Abstract
Objectives
Rare diseases are characterised by low incidence, often with little evidence for effective treatments. Isolated patients and specialist centres for rare diseases are increasingly connected, thanks to the internet. This scoping review aimed to identify issues facing people with a rare disease that authors report may be addressed by electronic resources (mobile applications, websites, social media platforms, telehealth and online portals).
Design
Scoping review guided by the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines.
Data sources
Medline, Embase and PsycInfo were searched, supplemented by hand searches of selected journals, in July 2021.
Eligibility criteria
Peer-reviewed literature in English was searched using terms for rare disease (incidence <1:2000), electronic modalities (eg, mobile phone) and patient support terms. No date limit was set. Conference abstracts were included.
Data extraction and synthesis
Data extracted: rare disease/group of diseases, name of the e-resource, need identified in the patient cohort, features of the e-resource, any other findings or observations of interest. From this, a framework was developed synthesising features across diseases and resources.
Results
Seventy-two papers were found (from 383). Fifty-six electronic resources were described in 64 papers, while 12 papers were exploratory studies. Cystic fibrosis (n=28) was the most frequently addressed, followed by haemophilia (n=16).
Four domains and 23 subdomains of needs were extracted from the papers. The domains of needs were: support for self-management, access to high-quality information, access to appropriate specialist services, and social support. Subdomains are sometimes related to needs of individual rare diseases (eg, social isolation due to infection risk in people with cystic fibrosis). Fifteen electronic resources were identified that supported parents of children with rare disorders.
Conclusions
While it can be argued that rare diseases, per se, may be no less distressing or onerous to care for than a high prevalence disease, rare diseases have unique features: the lengthy odyssey to find a diagnosis, then appropriate specialists, the lack of evidence around effective treatments, guidelines or access to knowledgeable general health service providers. Designers of electronic resources are urged to consult key stakeholders to enhance the effectiveness and usability of resources for people with a rare disease.
Keywords: quality in health care, organisation of health services, health & safety
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Individual named rare diseases/groups of diseases were included in the search terms to overcome deficiencies of searching only using ‘rare diseases’, but could not cover all rare diseases.
There are estimated to be 6–7000 rare diseases so searching by name (plus their synonyms) was not feasible.
Data extraction considered the type of electronic resource proposed, by disease and by the need of resource addressed.
Electronic resources were categorised into mobile applications, social support platforms, telehealth tools and online portals, and active (containing interactive content, eg, quizzes) and passive websites (information only).
Introduction
There are an estimated 6–7000 different types of rare disease, many of them are genetic.1 We define a rare disease as a condition that has an incidence of less than 1 per 2000 live births in the population.1 Examples of rare diseases are fragile X syndrome, haemophilia A, osteogenesis imperfecta, cystic fibrosis, spinal muscular atrophy type 1 and neurofibromatosis type 2. The low incidence of rare diseases mean that specifics of individual diseases are not covered in medical education programmes which must prioritise more common conditions, and also that many health professionals have never seen a case before.2 Rare diseases are often difficult to diagnose, leading to the often described ‘diagnostic odyssey’.3 The case has been made that even after this odyssey is concluded with a definitive diagnosis, the journey continues as people with a rare disease seek to access the best management care.4
Less than 5% of the estimated 7000 rare diseases currently have an effective treatment.1 The low number of cases of each rare disease means that evidence is often lacking to guide best practice. For example, CLN12 disease with an incidence of only one per million has too few people with the disease to set up a clinical trial to test the effectiveness of potential treatments or even map the ‘typical’ progression of the disease.5 Guidance on best practice must be determined through consensus recommendations of specialists in the condition,6 7 which are often enhanced by the input of consumers who are living with the condition.8
A number of studies have explored the specific needs of people with a rare condition.9–11 Access to appropriate specialist services, finding a generalist health provider who is willing to learn about the condition, living with uncertainty of what is best practice, and the trial and error nature of discovering it have all been reported.4
Electronic resources, by which we mean mobile applications, websites, virtual monitoring devices, social media platforms, telehealth capability and online portals, hold promise of greater connectivity and collaboration in the field of rare diseases. Electronic resources are already being used to improve understandings of rare diseases as national and international online registries,12 13 and virtual research consortiums14 15 pool their data and consolidate findings.
Electronic resources have a key role for people living with a rare disease. It is recognised that a useful lever to accessing the best management care for people with a rare disease is empowerment, in which people become knowledgeable about their illness and feel able to advocate for their care.16 Tools to foster empowerment are particularly relevant in this group, and electronic resources hold great promise to make information and resources more easily accessible. To our knowledge, no one has surveyed this fragmented field to determine the role of electronic resources for people with a rare disease.
This paper aims to systematically scope the peer-reviewed literature to (1) identify issues facing people with a rare disease that authors report may be addressed by electronic resources, and (2) to collate evidence around features of effective and user-friendly e-resources.
Methods
We systematically searched for peer-reviewed literature on consumer-facing electronic resources for people with a rare disease, guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews17 (see online supplemental file 1 for the completed PRISMA-ScR checklist). The search was supplemented with a hand search of relevant peer-reviewed journals. Patients and public were not directly involved in the design, reporting or dissemination plan of this paper.
bmjopen-2021-060394supp001.pdf (65.9KB, pdf)
Three databases, Medline, Embase and PsycInfo, were searched in July 2021. No date limits were set but we only included articles in the English language. We targeted empirical peer-reviewed full articles but initial exploratory searches showed that a large proportion of the retrieved items were conference presentations on resources not reported elsewhere. These were therefore also included in the review. Search terms were developed through exploration of Medical Subject Heading terms and key words from equivalent papers from other fields. Search strings combined terms for rare disease (including specific named rare disease conditions to maximise results), with patient and carer facing resources (eg, health resources, patient participation), and terms associated with electronic resources (eg, mobile applications, cell phone, e-health). In addition, a hand search was performed in Orphanet Journal of Rare Diseases (searching for patient focused electronic resources) and Journal of Medical Internet Research (searching for applications for rare diseases). Search strings are shown in online supplemental file 2.
bmjopen-2021-060394supp002.pdf (58.9KB, pdf)
The definition of a rare disease as having an incidence of less than 1:2000 was used as a guide only as the grouping together of related rare diseases muddied the waters on exact rates, as did the range of definitions employed when reporting on rare diseases. The search therefore drew on named rare conditions/groups of conditions and the most common types of rare diseases (based on research effort for therapeutic companies around the world).18 Imperfect as that list is, it retrieved many more useful articles than the generic rare disease terms. ‘Mitochondrial respiratory chain disorders’ was also added as a large group of rare diseases that are not amenable to pharmaceutical treatment. The condition groups searched for by name therefore were narcolepsy, primary biliary cholangitis, Fabry disease, cystic fibrosis, haemophilia, spinal muscular atrophy, retinal dystrophy, X-linked hypophosphatemia, urea cycle disorders, pulmonary arterial hypotension, cerebral adrenoleukodystrophy, hereditary angioedema, AA amyloidosis, Cushing’s syndrome and mitochondrial respiratory chain disorders.
