Abstract
Retroperitoneal liposarcomas are diagnostic and therapeutic challenge due to their expansive growth and tendency for recurrence. They represent the most of the sarcomas of the retroperitoneal space with the incidence of 41%. Most of them can grow in large proportions before symptom occurrence and change the anatomy of the retroperitoneum. Computerized tomography remains the main diagnostic tool in such cases that provides precise tumor location, size and relation to the adjacent organs. Surgery is the method of choice for treatment. Nevertheless, they tend to recur in 50%-80% of patients despite the appropriate surgery. We present a case of giant retroperitoneal liposarcoma in a female patient with significant left kidney displacement that recurred within 5 years of its removal.
Keywords: Retroperitoneal, Sarcoma, Liposarcoma, Recurrence
Introduction
Retroperitoneal liposarcomas (RL) are malignant tumors arising from the adipose cells in the retroperitoneum. They represent the majority of the retroperitoneal sarcomas (41%) followed by leiomyosarcoma and malignant fibrous histiocytoma with incidence rate of 0.5 per 100,000 of the population [1]. They have the tendency for enormous growth with organ involvement and/or their displacement from the antomic position [2]. RL can occur at any gender and age with the peak incidence in the sixth and seventh decade [3]. Their size at the time of the diagnosis is often large and their weigh can exceed 20 kg. These sarcomas are described as “giant” according to some authors [2,4,5]. We present a case of a 66-year-old female patient presented with giant retroperitoneal low grade liposarcoma with adjacent organ involvement (left ureter and left colon) with left kidney displacement.
Case presentation
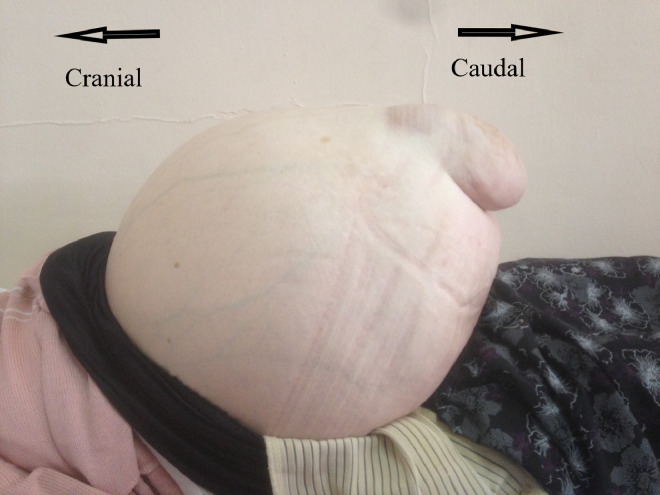
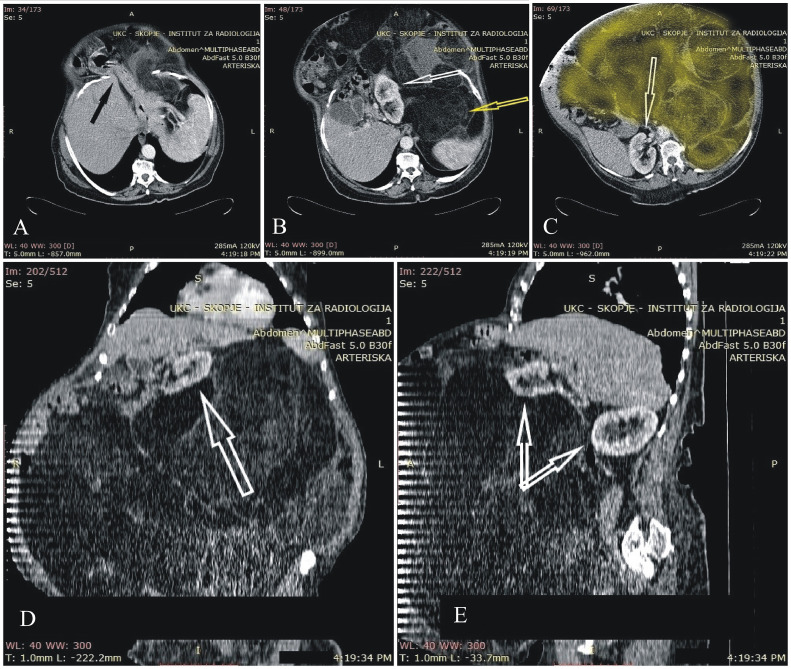
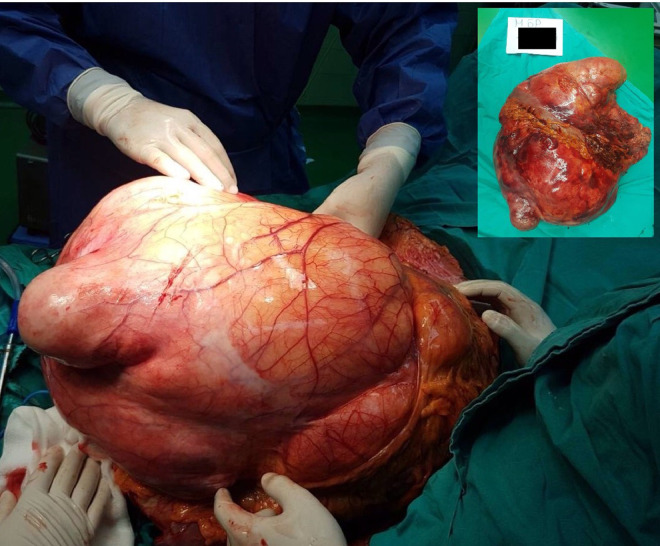
A 66-year-old female patient presented in the outpatient department due to abdominal fullness and persistent ventral hernia that “has grown fast recently”. Previous medical history comprehended hypertension. On physical examination inspection, the abdomen was above the level of the thorax with visual ventral hernia (Fig. 1). Palpation revealed large diffuse abdominal mass without definable boundaries. Abdominal