Abstract
Objective
To evaluate the clinical efficacy of high-flow nasal oxygen therapy (HFNC) and non-invasive ventilation (NIV) in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) after extubation.
Research Methods
This systematic review and meta-analysis was conducted following the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) statements. The primary outcome measures analyzed included: reintubation rate, mortality, complication rate, and ICU length of stay.
Results
Eight studies were included, with a total of 612 subjects, including 297 in the HFNC group and 315 in the NIV group. The effect of HFNC and NIV on the reintubation rate of AECOPD patients after extubation, RR (1.49 [95% CI,0.95 to 2.33], P = 0.082). Subgroup analysis with or without hypercapnia according to the included AECOPD population, with hypercapnia, RR (0.69 [95% CI,0.33 to 1.44], P=0.317), without hypercapnia, RR (2.61 [95% CI,1.41 to 4.83], P=0.002). Mortality, RR (0.92 [95% CI,0.56 to 1.52], P = 0.752). ICU length of stay, MD (−0.44 [95% CI,-1.01 to 0.13], P = 0.132). Complication rate, RR (0.22 [95% CI,0.13 to 0.39], P = 0.000). After subgroup analysis, the reintubation rate of HFNC and NIV has no statistical difference in patients with hypercapnia, but NIV can significantly reduce the reintubation rate in patients without hypercapnia. In the outcome measures of complication rate, HFNC significantly reduced complication rate compared with NIV. In mortality and ICU length of stay, analysis results showed that HFNC and NIV were not statistically different.
Conclusion
According to the available evidence, the application of HFNC can be used as an alternative treatment for NIV after extubation in AECOPD patients with hypercapnia, but in the patients without hypercapnia, HFNC is less effective than NIV.
Keywords: nasal high-flow oxygen therapy, acute exacerbation of chronic obstructive pulmonary disease, non-invasive ventilation, meta-analysis
Introduction
Chronic obstructive pulmonary disease (COPD) is a common chronic disease characterized by persistent airflow limitation.1 Over the past few decades, the morbidity and mortality of COPD has increased exponentially, affecting the global About 384 million people, it is now considered the third leading cause of death globally.2 Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is defined as an acute worsening of respiratory symptoms that require additional treatment, with significant negative impact on health status, hospitalization, readmission, disease progression, and mortality. It not only seriously affects the quality of life of patients, but also imposes a heavy economic burden on families, medical systems and society.3,4
Non-invasive ventilation (NIV) is the preferred initial mode of ventilator assistance for patients with acute hypercapnic breathing failure caused by AECOPD.5,6 Compared with invasive mechanical ventilation (IMV), AECOPD patients treated with NIV has lower in-hospital mortality, shorter hospital stay and lower cost.7,8 With the development of medicine, invasive-noninvasive sequential ventilation strategy has become an effective way to wean off invasive mechanical ventilation in patients with AECOPD. And it has significantly reduced weaning-related mortality, pneumonia and ventilation time.9
High Flow Nasal Cannula (HFNC) is a new type of non-invasive breathing assistance method that can improve ventilation and oxygen by providing precise oxygen concentration heated and humidified oxygen, better tolerance and comfort than NIV.10 It may reduce the volume of dead space and increase the alveolar volume, which can result in improvement of alveolar ventilation and gas exchange.11 For COPD patients with type II respiratory failure and pH between 7.25 and 7.35, HFNC was statistically non-inferior to NIV as initial ventilatory support in decreasing PaCO2 after 2h of treatment in patients with mild-to-moderate AECOPD.12 A recent meta-analysis study showed that HFNC is more beneficial than NIV in the treatment of COPD and hypercapnic respiratory failure.13 However, in the process of weaning of AECOPD patients, the therapeutic effect of HFNC and whether it can be used as an alternative therapy for NIV is still unclear. Therefore, in this study, the method of meta-analysis was used to analyze the therapeutic effect of HFNC and NIV in patients with AECOPD after extubation, in order to provide evidence-based basis for clinical practice.
Methods
This systematic review and meta-analysis was registered at PROSPERO (http://www.crd.york.ac.uk/prospero, CRD:42022312973) and designed as per the Cochrane Handbook for Systematic Reviews of Interventions14 and reported according to the PRISMA guidelines.15
Data Sources and Searches
Retrieval database: PubMed, Web of science, Embase, Cochrane Library database. Retrieval database date is from establishment to March 10, 2022. Retrieval combines subject headings and free words: Pulmonary Disease, Chronic Obstructive, High-Flow Nasal Cannula OR HFNC OR High-Flow Oxygen Therapy OR High-Flow nasal oxygen OR High nasal flow OR High-Flow nasal cannula oxygen therapy OR High-Flow oxygen, Noninvasive ventilation. For detailed search strategies, see in Supplementary Data S1.
Literature Data Inclusion and Exclusion Criteria
Inclusion criteria were as follows:(1) adults ≥ 18 years old,(2) Patients who meet the diagnostic criteria of COPD, have acute exacerbation and receive invasive intubation,(3) comparison of the effects of HFNC and NIV as the key study objective,(4) RCT study design,(5) at least one data outcome of interest available for extraction,(6) Chinese and English literature. Exclusion criteria are:(1) patients under the age of 18,(2) non-RCT studies,(3) data are incomplete or cannot be extracted,(4) full text is not available.
