Abstract
Background
Since the beginning of the pandemic, scientists and researchers are highly engaged in the discovery and production of vaccines and specific treatments for COVID-19. In China, the National Health Commission has declared the use of herbal medicine combined with Western medicine as a treatment for COVID-19 and has issued many guidelines on herbal medicine-related therapies. Ethiopians have a variety of medicinal herbs to treat various viral diseases. Hence, this study aimed to assess the perception of the respondent towards COVID-19 related symptoms and traditional medicine practice for their management.
Methods
A hospital-based cross-sectional study was done among 423 patients and patient attendants at the University of Gondar Comprehensive Specialized Hospital from August 6 to 27, 2021. Data were collected using a structured questionnaire, and the data were entered into Epi Info 7 and then analyzed with SPSS 20. The association between the independent and dependent variables was explained using chi-square test.
Results
A total of 423 respondents participated in the study; 414 (97.9%) participants heard about COVID-19 and responded correctly to the chief clinical symptoms. Fever is the most perceived symptom, reported by 378 (91.3) respondents, and the least reported symptom was loss of taste and smell by 30 (7.2%) respondents. This study showed that home remedies were practiced by 323 of the total respondents, and herbal medicines were the second most and practiced by 316 respondents. Monthly income and perceived knowledge about chief symptoms were statistically significantly associated (p < 0.05) with the use of complementary and alternative medicine for the management of COVID-19 related symptoms.
Conclusion
This study found that most of the respondents have knowledge about the signs and symptoms of COVID-19 and the traditional medicine is being practiced by most of the study participants as a management for COVID-19 and related symptoms.
Keywords: COVID-19, complementary and alternative medicine, Ethiopia
Introduction
In December 2019, a pneumonia associated with the COVID-19 emerged in Wuhan, Hubei Province, China.1 It is an infectious disease caused by SARS-CoV-2 virus, which is a serious infection of the respiratory tract which affects both the upper respiratory tract including throat, nose and sinuses, lower respiratory tract and lungs of an infected person.2 Among the infected patients, COVID-19 shows various unspecific symptoms, ranging from mild to severe. Fever (98%) is the most frequent symptom which is followed by cough (76%), myalgia or fatigue (44%), sputum production (28%), and headache (8%).3 Since the beginning of the pandemic, scientists and researchers are highly engaged in the discovery and production of vaccines and specific treatments for the COVID-19 disease.4 Due to the nature of the pandemic, different countries and regulatory organizations realized that they need to remove stringent patent rules on vaccines and medications for the treatment of this virus.5
Despite the fact that there are vaccines available for COVID-19 by different manufacturing industries, people in the community and researchers are making an ongoing trial to find the best way to cure the disease, including natural herbal remedies.6 In China, the National Health Commission has approved the use of herbal medicine combined with modern medicine as a treatment for COVID-19, and has developed many guidelines on herbal medicine-related therapy.7 In African countries such as Mali, Ghana, Zambia, and Nigeria, the first line of treatment for 60% of children with high fever resulting from malaria is the use of herbal medicines at home.8 Ethiopia has a long history of traditional medicine practice with about 80% of the population depending on traditional medicinal practices to safeguard their lives from various diseases.9 From the medicinal herbs available in Ethiopia;10,11 Allium cepa, Allium sativum, Nigella sativum, Brassica juncea, Zingiber officinale, Curcuma longa and Capsicum annum are mentioned in different literature for their antiviral activities (Table 1). Inspired by previous experiences, herbal remedies are being considered as one of the alternative approaches in the treatment of COVID-19.12 This study aimed to assess the perception of respondents towards Covid-19 related symptoms and traditional medicines used for their management of its symptoms by patients/attendants during the pandemic period.
Table 1.
