Abstract
Background:
Transnational immigration has increased since the 1950s. In countries such as the United States, immigrants now account for of the population. Although differences in health between immigrants and nonimmigrants are well documented, it is unclear how environmental exposures contribute to these disparities.
Objectives:
We summarized current knowledge comparing immigrants’ and nonimmigrants’ exposure to and health effects of environmental exposures.
Methods:
We conducted a title and abstract review on articles identified through PubMed and selected those that assessed environmental exposures or health effects separately for immigrants and nonimmigrants. After a full text review, we extracted the main findings from eligible studies and categorized each article as exposure-focused, health-focused, or both. We also noted each study’s exposure of interest, study location, exposure and statistical methods, immigrant and comparison groups, and the intersecting socioeconomic characteristics controlled for.
Results:
We conducted a title and abstract review on 3,705 articles, a full text review on 84, and extracted findings from 50 studies. There were 43 studies that investigated exposure (e.g., metals, organic compounds, fine particulate matter, hazardous air pollutants) disparities, but only 12 studies that assessed health disparities (e.g., mortality, select morbidities). Multiple studies reported higher exposures in immigrants compared with nonimmigrants. Among immigrants, studies sometimes observed exposure disparities by country of origin and time since immigration. Of the 50 studies, 43 were conducted in North America.
Discussion:
The environmental health of immigrants remains an understudied area, especially outside of North America. Although most identified studies explored potential exposure disparities, few investigated subsequent differences in health effects. Future research should investigate environmental health disparities of immigrants, especially outside North America. Additional research gaps include the role of immigrants’ country of origin and time since immigration, as well as the combined effects of immigrant status with intersecting socioeconomic characteristics, such as race/ethnicity, income, and education attainment. https://doi.org/10.1289/EHP9855
Introduction
Transnational immigration has increased since the 1950s, rising from immigrants per year in 1980 to per year in 2020.1–3 Of countries with reported statistics, the United States has the largest number of immigrants (i.e., foreign-born residents) at over or 15% of its total population.1,4,5 Estimates of immigrant populations are typically based on each country’s census and include residents who have crossed into its border for any reason. Some countries have fewer total immigrants overall but larger proportions of the total population who were foreign born.6 These countries include Germany (; 19%), Saudi Arabia (; 39%), United Arab Emirates (; 88%), Canada (; 21%), and Australia (; 30%).1 Among immigrants, there is diversity in race/ethnicity, country of origin/destination, socioeconomic status (SES), reason for immigration, refugee status, legal status, time since immigration, and more. These differences impact the immigrant experience, including access to housing, employment opportunities, and other factors that contribute to environmental exposures and ultimately, immigrant health.7–9 As immigrants become integrated into their host countries’ societies, understanding how the health of immigrants differs from nonimmigrants in relation to environmental exposures becomes increasingly important for each country’s public health and long-term health care planning.10
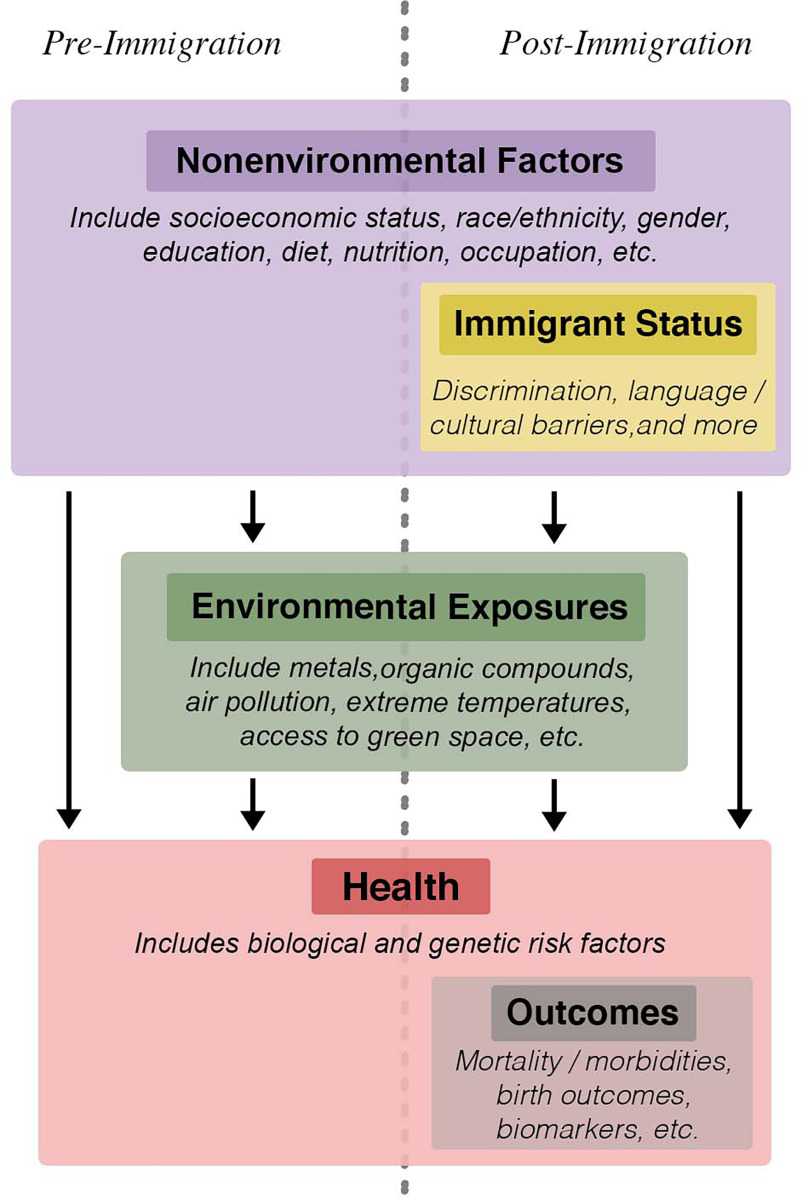
Health differences between immigrants and nonimmigrants in the general population are well documented.11–13 Depending on the health outcome, as well as individual characteristics such as race/ethnicity, country of origin, or time since immigration, immigrants may exhibit better or worse health outcomes compared with nonimmigrants.7,14 In the United States, although Black immigrants had a longer life expectancy than their nonimmigrant counterparts, Asian immigrants from China, Japan, and the Philippines had a shorter life expectancy compared with Asian nonimmigrants.7 For most immigrant groups in the United States, obesity was more prevalent among nonimmigrants compared with immigrants, but the reverse relationship was seen among those with origins in Cuba and India.14 Similarly, although diabetes risk among immigrants was lower compared with nonimmigrants overall, Black Caribbean and African immigrants had a higher risk compared with nonimmigrant Blacks in the United States.15 Time since immigration was also predictive of immigrant health trajectories in the United States: For diabetes, of which Black and Hispanic immigrants had a lower risk compared with Black and Hispanic nonimmigrants, the difference between immigrants and nonimmigrants became smaller as time since immigration grew.8 Previous studies on immigrant health disparities focused on differences in SES, race/ethnicity, diet, and cultural practices to explain immigrant health disparities.7,9 Differences in nonenvironmental factors, while contributing to immigrant health disparities, do not fully explain them.8,9,16,17 Thus, there is a need to explore other aspects of the immigrant experience, such as their environmental exposures, to assess whether they help explain immigrant health disparities. Figure 1 provides a conceptual framework of nonenvironmental factors and their relationships with environmental exposures and health. Differences between immigrants’ and nonimmigrants’ nonenvironmental experiences and environmental exposures may ultimately lead to health differences between the two groups.
Figure 1.
Conceptual figure of contributors to and pathways affecting immigrant health.
The contribution of the environment and related exposures to health disparities between immigrants and nonimmigrants is understudied. Prior work has documented numerous studies that explored exposure and health differences between immigrants and nonimmigrants in occupational settings.18,19 The present review focuses on environmental exposures but recognizes that occupational exposures are important health determinants; environmental and occupational exposures along with their health effects sometimes overlap and are difficult to separate. As early as the 1970s, some researchers have remarked that health differences between immigrants and nonimmigrants could be due to disparities in the environmental exposure itself or the health response to the environmental exposure.20–22 Environmental exposures, such as ambient fine particulate matter [PM in aerodynamic diameter ()] air pollution, are ubiquitous, and there is mounting evidence that they partially explain health disparities among groups of varying sociodemographic characteristics, such as race/ethnicity or SES.23–25 Environmental exposures are also regarded as a major cause for morbidity worldwide; of 84 risk factors, the Global Burden of Disease Study regards environmental exposures among the top contributors to lost disability-adjusted life years: ambient particulate air pollution ranked 10th, and unsafe water sources, 14th in 2017.26
To our knowledge, this work is the first attempt to comprehensively review the scientific literature at the intersection of environmental and immigrant health. Previous reviews focused on a related subtopic, such as environmental influences on immigrant respiratory health,27 the environmental health of Latino children,28 or the health of immigrants in Canada.29 To fill the knowledge gap, we conducted a state-of-the-science systematic review to describe and synthesize existing studies on a) environmental exposure disparities and b) health effect disparities attributable to environmental exposures among immigrants and between immigrants and nonimmigrants in the general population.
Methods
Literature Search
We conducted a systematic literature search for observational population exposure and epidemiologic studies that investigated environmental exposures and/or produced health effect estimates from environmental exposures separately for immigrants and nonimmigrants. Using the Medline/PubMed database, we searched for articles using a combination of the following keywords:
“environmental exposure,” “environment,” “exposure,” “pollution,” “air pollution,” “heat,” “temperature,” OR “weather,” AND
“immigrant,” “foreign born,” “nativity,” “migrant,” “native born,” or “US born.”
