Abstract
Background and Objectives:
The multiple endoclip retraction technique (MERT) was developed based on our experience with suturing renal parenchyma in laparoscopic partial nephrectomy. In this study we prospectively evaluated the one-year results of cases treated by transperitoneal laparoscopic Burch with the MERT.
Methods:
The patients were evaluated with stress test, one-hour pad test, and were requested to complete the International Continence Society Incontinence Questionnaire short form (ICIQ-SF) in the postoperative period. The follow-up periods were postoperative 3, 6, and 12 months.
Results:
The primary outcome of this study was surgical success, defined as being cured of stress urinary incontinence (SUI) (no symptoms), experiencing improved symptoms of SUI in ICIQ-SF and negative stress test, and less than 2g urine leakage in a one-hour pad test.
No statistically significant difference was found in terms of age, number of children, and body mass index (BMI) in patients according to the results of the 12 month postoperative stress test. We found statistically significant improvements at all control months in terms of stress test and pad weight. ICIQ-SF results showed a significant decrease at three months in patients who recovered after the operation. This rate has not changed in following control months. However, there was no statistical change in ICIQ-SF values in patients who did not recover after the operation.
Conclusion:
MERT seems to be one of the safe and effective modifications in the management of SUI with good one year outcomes when performed by suitably trained experienced surgeons.
Keywords: Laparoscopic, Stress incontinence, Surgery
INTRODUCTION
Stress urinary incontinence (SUI) in women is a multifactorial syndrome with significant social, medical, and psychological consequences; and a high prevalence rate. The major contributing factors to SUI are incontinence during pregnancy, weak pelvic floor muscles, especially in postmenopausal women, and assisted birth.
The most effective treatment for SUI is surgery.1 Retropubic colposuspension by the Burch technique is one of the most preferred procedures, especially in patients with bladder neck hypermobility.1 Unfortunately this technique has failed to gain momentum, and the midurethral sling (MUS) procedure has become the gold standard first-line surgical treatment for SUI due to the relative ease of applying the MUS.2
Burch can be performed via open conventional or retropubic-transperitoneal laparoscopic methods.3,4 This modality is easily modified and can be performed through retropubic or transperitoneal laparoscopic routes, using different meshes, type, and number of stitches near the urethra; some use one stitch near the urethra, whereas others opt for two or three stitches.5 Some surgeons prefer the open modality, whereas others prefer the retropubic or transperitoneal laparoscopic methods based on experience.
The multiple endoclip retraction technique (MERT) was developed based on our experience with suturing of renal parenchyma in laparoscopic partial nephrectomy. To the best of our knowledge, this is the first study to use endoclips in the Burch procedure. Herein, we prospectively evaluated the one-year results of cases treated by transperitoneal laparoscopic Burch with the MERT.
METHODOLOGY
This study was reviewed and approved by the institutional review board and performed in accordance with the Declaration of Helsinki. Each patient provided written informed consent. The study was conducted between January 1, 2021 and March 31, 2022. Clinical and demographic data, as well as perioperative findings and postoperative complications, were recorded. All patients had symptomatic SUI without urge incontinence. The patients who had bleeding diathesis, concomitant pelvic organ prolapse, neurologic disorders, medical conditions that prevented surgical intervention, or previous surgical treatment for urinary incontinence were excluded. In the pre-operative period, the cases were evaluated with a detailed history and physical examination including a stress test and one-hour pad test. We gave preweighed pads to all patients in our outpatient clinic and requested that they perform physical activities such as sitting, getting up, coughing, and walking quickly during a one-hour period. After one hour, the pads were reweighed to calculate urine loss after completion of the provocation tests. The stress test was evaluated and the weight of the pad was recorded by our urodynamic test nurse. Prior to surgery, patients underwent a complete blood count, urine analysis, urine culture, and if required, serum creatinine measurement, ultrasonography of the urinary system and postvoid residual urine (PVR), and a detailed anesthetic examination. Due to the coronavirus 2019 disease (COVID-19) pandemic, nasopharyngeal swabs were taken from all patients to exclude COVID infection.
