Abstract
Introduction
Sedation and analgesia are recommended to be employed in the intensive care unit (ICU) to enhance patient comfort and safety, facilitate mechanical ventilation and reduce oxygen demands. However, the increasing evidence demonstrates that excessive sedation and analgesia might prolong mechanical ventilation and increase costs and mortality. Acupuncture is known to be able to attenuate pain, anxiety and agitation symptoms while avoiding excessive sedation and analgesia caused by drugs. Therefore, we present a protocol to investigate whether acupuncture, used for sedation and analgesia, can reduce the duration of mechanical ventilation, save medical resources and reduce the mortality of critically ill patients receiving mechanical ventilation.
Methods and analysis
Prospective, randomised controlled trial is conducted on 180 adult medical/surgical ICU patients with mechanical ventilation needing sedation at 3 ICUs between 03 November 2021 and 16 August 2023. Patients will be treated with analgesia and sedation to achieve desired target sedation levels (Richmond Agitation Sedation Score of −2 to 1). Enrolled patients will be randomly assigned in a ratio of 1:1:1 to receive deep needle insertion with combined manual and alternating-mode electrical stimulation on acupoints (AC group), superficial needle insertion without manual stimulation and electrical stimulation on non-acupoints (SAC group), or no acupuncture intervention (NAC group). The primary outcome is the duration of mechanical ventilation from randomisation until patients are free of mechanical ventilation (including non-invasive) without reinstitution for the following 48 hours. Secondary endpoints include the dose of administered sedatives and analgesic at comparable sedation levels throughout the study, ICU length of stay, hospital length of stay. Additional outcomes include the prevalence and days of delirium in ICU, mortality in ICU and within 28 days after randomisation, and the number of ventilator free days in 28 days.
Ethics and dissemination
This trial was approved by the ethics committee at Guangdong Provincial Hospital of Chinese Medicine. We will publish the study results.
Trial registration number
ChiCTR2100052650.
Keywords: adult intensive & critical care, adult anaesthesia, pain management
Strengths and limitations of this study.
This study is an randomised controlled trial to investigate both the sedative and analgesic effects of acupuncture on critically ill patients needing mechanical ventilation in intensive care unit (ICU).
This study provides a sedative and analgesic strategy for mechanically ventilated critically ill patients with less side effects.
The primary endpoint is the duration of mechanical ventilation from randomisation until patients are free of mechanical ventilation (including non-invasive) without reinstitution for the following 48 hours.
Secondary endpoints include the dose of administered sedatives and analgesics at comparable sedation levels throughout the study, ICU length of stay, and hospital length of stay.
Limitations are the non-blinded interventions due to the nature of acupuncture.
Introduction
Sedative and analgesic medications are routinely administered to mechanically ventilated critically ill patients to reduce pain, anxiety and agitation, as well as to allow patients to tolerate invasive procedures in the intensive care unit (ICU).1 Opiates are most commonly used analgesics, while benzodiazepines, propofol, or dexmedetomidine are typically used to prevent or reduce anxiety and agitation.2 However, overuse of these medications is associated with worsened clinical outcomes, such as prolonged mechanical ventilation and hospital length of stay, increased risk of altered mental status, and even higher mortality.3 Thus, reducing the unnecessary dosage of sedative and analgesic medications, as well as their side effects while providing desired sedation has always been a key objective when caring for critically ill patients.
As a therapeutic modality with fewer adverse effects, acupuncture has been used in China and other Asian countries for thousands of years to treat various conditions.4–6 Studies of acupuncture usually focuses on its analgesic effect, such as relieving pain and partly reducing opioid-related side effects during or after surgical procedures.7–11 Particularly, the Centers for Medicare & Medicaid Services of the USA finalises a decision to cover acupuncture for chronic low back pain for Medicare beneficiaries in January 2020. Moreover, some studies have investigated the use of acupuncture on reducing sedative and analgesic drug demands, and the duration of mechanical ventilation, while improving patients’ experience during mechanical ventilation.12–15 However, there are still a few discrepant research findings on the sedative and analgesic effects of acupuncture.16 17 And studies investigating both the sedative and analgesic effects of acupuncture among all critically ill patients needing mechanical ventilation in ICU are limited.
Therefore, the PASSION (Prospective comparison of Acupuncture with Sham acupuncture to determine impact on SedatIOn and analgesia in mechaNically ventilated patients) study is designed to be an RCT which investigate the efficacy of acupuncture on sedation and analgesia in mechanically ventilated critically ill patients. We are going to test the hypothesis that acupuncture, as adjunctive therapy to sedation and analgesia therapies, could reduce the duration of mechanical ventilation, the dose of administered sedatives and analgesics, and subsequently improve other clinical outcomes for critically ill patients when compared with sham acupuncture or non-acupuncture.
Methods
Study design overview
This is a prospective, parallel-group, controlled trial will recruit 180 patients with a computer-generated allocation sequence and centralised randomisation at tertiary and regional ICUs in 3 hospitals (Guangdong Provincial Hospital of Chinese Medicine, Charity Hospital of Guangzhou, University Hospital) in South China. Recruitment officially began on 3 November 2021, and the final follow-up of the last subject will not exceed 16 August 2023. Eligible patients will be randomly assigned, in a ratio of 1:1:1, to receive deep needle insertion with combined manual and alternating-mode electrical stimulation on acupoints (AC group, n=60), superficial needle insertion without manual or electrical stimulation on non-acupoints (SAC group, n=60) for 30 min/day, or no acupuncture intervention (NAC group, n=60), respectively.
