This special issue of the Journal of the Indian Institute of Science (IISC) comes at a historic time. IISc, the oldest science institute in India is embarking on a new chapter in its history by starting a hospital, medical school and a public health center1.
In the words of Dr. Govindan Rangarajan, the Director of IISc, the proposed Center for Public Health “will interface between all the departments of the IISc Medical School, and also other science and engineering departments of IISc in the context of public health research. In particular, the Center will create a niche for health data science and analytics through close collaboration with the existing world-class computer science and data science departments at IISc, putting it on par with international counterparts like the Johns Hopkins Bloomberg School of Public Health”. The Centre will also “create world-class post-graduate education and research programmes in public health to redefine healthcare models for India and for the rest of the world. It will offer dual degree programmes such as Master of Public Health (MPH)-PhD (5–6 years) and Master of Public Health (MPH)-MTech Research (3 years)”2.
In this guest editorial, we take the opportunity to do the following:
Highlight the criticality of transdisciplinary research, education and action in public health practice.
Emphasize that public health cannot be separated from complex adaptive systems, social science, politics, economics, systems thinking, leadership and ethics.
Call for greater collaboration and co-production of knowledge and solutions between institutions like the IISc and organizations such as local government agencies, nongovernmental organizations and primary care practices involved in public health practice at the community level. These community practice-academic partnerships, with imagination and mutual support, can be harnessed as robust Practice-Based Research Networks (PBRNs).
Public Health Is Transdisciplinary
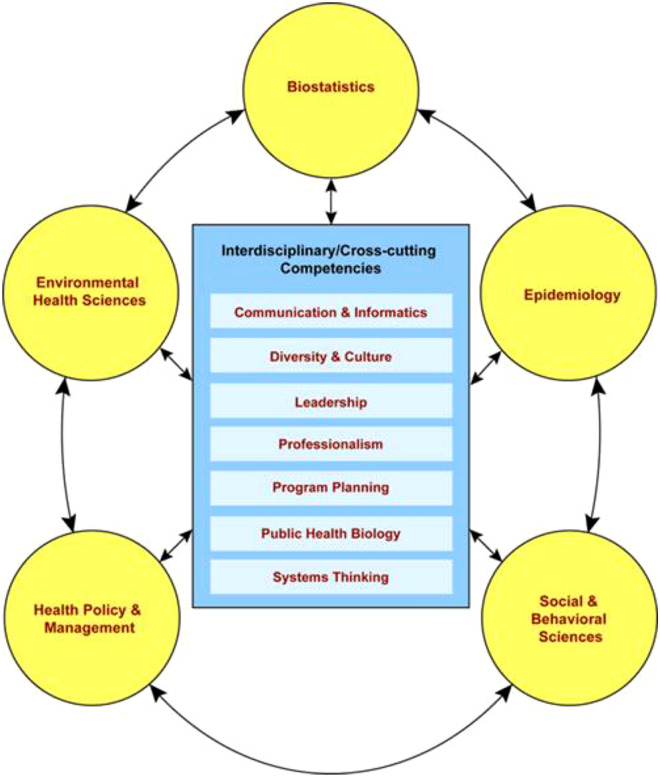
This issue richly represents the various forms of diversity that typify public health. Through the diversity of topics, anchoring institutions and backgrounds of the contributors, not to mention the obvious diversity in perspectives, it demonstrates the central role of trans-disciplinarity and cross-cutting competency domains of public health. Figure 1 shows the main competency domains of public health.
Figure 1:
Competency domains of public health. Reproduced from the Association of the Schools of Public Health3.
For example, just related to COVID-19, Ajmeriya et al.4 have elucidated the role of antibody-dependent enhancement of COVID-19 infection (Public Health Biology) while Kumar et al.5 have highlighted the broad range of animal species and animal cellular models that COVID-19 has been able to infect (Public Health Biology, One Health, Ecology and Environmental Public Health). Sanyal et al.6 have addressed the need to examine environmental drivers of pathogen spillover and the complex biotic and abiotic drivers of zoonoses (One Health, Ecology and Environmental Public Health). Both these groups emphasize the need for application of One Health principles in understanding the zoonotic leap of not only COVID-19 into humans but also other future pathogenic infections.
Keeping with the theme of the effect of the environment on human health, Das et al.7 write concisely about the role of environmental phthalates on human cancer. Their work also signals the need for health policy, management and governance measures (Health Policy and Management).