The following inclusion criteria needed to be met for a paper to be included: (1) the paper was framed around the needs of people diagnosed with a rare disease or group of rare diseases (defined as incidence <1:20001); (2) the focus was on how an electronic resource could meet that need in some way; (3) either proposed and described a particular electronic resource, or reported on the development, testing or evaluation of an actual electronic resource. Exclusion criteria were as follows: (1) not about a rare disease or group of rare diseases; (2) electronic resources were not consumer-facing (eg, virtual monitoring where the consumer has a passive role and no access to the data, applications that consumers used altruistically to collect data for researchers; electronic tools for healthcare professionals only).
Search results were downloaded into reference management software EndNote V.X9 and two researchers (JCL and SB) independently screened 50% of titles and abstracts using the eligibility criteria. Disagreements were discussed until consensus was met. Remaining articles were screened by JCL. Included articles were read in full and eligibility criteria again applied (by JCL and validated by SB). Data were extracted from the final set: rare disease/group of diseases, name of the e-resource, need identified in the patient cohort, features of the e-resource, any other findings or observations of interest.
The final step was collating and synthesising the needs of people with a rare disease discussed in the articles, looking for similarities and differences across different rare diseases and the electronic solutions proposed for each. From this, a framework was developed describing the synthesised domains of needs and examples of electronic resources designed to meet the need.
Results
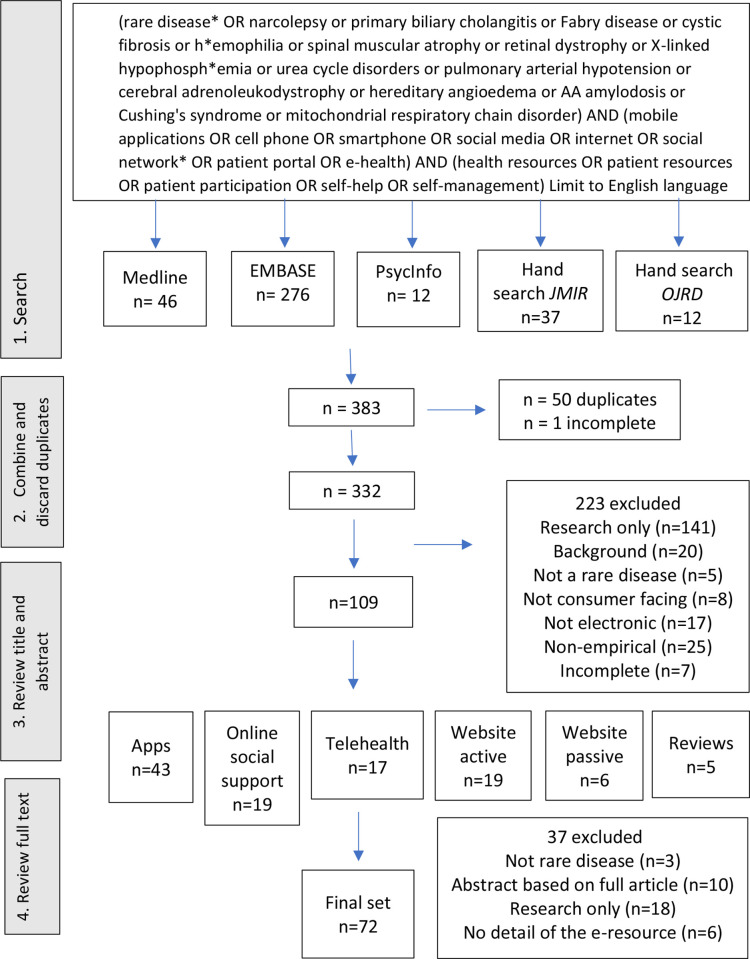
The search resulted in 383 papers. Title and abstract screening removed 223 papers and full text screening, another 33. This left 72 papers for data extraction and analysis. Figure 1 shows the PRISMA flow chart for the search.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart for the search. JMIR, Journal of Medical Internet Research; OJRD, Orphanet Journal of Rare Diseases.
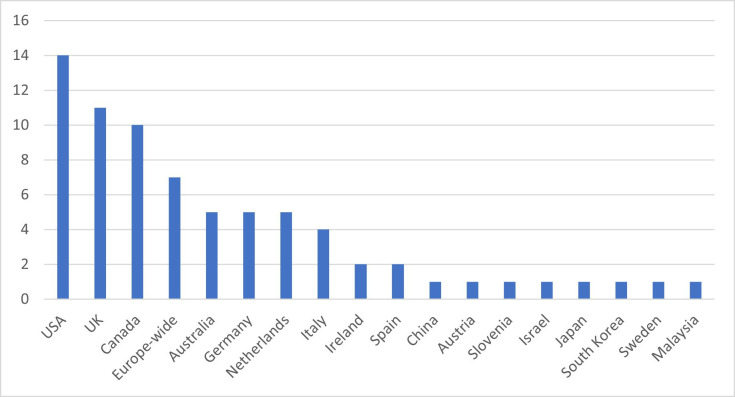
Studies were set in 16 different countries including seven papers that included all of Europe. The USA (n=14), the UK (n=11) and Canada (n=10) were the best represented countries. Figure 2 shows frequencies of all countries. Twenty-one different rare diseases were represented mostly in single papers, while eight papers focused on rare diseases generally (n=8). The most common rare disease reported was cystic fibrosis (n=28) followed by haemophilia (n=19). Table 1 shows the details.
Figure 2.
Countries in which included studies were undertaken (frequency of papers).
Table 1.
Overview of included papers
| Rare disease/group of diseases | Papers (n) |
| Acute intermittent porphyria | 1 |
| Addison’s disease | 3 |
| Autoimmune liver diseases | 1 |
| Bleeding disorders in women* | 1 |
| Complex regional pain syndrome | 1 |
| Congenital hypogonadotropic hypogonadism, Kallmann syndrome | 1 |
| Cystic fibrosis | 28 |
| Genetic eye disorders | 1 |
| Haemophilia | 19 |
| Hirschsprung’s disease | 1 |
| Idiopathic subglottic stenosis | 1 |
| Inborn errors of metabolism | 1 |
| Lymphangioleiomyomatosis | 1 |
| Narcolepsy | 2 |
| Osteogenesis imperfecta | 1 |
| Phenylketonuria, maple syrup urine disease or tyrosinemia | 1 |
| Rare and congenital anaemias | 1 |
| Rare diseases | 6 |
| Rare multisystemic vascular diseases | 1 |
| Thoracic outlet syndrome | 1 |
*Refers to papers focused on women with non-sex-specific Mendelian rare bleeding disorders.