Patients who underwent laparoscopic Burch were evaluated with a stress test and one-hour pad test and were asked to complete the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF) in the postoperative period. The follow-up periods were 3, 6, and 12 months after surgery. The primary outcome of this study was surgical success defined as being cured of SUI (no symptoms), experiencing improved symptoms of SUI on the ICIQ-SF and negative stress test, and less than 2 g urine leakage in one-hour pad test.6 Laparoscopic Burch colposuspension was performed by a single urologist with 15 years of experience in the profession.
Technique
The laparoscopic technique was performed by the transperitoneal route.7,8 All patients were placed in the lithotomy position with their feet down. We inserted 16-degree urinary catheters prior to surgery. For the transabdominal route, a 10-mm puncture was made in the umbilicus (optics); and another two auxiliary punctures were made at McBurney’s point, to the right (5 mm) and its mirror image point to the left (10 mm). After visualization of the bladder, the bladder was detached from both sides with sharp and blunt dissection, and the retropubic space was entered. The Retzius space was created by extraperitoneal dissection of fatty tissues from the lateral sides, allowing approaching the urethra, bladder neck, and Cooper’s ligament, aided by palpation of the 16 degree urethral catheter balloon and the identification of the vaginal cul-de-sac presented by vaginal mounted gauze. Then two or three stitches were applied with 1-0 polyglactin suture between the periurethral tissue and Cooper’s ligament. The number of stitches was determined by the area of the periurethral tissue and space of Retzius, based on imaging of this field. At the end of the procedure, cystoscopy was performed to evaluate bladder neck elevation and whether the sutures had passed through the bladder.
MERT
Per surgeons’ preferences, we used medium Hem-o-Lok™ (Weck™) clips instead of making knots. A surgical nurse prepared a 12 cm 1-0 polyglactin suture and attached a medium clip to the tail end. This was followed by extraperitoneal dissection of fatty tissues from the lateral sides, allowing approach of the urethra, bladder neck, and Cooper’s ligament. After each passing of the needle from the tissues (Periurethra or Cooper’s ligament), the suture was tracted by the surgeon and a clip was attached to the base. The determination of Cooper’s ligament may be challenging due to its wide area. Passing a needle through a hard tissue removes doubts about the right location of this ligament. On each side, the sutures were applied in a continuous manner, with the goal of elevating the tissues effectively by retraction secured by clips (Figure 1).
Figure 1.
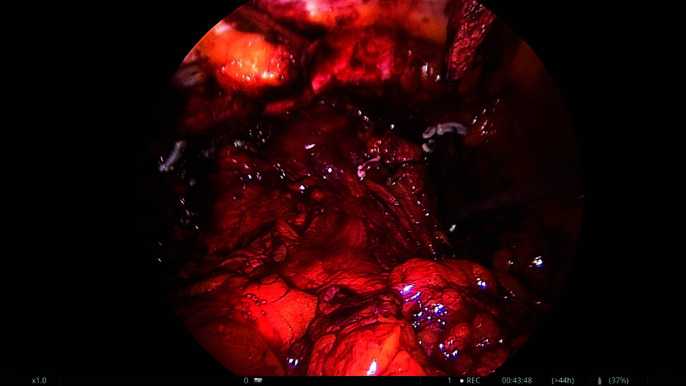
Periurethral fascia is attached to the Cooper’s ligament with Hem-o-Lok™ Clips (Weck™) on both sides.
Statistical Analyses
The conformity of data to normal distribution was evaluated with the Shapiro–Wilk test. Median and quartile values were used to represent the patients’ variables. The Mann–Whitney U test was used to compare the individual characteristics and test results of the patients who recovered (negative) and did not improve (positive) according to the results of the stress test at the postoperative month 12. The pad and stress test results of all patients were evaluated preoperatively and at 3, 6, and 12 months postoperatively by Cochran’s Q test, and the Friedman’s test was used to compare the ICIQ-SF values. Statistical analyses were performed with IBM SPSS 21 software. A P < .05 was considered statistically significant.
