Abstract
Dual antiplatelet therapy (DAPT) is a management cornerstone for intracranial aneurysms treated with flow diversion. However, combined dual antiplatelet plus anticoagulation (triple therapy) can be indicated in some patients with important associated risks. Here we present the case of a 72-year-old woman with prior history of subarachnoid hemorrhage who was started on triple therapy (enoxaparin and DAPT) following successful flow diversion of an enlarging but unruptured left fetal posterior communicating artery aneurysm. Her post-procedural course was complicated by in-stent thrombosis in the setting of a missed ticagrelor dose and subsequent development of deep venous thrombosis and pulmonary embolism. An early follow-up angiogram confirmed occlusion of the aneurysm. However, after initiation of triple therapy, the aneurysm partially recanalized and her symptoms recurred. Subsequent discontinuation of enoxaparin lead to prompt aneurysm re-occlusion. To our knowledge, this is the first reported instance of confirmed intra-aneurysmal thrombolysis in a successfully treated aneurysm after triple therapy initiation.
Keywords: Anticoagulation, Triple therapy, Flow diversion, Aneurysm recurrence
Introduction
DAPT is standard post treatment management in the setting of flow diversion for intracranial aneurysms. However, a small proportion of patients may require additional anticoagulation treatment for other medical comorbidities. The addition of anticoagulation to DAPT and its effects on aneurysmal thrombus formation are not well known. Consideration should be given to how triple therapy could affect intra-aneurysmal thrombosis, thrombolysis, and subsequent clinical management.
Here we describe our experience with a 72-year-old female who experienced symptomatic in-stent thrombosis after flow diversion with adjunct coiling of a left fetal posterior communicating aneurysm requiring emergent stent recanalization. Her hospital course was complicated by deep venous thrombosis and pulmonary embolism, requiring temporary addition of enoxaparin to DAPT for suspected antiphospholipid syndrome. During triple therapy, non-invasive imaging revealed intra-aneurysmal thrombolysis of her previously thrombosed aneurysm.
Case report
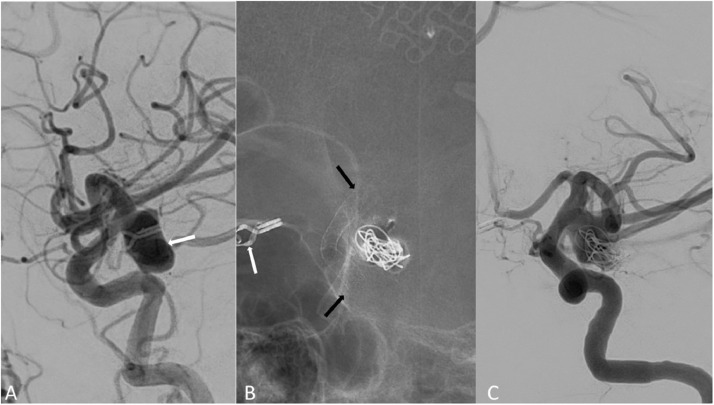
A 72-year-old woman with history of remote prior right anterior choroidal aneurysm rupture status post aneurysm clipping and ventriculoperitoneal shunt placement presented for management of new-onset partial left CN III palsy resulting from an enlarging unruptured 1.4 cm lobulated left fetal posterior communicating artery aneurysm (Fig. 1A).
Fig. 1.
(A) Digital subtraction angiography (DSA) demonstrating a lobulated left lobulated posterior communicating artery aneurysm (white arrow). (B) Subsequent coiling and placement of flow diversion stents with landing zones past the base of the aneurysm (black) arrows. Surgical clip from prior contralateral aneurysm clipping (white arrow). (C) Reduced opacification of the aneurysm dome immediately after flow diversion with adjunct coiling.
Given the patient's history of aneurysm rupture and a newly symptomatic aneurysm, she elected to undergo flow diversion with adjunct coiling. Forty-eight hours prior to her procedure she was placed on dual antiplatelet therapy (DAPT) of aspirin 81 mg daily and ticagrelor 90 mg twice daily. Treatment was performed using two overlapping Surpass Evolve flow diverting stents and Target XL coils (Stryker Inc, Kalamazoo, MI, USA; Fig. 1B, C). The patient left the angiographic suite in her baseline neurologic condition without any immediate complications. She was discharged on post procedure day 1 with instructions to continue DAPT.
