under with longer-term consequences for both mother and child.57
Perinatal care
Estimates of ANC visits and PNC coverage in Syria vary both before and during the conflict. Some sources suggest that the number of women attending at least one ANC visit was around 88% preconflict28 but that PNC coverage was only 27%.22 In the period after the uprising, ANC and PNC coverage has only been documented in specific regions, calculated based on attendance to specific facilities, rather than nationally. The proportion of women attending an adequate number of ANC visits varies by study and location with one study in Damascus reporting that 67.5% of women were attending four or more ANC visits25 and another reporting that 79% attended five or more.21 However, a study in Atmeh found that only 14% of women received four or more ANC visits.26
The estimates for the coverage by skilled health personnel at births also varies in the literature reportedly 96%22 28 prior to the conflict dropping to 72% in 201322 and as low as 25% in 2020.31
Limitations
Data were provided from SAMS’ facilities only; this accounted for a portion of the total number of facilities providing maternal healthcare in northwest Syria during the study period. We do not have accurate records as to the exact proportion, but it is estimated that 20% of health services in the northwest were by SAMS. We; therefore, do not have data for other agencies and different geographic areas in Syria. These data were collected during active conflict, therefore, there may be inaccuracy in recording, missing data or misdiagnosis due to inadequate resources or experienced staff. Furthermore, as is common in many humanitarian settings with restrictions to data collection58 59 it is not possible to analyse certain maternal health parameters, however, this work remains an important addition to the literature looking at underage pregnancies and caesarean sections in conflict settings. The changes to presentations to facilities as a result of episodes of increased conflict or other factors which influence healthcare access may also falsely skew the data.
Conclusion
We note a dearth of literature which explores maternal health in postconflict Syria. Identified literature, particularly around MMR, makes country-level generalisations when the variable effects of conflict across different regions require more granular investigation; this is particularly so given the fragmented nature of Syria’s health system. As such, future research which explores variations in maternal care in micro-contexts across Syria is required. In addition, research which explores the drivers of caesarean sections during conflict and the relationship between conflict, modes of birth and outcomes is required both in Syria and in the context of conflicts elsewhere. Our quantitative analysis using SAMS’ data (despite limitations) provides a useful addition to the literature around fluctuations in the proportion of caesarean section births and underage pregnancies during conflict in one of the largest available cohorts from the northwest of Syria.
Acknowledgments
We would like to thank the staff in SAMS’s offices and in the health information system team who were involved in the collection of the data.
Footnotes
Handling editor: Seema Biswas
Twitter: @fares_alahdab, @AulaAb
Contributors: AAi, MoH and MWA conceptualised and designed the study. SB and AS analysed the data under the guidance of AAi, MoH and MWA. SB, AAi, MWA, AS and MoH wrote the first draft of the manuscript and AAb, IH, AT, MuH, RL, FA and MK all edited and inputted heavily into the writing and editing. AA takes overall responsibility for the work conducted in the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Data used in this study are anonymised, aggregated data on consultations relating to maternal health and the total number of monthly consultations from 17 of SAMS’ (Syrian American Medical Society) health facilities in northwest Syria. Data requests can be made to the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Only anonymised data collected for routine clinical purposes and monitoring and evaluation were included; it was provided as aggregated monthly data. This was assessed and approved by SAMS’ research committee. A formal ethics review was therefore not required.