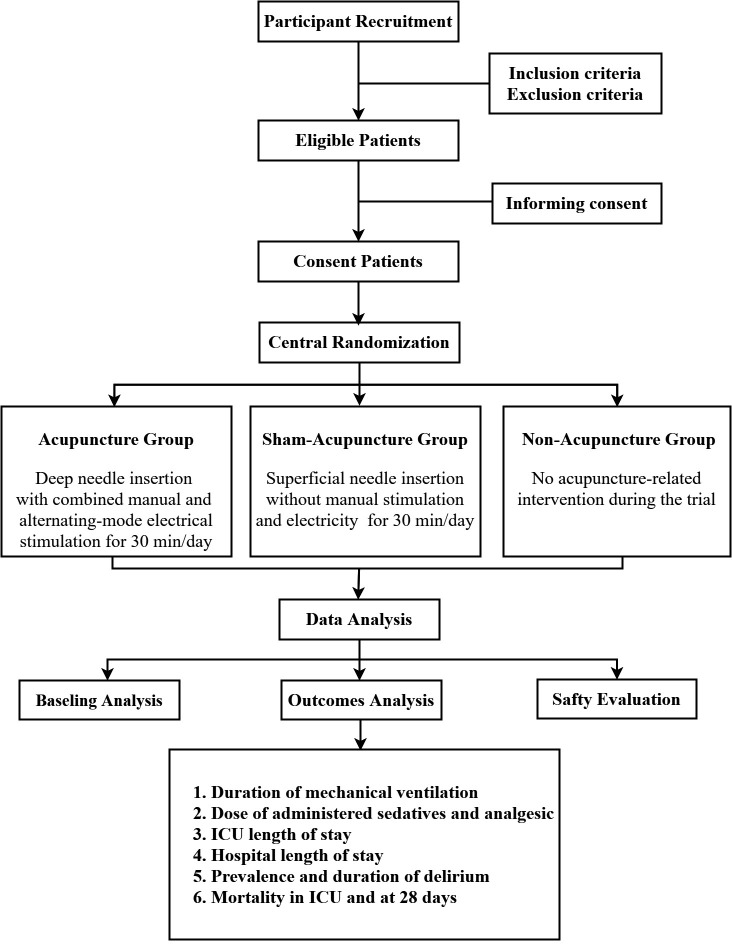
Participants will be assessed for the duration of mechanical ventilation, as well as the dose of administered sedatives and analgesics at comparable sedation levels, from randomisation until patients are free of mechanical ventilation (including non-invasive) without reinstitution for the following 48 hours. They will be also assessed for whether acupuncture can achieve better clinical outcomes than SAC and NAC treatment. The design of the trial is summarised in figure 1.
Figure 1.
Trial design of PASSION study.
Ethical requirements and registration
This protocol is approved by the Institutional Human Clinical Research Ethical Committee at Guangdong Provincial Hospital of Chinese Medicine (Guangzhou, China) in October 2021 with permission number ZF2021-144-01. The PASSION study was registered on 3 November 2021 (ClinicalTrials.gov, number ChiCTR2100052650) and will be conducted following the Declaration of Helsinki from 3 November 2021 to 16 August 2023.
Written informed consent will be provided before enrollment voluntarily. Considering that patients will be sedated following ICU admission, complete adherence to patient consent is deemed impossible. Patients or their authorised surrogates will be informed by the researchers of the investigational nature and details of the study, together with the possible risks and all the benefits. Written informed consent will be subsequently obtained from either of them. Patients from whom surrogate consent is obtained are asked again to provide informed consent once determined to be competent. They can also withdraw from the study at any time they wish. Also, the investigator can decide to withdraw a subject from the study for urgent medical reasons. The researcher should complete the case report form and record the reason for dropping out.
Patients
Patients from medical and surgical ICU, ageing from 18 to 80 years, for expected mechanical ventilation longer than 24 hours, with agitation and/or discomfort after recovering from drugs used to facilitate endotracheal intubation, requiring sedation and agitation by continuous intravenous administration deemed by the ICU physician, are eligible for participation as soon as they or their authorised surrogates are willing to give informed consent (table 1).
Table 1.
Inclusion and exclusion criteria
| A. Inclusion criteria | B. Exclusion criteria |
| 1. Aged 18 years or over and under 80 years; | 1. Skin lesions near the acupuncture points; |
| 2. Required mechanical ventilation>24 hours; | 2. Coagulopathy (bleeding time>4 min, thrombocytes<50 000/μl; |
| 3. Continuous intravenous administration of sedative and analgesic medications; | 3. Hypohepatia with Childs-Pugh class B or C; |
| 4. Willingness to provide informed consent prior to enrollment; | 4. Second-degree or third-degree atrioventricular block; |
| 5. Be able to comply with all follow-up evaluations (in investigator’s opinion). | 5. Severe dementia; |
| 6. Psychiatric disorder; | |
| 7. Neurological disease; | |
| 8. Active seizures; | |
| 9. Alcohol or drug abuse; | |
| 10. Benzodiazepine dependency; | |
| 11. Moribund state with the planned withdrawal of life support; | |
| 12. Family or physician refusal; | |
| 13. Pregnancy or lactation; | |
| 14. Currently participated in any other investigational therapeutic or device trial. |
Exclusion criteria include skin lesions near the acupuncture points, coagulopathy (bleeding time>4 min, thrombocytes<50 000/μL), neurological disease (previous stroke, cerebral palsy, etc.) that would confound the diagnosis of delirium, active seizures, severe dementia, relevant psychiatric disorder, hypohepatia with Childs-Pugh class B or C, second-degree or third-degree atrioventricular block, alcohol or drug abuse, benzodiazepine dependency, a moribund state with the planned withdrawal of life support, family or physician refusal, pregnancy or lactation, currently participating in any other investigational therapeutic or device trial (table 1).
ICU standard treatment
As a standard in each ICU of our study, mechanically ventilated critically ill patients will be treated in a single treatment room. They will be taken care of by a trained ICU physician responsible for all treatment decisions, including sedation analgesia management plans made in consultation with the bedside nurses. They will also receive one-to-one nursing care to adjust the treatment based on the patient’s response in time. A team of medical officers will review patient care every day.
Randomisation and blinding
Eligible patients will be stratified by participating sites to avoid patient-level contamination from the systems-level organisational change in sedation practice and, within each ICU, assigned to the AC, SAC, or NAC group in an equal ratio via computer-generated randomisation. In detail, an independent study coordinator will log into the central randomisation system using a password-protected account and enter inclusion and exclusion criteria to ensure eligibility. After entering a patient’s name and identification card number, a randomisation sequence will be generated in blocks of varying sizes and stratified by the site under the control of the central computer system. The random sequence will then be concealed in sealed envelopes and sent to an acupuncturist from the assigned patient’s site by the study coordinator.
Allocation of participants will be known to the study coordinator and acupuncturists who will not be involved in outcome assessment and be required to sign a confidentiality agreement about patient allocation. All patients will be treated in a single treatment room. In both AC and SAC groups, patients, bedside nurses and physicians will be blinded to which acupuncture method the patients will receive. The data collectors and the biostatisticians will be masked from the treatment assignment.
