Summary
Background
In low-and-middle income countries, corneal abrasions and ulcers are common and not always well managed. Previous studies showed better clinical outcomes with early presentation and treatment of minor abrasions, however, there have been no formal studies estimating the financial impact of early treatment of abrasions and ulcers compared to delayed treatment.
Methods
We used the LV Prasad Eye Institute's (LVPEI's) electronic health record system (eyeSmart) to estimate the impact of early presentation on clinical outcomes associated with abrasions and ulcers. 861 patients with corneal abrasion and 1821 patients with corneal ulcers were studied retrospectively, and 134 patients with corneal abrasion prospectively. A health economic model was constructed based on LVPEI cost data for a range of patient scenarios (from early presentation with abrasion to late presentation with ulcer).
Findings
Our findings suggest that delayed presentation of corneal abrasion results in poor clinical and economic outcomes due to increased risk of ulceration requiring more extensive surgical management, increasing associated costs to patients and the healthcare system. However, excellent results at low cost can be achieved by treatment of patients with early presentation of abrasions at village level health care centres.
Interpretation
Treatment of early minor corneal abrasions, particularly using local delivery of treatment, is effective clinically and economically. Future investment in making patients aware of the need to react promptly to corneal abrasions by accessing local healthcare resources (coupled with a campaign to prevent ulcerations occurring) will continue to improve clinical outcomes for patients at low cost and avoid complex and more expensive treatment to preserve sight.
Funding
This research was funded by the Medical Research Council, grant MR/S004688/1.
Keywords: Health economics, Corneal abrasion, Corneal ulcer, Early treatment, Health policy
Research in context.
Evidence before this study
Corneal ulceration is a leading cause of corneal blindness. An innocent looking corneal abrasion can lead to corneal ulcer if not taken care of with early management. There are studies on the early management of corneal abrasions from India, Nepal, Burma and Bhutan which are consistent on treating early abrasions to prevent their development into ulcers. There are however few reports on how this is to be achieved with associated economic implications. One study reported that the management of infectious keratitis is higher than the average monthly income of a patient from a developing country.
Added value of this study
Costing of the management of corneal abrasion is rarely reported in the literature. In this study we estimate the costs and outcomes for various scenarios wherein the patient has only corneal abrasions, management of corneal ulcers when small and the management of corneal ulcers when large with additional surgical management, travel costs, and lost wages. The structure of LVPEI allowed us to compare costs to both the health care system as well as the patients when patients are managed locally in village-based vision centres managed by healthcare staff with low levels of training compared to management of the same patients by more highly trained staff in secondary centres. Our study showed that patients did as well clinically in the local centres as in the centres with more highly trained staff providing abrasions were detected and treated early. We show the costs to the patient and healthcare system were less with local treatment.
Implications of all the available evidence
Our study shows that when corneal abrasions occur then local rapid treatment can produce good clinical and economic results for patients. Given the high incidence of corneal abrasions in the population then establishing local resources for prompt treatment to prevent ulcers developing is merited based on both clinical and economic evidence.
Alt-text: Unlabelled box
Introduction
Corneal ulceration, which is easily countered by early diagnosis and treatment in the Western world, is considered a “silent epidemic” in low-and-middle income countries (LMICs).1 The main cause of corneal ulcers varies with geographical locations: in developed countries it is typically associated with contact lens wear while in developing countries, corneal ulcers are often due to injury which primarily afflicts labourers involved in agriculture, manufacturing and domestic sectors.2, 3, 4, 5, 6, 7
There is a growing body of published literature showing that treatment of early-stage corneal abrasions leads to good clinical results.8 If treatment is delayed, the abrasion can be infected (by bacteria, fungi, or parasites) and lead to corneal ulceration.8 Once the cornea is ulcerated, it develops corneal opacity that adversely affects vision. Delayed presentation of corneal ulcers can result in extensive damage to corneas with consequent loss of vision or loss of the eye.9
Patients in LMIC face significant barriers in accessing eye care and infections are often treated only after severe delays, with unintended consequences. The health infrastructure is often poor or entirely lacking, and patients resort to using homemade remedies or traditional healers, thereby delaying the appropriate treatment10,11 As a result, simple corneal abrasions rapidly progress into corneal infections. The patients affected suffer from pain, red and watery eyes and are therefore unable to work resulting in huge financial implications due to lost livelihood and treatment costs.