Most papers reported on e-resources that were being trialled or were under development (n=56 e-resources from 64 papers), while 12 were framed as scoping exercises or explored usability of existing websites. For example, Nicholl and colleagues19 explored the needs of people with rare diseases that could be met by a consumer-facing website; Rüther and colleagues20 researched what people with rare liver disorders need in an app; and Aizawa and colleagues21 critiqued information available on the internet for people with narcolepsy.
e-Resources fell into five broad categories: (1) mobile applications (apps) for cell phones or tablets (n=22), (2) social networking platforms (n=14), (3) telehealth and virtual care platforms (n=13), (4) interactive websites (interactive content, eg, education modules with quizzes) (n=15) and (5) passive websites (passive content, eg, information) (n=7). Some e-resources fit into more than one category (eg, WhatsApp platform for parents of newly diagnosed infants with haemophilia provided social support from other parents as well as virtual consults with specialists).22 In these cases, the main function decided the category. Table 2 shows the types of resources, their features and their benefits.
Table 2.
Types of resources found, their features and their benefits
| Type of e-resource | Features and benefits |
| Mobile applications (apps) | Apps for phones and tablets can provide portable, always available and easily accessed information, data entry (eg, symptom trackers, guidelines, calculators) and links to other resources |
| Social networking platforms | Facilitating contact/emotional support between isolated people with the same rare disease; access to advice for day-to-day management queries |
| Telehealth and virtual care platforms | Rare disease specialists are also rare, often involving long journeys to see them face to face. Telehealth consults allow easier access. Virtual care, where patient uploaded data can be shared with a health professional, also overcomes the burden of travel and facilitates access to care from an appropriate specialist. |
| Websites (interactive) | Websites with interactive components allow the patient to enter their data and tailor content. Patient education through quizzes and games especially useful for younger people. |
| Websites (passive) | High-quality information can be made easily accessible on a website |
Synthesised themes from the data extraction led to the identification of 4 domains and 23 subdomains of needs of people with a rare disease or parents of children with a rare disease. A range of unique needs arising from features of individual diseases were identified (eg, risk of life-threatening acute episodes in Addison’s disease in a context of few emergency health professionals being knowledgeable or confident to deal with adrenal crisis23), as well as more global needs that were common across all presentations (eg, the scarcity of high quality, relevant information about individual rare diseases).19–21 23–51
Needs are summarised in table 3, giving examples of disease-specific needs in each subdomain and examples of the e-resources that had been developed or proposed to address those needs. Data extracted from the final set of items are given in full in online supplemental file 3.
Table 3.
Domains and subdomains of needs of people with a rare disease that can be solved or supported by a consumer-facing electronic resource
| Domain | Subdomains with disease-specific examples | e-Resource examples |
| Chronic diseases requiring self-management | Complicated self-management (eg, monitoring for bleeds and factor usage for haemophilia35 74) | Online tool (Metabolic DietAppSuite) for smartphones/desktops for 15 different inborn errors of metabolism. Creates a personalised dashboard including specific nutrient goals: food diary, nutrient counts73 |
| Some treatment regimes require detailed record keeping to optimise outcomes (eg, treatment of infections in CF33 51 56 75) | MyCBDR (linked to Canadian Bleeding Disorder Registry (CBDR) is an app that allows people with a bleeding disorder to track infusions and add symptoms. Data can be shared with all Haemophilia Treatment Centres in Canada.35 | |
| Transition to self-care as adolescents become adults (eg, teens with severe haemophilia29 76–78) | Smartphone app (Faccio Centro) aimed at adolescents with CF that lists daily therapy, with instructions on order, progress tracking, alerts for when to start and when checks are needed. Also can email questions to healthcare team.79 | |
| Exercise programmes need to be tailored to the rare disease (eg, reduced lung function and exercise tolerance in people with CF61 80 81) | LAM App on smartphone with interfacing wearable devices for women with lymphangioleiomyomatosis (LAM). Tailored exercise programme and physio check in.64 | |
| Monitoring changes in symptoms and treatments (eg, recognising bleeds in mild haemophilia58 82) | MyCyFAPP calculates pancreatic enzyme replacement therapy doses for fat digestion, a symptoms diary, educational material and linked to a web tool allowing health professionals to view data and give feedback28 30 55 | |
| Burden of hospital attendance (eg, living far away from only specialist centre for narcolepsy83); rare diseases with high disease burden (eg, CF84) | An ultrasound diagnostic solution for children with haemophilia, the EMO.TI.ON. System used at home by parents or caregivers to diagnose suspected bleeds. System can transfer live images to specialist physician.85 | |
| Depression, anxiety, distress affect adherence to treatment regimes, which in turn affect health and quality of life (eg, distress of parents of newly diagnosed children with haemophilia27) | Internet delivered cognitive–behavioural therapy sessions, eHealth CF-CBT guided by a qualified therapist for people with cystic fibrosis experiencing depression or anxiety62 | |
| Lack of high-quality information on all aspects of the rare disease | Information that is readable, accessible and from a credible source (eg, lack of specific information on rare and congenital anaemias59) | Newborn Screening Connect (NBS Connect) provides high-quality information for parents of children diagnosed with a disorder included in the newborn screening panel performed routinely in the USA43 |
| Information available in your language, appropriate for your culture (eg, Canadian haemophilia resources in English and French58 76) | Online education package for congenital hypogonadotropic hypogonadism and the olfacto-genital syndrome is available in 20 European languages. Readability score meets recommended level.26 | |
| Appropriate to age group or special needs (eg, information for teens with CF86) | Gene.vision website on genetic eye disorders optimised for people with impaired vision40 | |
| Access to relevant clinical trials, or new research findings may be difficult to find45 | NIH Rare Diseases Clinical Research Network (RDCRN) notifies registrants with a range of rare disorders of relevant studies45 | |
| Disease-specific information on niche topics like family planning (eg, for genetic disorders such as CF32) | Facebook group (MyGirlsBlood) for women with bleeding disorders where women can ask questions or share experiences especially around menstruation34 | |
| Urgent need for disease specific information during COVID-19 pandemic46 | Weekly webcasts on COVID-19 for people with CF with questions through Google forms. Email notifications of webcasts sent to known patients in the USA.46 | |