Acupuncture interventions and procedures
The acupuncture interventions will be developed by a consensus of acupuncture experts according to the Standards for Reporting of Controlled Trials in Acupuncture (STRICTA).18 Patients will be assigned in a ratio of 1:1:1 to AC group (n=60), SAC group (n=60), and NAC group (n=60). Besides, each group shares the same basic Sedation Analgesia Strategy.
For patients in the AC group, eight disposable sterile acupuncture needles (filiform needles made of stainless steel, Beijing Hanyi Medical Instruments, China) with a length of 40 mm and a diameter of 0.30 mm will be inserted into acupuncture points at Baihui (DU20), Yintang (EX-HN3), and bilateral acupoints of Shenmen (HT7), Hegu (LI4), Taichong (LR3) according to the theory of traditional Chinese medicine. The localisation of these points is measured with a unit of cun, a traditional Chinese unit of length. One cun of a person is defined as the width of the thumb himself, whereas four fingers are defined as 3 cun. The insertion will be followed by manual stimulation, a lifting and thrusting technique combined with twirling and rotating the needle sheath to produce a sensation of soreness, numbness, distention, or radiating. This sensation is known as ‘Deqi’ and is considered to be indicative of effective needling. Then, alternating-mode electrical stimulation will be given with the parameters: bursts alternating at 2 Hz and 100 Hz every 3 s, with 10–15 mA intensity inducing no discomfort and no muscle contraction.
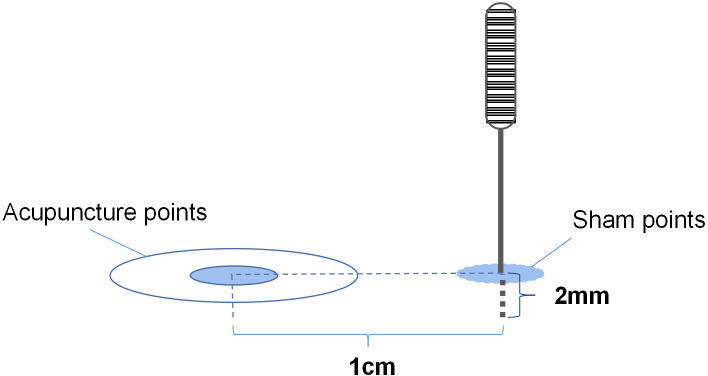
For patients in the SAC group, superficial needle insertion with a depth of 2 mm and no manual stimulation will be performed for 30 min/day. The same sort of needles with the AC group will be placed 1 cm distant lateral the used acupoints that are not known as AC points. The electrical stimulator will likewise be connected but without electrical stimulation (figure 2).
Figure 2.
Illustration of the sham points.
Patients in the NAC group will receive no acupuncture-related intervention during the trial. But they can receive a free 12-session daily acupuncture treatment after completing the study at their convenience.
Each site will be required to have two licensed acupuncturists with more than 3 years of experience and specialised training in the acupuncture protocols before starting the study. The acupuncturists will be responsible for the whole acupuncture process but are not further involved in this study.
Basic sedation analgesia strategy
In this study, diagnosis and therapeutic management of agitation and pain will be prescribed by the physicians responsible for the clinical care of each patient according to recommended guidelines.19 An interruptive sedation strategy will be adopted by bedside nurses, and sedation levels and pain intensity will be assessed with the Richmond Agitation Sedation Scale (RASS),20 21 the Behavioural Pain Scale (BPS), or the Numeric Rating Scale (NRS)22 23 every 4 hours in order to adapt sedatives and analgesics to avoid overuse. Authorised nurses will titrate infusions, including benzodiazepines, propofol and dexmedetomidine for sedatives and opiates for analgesia, instead of bolus dosing to minimise potential adverse effects.
The sedation analgesia strategy is designed to consider pain treatment before increasing sedatives to minimise the risk of oversedation. The pain will be assessed either by the BPS in patients unable to communicate or by the NRS, a 1–10 NRS, in those sufficiently oriented and awake to communicate with the medical staff. Efficacy of the study analgesics drug will be defined as the ability to achieve a score<3 in both of the pain scoring systems above, evaluated by the bedside nurse. Efficacy of the sedative drug will be defined as the ability to achieve a sedation score between −2 and 1, set by the patient’s medical team using the RASS (a highly reliable and well-validated sedation scale for use within patients) over time in the ICU.
Each morning, a daily interruption of sedation (DIS) will be performed at the clinical medical team’s discretion. Major opioid infusions needed for active pain will be continued. Recommended criteria to interrupt sedation are used: no drug-induced paralysis, no intracranial hypertension, no myocardial ischaemia in the previous 24 hours, primary disease healing in progress, haemodynamic stability, the partial pressure of arterial oxygen≥60 mm Hg, the fraction of inspired oxygen≤50%, and positive end-expiratory pressure≤8 cmH2O. The interruption of continuous sedation will be coupled with an assessment hourly for wakefulness, defined as the RASS score 1–4, and the ability to perform at least 3 of the following requests: eye-opening, tracking, hand squeezing and toe moving. With the criteria recommended, patients will be able to pass the DIS if they can tolerate it for 4 hours and keep awakening enough. Then, a spontaneous breathing trial (SBT) will immediately be managed.24 If patients are insufficient for the DIS, sedatives will be restarted at half the previous dose and then titrated to achieve patient comfort. DIS will be performed the next morning again.
Extubation test
Before extubation, patients will be managed with an SBT. During the SBT, without ventilatory support, patients will be allowed to breathe through a ventilatory circuit with 8 cm H2O PSV, 0 PEEP and unchanged FiO2 from the mechanical ventilation period leading up to the SBT.25 The criteria for a successful SBT are respiratory rate between 8 and 35 breaths/min, arterial oxygen saturation>88%, less than 20% change in mean arterial pressure or heart rate, no signs of respiratory distress and acute cardiac arrhythmia, no use of accessory muscles, no abdominal paradox, absence of sweating, agitation or impaired vigilance status. Patients will pass the SBT if they complete a 60 min trial meeting the criteria, and extubation will be implemented 6 hours later. Patients who fail the SBT will be ventilated immediately with the ventilator settings used before the trial, and sedatives will be restarted at half the previous dose and then titrated to achieve patient comfort. The SBT will be managed the next morning again. Extubation will be implemented following standardised criteria, but the decision to extubate remains on the authority of the attending physician in charge of the patient. Researchers will not participate in decisions to extubate patients.
