Abstract
Aggressive rehabilitation after anterior cruciate ligament (ACL) reconstruction may result in better clinical outcomes and fewer complications such as knee stiffness and weakness. We explored the effect of the Chinese knotting technique (CKT) for aggressive rehabilitation after ACL reconstruction.
Ninety-one anatomical ACL reconstruction cases from 2016 to 2020 were retrospectively reviewed. All patients were operated by the same senior physician and his team. According to the reconstruction with or without CKT, the patients were divided into 2 groups. Both groups received aggressive rehabilitation.
The follow-up time of 91 patients was more than 2 years. In total, 43 out of the 91 patients were in the CKT group, and 48 were in the routine group. The knee joint kinematics recorded by Opti_Knee revealed no significant difference among the CKT group, the routine group, and healthy adults at 3, 6, 12, and 24 months after the operation, respectively. The internal and external rotation angle and the anteroposterior displacement at 3 and 6 months after the operation in the CKT group were smaller than in the routine group and were similar to that of the healthy adults. There was no significant difference in flexion and extension angle, varus or valgus angle, proximal–distal displacement, or the internal or external displacement between the 2 groups. In addition, there was no significant difference in 6 degrees of freedom of the knee between the 2 groups at 12 and 24 months after the operation, respectively, which was similar to healthy adults. Compared to the routine group, the International Knee Documentation Committee scores were significantly higher in the CKT group at the 3, 6, and 12 months, respectively, but no difference was observed at 24 months (P = .749). The Lysholm score was significantly higher in the CKT group at the 3 and 6 months postoperatively, while there was no difference at 12 and 24 months, respectively.
In short-term observation, the ACL reconstruction with CKT, which can sustain aggressive rehabilitation and prevent the loosening of ACL graft, can lead to better clinical outcomes and kinematics recovery of the knee compared to routine technique.
Keywords: aggressive rehabilitation, anterior cruciate ligament, arthroscopy, internal brace, ligament augmented device, tension-relieving technique
1. Introduction
Due to the rapid popularization of sports globally, the rate of anterior cruciate ligament (ACL) rupture and the amount of ACL reconstruction have rapidly increased.[1,2] Currently, the anatomical ACL reconstruction with an autologous hamstring is considered the best treatment strategy for most ACL rupture cases.[3,4] However, there are still certain postoperative complications such as stiffness, pain, and muscle atrophy. Such complications occur due to delayed rehabilitation.[5–8] Accordingly, it is important to explore whether it is possible to improve any details or techniques in ACL reconstruction and how to implement the optimal rehabilitation based on successful surgery.[9] More aggressive rehabilitation, which includes initiating weight-bearing, exercise in knee flexion, extension, and muscle strength as early as possible after surgery, may prevent the occurrence of such complications.[7,8,10] Although aggressive rehabilitation has its advantages, it also may result in other complications like rerupture, tunnel expansion, and loosening of graft and may influence the healing of bone to graft.[5–11]
“Internal bracing technique” may be an effective solution to actively recover the above complications. Previous studies have confirmed that ACL repair has mechanical weaknesses at the suture site, and internal bracing technology can effectively limit the gap expansion at the suture site, reduce the risk of reinjury, and improve the postoperative joint function score.[12,13] In ACL reconstruction, the overall mechanical strength of the tendon graft will decline due to the disintegration of the original collagen fiber in the process of ligamentation, and it will also face the risk of fracture of the mechanical weak point during active rehabilitation.[14,15] In recent years, scholars have studied the feasibility and effectiveness of internal support technologies such as FiberTapeTM and InternalBraceTM in ACL reconstruction, and obtained good in vivo and in vitro biomechanical, histological, and clinical results.[16–19]
Chinese knotting technique (CKT) is a simple and inexpensive new internal support technique that uses EthibondTM sutures commonly used in implant preparation and is woven into FiberTapeTM-like sutures tape suspended between the titanium plate and anchor. In this study, CKT technique was used during ACL reconstruction, and active rehabilitation plan was adopted after surgery. International Knee Documentation Committee (IKDC) and Lysholm function scores of patients were followed up 2 years after surgery, and Opti_Knee[20–25] (Innomotion, Shanghai, China) was used for kinematic analysis. This study assumed that the CKT group could obtain better functional scores and kinematic analysis results.
2. Materials and Methods
2.1. General information
A total of 91 patients with isolated rupture of ACL were anatomically reconstructed using 4-strand hamstring tendon with aggressive rehabilitation between January 2016 and December 2020. They were randomly divided into 2 groups, namely CKT group and routine group. The CKT group received ACL reconstruction combined with CKT, while the routine group received routine ACL reconstruction without CKT.
Inclusion criteria: primary ACL single-bundle and anatomical reconstruction using autologous hamstring tendon; and use of postoperative aggressive rehabilitation.
Exclusion criteria: diagnosis of knee osteoarthritis and other arthropathies or tumor; multi-ligamentous injury; unreliable to follow medical instructions timely. All patients and their family members gave informed consent to this study and signed an informed consent form, which was approved by the hospital ethics committee.
2.2. Methods
2.2.1. Routine group.
A total of 48 patients with isolated rupture of ACL were anatomically reconstructed using 4-Strand hamstring tendon with aggressive rehabilitation. The 48 patients who underwent routine ACL anatomical reconstruction without CKT were assigned to the routine group (Fig. 1). The reconstruction with or without CKT was random.