We conducted the search on 26 September 2021. The results included articles published as early as 1961 and as recently as 2021. We documented our search strategy in greater detail using a Population, Intervention, Comparison, Outcome, and Study Design (PICOS) worksheet (see the section “PICOS Worksheet and Search Strategy” in the Supplemental Material).30
Screening
We screened each initially identified article’s title and abstract for inclusion in this systematic review. We included only English-language original research articles, disqualifying any reviews, commentaries, and editorials. Studies were restricted to those that focused on humans in population health and epidemiologic settings. Furthermore, articles needed to compare the levels and/or effects of an environmental exposure in, at minimum, one immigrant and one nonimmigrant group. Each team member was instructed to use their expert judgment in deciding if the exposure of interest was environmental, keeping in mind that the focus of the review was on nonbiological physical and chemical exposures. Thus, included studies were anticipated to include environmental exposures, such as metals, organic compounds, air pollution, heat, and green space, measured at the individual level (e.g., as an endogenous factor via blood sampling) or estimated at the population level (e.g., pollution levels estimated via land use regression). We did not consider viral or biological pathogens. Because we were interested in immigrants in the general population, we excluded studies in occupational settings. Included studies could have an exposure or health outcome if they were observational in study design; nonpopulation-based studies (i.e., those that involved experimental or randomized exposure schemes) were excluded. Procedurally, each article was considered for inclusion by two team members working independently. In instances of disagreement for inclusion, a third member adjudicated and made the final decision. After the titles and abstracts of each article were screened, the full text of each remaining article was scrutinized for eligibility. Each article’s full text was reviewed by two separate members of the team. When there was a disagreement, a third member reviewed the full text and made the final decision for inclusion. Figure S1 illustrates the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for study inclusion.31
Full Text Review
For studies that were deemed eligible after the initial title and abstract screening, as well as the full text review, two members of the study team independently extracted the following information from each article: study design, location, time period and duration of study, population size, population comparison groups (e.g., nonimmigrants), exposure(s) considered, health outcome(s), statistical methods, and main results. The first author of this manuscript (K.C.F.) then compiled the results and independently verified extracted details in cases of conflicting information.
Results
Literature Search
In total, we screened the titles and abstracts of 3,705 articles. We excluded 3,488 that were not performed in human populations, did not consider immigrant status, were on occupational exposures, did not have comparison groups, were not population based, or were reviews or commentaries. For the remaining 84 articles, we completed a full text review. Of these, 50 were selected for inclusion in the study (Figure S1). These were studies on environmental exposures or environmental exposure health effects in immigrants vs. nonimmigrants in a nonrandomized observational setting (i.e., cohort study, case–control study, cross-sectional study, ecologic study, or time-series).
The findings of each of the 50 studies are summarized in Excel Table S1, organized into three broad categories of exposure: endogenous factors (i.e., blood metal and biomarker concentrations), air pollution, or other. In total, 23 articles focused on endogenous factors (46% of total), 17 on air pollution (34%), and 10 on other exposures (20%), such as temperature or green space (Figure 2). The majority (, 62%) of the studies were conducted in the United States, with Canada being a distant second (, 24%) (Figure 2A). Most studies investigated only exposure disparities (, 76%) rather than health disparities (, 14%) (Figure 2B). The remainder (, 14%) assessed both exposure and health disparities. Most articles were published within the past decade (2011–2021) (Figure 2C).
Figure 2.
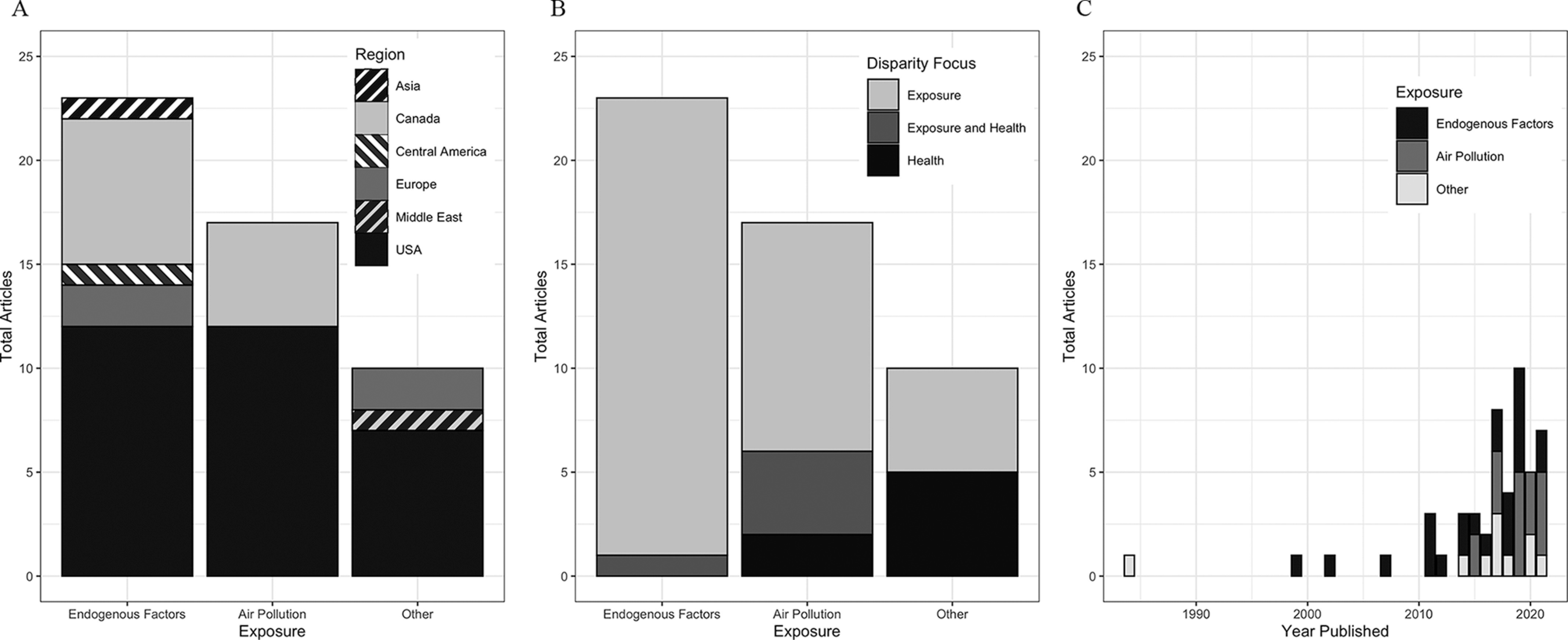
Included articles by exposures investigated, study region, disparity focus, and year published (). The graphs show the breakdown of the articles (A) between the region of study and the exposures investigated, (B) between disparity focus and exposures investigated, and (C) between exposures investigated and year published. Endogenous factors exposures include metals (lead, arsenic, mercury, cobalt, and cadmium) and organic compounds (e.g., phthalates, persistent organic pollutants) measured in sampled blood and urine; air pollution exposures include monitored or modeled ambient concentrations of nitrogen dioxide, ozone, black carbon, fine particulate matter (), and hazardous air pollutants assessed by the U.S. EPA in 2011; other exposures include parks/green space, flood risk, noise, sunlight, and extreme temperatures (extreme heat or cold). Raw data are found in Table S1. Note: EPA, Environmental Protection Agency.
Endogenous Factors
We identified 23 studies on endogenous factors, which included chemicals and metabolites detected in blood or other human tissues.32–54 Twelve were conducted in the United States, 7 in Canada, and 1 each in Costa Rica, Spain, Taiwan, and the United Kingdom. Of these studies, 22 estimated disparities in endogenous factors by immigrant status and not the resulting disparities in health effects from exposure. The remaining study investigated exposure and health (diabetes) disparities.32 There were 18 studies that investigated exposure disparities in metals, such as arsenic, lead, and cadmium, in blood or urine. Nine studies focused on organic compounds and included organobromines, such as polybrominated diethyl ether (PDBE; found in flame retardants), organochlorines, such as dichlorodiphenyldichloroethylene [; a metabolite of the pesticide dicholorodiphenyltrichloroethane (DDT, or )], and phthalates, which are found in many consumer products. Because metals and organic compounds have the propensity to affect fetal development,55,56 many of the studies focused on quantifying exposures in pregnant women or women of reproductive age. Some measured endogenous factors in newborns or young children, comparing those born to immigrant mothers to those born to nonimmigrant mothers.
The 18 articles that examined blood metal levels consistently found higher levels in immigrants compared with nonimmigrants.33–42,44–49,51,52 An early study in Los Angeles, California, measured blood lead levels (BLLs) in 1,932 pregnant women, of which 1,428 were immigrants.33 They found that immigrants had significantly higher BLLs and that 25 of the 30 cases of elevated BLL () were in immigrant women. Moreover, BLLs were dependent on time since immigration, with more recent immigrants having higher BLLs. A smaller study of 28 pregnant women conducted around the same time (1996–1999) in New York City also found that more recent immigrants had significantly higher BLLs.34
The comparison between immigrants and nonimmigrants in BLLs also applied to children.35–37,41 In a study of 1,148 refugee children in Massachusetts, the risk ratio for having an initial BLL was 12.3 [95% confidence interval (CI): 6.2, 24.5], comparing immigrant refugee children to nonimmigrant children.35 Among the immigrant refugee children, those who came from West Africa, the Near East, and South Asia were more likely to have elevated BLLs compared with those from Europe, Central Asia, and East Asia. Another study of BLLs further specified that immigrant refugee children from Nepal, Thailand, and Iraq to the United States had higher odds of elevated BLL compared with those from other countries.37 BLLs have also been measured in Burmese refugee children in Fort Wayne, Indiana.41 This relatively smaller study of 197 children with Burmese origins found that the prevalence of elevated BLL () was 7.1% among the Burmese refugee children compared with 0.7% among all children in Indiana.41 A study of the Burmese immigrant adult population residing in the Great Lakes Region in New York and reported consuming fish meals sourced from local water bodies in the past year found that they had higher blood cadmium, lead, and mercury levels than local licensed anglers who reported consuming fish caught in the past year.39 Using data from the U.S. National Health and Nutrition Examination Survey (NHANES) from 1999 onward, a study of children 6–18 years of age also found that BLLs were higher in immigrant children and adolescents than their nonimmigrant counterparts.36 Compared with immigrants of different world regions and to nonimmigrant adolescents, those from Mexico had the highest BLLs, blood mercury, and urinary cadmium levels. Among women of reproductive age (20–44 years of age), immigrants had higher blood lead, blood mercury, and urinary arsenic levels than nonimmigrants; these blood metal disparities by nativity were similar to those observed for race/ethnicity.38 Among pregnant women in Los Angeles, Hispanic immigrants also had higher urinary arsenic levels compared with Hispanic nonimmigrants.42 In the general NHANES adult population, data on 40,000 participants showed that urinary cobalt and blood cadmium levels were higher in immigrants compared with nonimmigrants.40
Similar to patterns observed for metals, organic compound exposures were often higher in immigrants compared with nonimmigrants.32,36,39,40,43,47,50,53,54 A small study of 24 pregnant women in California conducted with data collected from 1999 to 2001 found that immigrant women from Mexico had high blood PDBE concentrations.53 Among the immigrant women in this study, those who were more recent immigrants ( since arriving in the United States) had 4.2 ng/g lipid (calculated difference; 95% CI not available) lower PDBE concentrations than those who had been in the United States for longer. In adolescents 6–18 years of age sampled from NHANES, concentrations were higher in immigrants compared with nonimmigrants, with Mexican Americans as the population subgroup with the highest levels.36 Burmese immigrants consuming fish meals sourced from local waterbodies in the past year and residing in the Great Lakes Region in New York had higher blood concentrations of perfluoroalkyl substances (PFAS) than nonimmigrant licensed anglers consuming fish from local waterbodies in the past year and residing in the same area.39 In the general NHANES population, immigrants had higher organochlorine metabolite concentrations than nonimmigrants.40 However, for organic compounds, such as polychlorinated biphenyls and polyfluorinated compounds, immigrants had lower concentrations than nonimmigrants. This pattern held when comparing immigrants to nonimmigrants within racial/ethnic groups (non-Hispanic White, non-Hispanic Black, Hispanic). A more recent analysis of NHANES data found that urinary phthalate metabolite concentrations were generally higher among immigrants than nonimmigrants.43 In summary, although most studies based in the United States found that exposure to organic compounds was higher in immigrants compared with nonimmigrants, there were exceptions due to the variety and ubiquity of these pollutants in the environment.