Types of Outcome Measures
Our purpose is to evaluate the effect of HFNC and NIV on the prognosis of AECOPD patients after extubation, Therefore, the primary outcome indicator we selected is: reintubation rate. Secondary outcomes included: mortality, complication rate, and ICU length of stay, respiratory rate(RR), heart rate(HR), pH, oxygenation index (PaO2/FiO2), and partial pressure of carbon dioxide (PaCO2).
Data Extraction and Quality Assessment
Literature screening we imported the retrieved literature into the ENDNOTE software, and two researchers independently reviewed each retrieved document, according to the inclusion and exclusion criteria, preliminary screening of the documents by reading the title and abstract, and then preliminary screening by reading the full text. Filter the file for further filtering. For trials that met the inclusion criteria, we extracted basic information from the articles, such as the first author’s last name, year of publication, participant type, sample size, intervention, control and outcome. As for quality assessment, the quality of RCTs was assessed using the Cochrane risk of bias tool, including assessment of random sequence generation, allocation concealment, patient and intervention blinding, outcome measurer blinded, incomplete outcome data, selective reporting, and other potential biases. Each item was rated as “low risk”,’high risk’ or “unclear”, and the evaluation was conducted independently by two authors. Disagreements were resolved through arbitration by discussion and consultation with a third author.
Statistical Analysis
As for statistical analysis, all analyses were performed using STATA SE 15.1, binary variables were represented by risks ratio (RR), and continuous variables were represented by mean difference (MD) or standardized mean difference (SMD), and each effect size was represented by 95% confidence interval (CI). The heterogeneity among the results of the included studies was analyzed by the I2 test. P<0.05 was considered to be statistically significant. When the heterogeneity test P ≥ 0.05 and I2<50%, multiple similar studies were considered to have homogeneity. If P<0.05 and I2 ≥ 50%, a random-effects model was used. If multiple time points were reported for the outcome measure, we selected the common time point included in most experiments. Mean and SD values were estimated when outcome measures were reported as interquartile range and median range (or 95% confidence interval). The Engauge Digitizer (version 4.1) graphical data extraction software was used to extract data that were only provided by images. Funnel plots and Egger tests were not used to assess potential publication bias because the number of studies performed for quantitative analysis was <10, in which case funnel plots and Egger tests could produce misleading results.16 Sensitivity analysis was performed on the necessary outcome indicators to determine the stability of the results.
Subgroup Analysis
We performed a subgroup analysis based on baseline PaCO2 levels. We believe that the average PaCO2 ≥ 50 mmHg at the beginning of the trial or patients with type II respiratory failure were included in the study has hypercapnia, while the lower baseline PaCO2< 50 mmHg at the beginning of the trial has no hypercapnia.
Results
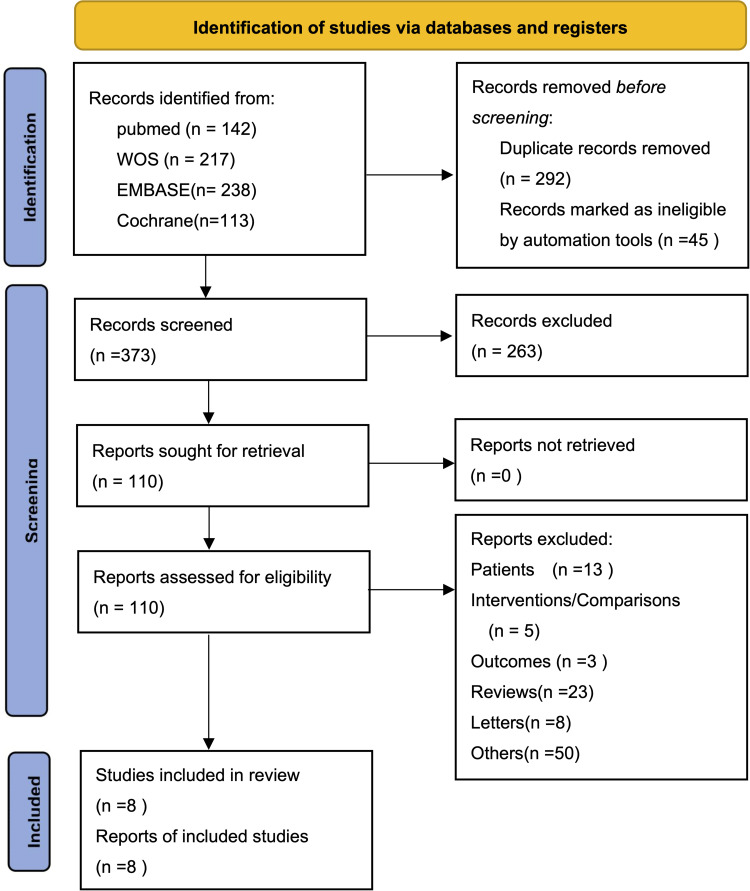
A total of 710 relevant studies were initially detected, and after reading the literature titles and abstracts, they were screened according to the inclusion and exclusion criteria, and 8 qualified clinical studies were finally included,17–24 a total of 612 subjects. There were 297 subjects in the HFNC group and 315 subjects in the NIV group. The screening process is shown in Figure 1, and the basic characteristics of the included studies are shown in Table 1.
Figure 1.
PRISMA (preferred reporting items for systematic reviews and meta-analysis) flow diagram.
Notes: Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:160. Creative Commons.15
Table 1.