Chandru et al.8 have brought out the need for reimagining primary care through the application of certain technology levers and as an essential component of public health (Communication and Informatics, Systems Thinking, Leadership). Mukadam et al.9 make the case for the training of clinician-scientists as agents of transformation while drawing upon programs across the globe and within the IISc experience (Professionalism, Leadership and Diversity and Culture). Singaram10 has also written about the need for cross-disciplinarity in public health. Krishnan11 has written an overarching introduction to public health and the various fields and philosophies associated with it (Systems Thinking)11.
Bhat et al12 take us on a historical journey of India’s response to the HIV/AIDS epidemic and highlight the ways by which tools such as mathematical modeling and innovative financing could be used for the control of other epidemics or pandemics (Epidemiology, Social and Behavioral Sciences, Health Policy and Management). Afsharinia and Gurtoo13 have studied the effect of the ecosystem factors of wealth, health and gender in influencing the dietary diversity and adequacy of Indian preschool children and show the critical roles of maternal education and timely access to care (Social and Behavioral Sciences, Health Policy and Management, Program Planning)13.
At a clinical practice level, Prasad and Rao14, in their roles as family physicians, reflect on how the clinical presentation is a result of not just biology and psychology but also a function of his or her social, ecological, economic–political context and the state and design of the health care delivery system (Systems Thinking, Social and Behavioral Sciences).
Public health also involves asking the following types of questions (Table 1):
Table 1:
Critical unresolved questions on Covid-19 in current public health discourse
| Unresolved but pertinent questions in the current public health discourse |
|---|
| How have the various COVID-19 policies worldwide played out, including in China? |
| Does sub-national heterogeneity reveal insights about COVID-19 in specific and public health in general going forward? |
| What are the incentives in public health after the evolution of the private space? |
| How does one resolve the seeming dichotomy of the technical dominance of large corporations with their charitable philanthropy? |
| How did COVID-19 impact inequities in access to health care? |
| What were some notable local examples of capacity building and systems resilience? |
| Does the NHS remain the global cornerstone for the developing world as the health model? |
| How has Ayush played out through COVID-19? |
| What is the real vaccine rollout data in India in terms of efficacy of scale and outcomes? |
| Given that IISc is an engineering, digital and science space, apart from off campus immersions, how does one encourage the biomedical and public health space? |
Transdisciplinary Learning, Collaboration, and Leadership—The Pillars of Public Health
Transdisciplinarity is critical to public health learning and problem solving. As Krishna and Prasad15 point out in their article, “the Indian biomedical landscape has been characterized by the existence of somewhat polarized institutional structures and professional growth. While some scientific and public health challenges have been met with existing structures, there is still a large unmet scientific and public health need. Broadly, the physical separation of science, engineering, medical campuses and industry has led to silos of excellence and accomplishment with huge gaps in innovation and implementation. The lack of interdisciplinary educational options has further reinforced the cultural underpinning of ‘guilds’ that have found it difficult to collaborate. Strikingly, with almost a comparable number of institutions that train doctors in the allopathic or traditional schools such as Ayurveda, Unani, etc., an ‘integrative medicine’ framework has not emerged, apart from an over reliance on specialization at the expense of primary care”.
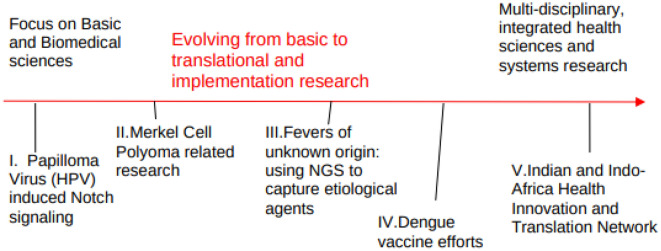
The article describes the transition in work done by Prof Sudhir Krishna’s lab from a basic biomedical research focus in human cervical cancer to an integrative, multi-disciplinary, network with clinicians, public health and policy experts and researchers (Fig. 2), informed by attempts to bridge the gap between Science, Primary Health Care and Public Health, through efforts with Dengue genomics and vaccine design15.
Figure 2:
The evolving transition from Basic science/Biomedical Research focus to a multidisciplinary translational network in the Krishna lab15.