The clinical research team will make sure that the overall research protocol, especially the criteria for sedation and definition of successful SBT, is strictly followed by the bedside nurse and medical teams in charge of the patients. Related information will be reported on the clinical research form.
Assessing delirium
Delirium will be measured by the bedside nurses according to the Confusion Assessment Method for the ICU (CAM-ICU) until out of ICU or hospital discharge.26 Patients will be considered in this state if they have a RASS score ≥−3 and a positive CAM-ICU, defined as positive with the symptoms of feature 1, feature 2 and either feature 3 or feature 4 as follows:
Feature 1: acute onset of mental status change or fluctuation of mental status.
Feature 2: inattention.
Feature 3: disorganised thinking.
Feature 4: altered level of consciousness.
Adverse event monitoring
Adverse events will also be defined a priori and prospectively monitored. Adverse events associated with acupuncture include bleeding, haematoma and local infection. Adverse events related to sedation and analgesia include inadequate pain and sedation management (either pain score>4 and RASS>1 for 2 consecutive hours or pain and agitation assumed present if receiving neuromuscular blockade), clinically significant iatrogenic withdrawal. Adverse events associated with mechanical ventilation include accidental removal of medical devices, extubation failure (reintubation within 24 hours), pressure ulcers, catheter-associated bloodstream infections, ventilator-associated pneumonia. Every day, research personnel will monitor and assess the seriousness of all adverse events and document all details to determine whether the events are related to acupuncture interventions or the study procedure, as well as developing further treatment strategies including whether it is necessary to uncover blindness. A report of all serious, unexpected and study-related adverse events will be presented to an independent data and safety monitoring board and the institutional review board within 7 days of occurrence.
Outcomes and data collection
The primary outcome is the duration of mechanical ventilation, defined as the time from randomisation to successful extubation without reinstitution for the following 48 hours. The secondary outcomes will include the dose of administered sedatives and opiate (absolute value as well as indexed value [total drug in mg/kg ÷ total number of hours from the start of infusion to its ultimate discontinuation]) at comparable clinically individualised target sedation goals throughout the study, the duration of ICU length of stay, and hospital length of stay. Additional outcomes include the prevalence and days of delirium in ICU, mortality in ICU and within 28 days after randomisation, and the number of ventilator-free days in 28 days.
The day of extubation is considered as the day of death for patients who died while still intubated. Censoring for ICU or hospital length analyses occurred at the time of death or study withdrawal. The number of ventilator-free days in 28 days is defined as days alive and not using mechanical ventilation between days 1 and 28. For the 28-day mortality analyses, patients are censored at the time of the last contact alive or at 28 days from enrolment, whichever is first.
Baseline demographic data will be collected from patients’ records by the medical team, including the reason for ICU admission, Acute Physiology and Chronic Health Evaluation II scores and diagnostic classification, Sequential Organ Failure Assessment scores, haematological and blood chemistry data, and clinical data (detailed information of sedative and analgesic medications administered to the patients before randomisation, cardiac safety profile including electrocardiograms and serum troponins, and liver function profile including serum bilirubin and glutamate pyruvate transaminase, etc). Vital signs such as blood pressure, heart rate, heart rhythm, temperature and oxygen saturations will be recorded and collected by the bedside nurses, as well as scores of RASS, BPS, NRS and CAM-ICU. Moreover, adverse events data will also be collected from patients’ records. All of data mentioned above will be entered using the double entry method.
Patient and public involvement statement
There is no patient or public involvement in the design, conduct, reporting or dissemination plans of this research.
Statistical analysis
Statistical power is estimated using the reduction in duration of mechanical ventilation as the primary outcome. According to Carrasco and colleagues, the mean (±SD) time for current sedation is 54.7±12.3 hours.27 We calculate that a sample size of 48 patients in each group will provide a power of 90% to detect a 15% relative reduction in intubation time at a twosided significance level of 0.05. With a dropout rate of 20%, the estimated sample size will be 60 patients per group. Thus, a total of 180 patients will be enrolled in the study.
The per-protocol set, including patients who complete the study without having major protocol violations, is used for the evaluation of clinical outcomes. While the full analysis set, determined according to the intention-to-treat population who undergo randomisation except for those who are excluded after randomisation, is not only used for evaluation of clinical outcomes but also baseline characteristics to measure the balance of the three groups before intervention. Missing data will be replaced by Markov Chain Monte Carlo method with 5–10 iterations according to the principle of multiple imputation. Continuous data will be presented as median and IQR, while categorical data as numbers and proportion. Normal distribution will be checked by the Kolmogorov test. For continuous variables, normal distributed data will be compared using one-way analysis of variance among three groups, and independent Student’s t-test between any of the two groups. While the comparison of non-normally distributed parameters among three groups will be applied by analysis of variance (Kruska Wallis), and then the Mann-Whitney U-test between any of the two groups. Categorical data will be compared by using Fisher’s exact test or the χ2 test. Other factors that may affect the efficacy will be considered as covariants for covariance analysis or Cox proportional hazards regression model. P≤0.05 will be considered to indicate statistical significance. All analyses will be done with R statistical software, V.4.0.2.
Discussion
This prospective trial is designed to provide evidence on the beneficial effect of acupuncture on reducing the duration of mechanical ventilation, avoiding excessive sedation and analgesia, as well as improving clinical outcomes in sedating mechanically ventilated ICU patients.
General analgesia and sedation are necessary for mechanically ventilated critically ill patients. However, overuse of sedative and analgesic medications may cause varying degrees of side effects, like respiratory drive reduction.28 These side effects are associated with worsened clinical outcomes, such as prolonged mechanical ventilation and hospital length of stay, increased risk of delirium, and even higher mortality.29 30 With many sophisticated attempts to mitigate this clinical problem, it has thus far been identified that optimising analgesia and sedation strategy is able to prevent excessive sedation and analgesia and improve the clinical outcome by reducing the duration and dosage of sedative and analgesic medications.31–33 Thus, it become a key objective to formulate an intensive sedative and analgesic medications strategy when caring for critically ill patients.