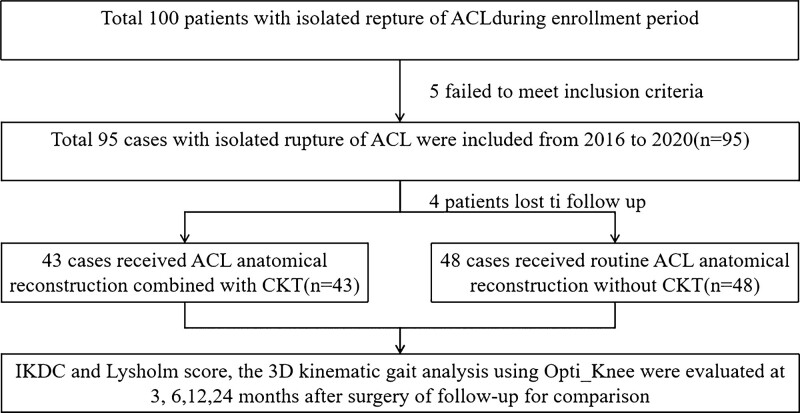
Figure 1.
Flowchart of the study. ACL = anterior cruciate ligament, CKT = Chinese knotting technique, IKDC = International Knee Documentation Committee.
2.2.2. CKT group.
A total of 43 cases who received ACL reconstruction combined with CKT were assigned to the CKT group. A medical team that was composed of sports medicine doctors, rehabilitation doctors, and several nurses was established. The medical team collects basic patient information and the progress of rehabilitation, establishes good doctor-patient communication; jointly learns the aggressive rehabilitation and CKT knowledge of ACL reconstruction, which are implemented by professional medical teams.
2.2.3. CKT procedure.
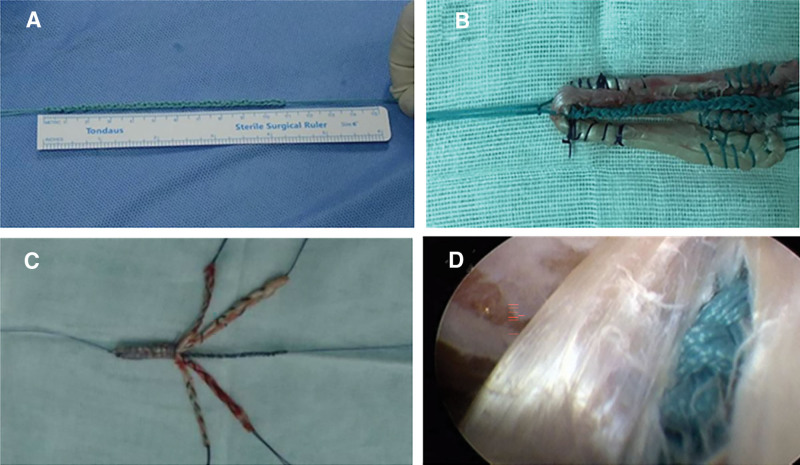
The CKT is a braided technique by 2 NO. 2 EthibondTM sutures (Depuy Synthes, American) with a length of 10 cm that represents the “Internal Bracing” device (Figs. 2 and 3A. It relies on Chinese-knitting to adjust the ductility and elasticity of the Ethibond suture line. When the length of each knot is 3 mm, the ductility and elasticity of the braided suture line were similar with the hamstring tendon. The gracilis tendon and semitendinosus tendons were folded into 4 bundles, and the CKT braided suture was placed in the middle of 4 bundles (Fig. 3B), after which the CKT braided suture was intertwined with graft (Fig. 3C).
Figure 2.
The special “CKT braided suture” made of Ethibond thread. CKT = Chinese knotting technique.
Figure 3.
(A) The special “CKT braided suture” made of Ethibond thread. (B) The “CKT braided suture” was placed in the middle of graft’s bundles. (C) The “CKT braided suture” was intertwined with the graft. (D) The “CKT braided suture” was intertwined with the graft well, and the tension was well under arthroscopy. CKT = Chinese knotting technique.
2.2.4. Surgical technique.
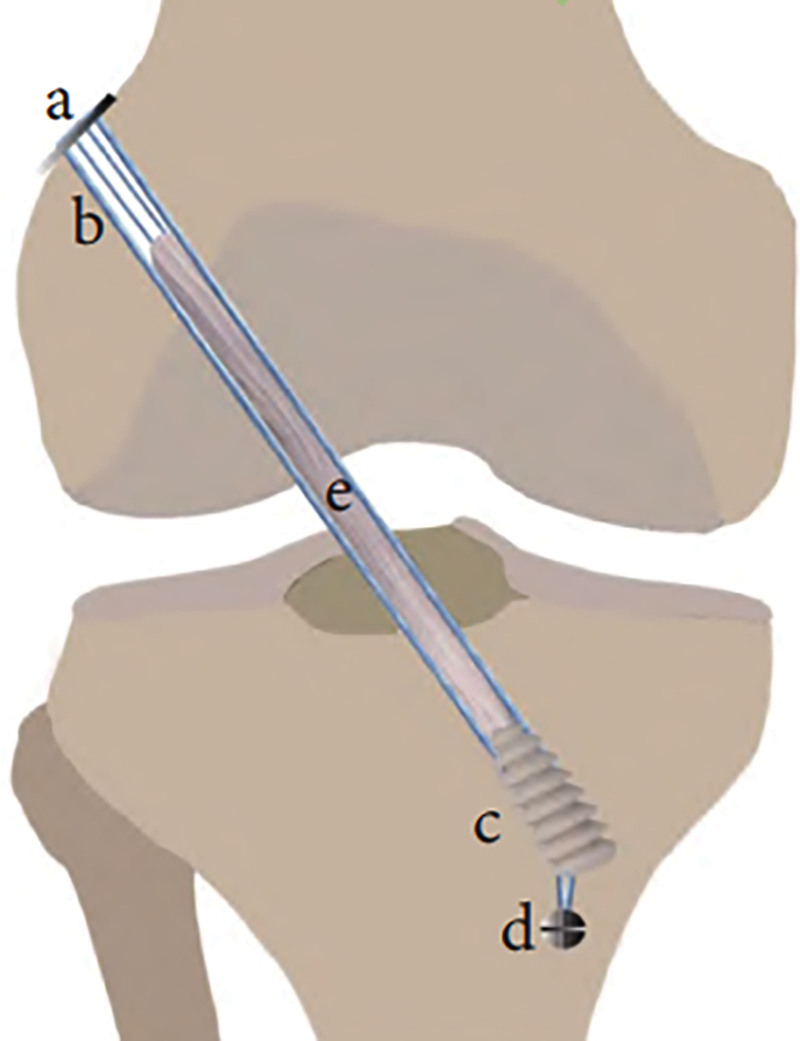
The reconstructions were performed under arthroscopy. The meniscus tear was repaired or partially resected at the same time. The gracilis and the semitendinosus tendon were harvested through 2 to 3 cm incision medial to the tibial tuberosity. In the anteromedial portal, the tibial locator was placed on the native center of the ACL tibial attachment, thus making the tibial tunnel. The femoral positioner was placed on the anatomical center of the ACL footprint, making the femoral tunnel. All tunnel centers were preoperatively designed by innovative computerized assisted technique.[18] After successfully placing the graft, the femoral ends were fixed with an Endobutton device (EndoButton; Smith & Nephew), and the tibial ends were fixed with absorbable interference screws (BioRCIHA; Smith & Nephew) and Anchor (Anchor; Smith & Nephew). This was intertwined with graft, its near end was fixed by an Endobutton device and its distal end was fixed by an Anchor near the tubercles of the tibia (Fig. 4). The graft’s place tension was satisfied under arthroscopy (Fig. 3D). The graft’s preparation, fixation, and other surgical steps in the routine group were the same as in the tension-relieving group except for CKT and its fixation.
Figure 4.
Independent hanging internal tension-relieving technology assists ACL reconstruction: (A) Endobutton; (B) CKT suture (blue); (C) Interface screw; (D) Anchor; (E) Tendon graft. ACL = anterior cruciate ligament, CKT = Chinese knotting technique.
2.2.5. Aggressive rehabilitation.
