Abstract
Background
There have been reports suggesting an increased incidence of acute ischemic stroke among anti-SARS-CoV-2 vaccinees. We aimed to systematically review the literature to summarize the available evidence on the association between SARS-CoV-2 vaccination and acute ischemic stroke.
Methods
A systematic literature search on MEDLINE, LitCovid and LIVIVO databases was performed for eligible randomized controlled trials, observational studies, registries and case reports that reported on imaging-confirmed acute ischemic stroke in the context of any SARS-CoV-2 vaccination with BNT162b2, mRNA-1273, Ad26.COV2.S, ChAdOx1 or Gam-COVID-Vac. Literature search was limited to English and German languages and publication date before October 19, 2021.
Results
We identified a total of 395,105,670 individuals who underwent vaccination. We found 21 sources, including 2 cohort studies, 4 registry studies, 3 randomized clinical trials, and 12 case reports. Individuals included in these studies were at least 16 years old. Cari et al observed a higher likelihood of acute ischemic stroke in vaccinees aged 18–64 years, compared to Whiteley et al observing vaccinees older than 70 years when vaccinated. In addition, differences in the likelihood of acute ischemic stroke were found among the vaccines studied, although no overall increased stroke incidence was demonstrated with vaccination.
Conclusion
In this systematic review of the available literature, we found that the risk of acute ischemic stroke does not appear to be increased in vaccinated individuals who have received any of the currently licensed SARS-CoV-2 vaccines compared with the baseline incidence of stroke.
Keywords: COVID-19, SARS-CoV-2, ischemic stroke, arterial thrombosis, vaccination
Introduction
For more than two years, the world has been facing a pandemic of coronavirus disease 2019 (COVID-19) elicited by the acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1,2 First vaccines against SARS-CoV-2 became available in western countries in December 20203 In January 2021, the messenger RNA (mRNA) vaccine Comirnaty by BioNTech and Pfizer was approved for emergency use by both the European Medicines Agency (EMA) and the Food and Drug Administration (FDA). Further vaccines including ChAdOx1, mRNA-1273, BNT162b2, Ad26.COV2.S were consecutively approved in the following months.
The currently most frequently used vaccines are mRNA (messenger RNA) and vector-based vaccines.4,5 Messenger RNA vaccines are using non-virulent coding SARS-CoV-2 mRNA, coated with lipid particles.6,7 This vaccination induces the synthesis of SARS-CoV-2 proteins through translation of mRNA in the cytoplasm. Detection of those foreign particles leads to an immune reaction with CD8+ and Th1-type CD4+ T-cell responses.7 Vector-based vaccines stimulate a humoral and cellular immune reaction by genetically processed adenoviruses containing SARS-CoV-2-gene sequences.8,9
In general, vaccine-induced immune response commonly triggers harmless side effects including mild fever, fatigue or local dermal reaction in approximately 1% of vaccinees. Serious side effects from vaccines, however, are less commonly seen and correspond to potentially severe health damage that goes beyond the usual extent of a vaccination reaction or vaccination disease.10 In SARS-CoV-2 vaccinees, new-onset autoimmune diseases like Guillain–Barré Syndrome, immune-mediated neuropathy, aseptic meningoencephalitis and myelitis as well as cerebrovascular events like ischemic stroke and cerebral venous thrombosis (CVT) have been increasingly reported.11–15 For instance, the European Medicines Agency (EMA) stated that ChAdOx1 may have caused CVT through the mechanism termed of vaccine-induced thrombotic thrombocytopenia (VITT) in about 25 of 20 million ChAdOx1 recipients.16–18 Vaccine-induced thrombotic thrombocytopenia (VITT) was described in an otherwise healthy young man not been exposed to heparin before.19,20 This prothrombotic condition, which is likely caused by platelet-activating antibodies, can also be triggered by multimolecular complexes between cationic anti-platelet factor 4 (PF-4) and anionic heparin. In recent years, it has been recognized that other triggers may also cause a prothrombotic state that is similar to heparin-induced thrombocytopenia (HIT), eg polyanionic drugs like pentosan polysulfate, the antiangiogenic agent PI-88 and hypersulfated chondroitin sulfate.9,19,21–24 Even more, this prothrombotic state has also been described in the context of viral and bacterial infections.19,25 Furthermore, it is known that vector-based vaccines may be involved in this pathway, as adenoviruses have a strong affinity for PF-4 and could lead to platelet activation.25 Vaccine-induced thrombotic thrombocytopenia may not only be associated with an increased risk of venous thromboembolic events but also with arterial ischemic complications in the cerebral vasculature as reported.26–28 To summarize the current evidence, we systematically searched the literature for studies reporting an association between SARS-CoV-2 vaccination and acute ischemic stroke, which is not necessarily associated with VITT as pathomechanisms other than VITT may also trigger arterial ischemic events in this patient population.
Methods
Data Sources and Search Strategy
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.29 Literature search with language restriction to English and German was performed using MEDLINE (https://pubmed.ncbi.nlm.nih.gov/), LIVIVO (https://www.livivo.de/) and LITCOVID (including MEDLINE and BASE; https://www.ncbi.nlm.nih.gov/research/coronavirus/) to identify relevant studies published between December 1st, 2020, and October 12th, 2021. Used combinations of search strings were “stroke”, “Vaccination”, “Vaccine”, “ChAdOx1”, “AZD1222”, “Vaxzevria”, “Moderna”, “mRNA-1273”, “Spikevax”, “BioNTech/Pfizer”, “BNT162b2”, “Comirnaty”, “Tozinameran”, “Janssen”, “Ad26.COV2.S”, “Gamaleya”, “Gam- COVID-Vac”, “Sputnik V” with the Boolean operators “AND” and “OR.” The reference lists of the identified articles and reviews supplemented the literature search. Titles and abstracts of the identified articles were screened according to eligibility criteria detailed below. Complete search strategy is provided in the “Appendix: Search terms”.