Characteristics of Included Studies
| Authors Year | Methods | Intervention | Language | Age (Years) | Gender (Male/Total) | APACHE II Score | PaCO2, mmHg | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HFNC | NIV | HFNC | NIV | HFNC | NIV | HFNC | NIV | |||||
| Zhang 201817 | RCT | HFNC vs NIV | Chinese | 64.5±5.3 | 66.1±6.6 | 18/21 | 20/24 | 16.3±1.4 | 16.7±1.6 | 42.9±7.7 | 43.3±8.1 | ①②③④⑤⑥ |
| Yu 201918 | RCT | HFNC vs NIV | Chinese | 62.4±10.1 | 63.5±11.2 | 24/36 | 21/36 | 28.6±2.8 | 28.5±3.4 | 73.56±6.9 | 73.50±6.23 | ①②③④⑤⑥⑦⑧⑨ |
| Jing 201919 | RCT | HFNC vs NIV | English | 77.4±6.8 | 73.9 ±6.9 | NA | NA | 11.8±3.1 | 10.4±2.5 | 53.2±6.7 | 53.7 ±8.6 | ①②③④⑤⑥⑦⑧⑨ |
| Yang 202020 | RCT | HFNC vs NIV | Chinese | 69±9 | 67±9 | 25/40 | 20/33 | 12.3±1.9 | 12.1±1.8 | 55±9 | 56±8 | ①②⑤ |
| Thille 202121 | RCT | HFNC vs NIV | English | 66±9 | 66±9 | 48/64 | 61/86 | NA | NA | 44±9 | 43±8 | ①②④ |
| Xu 202122 | RCT | HFNC vs NIV | English | 69.22 ±6.13 | 68.39 ±5.22 | NA | NA | NA | NA | NA | NA | ①③⑤⑥⑦ |
| Fang 202123 | RCT | HFNC vs NIV | Chinese | 67.9±6.9 | 72.3±7.8 | 14/20 | 11/24 | 14.3±3.8 | 15.0±2.9 | 39.4±6.5 | 40.0±8.9 | ①②③④⑤⑦⑧⑨ |
| Tan 202024 | RCT | HFNC vs NIV | English | 68.4± 9.3 | 71.4± 7.8 | 27/44 | 23/42 | 14(11–18.8) | 13(10.8–16) | 50.5(48–57.8) | 53(48.8–61.3) | ①②③④⑤⑥⑦⑧⑨ |
Notes: Outcomes:①reintubation rates②mortality③complication rates④ length of ICU stay ⑤PaCO2 ⑥ PaO2/FiO2 ⑦RR ⑧ HR ⑨PH.
Abbreviations: RCT, randomized controlled trial; HFNC, high-flow nasal cannula; NIV, non-invasive ventilation; NA, not applicable.
In the 8 RCT studies included,4 were in Chinese17,18,20,23 and 4 were in English.19,21,22,24 8 studies explicitly mentioned the method of generating random sequences, among which there are 4 items that mention allocation hiding. Due to differences in oxygen therapy equipment, it was difficult to blind study patients and interventionists. No other risk of bias was found in all findings. Details are shown in Supplementary Figure S2.
Primary Outcome
Reintubation Rates
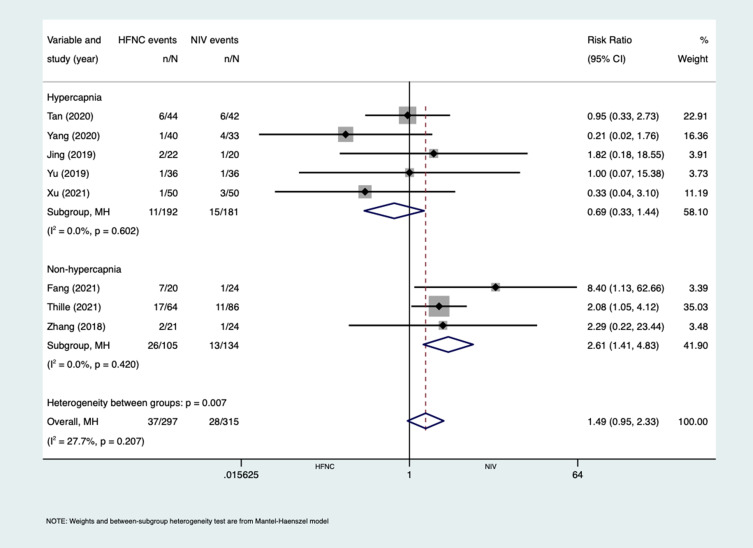
All of the eight studies17–24 reported the effect of HFNC on the reintubation rate of AECOPD patients after extubation, there are six studies17–20,22,24 observed reintubation rate within 3 days and two studies21,23 observed within 7 days (Figure 2), the heterogeneity test result was I2=27.7%, P=0.207, using a fixed effect model, the results showed RR (1.49 [95% CI,0.95 to 2.33], P=0.082), the difference was not statistically significant. Subgroup analysis was performed according to whether the included population was accompanied by hypercapnia. In the hypercapnia group, the heterogeneity test result was I2=0.00%, P=0.602, and the results showed RR (0.69 [95% CI,0.33 to 1.44], P=0.317), the difference was not statistically significant. It shows that compared with NIV, HFNC has no statistical difference in the reintubation rate of patients with AECOPD, and the two treatment effects are equivalent. In the non-hypercapnia group, the heterogeneity test result was I2=0.00%, P=0.420, the results showed RR (2.61 [95% CI,1.41 to 4.83], P=0.002), the difference was statistically significant, indicating that the reintubation rate of the HFNC group was higher, and the treatment effect was not as good as that of the NIV group.