List of Medicinal Plants Which Have Previous Antiviral Activities, 2021
| Scientific Name | Local Name | Previous Antiviral Activity | Ref No |
|---|---|---|---|
| Eucalyptus globulus labill. | Nech bahirzaf | Common cold | [37] |
| Nigella sativa | Tikur azmud | Common cold | |
| Zingiber officinale roscoe. | Zinjibile | Influenza | |
| Ruta chalepensis L. | Tena adam | Influenza | |
| Lepidium sativum | Fetto | Cough | [38] |
| Allium sativum | Nechshinkurt | Influenza virus | |
| Citrus aurantifolia | Lomi | Common cold | |
| Moringa oleifera | Moringa | Common cold | [39] |
| Zehneria scabra | Haregresa | Rabies | |
| Ocimum lamiifolium hochst | Damakese | Common cold | |
| Echinops kebericho | Kebericho | Cough | [38] |
| Otostegia integrifolia | Tinjut | Common cold |
Methods and Materials
Study Area and Periods
The study was conducted at the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. It is located in Central Gondar Zone, Amhara regional state of Ethiopia, and is 748 km far northwest of Addis Ababa, the capital of Ethiopia, and about 180 km from Bahir Dar city, the capital of Amhara regional state. The University of Gondar Comprehensive Specialized Hospital (UOGCSH) is a teaching hospital which serves more than five million people. It gives referral and specialized diagnostic and treatment services for clients. The UOGCSH was given quarantine of the suspected cases, treatment, and follow-up of COVID-19 patients by providing more than 320 beds.13 The study was conducted from August 6 to 27, 2021.
Study Design and Population
A hospital-based cross-sectional study design was conducted. All patients who visited the UOGCSH were the source population, whereas among the visitors, those who attended the UOGCSH during our study period were the study population. The visitors were selected from the emergency, inpatient, and outpatient wards.
Inclusion and Exclusion Criteria
All Adults (>18 years old) who attended the UOGCSH during the study period were included in the study, while visitors who were severely ill, psychiatric participants, and health professionals were excluded from the study.
Sample Size Determination and Sampling Procedure
The sample size was determined using the single population proportion formula by taking the following assumptions.
Confidence level (Cl), 95% Proportion = 50%, Margin of error 5%
Using the following single proportion formula:
 |
n=initial sample size, Z = 1.96, the corresponding Z-score for the 95% CI, P = Proportion = 50%, W = Margin of error = 5% = 0.05
 |
The sample size became 384, and after considering a 10% nonresponse rate, the adequate sample final sample size was 423. A nonprobability consecutive sampling method was employed to interview the study participants.
Study Variable
Traditional medicine utilization was a dependent variable, whereas socio-demographic related variables including sex, age, educational level, average monthly income, and visitor’s perceived knowledge about chief clinical symptoms were the independent variables.
Data Collection Procedure and Data Quality Assurance
Data were collected using a structured and pretested questionnaire. The questionnaire was pretested on 21 (5%) nonparticipant respondents, having similar characteristics to the study subjects, to identify the potential problems of the questionnaire, unanticipated interpretations, and cultural objections to any of the questions. Considering those respondents who cannot write and read, the questionnaire was read out to them by data collectors. The questionnaire incorporates socio-demographic characteristics, knowledge about COVID-19 symptoms, symptoms experienced by the respondents, and the type of traditional medicine used. The data were collected by four graduating class pharmacy students. The questionnaire was prepared in English and translated into Amharic and then back to English to maintain consistency.
Statistical Analysis
Completeness and consistency of the data was checked on a spot and daily basis by the supervisors and data collectors. The data were entered, cleaned, and coded using Epi info software version 7.2.4 and exported to Statistical Packages for Social Sciences (SPSS) version 20.0 Software for analysis. Descriptive statistics was used to summarize the frequency of study participant background characteristics. The association between the independent and dependent variables was explained using chi-square test. P-values were used to measure how likely is the association between variables and a variable with a p-value ≤0.05 with 95% confidence interval was considered significantly associated with the study outcome variable.
Ethical Consideration
The Helsinki Declaration’s ethical guidelines were followed throughout the study’s conduct. Ethical clearance was obtained from the Ethical Committee of School of Pharmacy, College of Medicine and Health Sciences, University of Gondar (No. SOP/272/2021). Before the data collection, the purpose of the study was explained, and written informed consent was obtained from the study participants. Individuals who were volunteers to participate in the study were also told as they have the right to withdraw from the study at any stage of the interview. The confidentiality of the study participants was ensured by avoiding possible identifiers. Furthermore, appropriate infection prevention practices and principles related to COVID-19 were considered during the data collection period. Data collectors provided health education for the respondents after the interview had been completed based on the gaps identified as appropriate.
Results
Socio-Demographic Characteristics
A total of 423 patients and attendants agreed to participate in the interview with a response rate of 100%. From the total respondents, around half (52%) were females, and more than half (61%) were in the age group between 18 and 34 years. Around three-fourths, 316 (74.7%) of the respondents were Orthodox Christian religion followers (Table 2).