Study Criteria
Implementing the PICOS question, the following eligibility criteria were applied: Population, male or female persons who received any vaccination against SARS-CoV-2 at any age; Intervention, vaccination against SARS-CoV-2, while vaccines were restricted to AstraZeneca: AZD1222 (ChAdOx1, Vaxzevria®), Moderna: mRNA-1273 (Spikevax®), BioNTech/Pfizer: BNT162b2 (Comirnaty®/Tozinameran), Janssen: Ad26.COV2.S and Gamaleya Institute: Gam-COVID-Vac (Sputnik V); Control, not applicable; Outcome, imaging-confirmed acute ischemic stroke; Study type, randomized controlled trial (RCT), observational study, registry or case report.
Study Selection
Literature search was conducted by one reviewer (JR) and complemented by a second reviewer (KB) if search results of the first reviewer were incongruent. Duplicate sources were deleted. Sources were searched based on the title and abstract. In cases of uncertainty, full texts were obtained. No automation tools were used.
Data Extraction
The following data was extracted and entered into an Excel spreadsheet (Microsoft, Redmond, WA): (1) study characteristics (type of the study, number of vaccinees, number of non-vaccinees, observation time), (2) participants’ baseline characteristics (Age, sex), (3) details of vaccination (type of vaccination, number of received dosages), (4) study outcome (incidence of observed acute ischemic stroke under vaccination, baseline incidence of acute ischemic stroke without vaccination, localization of thrombosis, evidence of antibodies to (PF-4), time to event).
Methodological Quality Assessment of Risk of Bias in Included Studies
Studies found eligible were checked according to their completeness of data, inclusion/exclusion criteria, selective reporting and other bias. The Cochrane risk of bias assessment tool was used for randomized controlled trials and the Downs and Black checklist for nonrandomized, observational studies, as recommended by the Cochrane Handbook for Systematic Reviews of Interventions.30
Results
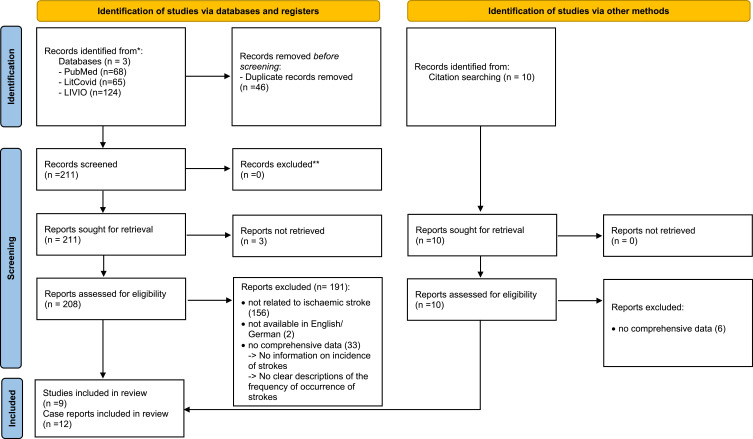
Overall, literature search revealed 257 articles, of which 208 remained for in-depth review following exclusion of duplicates (n = 46) and articles with limited access (n = 3) (Figure 1). Further 191 articles were excluded as these did not fulfill eligibility criteria (not reported on ischemic stroke, n = 156; incomplete data, n = 33; other language than English or German, n = 2). Additional 4 sources were included by searching the reference lists of identified articles. Twenty-one articles fulfilling eligibility criteria were eventually identified and selected for qualitative synthesis (case reports, n = 12; RCT, n = 3; registry, n = 4; cohort study, n = 2). The 12 case reports detailed a total of 16 patients.6,26–28,31–47
Figure 1.
PRISMA flow diagram.
Notes: Adapted from Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71.52
Included vaccines in these articles comprised vector-based vaccines like AZD1222 (ChAdOx1; Vaxzevria®), Ad26.COV2.S (COVID-19 Vaccine Janssen), Gam-COVID-Vac (Sputnik V) and messenger-ribonucleotide-acid (mRNA)-based vaccines like BNT162b2 (Tozinameran, Comirnaty® from BioNTech/Pfizer) and mRNA-1273 (Spikevax® from Moderna). All of the case reports and five of the included studies reported on recipients of the ChAdOx1 vaccine.
Two studies reported on BNT162b2 and ChAdOx1 vaccines, one study each reported singularly on ChAdOx1, BNT162b2, mRNA-1273, Gam-COVID-Vac and Ad26.COV2.S vaccines, and 2 studies included both BNT162b and mRNA-1273 and ChAdoX1 (see Table 1). 6,26–28,31–47 A total of 395,105,670 people underwent vaccination with any of these vaccines and were followed-up between 21 days and 6 months in the selected articles. Persons included were mostly 18 years or older, except in the articles by Polack et al (≥16 years old) and Klein et al (≥12 years old).6,31 A comprehensive summary of the included studies is provided in Table 1.
Table 1.