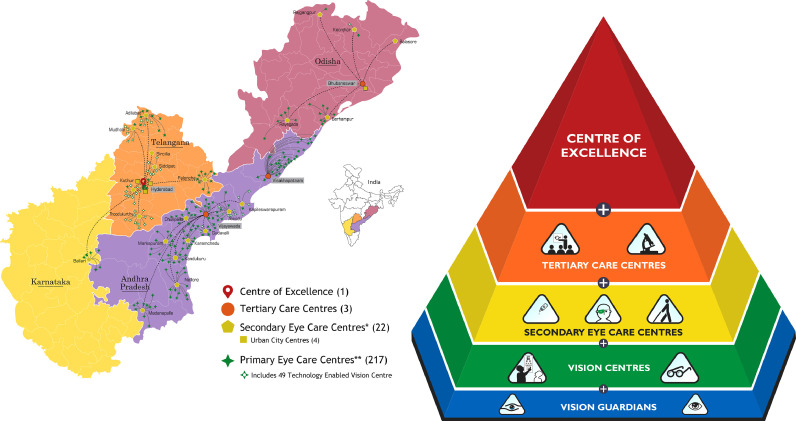
The LVPEI model of eye care comprises of a centre of excellence in Hyderabad located at the apex of a treatment pyramid. The next level has three tertiary eye care centres (TCs), each serving a population of 5m people (Figure 1).12 The third tier has twenty-two secondary centres (SCs) located in towns and smaller cities (within 350 km of a TC) predominantly providing basic surgical and diagnostic care, each serving a population of approximately 500,000 patients. A fourth layer of the pyramid consists of 217 primary vision centres (VCs) managed by a ‘vision technician’ and these are located in the village clusters, each serving approximately 50,000 people. These VCs are supported by the fifth layer, a network of ‘vision guardians’ (trained eye care volunteers who monitor the eye health of their community members).12
Figure 1.
LVPEI Eye Health Pyramid (showing five tiers and locations of the centres).
The third tier is the Secondary centres and the fourth is the Vision centres.
(Copyright – Ms Neha Hasija, Head, Communications Department, LVPEI, Hyderabad).
Though this approach brings treatment closer to the patients, there have been no formal studies looking at whether this approach actually delivers improvements in clinical outcomes for patients with corneal abrasion and ulceration or whether it reduces the financial burden in eye care among poor rural communities.13 The aim of this study is to compare the clinical and financial impact of early treatment of abrasions and ulcers compared to delayed treatment. To do this, we analysed both prospective and retrospective data collected at LV Prasad Eye Institute (LVPEI) and performed modelling to estimate the cost impacts and health outcomes of different scenarios.
Methods and data
Corneal abrasion and ulcer pathway
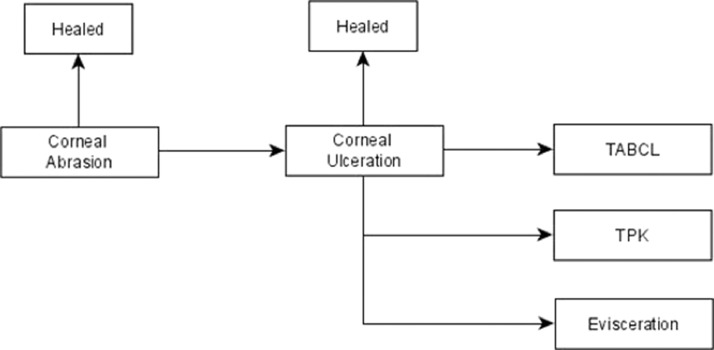
Pathways for management of corneal abrasions and corneal ulcers were developed to identify the key outcomes and cost data that needed to be captured from LVPEI. A detailed pathway for disease progression of corneal abrasion was developed in consultation with clinical experts and this detailed pathway was then consolidated to streamline the outcomes and treatment regimens. Figure 2 shows a simplified overview of outcomes identified in the management of corneal abrasions and ulcers.
Figure 2.
Corneal abrasion and ulcer pathway. Healing of corneal abrasion with medical management only, on worsening to corneal ulcer which either heals with medical management only or may need in addition to the medical management, Tissue adhesive and bandage contact lens application (TABCL), or therapeutic penetrating keratoplasty (TPK), or evisceration.
All patients with abrasions could either heal with topical treatment or worsen to corneal ulcers, which could also heal with topical treatment. The current practice for management of patients presenting with abrasion is to use topical antibiotics and with corneal ulcers is to use topical antibiotics and antifungal treatments (which include topical ciprofloxacin, fortified cefazolin, atropine, natamycin and oral ketoconazole), with the dosage and duration depending on the stage of the disease as outlined in the Appendix. Patients with corneal ulcers which do not heal need surgical procedures such as tissue adhesive and bandage contact lenses (TABCL) for treating thinning of the cornea or small perforations, therapeutic penetrating keratoplasty (TPK) for treating large perforations or larger ulcers, or even evisceration if the infection is too widespread in the eye and the eye is not salvageable.