Table 2.
Socio-Demographic Characteristics of Respondents, UOGCSH, Northwest Ethiopia, 2021 (N = 423)
| Variable | Frequency (%) | |
|---|---|---|
| Gender | Female | 220 (52) |
| Male | 203 (48) | |
| Age | 18–34 | 258 (61) |
| 35–49 | 112 (26.5) | |
| 50–65 | 50 (11.8) | |
| Above 65 | 3 (0.7) | |
| Religion | Orthodox | 316 (74.7) |
| Muslim | 47 (11.1) | |
| Protestant | 60 (14.2) | |
| Educational status | Basic education | 15 (3.5) |
| College diploma | 85 (20.1) | |
| First degree and above | 166 (39.2) | |
| Primary school | 25 (5.9) | |
| Secondary school | 81 (19.1) | |
| Illiterate | 44 (10.4) | |
| Religious education | 7 (1.7) | |
| Monthly income | 1651–3200 | 69 (16.3) |
| 3201–5250 | 54 (12.8) | |
| 5251–7800 | 38 (9) | |
| 7801–10,900 | 36 (8.5) | |
| 10,901 and above | 17 (4) | |
| No salary | 43 (10.2) | |
| Unknown income | 166 (39.2) |
COVID-19 Related Perceptions of the Study Participants
In our study, 414 (97.9%) participants responded that they heard about the signs and symptoms of COVID-19. Fever is the most perceived symptom and reported by 378 (91.3) respondents, and the least reported was loss of taste and smell by 30 (7.2%) respondents. Television was reported by 300 (72.5%) participants as a source of information. From 423 participants, 147 (35.5%) were experienced chief complaints of the virus. Among all participants, 90 (21.3%) were tested for COVID-19 and 81 (90%) of them were found to be positive (Table 3).
Table 3.
COVID-19-Related Perceptions Among Respondents About the Management of Signs and Symptoms of COVID-19, Northwest Ethiopia, 2021 (n = 423)
| Variables | Categories | Frequency (%) |
|---|---|---|
| Do you know the symptoms of COVID-19? | Yes | 414 (97.9) |
| No | 9 (2.1) | |
| If yes, what symptoms of COVID-19 do you know (n = 414) | Cough | 371 (89.6) |
| Shortness of breath | 218 (52.7) | |
| Fever | 378 (91.3) | |
| Sore throat | 79 (19.1) | |
| Muscle ache | 78 (18.8) | |
| Headache | 133 (32.1) | |
| Loss of smell or test | 30 (7.2) | |
| Nausea and vomiting | 52 (12.6) | |
| What is your usual source of information about COVID-19? (n = 414) | Radio | 120 (29) |
| Television | 300 (72.5) | |
| Social media | 171 (41.3) | |
| People (from relatives) | 19 (4.5) | |
| Have you ever experienced symptoms of COVID-19 | Yes | 147 (35.5) |
| No | 267 (64.5) | |
| If yes, what symptoms of COVID-19 did you experienced? (n = 147) | Nausea and vomiting | 15 (10.2) |
| Sore-throat | 104 (70.7) | |
| Facial pains and blocked sinus | 33 (22.4) | |
| Loss of smell and test | 52 (35.4) | |
| Headache | 111 (75.5) | |
| Shortness of breath | 36 (24.3) | |
| Cough | 98 (66.7) | |
| Fever | 77 (52.4) | |
| Fatigue | 70 (47.6) | |