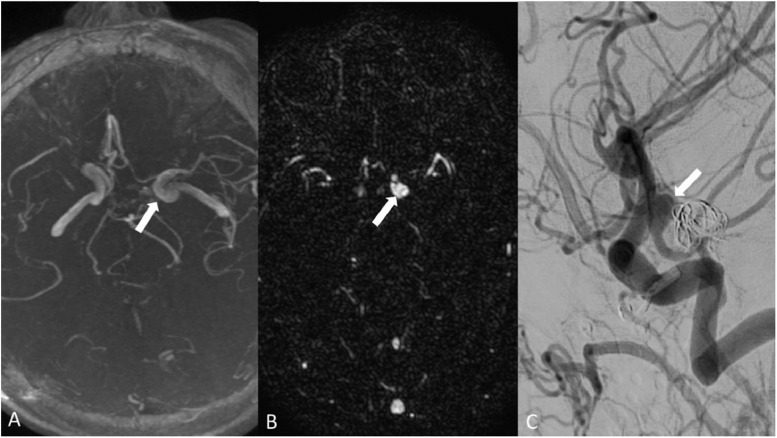
Her clinical course was complicated by symptomatic in-stent thrombosis in the setting of a single missed ticagrelor dose, and she was successfully treated with mechanical thrombectomy to recanalize the occluded stent at an outside hospital complicated by ipsilateral branch retinal artery occlusion. An MRI performed at this time showed complete occlusion of the treated aneurysm (Fig. 2A). Her hospitalization was further complicated by recurrent pulmonary emboli and deep venous thrombosis (DVT) with discovery of an atrial septal defect. The defect was closed and enoxaparin 80 mg twice daily was added to her DAPT for treatment of her pulmonary emboli and DVTs. She was suspected to have antiphospholipid antibody syndrome.
Fig. 2.
(A) MR imaging after thrombectomy for in-stent occlusion demonstrating no opacification of the excluded left posterior communicating artery aneurysm (white arrow). (B) Interval MR imaging 4 months post treatment demonstrating interval partial re-opacification of the aneurysm while patient was on enoxaparin in addition to DAPT (white arrow). (C) DSA 6 months post treatment and 2 months after discontinuation of enoxaparin demonstrating interval re-thrombosis with continued opacification of the aneurysm base (white arrow).
She continued to recover and was seen for follow up in clinic 2 months after treatment. Repeat MR imaging 4 months post initial stent placement demonstrated partial interval recanalization of the previously thrombosed aneurysm (Fig. 2B). Triple therapy was continued for approximately 4 months post initial stenting, until definitive testing for antiphospholipid antibody syndrome returned negative. The patient then continued to take DAPT only. A cerebral angiogram performed 6 months after initial stent placement demonstrated opacification of the aneurysm base with re-occlusion of the aneurysm dome (Fig. 2C). DAPT was then de-escalated to only aspirin 81 mg daily. Another angiogram 8 months post treatment demonstrated additional thrombus formation at the aneurysm base. The previously coiled portion of the aneurysm remained nonopacified.
Discussion
We describe a case of thrombolysis of an established intra-aneurysmal thrombus after flow diversion with adjunct coiling in the setting of triple therapy. Particularly unique to this case is the early imaging confirmation of aneurysm occlusion, followed by short interval MR imaging that confirmed partial aneurysmal recanalization after 3 months of triple therapy.
There are four case reports in the literature describing recurrence of a previously occluded aneurysm following flow diversion. Heit et al. describe a ruptured blister aneurysm that exhibited delayed hemorrhage following pipeline embolization attributed to device migration, and Bohara et al. describe a patient with a large aneurysm treated successfully with telescoping Pipeline devices that upon follow up was noted to recur. In both cases, recanalization was attributed to device migration resulting in uncovering of the aneurysm neck [1,2]. Trivelato et al. describe a case of a 2.1 cm saccular M1 middle cerebral artery aneurysm undergoing coil-assisted flow diversion, which was observed to have recanalized on 9 month follow up angiogram after confirmed complete occlusion on the 6 month angiogram [3]. Zhang et al. report a case of a right intra-cavernous carotid aneurysm undergoing Tubridge flow diversion with coiling and confirmed complete occlusion on 6 month follow up angiogram with recurrent filling of the residual aneurysm neck 2 years after treatment [4]. The case described here is the first in the literature to our knowledge of a short interval aneurysm recurrence attributable to the addition of anticoagulation therapy to the DAPT regimen.
Our findings highlight the need to consider the risk of aneurysm thrombolysis with triple therapy (DAPT plus anticoagulation). Reasons for aneurysm recurrence after treatment are variable. Several factors have been attributed to recurrence including patient age, large size of the aneurysm neck, large aneurysm dome size, degree of occlusion on initial treatment, treatment technique, rupture versus nonrupture status, and presence of a branch vessel arising from the aneurysm [5], [6], [7]. While it is possible that some of these factors could have played a role in recurrence in this case, the addition of enoxaparin to our standard DAPT was highly likely to be the cause given the temporal correlation of aneurysm recanalization following triple therapy administration, and subsequent re-occlusion on angiography after discontinuation of enoxaparin. Intracranial stent placement requires significant platelet inhibition in the early post procedural setting given risks of platelet aggregation at the stent interface prior to long-term endothelialization [8]. There is a paucity of literature regarding the effect of different anticoagulation regimens on rates of aneurysm occlusion following flow diversion with differences in regimens more commonly treated as a confounding variable or limitation of a study [5,6,9,10]. However, there is some evidence that more robust anticoagulation regimens can increase nonocclusion rates without additional clinical benefit. A limited retrospective study comparing patients on additional oral anticoagulants plus DAPT versus DAPT alone prior to flow diverter placement demonstrated that the complete obliteration rate of the excluded aneurysm was significantly lower in the oral anticoagulant group [11], in keeping with our report.