Findings from Canada on immigrant disparities in metals and organic compound exposures were similar to those reported in the United States.44–50 Across five cities in Canada, a study of 123 pregnant women found that immigrants had significantly higher levels of metals and persistent organic compounds.47 A quartet of papers described blood metal disparities between newcomer ( since immigration) immigrant women of reproductive age (19–45 years of age) residing in two major cities and nonimmigrant Canadian women measured through a previous biomonitoring study.44–46,48 In a sample of 211 persons residing in Toronto, newcomer immigrant women had higher concentrations of blood cadmium,46 lead,44 and mercury.45 This set of studies investigated differences among immigrants by region of origin. For blood lead, those from Bangladesh had the highest BLL compared with those from other parts of South Asia and East Asia.44 For blood cadmium and mercury, East Asian women had higher levels compared with South Asian women.45,46 In a separate sample of 164 women of reproductive age residing in Vancouver, researchers found similar disparities between newcomer immigrant and nonimmigrant women, and between South Asian and East Asian newcomer immigrant women.48
An ongoing and larger effort to study endogenous factors, the Maternal–Infant Research on Environmental Chemicals (MIREC) cohort, yielded two more studies showing similar patterns for arsenic and persistent organic pollutants.49,50 Recruiting from multiple sites across Canada, immigrant pregnant women () had higher blood and urinary arsenic levels compared with 2,934 nonimmigrant pregnant women.49 Specifically, average arsenic concentrations measured during the first and third trimesters were significantly higher among immigrant women (; 95% CI: 0.79, 0.90) than nonimmigrant women (; 95% CI: 0.66, 0.71). This disparity was larger than those observed between groups by household income, education, or maternal prepregnancy body mass index. By region of origin, those from Asia had the highest levels, followed by Europe, the Caribbean, and Africa. Also using the MIREC cohort, persistent organic pollutants, such as organochlorines and polychlorinated biphenyls, were higher in immigrant mothers compared with nonimmigrant mothers.50
We identified four studies in this exposure category that were conducted outside North America.32,51,52,54 A recent study in Spain found that among children 1–16 years of age, the odds ratio (OR) of immigrants having elevated BLL () compared with nonimmigrants was 11.9 (95% CI: 4.5, 31.3).51 In this analysis, immigrant status was the risk factor with the highest OR compared with others such as gender, SES, parental education level, iron bioavailability in diet, iron deficiency, and overweight status. In Taiwan, researchers looked at the heavy metals in baby meconium of immigrant compared with nonimmigrant mothers.52 Lead and arsenic levels in those born to immigrant mothers were significantly higher than those born to nonimmigrant mothers. They did not detect significant differences in mercury and cadmium levels. In another study, researchers in Costa Rica studied urinary ethylene, a metabolite proxy of Mancozeb, which is an aerially spayed agricultural fungicide.54 Immigrant women from Nicaragua () and El Salvador () had, on average, 6.2% (95% CI: 1.0, 13%) higher levels of ethylene thiourea than nonimmigrant women.54 In London, England, South Asian immigrants had three to nine times higher blood concentrations of organochlorines, such as , , beta-hexachlorocyclohexane (), and polychlorinated biphenyl-118 (PCB-118), compared with European White nonimmigrants.32 Furthermore, immigrant South Asians diagnosed with diabetes mellitus were much more likely to have high and levels compared with immigrant South Asians without a diabetes diagnosis.
Air Pollution
We identified 17 total studies that analyzed immigrant disparities in exposure to or health effects from air pollution.57–73 Of the 17 studies, 12 were based in the United States and 5 in Canada. These studies often found that immigrants or areas with higher immigrant proportions had higher exposures to air pollution compared with nonimmigrants or areas with lower immigrant proportions.
In the United States, there was a range of small area-level studies and large regional studies with individual data that found disparities in exposures to monitored black carbon (BC)72 and ozone (),68 as well as model-predicted fine particulate matter ()61,63,65,73 and hazardous air pollutants (HAPs).57,66,67,69 HAPs are 187 toxic air chemicals, including benzene, perchloroethylene, and methylene chloride, on a list maintained through the U.S. Environmental Protection Agency’s (EPA) 2011 National Air Toxics Assessment.74 In California, an area-level study found that communities with high immigrant Vietnamese populations had higher BC levels compared with the statewide mean BC concentrations.72 Two counties with a high Vietnamese immigrant proportion, Alameda and Orange, were the two counties with the highest levels in the state, with BC levels 10 times higher than the state average. A similar trend was found for . In a national cohort of 4,600 children, researchers found that overall, immigrant and nonimmigrant children of Mexican parental origin, compared with non-Hispanic White children, lived in counties with three times more days with elevated levels.68 On average, children of Mexican origins with at least one immigrant parent had, on average, 24.2 annual days with elevated , whereas children with Mexican origins with nonimmigrant parents had, on average, 21.4 annual days with elevated .
Four studies in the United States investigated immigrant exposure disparities to HAPs.57,66,67,69 In Miami, Florida, Hispanic immigrants were exposed to a larger number of HAPs than nonimmigrant Hispanics and nonimmigrant populations of other ethnicities.67 A separate national analysis with aggregated U.S. Census demographic estimates for each of 12,516 school districts concluded that the proportion of immigrant children in a school district was positively associated with higher levels of HAPs.66 In Houston, Texas, the proportion of residents who were immigrants in a census tract was positively associated with higher levels of HAPs from on-road sources, according to estimates from the 2011 U.S. EPA National-Scale Air Toxics Assessment.69 In the national Early Childhood Longitudinal Study, 32% of the children of immigrant mothers were exposed to the highest quartile of HAPs compared with 21% of children of nonimmigrant mothers.57 A recent study investigated multigenerational immigrant trajectories in exposure to among third-grade schoolchildren.65 Immigrant schoolchildren and nonimmigrant schoolchildren with two immigrant parents had significantly higher exposures than nonimmigrant schoolchildren with at least one nonimmigrant parent.
Another recent U.S. study investigated the relationship between immigrant proportion at the census tract level and concentrations.61 Overall, areas with a higher immigrant proportion had higher annual average in both 2000 and 2010, with higher levels in areas with higher proportions of immigrants from Asia, Latin America, and Africa. Another study using 2015 data from a different exposure prediction model also found that U.S. Census tract immigrant percentage was associated with higher exposures.63 In a smaller setting using Texas school districts, a similar analysis found county-level immigrant children proportion was positively associated with higher nitrogen dioxide () levels.58
Most studies in Canada were national in scale. Four studies used individual-level data collected through the Canadian Census, and model-predicted air pollution.59,62,64,71 The study with the longest study period, which combined data from separate cohorts spanning 1991 to 2016, found that immigrants had exposures 20% higher than residents born in Canada.64 The smallest Canadian study using only 2006 data similarly found that immigrants had higher exposure to than nonimmigrants.71 Notably, they found that even as time since immigration increased, immigrants in urban-core areas had higher exposure to (8.41–) than nonimmigrants (). The most recent study estimated long-term exposure to be among immigrants and among nonimmigrants.62 Another study found a similar overall pattern in exposure disparities but additionally reported that those with a longer time since immigration had lower exposures compared with those with shorter times since immigration.59 This study also found that average exposure was higher among immigrants () compared with nonimmigrants (), as was average exposure at for immigrants compared with in nonimmigrants. Aside from these national studies with individual data, a recent study on Toronto’s Census dissemination areas showed that ultrafine particle (UFP) concentrations along school commutes were higher in areas with a higher immigrant proportion.60
Six studies investigated the disparities between immigrants and nonimmigrants in health effects resulting from air pollution exposure.57,59,62,64,70,73 A study based in the San Joaquin Valley in California investigated the relationship between air pollution exposure to expectant Hispanic mothers and neural tube defects (NTDs) in their newborns.70 Although NTDs were more prevalent among those born to Hispanic immigrant mothers than U.S.-born Hispanic mothers, carbon monoxide, nitrogen oxide, and exposures were more strongly associated with NTDs among nonimmigrant mothers than among immigrant mothers. Another study, in Boston, Massachusetts, estimated that the negative effect of maternal exposure to during pregnancy on fetal growth, measured by infant birth weight, was more severe among those born to immigrant mothers than nonimmigrant mothers.73 In the children of the Early Childhood Longitudinal Study, the estimated effect of HAPs exposure on neurodevelopment measured via the Bayley’s Short Form–Research Edition (BSF-R) was more detrimental among children born to immigrant mothers than those born to nonimmigrant mothers, although the difference in effect estimates was not statistically significant [immigrant mothers: (95% CI , ) vs. nonimmigrant mothers: (95% CI , 0.03); ].57
In Canada, the direction and magnitude of the disparity between immigrants and nonimmigrants in the estimated effect of were inconsistent across years.64 Although immigrants enrolled in the cohort in 2001 had higher risk for various cardiovascular disease mortality associated with increased exposure compared with nonimmigrants, those enrolled in other years (1991, 1996, selected years from 2003 to 2016) did not. In a recent study, researchers reported that per increment in , since arrival had a hazard ratio of 0.98 (95% CI: 0.83, 1.16) for nonaccidental mortality, which was lower than that of nonimmigrants, whose hazard ratio was 1.14 (95% CI: 1.07, 1.23).59 For cardiovascular mortality, the hazard ratio for cardiovascular mortality per increment in was estimated to be 1.22 (95% CI: 1.12, 1.34) in immigrants, which was larger in magnitude compared with 1.12 (95% CI: 1.07, 1.18) in nonimmigrants, although the results were not statistically different.62 There were similar health effect disparities from exposure for cerebrovascular mortality and respiratory disease mortality. This study also observed that more recent immigrants (with since immigration) had a higher mortality risk from than more established immigrants and nonimmigrants. Disparities by place of birth, age of immigration, and neighborhood ethnic concentration were comparatively small and negligible. In summary, there was a small number of studies, most of which were conducted in Canada, that investigated immigrant disparities in health effects from air pollution.