| Chest pain | 21 (14.3) | |
| Diarrhea | 12 (2.8) | |
| Have you ever tested for COVID-19 | Yes | 90 (21.3) |
| No | 333 (78.7) | |
| If yes, what was the result (n = 90) | Positive | 81 (90) |
| Negative | 9 (10) |
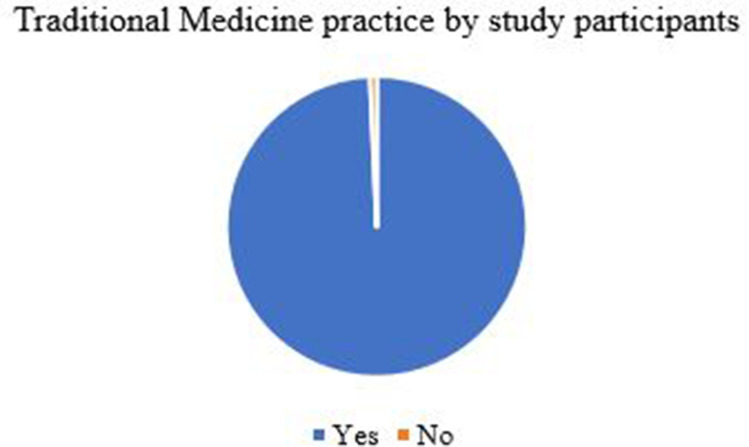
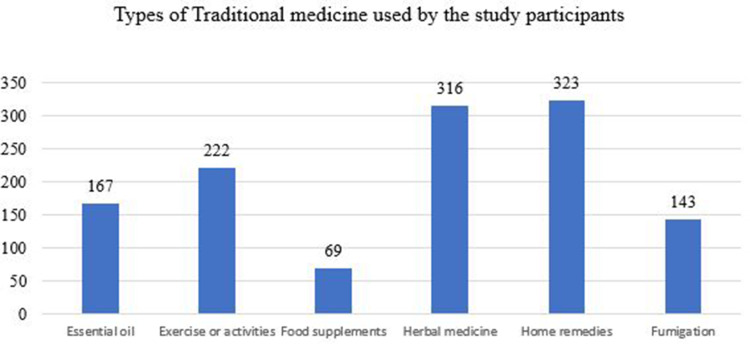
Traditional Medicine Practice for the Treatment of COVID-19 Related Symptoms
In the current study, almost all (99%) of the study participants were involved in practicing traditional medicine for the management of COVID-19 and related symptoms (Figure 1). Home remedies were the most reported types of traditional medicine practice by 323 of the total respondents, and herbal medicines were the second most practiced by 316 respondents (Figure 2).
Figure 1.
Traditional medicine practice by visitors of UOGCSH, Northwest Ethiopia, 2021 (n = 423).
Figure 2.
Types of traditional medicine used for the prevention and treatment of COVID-19 symptoms among visitors of UOGCSH, Northwest Ethiopia, 2021 (n = 423).
Mostly used herbal products by participants for the management of COVID-19 related symptoms were Eucalyptus, Damakese, Ginger, Rue, Fetto, Zingibil, Garlic, Lemon tea, and Moringa tea and fumigation of their home and environment with different herbs like Kebericho, Tinjut, Temenay (Table 4).
Table 4.
List of Medicinal Plants Used for the Prevention and Treatment of COVID-19 Symptoms Among Visitors of UOGCSH, Northwest Ethiopia, 2021 (N = 423)
| Type of Traditional Medicine | Local Name | Scientific Name |
|---|---|---|
| Essential oil | Nech Bahirzaf | Eucalyptus globulus |
| Tikur Azmud | Nigella sativa | |
| Herbal medicine | Zinjibil | Zingiber officinale |
| Tenadam | Ruta chalepensis | |
| Fetto | Lepidium sativum | |
| Nech Shinkurt | Allium sativum | |
| Home remedies | Zingibil (shay) | Zingiber officinale |
| Lomi (shay) | Citrus aurantifolia | |
| Moringa (shay) | Moringa oleifera | |
| Haregresa | Zehneria scabra | |
| Damakese | Ocimum lamiifolium Hochst | |
| Fumigation | Kebericho | Echinops kebericho |
| Tinjut | Otostegia integrifolia | |
| Temenay | Securidaca longepedunculata |
Association of Independent Variables with Complementary and Alternative Medicine Practice for the Prevention and Treatment of COVID-19 Symptoms
As (Table 5) shows, the statistical association between the independent variables and the practice of traditional medicine for the treatment of COVID-19 related symptoms was done using chi-square test analysis. In this analysis, monthly income and perceived knowledge about chief symptoms were statistically significantly associated with the use of complementary and alternative medicine for the management of COVID-19 related symptoms.
Table 5.