| Specialist centres may be geographically dispersed and hard to find | Identifying appropriate care for rare disease (eg, nearest specialist; appropriately trained allied health professionals (eg, physios who know risks of exercise with haemophilia87)) | Mobile app developed by VASCERN (European Reference Network on Rare Multisystemic Vascular diseases) contains an easily searchable directory to find closest expert and to find appropriate patient advocacy group within Europe44 |
| Burden of hospital attendance (eg, living far away from only specialist centre; rare diseases with high disease burden (eg, severe haemophilia88) | Virtual Reality Visual Feedback Module for people with complex regional pain syndrome (who have few treatment options and for whom travel is onerous). After initial in-person training and assessment, can be continued at home.89 | |
| Knowledgeable emergency care for acute events may be hard to find (eg, for infants with newly diagnosed haemophilia27) | Quick response (QR coded) bracelet has a scannable QR code that links to emergency management information for people in adrenal crisis23 | |
| Information on daily management may be lacking for both the person with the rare disease and the health professionals supporting them (eg, for parents of infants with Hirschsprung’s disease50) | Thoracic Outlet Syndrome (TOS) Awareness Facebook group for both people with TOS and health professionals. Most posts encouraging and giving sound advice.49 | |
| Social isolation from peers and advice networks | Unable to connect with people with the same disorder (eg, being the only parent you know with a child with a rare disorder25) | Online forum for people with Addison’s disease or Cushing’s syndrome, moderated by the Dutch Adrenal Society37 |
| Disorders that require isolation for infection control, or safety are isolated from unaffected peers as well (eg, fracture risk for children with OI in new surroundings31) | Online conferences (BreatheCon) for people with cystic fibrosis who must isolate for infection control32 | |
| Emotional support needed for distressed parents (eg, for parents of children with OI31) | Skype support groups for women with acute intermittent porphyria mediated by a porphyria experts90 | |
| Support for daily management issues (eg, online for people with idiopathic subglottic stenosis36) | Social media campaign around living with Hirschsprung’s disease: Shit happens on Facebook, Twitter, Blog posts50 | |
| Information and peer knowledge sharing for adolescents transitioning to full self-management (eg, for teens with CF86) | hiFIve—small online group for 11–19 year olds living with severe haemophilia. Closed to parents. Trying to harness peer to peer transmission of self-management skills.77 | |
| Social support associated with better mental health/health outcomes (eg, parents of newly diagnosed infants with phenylketonuria43) | Online peer support programme (CFOne) for adolescents and young adults with CF91 |
CF, cystic fibrosis; OI, osteogenesis imperfecta.
bmjopen-2021-060394supp003.pdf (235.4KB, pdf)
Chronic diseases requiring complicated self-management
Many rare diseases were described as having a high disease burden relying on complicated self-management regimes. The association of adherence to specific treatments with better health outcomes is strongly supported by evidence for cystic fibrosis,52 metabolic diseases requiring medical diets53 and haemophilia,54 providing a clear rationale for supporting self-management. Optimal self-management in many cases required careful record-keeping of symptoms and tracking of treatments. Mobile apps were often designed to assist with this need. Symptom trackers were a common feature with or without medication alerts or treatment information (pancreatic enzyme replacement therapy for people with cystic fibrosis28 55). Some had a function that allowed sharing of patient entered data with their healthcare team.56 57 Others tracked dietary intake for those on a medical diet.53
Lack of high-quality information
A common problem across all the rare diseases represented in this review was access to high-quality, culturally and demographically appropriate information from a credible source that was easy to find and understand. Information sought could be around the nature of the disease, medical treatments, prognoses, etc, for the person with the disease and sometimes also for the health professionals supporting them.23 26 49 Links to registries and research consortiums helped people stay up to date with treatment options.45 Information about day-to-day management issues was often sought from social networks of people with experience of the same disease rather than specialist health professionals.34 37 38 One paper critiqued existing online information on the rare disorder narcolepsy, following a study that showed access to high-quality web-based information could reduce time to diagnosis through better understanding of signs and symptoms.21 Some informational needs related to ‘niche’ topics, for example, an app for the subset of people with mild haemophilia to help them assess for cryptic bleeds after injury.58
Specialist centres for rare diseases may be geographically dispersed
Another common problem was the small number of rare disease specialist centres that could be widely dispersed geographically. Some e-resources provided directories for the nearest specialist centre,40 48 or nearest, appropriately skilled allied health provider or patient advocacy agency.59 Others proved virtual consultations60 or tailored exercise61 or mental health services62 via telehealth.
Social isolation from peers and advice networks
The social isolation that comes from having a rare disease is often discussed as a need unique to people with a rare disease. Khair and colleagues63 noted that for many adolescent boys with haemophilia, the only person other than their doctor who knows about their disease is their parent. Limited access to specialist services means people or parents of a child with a rare condition have to face non-urgent day-to-day issues by themselves unless they find appropriate social support. Social support could be with people with the same disease (eg, Facebook/Twitter group for Hirschsprung’s disease50) or include health professionals (eg, online support group for thoracic outlet syndrome49).
Discussion
This review found 72 papers outlining the needs of people with a rare disease, or their carers that could be addressed by an e-resource. Four domains and 23 subdomains of needs were identified and e-resources to address or support those needs were broadly categorised into five groups: mobile apps, social support platforms, telehealth and virtual health tools, and interactive and passive websites.
A range of unique needs arising from features of individual diseases were identified. Examples included the burden of constant physical isolation to prevent infection for people with cystic fibrosis,32 the acute distress of parents of infants with osteogenesis imperfecta at suspicions of child abuse that often preceded diagnosis31 and the difficulty of recognising signs of an impending adrenal crisis for people with Addison’s disease that can be life threatening.23 37 While the burden of disease for rare disorders may be similar to higher incidence conditions such as stroke or breast cancer, the added burden of the lack of a solid evidence base of effective treatments, best practice guidelines and competent and knowledgeable health service providers is not. The well-documented diagnostic odyssey for people with rare diseases3 and laments that health professionals had never heard of their disease4 is a burden unique to this group.