The aggressive rehabilitation protocol,[4,26] which was immediately initiated in both groups, included: Phase 1 (from the first day to the first week after surgery): CPM began from 0° to 50°, and quadriceps exercises of the knee were initiated soon after surgery with ice pressing. Unrestrictive full ROM exercise was initiated within the first week; weight-bearing was initiated with no pain, effusion, or increase in temperature. Crutches were used for 4 weeks. If the patient could not tolerate the pain of rehabilitation, the steps were postponed for 1 to 3 days; Phase 2 (from the second to the fourth week): the exercises in phase 1 were continued, including full weight-bearing without axillary device; Phase 3 (4th–7th week): the progressive exercises in phase 2 such as ROM and muscles strength exercise were continued and enhanced, emphasizing neuromuscular-control training, and functional activities such as cycling; Phase 4 (8th–12th week) included restoring full symmetrical passive ROM, increased muscle strengthening, and higher-level neuromuscular-control tasks; Phase 5 (12th–24th week) included progressive muscle strengthening, sport-specific neuromuscular-control training, plyometrics, sprinting, and cutting drills. Patients usually returned to their normal daily activities at this phase and were allowed to participate in noncompetitive sports; Phase 6 (After 6 months): patients were allowed to engage in sports activities. It is worth noticing that all cases, despite surgical techniques, should meet all the criteria at each phase before continuing to the next phase of the rehabilitation. The timetable was not so strict if the patient could not tolerate aggressive steps and the knee’s function was not satisfactorily restored. Furthermore, 12 months after surgery, the patients received a second look under arthroscopy and removed the door-shaped nail.
2.3. Outcome measures
The knee function was compared in 2 groups at 3, 6, 12, and 24 months after surgery using the IKDC and Lysholm score.[1–3]
The knee kinematics in 2 groups were compared at 3, 6, 12, and 24 months after surgery using Opti_Knee, a knee joint 3-dimensional motion analysis system (on Haiyidong Medical Technology Co., Ltd), recording the maximum step length, minimum step length, period of the limb walking, knee joint 6 degrees of freedom (flexion and extension angle, varus angle, internal and external rotation angle, front and back displacement, up and down displacement and internal and external displacement), and range of motion (maximum the difference from the minimum value).[20–25]
The second look examination under arthroscopy was performed 12 months after surgery.
2.4. Statistical analysis
The data were analyzed using SPSS 19.0 statistical software (Statistical Product and Service Solutions 19.0, IBM Corporation). Measurement data were expressed as mean ± standard deviation and counting data as frequency (percentage). Baseline variables for the 2 groups were compared with 2-sample t tests for continuous variables, chi-square test for binary variables. Multiple group comparisons were performed by SNK analysis. The level of statistical significance was α = 0.05.
3. Results
A total of 91 patients (54 males, 37 females) with a mean age of 29.3 years (22.2–58 years) who met inclusion and exclusion criteria were included in the study (Table 1). Complications such as stiffness, infection, nerve injury, and deep vein thrombosis after surgery were not observed in any of the groups. The average time of follow-up was 24 months. There were no significant differences (P > .05) in patients’ female ratio, age, and body mass index between groups.
Table 1.
Baseline information and operative characteristics for the 2 groups.
| Group | CKT group | Routine group | P value |
|---|---|---|---|
| Number of patients | 43 | 48 | |
| Gender female | 18 | 19 | .83 |
| Patient age (yr) | 28.6 ± 8.7 | 29.4 ± 9.6 | .67 |
| BMI (kg/m2) | 23.8 ± 1.8 | 23.3 ± 2.5 | .34 |
| Follow-up time (mo) | 23.8 ± 5.4 | 24.4 ± 7.6 | .67 |
BMI = body mass index, CKT = Chinese knotting technique.