Association of Independent Variables with Traditional Medicine Practice for the Prevention and Treatment of COVID-19 Symptoms Among Visitors of UOGCSH, Northwest Ethiopia, 2021 (N = 423)
| Variables | Categories | Do You Use CAM for Prevention or Treatment of COVID-19 Symptoms | P-value | |
|---|---|---|---|---|
| Yes | No | |||
| Gender | Female | 219 | 1 | 0.516 |
| Male | 201 | 2 | ||
| Age | 18–34 | 255 | 3 | 0.587 |
| 35–49 | 112 | 0 | ||
| 50–65 | 50 | 0 | ||
| Above 65 | 3 | 0 | ||
| Religion | Orthodox | 314 | 2 | 0.565 |
| Muslim | 47 | 0 | ||
| Protestant | 59 | 1 | ||
| Educational status | Basic education | 15 | 0 | 0.832 |
| College diploma | 85 | 0 | ||
| First degree and above | 165 | 1 | ||
| Primary education | 25 | 0 | ||
| Secondary education | 80 | 1 | ||
| Illiterate | 43 | 1 | ||
| Religious education | 7 | 0 | ||
| Monthly income | 1651–3200 | 69 | 0 | 0.047* |
| 3201–5250 | 54 | 0 | ||
| 5251–7800 | 36 | 2 | ||
| 7801–10,900 | 36 | 0 | ||
| 10,901 and above | 17 | 0 | ||
| No monthly income | 43 | 0 | ||
| Unknown monthly income | 165 | 1 | ||
| Do you know the symptoms of COVID-19 | Yes | 412 | 2 | 0.000* |
| No | 8 | 1 | ||
| Have you ever experienced COVID-19 symptoms | Yes | 145 | 2 | 0.056 |
| No | 267 | 0 | ||
Note: *P-value ≤0.05.
Discussion
In the current study, we assessed the practice of traditional medicine for the treatment COVID-19 related symptoms and independent factors associated with the practice at UOGCSH, Northwest Ethiopia. Natural products have always been intriguing to scientists for drug research to develop novel candidates.14
Medicinal plants are considered very useful by traditional healers in many societies for the management of several diseases and ailments.15 In this study, 414 (97.9%) of the respondents heard about the main clinical symptoms experienced by a person who had COVID-19. This finding was higher than the studies done in Ethiopia16,17 and Kenya.18 This increased result could be due to the variation of data collection period. Being more recent data, the information level of the population of our study participants is expected to be higher in the case of our study.
Regarding the source of information about COVID-19 signs and symptoms, most of the study participants use television as their primary source information followed by social media sources and this finding goes in line with other studies conducted in Ethiopia.19
Almost all (97.6%) of the study participants responded that they use traditional medicines for the prevention and treatment of COVID-19 related symptoms. The findings revealed that the population depends on traditional medicine for the treatment of COVID-19 related symptoms. The finding showed an increment than in studies conducted in Peru and Turkey, which showed the prevalence of the practice was 80.2% and 39.9%, respectively.20,21 This increased result could be due to our study including the practice of traditional medicine for both treatment and prevention of COVID-19 related symptoms; on the other hand, the studies listed above assessed the traditional medicine used for symptomatic treatment of COVID-19.
Natural products such as home remedies and herbal medicines were among the reported practices with the highest frequency. This result also goes in line with the findings from the study conducted in Turkey which showed that herbal medicine is the most commonly used type of traditional medicine for the treatment of COVID-19 related symptoms.21 Unavailability of modern medications for prevention and symptom treatment, the trust of the population for natural products, and the ease of preparation of home remedies could be the reason making them practice with the highest frequency.
Every method used by the study participants is supported by other studies done in different study populations. One of the relevant applicable medical manifestations of COVID-19 is the tremendous harm to the breathing tract, inflicting breathing difficulty which can cause death,22 and for this reason, traditional medicine practices were required since modern drugs to cure the disease are not available.23
The major intention behind the use of medicinal plants during the period of COVID-19 pandemic was to manage the symptoms with the claimed antiviral property characteristics of the listed practices.24 Products such as essential oils have been used for their antiviral and anti-inflammatory properties which include symptoms associated with COVID-19.20,25–28 Some types of special diet supplementation such as vitamins, minerals, amino acids, and omegas also play a fundamental role in the treatment of respiratory symptoms, because the products trigger an immune response to respiratory viruses in addition to their regulatory activity in the inflammation caused by COVID-19.29 Treating respiratory tract infections by traditional medicine is a common practice in every community. Plants such as ginger, rue (Tenadam), Lepidium sativum (Fetto), and garlic, Nigella sativa L. (Tikur azmud), seeds, slices of rhizomes of Zingiber officinale (Zinjibile), and juice of Citrus limon L. (Lomi) have been reported to be used as a treatment for symptoms associated with respiratory tract infections.30
Fumigation of home and environment can be employed for the treatment of respiratory symptoms.31 Home remedies such as ginger tea, lemon tea, and moringa tea, Haregresa (Zehneria scabra), Damakese (Ocimum lamiifolium hochst) are the most commonly used home remedies to treat respiratory tract symptoms.32
Foods and diets that specially used in the case of respiratory tract infections are also one of the common modalities that are employed in the treatment of respiratory tract infections.32 Our study also showed that food supplements such as honey, fruits and vegetables, soups, and spices have been used by the participants as treatment for symptoms associated with respiratory tract infections.