This burden of uniqueness spills over to other needs. Exercise is crucial for physical and mental well-being but for many people with a rare disease, any exercise programme must be tailored and supervised by a suitably knowledgeable health professional. Reduced exercise tolerance for people with cystic fibrosis and LAM, and risk of bleeds into their joints for people with haemophilia were addressed by telehealth or online modules.57 61 64–67 Social support of group exercise classes is known to be motivating but is not possible for people with cystic fibrosis who are at risk of cross infection. Online solutions went some way to solving this need.66
Resources supporting peer-to-peer support for people and carers of children with a rare disease were well represented in the articles. The value of social support from someone who is on the same journey is well documented.68 Although the quality of the advice and information exchanged on social support platforms is often criticised,69 there was no evidence of this in our sample, with some sites convened or facilitated by a trained health professional. Four studies critiqued the content of posts on social support platforms for people with different rare diseases and found them to be overwhelmingly positive and supportive.36 37 49 50 Real-time, knowledgeable solutions to problems, plus emotional support, were demonstrated as highly valuable to members and these benefits were noted as important goals for any proposed new e-resources.20 31
It has been argued that an often overlooked need for people with a rare disease is support for their parents or carers, on whom the burden of management often falls.70 This review identified 15 e-resources that supported carers (mostly parents). The distress that parents feel on diagnosis of a child with a rare disease was frequently discussed and provided the rationale for social support platforms and messaging apps, management support apps and telehealth tools. One German study provided parents of children with cystic fibrosis online writing-based therapy to alleviate psychological distress and anxiety.71
Readability of information found on the internet has been widely critiqued and criticised. A typical example is a review of online education resources from government and healthcare organisations on multiple sclerosis and rheumatoid arthritis (neither considered rare diseases) were found to be written at 11th or 12th grade standard, whereas the average American reads at a 5th grade standard.72 The authors state material that is too complex limits its usefulness and increases inequities. e-Resources in this review were often noted to be co-designed by health professionals, patient advocacy agencies, parents and people with a rare disease, as well as education experts, to mitigate this risk.26 73 Usability and acceptability studies were reported for some but not all the resources found in this review. Ensuring resources are easy to understand, appeal to the target group’s demographics (eg, adolescents vs older adults) and suited to the skills of the users is an obvious goal but one that this scoping review did not always find was done well. Patient advocacy agencies are noted in the broader literature to be particularly proactive in ensuring acceptable and easy to understand resources. A survey of patient advocacy groups for people with rare diseases found 100% of respondents would be interested in collaborating with relevant healthcare or research groups to develop complementary resources suited to their members, and avoid wasted effort involved in duplication.70
The very low incidence of rare diseases mean that patients and appropriate services are geographically widely distributed. Electronic resources such as telehealth, social networking platforms and specialised apps are therefore ideal solutions to provide appropriate care. Progress in understanding diseases that are rare has been accelerated in recent years as clinicians and scientists around the world pool the data they have on local. A similar benefit comes for patients as they find or are linked to others with knowledge and experience of their unique situation. Currently, the efficacy of e-resources for people with a rare disease is being realised one disease group at a time. While each disease has its unique features, we have shown here that the needs of all people with rare disease are basically the same. These domains of needs should be addressed by any team wishing to develop new e-resources for this cohort.
Strengths and limitations
The nature of the topic (e-resources) lent itself more to conference presentations rather than full peer-reviewed articles. A strength of our search was that we included these items, although a weakness is that limited information was able to be extracted from some abstracts. Further, there was likely an element of publication bias where only successfully developed e-resources were reported. The main limitation to our review was the difficulty capturing articles focused on people with a rare disease. Our search was systematic but does not claim to be exhaustive. In particular, the search terms to capture rare diseases were problematic. Since there are over 7000 rare diseases, it was not feasible to search for each by name. Our strategy was therefore to search for a limited number of named rare disease groups. The lists of needs identified are characteristic of any rare disease, and while some needs are unique to some specific disease manifestation, the majority were applicable to all. This generalisability will be useful for anyone designing e-resources to support people with a rare disease.
Conclusion
This review scoped the peer-reviewed literature to identify needs unique to people, or carers of people with a rare disease. It identified four broad domains of need: (1) support for complicated self-management regimes, (2) access to high-quality, easy to understand information, (3) access to appropriate specialist services and (4) social support. Most studies involved needs of people or carers of children with haemophilia or cystic fibrosis but also addressed another 20 named rare diseases or rare disease groups (eg, inborn errors of metabolism). While the physical burden of a rare disease may be comparable to higher prevalence conditions such as stroke or cancer, rare diseases have unique overlying issues: the lengthy odyssey to find a diagnosis, the quest to find appropriate specialists to manage your care, the lack of a solid evidence base of effective treatments or best practice guidelines, or access to competent and knowledgeable general health service providers are unique to those with a rare disease. e-Resources are well placed to address many of these problems but must be carefully co-designed with key stakeholders lest their complexity, narrow scope or cultural inappropriateness further disempower this already marginalised group.
Supplementary Material
Acknowledgments
The research conducted at the Murdoch Children’s Research Institute was supported by the Victorian Government's Operational Infrastructure Support Program. The Chair in Genomic Medicine awarded to JC is generously supported by The Royal Children’s Hospital Foundation.
Footnotes
Twitter: @JanetCLong
Contributors: JCL, SB, SH and BNGE designed the study. JCL and SB collected data and undertook the analysis. SH, ZF, BNGE, JC and JB critically reviewed and commented on the results. JCL wrote the first draft of the paper which was reviewed by SB, SH, ZF, BNGE, JC and JB. All authors approved the final version. JCL acts as guarantor for this study.