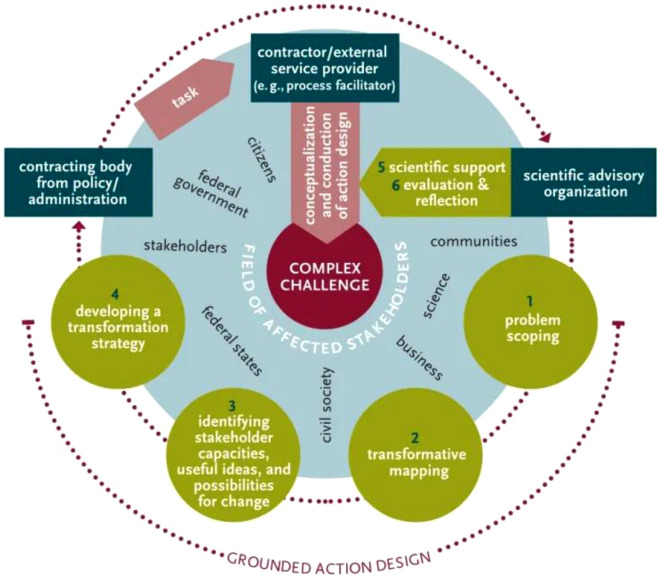
All organizations, including governments, public health agencies and civil society organizations (CSOs), need to approach, capture and frame the complexity of the problem itself as an essential first step. In this regard it is useful to have a framework (Fig. 3), especially a trans-disciplinary framework to facilitate problem framing and problem solving (For further reading, please see Ref.16).
Figure 3:
A transdisciplinary framework for public health problem solving. Source: Bruhns et al. (2019) from Ref.16.
Problem Solving in Public Health Rests on Leadership and Systems Thinking
It is critical to foster leadership among actors in public health. Table 2 shows the core leadership competencies of Public Health.
Table 2:
Leadership competency domains in public health (Source: Adapted from Ref.17).
| Leadership competency | Core domains |
|---|---|
| I. Core transformational competencies |
A. Visionary leadership B. Sense of mission C. Effective change agent |
| II. Political competencies |
A. Political processes B. Negotiation C. Ethics and power D. Marketing and education |
| III. Transorganizational competencies |
A. Understanding of organizational dynamics B. Interorganizational collaboration mechanisms C. Social forecasting and marketing |
| IV Team-building competencies |
A. Develop team-oriented structures and systems B. Facilitate development of teams and work groups C. Serve in facilitation and mediation roles D. Serve as an effective team member |
Successful Public health education also catalyzes a paradigm shift in personal values (Table 3).
Table 3:
Paradigm shifts in personal values for public health professionals and leaders (Source: Adapted from Ref.18).
| Conventional approach | Systems approach |
|---|---|
| Oversimplifying complex and interconnected problems by specialism (or reductionism) | Cultivating a sense of interconnectedness |
|
Focusing only on: Components Facts Quantities Size or scale Efficiency Consumers |
Focusing also on: Relationships Opinions and feelings Qualities Shape and scope Equity Citizens |
|
Celebrating Being a specialist Skills in measurement Being noticed by others |
Celebrating Being a generalist Ability to sense Noticing others |
| Trying to control | Aiming to catalyze |
|
Working “on the system” while “being apart” Marketing Measuring transactions (such as number of visits or number of patient encounters) |
Working “within the system” by “being a part” Building communities Nurturing relationships |
|
Belief in: Competition—to be fine I need to take care of myself Nature is a resource to be exploited by the economy Limited personal agency |
Belief in: Cooperation—when we support each other, we all will live in a better world Nature is the basis of life and we are sustained by it Power of personal leadership |
|
Having more Defending one’s world-view |
Being happy Listening deeply to world-views different from one’s own |
The Way Forward
Educational programs by specialists often tend to primarily focus on transfer of specialist knowledge rather than facilitating reflective learning, transdisciplinarity, collaboration, and enhancing problem solving skills by working in the community.
The goals of public health education should result in a sense of partnership between researchers, innovators, and entrepreneurs anchored at biomedical institutions (such as IISc) and community based practitioners that results in: (a) integration of the richness of context (that community based practitioners have) and the specialist knowledge that academicians might possess; (b) bidirectional learning; and (c) significant focus on problems and solutions that keep citizens and systems at the center of design and innovation.
Including community-based practitioners on institutional boards and academic committees that fosters parity (in terms of power) is another critical step to facilitate co-learning and transdisciplinary problem solving. Community-based organizations will similarly benefit from having scientists anchored at institutions on their organizational boards.
In conclusion, this editorial calls for greater collaboration and co-production of knowledge and solutions between institutions like the IISc and community-based public health practice, often carried out by local government agencies, nongovernmental organizations and family practice/ primary care practices which, with some support, can be harnessed as practice based research networks (PBRNs). Towards this, building an ecosystem that permits cross-pollination and cross-anchoring of ideas, approaches, students, mentors and dedicated investments is critical. Finally, we will have to provide time, training pathways, and funding to transdisciplinary teams and expect genuine cross-pollination, co-incubation, faculty cross-anchoring, co-learning, and co-production of knowledge and solutions. Government and philanthropy has a key role to play in this regard.