Clinical and Laboratory Characteristics of the 9 Included Studies in the Systematic Review
| Ref | Study Type | Age | Observation Time | Number of Participants | Control Cohort | Vaccine | Incidence AIS (Vaccination)/ Observed Events | Incidence AIS (Control) Expected Events |
|---|---|---|---|---|---|---|---|---|
| 1 | Cohort | 18–65 | 28 days | 281.264 | Population: Denmark (2016–18) Norway (2018–19) |
ChAdOx-1 | 27 (events) | 28 (events) |
| 2 | RCT | ≥18 | 6 months | 15.210 | N= 15.210/Placebo | mRNA-1273 | 2 (events) | 0 (events) |
| 3 | RCT | ≥16 | 14 weeks | 18.860 | N= 18.846/Placebo | BNT162b2 | 195 (events) | 166 (events) |
| 4.1 | Cohort | ≥18 | 28 days | 8.712.477 | Pre-vaccination or unvaccinated | BNT162b2 | ≤28 days= 670.6 (650.5–691.4) incidence rate per 100,000 p.a., >28days= 977.6 (940.3–1016.4 p.a. | 272.9 (269.8–276.1) incidence rate per 100,000 p.a. |
| 4.2 | ≥18 | 28 days | 12.481.337 | ChAdOx-1 | ≤28 days= 668.2 (648.6–688.4) incidence rate per 100,000 p.a., >28days= 851.2 (827.2–875.9) p.a. | |||
| 5.1 | Register | ≥18 | None | N.A. | No comparison group | BNT162b2 | Severe AEs/1,000,000 doses European mean=4.4 (18–64y), 8.8 (65+y) | - Increase of AIS rate in ChA vs BNT in 18–64 year subjects [fold risk mean (95% CI) p value]= 3.4 (3.1–3.7), p< 0.01 - Increase of AIS rate in ChA vs BNT in >64 year subjects [fold risk mean (95% CI) p value]= 3.3 (3.1–3.6) p< 0.0001 |
| 5.2 | ≥18 | N.A. | No comparison group | ChAdOx-1 | Severe AEs/1,000,000 doses European mean= 15.1 (18–64y), 28.6 (65+y) | |||
| 6.1 | Register | ≥18 | 94 days | 361.734. 967 distribution vaccines, N.R. | No comparison group | BNT162b2 | 561 of 1197 reported cases (46.9%) | N.R. |
| 6.2 | ChAdOx-1 | 219 of 630 reported cases (34.3%) | ||||||
| 6.3 | mRNA-1273 | 173 of 325 reported cases (53.1%) | ||||||
| 7.1 | Register | ≥12 | 6 months + Risk interval (day 0–21/ 22–42 days) |
6.754.348 | − 660.766 person-years of follow-up (risk interval) - 364.988 person-years (comparison interval) |
BNT162b2 | - Events in risk interval=1059 - Events/million person-years= 1611.8 |
Events in risk interval vaccinated vs unvaccinated= 1065 vs 3529 (6 months) |
| 7.2 | 5.090.780 | mRNA-1273 | Events in comparison interval= 650 - Events/million person-years= 1780.9 |
|||||
| 8 | RCT | ≥18 | 180 days | 1.6427 | N= 5.435 (placebo) | Gam-COVID-Vac | Cerebral circulation failure, N=1 (events) | Cerebral circulation failure, N= 0 (absolute values) |
| 9.1 | Register | ≥18 | none | N.R. | BNT162b | ChAdOx-1 | − 18–64y= 8.11 ± 0.75 (7.32–8.90) - >65y= 3.29 ± 0.44 (2.83–3.75) |
N.R. |
| 9.2 | ||||||||
| 9.3 | Ad26.COV2.S | − 18–64y= 8.99 ± 0.67 (8.29–9.70) - >65y= 6.06 ± 1.92 (4.04–8.08) |
Notes: 1= Pottegård et al (doi.org/10.1136/bmj.n1114), 2= Baden et al (DOI: 10.1056/NEJMoa2035389), 3= Polack et al (DOI: 10.1056/NEJMoa2034577), 4= Whitely et al (doi.org/10.1101/2021.08.18.21262222), 5= Cari et al (doi.org/10.1016/j.jaut.2021.102685), 6= Smadja et al (doi.org/10.1183/13,993,003.01111–2021), 7= Klein et al (doi:10.1001/jama.2021.15072), 8= Logunov et al (doi.org/10.1016/S0140-6736(21)00234–8), 9= Cari et al (doi.org/10.1016/j.jaut.2021.102742).
Abbreviations: RCT, N.R, not reported; N.A, not applicable; N, number; AIS, acute ischemic syndrome; chA, ChAdOx-1; BNT, BionTech Pfizer; AE, adverse event; p.a, per annum; Ref, references.
Randomized Controlled Trials
The safety and efficacy of the mRNA-1273 vaccine was investigated in an RCT including 30,420 participants who were randomly assigned to receive either two doses of mRNA-1273 or placebo. During the follow-up period with a median of 2 months embolic strokes were detected in 2 of 15,815 (0.0126%) participants in the mRNA-1273 vaccine group but not in the placebo group.32 Another RCT investigated the BNT162b2 vaccine in 43,548 participants who were randomly assigned to two doses of the vaccine or placebo. A subanalysis comparing placebo (n = 18,846) to BNT162b (n = 18,860) showed no difference regarding the frequency of acute ischemic stroke (195 [1%] vs 166 [0.9%]).6
Only one study was identified in the literature that reported on ischemic stroke in participants who were vaccinated with Gam-COVID-Vac. In this RCT, 21,977 adults were randomly assigned to Gam-COVID-Vac (n = 16,501) or placebo (n = 54,769). During the observational period of 4 months, no ischemic stroke was observed, neither in the vaccination nor in the placebo group.33
Observational Studies and Registries
Pottegård et al used the nationwide healthcare registries of Denmark and Norway to assess the 28-day post-vaccination hospitalization rate for arterial thromboembolic events presumably related to vaccination with ChAdOx1. The populations of Denmark (2016–18) and Norway (2018–19) served as comparator cohorts. According to the baseline incidence, 17 strokes per 100,000 vaccinations were expected during the observation period. In comparison, 16 per 100,000 cases who received vaccination with ChAdOx1 were reported having a stroke during the follow-up period of 28 days.34 The safety profiles concerning major cerebrovascular events of the vaccines ChAdOx1 and BNT162b2 were further explored in a population-based cohort study including 46 million adults in England.35 Of these, 8,712,477 people underwent vaccination with BNT162b2 and 12,481,337 with ChAdOx1. Compared with the annual incidence acute ischemic stroke in the population of England in 2019 (272.9 per 100,000 adults), the overall-age short-term (≤28 days) incidence rates of acute ischemic stroke were higher but did not differ relevantly between both vaccines (ChAdOx1: 668.2 [648.6–688.4] per 100,000 adults vs BNT162b2: 670.6 [650.5–691.4] per 100,000 adults.35 In long-term observation (>28 days), there was a difference in incidence rates favoring BNT162b2 (851.2 [827.2–875.9] per 100,000 adults vs 977.6 [940.3–1016.4] per 100,000 adults. In people <70 years, stroke incidence in both short- and long-term intervals (≤28 days: BNT162b2, 268.2 [251.7–285.1]; ChAdOx1, 