There were no significant differences (P > .05) in preoperative IKDC and Lysholm scores between the 2 groups (Table 2). In both groups, the postoperative IKDC and Lysholm score (3 months) was significantly improved (P < .05) compared to the preoperative score. The scores at 6 months were significantly improved (P < .05) compared to 3-month scores, while the scores at 12 months were significantly improved (P < .05) compared to those observed at 6 months, respectively. The postoperative IKDC scores in the CKT group were higher than in the routine group (P < .05) at 3, 6, and 12 months, respectively, but without significant difference (P > .05) at 24 months. The Lysholm scores in the CKT group were higher than in the routine group (P < .05) at 3 months and 6 months, while no significant difference (P > .05) was found between the 2 groups at 12 and 24 months, respectively.
Table 2.
Knee IKDC and Lysholm score in the 2 study groups (3, 6, 12, and 24 mo, postoperatively).
| Group | CKT group | Routine group | P value |
|---|---|---|---|
| IKDC (preoperative) | 41.77 ± 19.33 | 42.43 ± 17.68 | .87 |
| IKDC (3 mo postoperatively) | 62.10 ± 10.00* | 53.88 ± 11.61* | <.01 |
| IKDC (6 mo postoperatively) | 71.92 ± 7.70*,† | 66.25 ± 9.05*,† | <0.01 |
| IKDC (12 mo postoperatively) | 79.98 ± 4.50*,†,‡ | 74.37 ± 7.64*,†,‡ | <.01 |
| IKDC (24 mo postoperatively) | 80.07 ± 4.48 | 79.77 ± 4.59 | .75 |
| Lysholm (preoperative) | 41.09 ± 21.91 | 42.38 ± 18.10 | .76 |
| Lysholm (3 mo postoperatively) | 70.19 ± 12.04* | 61.54 ± 13.34* | <.01 |
| Lysholm (6 mo postoperatively) | 79.19 ± 11.10*,† | 71.73 ± 12.98*,† | <.01 |
| Lysholm (12 mo postoperatively) | 88.77 ± 6.67*,†,‡ | 87.93 ± 9.23*,†,‡ | .63 |
| Lysholm (24 mo postoperatively) | 89.28 ± 6.13 | 88.15 ± 8.75 | .63 |
CKT = Chinese knotting technique, IKDC = International Knee Documentation Committee.
There was significant difference (P < .05) in scores than preoperative score.
There was significant difference (P < .05) compared with 3 mo.
There was significant difference (P < .05) compared with 6 mo.
The knee joint kinematics recorded by Opti_Knee (3D motion analysis system for the knee) revealed no significant difference in maximum step length, minimum step length, and period of the limb walking between the experimental group and control group (Table 3) at 3, 6, and 12 months (P > .05). The internal and external rotation angle (F = 51.141, 13.204) and the anteroposterior displacement (F = 51.246, 12.207) at 3 and 6 months after the operation in the CKT group were smaller compared to the routine group (P < .05; Table 4). There was no significant difference in flexion and extension angle, varus or valgus angle, proximal–distal displacement, or the internal or external displacement between the 2 groups (P > .05). There was no significant difference in 6 freedom degrees of the knee between the 2 groups at 12 months after the operation (P > .05).
Table 3.
Knee kinematics (part 1) in the 2 study groups (3, 6, 12, and 24 mo postoperatively).
| Group | CKT group | Routine group | P value |
|---|---|---|---|
| The maximum step length (cm) | |||
| 3 mo postoperatively | 50.7 ± 3.9 | 50.6 ± 4.6 | >.05 |
| 6 mo postoperatively | 51.2 ± 4.7 | 50.8 ± 4.7 | >.05 |
| 12 mo postoperatively | 52.2 ± 3.3 | 51.6 ± 4.7 | >.05 |
| 24 mo postoperatively | 52.1 ± 4.1 | 51.8 ± 4.5 | >.05 |
| The minimum step length (cm) | |||
| 3 mo postoperatively | 45.0 ± 2.9 | 44.7 ± 2.5 | >.05 |
| 6 mo postoperatively | 44.6 ± 2.8 | 45.8 ± 2.6 | >.05 |
| 12 mo postoperatively | 46.0 ± 2.4 | 45.4 ± 2.8 | >.05 |
| 24 mo postoperatively | 46.1 ± 2.2 | 45.9 ± 3.0 | >.05 |
| The period of the limb walking (cm) | |||
| 3 mo postoperatively | 12.0 ± 0.6 | 12.4 ± 0.5 | >.05 |
| 6 mo postoperatively | 12.1 ± 0.6 | 12.0 ± 1.0 | >.05 |
| 12 mo postoperatively | 12.2 ± 0.8 | 12.1 ± 1.0 | >.05 |
| 24 mo postoperatively | 12.3 ± 0.7 | 12.2 ± 1.1 | >.05 |
CKT = Chinese knotting technique.
Table 4.