RESULTS
A total of 30 patients underwent laparoscopic Burch colposuspension between January 1, 2021 and March 31, 2022. The median age of the patients was 63 years. Patients’ characteristics are summarized in Table 1. Most women were multiparous with a median parity of two. Eight and three cases had previous caesarean and hysterectomy, respectively. Ninety percent of patients (n = 27) were postmenopausal. All cases had a negative COVID-19 nasopharyngeal swab test.
Table 1.
Characteristics of 30 Women Who Underwent Laparoscopic Burch
| Median (25 – 75 Quartile) | |
|---|---|
| Age | 63 (57.75, 67) |
| Parity | 2 (2,3) |
| Body Mass Index | 32.95 (29.7, 34.6) |
| Pre-op Stress Test | 1 (1,1) |
| Pre-op ICIQ-SF | 18 (16,19) |
| Pre-op Pad Weight (g) | 150 (90,180) |
Abbreviations: Pre-op, pre-operative; ICIQ-SF, International Continence Society Incontinence Questionnaire short form.
The average operation time was 37.1 min (30 – 68 min). Regarding perioperative complications, single point bladder perforation occurred in one case and was managed perioperatively. There were no significant hemorrhages and no conversions to laparotomy. One case experienced wound dehiscence and was managed conservatively; she also had concomitant diabetes mellitus. Urethral catheters were removed on postoperative day 1, with the exception of a patient with bladder perforation, who had her urethral catheter on postoperative day 7. One patient did not urinate spontaneously in the postoperative period and received clean intermittent catheterization. It disappeared after two months and she was able to urinate with minimal PVR. All of the other cases urinated spontaneously after removal of the urethral catheters. De novo urgency and urge incontinence developed in one patient. The symptoms in this patient completely disappeared in the third postoperative month with anticholinergic therapy. The median postoperative PVR and hospitalization was 27.5 mL and one day, respectively.
No statistically significant differences were found in terms of age, number of children, and BMI in patients who recovered (negative) and did not recover (positive) according to the results of the 12th postoperative month stress test (P > .05). Although it was not statistically significant, the patients who had a positive stress test were older and had more children (Table 2).
Table 2.
Comparison of the Patients According to Month 12 Stress Test Results
| Negative (n = 26) |
Positive (n = 4) |
P Value (Mann Whitney U Test) |
|
|---|---|---|---|
| Median (25% –75%) | Median (25% – 75%) | ||
| Age | 61 (57.75, 67) | 67.5 (48.5, 70.75) | P > 0.05 |
| Parity | 2 (2, 3) | 2.5 (1.25, 5.25) | P > 0.05 |
| Body Mass Index | 32.95 (29.9, 34.5) | 32.2 (29.5, 37.15) | P > 0.05 |
| Pre-op Stress Test | 1 (1,1) | 1 (1,1) | P > 0.05 |
| Pre-op ICIQ-SF | 18 (16,19) | 20 (16,21) | P > 0.05 |
| Pre-op Pad Weight | 155 (97.5,180) | 120 (78.25, 187.5) | P > 0.05 |
| Postop PVR (ml) | 27.5 (25, 30) | 25 (20, 60) | P > 0.05 |
| Hospitalization (days) | 1 (1,2) | 1 (1, 1.75) | P > 0.05 |
Abbreviations: Pre-op, pre-operative; ICIQ-SF, International Continence Society Incontinence Questionnaire short form; Postop, postoperative; PVR, post void residual urine.
We found a statistically significant improvement in all postoperative control months in terms of stress test and pad weight (P < .001), which is summarized in Tables 3 and 4. As expected, the ICIQ-SF results showed a significant decrease in the third postoperative month in patients who recovered (P < .001). This rate did not change in the subsequent control months. However, there was no statistical change in ICIQ-SF values in patients who did not recover after surgery (P = .062) (Table 5).
Table 4.