Figure 2.
Forest plot of reintubation rates, subgroup analysis was performed according to variable of hypercapnia and non-hypercapnia.
Secondary Outcomes
Mortality
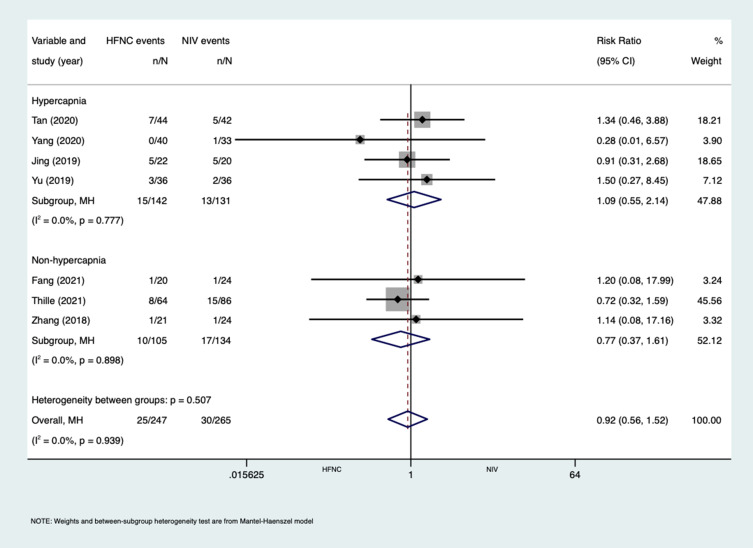
Seven studies17–21,23,24 reported the effect of HFNC on the mortality of AECOPD patients after extubation, four17,19,20,24 of them reported 28 day mortality and three18,21,23 of them reported mortality during hospitalization (Figure 3), the test result of the heterogeneity was I2=0.0%, P=0.939, using a fixed effect model, the results showed RR (0.92 [95% CI,0.56 to 1.52] P=0.752), the difference was not statistically significant. In subgroup analysis, with hypercapnia RR (1.09 [95% CI,0.55 to 2.14], P = 0.813), the difference was not statistically significant, without hypercapnia RR (0.77 [95% CI,0.37 to 1.61], P = 0.492), the difference was not statistically significant. It showed that there was no statistical difference between HFNC and NIV on the mortality of AECOPD patients regardless of whether it was accompanied by hypercapnia.
Figure 3.
Forest plot of mortality, subgroup analysis was performed according to variable of hypercapnia and non-hypercapnia.
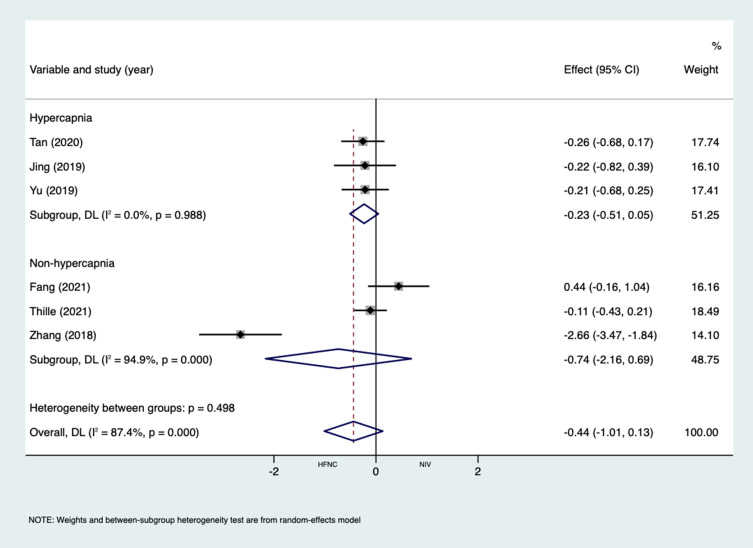
ICU Length of Stay
Six studies17–19,21,23,24 reported the effect of HFNC and NIV on the ICU length of stay in days in patients with AECOPD after extubation (Figure 4), the heterogeneity test result was I2=87.4%, P= 0.00, using a random effects model, the results showed that MD (−0.44 [95% CI,-1.01 to 0.13], P=0.132), the difference was not statistically significant. In subgroup analysis, there was no statistically significant difference in MD with hypercapnia (−0.23 [95% CI,-0.51 to 0.05], P = 0.102), and without hypercapnia (−0.74 [95% CI,-2.16 to 0.69], P = 0.313).
Figure 4.
Forest plot of ICU length of stay, subgroup analysis was performed according to variable of hypercapnia and non-hypercapnia.