References
- 1.Bendavid E, Boerma T, Akseer N, et al. The effects of armed conflict on the health of women and children. Lancet 2021;397:522–32. 10.1016/S0140-6736(21)00131-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United Nations Children’s Fund (UNICEF) . The impact of conflict on women and girls in West and central Africa and the UNICEF response. New York, 2005. [Google Scholar]
- 3.Boerma T, Tappis H, Saad-Haddad G, et al. Armed conflicts and national trends in reproductive, maternal, newborn and child health in sub-Saharan Africa: what can National health surveys tell us? BMJ Glob Health 2019;4:e001300. 10.1136/bmjgh-2018-001300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Namasivayam A, Arcos González P, Castro Delgado R, González P, Delgado R, et al. The effect of armed conflict on the utilization of maternal health services in Uganda: a population-based study. PLoS Curr 2017;9. 10.1371/currents.dis.557b987d6519d8c7c96f2006ed3c271a. [Epub ahead of print: 03 Oct 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karroum L, El-Harakeh A, Kassamany I. Health care workers in conflict and Post-Conflict settings: systematic mapping of the evidence. SSRN Elect J 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akseer N, Wright J, Tasic H, et al. Women, children and adolescents in conflict countries: an assessment of inequalities in intervention coverage and survival. BMJ Glob Health 2020;5:e002214. 10.1136/bmjgh-2019-002214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Syria Relief. 9 Years of Schools on the Front Line: The Impact of Airstrikes on Syria’s Schools [Internet], 2020. Available: https://reliefweb.int/sites/reliefweb.int/files/resources/No-School-Report.v02.pdf
- 8.Ri S, Blair AH, Kim CJ, et al. Attacks on healthcare facilities as an indicator of violence against civilians in Syria: an exploratory analysis of open-source data. PLoS One 2019;14:e0217905. 10.1371/journal.pone.0217905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.A Map of Attacks on Health Care in Syria [Internet]. Syriamap.phr.org, 2020. Available: http://syriamap.phr.org/#/en/findings
- 10.Cheung F, Kube A, Tay L. The impact of the Syrian conflict on population well-being. Nat Commun [Internet], 2020. Available: https://www.nature.com/articles/s41467-020-17369-0#citeas [DOI] [PMC free article] [PubMed]
- 11.International Committee of the Red Cross. Syria: Economic crisis compounds conflict misery as millions face deeper poverty, hunger [Internet], 2021. Available: https://reliefweb.int/report/syrian-arab-republic/syria-economic-crisis-compounds-conflict-misery-millions-face-deeper
- 12.United Nations Office for the Coordination of Humanitarian Affairs . Humanitarian Update Syrian Arab Republic [Internet], 2020. Available: https://reliefweb.int/sites/reliefweb.int/files/resources/HUMANITARIAN%20UPDATE%20NO.%209.pdf
- 13.REACH . northwest Syria: Situation Overview - 16 March 2020 [Internet], 2020. Available: https://reliefweb.int/sites/reliefweb.int/files/resources/REACH_SYR_Situation-Overview_northwest-Syria_16-March-2020-1.pdf(x2)
- 14.World Health Organisation . Monitoring emergency obstetric care A Handbook [Internet]. France, 2009. Available: https://www.unfpa.org/sites/default/files/pub-pdf/obstetric_monitoring.pdf
- 15.Cuesta JG, Trelles M, Naseer A, et al. Does the presence of conflict affect maternal and neonatal mortality during caesarean sections? Public Health Action 2019;9:107–12. 10.5588/pha.18.0045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hakeem O, Jabri S. Adverse birth outcomes in women exposed to Syrian chemical attack. Lancet Glob Health 2015;3:e196. 10.1016/S2214-109X(15)70077-X [DOI] [PubMed] [Google Scholar]
- 17.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet 2014;384:980–1004. 10.1016/S0140-6736(14)60696-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khachfe HH, Sammouri J, Salhab HA, et al. Maternal mortality and health in the Arab world: a 25-year epidemiological study. J Obstet Gynaecol Res 2019;45:2369–76. 10.1111/jog.14119 [DOI] [PubMed] [Google Scholar]
- 19.GBD 2015 Eastern Mediterranean Region Maternal Mortality Collaborators . Maternal mortality and morbidity burden in the eastern Mediterranean region: findings from the global burden of disease 2015 study. Int J Public Health 2018;63:47–61. 10.1007/s00038-017-1004-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nahidi F, Hajifoghaha M. Maternal mortality ratio in eastern Mediterranean region: a priority of reproductive health. Int J Women’s Health Reprod Sci 2017;8:1–9. 10.15296/ijwhr.2020.01 [DOI] [Google Scholar]
- 21.Roumieh M, Bashour H, Kharouf M, et al. Prevalence and risk factors for postpartum depression among women seen at primary health care centres in Damascus. BMC Pregnancy Childbirth 2019;19:519. 10.1186/s12884-019-2685-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeJong J, Ghattas H, Bashour H, et al. Reproductive, maternal, neonatal and child health in conflict: a case study on Syria using countdown indicators. BMJ Glob Health 2017;2:e000302. 10.1136/bmjgh-2017-000302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Hammami H. Prevalence of cesarean section at ALTAWLID Hospital during the Syrian crisis. JMPAS 2018;6:947–53. 10.22270/jmpas.v6i12.746 [DOI] [Google Scholar]
- 24.Aburas R, Najeeb A, Baageel L, et al. The brotherhood medical center: collaborative Foundation of maternity and children's healthcare facility for displaced Syrians. Front Public Health 2018;6:108. 10.3389/fpubh.2018.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kabakian-Khasholian T, Bashour H, El-Nemer A, et al. Women's satisfaction and perception of control in childbirth in three Arab countries. Reprod Health Matters 2017;25:16–26. 10.1080/09688080.2017.1381533 [DOI] [PubMed] [Google Scholar]
- 26.Terkawi AS, Bakri B, Alsadek AS, et al. Women's health in northwestern Syria: findings from Healthy-Syria 2017 study. Avicenna J Med 2019;9:94. 10.4103/ajm.AJM_190_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alsharif N, Alhomsi K. The increasing ratio of cesarean section births: causes and implications. European J Biomed Pharm Sci 2020;7:504–7. [Google Scholar]
- 28.Abdelgawad A. The association between health financing and maternal and child health in middle East and North Africa countries, 2020. Available: http://dar.aucegypt.edu/handle/10526/4253 [Accessed 26 Jul 2020].