Data
LVPEI has an established electronic record-keeping system (eyeSmart) that tracks patients with unique identifiers through the different tiers, allowing a wealth of data to be extracted retrospectively about treatment regimens and outcomes.14 For patients with corneal abrasions, retrospective data (861 patients) was supplemented with a small prospective study (134 patients) on patients with corneal abrasions attending VCs and SCs. Retrospective data also included 1821 patients with corneal ulcers (644 from SCs, 1177 from TCs). Institutional approval was sought from LVPEI (Ethics Ref No: Retrospective study: LEC BHR-R-04-21-603, Prospective study: LEC BHR-P-04-21-621). The months for prospective data collection were chosen at the start of the project for convenience. For retrospective data, we wanted to use the most recent data, and data that was not affected by the Covid-19 pandemic and hence we decided to use the 2019 data. Data for retrospective and prospective patients were extracted from electronic medical records using the electronic record-keeping system. Please see Appendix 1 for full details on the recruitment and data collection process. The prospective study had complete follow up and the retrospective study included only cases with full follow up.
Data on patients with corneal abrasion
Prospective data on new patients seen at VCs with the diagnosis of corneal abrasions or injury were collected for two months (May and June 2021) at 18 VCs and two SCs. The centres were selected based on having high volume of corneal patients and being geographically accessible. Patients gave informed consent. Teleconsultations for patients at VCs were performed with cornea specialists and appropriate treatment was provided. In the case of eyes worsening over the follow-up period, the patients were referred to the SCs. The same protocol was used at Secondary centres. Cornea specialists followed up the patients of corneal abrasions at SCs and worsening to corneal ulceration was noted.
Retrospective data for patients with corneal abrasions were captured from 19 SCs between January 2019 and December 2019, spread across four states in India, including the two SCs where the prospective arm of the study was done. All new patients with a first diagnosis of corneal abrasions were included, and the development of corneal ulceration in these patients was captured.
Data on patients with corneal ulceration
Retrospective data for patients with corneal ulcers were captured from 19 SCs as mentioned above and a TC between January 2019 and December 2019. The outcomes included healing of the ulcers with medical management only (either the ulcer healed or was in the healing stage at the last follow up), healing of the ulcer after tissue adhesive and bandage contact lens (TABCL) application, those patients who needed therapeutic penetrating keratoplasty (TPK) and those patients whose eyes were eviscerated.
Key variables
Two key aspects were studied: time of the presentation with abrasion and size of the ulcer. Data on patients with corneal abrasions was analysed to assess the impact of time of presentation on the clinical outcomes. Early presentation was defined as presenting within two days of abrasion while late presentation was defined as those presenting later than two days after abrasion. This analysis was performed separately on retrospective and prospective data to allow comparison of findings.
Data on patients with corneal ulcers was analysed to assess the impact of size of ulcer on the clinical outcomes. Size of corneal ulcers was measured as the product of the length at the widest dimension and at the perpendicular dimension. Small ulcers were defined as being less than 16 mm2 while large ulcers were defined as being greater than 16 mm2. This analysis was performed separately for SCs and TC, as it was suggested by clinical experts that TCs typically receive more complex cases than SCs.
Statistical analysis
We assessed the incidence of corneal ulcers among patients with corneal abrasion, and we also estimated the incidence separately among those presented within two days and later than two days. The incidence parameters were estimated as proportion of corneal abrasion patients who developed ulcers and proportion of corneal ulcer patients experiencing different outcomes. A Chi square test was used to analyse association between categorical data – proportions of abrasions that healed when presented early versus late (after two days). We also assessed the proportions that healed with medical management and surgical procedures in relation to the size of the ulcer and location of the patients. Univariate and multivariate analysis of risk factors was done for healing versus surgical management of corneal ulcers. Data was collected in a spreadsheet (MS Excel 2013) and statistical analysis was done using the Stata Software version 14.1 (StataCorp, Texas). A P value of <0.05 was considered statistically significant.
Scenario modelling
We performed scenario modelling to estimate the costs and clinical outcomes for the management of patients in three scenarios, ranging from the best case to the worst case.
The first scenario is early presentation with abrasion at VCs, where it was assumed that all patients with abrasion present within 2 days (i.e., early presenters) and treated at VCs, and it was assumed that any of the ulcers developed would be small (<16 mm2) and treated at SCs.
The second scenario is early presentation with ulcers at SCs, where it was assumed that all ulcers developed would be small (<16 mm2) and treated at SCs.
The third scenario is late presentation with ulcers at TCs, where it was assumed that all ulcers developed would be large (>16 mm2) and treated at TCs.
A de novo spreadsheet model was developed using results of the data analysis as inputs to estimate the clinical outcomes for the different scenarios. The model was populated with cost data, the health care costs and patient costs depending on the treatment setting for corneal ulcers or abrasions. The health care costs included the costs of topical treatment, costs of surgery and the hospital stay costs. The patient costs included the lost wages due to the condition and the travel costs. The health care costs were estimated from LVPEI hospital tariffs and the patient costs were estimated using bottom up costing methods, based on the resource use estimated by the clinical experts who were presented with the detail seen in the Appendix 2.