318.7 [301.9–336.4]; >28days: BNT162b, 157.9 [142.6–174.9]; ChAdOx1, 387.8 [350.6–429.0] was higher compared to the corresponding annual incidence of acute ischemic stroke in the general population (142.4 [140–144.8]). However, contrary results were found for participants over the age of 70 years in both short and long-term intervals for BNT162b2 and ChAdoX1 vaccines with lower stroke incidences (≤28 days: BNT162b2, 1209.9 [1168.6–1252.6]; ChAdOx1, 1271.6 [1227.1–1317.7]; >28days: BNT162b, 1359.3 [1319.4–1400.4]; ChAdOx1, 1330.4 [1275.5–1387.7] compared to those reported for the general population (1504.7 [1480–1528]). This observation might explain the increased overall incidence of acute ischemic stroke when compared with the general population-based incidence in England. Nevertheless, adjusted within-group analyses did not show an increased short-term risk (≤28 days) of acute ischemic stroke for participants receiving ChAdOx1 when stratified for age (<70 years: adjusted hazard ratio, 0.9; 95% CI: 0.83–0.97; ≥70 years: 0.71; 95% CI: 0.68–07.5). Neither there was an increased stroke risk for the long-term interval following vaccination (<70 years: adjusted hazard ratio, 0.94; 95% CI: 0.84–1.07; ≥70 years: 0.72; 95% CI: 0.67–0.78). Comparable results were seen for the BNT162b2 cohort.35 An analysis of the EudraVigilance registry including data from 21 European countries found an average acute ischemic stroke incidence rate of 4.4 per 1 million administered doses of ChAdOx1 or BNT162b2 in recipients aged 18 to 64 years. Recipients over the age of 64 years showed a nearly two-fold average incidence rate of ischemic stroke following vaccination with BNT162b2 (8.5 per 1 million administered doses) and even 7-fold for ChAdOx1 (28.6 per 1 million administered doses). However, the authors concluded that both underreporting and over reporting of adverse events appeared to be very challenging in analyses of such data.36 In a subsequent investigation, Cari et al compared the vaccines BNT162b2, ChAdOx1 and Ad26.COV2.S regarding their incidence of acute ischemic stroke using BNT162b2 as the reference vaccine. The rate of ischemic stroke after vaccination with BNT162b2 was reported to be 12.2 per 1 million doses administered. For ChAdOx1, the overall rate was 53.8 per 1 million doses and for Ad26.COV2.S, 65.3 per 1 million doses administered. It should be noted that recipients aged 18–64 years had higher odds of suffering from ischemic stroke than recipients over 64 years of age (ChAdOx1: hazard ratio 8.05 ± 0.76, 95% CI: [7.24–8.85] versus hazard ratio 3.26 ± 0.42, 95% CI: [2.83–3.70]; Ad26.COV2.S: hazard ratio 8.91 ± 0.54, 95% CI: [8.34–9.48] versus hazard ratio 6.03 ± 1.96, 95% CI: [3.96–8.09]). Direct comparison of Ad26.COV2.S and ChAdOx1 revealed a potentially increased risk of ischemic stroke in those vaccinated with AD26.2COV.2.37
Furthermore, the vaccines BNT162b2 and mRNA-1273 were compared in a population-based registry investigating comprising 3.6% of the population in the United States. In total, 6,754,348 doses of BNT162b2 and 5,090,780 doses of mRNA-1273 were administered and recipients were followed-up for two consecutive comparative intervals (1 to 21 days after vaccination [risk interval] and 22 to 42 days after their most recent vaccination [comparison interval]) to explore the immediate risk of ischemic stroke following the vaccination. Both vaccines were not individually analyzed. Within the first 21 days, acute ischemic stroke was evident in 1611.8 cases per 1,000,000 person-years and within the second 21 days period in 1780.9 per 1,000,000 person-years. Adjustments made for age, sex, race, ethnicity, health plans and calendar day resulted in a risk ratio of 0.97 (95% CI: 0.87–1.08) of suffering an ischemic stroke during the first 21 days compared with the second 21-days period. This result was found to be non-significant (p = 0.61). The investigators additionally conducted an analysis considering unvaccinated participants as comparator group. Within the first 21 days, acute ischemic stroke was observed in 1065 vaccinated participants and in 3529 unvaccinated participants resulting in an adjusted risk ratio of 0.91 (95% CI: 0.84–0.99; p = 0.02).31
Smadja et al conducted an analysis of the World Health Organization (WHO) Global Database for Individual Case Safety Reports (VigiBase) to assess the thrombotic risk related to SARS-CoV-2 vaccination. In this registry, 361,734,967 participants received the vaccines BNT162b2, mRNA-1273 or ChAdOx1 between December 13th and March 16th, 2021. Of 1197 reported thrombotic events in BNT162b2 vaccinees, 46.9% corresponded to ischemic strokes. In mRNA-1273 vaccinees, 53.1% of 325 reported thrombotic events included ischemic strokes and in ChAdOx1 vaccinees 34.3% of 639 reported thrombotic events. Most strokes in all vaccines occurred within a median of 2 days after vaccination.38
Case Reports
Literature search yielded 12 case reports including 16 patients who suffered from ischemic stroke after vaccination with ChAdOx1.26–28,39–47 There was no case report describing an ischemic stroke in the context of any other SARS-CoV-2 vaccination. Of these 16 patients, 9 (56.3%) were female and the median age was 45.5 years (range 21–69). Ischemic stroke occurred at a median of 8.5 days (range 2–21) after vaccination. All of the patients had large vessel occlusive stroke and two required decompressive hemicraniectomy due to space-occupying brain edema.26,28 In addition to large vessel occlusion, two patients suffered from CVT.28,43 Testing for antibodies to PF-4 was positive in 12 patients. Thirteen patients had platelet counts below 150,000GpT/l and of these 84.6% (11/13) antibodies against PF-4. Outcomes were detailed in 7 out of 16 patients. One patient was declared braindead during hospitalization, and three patients had mild hemiparesis at discharge.27,28,39,46 One patient was described asymptomatic at discharge.45 Included case reports are detailed in Table 2.