- 29.World Health Organization . Trends in maternal mortality: 1990 to 2015, 2015. [Google Scholar]
- 30.World Health Organization . Trends in maternal mortality: 2000 to 2017, 2019. [Google Scholar]
- 31.Human Appeal . Risking death to give birth: the consequences of conflict on the health needs of women and girls in Syria, 2020. Available: https://reliefweb.int/report/syrian-arab-republic/risking-death-give-birth-consequences-conflict-health-needs-women-and [Accessed 26 Jul 2020].
- 32.Syrian American Medical Society . Disrupted health care in Syria: the state of reproductive health, 2019. Available: https://reliefweb.int/report/syrian-arab-republic/disrupted-health-care-syria-state-reproductive-health [Accessed 26 Jul 2020].
- 33.United Nations Population Fund . Regional situation report for Syria crisis, 2017. Available: https://www.unfpa.org/resources/regional-situation-report-syria-crisis-54-1-28-february-2017 [Accessed 26 Jul 2020].
- 34.Médecins Sans Frontières . International activity report 2015. Available: https://www.msf.org.uk/sites/uk/files/international_activity_report_2015_en_0.pdf [Accessed 26 Jul 2020].
- 35.World Health Organization, . HeRAMS Annual Report: January - December 2015 Public Hospitals In The Syrian Arab Republic, 2015. Available: https://reliefweb.int/report/syrian-arab-republic/herams-annual-report-january-december-2015-public-hospitals-syrian-arab [Accessed 26 Jul 2020].
- 36.World Health Organisation . Maternal mortality in 2000-2017: Internationally comparable MMR estimates by the Maternal Mortality Estimation Inter-Agency Group (MMEIG) WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division [Internet], 2019. Available: https://www.who.int/gho/maternal_health/countries/syr.pdf?ua=1
- 37.Fouad FM, Sparrow A, Tarakji A, et al. Health workers and the weaponisation of health care in Syria: a preliminary inquiry for the Lancet-American University of Beirut Commission on Syria. Lancet 2017;390:2516–26. 10.1016/S0140-6736(17)30741-9 [DOI] [PubMed] [Google Scholar]
- 38.Ali H. COVID-19 and civil wars in the Arab world: the cases of Syria, Libya and Yemen. Asian Aff 2020;51:838–55. 10.1080/03068374.2020.1837540 [DOI] [Google Scholar]
- 39.Boerma T, Mathers CD. The world Health organization and global health estimates: improving collaboration and capacity. BMC Med 2015;13:50. 10.1186/s12916-015-0286-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organisation . Maternal Death Surveillance and Response country profiles [Internet], 2015. Available: https://cdn.who.int/media/docs/default-source/mca-documents/maternal-death-surveillance-and-response-country-profiles.pdf?sfvrsn=37a3cc21_1&download=true
- 41.World Health Organisation . WHO Statement on caesarean Section Rates [Internet], 2015. Available: https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf;jsessionid=D115090500655BA74017B0F8743139D1?sequence=1
- 42.Jurdi R, Khawaja M. Caesarean section rates in the Arab region: a cross-national study. Health Policy Plan 2004;19:101–10. 10.1093/heapol/czh012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramos Jaraba SM, Quiceno Toro N, Ochoa Sierra M, et al. Health in conflict and post-conflict settings: reproductive, maternal and child health in Colombia. Confl Health 2020;14:33. 10.1186/s13031-020-00273-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mulinganya G, Bwenge Malembaka E, Lukula Akonkwa M, et al. Applying the Robson classification to routine facility data to understand the caesarean section practice in conflict settings of South Kivu, eastern DR Congo. PLoS One 2020;15:e0237450. 10.1371/journal.pone.0237450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hesham H, Hesham M, Goodman A. Obstetric care among refugees: the complex interplay of barriers to care, culture, health resources and the healthcare infrastructure of host countries. Open J Obstet Gynecol 2019;09:170–85. 10.4236/ojog.2019.92018 [DOI] [Google Scholar]