The clinical outcomes for the different scenarios were combined with the cost estimates at different settings to estimate the total costs of management under different scenarios, from a healthcare system perspective (which included the health care costs only) and a societal perspective (which included both health care and patient costs). Probabilistic analyses were performed using Monte Carlo simulations to capture the uncertainty in the input parameters, beta distributions were used for the clinical parameters and the cost parameters were varied within +/- 10% of the mean values. The results were estimated as the average of 1000 model runs.
Role of the funding source
The funder of the study had no role in the study design, collection, analysis, and the interpretation of data, or writing of the manuscript.
Results
Data on patients with corneal abrasions
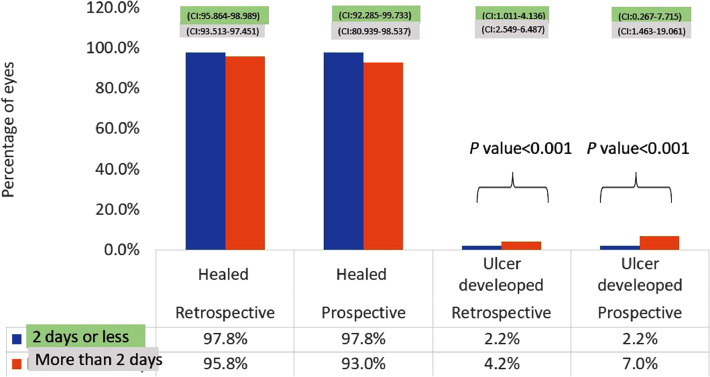
Prospective data included 134 patients with corneal abrasions (88 from VCs, 46 from SCs) while retrospective data comprised of 861 patients with corneal abrasions managed in SCs. Figure 3 shows the comparison of prospective and retrospective data for patients with corneal abrasions, and more detailed results are presented in the Appendix 1.
Figure 3.
Outcomes of patients presenting with corneal abrasions presented as prospective and retrospective data, and early vs late presenters.
Early presenters in both prospective and retrospective study had lesser number of patients developing corneal ulcer compared to delayed presentation in both prospective and retrospective study. (SC – Secondary Centre, TC Tertiary Centre, CI: Confidence Interval).
Results of the prospective data analysis suggested that of the total 134 patients who had corneal abrasions, five of those patients receiving treatment at VCs/SCs developed ulceration 3·7% (5/134; CI 1·222, 8·493). However, only 2·2 % (2/91; CI 0·267, 7·715) of early presenters (who presented within two days of getting injured) developed ulcers but 7% (3/43; CI, 1·463, 19·061) of late presenters (who presented after two days of injury) developed ulcers. The P value was statistically significant (P value <0·001).
Results of the retrospective data analysis substantiated these findings. Corneal ulcers developed in 27/861 patients (3.7%), with corneal ulcers developing in 2·2% (9/409; CI 1·011, 4·136) of those who presented early within two days and in 4·2% (19/452; CI, 2·549. 6·487) of the late presenters who presented after two days. The P value was statistically significant (P value <0·001).
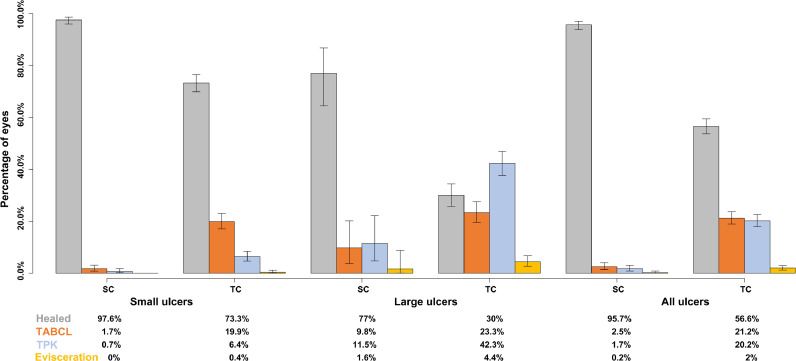
Data on patients with corneal ulceration
Retrospective data included 1821 patients with corneal ulcers (644 from SCs, 1177 from TCs). Of these, 71·72% had small ulcers and 28·28% had large ulcers. Healing was noted in 70·35% of patients with medical management, 14·66% patients had TABCL. 13·67% of patients underwent TPK, and 1·32% of patients underwent evisceration. The P value was statistically significant (P value <0·001) for healing when compared to the size of the ulcers and when compared to the location of the patients. Figure 4 shows the comparison of outcomes by the size of corneal ulcers and the setting of treatment, suggesting that outcomes were worst for patients with large ulcers receiving treatment at TCs. Age at the time of presentation (elderly people), large ulcers, delayed presentation, and poor socioeconomic status were associated with higher risk of surgical intervention. More detailed results are presented in the Appendix 1.
Figure 4.
Influence of corneal ulcer size and treatment location on clinical outcomes.