Pad Test
| Pad Test |
||
|---|---|---|
| Negative n (%) |
Positive n (%) |
|
| Pre-operative | 0 (0%) | 30 (100%) |
| 3rd month | 26 (86.7%) | 4 (13.3%) |
| 6th month | 27 (90.0%) | 3 (10.0%) |
| 12th month | 25 (83.3%) | 5 (16.7%) |
| P values (Related sample Cochran’s Q test) | P < 0.001 | |
Table 5.
International Continence Society Incontinence Questionnaire Short Form Score Change According to the Stress Test
| Negative (n = 26) | Positive (n = 4) | |
|---|---|---|
| Median (25% – 75%) | Median (25% – 75%) | |
| Pre-operative | 18 (16, 18.25) | 20 (16, 21) |
| 3rd month | 2 (1,3) | 14 (12.5, 15.5) |
| 6th month | 2 (1,3) | 14 (12.5, 15.5) |
| 12th month | 2 (1,3) | 14.5 (8, 15.75) |
| P values (Related sample Friedman’s test) | P < 0.001 | P = 0.062 |
Table 3.
Stress Test Results
| Stress Test |
||
|---|---|---|
| Negative n (%) |
Positive n (%) |
|
| Pre-operative | 0 (0%) | 30 (100%) |
| 3rd month | 26 (86.7%) | 4 (13.3%) |
| 6th month | 26 (86.7%) | 4 (13.3%) |
| 12th month | 26 (86.7%) | 4 (13.3%) |
| P values (Related sample Cochran’s Q test) | P < 0.001 | |
DISCUSSION
Open traditional or laparoscopic Burch colposuspension has been the procedure of choice for many urologists and gynecologists for the treatment of SUI due to the good long-term results obtained.9 The laparoscopic Burch procedure has become popular due to its advantages such as minimal intraoperative blood loss and lower requirement of analgesics in the postoperative period, easier access to the Retzius space, improved visualization in the surgical field, smaller incisions with better aesthetic results, lower cost, and shorter hospital stay and rehabilitation period.10 When open traditional Burch was compared to the laparoscopic approach, success rates were similar and as high as 90%.11,12 In our clinic, the transperitoneal laparoscopic route is preferred for the Burch procedure. Our success rates in the 12th month in terms of the stress test and pad test were 86.7% and 83.3%, respectively, similar to the results in the literature.11,12
However, laparoscopic suturing, especially in a narrow space like the retropubic area, is very difficult and can take years to master. For this reason, the Burch procedure has the tendency to be modified, and many technical facilities (biological glues, bone fixators, synthetic meshes, staplers) were reported to make the performance of laparoscopic Burch surgery faster, easier, and consequently, more accessible to surgeons.13 Even in the presence of these modifications, it is crucial that surgeons have the necessary skills for laparoscopic suturing and knot tying. However, no definitive conclusion has been drawn about such modifications. It is not known if they impair the efficacy that was previously established for the open technique since global results are controversial. There are several other conflicting results in the literature about the efficacy of modification of the laparoscopic technique, as well as its comparison with the open technique. This was evaluated in a recent article that concluded that these conflicting results may be attributed to the cure definition, method of reporting success rate, and preferred questionnaires.14 Some have very strict criteria such as defining cure and success as no SIU recurrence (self-reported) and no re-operation, whereas others have accepted these criteria as improvement in SUI symptoms. In this study, our modification was using endoclips instead of making knots in laparoscopic Burch. The inspiration for this modification was using these clips for retraction in laparoscopic renal parancyma suturing. To the best of our knowledge, this is the first study about this modification in Burch surgery. Success was defined as being cured of SUI (no symptoms), experiencing improved symptoms of SUI in the ICIQ-SF and negative stress test, and less than 2 g urine leakage in the one-hour pad test. For avoidance of subjectivity in self-reporting questionnaires, we tried to combine both ICIQ-SF and objective findings evaluated by clinicians.
