Abstract
Merkel cell carcinoma (MCC) is a neuroendocrine skin cancer with a higher propensity for recurrence and metastasis than melanoma or squamous cell carcinoma. Despite aggressive behavior and the tripling of its reported incidence in the past 20 years, there is extensive confusion about how MCC should be managed. Here we address two issues that have impeded optimal MCC management: lack of a consensus staging system and lack of unique diagnostic codes for MCC. Five conflicting systems currently used to stage MCC will be replaced by one system in 2010 that will diminish confusion about prognosis and management among physicians and patients. The diagnostic bundling of MCC with numerous less aggressive skin cancers leads to care refusals by insurance and an inability to track MCC care costs. Worldwide adoption in 2009 of specific diagnostic codes for MCC will also improve understanding and management of this often-lethal skin cancer.
Keywords: Merkel cell carcinoma, skin cancer, neuroendocrine
Resumen.
El carcinoma de células de Merkel (CCM) es una neoplasia cutánea neuroendocrina con una mayor propensión para desarrollar recurrencias y metástasis que el melanoma o el carcinoma epidermoide. A pesar de su comportamiento agresivo, y el hecho de que su incidencia se haya triplicado en los últimos 20 años, aún existe una gran confusión respecto al tratamiento del CCM. En esta revisión abordaremos dos cuestiones que han dificultado el tratamiento óptimo del CCM: la carencia de un sistema de estadificación consensuado y la falta de códigos diagnósticos exclusivos para el CCM. Los 5 sistemas contradictorios que actualmente se utilizan para estadificar el CCM serán reemplazados solamente por uno en 2010, lo que disminuirá la confusión sobre el pronóstico y el tratamiento entre los médicos y pacientes. La codificación diagnóstica del CCM, junto con numerosas neoplasias cutáneas menos agresivas, ha condicionado la denegación de atención por parte de las compañías aseguradoras y la incapacidad para evaluar los costes de la atención sanitaria por CCM.
La adopción, que se ha efectuado en 2009, de códigos diagnósticos específicos para el CCM también mejorará la comprensión y el tratamiento de esta neoplasia cutánea frecuentemente letal.
Palabras clave: carcinoma de células de Merkel, cáncer cutáneo, neuroendocrino
Introduction
In looking toward the future of dermatology in this journal’s centennial celebratory issue, here we describe recent progress in Merkel cell carcinoma (MCC), an unusually aggressive skin malignancy. MCC is the second most common cause of non-melanoma skin cancer death with a relative mortality at 5 years of approximately 38 %1 as compared to approximately 15 % for melanoma2. An average melanoma (0.63 mm)3 has < 1 % chance of having spread to lymph nodes at the time of diagnosis4 as compared to 33 % for MCC5. The annual reported incidence of MCC in the United States is currently approximately 1,500 cases6, a figure that has tripled in the past 20 years7. The factors contributing to this increase include: a) improved diagnosis through routine use of cytokeratin-20 staining; b) increased numbers of immunosuppressed patients and c) an increase in the number of older individuals with prior extensive sun exposure.
Risk Factors and Clinical Features
MCC arises predominantly on the sun-exposed skin of older, fair-skinned individuals and is more frequent in men than in women1,8. There is a 10-fold increased risk of MCC among patients receiving immunosuppressive medication for solid organ transplant9, 13.4 fold for patients with HIV10, and 30–50 fold for patients with chronic lymphocytic leukemia11. Despite the increased risk for immune suppressed individuals, approximately 90 % of MCC cases occur in people with no known chronic immune suppression.
MCC typically presents as a rapidly growing, painless lesion that may resemble a cyst11 (fig. 1). The acronym, AEIOU, has been proposed to summarize common clinical features in MCC: a) Asymptomatic/lack of tenderness; b) Expanding rapidly; c) Immune suppression; d) Older than 50 years; e) Ultraviolet-exposed site on a person with fair skin11.
Figure 1.