A higher number of patients healed when presented with small ulcers (at both SC and TC), and more number of patients needed surgical treatment when presented at TC. (SC- Secondary Centre, TC – Tertiary Centre, CI: Confidence Interval).
Scenario analysis assuming early presenters with abrasion at VC
In this scenario, it was assumed that all patients with abrasions present within 2 days (early presenters) and treated at VCs, and it was assumed that any of the ulcers developed would be small (<16 mm2) and treated at SCs. As such, using the data from Figure 3, 97·8% of patients heal at VCs and only 2·2% of the patients develop ulcers. Using the data on outcomes for small ulcers treated at SCs from Figure 4, we estimate that a further 2·1% achieve healing while the rest need TABCL, TPK or evisceration. Combining these, we estimate that in this scenario, 99·94% of the patients are healed while 0·04% need TABCL, 0·02% need TPK, and almost none need evisceration.
The health care costs (including treatment costs, drug costs and hospital stay costs) were estimated for healing at VC (INR 18), healing at SC (INR 2100), TABCL at SC (INR 5800), TPK at SC (INR 29,200) and evisceration at TC (INR 19,100). Combining these health care costs with the outcomes outlined above, results in an average health care cost of INR 70 per patient if patients with abrasions are treated early at VCs. The patient costs (for lost livelihood and transport costs) are an average additional cost of INR 210 per patient with abrasions. Combining these results gave an average societal cost of INR 280 if patients with abrasions are treated early at VCs.
Scenario analysis assuming early presenters with ulcers at SC
In this scenario, it was assumed that all ulcers that developed would be small (<16 mm2) and treated at SCs. As such, using the data from Figure 4, almost 98% of patients with ulcers heal at SCs and only 2% of the patients need TABCL, TPK or evisceration.
The health care costs were estimated for treatment of ulcers at SC (INR 2100), TABCL at SC (INR 5800), TPK at TC (INR 29,200) and evisceration at TC (INR 19,100). Combining these health care costs with the outcomes outlined above, results in an average health care cost of INR 2400 per patient, if patients with ulcers are treated early at SCs. The patient costs (for lost livelihood and transport costs) are an average cost of INR 9320 per patient with ulcer, if treated early at SCs. Combining these, results in an average societal cost of INR 11,720 if patients with ulcers are treated early at SCs.
Scenario assuming late presenters with ulcer at TC
In this scenario, it was assumed that all ulcers developed would be large (>16 mm2) and treated at TCs. As such, using the data from Figure 4, only 30% of patients with ulcers heal at TCs while 23% need TABCL, 42% need TPK, and 4% need evisceration.
The health care costs were estimated for treatment for ulcers at TC (INR 12,800), TABCL at TC (INR 17,400), TPK at TC (INR 29,200) and evisceration at TC (INR 19,100). Combining these health care costs with the outcomes outlined above, results in an average health care cost of INR 21,100 per patient, if patients with ulcers are treated late at TC. The patient costs (for lost livelihood and transport costs) are an average cost of INR 37,750 per patient with ulcer, with delayed treatment at TC. Combining these, results in an average societal cost of INR 58,850, if patients with ulcers are treated late at TCs.
Summary of the results
Table 1 presents the summary results of the mean values and confidence intervals of clinical and cost outcomes for the three different scenarios. The cost outcomes are presented from a health care perspective, patient perspective and total costs from societal perspective, which includes the patient costs along with the health care costs.
Table 1.
Clinical and cost outcomes for the different scenarios.
| Scenario | Proportion healed | Proportion needing TABCL | Proportion needing TPK | Proportion needing evisceration | Average health care costs in INR | Average patient costs in INR | Average societal costs* in INR |
|---|---|---|---|---|---|---|---|
| Early presenters with abrasions at VC | 99·94% (99.91%, 99.99%) | 0·04% (0.00%, 0.07%) | 0·02% (0.00%, 0.03%) | 0.00% (0.00%, 0.02%) | 70 (40, 105) | 210 (75, 340) | 280 (110, 440) |
| Early presenters with ulcers at SC | 97.60% (96.81%, 99.08%) | 1·7% (0.69%, 2.73%) | 0·69% (0.02%, 1.36%) | 0.01% (0.00%, 0.93%) | 2400 (2010, 2800) | 9320 (7890, 10,800) | 11,720 (9950, 13,500) |
| Late presenters with ulcers at TC | 30.33% (24.25%, 36.40%) | 23.26% (19.51%, 27.02%) | 42.26% (37.90%, 46.63%) | 4.15% (2.35%, 5.94%) | 21,100 (18,800, 23,400) | 37,750 (34,070, 41,430) | 58,850 (53,200, 64,500) |
Includes both health care costs and patient costs.
TABCL – Tissue adhesive and bandage contact lens.
TPK – Therapeutic penetrating keratoplasty.