Funding: This project was funded by a Mito Foundation Project Grant 2019-21.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Boycott KM, Vanstone MR, Bulman DE, et al. Rare-disease genetics in the era of next-generation sequencing: discovery to translation. Nat Rev Genet 2013;14:681–91. 10.1038/nrg3555 [DOI] [PubMed] [Google Scholar]
- 2.Ramalle-Gómara E, Domínguez-Garrido E, Gómez-Eguílaz M, et al. Education and information needs for physicians about rare diseases in Spain. Orphanet J Rare Dis 2020;15:18. 10.1186/s13023-019-1285-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thevenon J, Duffourd Y, Masurel-Paulet A, et al. Diagnostic odyssey in severe neurodevelopmental disorders: toward clinical whole-exome sequencing as a first-line diagnostic test. Clin Genet 2016;89:700–7. 10.1111/cge.12732 [DOI] [PubMed] [Google Scholar]
- 4.Long JC, Best S, Hatem S, et al. The long and winding road: perspectives of people and parents of children with mitochondrial conditions negotiating management after diagnosis. Orphanet J Rare Dis 2021;16:310. 10.1186/s13023-021-01939-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Augustine EF, Adams HR, Mink JW. Clinical trials in rare disease: challenges and opportunities. J Child Neurol 2013;28:1142–50. 10.1177/0883073813495959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parikh S, Goldstein A, Koenig MK, et al. Diagnosis and management of mitochondrial disease: a consensus statement from the mitochondrial medicine Society. Genet Med 2015;17:689–701. 10.1038/gim.2014.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geberhiwot T, Moro A, Dardis A, et al. Consensus clinical management guidelines for Niemann-Pick disease type C. Orphanet J Rare Dis 2018;13:50. 10.1186/s13023-018-0785-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaufmann P, Pariser AR, Austin C. From scientific discovery to treatments for rare diseases - the view from the National Center for Advancing Translational Sciences - Office of Rare Diseases Research. Orphanet J Rare Dis 2018;13:196. 10.1186/s13023-018-0936-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Depping MK, Uhlenbusch N, von Kodolitsch Y, et al. Supportive care needs of patients with rare chronic diseases: multi-method, cross-sectional study. Orphanet J Rare Dis 2021;16:44. 10.1186/s13023-020-01660-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kreuter M, Bendstrup E, Russell A-M, et al. Palliative care in interstitial lung disease: living well. Lancet Respir Med 2017;5:968–80. 10.1016/S2213-2600(17)30383-1 [DOI] [PubMed] [Google Scholar]
- 11.Quinn L, Davis K, Yee A, et al. Understanding genetic learning needs of people affected by rare disease. J Genet Couns 2020;29:1050–8. 10.1002/jgc4.1233 [DOI] [PubMed] [Google Scholar]
- 12.Rubio-Gozalbo ME, Haskovic M, Bosch AM, et al. The natural history of classic galactosemia: lessons from the GalNet registry. Orphanet J Rare Dis 2019;14:86. 10.1186/s13023-019-1047-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scalco RS, Lucia A, Santalla A, et al. Data from the European Registry for patients with McArdle disease and other muscle glycogenoses (EUROMAC). Orphanet J Rare Dis 2020;15:330. 10.1186/s13023-020-01562-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woodward L, Johnson S, Walle JV, et al. An innovative and collaborative partnership between patients with rare disease and industry-supported registries: the global aHUS registry. Orphanet J Rare Dis 2016;11:154. 10.1186/s13023-016-0537-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pavan S, Rommel K, Mateo Marquina ME, et al. Clinical practice guidelines for rare diseases: the Orphanet database. PLoS One 2017;12:e0170365. 10.1371/journal.pone.0170365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Le Cam Y, Bolz-Johnson M. Expert by experience: Valuing patient engagement in healthcare. In: Pomey M-P, Denis J-L, Dumez V, eds. Patient engagement: how patient-provider partnerships transform healthcare organisations. Cham, Switzerland: Palgrave Macmillan, 2019: 233–67. [Google Scholar]
- 17.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 18.Ghosh I. Infographic: which rare diseases are the most common? : Visual Capitalist, 2019. Available: https://www.visualcapitalist.com/which-rare-diseases-are-the-most-common/
- 19.Nicholl H, Tracey C, Begley T, et al. Internet use by parents of children with rare conditions: findings from a study on parents' web information needs. J Med Internet Res 2017;19:e51. 10.2196/jmir.5834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rüther DF, Sebode M, Lohse AW, et al. Mobile APP requirements for patients with rare liver diseases: a single center survey for the ERN RARE-LIVER. Clin Res Hepatol Gastroenterol 2021;45:101760. 10.1016/j.clinre.2021.101760 [DOI] [PubMed] [Google Scholar]
- 21.Aizawa R, Sunahara H, Kume K, et al. Status of narcolepsy-related information available on the Internet in Japan and its effective use. Sleep Biol Rhythms 2008;6:201–7. 10.1111/j.1479-8425.2008.00362.x [DOI] [Google Scholar]
- 22.Barazani Brutman T, Bashari D, Lenda H. New communication technologies improve hemophilia care. Haemophilia 2017:134–5.29115006 [Google Scholar]
- 23.Colman AW, Sellick JFK, Weaver JU. Use of Quick Response (QR) coded bracelets and cards for the improvement of cortisol deficiency/Addison’s disease management: an audit of quality of care of the management of steroid deficiency in acute illness. BMJ Innovations 2018;4:115–22. 10.1136/bmjinnov-2017-000226 [DOI] [Google Scholar]
- 24.Ackbarali TA, Croteau SE, Pipe SW, et al. Assessing patient and provider perspectives, clinical practice, behaviors, and knowledge on hemophilia a care. Blood 2020;136:24–5. 10.1182/blood-2020-14165732430494 [DOI] [Google Scholar]
- 25.et alArmayones M, Hernandez-Encuentra E, Gomez-Zuniga B. APTIC: a social network to improve the quality of life of members of patients' associations. Orphanet Journal of Rare Diseases Conference: 5th European Conference on Rare Diseases,. ECRD, 2010. [Google Scholar]
- 26.COST Action BM1105, Badiu C, Bonomi M, et al. Developing and evaluating rare disease educational materials co-created by expert clinicians and patients: the paradigm of congenital hypogonadotropic hypogonadism. Orphanet J Rare Dis 2017;12:57. 10.1186/s13023-017-0608-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barazani Brutman T, Bashari D, Lenda H. New communication technologies improve hemophilia care. Haemophilia 2017;23:134–5. [Google Scholar]
- 28.Boon M, Calvo-Lerma J, Claes I, et al. Use of a mobile application for self-management of pancreatic enzyme replacement therapy is associated with improved gastro-intestinal related quality of life in children with cystic fibrosis. J Cyst Fibros 2020;19:562–8. 10.1016/j.jcf.2020.04.001 [DOI] [PubMed] [Google Scholar]
- 29.Breakey VR, Ignas DM, Warias AV, et al. A pilot randomized control trial to evaluate the feasibility of an Internet-based self-management and transitional care program for youth with haemophilia. Haemophilia 2014;20:784–93. 10.1111/hae.12488 [DOI] [PubMed] [Google Scholar]