contrast-enhanced computerized tomography (CT) scan was ordered. It confirmed the existence of the ventral hernia with intraabdominal organ herniation and a giant retroperitoneal tumor (possible retroperitoneal sarcoma) with dimensions 42 × 20 cm and abdominal organ displacement (Figs. 2A-E). Tumor removal was offered to the patient. Her preoperative serum biochemistry was within normal ranges with exception of elevated value of C-reactive protein (13 mg/L). Intraoperatively, the tumor infiltrated the left kidney and the descendent colon. All of the involved organs were removed with the tumor “in toto” with partial omentectomy, left nephrectomy and left colectomy (Fig. 3). During surgery an iatrogenic lesion of the right ureter occurred and it was repaired over a ureteral double J stent. The colon was reconstructed with primary anastomosis. Pathology report defined the existence of low grade liposarcoma in the removed tumor mass with total dimensions of 56 × 52 × 20 cm and total weight of 32.9 kg. The sarcoma was described as multilobular and encapsulated. It was composed of yellowish lipomatose neoplasm with cystic components and zones of necrosis. Microscopic analysis defined matured adipose tissue with atypical lipoblasts and rare mitoses. The resected colon showed changes in terms of chronic colitis. The kidney was with hydropic degeneration and low grade of hydronephrosis. The postoperative period was uneventful, and the patient was discharged on postoperative day 8. The ureteral double J stent was removed in urology outpatient setting 3 weeks after the discharge.
Fig. 1.
Clinical presentation of the patient.
Fig. 2.
(A-E) Axial, coronal, and sagittal CT scan of the abdomen. (A) Axial CT scan with herniation of intraabdominal organs through the hernia defect (black arrow). (B) Axial CT scan of the abdomen demonstrates left kidney displacement (white arrow) due to tumor expansive growth (yellow arrow). (C) Axial CT scan of the abdomen showing right kidney (white arrow) and its relation to the tumor (area painted with yellow). (D) Coronal CT scan of the abdomen showing sub hepatic position of the left kidney (white arrow). (E) Sagittal CT scan of the abdomen presenting the “anatomic” relation of the kidneys (white arrows).
Fig. 3.
Intraoperative finding and removed specimen (inset).