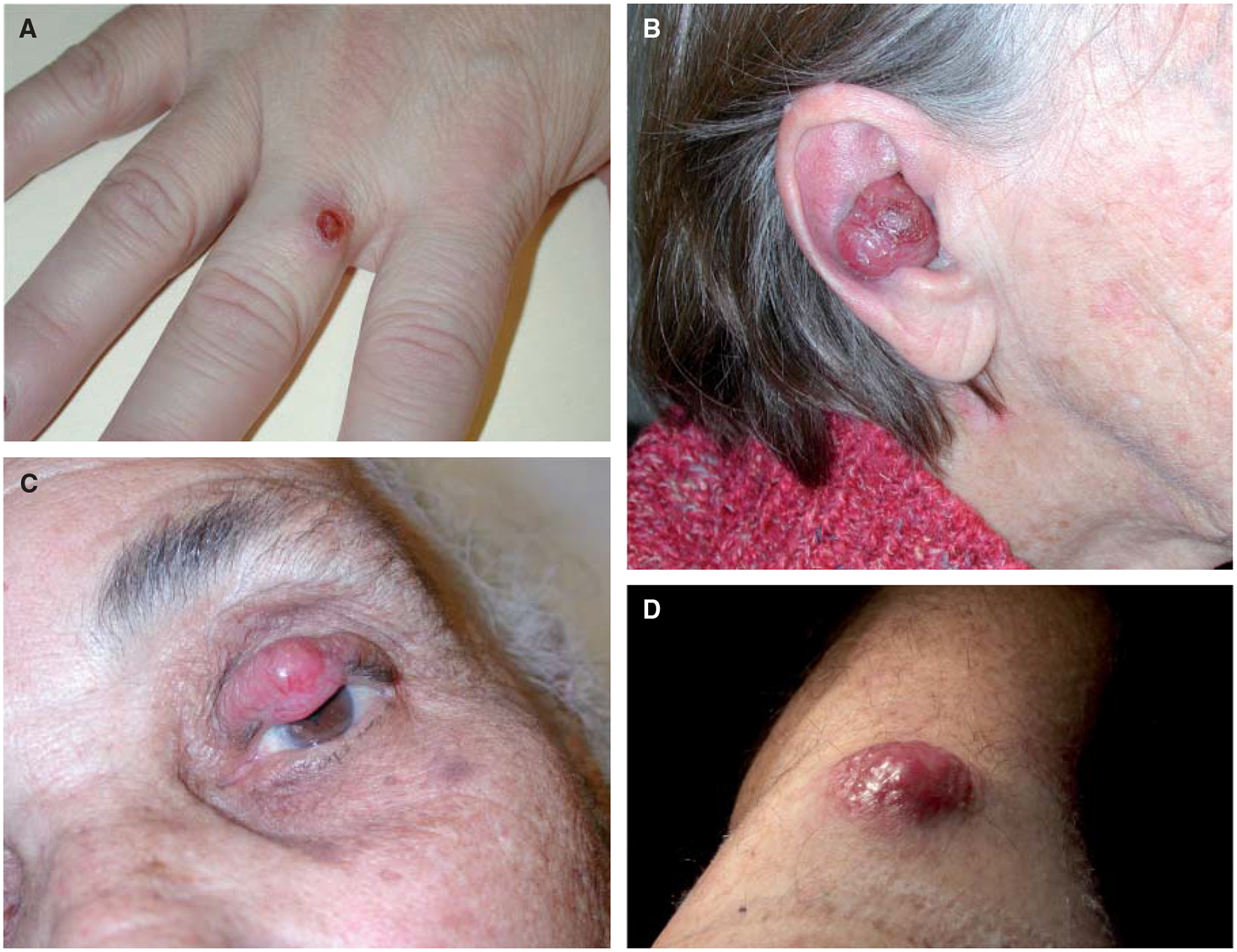
Clinical Presentation of Merkel Cell Carcinoma. Examples of MCC tumors occurring in sun-exposed areas including on the middle finger (A), ear (B), eyelid (C) and upper arm (D). Prior to biopsy, MCC is commonly thought to be a cyst. Although MCC lesions often resemble a rapidly growing red/purple inflamed cyst, the lack of tenderness (88 % MCCs are non-tender), can be an important clue that such a lesion (especially in sun-exposed skin of an elderly or immune suppressed person) should not readily be dismissed as a benign cyst.