- 30.Calvo-Lerma J, Boon M, Hulst J, et al. Change in nutrient and dietary intake in European children with cystic fibrosis after a 6-month intervention with a self-management mHealth tool. Nutrients 2021;13:1801. 10.3390/nu13061801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castro AR, Chougui K, Bilodeau C, et al. Exploring the views of osteogenesis imperfecta caregivers on Internet-based technologies: qualitative descriptive study. J Med Internet Res 2019;21:e15924. 10.2196/15924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cipriani D, Dulcan E. See and be seen: the CF community. Pediatric Pulmonology 2017:147–8.27749021 [Google Scholar]
- 33.Cummings E, Hauser J, Cameron-Tucker H, et al. Enhancing self-efficacy for self-management in people with cystic fibrosis. Stud Health Technol Inform 2011;169:33–7. [PubMed] [Google Scholar]
- 34.D'Ambrosio C. Open versus closed social networking groups. Haemophilia 2014:183. [Google Scholar]
- 35.Decker K, Meilleur C. CBDR and MyCBDR advancing hemophilia nursing practice in Canada. Haemophilia 2018:37.29878657 [Google Scholar]
- 36.Haik D, Kashanchi K, Tajran S, et al. The online support group as a community: a thematic content analysis of an online support group for idiopathic subglottic stenosis. Ann Otol Rhinol Laryngol 2019;128:293–9. 10.1177/0003489418820348 [DOI] [PubMed] [Google Scholar]
- 37.Kauw D, Repping-Wuts H, Noordzij A, et al. The contribution of online peer-to-peer communication among patients with adrenal disease to patient-centered care. J Med Internet Res 2015;17:e54. 10.2196/jmir.3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kirk S, Milnes L. An exploration of how young people and parents use online support in the context of living with cystic fibrosis. Health Expect 2016;19:309–21. 10.1111/hex.12352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kühnle L, Mücke U, Lechner WM, et al. Development of a social network for people without a diagnosis (RarePairs): evaluation study. J Med Internet Res 2020;22:e21849. 10.2196/21849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yeong JL, Thomas P, Buller J, et al. A newly developed web-based resource on genetic eye disorders for users with visual impairment (Gene.Vision): usability study. J Med Internet Res 2021;23:e19151. 10.2196/19151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Manu-Pereira MM, Gutierrez-Valle V, Vives-Corrons JL. ENERCA: towards a European reference network (ERN) in rare haematological diseases. British Journal of Haematology 2016:39–40. [Google Scholar]
- 42.Moon H, Moon J. Comparative readability analysis of information on exercise for hemophilia patients. Haemophilia 2021;27:57. [Google Scholar]
- 43.Osara Y, Coakley K, Devarajan A, et al. Development of newborn screening connect (Nbs connect): a self-reported patient registry and its role in improvement of care for patients with inherited metabolic disorders. Orphanet J Rare Dis 2017;12:132. 10.1186/s13023-017-0684-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paglialonga A, Gaetano R, Robert L, et al. eHealth for patients with rare diseases: the eHealth Working group of the European reference network on rare multisystemic vascular diseases (VASCERN). Orphanet J Rare Dis 2021;16:164. 10.1186/s13023-020-01604-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Richesson RL, Lee HS, Cuthbertson D, et al. An automated communication system in a contact Registry for persons with rare diseases: scalable tools for identifying and recruiting clinical research participants. Contemp Clin Trials 2009;30:55–62. 10.1016/j.cct.2008.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rits S, Snell C, Uluer AZ. Weekly patient webcasts: An adult CF center’s response to the COVID-19 pandemic. Pediatric Pulmonology 2020:78. [Google Scholar]
- 47.Rodman J, Krivec U, Jackson A. WS23.6 patient perspectives on electronic access to registry health records: an Irish-Slovene online survey. Journal of Cystic Fibrosis 2016;15:S36. 10.1016/S1569-1993(16)30187-4 [DOI] [Google Scholar]
- 48.Storf H, Hartz T, Tegtbauer N. Vision and challenges of a cartographic representation of expert medical centres for rare diseases. Stud Health Technol Inform 2014;205:677–81. [PubMed] [Google Scholar]
- 49.Walker KK. Cognitive and affective uses of a thoracic outlet syndrome Facebook support group. Health Commun 2014;29:773–81. 10.1080/10410236.2013.800830 [DOI] [PubMed] [Google Scholar]
- 50.Wittmeier K, Holland C, Hobbs-Murison K, et al. Analysis of a parent-initiated social media campaign for Hirschsprung's disease. J Med Internet Res 2014;16:e288. 10.2196/jmir.3200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wood J, Jenkins S, Putrino D, et al. A smartphone application for reporting symptoms in adults with cystic fibrosis improves the detection of exacerbations: results of a randomised controlled trial. J Cyst Fibros 2020;19:271–6. 10.1016/j.jcf.2019.09.002 [DOI] [PubMed] [Google Scholar]
- 52.Sanders DB, Bittner RCL, Rosenfeld M, et al. Failure to recover to baseline pulmonary function after cystic fibrosis pulmonary exacerbation. Am J Respir Crit Care Med 2010;182:627–32. 10.1164/rccm.200909-1421OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cipriano LE, Rupar CA, Zaric GS. The cost-effectiveness of expanding newborn screening for up to 21 inherited metabolic disorders using tandem mass spectrometry: results from a decision-analytic model. Value Health 2007;10:83–97. 10.1111/j.1524-4733.2006.00156.x [DOI] [PubMed] [Google Scholar]
- 54.Nilsson IM, Berntorp E, Löfqvist T, et al. Twenty-Five years' experience of prophylactic treatment in severe haemophilia A and B. J Intern Med 1992;232:25–32. 10.1111/j.1365-2796.1992.tb00546.x [DOI] [PubMed] [Google Scholar]
- 55.Calvo-Lerma J, Boon M, Colombo C, et al. Clinical evaluation of an evidence-based method based on food characteristics to adjust pancreatic enzyme supplements dose in cystic fibrosis. J Cyst Fibros 2021;20:e33-e39. 10.1016/j.jcf.2020.11.016 [DOI] [PubMed] [Google Scholar]
- 56.Floch J, Vilarinho T, Zettl A, et al. Users' experiences of a mobile health self-management approach for the treatment of cystic fibrosis: mixed methods study. JMIR Mhealth Uhealth 2020;8:e15896. 10.2196/15896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Howard S, Speight L, Mills-Bennett R, et al. WS9.6 the all Wales adult cystic fibrosis centre (AWACFC) virtual instruction of exercise with technology to enhance care – VIEWTEC programme. Journal of Cystic Fibrosis 2014;13:S20. 10.1016/S1569-1993(14)60063-1 [DOI] [Google Scholar]
- 58.Lomotey RK, Mulder K, Nilson J, et al. Mobile self-management guide for young men with mild hemophilia in cases of minor injuries. Network Modeling Analysis in Health Informatics and Bioinformatics 2014;3. 10.1007/s13721-014-0064-z [DOI] [Google Scholar]
- 59.Manu-Pereira MM, Gutierrez-Valle V, Vives-Corrons JL. ENERCA: towards a European reference network (ERN) in rare haematological diseases. British Journal of Haematology 2016;173:39–40. [Google Scholar]
- 60.Sottilotta G, Arrigo P, Drago L. The HEMONLINE project: preliminary results. Haemophilia 2012;3:77. [Google Scholar]