Acknowledgements
The authors acknowledge the contributions of Dr. Varsha Shridhar and Mrs. Kranthi Kumari for critical reading of the editorial, thoughtful comments, and insights for improvement.
Biographies
Ramakrishna Prasad
President, Academy of Family Physicians of India (AFPI), Karnataka and Co-founder, PCMH Restore Health & Wellness LLP. He is a practicing Family Medicine physician with expertise in Infectious Diseases and Public Health.
Sudhir Krishna
Distinguished Visiting Professor at the Indian Institute of Technology (IIT), Goa and Former Professor at the National Center for Biological Sciences (NCBS), Bangalore.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.“IISc Receives its Single Largest Private Donation”. From the IISc Office of Communications https://iisc.ac.in/events/indian-institute-of-science-iisc-receives-its-single-largest-private-donation-of-inr-425-crore-to-help-build-an-800-bed-multi-speciality-hospital/. Accessed 20 June 2022
- 2.“IISc Inks MoU with Ajit and Sarah Isaac to Set Up Center for Public Health” From the IISc Office of Communications https://iisc.ac.in/events/indian-institute-of-science-iisc-inks-mou-with-ajit-and-sarah-isaac-to-set-up-centre-for-public-health/. Accessed 20 June 2022
- 3.ASSPH Education Committee (2006) Masters Degree in Public Health Core Competency Development Project v2.3
- 4.Swati A, Amit K, Subhradip K, Shweta R, Harpreet S (2022). Neutralizing antibodies and antibody-dependent enhancement in COVID-19: a perspective. J Ind Int Sci (in press) [DOI] [PMC free article] [PubMed]
- 5.Kumar D, Bayry J, Hegde NR (2022) COVID-19: a veterinary and one health perspective. J Ind Int Sci (in press) [DOI] [PMC free article] [PubMed]
- 6.Sanyal A, Agarwal S, Ramakrishnan U, Kritika MG, Chattopadhyay B (2022) Using environmental sampling to enable zoonotic pandemic preparedness. J Ind Int Sci (in press) [DOI] [PMC free article] [PubMed]
- 7.Das AM, Gogia A, Janardhanan R, Babu-Rajendran R, Bhudev CD (2022) Environmental contamination and chronic exposure to endocrine-disrupting phthalates: an overlooked and emerging determinant for hormone-sensitive cancers. J Ind Int Sci (in press)
- 8.Vijay C, Sharad S, Raghu D (2022) Reimagining India’s health system: technology levers for universal health care. J Ind Int Sci (in press) [DOI] [PMC free article] [PubMed]
- 9.Mukadam FA, Mathew JKK, Nundy M, Perumalla SK, Jhunjhunwala S (2022) Clinician scientists in the Indian context. J Ind Int Sci (in press)
- 10.Singram M (2022) Role of translational research in public health—cross fertilisation of public health and translational research. J Ind Int Sci (in press)
- 11.Krishnan A (2022) A different kind of security: public healthcare in India. J Ind Int Sci (in press) [DOI] [PMC free article] [PubMed]
- 12.Bhat R, Sudhakar K, Kurien T, Rao AS (2022) Strengthening India’s response to the HIV/AIDS epidemic through strategic planning, innovative financing and mathematical modeling: key achievements over the last three decades. J Ind Int Sci (in press) [DOI] [PMC free article] [PubMed]
- 13.Bita A, Anjula G (2022) Wealth, health and gender impact on dietary adequacy: empirical analysis of Indian preschool children. J Ind Int Sci (in press)
- 14.Prasad R, Rao BC (2022) Embracing our larger role: family Physicians as catalysts of social and planetary well-being. J Ind Int Sci (in press)
- 15.Sudhir K, Ramakrishna P (2022). Building Indian biomedical leadership to bridge the gap between science, primary health care, and public health. J Ind Int Sci (in press) [DOI] [PMC free article] [PubMed]
- 16.Framework #9: Grounded action design—transdisciplinary co-creation for better transformative processes. By Thomas Bruhn, Jeremias Herberg, Giulia Molinengo, Daniel Oppold, Dorota Stasiak and Patrizia Nanz. GAIA 28/4: 336. 10.14512/gaia.28.4.3
- 17.Wright K, Rowitz L, Merkle A, et al. Competency development in public health leadership. Am J Public Health. 2000;90(8):1202–1207. doi: 10.2105/AJPH.90.8.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maira A (2019) Transforming systems: why the world needs a new ethical toolkit. Rupa Publications