Discussion
To the best of our knowledge, this is the first study to show the costs and outcomes of early management of corneal abrasions and to show the increasing cost and the complexity of the management as the delay increases. We developed a de novo model to estimate the costs and clinical outcomes of different scenarios for diagnosis and treatment of corneal ulcer. The model is based on robust prospective and retrospective data from a large representative sample of LVPEI patients in different treatment settings. Furthermore, cost data was based on bottom-up costing for the different health care and patient costs, based on the type of treatment and the treatment setting. Data analysis suggested that the clinical outcomes are better when patients present early, and when the ulcers are small. Scenario modelling showed clearly that the best outcomes and lowest costs are when patients present early at the abrasion stage and the costs when patients present with ulcers are substantially higher along with poorer outcomes, especially when presenting late with large ulcers at TCs.
Our study confirms previous findings that patients who present early with small abrasions experience a better clinical outcome than those presenting late with infected ulcers.8,15,16 Upadhyay et al. performed a two-year study on 34,902 individuals in Nepal and reported that prophylactic antibiotics after corneal abrasion can help avoid corneal ulceration (with only 4% of the patients developing ulcers which is similar to the rates observed in our study), with earlier treatment associated with better clinical outcomes similar to the findings in our study.8 Getshen et al. have reported no cases of ulceration in Bhutan, when the abrasions were treated within 48 hours with antibiotics.17 Similar findings were reported from Burma when topical antifungal and antibacterial were combined and no ulcers were reported.18 Srinivasan et al. have reported a similar regimen used in South India looking at topical antibiotics and a placebo group and compared with topical antibiotics and antifungals and reported healing in 98.5% of patients with few having adverse events and two developed infiltrates in the placebo group which were microbiologically sterile and managed with Natamycin eye drops.19 Recent studies by Srinivasan et al. and O'Brien et al. did not find any difference in the reduction of the incidence of corneal ulceration in community-based corneal ulcer prevention programme.20,21 Whilst our study was not randomized, given the sample size in our study and the broad catchment area (LVPEI covers fours states of India and has patients reporting from all over the country), we believe LVPEI is representative of the general population in India.
Delayed treatment involves patient costs for travel (to SCs and TCs) and lost wages, resulting in substantial financial impact and physical suffering for patients. While there are other studies looking at cost outcomes associated with early treatment of abrasions or ulcers, there is no study (as far as we know) that has developed comprehensive scenarios to model the potential cost and clinical impact of treating patients earlier at VCs/SCs. A recent study by Komal et al. presented the economic benefits associated with the use of a teleophthalmology vision centre in treating corneal disorders in southern India.22 The study reported reduced travel costs for the patients and reported that a patient can save approximately a minimum of INR 1200 (USD 16) by being treated closer to home than requiring travel to a hospital.22 However, this study did not model the clinical outcomes in details and did not incorporate the impact of delayed treatment on the outcomes and the costs.22
There were certain assumptions used to estimate the costs, which may not always hold true, but they represent our best knowledge about the treatment practices at LVPEI in India. For example, the costs of topical treatments used in the model are estimated on the assumption of the use of a ‘cocktail’ therapy of both anti-fungal and anti-bacterial treatments as fungi and bacteria are the most common pathogens in India associated with corneal infections. While it is possible to target the most appropriate therapy (i.e., fungal, or bacterial) based on results of diagnostic testing, these facilities are not always available in each setting. Also, we have not included the costs for any side effects to the medications (e.g., allergic reactions) due to the low likelihood of such side effects. Further, the costs used in the model such as the surgery costs and hospital stay costs (and the patient costs) may not be completely transferable to other settings. The costs used in the study are based on the data available at LVPEI and reflect the patient journeys with corneal abrasions and ulcers. Other limitations of the study include the prospective study being carried out during the recent pandemic and travel cost of patients’ attendants not being considered. Furthermore, as the focus was to estimate clinical and cost impact of different scenarios at a population level, none of the analyses were adjusted for populations characteristics and other risk factors.
Corneal ulceration is a disease that begins as a simple minor trauma or abrasion but can finally end up with unnecessary and often prolonged physical and financial suffering and is of concern in the population that has limited resources to take care of this problem.8 Corneal infection in developing nations is estimated to be 10 times more than in developed nations. This being a major and large unmet global health need, WHO has estimated 1.5-2.0 million new cases of unilateral blindness each year worldwide. Despite the high incidence and the poor outcomes, preventative strategies are not common.8,16, 17, 18 Whilst use of eye protection during labour is recommended, it is typically not used in India and LMICs, so early diagnosis and treatment is currently the most effective strategy.23 The underlying objective is to prevent corneal abrasions becoming ulcers, identifying abrasions and initiating appropriate treatment can prevent infection and further referrals to distant higher centres. Also, liberal use of antibiotics is known to cause the rise of anti-microbial resistance and may make future treatment challenging.24, 25, 26
With the extensive patient population managed through the LVPEI pyramidal model which has invested in training of village-based eye care workers then the cost is spread across a large patient population. This improves affordability, whereas the costs would be higher in sparsely populated settings or if the incidence of corneal abrasions were lower. In other words, this model of investing in training of low-skilled technical staff distributed to be village based, developed in response to perceived clinical need, is working both clinically and economically.