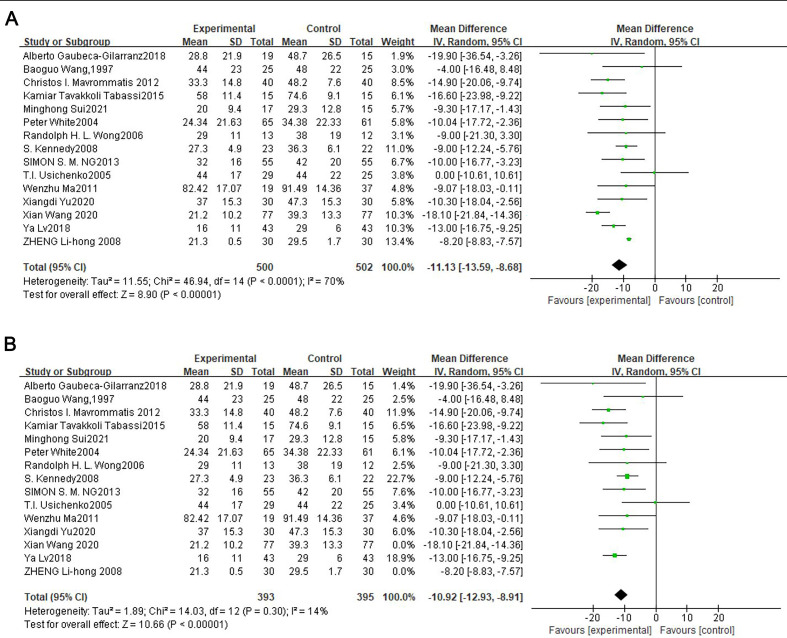
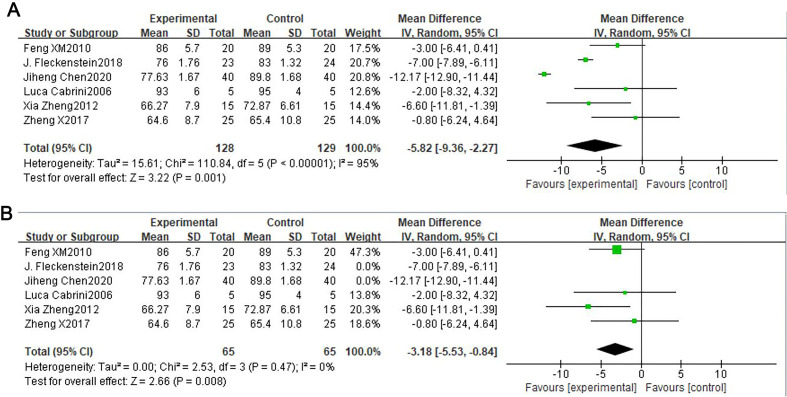
The rationale for evaluating the ability of acupuncture on this subject is based on research findings that acupuncture can manage pain relief and facilitate opioid tapering by increasing the μ-opioid receptor binding ability and the release of the opioid peptide.34 35 According to the meta-analysis of acupuncture on pain relief, visual analogue scale pain scores in the AC group is lower than that in the NAC group (MD=−11.13, 95% CI (−13.59 to –8.68), Z=8.9, p<0.00001, figure 3A).36–50 However, there is a substantial heterogeneity of results in these trials (I2=70%). As shown in figure 3B, heterogeneity decreases (I2=14%) when the studies by Xian Wang and Zheng Lihong are excluded, and the AC group consistently shows a greater pain relief compared with NAC group (MD=−10.92, 95% CI (−12.93 to –8.91), Z=10.66, p<0.00001). Meanwhile, acupuncture, without adverse effects, has been shown to exert sedation effects in various medical conditions. As it shown in the meta-analysis, with a high heterogeneity(I2=95%), the bispectral index value in the AC group is also lower than that in the NAC group (MD=−5.82, 95%CI (−9.36 to –2.27), Z=3.22, p=0.001, figure 4A).51–56 As shown in figure 4B, heterogeneity decreases (I2=0%) when the studies by J. Fleckenstein and Jiheng Chen are excluded, and the AC group consistently shows a better sedative effect compared with NAC group (MD=−3.18, 95%CI (−5.53 to –0.84), Z=2.66, p<0.008). In addition, previous studies have shown that Yintang (EX-HN3) and Shenmen (HT7) have good sedative effects, Hegu (LI4) and Taichong (LR3) have analgesic advantages, while Baihui (DU20) appears both sedative and analgesic effects.54 57–60 With these promising results, it is meaningful to assess acupuncture as a potential analgesia and sedation strategy in ameliorating the clinical outcomes in mechanically ventilated critically ill patients.
Figure 3.
Forest plot of AC group versus NAC group.
Figure 4.
Forest plot of AC group versus NAC group.
RCT has been recognised as the gold standard for clinical trials since the late 20th century.61 Another important designed technique to improve the quality of clinical trials is blinding. Over the past several decades, RCT and blinding have been used to avoid bias (selection bias, performance bias, and ascertainment bias) in clinical trials and improve the reliability of effects assessment. Sham acupuncture, aiming to blind the participants and control therapeutic components, is designed as a placebo control. However, this acupuncture technique is relatively difficult to fabricate because it should be both biologically inert and psychologically indistinguishable.62 Even previous experience of acupuncture feeling might impact the present perception of verum and sham acupuncture intervention.
In PASSION study, we use a rigorous set of methods to minimise bias, such as computer-generated central randomisation, parallel control design and statistical analysis according to the intent-to-treat principle. In control design, the superficial needle insertion without manual or electrical stimulation at the non-point is applied to simulate deep skin penetration in the SAC group, which is used as the most predominant type of sham electropuncture method to ensure blinding according to the published literature.63 However, a few studies reported that superficial needle insertion at non-acupoints might not be physiologically inert since the locations of points are nearby true acupoints.64 65 Moreover, researchers found that even mechanical non-penetration can evoke slight acupressure effects and physiological activity.66 Both of these factors will affect the effect assessment of acupuncture. Thus, the NA group, avoiding all therapeutic components, is designed to clarify whether the sham acupuncture can be regarded as physiologically inert, as well as compared with the results of the AC group.