- 46.Østby G, Urdal H, Tollefsen AF, et al. Organized violence and institutional child delivery: Micro-Level evidence from sub-Saharan Africa, 1989-2014. Demography 2018;55:1295–316. 10.1007/s13524-018-0685-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Syrian American Medical Society Foundation . SAMS 2018 Annual Report [Internet], 2019. Available: https://reliefweb.int/sites/reliefweb.int/files/resources/SAMS-Annual-Report-2018-V5-compressed.pdf [Accessed 26 Feb 2021].
- 48."Targeting Life in Idlib" [Internet]. Human Rights Watch, 2021. Available: https://www.hrw.org/report/2020/10/15/targeting-life-idlib/syrian-and-russian-strikes-civilian-infrastructure#_ftn17
- 49.Congressional Research Service . Armed Conflict in Syria: Overview and U.S. Response [Internet], 2020. Available: https://fas.org/sgp/crs/mideast/RL33487.pdf [Accessed 26 Feb 2021].
- 50.Abbara A, Rayes D, Khalil M, et al. Humanitarian catastrophe for civilians in northwest Syria. BMJ 2020;368:m451. 10.1136/bmj.m451 [DOI] [PubMed] [Google Scholar]
- 51.Idlib Between September 2015 and May 2020: A Timeline [Internet]. International Crisis Group, 2022. Available: https://www.crisisgroup.org/middle-east-north-africa/eastern-mediterranean/syria/idlib-between-september-2015-and-may-2020-timeline
- 52.Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, et al. Maternal age and risk of labor and delivery complications. Matern Child Health J 2015;19:1202–11. 10.1007/s10995-014-1624-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marvin-Dowle K, Kilner K, Burley VJ, et al. Impact of adolescent age on maternal and neonatal outcomes in the born in Bradford cohort. BMJ Open 2018;8:e016258. 10.1136/bmjopen-2017-016258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wagner Z, Heft-Neal S, Wise PH, et al. Women and children living in areas of armed conflict in Africa: a geospatial analysis of mortality and orphanhood. Lancet Glob Health 2019;7:e1622–31. 10.1016/S2214-109X(19)30407-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Neal S, Stone N, Ingham R. The impact of armed conflict on adolescent transitions: a systematic review of quantitative research on age of sexual debut, first marriage and first birth in young women under the age of 20 years. BMC Public Health 2016;16:225. 10.1186/s12889-016-2868-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Indarti J, Al Fattah AN, Dewi Z, et al. Teenage pregnancy: obstetric and perinatal outcome in a tertiary centre in Indonesia. Obstet Gynecol Int 2020;2020:1–5. 10.1155/2020/2787602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yussif A-S, Lassey A, Ganyaglo GY-K, et al. The long-term effects of adolescent pregnancies in a community in northern Ghana on subsequent pregnancies and births of the young mothers. Reprod Health 2017;14:178. 10.1186/s12978-017-0443-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Strongman H, Williams R, Meeraus W, et al. Limitations for health research with restricted data collection from UK primary care. Pharmacoepidemiol Drug Saf 2019;28:777–87. 10.1002/pds.4765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Panhuis WG, Paul P, Emerson C, et al. A systematic review of barriers to data sharing in public health. BMC Public Health 2014;14:1144. 10.1186/1471-2458-14-1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-008001supp001.pdf (336.8KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data used in this study are anonymised, aggregated data on consultations relating to maternal health and the total number of monthly consultations from 17 of SAMS’ (Syrian American Medical Society) health facilities in northwest Syria. Data requests can be made to the corresponding author.