Other Exposures
We identified 10 studies that investigated immigrant environmental disparities other than endogenous factors or air pollution.75–84 Seven of the 10 studies were conducted in the United States. They examined environmental disparities in proximity to green spaces/parks, chemical concentrations, and residence within flooding zones. For disparities in health response to environmental conditions, studies examined self-reported health and mortality from green space exposure, insomnia from noise, melanoma from sun exposure, and heat- and cold-related mortality.
Two studies investigated immigrant disparities in proximity to green space or park access.76,77 Both studies were area based and used U.S. Census data to ascertain immigrant proportion. The first, conducted in El Paso, Texas, found that neither the number of park facilities nor amenities was associated with tertiles of immigrant proportion by census tract.77 The second study, which was national in geographic scope, found that immigrant proportion in a U.S. Census tract was negatively associated with green space, measured as normalized difference vegetation index (NDVI) and the enhanced vegetation index (EVI), which are two related satellite remote sensing greenness indices.76 Furthermore, they found differences in associations between immigrant proportion and greenness depending on the immigrant’s region of origin, with the strongest negative associations with greenness for tracts with high immigrant proportion of immigrants from Latin America.
Another study employed an area-level approach to compare toxicity-weighted chemical concentrations in immigrants vs. nonimmigrants in the United States.84 The area unit of analysis was a public use microdata area (PUMA), which is a U.S. Census Bureau–defined area with at least 100,000 residents. The toxicity-weighted chemical concentration in each census tract was based on the Risk-Screening Environmental Indicators model from the U.S. EPA.85 Nationally, they found that immigrant proportion (i.e., the fraction of the population that was immigrants) was not associated with higher chemical releases reported in the Toxics Release Inventory for PUMAs. However, when assessing only the wealthier areas, immigrants from Mexico were more likely than immigrants from Europe, Asia, or Latin America (excluding Mexico) to reside in areas with the highest chemical toxin release.
Seven studies used individual-level data.75,78–83 In a sample of 213 Hispanic immigrants and 867 nonimmigrants residing in two U.S. cities, researchers found that Hispanic immigrants were more likely to reside in historically flood-prone areas in Houston, but not in Miami.78 A study in Brussels, Belgium, found disparities in health response to urban green space measured via NDVI.79 Given the same NDVI increment, immigrants to Belgium from high-income countries had the lowest odds for poor self-rated health and natural cause mortality compared to nonimmigrants or immigrants from low- and middle-income countries, as did nonimmigrants. Disparities between the effect estimates were not statistically significant. Four studies used individual-level data to explore differences in the health response to environmental conditions, such as sunlight, noise, and weather.75,81–83 An early study in Australia observed that immigrants had much lower odds of developing malignant melanoma compared with nonimmigrants, even when the nonimmigrants had relatively low total hours of sunlight exposure.81 Among immigrants, those who arrived later in life had lower risks for melanoma compared with immigrants who arrived during childhood. Disparities in insomnia due to noise exposure were investigated among immigrant and nonimmigrant Latinos residing in the United States in Chicago, Miami, the Bronx, and San Diego.82 This questionnaire-based study found that although overall increased noise exposure was associated with insomnia, the findings did not provide strong evidence that immigrant Latinos were differentially affected compared with nonimmigrants. A study in the United States used citizenship as a proxy for immigrant status to estimate disparities in heat-related mortality.83 Using data on the cause of death on death certificates for persons 5–64 years of age, the researchers found that noncitizens were more likely to die from heat exposure than U.S. citizens. The differences in standardized heat-related mortality ratio between noncitizens and citizens were largest in the 5- to 17- and the 18- to 24-years-of-age ranges. In France, researchers conducted a large matched case–control study of 573,384 immigrant deaths matched to an equal number of nonimmigrant deaths based on sex, month-year of birth, and residential commune to estimate potential disparities in temperature effects on mortality.75
Overall, the estimated effects of temperature on mortality were similar between immigrants and nonimmigrants. There were some significant differences when comparing those who emigrated from Southern Europe to their nonimmigrant controls: In the Mediterranean and Continental regions of France, the Southern Europe immigrants’ attributable mortality fraction due to cold exposure was higher than nonimmigrants; in the Northern regions of France, the Southern Europe immigrants’ attributable mortality fraction due to heat exposure was lower. A separate study using daily mortality data in Kuwait from 2010 to 2016 found that non-Kuwaitis had a higher mortality risk from extreme heat exposure compared with Kuwaitis.80
In this group of studies that explored exposures other than endogenous factors and air pollution, there was a variety of increasingly health-relevant factors (e.g., green space, heat, flood risk). In the 10 included studies, there was a balance between area- and individual-based analyses. Compared with the endogenous factors and air pollution groups of studies, there was a larger proportion that investigated health disparities. Similar to the previous groups of studies, the overwhelming majority of the articles were conducted on populations in North America.
Research Synthesis
Overall, most included studies reported that immigrants, compared with nonimmigrants in the same country of residence, were exposed to higher levels of detrimental environmental stressors such as metals, organic chemicals, and air pollutants (Tables 1 and 2). Compared with the number of studies documenting exposure disparities by immigrant status, there were relatively few studies that reported that immigrants were differentially affected by environmental exposures compared with nonimmigrants in their respective countries.
Table 1.
Summary of findings on exposure disparities from the literature review.
| Exposure | Main findings |
|---|---|
| Endogenous factors | |
| Metals (biomarkers such as lead, arsenic, mercury, cobalt, cadmium measured in blood and urine) |
|
| Organic compounds (biomarkers of exposure measured in blood and urine) |
|
| Air pollution | |
| Black carbon (monitored at ground level) |
|
| Ozone (monitored at ground level) |
|
| (modeled) |
|
| HAPs (2011 U.S. EPA National Air Toxics Assessment) |
|
| (variety of exposure prediction models) |
|
| Other | |
| Green space (city-level map or satellite imagery) | |
| Flood risk (historical maps) |
|
Note: Further details on each study are found in Excel Table S1. EPA, Environmental Protection Agency; HAPs, hazardous air pollutants; , nitrogen dioxide; PDBE, polybrominated diethyl ether; PFAS, perfluoroalkyl substances; , fine particulate matter; , dichlorodiphenyldichloroethylene.
Table 2.
Summary of findings on health disparities from literature review.
| Outcome | Main findings |
|---|---|
| Endogenous factors | |
| Diabetes mellitus (prospective cohort) |
|
| Air pollution | |
| NTDs (birth defects monitoring) |
|
| Fetal growth (birth cohort) |
|
| Mortality (census-based cohort and health survey) | |
| Other | |
| Insomnia (home sleep testing) |
|
| Mortality (national death certificate registrssssies) |
|
| Melanoma (national schoolchildren cohort) |
|
Note: Further details on each study are found in Excel Table S1. , beta-hexachlorocyclohexane; , fine particulate matter; , nitrogen dioxide; NTD, neural tube defect; , dichlorodiphenyldichloroethylene.
Excel Table S1 details each of the included studies, including the disparity focus, exposure, study location, methods, immigrant and comparison groups, and results and main conclusions. It also summarizes whether a study controlled for SES characteristics that intersect with immigrant status in affecting environmental exposure or health disparities. These characteristics include race/ethnicity, income, education, among other related variables. Although 32 of the 50 studies controlled for SES characteristics, only 7 studies calculated immigrant subgroup-specific exposure or health effect estimates (e.g., among immigrants, the effect of income or education) via stratification, interactive terms, or effect modification analyses. This points to a research gap in understanding immigrant environmental health disparities.
Discussion
We propose a conceptual framework to illustrate the contributors to and pathways affecting immigrant health (Figure 1). Individual immigrant status can intersect with SES, race/ethnicity, gender, and other characteristics to affect levels of discrimination, language and cultural barriers, and other challenges of access, which, along with directly affecting individual health outcomes, can affect one’s environment, including their residence and its surroundings.18,86–88 Along with other nonenvironmental factors, individual immigrant status can lead to differences in that individual’s community-level vulnerability, which includes environmental exposures, such as metals, air pollution, and extreme temperatures, among others, and ultimately affects individual-level risk of health outcomes.89 In fact, immigrant status can affect environmental exposure levels and consequent health effects through multiple pathways, likely on different spatial scales. Contextual factors at the household and community (e.g., municipal, national) levels could interact with individual immigrant status to affect environmental exposure and health.9,86,87 For example, an immigrant in one community that has had low rates of immigration may experience challenges that increase their levels to or health risks from environmental exposures compared with a comparable immigrant in another community with higher rates of immigration and increased resources to integrate newcomers into its society (e.g., assistance for housing, health literacy programs). Although Figure 1 does not exhaustively list all health determinants and potential pathways, it illustrates that pre- and post-immigration nonenvironmental factors and environmental exposures together can theoretically affect health and observed post-immigration outcomes through distinct pathways.