The Merkel cell polyomavirus
Because of the increased risk of MCC with immune suppression, a search for an infectious agent yielded a major breakthrough in 2008; the discovery of the Merkel cell polyomavirus (MCPyV)12. Numerous studies have rapidly validated the association of MCC with this virus that is integrated in approximately 80 % of MCC tumors13,14. Subsequent studies have also shown that viral onco-proteins (T antigens) believed to promote cell cycle progression are expressed in a persistent manner in the majority of MCC tumors15. The fact that such non-self viral proteins are expressed in MCC tumors in a majority of cases helps to explain the link between immune function and MCC as well as to suggest a role for immuno-therapeutic approaches in the future.
While the association between MCC and the Merkel cell polyomavirus is now well established, it is also clear that this virus is not required for MCC as approximately 20 % of these tumors contain no detectable MCPyV. Moreover, it is clear that MCPyV is not sufficient for developing MCC as it remains a rare cancer despite the fact that over half of adults have antibodies to MCPyV and hence were exposed to the virus, typically in childhood16,17.
Creating A Common Language for MCC Staging and Prognosis
When facing a new diagnosis of any cancer, the stage at presentation is a key determinant of prognosis as well as of recommended treatment. Currently, any one of five conflicting staging systems may be used for MCC18–22. Each of these systems was based on at most 251 cases derived from three or fewer institutions (table 1). Contradictions between these five systems include:
Three-stage vs. four-stage systems.
Regional nodal disease variably defined as stage II or stage III.
Different tumor size thresholds for determining the Tumor (T) categories for primary lesions. Depending on which system a physician uses to stage a patient, “Stage III MCC” could refer to invasive local-only disease, regional nodal disease, or distant metastatic MCC, all of which have different prognoses and optimal management. Since all five staging systems are still in use, significant confusion exists within the literature and among physicians, patients and researchers. MCC thus lacks a common language to describe prognosis and extent of disease at presentation.
Table 1.
Summary of the Five Existing Staging Systems for MCC
| Study & year | Data | Stage I | Stage II | Stage III | Stage IV |
|---|---|---|---|---|---|
| Yiengpruksawan, et al. 1991 | 70 patients 1 institution | Local | Regional Nodal | Distant Metastatic | – |
| Allen, et al. 1999 | 190 patients 1 institution | IA: Local < 2 cm IB: Local ≥ 2cm |
Regional Nodal | Distant Metastatic | – |
| AJCC* (6th edition) 2002 | No data | Local ≤ 2cm | Local > 2 cm | Local extradermal deep invasion Regional Nodal | Distant Metastatic |
| Allen, et al. 2005 | 251 patients 1 institution | Local < 2cm | Local ≥ 2 cm | Regional Nodal | Distant Metastatic |
| Clark, et al. 2007 | 110 patients 3 institutions | Local ≤ 1cm | IIA: Local ≤ 1 cm & ≤ 2 positive regional lymph nodes IIB: Local ≥ 2cm |
> 2 positive regional lymph nodes | Distant Metastatic |
AJCC: American Joint Committee on Cancer;
Includes MCC with 82 other non-melanoma skin cancers in a chapter titled “Carcinoma of the Skin.”
In the current American Joint Committee on Cancer (AJCC) system, MCC is grouped with 81 other carcinomas of the skin21 including basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). BCC in particular is exceedingly common, kills very few patients and is not required to be reported. Thus the quality and frequency of careful reporting carried out for MCC is compromised because it is currently grouped with numerous skin cancers that require less aggressive management.
A new international consensus staging system for MCC was created using over 5,000 cases from the National Cancer Data Base (NCDB). This system has been adopted for use by both the AJCC and the International Union Against Cancer (UICC) and will aid in standardizing language used to describe MCC and its prognosis.
Overview of the New MCC Staging System
The new staging system is a 4-stage system as summarized in table 2. The most important feature of the new system is the addition of sub-stages for both local and nodal disease. These sub-stages are based on the method of nodal examination for local disease and extent of involvement for nodal disease. The more favorable (‘a’ substage; Ia, IIa) applies if negative node status was determined by microscopic examination of nodes. If only clinical nodal staging was performed (‘b’ substage; Ib, IIb), the chance of missing microscopic nodal involvement is approximately 32 %5. Sentinel lymph node biopsy is an important procedure to determine microscopic involvement of nodes and thus the prognosis as well as need for nodal basin therapy5,20. In Stage III, node-positive patients are segregated into those with only microscopic involvement (IIIa) and those with clinically apparent nodal disease (IIIb). Complete details of the new staging system are described elsewhere23 and the prognostic analysis for its derivation has been submitted24.