Practices of fumigation of the home and environment with herbal materials were used by about 34% of our study participants as management for COVID-19 related symptoms. This method has also been practiced and reported by different studies. Some local herbs reported by our study participants like kebericho, tinjut, and temenay were used for treatment purposes of respiratory tract symptoms.
The use of traditional medicines for preventive purposes of symptoms associated with respiratory tract infections and inflammatory reactions is also a common process among different groups of the population.20,28 Indeed, the proper functioning of the immunity makes the body able to fight effectively against every kind of infection.33 This is why it is essential to strengthen it to prevent and treat possible infections, such as colds, fever, shortness of breath, and sore throat, symptoms similar to those of this pandemic virus.34 The findings from the current study also support this practice. The study participants, other than those who experienced the symptoms of COVID-19, took the traditional medicines for their preventive purpose. Herbal products such as Allium sativum L., eucalyptus, ginger, garlic, lemon, thyme, ginger, and honey were reported to have immunomodulatory properties in a number of in vitro and in vivo studies and can be used prophylactically in the prevention of viral infections.33 Some herbal medicines such as Moringa oleifera have established in vivo and in vitro antiviral activity against Newcastle disease virus, HIV/AIDS, and herpes simplex virus type 1 (HSV-1).35,36
As for the socio-demographic factors associated with the use of traditional medicine for the management of respiratory symptoms related to COVID-19, our study reported that the monthly income (p = 0.047) and the perception of respondents about clinical symptoms (p value 0.000) have statistically significantly associated.
Limitations of the Study
The nonprobability of consecutive sampling method used to approach the study participants may raise some difficulties with inference findings for the general population. Another limitation might be the bias occurred as a result of the cross-sectional study design to determine definitive cause and effect associations. Our study participants are inclined to the young age that the virus was milder than elderly patients. This might affect the perception of the respondent and traditional medicine practice for the management of COVID-19 related symptoms. With these limitations, the findings of this study should not be undermined.
Conclusion
This study found that most of the respondents have heard about the COVID-19 pandemic and know the symptoms experienced by a person infected with this. The prevalence of traditional medicine use for the prevention and treatment of COVID-19 related symptoms was very high. The mostly used traditional or alternative medicines were essential oils, exercise or activities, and special and herbal medicines. Monthly income and perceived knowledge about chief clinical symptoms were statistically significantly associated with the use of complementary and alternative medicine for the management of COVID-19 and related symptoms. The investigators suggest that researchers should look into the medicinal herbs that were employed during COVID-19 for its management. Validity and reliability of therapeutic plants should be further evaluated through phytochemical and pharmacological studies about the bioactive compounds and the proper education about the rational use of traditional medicines should be given to the community.
Acknowledgments
The authors are grateful for the study participants, School of Pharmacy, University of Gondar, and data collectors.
Data Sharing Statement
The corresponding author has the dataset and will provide it upon reasonable request.
Author Contributions
Each author contributed significantly to the conception and design, acquisition of data, or analysis and interpretation of data; participated in the writing of the article or critically reviewed it for crucial intellectual content; agreed to submit to the current journal; finalized approval of the published version; and accept liability for all aspects of the work.
Disclosure
The authors affirm that they have no conflicts of interest.