A potential limitation of this trial is blinding. Given the nature of acupuncture, the patients and members of the medical team in the NA group are impossible to be blinded throughout the entire duration of this trial. However, adequate measures will be taken to put the patients and medical team members of the other two groups in a masked state. For example, we will formulate a set of isolation and secrecy strategies for the study coordinator and acupuncturists to achieve satisfactory blinding levels in treatment administration. Thus, in both AC and SAC groups, patients and their medical team members will be blinded to the patients’ acupuncture method. The data collectors and the biostatisticians will also be masked from the treatment assignment.
The PASSION study is designed to demonstrate the efficacy of acupuncture on sedation and analgesia in mechanically ventilated critically ill patients. We expect the finding can provide evidence-based recommendations for acupuncture use for sedation and analgesia in critically ill patients with mechanical ventilation.
Supplementary Material
Footnotes
Contributors: YZ and SM drafted this manuscript. GY, JW and FC made statistical analysis. M-ZZ made a critical revision of the manuscript and contributed to the rationalisation of the study. All authors read and approved the final manuscript.
Funding: This study was funded by National Science Foundation (grant No. 81703877&82074216&82004135), Science and Technology Planning Project of Guangzhou (202102010301).
Disclaimer: The sponsors have had no role in the project development, in the collection of data, in the preparation of this manuscript, nor the decision to publish. The researchers have complete independence from the sources of funding in all aspects of this study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained from parent(s)/guardian(s)
References
- 1.Coursin DB, Skrobik Y. What is safe sedation in the ICU? N Engl J Med 2019;380:2577–8. 10.1056/NEJMe1906522 [DOI] [PubMed] [Google Scholar]
- 2.Subramaniam B, Shankar P, Shaefi S, et al. Effect of intravenous acetaminophen vs placebo combined with propofol or dexmedetomidine on postoperative delirium among older patients following cardiac surgery: the DEXACET randomized clinical trial. JAMA 2019;321:686–96. 10.1001/jama.2019.0234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shelton KT, Qu J, Bilotta F, et al. Minimizing ICU neurological dysfunction with dexmedetomidine-induced sleep (MINDDS): protocol for a randomised, double-blind, parallel-arm, placebo-controlled trial. BMJ Open 2018;8:e020316. 10.1136/bmjopen-2017-020316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao L, Li D, Zheng H, et al. Acupuncture as adjunctive therapy for chronic stable angina: a randomized clinical trial. JAMA Intern Med 2019;179:1388–97. 10.1001/jamainternmed.2019.2407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia MK, Meng Z, Rosenthal DI, et al. Effect of true and sham acupuncture on radiation-induced xerostomia among patients with head and neck cancer: a randomized clinical trial. JAMA Netw Open 2019;2:e1916910. 10.1001/jamanetworkopen.2019.16910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pei W, Peng R, Gu Y, et al. Research trends of acupuncture therapy on insomnia in two decades (from 1999 to 2018):a bibliometric analysis. BMC Complement Altern Med 2019;19:225. 10.1186/s12906-019-2606-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He Y, Guo X, May BH, et al. Clinical evidence for association of acupuncture and Acupressure with improved cancer pain: a systematic review and meta-analysis. JAMA Oncol 2020;6:271–8. 10.1001/jamaoncol.2019.5233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith CA, Armour M, Zhu X, et al. Acupuncture for dysmenorrhoea. Cochrane Database Syst Rev 2016;4:CD007854. 10.1002/14651858.CD007854.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manheimer E, Cheng K, Wieland LS, et al. Acupuncture for hip osteoarthritis. Cochrane Database Syst Rev 2018;5:CD013010. 10.1002/14651858.CD013010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dingemann J, Plewig B, Baumann I, et al. Acupuncture in posttonsillectomy pain: a prospective, double-blinded, randomized, controlled trial. HNO 2017;65:73–9. 10.1007/s00106-016-0289-5 [DOI] [PubMed] [Google Scholar]
- 11.Wu M-S, Chen K-H, Chen I-F, et al. The efficacy of acupuncture in post-operative pain management: a systematic review and meta-analysis. PLoS One 2016;11:e0150367. 10.1371/journal.pone.0150367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y, Li Y, Zhang W-chen. [Effects of acupuncture in Siguan points on man-machine counteraction in respiratory failure patients during mechanical ventilation]. Zhongguo Zhong Xi Yi Jie He Za Zhi 2006;26:930–2. [PubMed] [Google Scholar]
- 13.Tsay S-L, Wang J-C, Lin K-C, et al. Effects of acupressure therapy for patients having prolonged mechanical ventilation support. J Adv Nurs 2005;52:142–50. 10.1111/j.1365-2648.2005.03576.x [DOI] [PubMed] [Google Scholar]
- 14.AminiSaman J, Mohammadi S, Karimpour H, et al. Transcutaneous electrical nerve stimulation at the acupuncture points to relieve pain of patients under mechanical ventilation: a randomized controlled study. J Acupunct Meridian Stud 2018;11:290–5. 10.1016/j.jams.2018.06.008 [DOI] [PubMed] [Google Scholar]
- 15.Yuan S-C, Huang X-L, Hua S-Y, et al. [Effect of acupuncture on diaphragmatic function in patients with AECOPD typeⅡ respiratory failure evaluated by ultrasound detection]. Zhongguo Zhen Jiu 2021;41:703–10. 10.13703/j.0255-2930.20200606-k0007 [DOI] [PubMed] [Google Scholar]