Knee kinematics (part 2) in the 2 study groups (3, 6, 12, and 24 mo postoperatively).
| Group | CKT group | Routine group | P value |
|---|---|---|---|
| The flexion and extension angle (°) | |||
| 3 mo postoperatively | 57.12 ± 2.86 | 56.93 ± 1.95 | >.05 |
| 6 mo postoperatively | 57.71 ± 2.22 | 57.93 ± 1.84 | >.05 |
| 12 mo postoperatively | 57.51 ± 1.90 | 57.94 ± 1.80 | >.05 |
| 24 mo postoperatively | 57.63 ± 1.98 | 57.84 ± 1.95 | >.05 |
| The varus and valgus angle (°) | |||
| 3 mo postoperatively | 5.68 ± 0.28 | 5.71 ± 0.24 | >.05 |
| 6 mo postoperatively | 5.76 ± 0.44 | 5.67 ± 0.42 | >.05 |
| 12 mo postoperatively | 5.70 ± 0.47 | 5.61 ± 0.39 | >.05 |
| 24 mo postoperatively | 5.69 ± 0.35 | 5.66 ± 0.47 | >.05 |
| The internal and external rotation angle (°) | |||
| 3 mo postoperatively | 12.06 ± 1.23 | 18.06 ± 2.22 | <.05 |
| 6 mo postoperatively | 11.87 ± 1.47 | 15.57 ± 2.75 | <.05 |
| 12 mo postoperatively | 11.79 ± 1.24 | 12.17 ± 1.14 | >.05 |
| 24 mo postoperatively | 11.65 ± 1.33 | 11.77 ± 1.38 | >.05 |
| The anteroposterior displacement (cm) | |||
| 3 mo postoperatively | 1.29 ± 0.37 | 3.34 ± 0.71 | <.05 |
| 6 mo postoperatively | 1.37 ± 0.41 | 2.42 ± 0.81 | <.05 |
| 12 mo postoperatively | 1.24 ± 0.21 | 1.30 ± 0.34 | >.05 |
| 24 mo postoperatively | 1.23 ± 0.25 | 1.26 ± 0.32 | >.05 |
| The proximal–distal displacement (cm) | |||
| 3 mo postoperatively | 1.30 ± 0.34 | 1.37 ± 0.44 | >.05 |
| 6 mo postoperatively | 1.32 ± 0.41 | 1.37 ± 0.28 | >.05 |
| 12 mo postoperatively | 1.38 ± 0.33 | 1.35 ± 0.32 | >.05 |
| 24 mo postoperatively | 1.35 ± 0.31 | 1.35 ± 0.36 | >.05 |
| The internal and external displacement (cm) | |||
| 3 mo postoperatively | 0.67 ± 0.24 | 0.74 ± 0.27 | >.05 |
| 6 mo postoperatively | 0.68 ± 0.27 | 0.73 ± 0.24 | >.05 |
| 12 mo postoperatively | 0.73 ± 0.22 | 0.72 ± 0.27 | >.05 |
| 24 mo postoperatively | 0.70 ± 0.25 | 0.71 ± 0.30 | >.05 |
CKT = Chinese knotting technique.
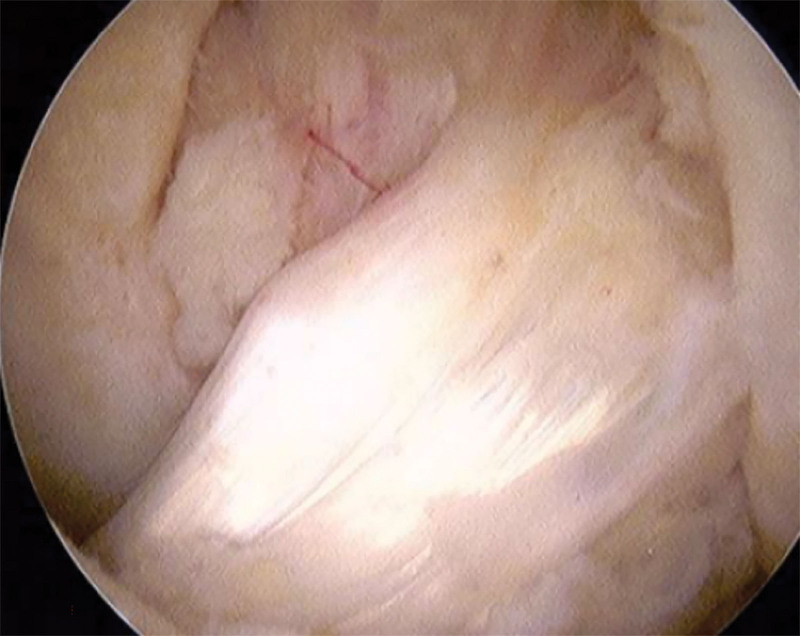
The second arthroscopy examination showed that most grafts grew well in the CKT group (Fig. 5) at 1 year after surgery. The graft was fully covered by synovium, and the tension and shape of the graft looked satisfactory.
Figure 5.
The second arthroscopy examination (12 mo after surgery) showed that all the grafts grew well in the CKT group. The graft was covered by synovium. CKT = Chinese knotting technique.
4. Discussion
In 1980, Kennedy et al[27] proposed the use of ligament augmentation devices to protect the graft, but complications caused by material problems made this technology gradually withdraw from the clinic.[28] With the development of medical biomaterials, FiberTapeTM, EthibondTM, and other high-strength suture (belt) was developed. They exhibit good mechanical properties and biocompatibility.[29–33] The CKT is a braided technique of suture line that only relies on hand-knitting to adjust the ductility and elasticity of the suture line. When the length of each knot is 3 mm, the ductility and elasticity of the braided suture line were similar with the hamstring tendon.[34] EthibondTM suture line braided by CKT can achieve the same shape as the FiberTapeTM. The EthibondTM suture line has been proven to be safe, effective, and biocompatible.[35] When the reconstructed ligament is stretched, it can share a part of the stress with the reconstructed ligament.[36] Before the reconstructed ligament is healed and able to bear external forces, it shares a part of the force and participates in protecting and rebuilding the ligament in the early stage.[37] The results of our study showed that the IKDC scores in the CKT group were significantly higher than in the routine group at 3, 6, and 12 months after surgery, while no difference was observed at 24 months, respectively. The Lysholm scores in the CKT group were significantly higher than in the routine group at 3 and 6 months after surgery, while there was no difference at 12 and 24 months, respectively. The internal and external rotation angle (F = 51.141, 13.204) and the anteroposterior displacement (F = 51.246, 12.207) at 3 and 6 months after the operation in the CKT group were smaller than in the control group (P < .05) and were similar to those observed in the healthy adults (P > .05). These results indicated that the function and stability of the knee in the CKT group were better than in the routine group at an early stage after surgery. These results may be due to the following: besides mature surgical skill and aggressive rehabilitation, the innovative tension-relieving technique with “CKT braided suture” was applied in the CKT group, which may have a critical role in improving the restoring knee’s function, and preventing laxity of graft. Compared to Qi et al’s[38] report, the “CKT braiding suture” leads to such improvements: The internal tensioning relieving technique based on nonabsorbable high-strength sutures can reduce the risk of relaxation and rupture by enhancing the biomechanical strength of tendon grafts. Then it improves postoperative initial joint stability, range of motion, and functional scores in clinical practice. The feasible fast postoperative rehabilitation promotes patients to return to preinjury exercise level by fast postoperative rehabilitation without serious complications.