Table 2.
Overview of the Consensus Staging System for Merkel cell carcinoma
| Stage I: Local, tumor diameter ≤ 2cm | |
| Ia: | Nodes microscopically negative and not clinically detectable |
| Ib: | Nodes not clinically detectable (no pathologic eval of nodes done) |
| Stage II: Local, tumor diameter > 2cm | |
| IIa: | Nodes microscopically negative and not clinically detectable |
| IIb: | Nodes not clinically detectable (no pathologic eval of nodes done) |
| IIc: | Primary tumor invading bone/muscle/fascia/cartilage |
| Stage III: Regional Nodal Disease | |
| IIIa: | Micrometastasis |
| IIIb: | Macrometastasis (clinically detectable) |
| Stage IV: Distant Metastatic Disease | |
Establishing a New Disease Classification that Separates MCC from BCC and Other Skin Cancers
The International Classification of Diseases (ICD) is widely used for health management and tracking specific diseases throughout the world. ICD-CM (clinical modification) codes are the official system used to categorize diagnoses and medical procedures. This ICD system was previously managed by the World Health Organization and since 1978 has been implemented by the Centers for Disease Control and Prevention (CDC) in the United States.
Until late 2009, MCC was coded in the ICD system as 173.x: “Other malignant neoplasm of skin” along with BCC, SCC and many other skin cancers. This sometimes impedes management of MCC patients as insurance companies use these codes to determine whether or not a test, scan or treatment is appropriate for the diagnosis in question. When a disease does not have a code that appropriately captures its management and treatment, multiple codes must be used to attempt to justify proposed therapies for insurance and billing approvals. This was certainly the case for MCC as it was grouped with BCC and other benign diagnoses that rarely require aggressive management or inpatient care.
To address this issue, a petition was made to the CDC on behalf of the Merkel cell carcinoma Multi-center Interest Group (MMIG) (http://merkelcell.org/MMIG.html) to create specific ICD-CM codes for MCC. The rationale for this petition included the fact that other distinctive skin cancers with potentially aggressive behavior have unique codes. These include cutaneous T cell lymphoma (CTCL) whose incidence is approximately that of MCC25 (code 202.x) as well as malignant melanoma (172.x). In January 2009, the CDC granted 7 MCC-specific codes that became active as of October 1, 2009 (table 3). The introduction of these specific codes will facilitate MCC patients in obtaining insurance approval for the appropriate treatment, help track MCC-associated costs and aid researchers in identifying and following MCC patients.
Table 3.
The New ICD Codes For Merkel Cell Carcinoma
| ICD CODE | |
|---|---|
| 209.31 | Merkel cell carcinoma of the face |
| 209.32 | Merkel cell carcinoma of the scalp and neck |
| 209.33 | Merkel cell carcinoma of the upper limb |
| 209.34 | Merkel cell carcinoma of the lower limb |
| 209.35 | Merkel cell carcinoma of the trunk |
| 209.36 | Merkel cell carcinoma of the other sites |
| 209.75 | Secondary Merkel cell carcinoma* |
| V10.91 | Personal history of malignant neuroendocrine tumor |
Secondary Merkel cell carcinoma here refers to MCC presenting in nodal or visceral sites without a known primary.
Current Management of Merkel Cell Carcinoma
The National Comprehensive Cancer Network (NCCN) publishes multi-disciplinary treatment guidelines for many cancers including Merkel cell carcinoma that are updated annually26. The groups that create and edit these guidelines make use of the best available published data as well as incorporate current standards of practice at over a dozen major cancer care institutions. These guidelines are freely available from the NCCN website and recommendations include surgical management, radiation therapy and chemotherapy (http://www.nccn.org).
Compared with other skin cancers, MCC is an unusually radiation sensitive tumor. Multiple studies have shown that addition of adjuvant radiation is associated with lower rates of local recurrence of MCC as compared with surgical excision alone27. In our experience, it appears that surgical excision alone yields an extremely high rate of local control for some low-risk cases (primary tumor ≤ 1 cm, negative sentinel lymph node biopsy, no chronic immune suppression, no lymphovascular invasion in the primary tumor, confidently negative microscopic margins after excision).