The LVPEI pyramidal model suggests that patients being treated at the early abrasion stage minimises the costs and achieves good health outcomes. However, delayed treatment, due to some not seeking health care until abrasions become ulcers, results in substantial financial implications with potentially serious health consequences. As the VCs are equipped with teleconsultations facilities, unnecessary travel and loss of income for patients and their families is prevented. The important role played by vision guardians and community health workers with relatively little training is highlighted in this study. They can also play a crucial role to increase awareness among such patients, where the incidence of corneal abrasions in the population is high, other LMICs can follow the LVPEI model and reach out to patients in their local settings.
Conclusions
Early treatment of corneal abrasions is crucial in prevention of ulceration and thereby the cascade of the management of the corneal ulcer in patients and the cost borne by them, as proven by both prospective and retrospective analysis as well as scenario modelling. Increasing awareness with campaigns so that patients will act promptly when they develop corneal abrasions by accessing the local healthcare with early treatment, may help in prevention of ulcerations and improve clinical outcome at low cost and will avoid complex and expensive treatment thus preserving sight and reducing corneal blindness.
Contributors
VMR, PT, SM, RCK, PM and PG conceptualized the manuscript. VMR, PG and RCK were responsible for data collection and figures. VMR, PT, SM and RCK participated in formal analysis. VMR, PT, SM, RCK, PM and PG were involved in the methodology, data analysis, data interpretation, and writing the manuscript. PT, PG, SM and PM were involved in the funding acquisition. PG, RCK, PM and SM supervised. Literature search was done by VMR, PT, RCK and PG.
Data sharing statement
Anonymised participant data will be made available, upon requests based on the scientific merit of the request and data can be shared after signing a data access agreement after all authors approval.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
PM reports funding for the current study from Medical Research Council and PM is a co-inventor on a patent (WO2021175809 02/03/21) for a new treatment for epithelial infections. The treatment is not mentioned here. PG has reported grant from Indian Council of Medical Research, Department of biotechnology, Government of India in Institute's name. RCK has reported grant from Lions Club International SightFirst Research Grant (SFP2170/UND) and United States Agency for International Development (USAID) (Grant No CBP 033) in Institute's name. Rest of the authors declare no competing interests.
Funding
This research was funded by the Medical Research Council, grant MR/S004688/1. For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lansea.2022.100038.
Appendix. Supplementary materials
References
- 1.Whitcher JP, Srinivasan M. Corneal ulceration in the developing world–a silent epidemic. Br J Ophthalmol. 1997;81(8):622–623. doi: 10.1136/bjo.81.8.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Truong DT, Bui MT, Cavanagh HD. Epidemiology and outcome of microbial keratitis: private university versus urban public hospital care. Eye Contact Lens. 2018;44(suppl 1):S82–S86. doi: 10.1097/ICL.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Szczotka-Flynn LB, Shovlin JP, Schnider CM, et al. American academy of optometry microbial keratitis think tank. Optom Vis Sci. 2021;98(3):182–198. doi: 10.1097/OPX.0000000000001664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ung L, Bispo PJM, Shanbhag SS, Gilmore MS, Chodosh J. The persistent dilemma of microbial keratitis: global burden, diagnosis, and antimicrobial resistance. Surv Ophthalmol. 2019;64(3):255–271. doi: 10.1016/j.survophthal.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dandona R, Dandona L. Corneal blindness in a Southern Indian population: need for health promotion strategies. Br J Ophthalmol. 2003;87(2):133–141. doi: 10.1136/bjo.87.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khor WB, Prajna VN, Garg P, et al. The Asia Cornea Society Infectious Keratitis Study: a prospective multicenter study of infectious keratitis in Asia. Am J Ophthalmol. 2018;195:161–170. doi: 10.1016/j.ajo.2018.07.040. [DOI] [PubMed] [Google Scholar]
- 7.Tran TM, Duong H, Bonnet C, Kashanchi A, Buckshey A, Aldave AJ. Corneal blindness in Asia: a systematic review and meta-analysis to identify challenges and opportunities. Cornea. 2020;39(9):1196–1205. doi: 10.1097/ICO.0000000000002374. [DOI] [PubMed] [Google Scholar]