- 16.Irnich D, Behrens N, Molzen H, et al. Randomised trial of acupuncture compared with conventional massage and "sham" laser acupuncture for treatment of chronic neck pain. BMJ 2001;322:1574–8. 10.1136/bmj.322.7302.1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kong J-T, Puetz C, Tian L, et al. Effect of electroacupuncture vs sham treatment on change in pain severity among adults with chronic low back pain: a randomized clinical trial. JAMA Netw Open 2020;3:e2022787. 10.1001/jamanetworkopen.2020.22787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacPherson H, Altman DG, Hammerschlag R, et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med 2010;28:83–93. 10.1136/aim.2009.001370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306. 10.1097/CCM.0b013e3182783b72 [DOI] [PubMed] [Google Scholar]
- 20.Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 2003;289:2983–91. 10.1001/jama.289.22.2983 [DOI] [PubMed] [Google Scholar]
- 21.Sessler CN, Gosnell MS, Grap MJ, et al. The richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002;166:1338–44. 10.1164/rccm.2107138 [DOI] [PubMed] [Google Scholar]
- 22.Payen JF, Bru O, Bosson JL, et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med 2001;29:2258–63. 10.1097/00003246-200112000-00004 [DOI] [PubMed] [Google Scholar]
- 23.Chanques G, Viel E, Constantin J-M, et al. The measurement of pain in intensive care unit: comparison of 5 self-report intensity scales. Pain 2010;151:711–21. 10.1016/j.pain.2010.08.039 [DOI] [PubMed] [Google Scholar]
- 24.Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (awakening and breathing controlled trial): a randomised controlled trial. Lancet 2008;371:126–34. 10.1016/S0140-6736(08)60105-1 [DOI] [PubMed] [Google Scholar]
- 25.Subirà C, Hernández G, Vázquez A, et al. Effect of pressure support vs T-piece ventilation strategies during spontaneous breathing trials on successful extubation among patients receiving mechanical ventilation: a randomized clinical trial. JAMA 2019;321:2175–82. 10.1001/jama.2019.7234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hui D, Frisbee-Hume S, Wilson A, et al. Effect of lorazepam with haloperidol vs haloperidol alone on agitated delirium in patients with advanced cancer receiving palliative care: a randomized clinical trial. JAMA 2017;318:1047–56. 10.1001/jama.2017.11468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carrasco G, Molina R, Costa J, et al. Propofol vs midazolam in short-, medium-, and long-term sedation of critically ill patients. A cost-benefit analysis. Chest 1993;103:557–64. 10.1378/chest.103.2.557 [DOI] [PubMed] [Google Scholar]
- 28.Liu L, Wu A-P, Yang Y, et al. Effects of propofol on respiratory drive and patient-ventilator synchrony during pressure support ventilation in postoperative patients: a prospective study. Chin Med J 2017;130:1155–60. 10.4103/0366-6999.205864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kollef MH, Levy NT, Ahrens TS, et al. The use of continuous IV sedation is associated with prolongation of mechanical ventilation. Chest 1998;114:541–8. 10.1378/chest.114.2.541 [DOI] [PubMed] [Google Scholar]
- 30.Ouimet S, Kavanagh BP, Gottfried SB, et al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 2007;33:66–73. 10.1007/s00134-006-0399-8 [DOI] [PubMed] [Google Scholar]
- 31.Chanques G, Conseil M, Roger C, et al. Immediate interruption of sedation compared with usual sedation care in critically ill postoperative patients (SOS-Ventilation): a randomised, parallel-group clinical trial. Lancet Respir Med 2017;5:795–805. 10.1016/S2213-2600(17)30304-1 [DOI] [PubMed] [Google Scholar]
- 32.Mehta S, Burry L, Cook D, et al. Daily sedation interruption in mechanically ventilated critically ill patients cared for with a sedation protocol: a randomized controlled trial. JAMA 2012;308:1985–92. 10.1001/jama.2012.13872 [DOI] [PubMed] [Google Scholar]
- 33.Asmussen S, Przkora R, Maybauer DM, et al. Meta-Analysis of electroacupuncture in cardiac anesthesia and intensive care. J Intensive Care Med 2019;34:652–61. 10.1177/0885066617708558 [DOI] [PubMed] [Google Scholar]
- 34.Harris RE, Zubieta J-K, Scott DJ, et al. Traditional Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on mu-opioid receptors (MORs). Neuroimage 2009;47:1077–85. 10.1016/j.neuroimage.2009.05.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Han J-S. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci 2003;26:17–22. 10.1016/S0166-2236(02)00006-1 [DOI] [PubMed] [Google Scholar]
- 36.Wang B, Tang J, White PF, et al. Effect of the intensity of transcutaneous acupoint electrical stimulation on the postoperative analgesic requirement. Anesth Analg 1997;85:406–13. 10.1097/00000539-199708000-00029 [DOI] [PubMed] [Google Scholar]
- 37.Usichenko TI, Dinse M, Hermsen M, et al. Auricular acupuncture for pain relief after total hip arthroplasty - a randomized controlled study. Pain 2005;114:320–7. 10.1016/j.pain.2004.08.021 [DOI] [PubMed] [Google Scholar]
- 38.White P, Lewith G, Prescott P, et al. Acupuncture versus placebo for the treatment of chronic mechanical neck pain: a randomized, controlled trial. Ann Intern Med 2004;141:911–9. 10.7326/0003-4819-141-12-200412210-00007 [DOI] [PubMed] [Google Scholar]
- 39.Gaubeca-Gilarranz A, Fernández-de-Las-Peñas C, Medina-Torres JR, et al. Effectiveness of dry needling of rectus abdominis trigger points for the treatment of primary dysmenorrhoea: a randomised parallel-group trial. Acupunct Med 2018;36:302–10. 10.1136/acupmed-2017-011566 [DOI] [PubMed] [Google Scholar]
- 40.Kennedy S, Baxter GD, Kerr DP, et al. Acupuncture for acute non-specific low back pain: a pilot randomised non-penetrating sham controlled trial. Complement Ther Med 2008;16:139–46. 10.1016/j.ctim.2007.03.001 [DOI] [PubMed] [Google Scholar]
- 41.Lv Y, He H, Xie J, et al. Effects of transcutaneous acupoint electrical stimulation combined with low-dose sufentanil pretreatment on the incidence and severity of etomidate-induced myoclonus: a randomized controlled trial. Medicine 2018;97:e10969. 10.1097/MD.0000000000010969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ma W, Bai W, Lin C, et al. Effects of Sanyinjiao (SP6) with electroacupuncture on labour pain in women during labour. Complement Ther Med 2011;19:S13–18. 10.1016/j.ctim.2010.09.001 [DOI] [PubMed] [Google Scholar]