Our review identified articles that support links between immigrant status and environmental exposure levels, which can be consequential for health (Figure 1). Such disparities in endogenous factors and air pollution exposure could potentially lead to important differences in health outcomes between immigrants and nonimmigrants, as well as among immigrants themselves. Of the 50 studies reviewed, 43 investigated disparities in exposures that are known to be harmful to human health. Metals such as arsenic are linked to increased risk for cancer,90 diabetes,90 and cardiovascular disease among adults.55,91 Furthermore, these exposures were often measured in reproductive age or pregnant women because they can cross the placenta and into the fetus, affecting neurodevelopment.92–94 Similarly, organic chemicals such as organobromines (e.g., polybrominated diphenyl ethers; PDBE), organochlorines (e.g., ), and phthalates disrupt endocrine function and can impair human reproduction, neurodevelopment, and the allergic response.95,96 Besides metals and organic chemicals, we found evidence for disparities in exposures to HAPs and in studies conducted in the United States. The list of HAPs is maintained by the U.S. EPA and includes air pollutants known to cause cancer and other serious effects.74 The identified studies suggest that Hispanic immigrants living in the United States would have higher lifetime cancer risks compared with nonimmigrant populations.66,67,69 Another class of air pollutants, , consists of ambient particles that can reach the alveoli, the deepest parts of human lungs responsible for gas exchange. exposure has been linked to oxidative stress, inflammation, among other negative health effects.23,97 The identified studies estimated that exposure disparities lead to higher mortality and morbidity burdens in immigrants compared with nonimmigrants.61,64,71
Potential differences in environmental exposures by immigrant status may be linked to nonenvironmental factors, such as settlement patterns, cultural differences, and dietary preferences. In North America, immigrants have historically settled in more urban areas in gateway cities, close to places where they have existing family or cultural ties.98,99 Overall, immigrants also tend to have lower annual household incomes than nonimmigrants.100 Given that more affordable urban areas are often more polluted,25,84 immigrants with limited financial resources are more likely to live in more polluted areas, exposing them to higher chemical and other pollution compared with nonimmigrants overall. In addition to differences in affordability between neighborhoods, immigrants face nonenvironmental factors, such as discrimination, which can residentially segregate them to neighborhoods of lower environmental quality (e.g., dirty air, poor water supply, contaminated land).18,101
Thus, when comparing communities, there could be associations between immigrant composition and environmental risks. For example, Hispanic immigrants were more likely than nonimmigrants to reside in flood zones in Houston, but not in Miami.78 The researchers suggested that this could be because Miami’s desirable and higher SES neighborhoods are more likely to be in flood zones. Another study linked housing conditions to immigrant disparities, finding that, in Costa Rica, immigrants had lower access to proper housing conditions, which likely led to higher exposures to pesticides.54 Aside from settlement patterns, immigrants maintain cultural practices that persist after immigration that can lead to higher levels of endogenous factors. One study referred to the use of traditional remedies as a likely cause of high blood levels among Burmese immigrants.41 A digestive remedy, Daw Tway, was tested to have lead concentrations of 520 ppm. The use of imported cosmetics or pottery with high metal content and oral exposure via pica or through metal jewelry could also explain higher metal concentrations detected in immigrants.33,34,39,48 Also, immigrants can have markedly different diets compared with nonimmigrants. Consumption of imported foods could explain higher metal and organic chemical concentrations in immigrants.32,48 One study documented that Burmese immigrants consumed caught sportfish from the Great Lakes region at higher rates than nonimmigrant licensed anglers, likely explaining higher blood mercury in this group of immigrants.45 Although higher blood metal concentrations among immigrants compared with nonimmigrants could partially be due to pre-immigration exposures, the identified literature included numerous examples of higher exposures post-immigration as a result of settlement patterns,54,78 cultural practices,39,41,48 and dietary practices.32,39,45,48
Aside from disparities in environmental exposure levels, differences can also exist between immigrants and nonimmigrants in their health responses associated with a given level of environmental exposure owing to effect modification or interactions with nonenvironmental factors. However, few studies (12 of the 50 studies) investigated health disparities associated with environmental exposures by immigrant status (Figure 2B). Collectively, these studies provide evidence of more severe health detriments from air pollution (i.e., , , carbon monoxide) in immigrants compared with nonimmigrants on fetal growth,73 risk for NTDs,70 and mortality.59,62,64 Although the Canadian studies used national data,59,62,64 many of the studies in the United States were regional in geographic scope.70,73 Besides air pollution exposure, one study found no evidence of immigrant disparities in the health effects of noise and insomnia,82 whereas three identified disparities in the effect of extreme temperature on mortality.75,80,83 In summary, there are few studies that estimated differences in health response associated with a given level of environmental exposure. Adding to this, the Canadian air pollution studies used similar data sets to estimate health effects. Thus, assessing disparities in health effects from environmental exposures by immigrant status is a clear knowledge gap that future studies should aim to address.
Future studies should aim to elucidate how environmental exposure and environmental health disparities differ among immigrants themselves. As illustrated in Figure 1, immigrant status encompasses not only whether or not one is foreign born but also detailed characteristics such as time since immigration and place of origin, which can be consequential for health. Time since immigration is a distinguishing characteristic among immigrants because it approximates the level of acculturation: the degree to which immigrants resemble nonimmigrants in the destination country. As immigrants become acculturated and integrated into the society of their destination countries, they may adopt residential, cultural, and dietary preferences that more closely resemble those of nonimmigrants. Studies showing declining environmental exposure disparities between immigrants and nonimmigrants based on time since immigration support this acculturation hypothesis.33,34,59 Furthermore, the health risk from was found to be more similar between established immigrants and nonimmigrants than between recent ( since immigration) immigrants and nonimmigrants.62
Studying immigrant differences by time since immigration requires understanding that paths toward acculturation are not equally available to all immigrants. How acculturated immigrants become may depend on race/ethnicity, SES, education, and other factors.9 Immigration acculturation may also be influenced by area-level factors, such as the presence or formation of immigrant enclaves. Another important distinguishing feature among immigrants is their place of origin. Depending on the immigrant’s place of origin, pre-immigration environmental exposures and nonenvironmental factors would differ. Although many studies did not investigate disparities by place of origin, some other studies identified exposure disparities by place of origin.32,37,45,49,61,75 In total, among the 50 identified articles, 11 explored differences by time since immigration and 14 explored differences among immigrants by place of origin. An additional knowledge gap is the contribution of refugee status, which can impact access to housing, employment opportunities, health care, and other factors leading to environmental exposure or consequent health disparities when compared with other immigrants or the native-born. The four reviewed studies that specified refugees as their study population did not investigate differences in environmental exposures or health outcomes between refugees and nonrefugee immigrants.35,37,39,41 Given that immigrants are not a monolithic group, future studies are needed to gain a deeper understanding of how environmental health disparities arise between immigrants and nonimmigrants as well as among immigrants by evaluating potential differences by characteristics such as time since immigration, place of origin, and refugee status. Moreover, immigrant status intersects with SES characteristics, such as income and education, in ways that could affect environmental exposure levels and health disparities. Although 32 of the reviewed studies accounted for SES characteristics in their analysis of exposure levels or health effects in immigrants compared with nonimmigrants (Excel Table S1), only 7 conducted further analysis with stratification, interactive model terms, or effect modification by intersecting SES characteristics, such as race/ethnicity,36,42,43,65,83 income,79 or neighborhood acculturation factors, such community immigrant proportion and foreign language speakers.70 When possible, future studies should address knowledge gaps in the combined effects of immigrant status and SES, race/ethnicity, or related characteristics, as well as the pathways through which immigrant status could influence environmental health by including household or area-level contextual variables.
Although published work on this topic has increased in recent years (Figure 2), challenges remain to conducting research on the environmental health of immigrants. The collection and availability of health data that contain or are linked to information on immigrant status are limited, especially outside of North America. Evidence is particularly needed for areas outside of North America, given that 43 of the 50 studies identified in this review were conducted in the United States or Canada. Although this is partially explained by the United States and Canada being top destinations for immigrants in the late 20th and early 21st centuries,1 it points to a lack of research on transnational immigrant health outside North America. Increased resources dedicated to studying the environmental health of immigrants can lead to new insights on health in a world with increased mobility. For example, although studies have addressed disparities among immigrants by country of origin in a destination country (e.g., how different immigrant groups fare in the United States), an analysis that investigates potential exposure or health disparities by destination country among immigrants from a specific place (e.g., country or region) of origin was not identified (e.g., how immigrants from Mexico fare across different destination countries). With increased collaboration leading to multicountry data, such a study could inform on potential environmental health disparities experienced by immigrants from a specific region in different destination countries.
Similarly, a multicountry comparison of immigrants by time since immigration could inform on whether acculturation effects (i.e., immigrants experiencing similar exposures and health effects as nonimmigrants) differ between destination countries. A prior review of mortality risks of immigrants in different destination countries found complex patterns.102 Those who immigrated to a country with a similar climate as their originating country tended to have lower mortality risks compared with the nonimmigrants of their destination country, or a mortality advantage. In contrast, those who moved from a country with a warmer climate to a country with a colder climate did not have a mortality advantage and exhibited higher cardiovascular mortality compared with the nonimmigrants of the destination country. That study did not estimate temperature exposure or temperature–mortality disparities between immigrants and nonimmigrants. Increasing efforts to collect data on place of origin and time since immigration would also address a limitation of exposure assessment. Specifically, although disparities by immigrant status in air pollution, temperature, noise, and green space can be evaluated in the destination countries post-immigration, disparities in endogenous factors, such as metals and organic compounds, cannot be explicitly linked to the post-immigration environment. In other words, for endogenous factors, the pre- and post-immigration environments need to be considered because, depending on the specific metal or organic compound, endogenous factors could accumulate and be present in the blood or other body samples years after exposure. This motivates the collection of time since immigration and place of origin data because such variables can potentially adjust for pre-immigration exposures that were not measured. In summary, assessing environmental health disparities between immigrants and nonimmigrants, as well as among immigrants, remains challenging due to data limitations.
Our review has some limitations. In our search for studies on environmental health disparities between immigrants and nonimmigrants, some relevant studies may have not been captured by our search terms. Because this research area is relatively small and often a peripheral focus of larger studies, there is not a consistent list of terms that encapsulates the topic of immigrant environmental health disparities. To maximize our chances of screening all relevant studies, we used terms as general as “environmental exposure” and “pollution” but also specific terms of well-established exposures such as “air pollution” and “temperature.” Along the same lines, to increase our chances of finding studies that involved comparisons between immigrants and nonimmigrants, we used terms such as “migrant,” “nativity,” and “foreign born.” However, we likely missed studies that could have been relevant for this systematic review. For example, studies on immigrant disparities in water contamination, soil contamination, and specific pathogens could have been missed by our search terms. Adding to this, although we included “US born” as a search term because of an understanding that it is an established term and that many immigrant health disparities have been conducted in the United States, doing so could have biased our literature search toward studies based in the United States and excluded studies in other locales. Although we did not require the term “US born” and included other relevant terminology (“immigrant,” “foreign born,” “nativity,” “migrant,” or “native born”), we did not incorporate analogous terms for other countries (e.g., “Canadian born”).