References
- 1.She J, Jiang J, Ye L, et al. 2019 novel coronavirus of pneumonia in Wuhan, China: emerging attack and management strategies. Clin Transl Med. 2020;9(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Subbarao K, Mahanty SJI. Respiratory virus infections: understanding COVID-19. Immunity. 2020;52(6):905–909. doi: 10.1016/j.immuni.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nugraha RV, Ridwansyah H, Ghozali M, Khairani AF, Atik N. Traditional herbal medicine candidates as complementary treatments for COVID-19: a review of their mechanisms, pros and cons. Evid Based Complement Altern Med. 2020;2020. doi: 10.1155/2020/2560645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forman R, Shah S, Jeurissen P, Jit M, Mossialos E. COVID-19 vaccine challenges: what have we learned so far and what remains to be done? Health Policy. 2021;125(5):553–567. doi: 10.1016/j.healthpol.2021.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le TT, Andreadakis Z, Kumar A, et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19(5):305–306. [DOI] [PubMed] [Google Scholar]
- 6.Cleve MJN. What the lightning-fast quest for Covid vaccines means for other diseases. Nature. 2021;589:16–18. [DOI] [PubMed] [Google Scholar]
- 7.Yang Y, Islam MS, Wang J, Li Y, Chen X. Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): a review and perspective. Int J Biol Sci. 2020;16(10):1708. doi: 10.7150/ijbs.45538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akinyemi O, Oyewole S, Jimoh K. Medicinal plants and sustainable human health: a review. Hortic Int J. 2018;2(4):194–195. [Google Scholar]
- 9.Kassaye KD, Amberbir A, Getachew B, Mussema Y. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiop J Health Dev. 2006;20(2):127–134. [Google Scholar]
- 10.Ashfaq F, Ali Q, Haider M, Hafeez M, Malik A. Therapeutic activities of garlic constituent phytochemicals. Biol Clin Sci Res J. 2021;2021(1). doi: 10.54112/bcsrj.v2021i1.53 [DOI] [Google Scholar]
- 11.Wondmkun Y, Mohammed O. Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-COV-2) inhibition and other antiviral effects of Ethiopian medicinal plants and their compounds. J in silico in vitro Pharmaco. 2020;6(2):4. [Google Scholar]
- 12.Ang L, Song E, Lee HW, Lee MS, Chandran J, Abhilash KPP. Herbal medicine for the treatment of coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis of randomized controlled trials. J Family Med Primary Care. 2020;9(5):1583. doi: 10.4103/jfmpc.jfmpc_1081_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abate H, Mekonnen CK. Knowledge, attitude, and precautionary measures towards covid-19 among medical visitors at the university of Gondar comprehensive specialized hospital northwest Ethiopia. Infect Drug Resist. 2020;13(4355):4355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beutler JA. Natural products as a foundation for drug discovery. Curr Protoc Pharmacol. 2009;46(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tuasha N, Petros B, Asfaw Z. Medicinal plants used by traditional healers to treat malignancies and other human ailments in Dalle District, Sidama Zone, Ethiopia. J Ethnobiol Ethnomed. 2018;14(1):1–21. doi: 10.1186/s13002-018-0213-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akalu Y, Ayelign B, Molla MD. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infect Drug Resist. 2020;13:1949. doi: 10.2147/IDR.S258736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nigussie TF, Azmach NN. Knowledge, attitude and practice towards covid-19 among Arba Minch town, southern Ethiopia. GSJ. 2020;8(6):1283–1307. [Google Scholar]
- 18.Austrian K, Pinchoff J, Tidwell JB, et al. COVID-19 related knowledge, attitudes, practices and needs of households in informal settlements in Nairobi, Kenya. SSRN Elect J. 2020. doi: 10.2139/ssrn.3576785 [DOI] [Google Scholar]
- 19.Tadesse AW, Abebe NM, Tadesse SE, Wube MC, Abate AA. Preventive practice and associated factors towards COVID-19 among college students in Amhara Region, Ethiopia: a cross-sectional study. Ethiopian J Health Sci. 2021;31(1):3–14. doi: 10.4314/ejhs.v31i1.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Villena-Tejada M, Vera-Ferchau I, Cardona-Rivero A, et al. Use of medicinal plants for COVID-19 prevention and respiratory symptom treatment during the pandemic in Cusco, Peru: a cross-sectional survey. PLoS One. 2021;16(9):e0257165. doi: 10.1371/journal.pone.0257165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karataş Y, Khan Z, Bilen Ç, et al. Traditional and Complementary Medicine use and beliefs during COVID-19 outbreak: a cross-sectional survey among the general population in Turkey. Adv Integrat Med. 2021;8(4):261–266. doi: 10.1016/j.aimed.2021.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). Statpearls; 2022. [PubMed] [Google Scholar]