West et al[39] treated quadriceps and patellar ruptures with a primary repair augmented with a single No. 5 Ethibond suture, reporting that the repairs protected by a relaxing suture were strong enough to safely permit early motion weight-bearing and brace-free ambulation while producing good and excellent results. Hakimi et al[40] confirmed that Ethibond suture showed the best performance in cell attachment and increased biomass. Considering graft fixation, we used Rigfix transverse nail in the femur and absorbable interference screw in the tibia, which is closer to the graft’s intra-articular tunnel entrance. Such more rigid fixation can be used to avoid greater anterior knee laxity and larger graft-tunnel motion, which in turn can lead to so-called “wiping effect” and “bungee effect.”[41–43] Tsuda et al[42] confirmed that, compared to elastic graft fixation like Endobutton, there are 2 adverse effects, that is, horizontal and vertical fretting, respectively. Such adverse effects result in poor bone-graft healing and severe tunnel expansion, which are responsible for graft failure. Besides, such rigid fixation can increase the effective contact area of the grafted bone and reduce the tendon micro-motion. All these advantages can improve tendon–bone healing.[41,43] Consequently, we used the rigid fix system in the femur and in the tibia tunnel to guarantee the least motion between graft and tunnel and greater bone-graft healing. In addition, besides rigid fixation, some researchers have been exploring more auxiliary devices for reducing the passive tension and micro-motion of graft in the rehabilitative process. Sasaki Sandra et al[44] reported that the Ethibond suture could provide ideal fixation strength under cyclic loading conditions. Qi et al[38] applied a tension-relieving technique on graft by using 2 polyester sutures (Ethibond, Depuy Synthes, American) to be intertwined with graft and fixed together. Compared to routine ACL reconstruction, the tension-relieving group acquired a better functional score and stability of the knee in short-term observation, indicating that the tension-relieving suture might reduce the passive force and micro-motion of graft, thus resulting in better bone-graft healing and improved knee function. Ma et al[45] also indicated that early high forces on the ACL graft appear to impair graft-tunnel osseointegration. Hamido et al[46] reported that an augmented short undersized hamstring tendon with LARS artificial ligament could increase the diameter of the graft and improve the clinical outcomes. Sakaguchi et al[47] reported that a special stitch configuration of Ethibond suture could provide a superior locking mechanism, which could prevent slippage. Accordingly, we assumed the CKT technique made by Ethibond suture might ensure the superior biomechanical property of graft, which was in line with Qi et al, Hamido et al, and Sakaguchi et al’s report.[38,46,47]
In conclusion, CKT-assisted ACL reconstruction and active postoperative rehabilitation plan resulted in better knee function score and 3D gait analysis in the early postoperative period. All of which effectively improve the recovery degree of knee joint function and quality of life of patients after surgery. And it does not increase the incidence of postoperative complications. However, the present study has some limitations. First, the sample in this retrospective study was not large, and the follow-up was relatively short (24 months). Future studies should expand the sample of objects and extend the follow-up. Also, new prospective studies with more detailed designs are necessary to strengthen reported conclusions.
5. Conclusions
The application of CKT combined with aggressive rehabilitation can improve the clinical effects of patients without complications. This enhanced ACL reconstruction method may be implemented as a general practice to treat ACL rupture.
Author contributions
YY, XY, and GW participated in the acquisition of the data.
XY, CH, and DL contributed to data analysis.
YY and YL revised the manuscript carefully for important content.
YY, XY, and YL conceived, designed, and led the study.
YY and XY made contributions to the drafting of the manuscript.
All authors read and approved the final manuscript.
Conceptualization: Dejian Liu, Yang Yu, Yanlin Li.
Data curation: Guoliang Wang, Xianguang Yang.
Formal analysis: Xianguang Yang.
Funding acquisition: Yanlin Li.
Methodology: Chuan He, Guoliang Wang, Yang Yu.
Project administration: Chuan He.
Resources: Dejian Liu, Xianguang Yang, Yang Yu, Yanlin Li.
Software: Guoliang Wang.
Supervision: Chuan He.
Validation: Chuan He, Dejian Liu.
Visualization: Dejian Liu, Guoliang Wang.
Writing – original draft: Xianguang Yang, Yang Yu.
Writing – review & editing: Yang Yu.
Abbreviations:
- ACL =
- anterior cruciate ligament
- CKT =
- Chinese knotting technique
- IKDC =
- International Knee Documentation Committee
YY and XY contributed equally to this work.