Table 2.
Clinical and Laboratory Characteristics of the Case Reports Included in the Systematic Review
| Ref | Age | Sex | Dose (N) | Time (d) | PF | Thrombocytopenia Nadir (GpT/l) | Localization of Thrombosis | PLEX | EVT | IVIG | Steroids | rtPA | Received Anticoagulants | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 31 | m | 1 | 8 | + | >50% decrease | MCA left | - | - | - | - | + | Aspirin + Danaparoid | Phonemic paraphasia and difficulties in complex cognitive tasks (d28) |
| 2 | 60 | f | 1 | 7 | + | 65.000 | Right ICA | - | - | - | + | - | Dalteparin | Death d6 |
| 3 | 55 | m | 1 | 7 | + | 30.000 | Left MCA infarction no evidence of thrombus, superior ophthalmic vein | - | - | - | + | - | Heparin | Left hospital at d26 after admission (Outcome N.R.) |
| 4 | 35 | f | 1 | 6 | + | 64.000 | MCA right | + | - | + | - | - | Fondaparinux | Death (day N.R.) |
| 5 | 37 | f | 1 | 12 | + | 34.000 | Left and right ICA, left transverse sinus thrombosis | + | - | + | + | - | Fondaparinux | N.R. |
| 6 | 43 | m | N.R. | 21 | + | 24.000 | Left MCA | - | - | + | - | - | Fondaparinux | N.R. |
| 7 | 26 | f | 1 | 3 | + | 17.000 | Left MCA | - | + | - | - | - | N.R. | N.R. |
| 8 | 43 | m | 1 | 3 | N.R. | 218.000 | Left MCA infarction no evidence of thrombus | - | - | - | - | - | Antiplatelets | N.R. |
| 9 | 42 | f | 1 | 9 | + | 40.000 | Left ICA | - | - | + | - | - | Argatroban | Discharged on d15 with no neurological deficits |
| 10 | 51 | f | 1 | 7 | + | 54.000 | MCA | - | + | + | - | - | Fondaparinux | Discharge: NIHSS 4, mRS 2 |
| 11 | 39 | f | N.R. | 10 | - | 57.000 | MCA | - | - | - | - | - | N.R. | Alive (not specified) |
| 12 | 21 | m | N.R. | 10 | - | 113.000 | MCA | - | - | - | - | - | N.R. | Alive (not specified) |
| 13 | 57 | f | 1 | 9 | + | 23.000 | Right MCA | + | + | + | + | - | Fondaparinux | N.R. |
| 14 | 55 | f | 1 | 10 | + | 59.000 | Left MCA | - | - | + | + | - | N.R. | Death d1 |
| 15 | 69 | m | N.R. | 12 | + | 106.000 | Right MCA + ICA, right cerebral transverse +sigmoid sinuses, right, internal jugular-, hepatic- and distal lower-limb vein; pulmonary veins | + | - | + | - | - | Fondaparinux | N.R. |
| 16 | 64 | m | 1 | 2 | N.R. | N.R. | Left MCA infarction no evidence of thrombus | - | - | - | - | - | N.R. | Paresis in the right limbs (d7 discharge) |
Notes: 1= Walter et al (doi: 10.1212/WNL.0000000000012576), 2= Blauenfeldt et al (doi: 10.1111/jth.15347), 3= Bayas et al (oi.org/10.1016/S0140-6736(21)00872–2), 4–6= Al-Mayhani et al (doi:10.1136/jnnp-2021-326,984), 7= Constentin et al (doi.org/10.1016/j.jstrokecerebrovasdis.2021.105942), 8= Alammar et al (doi: 10.15537/smj.2021.42.10.20210326), 9= Goereci et al (doi.org/10.1186/s42466-021-00151-y, 10= Kenda et al (doi.org/10.1016/j.jstrokecerebrovasdis.2021.106072), 11, 12= Scully et al (doi: 10.1056/NEJMoa2105385), 13, 14= Michele et al (doi.org/10.1038/s41467-021-25,010-x), 15= Bourguignon et al (doi: 10.1056/NEJMoa2107051), 16= Correa et al (doi.org/10.1016/j.clinimag.2021.08.021).
Abbreviations: sex m, male; f, female; Dose, received doses of vaccine; PF, detected platelet factor 4 antibodies; Time, time from vaccination to onset of symptoms; PLEX, plasmapheresis; EVT, endovascular therapy; IVIG, intravenous immunoglobulins; Steroids, cortisone or their derivate; rtPA, recombinant tissue plasminogen activator; d, days; NIHSS, National Institutes of Health and Stroke Scale; mRS, modified Rankin Scale; N.R, not reported; MCA, middle cerebral artery; ICA, internal carotid artery; +, yes; -, no; GpT/l, giga particles per liter; Ref, references.