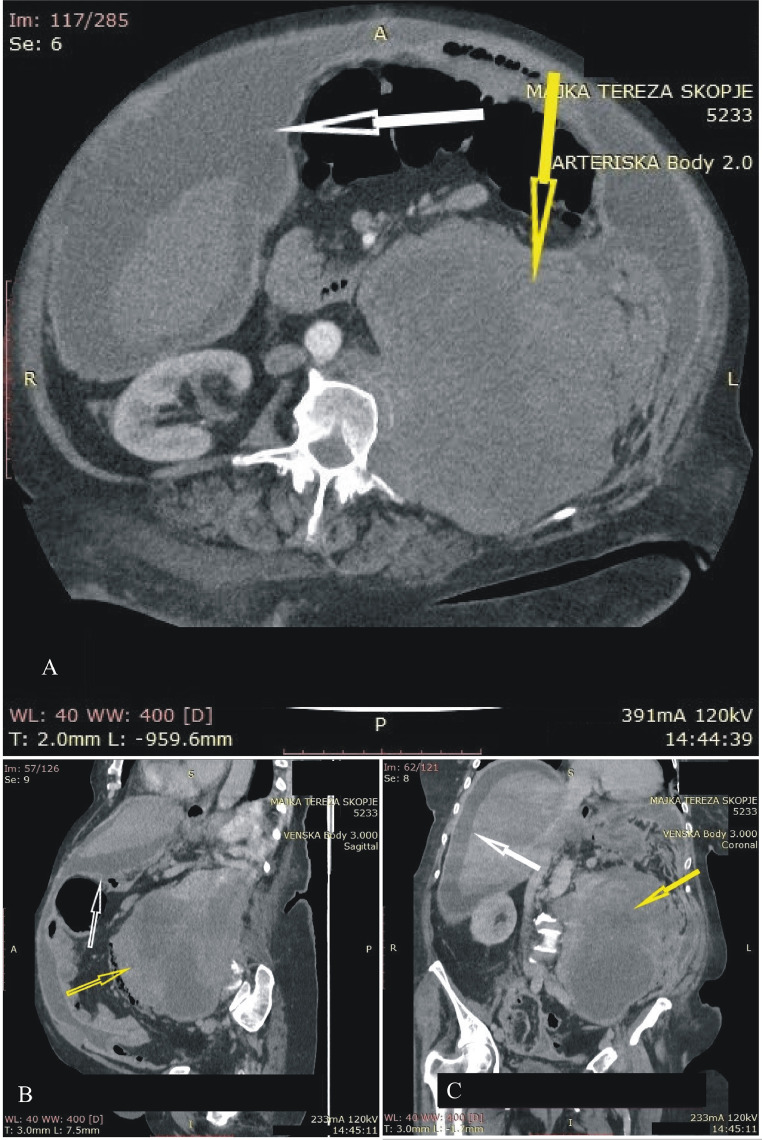
The patient showed only for the skin sutures removal and lived for 5 years. She never visited the surgeon after surgery again. Subsequently, she presented with a tumor recurrence in the emergency department in May 2022 with worsened general condition. CT scan report confirmed tumor recurrence in the left part of the retroperitoneum with dimensions 12.5 × 15.4 × 20 cm and presence of free intraperitoneal fluid (Figs. 4A-C). Due to the poor condition of the patient, emergency surgery was not indicated at this point. Patients’ family refused hospital admission and soon after, the patient died.
Fig. 4.
(A-C) (obtained 5 years after surgery). (A) Axial, (B) sagittal, and (C) coronal CT scan showing liposarcoma recurrence in the retroperitoneum (yellow arrow) and free intraperitoneal fluid (white arrow).
Discussion
RL is rare malignant mesenchymal neoplasm that represents only 0.07%-0.2% of all neoplasia [6]. Yet, it is the most common soft tissue sarcoma with the incidence of newly diagnosed cases of 20% [7]. Five subtypes of liposarcomas are: well-differentiated, myxoid, dedifferentiated, round-cell, and pleomorphic [8].
RL's slow growth remains subclinical due to the large retroperitoneal space. By exceeding large proportions, they finally present with nonspecific symptoms (abdominal pain/fullness, flank pain, early satiety, lower extremity swelling, or pain). Additionally, local tumor invasion and compression effects may cause neurologic, musculoskeletal and obstructive symptoms on the ureters and the bowel [1,3].
The mainstay in the diagnosis of retroperitoneal sarcomas is the CT scan. It gives precise view on the tumor size, location and its relation to the adjacent organs. Organ displacement can also be detected as in our case. Magnetic resonance imaging can be useful in cases of neurovascular and muscular invasion suspicion [1,9]. There are reports of additional diagnostic fine needle aspiration cytology [10].
RL is treated with surgery. The surgeon should always have the intention for performing a negative microscopic margin (R0 resection). Statistically significant difference in median survival between the patients with R0 and positive margin resections have been reported by Lewis [11]. Achievement of microscopically negative margins in such large tumors is challenging. Complete surgical removal can require en-block resection of the affected surrounding organs [12].
Due to the great radio sensitivity of the retroperitoneal liposarcomas, strong suggestions on the addition of adjuvant radiotherapy have been reported in order to reduce the risk for local recurrence. Different radiation delivery methods are described (external beam radiotherapy, intraoperative radiotherapy, intensity-modulated RT, 3-dimensional radiation therapy, helical tomotherapy, respiratory-guided therapy, image-guided radio therapy, proton or heavy ion radio therapy, and stereotactic radio therapy). Yet, the toxic radiologic effects on the surrounding tissue (treatment-related toxicity) to the radio-sensitive viscera are still spreading dose of controversy on its use [1].