- 43.Mavrommatis CI, Argyra E, Vadalouka A, et al. Acupuncture as an adjunctive therapy to pharmacological treatment in patients with chronic pain due to osteoarthritis of the knee: a 3-armed, randomized, placebo-controlled trial. Pain 2012;153:1720–6. 10.1016/j.pain.2012.05.005 [DOI] [PubMed] [Google Scholar]
- 44.Ng SSM, Leung WW, Mak TWC, et al. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer. Gastroenterology 2013;144:307–13. 10.1053/j.gastro.2012.10.050 [DOI] [PubMed] [Google Scholar]
- 45.Sui M, Jiang N, Yan L, et al. Effect of electroacupuncture on shoulder subluxation in poststroke patients with hemiplegic shoulder pain: a sham-controlled study using multidimensional musculoskeletal ultrasound assessment. Pain Res Manag 2021;2021:1–9. 10.1155/2021/5329881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tabassi KT, Amini P, Mohammadi S, et al. The effect of acupuncture on pain score after open kidney surgery. J Complement Integr Med 2015;12:241–4. 10.1515/jcim-2014-0071 [DOI] [PubMed] [Google Scholar]
- 47.Wang X, Yin X, Guo X-T, et al. Effects of the pestle needle therapy, a type of acupoint stimulation, on post-hemorrhoidectomy pain: a randomized controlled trial. J Integr Med 2020;18:492–8. 10.1016/j.joim.2020.08.001 [DOI] [PubMed] [Google Scholar]
- 48.Wong RHL, Lee TW, Sihoe ADL, et al. Analgesic effect of electroacupuncture in postthoracotomy pain: a prospective randomized trial. Ann Thorac Surg 2006;81:2031–6. 10.1016/j.athoracsur.2005.12.064 [DOI] [PubMed] [Google Scholar]
- 49.Yu X, Zhang F, Chen B. The effect of TEAS on the quality of early recovery in patients undergoing gynecological laparoscopic surgery: a prospective, randomized, placebo-controlled trial. Trials 2020;21:43. 10.1186/s13063-019-3892-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zheng L-hong, Sun H, Wang G-nian, et al. Effect of transcutaneous electrical acupoint stimulation on nausea and vomiting induced by patient controlled intravenous analgesia with tramadol. Chin J Integr Med 2008;14:61–4. 10.1007/s11655-007-9006-2 [DOI] [PubMed] [Google Scholar]
- 51.Chen J, Zhang Y, Li X, et al. Efficacy of transcutaneous electrical acupoint stimulation combined with general anesthesia for sedation and postoperative analgesia in minimally invasive lung cancer surgery: a randomized, double-blind, placebo-controlled trial. Thorac Cancer 2020;11:928–34. 10.1111/1759-7714.13343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fleckenstein J, Baeumler P, Gurschler C, et al. Acupuncture reduces the time from extubation to 'ready for discharge' from the post anaesthesia care unit: results from the randomised controlled AcuARP trial. Sci Rep 2018;8:15734. 10.1038/s41598-018-33459-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cabrini L, Gioia L, Gemma M, et al. Bispectral index evaluation of the sedative effect of acupuncture in healthy volunteers. J Clin Monit Comput 2006;20:311–5. 10.1007/s10877-006-9026-z [DOI] [PubMed] [Google Scholar]
- 54.Zheng X, Meng JB, Fang Q. Electroacupuncture reduces the dose of midazolam monitored by the bispectral index in critically ill patients with mechanical ventilation: an exploratory study. Acupunct Med 2012;30:78–84. 10.1136/acupmed-2011-010095 [DOI] [PubMed] [Google Scholar]
- 55.Feng X-min, Li J, Wu Y. [Effect of combined electroacupuncture and epidural anesthesia in gynecological operation evaluated by bispectral index]. Zhongguo Zhong Xi Yi Jie He Za Zhi 2010;30:150–2. [PubMed] [Google Scholar]
- 56.Zheng X, Wan L, Gao F, et al. [Effect of ear point embedding on plasma and effect site concentrations of propofol-remifentanil in elderly patients after target-controlled induction]. Zhongguo Zhen Jiu 2017;37:869–73. 10.13703/j.0255-2930.2017.08.017 [DOI] [PubMed] [Google Scholar]
- 57.Lee K-C, Chao Y-FC, Lin Y-P, et al. Effectiveness of self-administered Acupressure for family caregivers of advanced cancer patients with insomnia: a randomized controlled trial. Cancer Nurs 2022;45:E1–9. 10.1097/NCC.0000000000000870 [DOI] [PubMed] [Google Scholar]
- 58.Chen Q-Q, Wei Q-L, Zhang X-H. [Effects of electroacupuncture on supplementary analgesia and improvement of adverse reactions induced by dolantin in oocyte retrieval]. Zhongguo Zhen Jiu 2012;32:1113–6. [PubMed] [Google Scholar]
- 59.Xiao J, Yi W, Wu L. Effects of electroacupuncture on reducing labor pain and complications in the labor analgesia process of combined spinal-epidural analgesia with patient-controlled epidural analgesia. Arch Gynecol Obstet 2019;299:123–8. 10.1007/s00404-018-4955-6 [DOI] [PubMed] [Google Scholar]
- 60.Chen TY, Zhou J, Wang K. Electroacupuncture intervention combined with anesthetics for analgesia and post-surgical gastrointestinal recovery in Pneumectomy patients. Zhen Ci Yan Jiu 2019;40:461–4. [PubMed] [Google Scholar]
- 61.Meldrum ML. A brief history of the randomized controlled trial. from oranges and lemons to the gold standard. Hematol Oncol Clin North Am 2000;14:745–60. 10.1016/s0889-8588(05)70309-9 [DOI] [PubMed] [Google Scholar]
- 62.Boutron I, Guittet L, Estellat C, et al. Reporting methods of blinding in randomized trials assessing nonpharmacological treatments. PLoS Med 2007;4:e61–80. 10.1371/journal.pmed.0040061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen Z-X, Li Y, Zhang X-G, et al. Sham electroacupuncture methods in randomized controlled trials. Sci Rep 2017;7:40837. 10.1038/srep40837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med 2006;24:13–15. 10.1136/aim.24.1.13 [DOI] [PubMed] [Google Scholar]
- 65.Lundeberg T, Lund I, Näslund J, et al. The Emperors sham - wrong assumption that sham needling is sham. Acupunct Med 2008;26:239–42. 10.1136/aim.26.4.239 [DOI] [PubMed] [Google Scholar]
- 66.Kim T-H, Lee MS, Alraek T, et al. Acupuncture in sham device controlled trials may not be as effective as acupuncture in the real world: a preliminary network meta-analysis of studies of acupuncture for hot flashes in menopausal women. Acupunct Med 2020;38:37–44. 10.1136/acupmed-2018-011671 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.