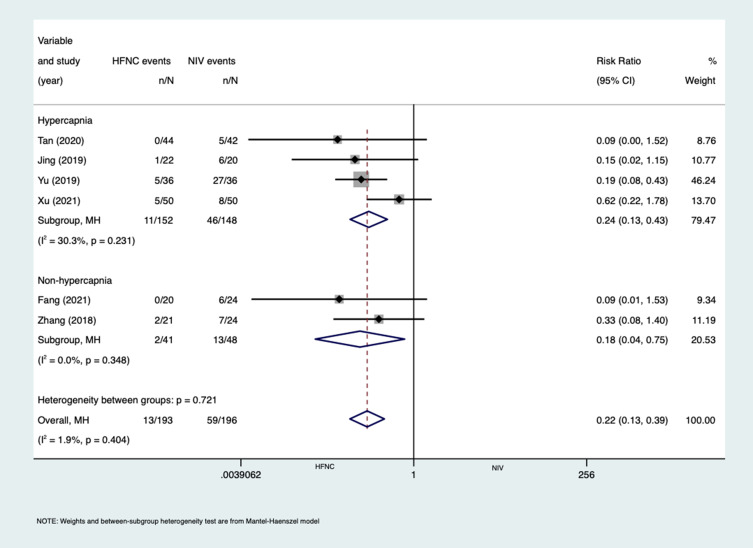
Complication Rates
Six studies17–19,22–24 reported the effect of HFNC and NIV on the complication rate of AECOPD patients after extubation, Complications mainly include nasal facial skin breakdown and aspiration and flatulence during the treatment, no serious adverse events were reported (Figure 5), the heterogeneity test result was I2=1.9%, P =0.404, using a fixed effect model, the results showed RR (0.22 [95% CI,0.13 to 0.39], P=0.00), the difference was statistically significant. In subgroup analysis, with hypercapnia RR (0.24 [95% CI,0.13 to 0.43], P = 0.000)was statistically significant, and non hypercapnia RR (0.18 [95% CI,0.04 to 0.75], P = 0.018), the difference was statistically significant. Compared with NIV, it indicated that HFNC could significantly reduce the complications of post-extubation patients.
Figure 5.
Forest plot of complication rates, subgroup analysis was performed according to variable of hypercapnia and non-hypercapnia.
Other Outcomes
The following data of all outcome indicators are selected from all studies with a total time of 24 hours. Seven studies17–20,22–24 reported the effect of HFNC and NIV on PaCO2 in patients with AECOPD after extubation. The results of heterogeneity test were I2=91.1%, P=0.00, using Random effects model, the results showed that MD (−0.19 [95% CI,-0.84 to 0.45], P=0.561), the difference was not statistically significant. In subgroup analysis, there was no significant difference in MD (−0.37 [95% CI,-1.21 to 0.46], P=0.378) with hypercapnia, and MD (0.28 [95% CI,-0.14 to 0.70], P=0.186) without hypercapnia. Four studies18,19,23,24 reported the effect of HFNC and NIV on the heart rate of AECOPD patients after extubation. The results of the heterogeneity test were I2=69.2%, P=0.021, using a random effect model, the results showed that MD (−0.38 [95% CI,-0.85 to 0.09], P=0.115), the difference was not statistically significant. In subgroup analysis, there was no significant difference in MD (−0.42 [95% CI,-1.05 to 0.21], P=0.191)with hypercapnia, without hypercapnia MD (−0.24 [95% CI,-0.83 to 0.36], P=0.435), the difference was not statistically significant. Five studies18,19,22–24 reported the effect of HFNC and NIV on the respiratory rate of AECOPD patients after extubation. The results of heterogeneity test were I2=20%, P=0.288, using a fixed effect model, the results showed that MD (−0.51 [95% CI,-0.73 to −0.30], P=0.000), the difference was statistically significant. Subgroup analysis was performed, with hypercapnia MD (−0.58 (95% CI,-0.81 to −0.35), P=0.000), the difference was statistically significant, without hypercapnia MD (−0.07 [95% CI,-0.67 to 0.52], P=0.807), the difference was not statistically significant. It indicated that HFNC significantly reduced the respiratory rate in AECOPD patients with hypercapnia, but in AECOPD patients without hypercapnia, the difference was not statistically significant and the treatment effect is equivalent. Four studies18,19,23,24 reported the effect of HFNC and NIV on the acid-base balance of patients with AECOPD after extubation. The results of the heterogeneity test were I2=81.7%, P=0.001, using a random effect model, the results showed that MD (0.37 [95% CI,-0.25 to 0.98], P=0.24), the difference was not statistically significant. Subgroup analysis was performed, with hypercapnia MD (0.52 [95% CI,-0.26 to 1.30], P=0.191), the difference was not statistically significant, without hypercapnia MD (−0.10 [95% CI,-0.69 to 0.49], P=0.739), the difference was not statistically significant. Five studies17–19,22,24 reported the effect of HFNC and NIV on PaO2/FiO2 in patients with AECOPD after extubation. The results of heterogeneity test were I2=71.0%, P=0.008, using random effects model, the results showed MD (0.14 [95% CI,-0.27 to 0.54], P=0.514), the difference was not statistically significant. Subgroup analysis was performed, with hypercapnia MD (0.30 [95% CI,-0.05 to 0.64], P=0.093), the difference was not statistically significant, without hypercapnia MD (−0.55 [95% CI,-1.15 to 0.05], P=0.070), the difference was not statistically significant. (See in Table 2, Supplementary Figure S3 for detailed forest diagrams.)
Table 2.