In patients for whom complete surgical excision is not an option, radiation mono-therapy is a reasonable treatment plan28. An 85 year old woman treated with radiation mono-therapy to the left eyelid is shown in figure 1C. The patient had complete resolution of her lesion and is disease-free more than 5 years following her initial diagnosis. Figure 2 shows an 87 year old woman with MCC of the right ear. The patient refused to undergo surgical excision and received radiation mono-therapy. Two years following her treatment, the patient had no MCC recurrence and she died of unrelated causes.
Figure 2.
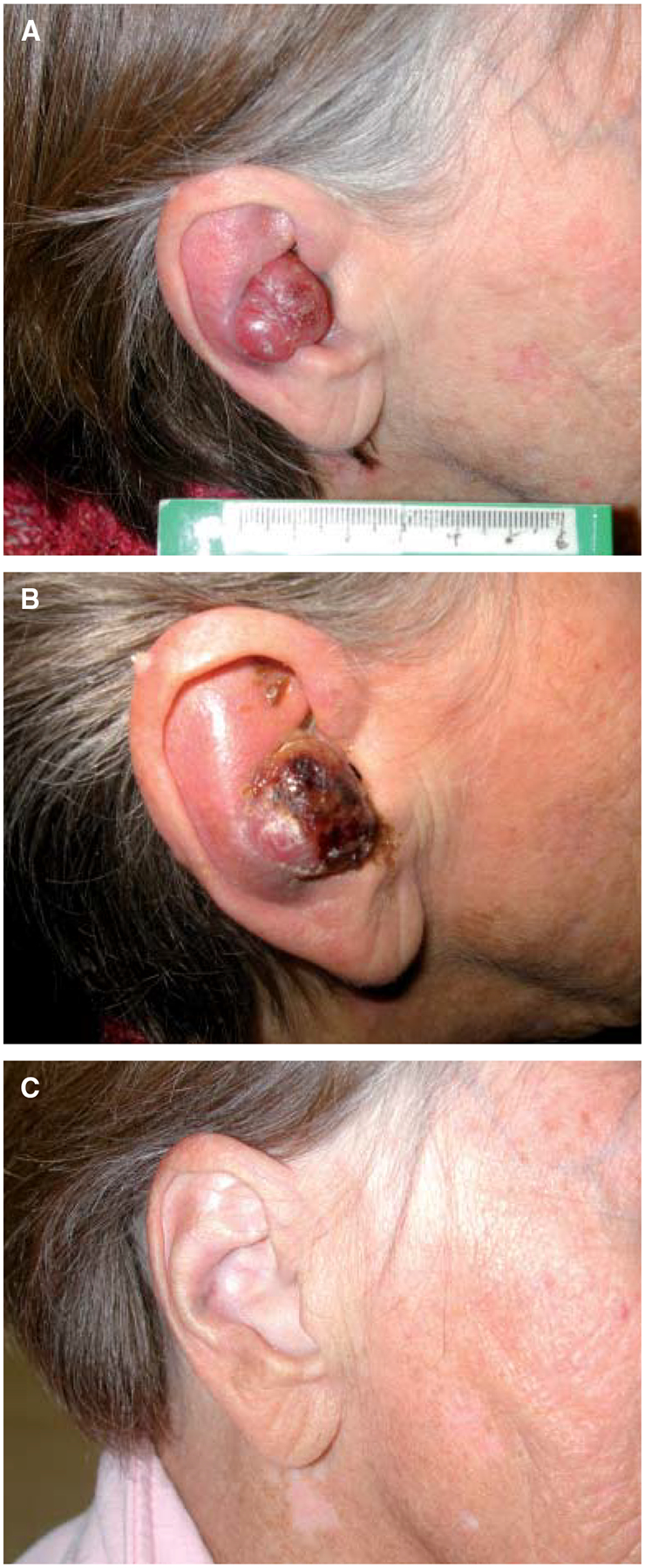
Merkel Cell Carcinoma is a Radiation Sensitive Cancer. A: An 87 year old woman presented with an MCC of the R ear. She refused surgical excision and underwent radiation monotherapy. B: Necrosis of the lesion 3 weeks after beginning radiation therapy. C: Complete resolution of the MCC tumor several months after completing radiation therapy. Approximately 24 months after completing radiation therapy she died of unrelated causes and had no evidence of MCC recurrence.