Discussion
In this systematic review of the available literature, the risk of acute ischemic stroke did not appear to be increased in vaccinees who received any of the currently approved SARS-CoV-2 vaccines compared to the stroke incidence in different comparator populations. None of the studies identified in this qualitative synthesis of the literature, however, specifically reported on the occurrence of ischemic stroke beyond six months after vaccination. Thus, assuming that similar pathomechanisms as described for heparin-induced thrombocytopenia also contribute to thromboembolic events post SARS-CoV-2 vaccination, such complications are unlikely to occur later than 6 months after index vaccination.43–45 For instance, thrombotic events following ChAdOx1 vaccination were solely observed within 21 days from vaccination. Due to an increased incidence of venous thromboembolic complications observed in ChAdOx1 vaccines, it is not surprising that the identified patient cases in the literature exclusively reported on ischemic stroke after vaccination with ChAdOx1. Interestingly, thrombocytopenia was found in thirteen of these patients and anti-PF-4 antibodies were detected in most of them. Laboratory evidence of antibodies to PF-4 or thrombocytopenia has immediate implications for clinical practice. A recent report showed that ChAdOx1 recipients presenting to the emergency department with severe headache were at imminent risk for development of CVT, if laboratory testing yielded high titers of anti-PF-4 antibodies, thrombocytopenia and high D-dimer levels.48 None of these patients had radiogenic evidence of CVT at the time of presentation. Early initiation of treatment with intravenous immune globulin and therapeutic-dose anticoagulation might be therefore pivotal to prevent incident or recurrent thromboembolic complications in the venous but possibly also in the arterial vasculature.49–51 Although VITT can be considered a very rare cause of stroke, its largely unknown pathomechanism requires further research to tailor preventive measures and specific therapies for patients susceptible to this prothrombotic condition.
Our systematic review has limitations. First, the observational nature of most studies included bears a high risk of confounding, especially introduction of reporting bias. The true results may therefore be skewed towards a lower risk of ischemic stroke. However, when we solely considered randomized controlled trials, risk of ischemic stroke was not accentuated compared to that reported in the included observational studies or registries. Second, most of the studies included reported on the vaccines BNT162b2 and ChAdOx1 leaving a gap in our understanding of the association between ischemic stroke risk and other SARS-CoV-2 vaccines. The fact that BNT162b2 and ChAdOx1 represent two major types of vaccination, mRNA-based and vector-based, allows the assumption that the ischemic stroke risk following vaccination might be eventually balanced among different vaccines though. Third, observational intervals in the included studies were largely different from each other, limiting the comparability of the outcome results. Strengths of our systematic review include the strict adherence to PRISMA guidelines and the standardized approach to address the research question of whether currently approved SARS-CoV-2 vaccines are associated with an increased incidence of ischemic stroke. To our knowledge, this is also the first systematic review of case reports relevant to ChadOx1–associated thromboembolic complications.
Conclusion
Comprehensive review of the current literature did not reveal an increased risk of ischemic stroke in recipients of currently approved SARS-CoV-2 vaccines. Some case reports, however, point to the presence of VITT in ChadOx1-recipients with ischemic stroke. Although very rare, clinicians should be aware of this prothrombotic condition as immediate treatment might be decisive for prevention of thromboembolic complications and unfavorable clinical outcomes.
Funding Statement
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Abbreviations
AE, adverse events; ELISA, Enzyme-linked Immunosorbent Assay; EMA, European Medicines Agency; FDA, The American Food and Drug Association; CI, confidence interval; CVT, cerebral venous thrombosis; CVST, cerebral venous sinus thrombosis; HIT, heparin-induced thrombocytopenia; IVIG, intravenous immunoglobulins; NHS, National Health System; OMD, one million doses; PCR, polymerase-chain reaction; PF-4, platelet factor 4; RR, rate ratio; SAE, severe adverse events; SVT, splanchnic venous thrombosis; VITT, vaccine induced thrombotic thrombocytopenia; WHO, World Health Organization.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr Timo Siepmann and Dr. Kristian Barlinn report Dr Siepmann and Dr. Kristian Barlinn are editorial board member at Neuropsychiatric Disease and Treatment. The authors report no conflicts of interest in this work.
References
- 1.Sun J, He WT, Wang L., et al. COVID-19: epidemiology, evolution, and cross-disciplinary perspectives. Trends Mol Med. 2020;26(5):483–495. doi: 10.1016/j.molmed.2020.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang X, Wu C, Li X, et al. On the origin and continuing evolution of SARS-CoV-2. Natl Sci Rev. 2020;7(6):1012–1023. doi: 10.1093/nsr/nwaa036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.3 Impfstoffe aus China drängen auf weltweiten Einsatz [homepage on the Internet]. Available from: https://www.aerzteblatt.de/nachrichten/120839/3-Impfstoffe-aus-China-draengen-auf-weltweiten-Einsatz. Accessed July 24, 2022.
- 4.COVID 19 tracker [homepage on the internet]. McGill COVID19 Vaccine Tracker Team: COVID-19 Vaccine Tracker. McGill University. Available from: https://covid19.trackvaccines.org/. Accessed July 24, 2022.
- 5.Which Covid-19 Vaccines Are Most Widely Used? [homepage on the internet]. Available from: https://www.statista.com/chart/24191/number-of-countries-using-selected-covid-19-vaccines/. Accessed July 24, 2022.