Retroperitoneal liposarcomas tend to recur frequently after the initial surgical resection. Approximately between 50% and 80% of the completely resected RL recur within 5 years depending on their differentiation [13]. Due to the late recognition of the recurrence, in many of the patients complete removal of the recurrent tumor is not achieved, thus leading to re-recurrence in about 50% of cases [14]. In our case, the patients also presented with local recurrence within 5 years after the surgery.
In conclusion, precise preoperative diagnosis with CT scan in combination with complete tumor removal remains the diagnostic and treatment strategy for retroperitoneal liposarcomas.
Patient consent
We declare that an informed written consent for publication of the case report article: “Giant retroperitoneal low grade liposarcoma with left kidney displacement: A case report” is obtained from the patient's sibling.
Footnotes
Competing Interests: The authors declare no conflicts of interests.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2022.07.107.
Appendix. Supplementary materials
References
- 1.Vijay A., Ram L. Retroperitoneal liposarcoma: a comprehensive review. Am J Clin Oncol Cancer Clin Trials. 2015;38:213–219. doi: 10.1097/COC.0b013e31829b5667. [DOI] [PubMed] [Google Scholar]
- 2.Oh S.D, Oh S.J, Suh B.J, Shin J.Y, Oh C.K, Park J.K, et al. A giant retroperitoneal liposarcoma encasing the entire left kidney and adherent to adjacent structures: a case report. Case Rep Oncol. 2016;9:368–372. doi: 10.1159/000447488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chouairy C.J., Abdul-Karim F.W., MacLennan G.T. Retroperitoneal liposarcoma. J Urol. 2007;177:1145. doi: 10.1016/j.juro.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Bradley J.C., Caplan R. Giant retroperitoneal sarcoma: a case report and review of the management of retroperitoneal sarcomas. Am Surg. 2002;68:52–56. [PubMed] [Google Scholar]
- 5.Herrera-Gómez Á., Ortega-Gutiérrez C., Betancourt A.M., Luna-Ortiz K. Giant retroperitoneal liposarcoma. World J Surg Oncol. 2008;6:1–6. doi: 10.1186/1477-7819-6-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Echenique-Elizondo M., Amondarain-Arratíbel J.A. Liposarcoma retroperitoneal gigante. Cir Esp. 2005;77:293–295. doi: 10.1016/s0009-739x(05)70857-5. [DOI] [PubMed] [Google Scholar]
- 7.Crago AM, Singer S. Clinical and molecular approaches to well differentiated and dedifferentiated liposarcoma. Curr Opin Oncol. 2011. [DOI] [PMC free article] [PubMed]
- 8.Evans HL. Liposarcoma: a study of 55 cases with a reassessment of its classification. Am J Surg Pathol. 1979;3(6):507–523. doi: 10.1097/00000478-197912000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Munk P.L, Lee M.J., Poon P.Y., Goddard K.J., Knowling M.A., Hassell P.R. Computed tomography of retroperitoneal and mesenteric sarcomas: a pictorial essay. Can Assoc Radiol J. 1996;47:335–341. [PubMed] [Google Scholar]
- 10.Xu C., Ma Z., Zhang H., Yu J., Chen S. Giant retroperitoneal liposarcoma with a maximum diameter of 37 cm: a case report and review of literature. Ann Transl Med. 2020;8:1248. doi: 10.21037/atm-20-1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis J.J., Leung D., Woodruff J.M., Brennan M.F. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg. 1998;228:355–365. doi: 10.1097/00000658-199809000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erzen D., Sencar M., Novak J. Retroperitoneal sarcoma: 25 years of experience with aggressive surgical treatment at the Institute of Oncology, Ljubljana. J Surg Oncol. 2005;91:1–9. doi: 10.1002/jso.20265. [DOI] [PubMed] [Google Scholar]
- 13.Singer S, Corson J.M, Demetri G.D, Healey E.A, Marcus K, Eberlein T.J. Prognostic factors predictive of survival for truncal and retroperitoneal soft-tissue sarcoma. Ann Surg. 1995;221:185–195. doi: 10.1097/00000658-199502000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sogaard A.S, Laurberg J.M, Sorensen M, Sogaard O.S, Wara P, Rasmussen P, et al. Intraabdominal and retroperitoneal soft-tissue sarcomas—outcome of surgical treatment in primary and recurrent tumors. World J Surg Oncol. 2010;8:2–6. doi: 10.1186/1477-7819-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.