Veit-Rubin et al.2 reported that the laparoscopic operation took longer to perform than the open technique in their recent review article. However, the average operation duration in patients who underwent laparoscopy was about 40 min. in our study and this might be accepted as a short duration for surgery. This duration might be explained by our experience in laparoscopic skills and MERT. Both transabdominal and retropubic laparoscopic surgeries are routinely performed in our clinic.
There are conflicting results on the number of stitches used on each side of the urethra in Burch surgery.5 Only one study by Persson et al.15 reported that the group with two stitches achieved an objective cure rate of 83% and symptom improvement in 12% after one year. On the other hand, these rates for the group with one stitch was 58% and 27%, respectively (P = .001). Souza et al.5 also concluded that despite the lack of clear evidence, when Burch is performed by laparoscopy, the best option seems to be the use of two stitches, especially currently, when there is a trend in the advancement of laparoscopic suture techniques. As is routine in our clinic, we also applied two or more stitches on each side of the urethra in our technique. The number of stitches was determined by area of periurethral tissue and space of Retzius.
Another point is using absorbable or nonabsorbable sutures in Burch colposuspension. There is no consensus in the current literature with regard to the suture material to be used. In their review on this issue, Smits-Braat reported an equal cure rate of 87% whether absorbable or permanent sutures were preferred.2,16 We used absorbable suture (1-0 polyglactin) in our cases. This was a necessity, because the Hem-o-Lok™ clips cannot grip nonabsorbable sutures like polypropylene due to its slippery property during retraction.
This study had some limitations. First, it was a prospective case series with a limited number of patients, without independent assessment or comparative controls, and was thus subject to bias. Also, objective urodynamic data were not recorded for analysis. The main reason for not obtaining urodynamic examination was the COVID-19 pandemic, as we did not want patients to increase abdominal pressure by coughing in a closed room with our urodynamic nurse. Another reason was that urodynamic studies are not required for patients with obvious clinical symptoms of isolated SUI, in line with the recommendations of the National Institutes of Health.17 However, we believe that utilizing subjective data is more clinically relevant for practitioners and their patients. The number of patients in this study could have been increased, but the pandemic led to a decrease in the admission of patients to our outpatient clinic according to each symptom type including incontinence. Finally, all procedures were performed by a single experienced surgeon. While this provides a standardization in the surgical technique, it makes the results less suitable to the wider community and limits its external validity. We believe that the limited number of patients in this study should not permit broad generalizations.
CONCLUSIONS
Laparoscopic Burch colposuspension is an effective procedure for SUI treatment. To facilitate suturing and to achieve the best results, many surgeons search for different modifications in this modality. We believe that MERT is one of the safe and effective modifications in the management of SUI with good one-year outcomes, when performed by suitably trained experienced surgeons. Long-term results from prospective standardized studies including high number of the patients will reveal the true reliability of this method in the future.
Footnotes
Acknowledgements: none.
Disclosure: none.
Funding sources: none.
Conflict of interests: none.
Informed consent: Dr. Mert Ali Karadag declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Mert Ali Karadag, Department of Urology, University of Health Sciences Medical Faculty of Kayseri, Kayseri City Hospital, Kayseri, Turkey..
Fatih Demir, Department of Urology, University of Health Sciences Medical Faculty of Kayseri, Kayseri City Hospital, Kayseri, Turkey..
Gokhan Sonmez, Department of Urology, Erciyes University Faculty of Medicine, Kayseri, Turkey..
Murat Keske, Department of Urology, University of Health Sciences Medical Faculty of Kayseri, Kayseri City Hospital, Kayseri, Turkey..