- 23.Hironaka LK, Paasche-Orlow MK. The implications of health literacy on patient–provider communication. Archiv Dis Childhood. 2008;93(5):428–432. doi: 10.1136/adc.2007.131516 [DOI] [PubMed] [Google Scholar]
- 24.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Archiv Intern Med. 2005;165(17):1946–1952. doi: 10.1001/archinte.165.17.1946 [DOI] [PubMed] [Google Scholar]
- 25.Grigore A, Cord D, Tanase C, Albulescu R. Herbal medicine, a reliable support in COVID therapy. J Immunoassay Immunochem. 2020;41(6):976–999. doi: 10.1080/15321819.2020.1862867 [DOI] [PubMed] [Google Scholar]
- 26.Khazdair MR, Ghafari S, Sadeghi M. Possible therapeutic effects of Nigella sativa and its thymoquinone on COVID-19. Pharmaceut Biol. 2021;59(1):696–703. doi: 10.1080/13880209.2021.1931353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Panikar S, Shoba G, Arun M, et al. Essential oils as an effective alternative for the treatment of COVID-19: molecular interaction analysis of protease (Mpro) with pharmacokinetics and toxicological properties. J Infect Public Health. 2021;14(5):601–610. doi: 10.1016/j.jiph.2020.12.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valussi M, Antonelli M, Donelli D, Firenzuoli F. Appropriate use of essential oils and their components in the management of upper respiratory tract symptoms in patients with COVID-19. J Herbal Med. 2021;28:100451. doi: 10.1016/j.hermed.2021.100451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhuiyan FR, Howlader S, Raihan T, Hasan M. Plants metabolites: possibility of natural therapeutics against the COVID-19 pandemic. Front Med. 2020;7(444). doi: 10.3389/fmed.2020.00444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Azam MNK, Al Mahamud R, Hasan A, Jahan R, Rahmatullah M. Some home remedies used for treatment of COVID-19 in Bangladesh. J Med Plants Stud. 2020;8(4):27–32. [Google Scholar]
- 31.Oyeyemi A, Adesina A, Ogoina D. Fumigation of schools for COVID-19 prevention in Nigeria: the need for a rethink. Am J Trop Med Hyg. 2020;103(4):1370. doi: 10.4269/ajtmh.20-1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pieroni A, Vandebroek I, Prakofjewa J, et al. Taming the Pandemic? The Importance of Homemade Plant-Based Foods and Beverages as Community Responses to COVID-19. Springer; 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gourch A, Zejli H, Lfitat A, et al. Preventive impact of traditional medicine against covid-19. J Anal Sci Appl Biotechnol. 2020;2(2):78–82. [Google Scholar]
- 34.Yousfi N, Bragazzi NL, Briki W, Zmijewski P, Chamari K. The COVID-19 pandemic: how to maintain a healthy immune system during the lockdown–a multidisciplinary approach with special focus on athletes. Biol Sport. 2020;37(3):211–216. doi: 10.5114/biolsport.2020.95125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Komolafe K, Komolafe TR, Fatoki TH, et al. Coronavirus disease 2019 and herbal therapy: pertinent issues relating to toxicity and standardization of phytopharmaceuticals. Revista brasileira de farmacognosia. 2021;31(2):142–161. doi: 10.1007/s43450-021-00132-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Okorie C, Ajibesin K, Sanyaolu A, et al. A review of the therapeutic benefits of Moringa oleifera in controlling high blood pressure (hypertension). Curr Tradit Med. 2019;5(3):232–245. [Google Scholar]
- 37.Tegen D, Dessie K, Damtie D. Candidate anti-COVID-19 medicinal plants fro m Ethiopia: a review of plants traditionally used to treat viral diseases, Evid. Evid Based Complement Altern Med. 2021;2021:6622410. doi: 10.1155/2021/6622410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Infusino F, Marazzato M, Mancone M, et al. Diet supplementation, probiotics, and nutraceuticals in SARS-CoV-2 infection: a scoping review. Orthop Surg. 2020;12(6):1718. doi: 10.1111/os.12766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tegen D, Dessie K, Damtie D, Medicine A. Candidate anti-COVID-19 medicinal plants from Ethiopia: a review of plants traditionally used to treat viral diseases. Evid Based Complement Altern Med. 2021;2021:6622410. [DOI] [PMC free article] [PubMed] [Google Scholar]