Other Outcome Measures
| Outcomes (Units) | Pooling Model | Subgroup | Inclusion Studies | Results | ||
|---|---|---|---|---|---|---|
| I2 (%) | MD (95% CI) | P-value | ||||
| PaCO2 (mmHg) | Random | Hypercapnia | 518–20,22,24 | 93.3 | −0.37 (−1.21,0.46) | 0.378 |
| Non-hypercapnia | 217,23 | 0.0 | 0.28 (−0.14,0.70) | 0.186 | ||
| Overall | 7 | 91.1 | −0.19 (−0.84,0.45) | 0.561 | ||
| HR (bpm) | Random | Hypercapnia | 318,19,24 | 78.9 | −0.42 (−1.05,0.21) | 0.191 |
| Non-hypercapnia | 123 | 0.00 | −0.24 (−0.83,0.36) | 0.435 | ||
| Overall | 4 | 69.2 | −0.38 (−0.85,0.09) | 0.115 | ||
| RR (bpm) | Fixed | Hypercapnia | 418,19,22,24 | 0.0 | −0.58 (−0.81,-0.35) | 0.000 |
| Non-hypercapnia | 123 | 63.6 | −0.07 (−0.67,0.52) | 0.807 | ||
| Overall | 5 | 20.0 | −0.51 (−0.73,-0.30) | 0.000 | ||
| PH | Random | Hypercapnia | 318,19,24 | 85.9 | 0.52 (−0.26,1.30) | 0.191 |
| Non-hypercapnia | 123 | 0.0 | −0.10 (−0.69,0.49) | 0.739 | ||
| Overall | 4 | 81.7 | 0.37 (−0.25,0.98) | 0.240 | ||
| PaO2/FiO2 (mmHg) | Random | Hypercapnia | 418,19,22,24 | 54.0 | 0.30 (−0.05,0.64) | 0.093 |
| Non-hypercapnia | 117 | 0.0 | −0.55 (−1.15,0.05) | 0.070 | ||
| Overall | 5 | 71.0 | 0.14 (−0.27,0.54) | 0.514 | ||
Abbreviations: PaCO2, partial pressure of arterial carbon dioxide; HR, heart rate; RR, respiratory rate; PaO2, partial pressure of oxygen; FiO2, fraction of inspired oxygen.
We performed subgroup analyses for all outcomes, most of which showed good homogeneity, and we performed sensitivity analyses for outcomes with higher heterogeneity, sensitivity analysis was performed to exclude studies one by one, all the results remained unchanged (see in Supplementary Figure S4).
Discussion
Mechanical ventilation is widely used in the treatment of respiratory failure caused by various reasons, and is of great significance in the clinical treatment of chronic obstructive pulmonary disease. The difficulty of weaning patients with acute exacerbation of chronic obstructive pulmonary disease is one of the important clinical problems, The reasons were ventilator fatigue and worsening respiratory mechanics.25 NIV can supply stable high-concentration oxygen, relaunched alveoli, improve gas exchange, and reduce intubation and mortality in patients with respiratory failure, especially those with exacerbated chronic obstructive pulmonary disease. However, NIV can lead to many complications, such as skin damage, eye irritation, claustrophobia, dryness of the oropharynx, flatulence, aspiration and expectoration difficulties, and affects eating and communication, resulting in poor tolerance and comfort, and extremely greatly limit its clinical application.26,27 HFNC can provide high-flow gas to patients, and HFNC can generate positive airway pressure, increase functional residual capacity, improve oxygenation,28 and allow patients to receive a constant oxygen concentration.29 Heated and humidified gas can promote airway secretions It can clear the airway, protect airway epithelial cells, and reduce the discomfort of patients.30
In this study, we mainly compared the reintubation rate of HFNC and NIV in the post-extubation treatment of AECOPD patients, this is different from previous systematic reviews, even the seven included studies were in the last 3 years. The results of reintubation rate showed that there was no statistical difference between them, Subgroup analysis was conducted between hypercapnia and non-hypercapnia, and the results showed that there was no significant difference in patients with hypercapnia, but in patients without hypercapnia, the reintubation rate in HFNC group was significantly higher than the NIV group, This result suggests that the effect of HFNC in AECOPD patients with hypercapnia is similar to NIV, which may be related to the reduction of respiratory muscle load and respiratory overwork by both of them, which is consistent with the results of previous studies.12,31,32 It can be used as an alternative treatment for NIV after extubation in AECOPD patients with hypercapnia, and has certain advantages, but in AECOPD patients without hypercapnia, the treatment effect of HFNC is not as good as NIV, It may be related to the lower respiratory pressure provided by HFNC than NIV. Although all included studies have given the judgment criteria for failure of HFNC or NIV treatment, mainly focusing on the patient’s respiratory rate, blood gas analysis, consciousness status and clinician’s decision-making, the judgment criteria are different, and there are risks of delayed intubation and increased complications. In future studies, if an effective standard, such as Rox or mrox or hacor33–36 can be used, the results will be more reliable.