Controversies in Merkel Cell Carcinoma Management
There are numerous discrepancies in the treatment of MCC between physicians and institutions around the world. Some centers focus almost entirely on surgical excision while others rely on radiation, chemotherapy or combinations. Prospective, high quality, multi-institutional studies are severely lacking for this cancer. Some of the most controversial unanswered questions include:
Which primary MCC tumors would benefit from the inclusion of adjuvant radiation therapy?
What is the optimal surgical or radiation management for microscopic or clinically apparent nodal MCC?
Should adjuvant chemotherapy be included for patients with regional lymph node involvement?
Toward the Future
Having a standardized language to stage and code Merkel cell carcinoma will facilitate future clinical studies for this cancer. In particular, a key goal for this uncommon cancer will be the establishment of multi-institutional, prospective, clinical studies through international collaborations. An initial approach that would yield significant insights would be to follow MCC patients prospectively over a period of time and evaluate the results of treatment in the context of clinical parameters that are carefully collected. Once effective collaborative research alliances are formed in this uncommon cancer, the next goal would be prospective interventional trials of existing and novel therapeutic agents.
Discovery of the Merkel cell polyomavirus (MCPyV) presents many exciting opportunities to better understand and potentially treat this cancer. MCPyV is now known to be present in approximately 80 % of MCC tumors. Certain MCPyV proteins that may be involved in oncogenesis are known to be persistently expressed in most MCC tumors15. Since these viral proteins are foreign antigens, the development of cellular adoptive immune therapy using these proteins as targets is an appealing possibility in treating this often-lethal skin cancer.
Disclosure of any grants or funding of the study:
Supported by American Cancer Society RSG-08-115-01-CCE, ACS-Jerry Wachter MCC Fund to PN, NIH K24-CA139052, David and Rosalind Bloom Endowment to the University of Washington and the UW MCC Patient Gift Fund.
Footnotes
Conflict of interest
Authors have no conflict of interest to declare.
References
- 1.Agelli M, Clegg LX. Epidemiology of primary Merkel cell carcinoma in the United States. J Am Acad Dermatol. 2003;49:832–41. [DOI] [PubMed] [Google Scholar]
- 2.Balch CM, Soong SJ, Gershenwald JE, Thompson JF, Reintgen DS, Cascinelli N, et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. J Clin Oncol. 2001;19:3622–34. [DOI] [PubMed] [Google Scholar]
- 3.Goggins W, Daniels GH, Tsao H. Elevation of thyroid cancer risk among cutaneous melanoma survivors. Int J Cancer. 2006;118:185–8. [DOI] [PubMed] [Google Scholar]
- 4.Lens MB, Dawes M, Newton-Bishop JA, Goodacre T. Tumour thickness as a predictor of occult lymph node metastases in patients with stage I and II melanoma undergoing sentinel lymph node biopsy. Br J Surg. 2002;89:1223–7. [DOI] [PubMed] [Google Scholar]
- 5.Gupta SG, Wang LC, Peñas PF, Gellenthin M, Lee SJ, Nghiem P. Sentinel lymph node biopsy for evaluation and treatment of patients with Merkel cell carcinoma: The Dana-Farber experience and meta-analysis of the literature. Arch Dermatol. 2006;142:685–90. [DOI] [PubMed] [Google Scholar]
- 6.Lemos B, Nghiem P. Merkel cell carcinoma: more deaths but still no pathway to blame. J Invest Dermatol. 2007;127: 2100–3. [DOI] [PubMed] [Google Scholar]
- 7.Hodgson NC. Merkel cell carcinoma: changing incidence trends. J Surg Oncol. 2005;89:1–4. [DOI] [PubMed] [Google Scholar]
- 8.Albores-Saavedra J, Batich K, Chable-Montero F, Sagy N, Schwartz AM, Henson DE. Merkel cell carcinoma demographics, morphology, and survival based on 3,870 cases: a population based study. J Cutan Pathol. 2009. [in press] [DOI] [PubMed] [Google Scholar]