This study was supported by Yunnan Province Major Science and Technology Special Project [202102AA100015] and Yunnan Province Clinical Center for Bone and Joint Diseases [no. ZX2019-03-04]. The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Yu Y, Yang X, He C, Wang G, Liu D, Li Y. The Chinese knotting technique assist anatomical anterior cruciate ligament reconstruction for aggressive rehabilitation. Medicine 2022;101:35(e30107).
Contributor Information
Yang Yu, Email: 575766076@qq.com.
Xianguang Yang, Email: 844101652@qq.com.
Chuan He, Email: hczraul@sina.com.
Guoliang Wang, Email: 200301144@163.com.
Dejian Liu, Email: 79033475@qq.com.
References
- [1].Chen T, Zhang P, Chen J, et al. Long-term outcomes of anterior cruciate ligament reconstruction using either synthetics with remnant preservation or hamstring autografts: a 10-year longitudinal study. Am J Sports Med. 2017;45:2739–50. [DOI] [PubMed] [Google Scholar]
- [2].Chee MY, Chen Y, Pearce CJ, et al. Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy. 2017;33:450–63. [DOI] [PubMed] [Google Scholar]
- [3].Salmon LJ, Heath E, Akrawi H, et al. 20-Year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46:531–43. [DOI] [PubMed] [Google Scholar]
- [4].Jia C, Aiqun G, Haitao J, et al. A comparison of acute and chronic anterior cruciate ligament reconstruction using LARS artificial ligament: a randomized prospective study with a 5-year follow-up. Arch Orthop Trauma Surg. 2015;135:95–102. [DOI] [PubMed] [Google Scholar]
- [5].Setuain I, Izquierdo M, Idoate F, et al. Differential effects of 2 rehabilitation programs following anterior cruciate ligament reconstruction. J Sport Rehabil. 2017;26:544–55. [DOI] [PubMed] [Google Scholar]
- [6].Pamukoff DN, Pietrosimone BG, Ryan ED, et al. Quadriceps function and hamstrings co-activation after anterior cruciate ligament reconstruction. J Athl Train. 2017;52:422–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Eckenrode BJ, Carey JL, Sennett BJ, et al. Prevention and management of post-operative complications following ACL reconstruction. Curr Rev Musculoskelet Med. 2017;10:315–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ebert JR, Edwards P, Yi L, et al. Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:2353–61. [DOI] [PubMed] [Google Scholar]
- [9].van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506–15. [DOI] [PubMed] [Google Scholar]
- [10].Whitehead TS. Failure of anterior cruciate ligament reconstruction. Clin Sports Med. 2013;32:177–204. [DOI] [PubMed] [Google Scholar]
- [11].Christensen Jesse C, Goldfine Laura R, WestHugh S. The effects of early aggressive rehabilitation on outcomes after anterior cruciate ligament reconstruction using autologous hamstring tendon: a randomized clinical trial. J Sport Rehabil. 2013;22:191–201. [DOI] [PubMed] [Google Scholar]
- [12].Bachmaier S, DiFelice GS, Sonnery-Cottet B, et al. Treatment of acute proximal anterior cruciate ligament tears-part 2: the role of internal bracing on gap formation and stabilization of repair techniques. Orthop J Sports Med. 2020;8:2325967119897423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Barnaś M, Kentel M, Morasiewicz P, et al. Clinical assessment and comparison of ACL reconstruction using synthetic graft (Neoligaments versus FiberTape). Adv Clin Exp Med. 2021;30:491–8. [DOI] [PubMed] [Google Scholar]
- [14].Yung PS, Lee YW, Fu SC, et al. Differential MMP 1 and MMP 13 expression in proliferation and ligamentization phases of graft remodeling in anterior cruciate ligament reconstruction. Connect Tissue Res. 2021;62:681–8. [DOI] [PubMed] [Google Scholar]
- [15].Frangie R, Warth RJ, Harner CD. Editorial commentary: will suture tape augmentation prove to be the answer to anterior cruciate ligament graft remodeling, ultimate strength, and safe return to play? Arthroscopy. 2020;36:490–1. [DOI] [PubMed] [Google Scholar]
- [16].Bachmaier S, Smith PA, Bley J, et al. Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: a biomechanical full construct model. Arthroscopy. 2018;34:490–9. [DOI] [PubMed] [Google Scholar]
- [17].Noonan BC, Bachmaier S, Wijdicks CA, et al. Independent suture tape reinforcement of tripled smaller-diameter and quadrupled grafts for anterior cruciate ligament reconstruction with tibial screw fixation: a biomechanical full construct model. Arthroscopy. 2020;36:481–9. [DOI] [PubMed] [Google Scholar]
- [18].Matava MJ, Koscso J, Melara L, et al. Suture tape augmentation improves the biomechanical performance of bone-patellar tendon-bone grafts used for anterior cruciate ligament reconstruction. Arthroscopy. 2021;37:3335–43. [DOI] [PubMed] [Google Scholar]
- [19].Smith PA, Bradley JP, Konicek J, et al. Independent suture tape internal brace reinforcement of bone-patellar tendon-bone allografts: biomechanical assessment in a full-ACL reconstruction laboratory model. J Knee Surg. 2020;33:1047–54. [DOI] [PubMed] [Google Scholar]
- [20].Zhang Y, Yao Z, Wang S, et al. Motion analysis of Chinese normal knees during gait based on a novel portable system. Gait Posture. 2015;41:763–8. [DOI] [PubMed] [Google Scholar]
- [21].Zhang Y, Huang W, Yao Z, et al. Anterior cruciate ligament injuries alter the kinematics of knees with or without meniscal deficiency. Am J Sports Med. 2016;44:3132–9. [DOI] [PubMed] [Google Scholar]