In the analysis of complication rates, HFNC was significantly lower than NIV, and there was no change in the results of subgroup analysis, which may be related to NIV and the intolerance to the interface and poor patient–ventilator interaction and Synchronization.37,38 In the analysis of respiratory rate, compared with NIV, HFNC can reduce the respiratory rate of patients with AECOPD after extubation, and the subgroup analysis results suggest that HFNC has a strong effect on reducing respiratory rate in AECOPD with hypercapnia, in AECOPD patients without hypercapnia, its performance was not statistically different from NIV. The reason for the analysis may be that the long-term airflow limitation in AECOPD patients will lead to increased diaphragm load, resulting in diaphragm injury and diaphragm fatigue, which is not conducive to Patient breathing.39 HFNC can provide heated and humidified oxygen, sufficient oxygen flow and positive end-expiratory pressure, which can limit the inflammatory response and bronchial epithelial cell damage, reduce the body’s hyperresponsiveness or irritation, promote the improvement of the airway, and effectively flush the airway, promote the recovery of respiratory ciliary function, effectively remove excess carbon dioxide in the body, promote pulmonary gas exchange, improve oxygen utilization, improve patient ventilation function, and reduce respiratory power consumption, thereby helping to improve diaphragm fatigue and reduce diaphragm damage.40–43 In the analysis of mortality, ICU length of stay, PaCO2, pH, HR, PaO2/FiO2, there was no statistical difference between HFNC and NIV, showing the treatment effect is equivalent.
Recent studies have shown that compared with HFNC alone, extubation Immediately applied HFNC plus NIV significantly reduced the risk of reintubation and post-extubation respiratory failure in patients at high risk of extubation failure.44 The result may provide further insight into the choice of respiratory support methods after extubation, and provide a possibility for the combined and alternate application of HFNC and NIV in the future.
In general, According to the available evidence, the application of HFNC can be used as a treatment option for AECOPD patients with hypercapnia. It has certain advantages as an alternative to NIV after extubation, but in AECOPD patients without hypercapnia, HFNC is not as effective as NIV, the result needs further evaluation.
Limitations
The limitations of this study are as follows: firstly, the number of included studies is relatively small, with a total of 8 articles involving 612 subjects (297 in the HFNC group and 315 in the NIV group). secondly, the quality of the included studies is generally not high. Because of differences in oxygen therapy equipment, it is difficult to blind study patients and interventionists, which may affect the estimation of outcome measures. Thirdly, all included studies have given the judgment criteria for failure of HFNC or NIV treatment are different, may affect the results. Fourthly, a total of 8 studies included, seven of which are from China, may have regional differences and cannot be used as evidence of globalization. High-quality, multi-center RCT studies worldwide are still needed to further evaluate the effect of HFNC in patients after extubation of AECOPD. In conclusion, the results of the study should be interpreted with caution.
Conclusion
According to the Meta-analysis results of the existing evidence, the application of HFNC can be used as an alternative treatment for NIV after extubation in AECOPD patients with hypercapnia, and there are certain advantages, but whether HFNC can be used as an alternative treatment for NIV in AECOPD patients without hypercapnia after extubation still needs to be further studied. In the future, more high-quality, multicenter RCT studies are still needed to further verify the effect of HFNC in patients after extubation of AECOPD.
Funding Statement
There is no funding to report.
Consent for Publication
All authors agree that all the details of the article and the image to be published in this article can be presented. If necessary, all authors can provide a copy of the signed consent to the editorial department of the journal.
Author Contributions
All authors have made significant contributions to the work of the report, whether in terms of concept, research design, implementation, data acquisition, analysis and interpretation, or in all these areas; Participate in the drafting, modification or critical review of the clause; Final approval of the forthcoming edition; An agreement has been reached on the journal to submit the article; And agree to be responsible for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Vogelmeier CF, Criner GJ, Martinez FJ., et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–582. doi: 10.1164/rccm.201701-0218PP [DOI] [PubMed] [Google Scholar]
- 2.Augusti A, Beasley R, Celli BR, et al. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnoses, management, and prevention of COPD; 2020. Available from: http://www.goldcopd.org. Accessed May 27, 2021.
- 3.Osadnik CR, Tee VS, Carson-Chahhoud KV, Picot J, Wedzicha JA, Smith BJ. Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;7(7):CD004104. doi: 10.1002/14651858.CD004104.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kunadharaju R, Sethi S. Treatment of acute exacerbations in chronic obstructive pulmonary disease. Clin Chest Med. 2020;41(3):439–451. doi: 10.1016/j.ccm.2020.06.008 [DOI] [PubMed] [Google Scholar]
- 5.Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi: 10.1183/13993003.02426-2016 [DOI] [PubMed] [Google Scholar]
- 6.Gong Y, Sankari A. Noninvasive Ventilation. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 7.Hill NS, Brennan J, Garpestad E, Nava S. Nava, Stefano MD Noninvasive ventilation in acute respiratory failure. Crit Care Med. 2007;35(10):2402–2407. doi: 10.1097/01.CCM.0000284587.36541.7F [DOI] [PubMed] [Google Scholar]