Conclusion
Our case is the first in the literature demonstrating the possibility of thrombolysis of established intra aneurysmal clot after aneurysm flow diversion treatment in the setting of additional anticoagulation to the standard DAPT regimen. This complication may need to be considered in addition to other factors associated with post treatment recurrence when planning follow-up management for patients undergoing flow diversion treatment who also require long-term anticoagulation.
Patient consent
Informed written consent was obtained from the patient for publication of their case.
Footnotes
Competing Interests: None.
References
- 1.Heit JJ, Telischak NA, Do HM, Dodd RL, Steinberg GK, Marks MP. Pipeline embolization device retraction and foreshortening after internal carotid artery blister aneurysm treatment. Interv Neuroradiol. 2017;23:614–619. doi: 10.1177/1591019917722514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bohara M, Teranishi K, Yatomi K, Fujii T, Kitamura T, Yamamoto M, et al. Very delayed discontinuation of telescoped Pipeline embolization devices: a case report. Interv Neuroradiol. 2019;25:182–186. doi: 10.1177/1591019918809932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trivelato FP, Ulhôa AC, Rezende MT, Castro-Afonso LH, Abud DG. Republished: Recurrence of a totally occluded aneurysm after treatment with a pipeline embolization device. J Neurointerv Surg. 2019;11:e5. doi: 10.1136/neurintsurg-2018-013842.rep. –e5. [DOI] [PubMed] [Google Scholar]
- 4.Zhang X, Lv N, Wang C, Cao W, Liu J, Huang Q. Republished: Late recurrence of a completely occluded large intracranial aneurysm treated with a Tubridge flow diverter. J Neurointerv Surg. 2017;9:e6. doi: 10.1136/neurintsurg-2016-012268.rep. –e6. [DOI] [PubMed] [Google Scholar]
- 5.Han Y, Liu J, Tian Z, Lv M, Yang X, Wu Z, et al. Factors affecting recurrence and management of recurrent cerebral aneurysms after initial coiling. Interv Neuroradiol. 2020;26:300–308. doi: 10.1177/1591019919901037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bender MT, Colby GP, Lin LM, Jiang B, Westbroek EM, Xu R, et al. Predictors of cerebral aneurysm persistence and occlusion after flow diversion: a single-institution series of 445 cases with angiographic follow-up. J Neurosurg. 2019;130:259–567. doi: 10.3171/2017.11.JNS171738. [DOI] [PubMed] [Google Scholar]
- 7.Adeeb N, Moore JM, Wirtz M, Giressenaur CJ, Foreman PM, Shallwani H, et al. Predictors of Incomplete Occlusion following Pipeline Embolization of Intracranial Aneurysms: Is It Less Effective in Older Patients? AJNR Am J Neuroradiol. 2017;38:2295–2300. doi: 10.3174/ajnr.A5375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang G, Kim JG, Song KS, Lee YJ, Villavicencio JB, Suroto NS, et al. Delayed ischemic stroke after stent-assisted coil placement in cerebral aneurysm: characteristics and optimal duration of preventative dual antiplatelet therapy. Radiology. 2014;273:194–201. doi: 10.1148/radiol.14140070. [DOI] [PubMed] [Google Scholar]
- 9.Chiu AHY, Cheung AK, Wenderoth JD, De Villiers L, Rice H, Phatouros CC, et al. Long-term follow-up results following elective treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol. 2015;36:1728. doi: 10.3174/ajnr.A4329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kallmes DF, Brinjikji W, Cekirge S, Fiorella D, Hanel RA, Jabbour P, et al. Safety and efficacy of the pipeline embolization device for treatment of intracranial aneurysms: a pooled analysis of 3 large studies. J Neurosurg. 2017;127:775–780. doi: 10.3171/2016.8.JNS16467. [DOI] [PubMed] [Google Scholar]
- 11.Fujii T, Oishi H, Teranishi K, Yatomi K, Suzuki K, Arai H. Outcome of flow diverter placement for intracranial aneurysm with dual antiplatelet therapy and oral anticoagulant therapy. Interv Neuroradiol. 2020;26:532. doi: 10.1177/1591019920947878. [DOI] [PMC free article] [PubMed] [Google Scholar]