- [22].Zhong G, Zeng X, Xie Y, et al. Prevalence and dynamic characteristics of generalized joint hypermobility in college students. Gait Posture. 2021;84:254–9. [DOI] [PubMed] [Google Scholar]
- [23].Zeng X, Ma L, Lin Z, et al. Relationship between Kellgren-Lawrence score and 3D kinematic gait analysis of patients with medial knee osteoarthritis using a new gait system. Sci Rep. 2017;7:4080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Tian F, Li N, Zheng Z, et al. The effects of marathon running on three-dimensional knee kinematics during walking and running in recreational runners. Gait Posture. 2020;75:72–7. [DOI] [PubMed] [Google Scholar]
- [25].Wang S, Zeng X, Huangfu L, et al. Validation of a portable marker-based motion analysis system. J Orthop Surg Res. 2021;16:425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Smith JO, Yasen SK, Palmer HC, et al. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc. 2016;24:1845–51. [DOI] [PubMed] [Google Scholar]
- [27].Kennedy JC, Roth JH, Mendenhall HV, et al. Presidential address: intraarticular replacement in the anterior cruciate ligament-deficient knee. Am J Sports Med. 1980;8:1–8. [DOI] [PubMed] [Google Scholar]
- [28].Kumar K, Maffulli N. The ligament augmentation device: an historical perspective. Arthroscopy. 1999;15:422–32. [DOI] [PubMed] [Google Scholar]
- [29].Lewis TL, Joseph A, Patel A, et al. Modified Broström repair with suture tape augmentation for lateral ankle instability: a systematic review. Foot Ankle Surg. 2021;27:278–84. [DOI] [PubMed] [Google Scholar]
- [30].Saper MG. Quadriceps tendon autograft anterior cruciate ligament reconstruction with independent suture tape reinforcement. XXXArthrosc Tech. 2018;7:e1221–e1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].McGee R, Daggett M, Jacks A, et al. Patellar tendon graft anterior cruciate ligament reconstruction technique with suture tape augmentation. Arthrosc Tech. 2019;8:e355–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Anderson SR, Youssefzadeh KA, Limpisvasti O. Anterior cruciate ligament reconstruction with suture tape augmentation: a surgical technique. Arthrosc Tech. 2019;8:e1579–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Benson DM, Hopper GP, Wilson WT, et al. Anterior cruciate ligament reconstruction using bone-patellar tendon-bone autograft with suture tape augmentation. Arthrosc Tech. 2021;10:e249–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Mao J, Yanlin L I, Wang G, et al. Anterior cruciate ligament tear treated by arthroscopic tension-relieving reconstruction and enhanced recovery after surgery [in Chinese]. Chin J Orthop Trauma. 2018;20:38–44. [Google Scholar]
- [35].Smith PA, Bozynski CC, Kuroki K, et al. Intra-articular biocompatibility of multistranded, long-chain polyethylene suture tape in a canine ACL model. J Knee Surg. 2019;32:525–31. [DOI] [PubMed] [Google Scholar]
- [36].van Eck CF, Limpisvasti O, ElAttrache NS. Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med. 2018;46:2291–8. [DOI] [PubMed] [Google Scholar]
- [37].Yoo JS, Yang EA. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17:353–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Qi Y, Fan YG, Sun HT. Clinical study of internal tension-relieving technique in arthroscopic assisted anterior cruciate ligament reconstruction. Chin J Repar Reconst Surg, 2016;30:138–42. [PubMed] [Google Scholar]
- [39].West JL, Keene JS, Kaplan LD, et al. Early motion after quadriceps and patellar tendon repairs: outcomes with single-suture augmentation. Am J Sports Med. 2008;36:316–23. [DOI] [PubMed] [Google Scholar]
- [40].Hakimi O, Chaudhury S, Murphy R, et al. Differential growth on sutures of tendon cells derived from torn human rotator cuff. J Biomed Mater Res B Appl Biomater. 2012;100:685–92. [DOI] [PubMed] [Google Scholar]
- [41].Parkinson B, Robb C, Thomas M, et al. Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:1529–36. [DOI] [PubMed] [Google Scholar]
- [42].Tsuda E, Fukuda Y, Loh JC, et al. The effect of soft-tissue graft fixation in anterior cruciate ligament reconstruction on graft-tunnel motion under anterior tibial loading. Arthroscopy. 2002;18:960–7. [DOI] [PubMed] [Google Scholar]
- [43].Antonogiannakis E, Yiannakopoulos CK, Hiotis I, et al. Arthroscopic anterior cruciate ligament reconstruction using quadriceps tendon autograft and bioabsorbable cross-pin fixation. Arthroscopy. 2005;21:894. [DOI] [PubMed] [Google Scholar]
- [44].Sasaki Sandra U, da Mota e Albuquerque RF, Amatuzzi MM, et al. Open screw fixation versus arthroscopic suture fixation of tibial posterior cruciate ligament avulsion injuries: a mechanical comparison. Arthroscopy. 2007;23:1226–30. [DOI] [PubMed] [Google Scholar]
- [45].Ma R, Schär M, Chen T, et al. Effect of dynamic changes in anterior cruciate ligament in situ graft force on the biological healing response of the graft-tunnel interface. Am J Sports Med. 2018;46:915–23. [DOI] [PubMed] [Google Scholar]
- [46].Hamido F, Al Harran H, Al Misfer AR, et al. Augmented short undersized hamstring tendon graft with LARS® artificial ligament versus four-strand hamstring tendon in anterior cruciate ligament reconstruction: preliminary results. Orthop Traumatol Surg Res. 2015;101:535–8. [DOI] [PubMed] [Google Scholar]
- [47].Katsunobu S, Yomei T, Hiromi O. Biomechanical properties of porcine flexor tendon fixation with varying throws and stitch methods. Am J Sports Med. 2012;40:1641–5. [DOI] [PubMed] [Google Scholar]