- 61.Carr SB, Ronan P, Lorenc A, et al. Children and adults tai chi study (CF-CATS2): a randomised controlled feasibility study comparing internet-delivered with face-to-face tai chi lessons in cystic fibrosis. ERJ Open Res 2018;4:00042-2018. 10.1183/23120541.00042-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Verkleij M, Georgiopoulos AM, Friedman D. Development and evaluation of an Internet-based cognitive behavioral therapy intervention for anxiety and depression in adults with cystic fibrosis (eHealth CF-CBT): an international collaboration. Internet Interv 2021;24:100372. 10.1016/j.invent.2021.100372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khair K, Holland M, Carrington S. Social networking for adolescents with haemophilia. Haemophilia 2011:369. [DOI] [PubMed] [Google Scholar]
- 64.Guilliams JM, Garvin M, Sizelove H. Feasibility and usefulness of a mobile health exercise intervention in women with lymphangioleiomyomatosis. Cardiopulmonary Physical Therapy Journal 2021:e7. [Google Scholar]
- 65.Cox NS, Eldridge B, Rawlings S, et al. A web-based intervention to promote physical activity in adolescents and young adults with cystic fibrosis: protocol for a randomized controlled trial. BMC Pulm Med 2019;19:253. 10.1186/s12890-019-0942-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lewis T. Improving quality of life in patients with cystic firbosis with exercise: CF Foundation impact grant update. Pediatric Pulmonology 2019:385–6. [Google Scholar]
- 67.Wagner B, Seuser A, Krüger S, et al. Establishing an online physical exercise program for people with hemophilia. Wien Klin Wochenschr 2019;131:558–66. 10.1007/s00508-019-01548-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Foronda CL, Kelley CN, Nadeau C, et al. Psychological and socioeconomic burdens faced by family caregivers of children with asthma: an integrative review. J Pediatr Health Care 2020;34:366–76. 10.1016/j.pedhc.2020.02.003 [DOI] [PubMed] [Google Scholar]
- 69.Suarez-Lledo V, Alvarez-Galvez J. Prevalence of health misinformation on social media: systematic review. J Med Internet Res 2021;23:e17187. 10.2196/17187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McMullan J, Crowe AL, Bailie C, et al. Improvements needed to support people living and working with a rare disease in Northern Ireland: current rare disease support perceived as inadequate. Orphanet J Rare Dis 2020;15:315. 10.1186/s13023-020-01559-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fidika A, Herle M, Lehmann C, et al. A web-based psychological support program for caregivers of children with cystic fibrosis: a pilot study. Health Qual Life Outcomes 2015;13:11. 10.1186/s12955-015-0211-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Linton L, Aruru M. Evaluating the readability of patient education materials across multiple sclerosis and rheumatoid arthritis disease states. J Am Pharm Assoc 2013;53:e28. [Google Scholar]
- 73.Ho G, Ueda K, Houben RFA, et al. Metabolic diet APP suite for inborn errors of amino acid metabolism. Mol Genet Metab 2016;117:322–7. 10.1016/j.ymgme.2015.12.007 [DOI] [PubMed] [Google Scholar]
- 74.Huang X, Chen L, Shao S. Developing and evaluating HE-APP: acceptability and usability of a smartphone APP system to improve self-management in Chinese patients with hemophilia. Haemophilia 2020:99. [Google Scholar]
- 75.Grande SW, Kotzbauer G, Hager A. Improving care for pediatric cystic fibrosis in Sweden using a successful mHealth patient support system. Pediatric Pulmonology 2017:435. [Google Scholar]
- 76.Breakey VR, Warias A, Ignas DM, et al. Usability testing of an online transition program for adolescents with hemophilia. Haemophilia 2012:31. [Google Scholar]
- 77.Khair K, Collier C, Holland M. The role of social networking in haemophilia management. Haemophilia 2010:129–30. [Google Scholar]
- 78.Khair K, Holland M, Carrington S. Social networking for adolescents with severe haemophilia. Haemophilia 2012;18:e290–6. 10.1111/j.1365-2516.2011.02689.x [DOI] [PubMed] [Google Scholar]
- 79.Balestri E, Vergnani S, Dall'Ara S. 'F (accio) C (entro)': Project for a smartphone application to increase adherence to aerosol treatment in adolescents with cystic fibrosis. Italian Journal of Pediatrics Conference: 25th Italian Congress of Cystic Fibrosis and the 15th National Congress of Cystic Fibrosis Italian Society Milan Italy, 2020. [Google Scholar]
- 80.Cox NS, Alison JA, Button BM, et al. Feasibility and acceptability of an Internet-based program to promote physical activity in adults with cystic fibrosis. Respir Care 2015;60:422–9. 10.4187/respcare.03165 [DOI] [PubMed] [Google Scholar]
- 81.Howard S, Speight L, Mills-Bennett R, et al. WS9.6 the all Wales adult cystic fibrosis centre (AWACFC) virtual instruction of exercise with technology to enhance care – VIEWTEC programme. J Cystic Fibrosis 2014;13:S20. 10.1016/S1569-1993(14)60063-1 [DOI] [Google Scholar]
- 82.Nilson J, Mulder K, Schachter C. Development, evaluation and updates of Hirt? (hemophilia injury recognition tool). Haemophilia 2018:136.30520541 [Google Scholar]
- 83.Ingravallo F, Vignatelli L, Pagotto U. Telemedicine with mobile Internet devices for innovative multidisciplinary patientcentred care of patients with narcolepsy. protocol of the randomized controlled trial TENAR (telemedicine for narcolepsy). Euro J Neurol 2020:516. [Google Scholar]
- 84.Parrott H, Elborn S, Madge S. ePS5.04 a digital solution for virtual consultation and sharing health data in adults with cystic fibrosis. Journal of Cystic Fibrosis 2019;18:S51. 10.1016/S1569-1993(19)30282-6 [DOI] [Google Scholar]
- 85.Lassandro G, Annichiarico G, Scherillo MR. EMO.TI.ON.: technologies for the safety of children with hemophilia. Blood Transfusion 2017:s539. [Google Scholar]
- 86.Rudolf I, Pieper K, Nolte H, et al. Assessment of a mobile APP by adolescents and young adults with cystic fibrosis: pilot evaluation. JMIR Mhealth Uhealth 2019;7:e12442. 10.2196/12442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Timmer MA, Kloek CJJ, de Kleijn P, et al. A blended physiotherapy intervention for persons with hemophilic arthropathy: development study. J Med Internet Res 2020;22:e16631. 10.2196/16631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sottilotta G, Arrigo P, Drago L. The HEMONLINE project: preliminary results. Haemophilia 2012:77. [Google Scholar]
- 89.Won AS, Barreau AC, Gaertner M, et al. Assessing the feasibility of an open-source virtual reality mirror visual feedback module for complex regional pain syndrome: pilot usability study. J Med Internet Res 2021;23:e16536. 10.2196/16536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Naik H, Balwani M, Doheny D. Experience with a pilot skype Internet support group for symptomatic patients with acute intermittent porphyria. Clinical Chemistry and Laboratory Medicine 2013:eA10. [Google Scholar]
- 91.Blackwell LS, Romero SL, Romero CV. CFfone: a social networking site for adolescents and young adults with CF. Pediatric Pulmonology 2012:430. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-060394supp001.pdf (65.9KB, pdf)
bmjopen-2021-060394supp002.pdf (58.9KB, pdf)
bmjopen-2021-060394supp003.pdf (235.4KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as supplementary information.