- 9.Penn I, First MR. Merkel’s cell carcinoma in organ recipients: report of 41 cases. Transplantation. 1999;68:1717–21. [DOI] [PubMed] [Google Scholar]
- 10.Engels EA, Frisch M, Goedert JJ, Biggar RJ, Miller RW. Merkel cell carcinoma and HIV infection. Lancet. 2002;359: 497–8. [DOI] [PubMed] [Google Scholar]
- 11.Heath M, Jaimes N, Lemos B, Mostaghimi A, Wang LC, Peñas PF, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008;58:375–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feng H, Shuda M, Chang Y, Moore PS. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008;319:1096–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kassem A, Technau K, Kurz AK, Pantulu D, Löning M, Kayser G, et al. Merkel cell polyomavirus sequences are frequently detected in nonmelanoma skin cancer of immunosuppressed patients. Int J Cancer. 2009;125:356–61. [DOI] [PubMed] [Google Scholar]
- 14.Garneski KM, Warcola AH, Feng Q, Kiviat NB, Leonard JH, Nghiem P. Merkel Cell Polyomavirus Is More Frequently Present in North American than Australian Merkel Cell Carcinoma Tumors. J Invest Dermatol. 2009;129:246–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Busam KJ, Jungbluth AA, Rekthman N, Coit D, Pulitzer M, Bini J, et al. Merkel cell polyomavirus expression in Merkel cell carcinomas and its absence in combined tumors and pulmonary neuroendocrine carcinomas. Am J Surg Pathol. 2009; 33:1378–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tolstov YL, Pastrana DV, Feng H, Becker JC, Jenkins FJ, Moschos S, et al. Human Merkel cell polyomavirus infection II. MCV is a common human infection that can be detected by conformational capsid epitope immunoassays. Int J Cancer. 2009;125:1250–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carter J, Paulson K, Wipf G, Miranda D, Madeleine MM, Johnson LG, et al. Antibodies to Merkel cell polyomavirus are associated with Merkel cell carcinoma. J Natl Cancer Inst. 2009. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yiengpruksawan A, Coit DG, Thaler HT, Urmacher C, Knapper WK. Merkel cell carcinoma. Prognosis and management. Arch Surg. 1991;126:1514–9. [DOI] [PubMed] [Google Scholar]
- 19.Allen PJ, Zhang ZF, Coit DG. Surgical management of Merkel cell carcinoma. Ann Surg. 1999;229:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Allen PJ, Bowne WB, Jaques DP, Brennan MF, Busam K, Coit DG. Merkel cell carcinoma: prognosis and treatment of pa tients from a single institution. J Clin Oncol. 2005;23:2300–9. [DOI] [PubMed] [Google Scholar]
- 21.AJCC Cancer Staging Manual. 6th ed. Chicago: Springer; 2002. [Google Scholar]
- 22.Clark JR, Veness MJ, Gilbert R, O’Brien CJ, Gullane PJ. Merkel cell carcinoma of the head and neck: Is adjuvant radiotherapy necessary? Head Neck. 2007;29:249–57. [DOI] [PubMed] [Google Scholar]
- 23.AJCC Cancer Staging Manual. Merkel Cell Carcinoma. Chapter 30. 7th ed. Chicago: Springer; 2009. [Google Scholar]
- 24.Lemos BD, Storer BE, Iyer JG, Phillips JL, Bichakjian CK, Fang LC, et al. Development of the first American Joint Committee on Cancer Staging System for Merkel cell carcinoma based on prognostic factors analysis of 5,823 National Cancer Data Base cases Submitted.
- 25.Criscione VD, Weinstock MA. Incidence of cutaneous T-cell lymphoma in the United States, 1973–2002. Arch Dermatol. 2007;143:854–9. [DOI] [PubMed] [Google Scholar]
- 26.Miller SJ, Alam M, Andersen J, Berg D, Bichakjian CK, Bowen G, et al. Merkel cell carcinoma. J Natl Compr Canc Netw. 2009;7:322–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewis KG, Weinstock MA, Weaver AL, Otley CC. Adjuvant local irradiation for Merkel cell carcinoma. Arch Dermatol. 2006;142:693–700. [DOI] [PubMed] [Google Scholar]
- 28.Mortier L, Mirabel X, Fournier C, Piette F, Lartigau E. Radiotherapy alone for primary Merkel cell carcinoma. Arch Dermatol. 2003;139:1587–90. [DOI] [PubMed] [Google Scholar]