- 6.Polack FP, Thomas SJ, Kitchin N, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahin U, Muik A, Vogler I, et al. BNT162b2 vaccine induces neutralizing antibodies and poly-specific T cells in humans. Nature. 2021;595(7868):572–577. doi: 10.1038/s41586-021-03653-6 [DOI] [PubMed] [Google Scholar]
- 8.Voysey M, Costa Clemens SA, Madhi SA, et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials. Lancet. 2021;397(10277):881–891. doi: 10.1016/S0140-6736(21)00432-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramasamy MN, Minassian AM, Ewer KJ, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, Phase 2/3 trial. Lancet. 2021;396(10267):1979–1993. doi: 10.1016/S0140-6736(20)32466-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loughlin AM, Marchant CD, Adams W, et al. Causality assessment of adverse events reported to the Vaccine Adverse Event Reporting System (VAERS). Vaccine. 2012;30(50):7253–7259. doi: 10.1016/j.vaccine.2012.09.074 [DOI] [PubMed] [Google Scholar]
- 11.Saito K, Shimizu T, Suzuki-Inoue K, Ishida T, Wada Y. Aseptic meningitis after vaccination of the BNT162b2 mRNA COVID-19 vaccine. Neurol Sci. 2021;42(11):4433–4435. doi: 10.1007/s10072-021-05543-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan AC, Tan BY, Goh Y, Tan SS, Tambyah PA. Aseptic meningitis after BNT-162b2 COVID-19 vaccination. Brain Behav Immun Health. 2022;19:100406. doi: 10.1016/j.bbih.2021.100406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Román GC, Gracia F, Torres A, Palacios A, Gracia K, Harris D. Acute Transverse Myelitis (ATM): clinicalReview of 43 Patients With COVID-19-Associated ATM and 3 Post-Vaccination ATM Serious Adverse Events With the ChAdOx1 nCoV-19 Vaccine (AZD1222). Front Immunol. 2021;12:653786. doi: 10.3389/fimmu.2021.653786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waheed W, Carey ME, Tandan SR, Tandan R. Post COVID-19 vaccine small fiber neuropathy. Muscle Nerve. 2021;64(1):E1–E2. doi: 10.1002/mus.27251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wack S, Patton T, Ferris LK. COVID-19 vaccine safety and efficacy in patients with immune-mediated inflammatory disease: review of available evidence. J Am Acad Dermatol. 2021;85(5):1274–1284. doi: 10.1016/j.jaad.2021.07.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.European Medicines Agency. AstraZeneca’s COVID-19 vaccine: EMA finds possible link to very rare cases of unusual blood clots with low blood platelets. [homepage on the internet]. Available from: https://www.ema.europa.eu/en/news/astrazenecas-covid-19-vaccine-ema-finds-possible-link-very-rare-cases-unusual-blood-clots-low-blood. Accessed July 24, 2022.
- 17.Taquet M, Husain M, Geddes JR, Luciano S, Harrison PJ. Cerebral venous thrombosis and portal vein thrombosis: a retrospective cohort study of 537,913 COVID-19 cases. EClinicalMedicine. 2021;39:101061. doi: 10.1016/j.eclinm.2021.101061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.European Medicines Agency. Available from: https://www.ema.europa.eu/en/news/covid-19-vaccine-astrazeneca-benefits-still-outweigh-risks-despite-possible-link-rare-blood-clots. Accessed July 24, 2022.
- 19.Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N Engl J Med. 2021;384(22):2092–2101. doi: 10.1056/NEJMoa2104840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination. N Engl J Med. 2021;384(22):2124–2130. doi: 10.1056/NEJMoa2104882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tardy-Poncet B, Tardy B, Grelac F, et al. Pentosan polysulfate-induced thrombocytopenia and thrombosis. Am J Hematol. 1994;45(3):252–257. doi: 10.1002/ajh.2830450312 [DOI] [PubMed] [Google Scholar]
- 22.Rosenthal MA, Rischin D, McArthur G, et al. Treatment with the novel anti-angiogenic agent PI-88 is associated with immune-mediated thrombocytopenia. Ann Oncol. 2002;13(5):770–776. doi: 10.1093/annonc/mdf117 [DOI] [PubMed] [Google Scholar]
- 23.Moores G, Warkentin TE, Farooqi MAM, Jevtic SD, Zeller MP, Perera KS. Spontaneous Heparin-Induced Thrombocytopenia Presenting as Cerebral Venous Sinus Thrombosis. Neurol Clin Pract. 2021;11(6):e929–e931. doi: 10.1212/CPJ.0000000000000805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warkentin TE, Makris M, Jay RM, Kelton JG. A spontaneous prothrombotic disorder resembling heparin-induced thrombocytopenia. Am J Med. 2008;121(7):632–636. doi: 10.1016/j.amjmed.2008.03.012 [DOI] [PubMed] [Google Scholar]
- 25.Denard J, Rouillon J, Leger T, et al. AAV-8 and AAV-9 Vectors Cooperate with Serum Proteins Differently Than AAV-1 and AAV-6. Mol Ther Methods Clin Dev. 2018;10:291–302. doi: 10.1016/j.omtm.2018.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blauenfeldt RA, Kristensen SR, Ernstsen SL, Kristensen CCH, Simonsen CZ, Hvas AM. Thrombocytopenia with acute ischemic stroke and bleeding in a patient newly vaccinated with an adenoviral vector-based COVID-19 vaccine. J Thromb Haemost. 2021;19(7):1771–1775. doi: 10.1111/jth.15347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corrêa DG, Cañete LAQ, Dos Santos GAC, de Oliveira RV, Brandão CO. Neurological symptoms and neuroimaging alterations related with COVID-19 vaccine: cause or coincidence? Clin Imaging. 2021;80:348–352. doi: 10.1016/j.clinimag.2021.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Mayhani T, Saber S, Stubbs MJ, et al. Ischaemic stroke as a presenting feature of ChAdOx1 nCoV-19 vaccine-induced immune thrombotic thrombocytopenia. J Neurol Neurosurg Psychiatry. 2021;92(11):1247–1248. doi: 10.1136/jnnp-2021-326984 [DOI] [PubMed] [Google Scholar]
- 29.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). 2022. Available from: www.training.cochrane.org/handbook. Accessed August 23, 2022.