An additional limitation of our search terms is the lack of terms such as “health” or “health disparities.” Our search could have missed studies that focused specifically on immigrant health disparities; however, this subset would have been unlikely to yield additional studies that investigated immigrant health disparities from environmental exposures, given that the latter was well covered by our search terms. Besides search terms, some studies may have been missed because we considered only English language publications. Moreover, as we targeted observational population exposure and epidemiologic studies, we may have excluded potentially informative clinical and randomized controlled studies that describe immigrant disparities related to environmental exposures and consequent health outcomes. In the future, as more studies investigate immigrant environmental health disparities, we anticipate increased consistency in the terms used to describe research on environmental health disparities between immigrants and nonimmigrants. More studies would allow a more extensive evaluation of the existence of immigrant disparities in environmental exposure levels and health effects.
Another limitation is that there is substantial overlap between exposures experienced in occupational and nonoccupational settings. For our review, we focused on research in nonoccupational settings. However, for some studies, especially those on endogenous factors measuring levels of metals and organic compounds, disparities between immigrants and nonimmigrants were likely related to different experiences in occupational and nonoccupational settings.33,38,40,42,43,54 For assessing environmental exposures and their health consequences, the demarcation between exposures from occupational and nonoccupational settings is not clear-cut. Researchers will continue to face the challenge of distinguishing between occupational and nonoccupational exposures when investigating immigrant environmental health disparities. In the future, we could strive to disentangle exposure and health differences stemming from occupational and nonoccupational settings by simultaneously collecting data on immigrant status and occupation. Finally, as with all literature reviews, publication bias most likely limited our ability to identify all studies that investigated immigrant environmental exposure and health disparities. This bias likely reduced the number of included studies that had null findings (e.g., no differences in exposure or health disparities stemming from exposure between immigrants and nonimmigrants).
Despite some limitations, this review has numerous strengths. We posed a question at the innovative intersection of immigrant and environmental health then summarized findings on whether immigrants experience disparate levels of or effects from environmental exposures. Our review was comprehensive in that it covered a wide variety of exposures ranging from metals to organic compounds, air pollution to noise to extreme temperatures, green space to flood risk, and more. Furthermore, our review addresses an area of increasing public health relevance. In countries with high immigrant populations, often with an increasing number of aging immigrants, it is a priority to better understand the role of the environment in the etiology of health differences between immigrants and nonimmigrants.103
Conclusion
The environmental health of immigrants in the general population has received increased research interest in recent years, as demonstrated by a growing number of relevant studies. However, when compared with the body of literature on disparities by sociodemographic characteristics, such as race/ethnicity and SES, there remains a dearth of original research on environmental health disparities by immigrant status. In this state-of-the-science review, we found numerous studies concluding higher metal, organic compound, and air pollution (i.e., hazardous air pollutants or ) exposures in immigrants compared with nonimmigrants.
Our review points to clear research gaps and future directions in the environmental health of immigrants, thus we offer the following specific recommendations. First, future studies should seek to investigate differential health effects from environmental exposures between immigrants and nonimmigrants. This includes the need for studies focused both on exposure itself and on the subsequent health outcomes. Our literature search yielded relatively few studies on differential health effects from environmental exposures. Furthermore, the severity to which immigrants experience health effects from environmental exposures compared with nonimmigrants is unclear. Second, the majority of the reviewed studies were conducted in North America, pointing to a need for research in other countries that have large immigrant populations (e.g., Germany, Saudi Arabia, United Arab Emirates, Australia). Furthermore, in the reviewed literature, few studies looked beyond immigrant status (i.e., whether one is foreign born). Some studies showed that there could be additional environmental exposure and health disparities by detailed immigrant characteristics, such as country of origin and time since immigration. Therefore, future analyses of immigrant environmental health should explore disparities beyond simply foreign-born status. Adding to this, immigrant status may interact with SES; future research should address the combined effects of immigrant status with intersecting characteristics such as race/ethnicity, income, and education attainment. Finally, given that data on these issues are often unavailable, more detailed data collection and curation are needed for impactful research on this emerging topic because many countries have substantial and growing immigrant populations. With a greater understanding of the role environmental exposures play in influencing immigrant health disparities, stakeholders would better anticipate emerging health needs of the population and design appropriate environmental and health policies.
Supplementary Material
Acknowledgments
This publication was developed under assistance agreement RD835871 awarded by the U.S. Environmental Protection Agency (EPA) to Yale University (to M.L.B.). It has not been formally reviewed by the U.S. EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the agency. The U.S. EPA does not endorse any products or commercial services mentioned in this publication. Research reported in this publication was also supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health (NIH) under award R01MD012769 (to M.L.B.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Migration Policy Institute. 2021. International migration statistics. https://www.migrationpolicy.org/programs/data-hub/international-migration-statistics [accessed 29 October 2021].
- 2.Martin P. 2013. The global challenge of managing migration. Popul Bull 68(2):1–16.25995521 [Google Scholar]
- 3.Global Migration Data Portal. 2021. International migrant stocks. https://www.migrationdataportal.org/themes/international-migrant-stocks [accessed 28 October 2021].
- 4.U.S. Census Bureau. 2019. American Community Survey. https://data.census.gov [accessed 28 October 2021].
- 5.United Nations Department of Economic and Social Affairs: Population Division. 2020. International Migrant Stock 2020: Destination, Table 1: International Migrant Stock at Mid-Year by Sex and by Region, Country or Area of Destination, 1990–2020. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/undesa_pd_2020_ims_stock_by_sex_and_destination.xlsx [accessed 29 October 2021].
- 6.Pison G. 2019. The number and proportion of immigrants in the population: International comparisons. Popul Soc (Paris) 563(2):1–4. [Google Scholar]
- 7.Singh GK, Miller BA. 2004. Health, life expectancy, and mortality patterns among immigrant populations in the United States. Can J Public Health 95(3):I14–I21, PMID: , 10.1007/BF03403660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engelman M, Ye LZ. 2019. The immigrant health differential in the context of racial and ethnic disparities: the case of diabetes. Adv Med Sociol 19:147–171, PMID: , 10.1108/S1057-629020190000019008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arandia G, Nalty C, Sharkey JR, Dean WR. 2012. Diet and acculturation among Hispanic/Latino older adults in the United States: a review of literature and recommendations. J Nutr Gerontol Geriatr 31(1):16–37, PMID: , 10.1080/21551197.2012.647553. [DOI] [PubMed] [Google Scholar]
- 10.Bustamante AV, Van der Wees PJ. 2012. Integrating immigrants into the U.S. health system. Virtual Mentor 14(4):318–323, PMID: , 10.1001/virtualmentor.2012.14.4.stas1-1204. [DOI] [PubMed] [Google Scholar]
- 11.Hall E, Cuellar NG. 2016. Immigrant health in the United States: a trajectory toward change. J Transcult Nurs 27(6):611–626, PMID: , 10.1177/1043659616672534. [DOI] [PubMed] [Google Scholar]
- 12.Diaz E, Ortiz-Barreda G, Ben-Shlomo Y, Holdsworth M, Salami B, Rammohan A, et al. 2017. Interventions to improve immigrant health. A scoping review. Eur J Public Health 27(3):433–439, PMID: , 10.1093/eurpub/ckx001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Derr AS. 2016. Mental health service use among immigrants in the United States: a systematic review. Psychiatr Serv 67(3):265–274, PMID: , 10.1176/appi.ps.201500004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh GK, Siahpush M. 2002. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol 74(1):83–109, PMID: , 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- 15.Horlyck-Romanovsky MF, Wyka K, Echeverria SE, Leung MM, Fuster M, Huang TTK. 2019. Foreign-born blacks experience lower odds of obesity but higher odds of diabetes than US-born blacks in New York City. J Immigr Minor Health 21(1):47–55, PMID: , 10.1007/s10903-018-0708-7. [DOI] [PubMed] [Google Scholar]
- 16.Riosmena F, Wong R, Palloni A. 2013. Migration selection, protection, and acculturation in health: a binational perspective on older adults. Demography 50(3):1039–1064, PMID: , 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elo IT, Mehta NK, Huang C. 2011. Disability among native-born and foreign-born blacks in the United States. Demography 48(1):241–265, PMID: , 10.1007/s13524-010-0008-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eamranond PP, Hu H. 2008. Environmental and occupational exposures in immigrant health. Environ Health Insights 1:45–50, PMID: , 10.4137/ehi.s847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moyce SC, Schenker M. 2017. Occupational exposures and health outcomes among immigrants in the USA. Curr Environ Health Rep 4(3):349–354, PMID: , 10.1007/s40572-017-0152-1. [DOI] [PubMed] [Google Scholar]
- 20.Ulman R, Abernethy JD. 1975. Blood pressure and length of stay in Australia of Italian immigrants in the Australian National Blood Pressure Study. Int J Epidemiol 4(3):213–215, PMID: , 10.1093/ije/4.3.213. [DOI] [PubMed] [Google Scholar]
- 21.Abramson JH, Avitzour M, Peritz E. 1975. Mortality from lymphomas in Israel, 1950–71: the possible role of environmental factors. Int J Epidemiol 4(4):321–329, PMID: , 10.1093/ije/4.4.321. [DOI] [PubMed] [Google Scholar]
- 22.Drew JH, Kitchen WH. 1976. Jaundice in infants of Greek parentage: the unknown factor may be environmental. J Pediatr 89(2):248–252, PMID: , 10.1016/S0022-3476(76)80457-X. [DOI] [PubMed] [Google Scholar]
- 23.Heo S, Fong KC, Bell ML. 2019. Risk of particulate matter on birth outcomes in relation to maternal socio-economic factors: a systematic review. Environ Res Lett 14(12):123004, PMID: , 10.1088/1748-9326/ab4cd0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laurent O, Bard D, Filleul L, Segala C. 2007. Effect of socioeconomic status on the relationship between atmospheric pollution and mortality. J Epidemiol Community Health 61(8):665–675, PMID: , 10.1136/jech.2006.053611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hajat A, Hsia C, O’Neill MS. 2015. Socioeconomic disparities and air pollution exposure: a global review. Curr Environ Health Rep 2(4):440–450, PMID: , 10.1007/s40572-015-0069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.GBD 2017 Risk Factor Collaborators. 2018. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159):1923–1994, PMID: , 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pappalardo AA, Mosnaim G. 2018. Immigrant respiratory health: a diverse perspective in environmental influences on respiratory health. Curr Allergy Asthma Rep 18(4):21, PMID: , 10.1007/s11882-018-0779-5. [DOI] [PubMed] [Google Scholar]