References:
- 1.Bezerra CA, Rodrigues AO, Seo AL, Ruano JM, Borrelli M, Wroclawski ER. Laparoscopic Burch surgery: is there any advantage in relation to open approach? Int Braz J Urol. 2004;30(3):230–236. [DOI] [PubMed] [Google Scholar]
- 2.Veit-Rubin N, Dubuisson J, Ford A, Dubuisson J-B, Mourad S, Digesu A. Burch colposuspension. Neurourol Urodyn. 2019;38(2):553–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sivaslioglu AA, Unlubilgin E, Keskin HL, Gelisen O, Dolen I. The management of recurrent cases after the Burch colposuspension: 7 years experience. Arch Gynecol Obstet. 2011;283(4):787–790. [DOI] [PubMed] [Google Scholar]
- 4.Vancaillie TG, Schuessler W. Laparoscopic bladderneck suspension. J Laparoendosc Surg. 1991;1(3):169–173. [DOI] [PubMed] [Google Scholar]
- 5.Souza RJ, Resende JAD, Miglio CG, Brollo LCS, Oliveira MAP, Crispi CP. Can reducing the number of stitches compromise the outcome of laparoscopic Burch surgery in the treatment of stress urinary incontinence? Systematic review and meta-analysis. Rev Col Bras Cir. 2017;44(6):649–654. [DOI] [PubMed] [Google Scholar]
- 6.Kurimura Y, Haga N, Yanagida T, et al. The preoperative pad test as a predictor of urinary incontinence and quality of life after robot-assisted radical prostatectomy: a prospective, observational, clinical study. Int Urol Nephrol. 2020;52(1):67–76. [DOI] [PubMed] [Google Scholar]
- 7.Carter JE. Laparoscopic Burch procedure for stress urinary incontinence: the Carter modification. Keio J Med. 1996;45(3):168–171. [DOI] [PubMed] [Google Scholar]
- 8.Saidi MH, Shannon G, Ingrid PS, Saidi J, Sadler RK, Diaz KC. Extraperitoneal laparoscopic colposuspension: short-term cure rate, complications, and duration of hospital stay in comparison with Burch Colposuspension. Obst Gynecol. 1998;92(4, Part 1):619–621. [DOI] [PubMed] [Google Scholar]
- 9.Burch JC. Urethrovaginal fixation to Cooper’s ligament for the correction of stress incontinence, cystocele, and prolapse. Am J Obstet Gynecol. 1961;81(2):281–290. [DOI] [PubMed] [Google Scholar]
- 10.Ross JV. Laparoscopic Burch repair compared to laparotomy Burch for cure of urinary stress incontinence. Int Urogynecol J. 1995;6(6):323–328. [Google Scholar]
- 11.Persson J, Teleman P, Eten-Bergquist C, Wolner-Hanssen P. Costanalyzes based on a prospective, randomized study comparing laparoscopic colposuspension with a tension-free vaginal tape procedure. Acta Obstet Gynecol Scand. 2002;81(11):1066–1073. [DOI] [PubMed] [Google Scholar]
- 12.Ustun Y, Engin-Ustun Y, Gungor M, Tezcan S. Tension-free vaginal tape compared with laparoscopic Burch urethropexy. J Am Assoc Gynecol Laparosc. 2003;10(3):386–389. [DOI] [PubMed] [Google Scholar]
- 13.Miklos JR, Kohli N. Laparoscopic paravaginal repair plus Burch colposuspension: review and descriptive technique. Urology. 2000;56(6 Suppl 1):64–69. [DOI] [PubMed] [Google Scholar]
- 14.Kuprasertkul A, Zimmern P. Challenges of very long-term reporting in stress urinary incontinence surgeries in women. Urology. 2020. May;139:50–59. [DOI] [PubMed] [Google Scholar]
- 15.Persson J, Wølner-Hanssen P. Laparoscopic Burch colposuspension for stress urinary incontinence: a randomized comparison of one or two sutures on each side of the urethra. Obstet Gynecol. 2000;95(1):151–155. [DOI] [PubMed] [Google Scholar]
- 16.Smits-Braat M, Vierhout ME. Permanent or absorbable sutures for bureh colposuspension? Int Urogynecol J. 1995;6(6):350–352. [Google Scholar]
- 17.National Collaborating Centre for Women's and Children's Health (UK). Urinary Incontinence in Women: The Management of Urinary Incontinence in Women. London: Royal College of Obstetricians and Gynaecologists (UK); September 2013. [PubMed] [Google Scholar]