- 8.Upadhyay MP, Karmacharya PC, Koirala S, et al. The Bhaktapur eye study: ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br J Ophthalmol. 2001;85(4):388–392. doi: 10.1136/bjo.85.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kunimoto DY, Sharma S, Garg P, Gopinathan U, Miller D, Rao GN. Corneal ulceration in the elderly in Hyderabad, South India. Br J Ophthalmol. 2000;84(1):54–59. doi: 10.1136/bjo.84.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prajna NV, Pillai MR, Manimegalai TK, Srinivasan M. Use of traditional eye medicines by corneal ulcer patients presenting to a hospital in South India. Indian J Ophthalmol. 1999;47(1):15–18. [PubMed] [Google Scholar]
- 11.Adekoya BJ, Ayanniyi AA, Adepoju FG, Omolase CO, Owoeye JF. Minimising corneal scarring from the use of harmful traditional eye remedies in developing countries. Nig Q J Hosp Med. 2012;22(2):138–142. [PubMed] [Google Scholar]
- 12.Rao GN. The Barrie Jones Lecture-Eye care for the neglected population: challenges and solutions. Eye. 2015;29(1):30–45. doi: 10.1038/eye.2014.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rathi VM, Murthy SI, Vaddavalli PK, Khanna RC. Feasibility and outcomes of corneal transplantation performed at rural centers: an extension of the pyramidal model of enhanced eye care at rural outreach. Cornea. 2022;41(2):211–218. doi: 10.1097/ICO.0000000000002839. [DOI] [PubMed] [Google Scholar]
- 14.Kammari P, Ambadker MC, Loomba A, et al. A novel technology tool to capture the clinical information of patients across rural vision centers in a three-tier eye care network in India using the eyeSmart EMR App. Rural Remote Health. 2019;19(3):5255. doi: 10.22605/RRH5255. [DOI] [PubMed] [Google Scholar]
- 15.Ting DSJ, Cairns J, Gopal BP, et al. Risk factors, clinical outcomes, and prognostic factors of bacterial keratitis: the Nottingham Infectious Keratitis Study. Front Med. 2021;8 doi: 10.3389/fmed.2021.715118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Srinivasan M. Prevention of traumatic corneal ulcer in South East Asia. Commun Eye Health. 2017;30(99):S15–S17. [PMC free article] [PubMed] [Google Scholar]
- 17.Getshen K, Srinivasan M, Upadhyay MP, Priyadarsini B, Mahalaksmi R, Whitcher JP. Corneal ulceration in South East Asia. I: a model for the prevention of bacterial ulcers at the village level in rural Bhutan. Br J Ophthalmol. 2006;90(3):276–278. doi: 10.1136/bjo.2005.076083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maung N, Thant CC, Srinivasan M, et al. Corneal ulceration in South East Asia. II: a strategy for the prevention of fungal keratitis at the village level in Burma. Br J Ophthalmol. 2006;90(8):968–970. doi: 10.1136/bjo.2006.094706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Srinivasan M, Upadhyay MP, Priyadarsini B, Mahalakshmi R, Whitcher JP. Corneal ulceration in south-east Asia III: prevention of fungal keratitis at the village level in south India using topical antibiotics. Br J Ophthalmol. 2006;90(12):1472–1475. doi: 10.1136/bjo.2006.103028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O'Brien KS, Byanju R, Kandel RP, et al. Village-integrated eye workers for prevention of corneal ulcers in Nepal (VIEW study): a cluster-randomised controlled trial. Lancet Glob Health. 2022;10(4):e501–e509. doi: 10.1016/S2214-109X(21)00596-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Srinivasan M, Ravilla T, Vijayakumar V, et al. Community health workers for prevention of corneal ulcers in South India: a cluster-randomized trial. Am J Ophthalmol. 2022;237:259–266. doi: 10.1016/j.ajo.2021.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Komal S, Radhakrishnan N, Vardhan SA, Prajna NV. Effectiveness of a teleophthalmology vision center in treating corneal disorders and its associated economic benefits. Cornea. 2021;41(6):688–691. doi: 10.1097/ICO.0000000000002784. [DOI] [PubMed] [Google Scholar]
- 23.Sil Ak Do DNBM. “Save your eyes for thirty rupees”: a case study. Commun Eye Health. 2017;30(99):S18–S19. [PMC free article] [PubMed] [Google Scholar]
- 24.Lalitha P, Manoharan G, Karpagam R, et al. Trends in antibiotic resistance in bacterial keratitis isolates from South India. Br J Ophthalmol. 2017;101(2):108–113. doi: 10.1136/bjophthalmol-2016-308487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garg P, Sharma S, Rao GN. Ciprofloxacin-resistant Pseudomonas keratitis. Ophthalmology. 1999;106(7):1319–1323. doi: 10.1016/S0161-6420(99)00717-4. [DOI] [PubMed] [Google Scholar]
- 26.Ting DSJ, Ho CS, Cairns J, et al. 12-year analysis of incidence, microbiological profiles and in vitro antimicrobial susceptibility of infectious keratitis: the Nottingham Infectious Keratitis Study. Br J Ophthalmol. 2021;105(3):328–333. doi: 10.1136/bjophthalmol-2020-316128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.