- 28.Carter-Pokras O, Zambrana RE, Poppell CF, Logie LA, Guerrero-Preston R. 2007. The environmental health of Latino children. J Pediatr Health Care 21(5):307–314, PMID: , 10.1016/j.pedhc.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beiser M. 2005. The health of immigrants and refugees in Canada. Can J Public Health 96(suppl 2):S30–S44, PMID: , 10.1007/BF03403701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centre for Reviews and Dissemination. 2008. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York, UK: Centre for Reviews and Dissemination, University of York. [Google Scholar]
- 31.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P, PRISMA Group. 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535, PMID: , 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daniels SI, Chambers JC, Sanchez SS, La Merrill MA, Hubbard AE, Macherone A, et al. 2018. Elevated levels of organochlorine pesticides in South Asian immigrants are associated with an increased risk of diabetes. J Endocr Soc 2(8):832–841, PMID: , 10.1210/js.2017-00480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rothenberg SJ, Manalo M, Jiang J, Khan F, Cuellar R, Reyes S, et al. 1999. Maternal blood lead level during pregnancy in South Central Los Angeles. Arch Environ Health 54(3):151–157, PMID: , 10.1080/00039899909602253. [DOI] [PubMed] [Google Scholar]
- 34.Klitzman S, Sharma A, Nicaj L, Vitkevich R, Leighton J. 2002. Lead poisoning among pregnant women in New York City: risk factors and screening practices. J Urban Health 79(2):225–237, PMID: , 10.1093/jurban/79.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eisenberg KW, van Wijngaarden E, Fisher SG, Korfmacher KS, Campbell JR, Fernandez ID, et al. 2011. Blood lead levels of refugee children resettled in Massachusetts, 2000 to 2007. Am J Public Health 101(1):48–54, PMID: , 10.2105/AJPH.2009.184408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perla ME, Rue T, Cheadle A, Krieger J, Karr CJ. 2015. Population-based comparison of biomarker concentrations for chemicals of concern among Latino-American and non-Hispanic White children. J Immigr Minor Health 17(3):802–819, PMID: , 10.1007/s10903-014-0002-2. [DOI] [PubMed] [Google Scholar]
- 37.Pezzi C, Lee D, Kennedy L, Aguirre J, Titus M, Ford R. 2019. Blood lead levels among resettled refugee children in select US states, 2010–2014. Pediatrics 143(5):e20182591, PMID: , 10.1542/peds.2018-2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bulka CM, Bommarito PA, Fry RC. 2019. Predictors of toxic metal exposures among US women of reproductive age. J Expo Sci Environ Epidemiol 29(5):597–612, PMID: , 10.1038/s41370-019-0152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Savadatti SS, Liu M, Caglayan C, Reuther J, Lewis-Michl EL, Aldous KM, et al. 2019. Biomonitoring of populations in Western New York at risk for exposure to Great Lakes contaminants. Environ Res 179(pt A):108690, PMID: , 10.1016/j.envres.2019.108690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muennig P, Song X, Payne-Sturges DC, Gee GC. 2011. Blood and urine levels of long half-life toxicants by nativity among immigrants to the United States. Sci Total Environ 412–413:109–113, PMID: , 10.1016/j.scitotenv.2011.09.077. [DOI] [PubMed] [Google Scholar]
- 41.Ritchey MD, Scalia Sucosky M, Jefferies T, McCormick D, Hesting A, Blanton C, et al. 2011. Lead poisoning among Burmese refugee children—Indiana, 2009. Clin Pediatr (Phila) 50(7):648–656, PMID: , 10.1177/0009922811398958. [DOI] [PubMed] [Google Scholar]
- 42.Farzan SF, Howe CG, Chavez TA, Hodes TL, Johnston JE, Habre R, et al. 2021. Demographic predictors of urinary arsenic in a low-income predominantly Hispanic pregnancy cohort in Los Angeles. J Expo Sci Environ Epidemiol 31(1):94–107, PMID: , 10.1038/s41370-020-0251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mitro SD, Chu MT, Dodson RE, Adamkiewicz G, Chie L, Brown FM, et al. 2019. Phthalate metabolite exposures among immigrants living in the United States: findings from NHANES, 1999–2014. J Expo Sci Environ Epidemiol 29(1):71–82, PMID: , 10.1038/s41370-018-0029-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Parnia A, Chakravartty D, Wiseman CLS, Archbold J, Copes R, Zawar N, et al. 2018. Environmental factors associated with blood lead among newcomer women from South and East Asia in the Greater Toronto Area. Sci Total Environ 624:558–566, PMID: , 10.1016/j.scitotenv.2017.11.336. [DOI] [PubMed] [Google Scholar]
- 45.Wiseman CLS, Parnia A, Chakravartty D, Archbold J, Copes R, Cole D. 2019. Total, methyl and inorganic mercury concentrations in blood and environmental exposure sources in newcomer women in Toronto, Canada. Environ Res 169:261–271, PMID: , 10.1016/j.envres.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 46.Wiseman CLS, Parnia A, Chakravartty D, Archbold J, Zawar N, Copes R, et al. 2017. Blood cadmium concentrations and environmental exposure sources in newcomer South and East Asian women in the Greater Toronto Area, Canada. Environ Res 154:19–27, PMID: , 10.1016/j.envres.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 47.Foster WG, Cheung AP, Davis K, Graves G, Jarrell J, Leblanc A, et al. 2012. Circulating metals and persistent organic pollutant concentrations in Canadian and non-Canadian born primiparous women from five Canadian centres: results of a pilot biomonitoring study. Sci Total Environ 435–436:326–336, PMID: , 10.1016/j.scitotenv.2012.06.070. [DOI] [PubMed] [Google Scholar]
- 48.Dix-Cooper L, Kosatsky T. 2018. Blood mercury, lead and cadmium levels and determinants of exposure among newcomer South and East Asian women of reproductive age living in Vancouver, Canada. Sci Total Environ 619–620:1409–1419, PMID: , 10.1016/j.scitotenv.2017.11.126. [DOI] [PubMed] [Google Scholar]
- 49.Ettinger AS, Arbuckle TE, Fisher M, Liang CL, Davis K, Cirtiu CM, et al. 2017. Arsenic levels among pregnant women and newborns in Canada: results from the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort. Environ Res 153:8–16, PMID: , 10.1016/j.envres.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 50.Fisher M, Arbuckle TE, Liang CL, LeBlanc A, Gaudreau E, Foster WG, et al. 2016. Concentrations of persistent organic pollutants in maternal and cord blood from the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort study. Environ Health 15(1):59, PMID: , 10.1186/s12940-016-0143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ruiz-Tudela L, Vázquez-López MA, García-Escobar I, Cabrera-Sevilla JE, Gómez-Bueno S, Martín-Gonzalez M, et al. 2021. Blood lead level in a paediatric population of south-eastern Spain and associated risk factors. Int J Environ Res Public Health 18(4):1825, PMID: , 10.3390/ijerph18041825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang CB, Hsi HC, Fan CH, Chien LC. 2014. Fetal exposure to environmental neurotoxins in Taiwan. PLoS One 9(10):e109984, PMID: , 10.1371/journal.pone.0109984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bradman A, Fenster L, Sjödin A, Jones RS, Patterson DG Jr, Eskenazi B. 2007. Polybrominated diphenyl ether levels in the blood of pregnant women living in an agricultural community in California. Environ Health Perspect 115(1):71–74, PMID: , 10.1289/ehp.8899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van Wendel de Joode B, Mora AM, Córdoba L, Cano JC, Quesada R, Faniband M, et al. 2014. Aerial application of mancozeb and urinary ethylene thiourea (ETU) concentrations among pregnant women in Costa Rica: the Infants’ Environmental Health Study (ISA). Environmental Health Perspectives 122(12):1321–1328, PMID: , 10.1289/ehp.1307679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vahter M. 2009. Effects of arsenic on maternal and fetal health. Annu Rev Nutr 29:381–399, PMID: , 10.1146/annurev-nutr-080508-141102. [DOI] [PubMed] [Google Scholar]
- 56.Kamai EM, McElrath TF, Ferguson KK. 2019. Fetal growth in environmental epidemiology: mechanisms, limitations, and a review of associations with biomarkers of non-persistent chemical exposures during pregnancy. Environ Health 18(1):43, PMID: , 10.1186/s12940-019-0480-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Araya F, Stingone JA, Claudio L. 2021. Inequalities in exposure to ambient air neurotoxicants and disparities in markers of neurodevelopment in children by maternal nativity status. Int J Environ Res Public Health 18(14):7512, PMID: , 10.3390/ijerph18147512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chakraborty J. 2022. Children’s exposure to vehicular pollution: environmental injustice in Texas, USA. Environ Res 204(pt A):112008, PMID: , 10.1016/j.envres.2021.112008. [DOI] [PubMed] [Google Scholar]
- 59.Christidis T, Erickson AC, Pappin AJ, Crouse DL, Pinault LL, Weichenthal SA, et al. 2019. Low concentrations of fine particle air pollution and mortality in the Canadian Community Health Survey cohort. Environ Health 18(1):84, PMID: , 10.1186/s12940-019-0518-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elford S, Adams MD. 2021. Associations between socioeconomic status and ultrafine particulate exposure in the school commute: an environmental inequality study for Toronto, Canada. Environ Res 192:110224, PMID: , 10.1016/j.envres.2020.110224. [DOI] [PubMed] [Google Scholar]
- 61.Fong KC, Bell ML. 2021. Do fine particulate air pollution (PM2.5) exposure and its attributable premature mortality differ for immigrants compared to those born in the United States? Environ Res 196:110387, PMID: , 10.1016/j.envres.2020.110387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Erickson AC, Christidis T, Pappin A, Brook JR, Crouse DL, Hystad P, et al. 2020. Disease assimilation: the mortality impacts of fine particulate matter on immigrants to Canada. Health Rep 31(3):14–26, PMID: , 10.25318/82-003-x202000300002-eng. [DOI] [PubMed] [Google Scholar]
- 63.Ard K, Fisher-Garibay D, Bonner D. 2021. Particulate matter exposure across Latino ethnicities. Int J Environ Res Public Health 18(10):5186, PMID: , 10.3390/ijerph18105186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brauer M, Brook JR, Christidis T, Chu Y, Crouse DL, Erickson A, et al. 2019. Mortality-Air Pollution Associations in Low-Exposure Environments (MAPLE): phase 1. Research Report 204. Boston, MA: Health Effects Institute. https://www.healtheffects.org/publication/mortality%E2%80%93air-pollution-associations-low-exposure-environments-maple-phase-1 [accessed 7 April 2022]. [PMC free article] [PubMed] [Google Scholar]
- 65.Grineski S, Collins T, Renteria R, Rubio R. 2021. Multigenerational immigrant trajectories and children’s unequal exposure to fine particulate matter in the US. Soc Sci Med 282:114108, PMID: , 10.1016/j.socscimed.2021.114108. [DOI] [PubMed] [Google Scholar]
- 66.Grineski SE, Collins T. 2019. Lifetime cancer risks from hazardous air pollutants in US public school districts. J Epidemiol Community Health 73(9):854–860, PMID: , 10.1136/jech-2018-211832. [DOI] [PubMed] [Google Scholar]
- 67.Grineski SE, Collins TW, Chakraborty J, Montgomery M. 2017. Hazard characteristics and patterns of environmental injustice: household-level determinants of environmental risk in Miami, Florida. Risk Anal 37(7):1419–1434, PMID: , 10.1111/risa.12706. [DOI] [PubMed] [Google Scholar]
- 68.Hillemeier MM, Landale NS, Oropesa RS. 2015. Asthma in US Mexican-origin children in early childhood: differences in risk and protective factors by parental nativity. Acad Pediatr 15(4):421–429, PMID: , 10.1016/j.acap.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Loustaunau MG, Chakraborty J. 2019. Vehicular air pollution in Houston, Texas: an intra-categorical analysis of environmental injustice. Int J Environ Res Public Health 16(16):2968, PMID: , 10.3390/ijerph16162968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Padula AM, Yang W, Carmichael SL, Lurmann F, Balmes J, Hammond SK, et al. 2017. Air pollution, neighborhood acculturation factors, and neural tube defects among Hispanic women in California. Birth Defects Res 109(6):403–422, PMID: , 10.1002/bdra.23602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pinault L, van Donkelaar A, Martin RV. 2017. Exposure to fine particulate matter air pollution in Canada. Health Rep 28(3):9–16, PMID: . [PubMed] [Google Scholar]
- 72.Quach T, Garcia E, Von Behren J, Tran J, Tran TD, Fu L, et al. 2015. Environmental street audits and black carbon measurements in Vietnamese immigrant communities. Prog Community Health Partnersh 9(2):179–190, PMID: , 10.1353/cpr.2015.0036. [DOI] [PubMed] [Google Scholar]
- 73.Rhee J, Fabian MP, Ettinger de Cuba S, Coleman S, Sandel M, Lane KJ, et al. 2019. Effects of maternal homelessness, supplemental nutrition programs, and prenatal PM2.5 on birthweight. Int J Environ Res Public Health 16(21):4154, PMID: , 10.3390/ijerph16214154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.U.S. EPA (U.S. Environmental Protection Agency). 2020. Hazardous Air Pollutants. https://www.epa.gov/haps [accessed 7 December 2020].