- 31.Klein NP, Lewis N, Goddard K, et al. Surveillance for Adverse Events After COVID-19 mRNA Vaccination. JAMA. 2021;326(14):1390–1399. doi: 10.1001/jama.2021.15072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baden LR, El Sahly HM, Essink B, et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021;384(5):403–416. doi: 10.1056/NEJMoa2035389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Logunov DY, Dolzhikova IV, Zubkova OV, et al. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised Phase 1/2 studies from Russia. Lancet. 2020;396(10255):887–897. doi: 10.1016/S0140-6736(20)31866-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pottegård A, Lund LC, Karlstad Ø, et al. Arterial events, venous thromboembolism, thrombocytopenia, and bleeding after vaccination with Oxford-AstraZeneca ChAdOx1-S in Denmark and Norway: population based cohort study. BMJ. 2021;373:n1114. doi: 10.1136/bmj.n1114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whiteley WN, Ip S, Cooper JA, et al. Association of COVID-19 vaccines ChAdOx1 and BNT162b2 with major venous, arterial, or thrombocytopenic events: a population-based cohort study of 46 million adults in England. PLoS Med. 2022;19(2):e1003926. doi: 10.1371/journal.pmed.1003926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cari L, Fiore P, Naghavi Alhosseini M, Sava G, Nocentini G. Blood clots and bleeding events following BNT162b2 and ChAdOx1 nCoV-19 vaccine: an analysis of European data. J Autoimmun. 2021;122:102685. doi: 10.1016/j.jaut.2021.102685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cari L, Alhosseini MN, Fiore P, et al. Cardiovascular, neurological, and pulmonary events following vaccination with the BNT162b2, ChAdOx1 nCoV-19, and Ad26.COV2.S vaccines: an analysis of European data. J Autoimmun. 2021;125:102742. doi: 10.1016/j.jaut.2021.102742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smadja DM, Yue QY, Chocron R, Sanchez O, Lillo-Le Louet A. Vaccination against COVID-19: insight from arterial and venous thrombosis occurrence using data from VigiBase. Eur Respir J. 2021;58(1):2100956. doi: 10.1183/13993003.00956-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walter U, Fuchs M, Grossmann A, et al. Adenovirus-Vectored COVID-19 Vaccine-Induced Immune Thrombosis of Carotid Artery: a Case Report. Neurology. 2021;10:548. doi: 10.1212/WNL.0000000000012576 [DOI] [PubMed] [Google Scholar]
- 40.Bayas A, Menacher M, Christ M, Behrens L, Rank A, Naumann M. Bilateral superior ophthalmic vein thrombosis, ischaemic stroke, and immune thrombocytopenia after ChAdOx1 nCoV-19 vaccination. Lancet. 2021;397(10285):e11. doi: 10.1016/S0140-6736(21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Costentin G, Ozkul-Wermester O, Triquenot A, et al. Acute Ischemic Stroke Revealing ChAdOx1 nCov-19 Vaccine-Induced Immune Thrombotic Thrombocytopenia: impact on Recanalization Strategy. J Stroke Cerebrovasc Dis. 2021;30(9):105942. doi: 10.1016/j.jstrokecerebrovasdis.2021.105942 [DOI] [PubMed] [Google Scholar]
- 42.Alammar MA. Ischemic stroke after AstraZeneca (Covid-19) vaccination. Saudi Med J. 2021;42(10):1136–1139. doi: 10.15537/smj.2021.42.10.20210326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bourguignon A, Arnold DM, Warkentin TE, et al. Adjunct Immune Globulin for Vaccine-Induced Immune Thrombotic Thrombocytopenia. N Engl J Med. 2021;385(8):720–728. doi: 10.1056/NEJMoa2107051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scully M, Singh D, Lown R, et al. Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 nCoV-19. New England Journal of Medicine. 2021;384(23):2202–2211. doi: 10.1056/NEJMoa2105385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goereci Y, Kleineberg NN, Madlener M, et al. Successful treatment of thromboses of major arteries after ChAdOx1 nCov-19 vaccination. Neurol Res Pract. 2021;3(1):52. doi: 10.1186/s42466-021-00151-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kenda J, Lovrič D, Škerget M, Milivojević N. Treatment of ChAdOx1 nCoV-19 Vaccine-Induced Immune Thrombotic Thrombocytopenia Related Acute Ischemic Stroke. J Stroke Cerebrovasc Dis. 2021;30(11):106072. doi: 10.1016/j.jstrokecerebrovasdis.2021.106072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.De Michele M, Iacobucci M, Chistolini A. Malignant cerebral infarction after ChAdOx1 nCov-19 vaccination: a catastrophic variant of vaccine-induced immune thrombotic thrombocytopenia. Nat Commun. 2021;12(1):4663. doi: 10.1038/s41467-021-25010-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Salih F, Schönborn L, Kohler S, et al. Vaccine-Induced Thrombocytopenia with Severe Headache. N Engl J Med. 2021;385(22):2103–2105. doi: 10.1056/NEJMc2112974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Warkentin TE, Bernstein RA. Delayed-onset heparin-induced thrombocytopenia and cerebral thrombosis after a single administration of unfractionated heparin. N Engl J Med. 2003;348(11):1067–1069. doi: 10.1056/NEJM200303133481120 [DOI] [PubMed] [Google Scholar]
- 50.Warkentin TE, Kelton JG. Temporal aspects of heparin-induced thrombocytopenia. N Engl J Med. 2001;344(17):1286–1292. doi: 10.1056/NEJM200104263441704 [DOI] [PubMed] [Google Scholar]
- 51.Rice L, Attisha WK, Drexler A, Francis JL. Delayed-onset heparin-induced thrombocytopenia. Ann Intern Med. 2002;136(3):210–215. doi: 10.7326/0003-4819-136-3-200202050-00009 [DOI] [PubMed] [Google Scholar]
- 52.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]