- 75.Mercereau L, Todd N, Rey G, Valleron AJ. 2017. Comparison of the temperature–mortality relationship in foreign born and native born died in France between 2000 and 2009. Int J Biometeorol 61(10):1873–1884, PMID: , 10.1007/s00484-017-1373-6. [DOI] [PubMed] [Google Scholar]
- 76.Fong KC, Mehta NK, Bell ML. 2020. Disparities in exposure to surrounding greenness related to proportion of the population that were immigrants to the United States. Int J Hyg Environ Health 224:113434, PMID: , 10.1016/j.ijheh.2019.113434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kamel AA, Ford PB, Kaczynski AT. 2014. Disparities in park availability, features, and characteristics by social determinants of health within a U.S.–Mexico border urban area. Prev Med 69(suppl 1):S111–S113, PMID: , 10.1016/j.ypmed.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 78.Maldonado A, Collins TW, Grineski SE, Chakraborty J. 2016. Exposure to flood hazards in Miami and Houston: are Hispanic immigrants at greater risk than other social groups? Int J Environ Res Public Health 13(8):775, PMID: , 10.3390/ijerph13080775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rodriguez-Loureiro L, Casas L, Bauwelinck M, Lefebvre W, Vanpoucke C, Vanroelen C, et al. 2021. Social inequalities in the associations between urban green spaces, self-perceived health and mortality in Brussels: results from a census-based cohort study. Health Place 70:102603, PMID: , 10.1016/j.healthplace.2021.102603. [DOI] [PubMed] [Google Scholar]
- 80.Alahmad B, Shakarchi AF, Khraishah H, Alseaidan M, Gasana J, Al-Hemoud A, et al. 2020. Extreme temperatures and mortality in Kuwait: who is vulnerable? Sci Total Environ 732:139289, PMID: , 10.1016/j.scitotenv.2020.139289. [DOI] [PubMed] [Google Scholar]
- 81.Holman CD, Armstrong BK. 1984. Cutaneous malignant melanoma and indicators of total accumulated exposure to the sun: an analysis separating histogenetic types. J Natl Cancer Inst 73(1):75–82, PMID: , 10.1093/jnci/73.1.75. [DOI] [PubMed] [Google Scholar]
- 82.Simonelli G, Dudley KA, Weng J, Gallo LC, Perreira K, Shah NA, et al. 2017. Neighborhood factors as predictors of poor sleep in the Sueño ancillary study of the Hispanic Community Health Study/Study of Latinos. Sleep 40(1):zsw025, PMID: , 10.1093/sleep/zsw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Taylor EV, Vaidyanathan A, Flanders WD, Murphy M, Spencer M, Noe RS. 2018. Differences in heat-related mortality by citizenship status: United States, 2005–2014. Am J Public Health 108(S2):S131–S136, PMID: , 10.2105/AJPH.2017.304006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bakhtsiyarava M, Nawrotzki RJ. 2017. Environmental inequality and pollution advantage among immigrants in the United States. Appl Geogr 81:60–69, PMID: , 10.1016/j.apgeog.2017.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.U.S. EPA. 2015. EPA’s Risk-Screening Environmental Indicators (RSEI) Methodology. RSEI Version 2.3.3. https://www.epa.gov/sites/default/files/2015-08/documents/rsei_methodology_v2_3_3_0.pdf [accessed 23 June 2022].
- 86.Edge S, Newbold B. 2013. Discrimination and the health of immigrants and refugees: exploring Canada’s evidence base and directions for future research in newcomer receiving countries. J Immigr Minor Health 15(1):141–148, PMID: , 10.1007/s10903-012-9640-4. [DOI] [PubMed] [Google Scholar]
- 87.Esses VM. 2021. Prejudice and discrimination toward immigrants. Annu Rev Psychol 72(1):503–531, PMID: , 10.1146/annurev-psych-080520-102803. [DOI] [PubMed] [Google Scholar]
- 88.Teixeira C, Li W. 2009. Immigrant and refugee experiences in North American cities. J Immigr Refug Stud 7(3):221–227, 10.1080/15562940903150030. [DOI] [Google Scholar]
- 89.Gee GC, Payne-Sturges DC. 2004. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect 112(17):1645–1653, PMID: , 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rehman K, Fatima F, Waheed I, Akash MSH. 2018. Prevalence of exposure of heavy metals and their impact on health consequences. J Cell Biochem 119(1):157–184, PMID: , 10.1002/jcb.26234. [DOI] [PubMed] [Google Scholar]
- 91.Kononenko M, Frishman WH. 2021. Association between arsenic exposure and cardiovascular disease. Cardiol Rev 29(4):217–221, PMID: , 10.1097/CRD.0000000000000357. [DOI] [PubMed] [Google Scholar]
- 92.Gómez-Roig MD, Pascal R, Cahuana MJ, García-Algar O, Sebastiani G, Andreu-Fernández V, et al. 2021. Environmental exposure during pregnancy: influence on prenatal development and early life: a comprehensive review. Fetal Diagn Ther 48(4):245–257, PMID: , 10.1159/000514884. [DOI] [PubMed] [Google Scholar]
- 93.Concha G, Vogler G, Lezcano D, Nermell B, Vahter M. 1998. Exposure to inorganic arsenic metabolites during early human development. Toxicol Sci 44(2):185–190, PMID: , 10.1006/toxs.1998.2486. [DOI] [PubMed] [Google Scholar]
- 94.Gundacker C, Hengstschläger M. 2012. The role of the placenta in fetal exposure to heavy metals. Wien Med Wochenschr 162(9–10):201–206, PMID: , 10.1007/s10354-012-0074-3. [DOI] [PubMed] [Google Scholar]
- 95.Braun JM, Sathyanarayana S, Hauser R. 2013. Phthalate exposure and children’s health. Curr Opin Pediatr 25(2):247–254, PMID: , 10.1097/MOP.0b013e32835e1eb6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mariana M, Feiteiro J, Verde I, Cairrao E. 2016. The effects of phthalates in the cardiovascular and reproductive systems: a review. Environ Int 94:758–776, PMID: , 10.1016/j.envint.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 97.Brook RD, Rajagopalan S, Pope CA III, Brook JR, Bhatnagar A, Diez-Roux AV, et al. 2010. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121(21):2331–2378, PMID: , 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 98.Hempstead K. 2007. Mobility of the foreign-born population in the United States, 1995–2000: the role of gateway states. Int Migr Rev 41(2):466–479, 10.1111/j.1747-7379.2007.00075.x. [DOI] [Google Scholar]
- 99.National Academies of Sciences E, and Medicine. 2015. The Integration of Immigrants into American Society. Washington, DC: National Academies Press. [Google Scholar]
- 100.Singh GK, Hiatt RA. 2006. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979–2003. Int J Epidemiol 35(4):903–919, PMID: , 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- 101.Boeri T, De Philippis M, Patacchini E, Pellizzari M. 2015. Immigration, housing discrimination and employment. Econ J (London) 125(586):F82–F114, 10.1111/ecoj.12232. [DOI] [Google Scholar]
- 102.Shor E, Roelfs D. 2019. Climate shock: moving to colder climates and immigrant mortality. Soc Sci Med 235:112397, PMID: , 10.1016/j.socscimed.2019.112397. [DOI] [PubMed] [Google Scholar]
- 103.NIMHD (National Institute on Minority Health and Health Disparities). 2020. Addressing the etiology of health disparities and health advantages among immigrant populations. https://grants.nih.gov/grants/guide/pa-files/PAR-21-080.html [accessed 15 December 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.