- 8.Ambrosino N, Vagheggini G. Noninvasive positive pressure ventilation in the acute care setting: whereare we? Eur Respir J. 2008;31(4):874–886. doi: 10.1183/09031936.00143507 [DOI] [PubMed] [Google Scholar]
- 9.Karen E, et al. Non-invasive ventilation versus invasive weaning in critically ill adults: a systematic review and meta-analysis. Thorax. 2021;2021:216993. doi: 10.1136/thoraxjnl-2021-216993 [DOI] [PubMed] [Google Scholar]
- 10.Frat J-P, Brugiere B, Ragot S, et al. Sequential application of oxygen therapy via high-flow nasal cannula and noninvasive ventilation in acute respiratory failure: an observational pilot study. Respir Care. 2015;60(2):170–178. doi: 10.4187/respcare.03075 [DOI] [PubMed] [Google Scholar]
- 11.Möller W, Feng S, Domanski U, et al. Nasal high flow reduces dead space. J Appl Physiol. 2017;122(1):191–197. doi: 10.1152/japplphysiol.00584.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cortegiani A, Longhini F, Madotto F, et al. High flow nasal therapy versus noninvasive ventilation as initial ventilatory strategy in COPD exacerbation: a multicenter non-inferiority randomized trial. Critical Care. 2020;24(1):692. doi: 10.1186/s13054-020-03409-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu Z, Zhu L, Zhan J, et al. The efficacy and safety of high-flow nasal cannula therapy in patients with COPD and type II respiratory failure: a meta-analysis and systematic review. Eur J Med Res. 2021;26(1):122. doi: 10.1186/s40001-021-00587-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins JPT, Thomas J, Chandler J, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd. Chichester (UK): John Wiley & Sons; 2019. http://www.cochrane-handbook.org. Accessed August 26, 2022. [Google Scholar]
- 15.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:160. doi: 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP, Altman DG, Gøtzsche PC, et al.; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang JC, Wu FX, Meng LL, Zeng CY, Lu YQ. [A study on the effects and safety of sequential humidified high flow nasal cannula oxygenation therapy on the COPD patients after extubation].. Zhonghua Yi Xue Za Zhi. 2018;98(2):109–112. doi: 10.3760/cma.j.issn.0376-2491.2018.02.007 [DOI] [PubMed] [Google Scholar]
- 18.Yu ZH, Zhang R, Huang H, Li J, Geng S. Efficacy and safety of humidified high flow nasal cannula in chronic obstructive pulmonary disease complicated with type 2 respiratory failure patients after extubation: a randomized controlled trial. Acad j Second Military Med Univ. 2019;40(9):989‐994. doi: 10.16781/j.0258-879x.2019.09.0989 [DOI] [Google Scholar]
- 19.Jing G, Li J, Hao D, et al. Comparison of high flow nasal cannula with noninvasive ventilation in chronic obstructive pulmonary disease patients with hypercapnia in preventing postextubation respiratory failure: a pilot randomized controlled trial. Res Nurs Health. 2019;42(3):217–225. doi: 10.1002/nur.21942 [DOI] [PubMed] [Google Scholar]
- 20.Yang SQ, Liu Z, Meng SQ, et al. [Application value of non-invasive ventilation combined with high flow nasal cannula oxygen therapy in sequential treatment of patients with chronic obstructive pulmonary disease after mechanical ventilation]. Zhonghua Yi Xue Za Zhi. 2020;100(27):2116–2120. Chinese. doi: 10.3760/cma.j.cn112137-20200306-00616 [DOI] [PubMed] [Google Scholar]
- 21.Thille AW, Coudroy R, Nay MA, et al. Non-invasive ventilation alternating with high-flow nasal oxygen versus high-flow nasal oxygen alone after extubation in COPD patients: a post hoc analysis of a randomized controlled trial. Ann Intensive Care. 2021;11(1):30. doi: 10.1186/s13613-021-00823-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu S, Liu X. Sequential treatment of chronic obstructive pulmonary disease concurrent with respiratory failure by high-flow nasal cannula therapy. Am J Transl Res. 2021;13(4):2831–2839. [PMC free article] [PubMed] [Google Scholar]
- 23.Fang G, Wan Q, Tian Y, et al. [Comparative study on pros and cons of sequential high-flow nasal cannula and non-invasive positive pressure ventilation immediately following early extubated patients with severe respiratory failure due to acute exacerbations of chronic obstructive pulmonary disease]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2021;33(10):1215–1220. Chinese. doi: 10.3760/cma.j.cn121430-20210623-00939 [DOI] [PubMed] [Google Scholar]
- 24.Tan D, Walline JH, Ling B, et al. High-flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease patients after extubation: a multicenter, randomized controlled trial. Crit Care. 2020;24(1):489doi: 10.1186/s13054-020-03214-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ouanes-Besbes L, Ouanes I, Dachraoui F, Dimassi S, Mebazaa A, Abroug F. Weaning difficult-to-wean chronic obstructive pulmonary disease patients: a pilot study comparing initial hemodynamic effects of levosimendan and dobutamine. J Crit Care. 2011;26(1):15–21. doi: 10.1016/j.jcrc.2010.01.002 [DOI] [PubMed] [Google Scholar]
- 26.Lindenauer PK, Stefan MS, Shieh MS, Pekow PS, Rothberg MB, Hill NS. Outcomes associated with invasive and noninvasive ventilation among patients hospitalized with exacerbations of chronic obstructive pulmonary disease. JAMA Intern Med. 2014;174(12):1982–1993. doi: 10.1001/jamainternmed.2014.5430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferrer M, Valencia M, Nicolas JM, Bernadich O, Badia JR, Torres A. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med. 2006;173(2):164–170. doi: 10.1164/rccm.200505-718OC [DOI] [PubMed] [Google Scholar]
- 28.Riera J, Pérez P, Cortés J, Roca O, Masclans JR, Rello J. Effect of high-flow nasal cannula and body position on end-expiratory lung volume: a cohort study using electrical impedance tomography. Respir Care. 2013;58(4):589–596. doi: 10.4187/respcare.02086 [DOI] [PubMed] [Google Scholar]
- 29.Chidekel A, Zhu Y, Wang J, Mosko JJ, Rodriguez E, Shaffer TH. The effects of gas humidification with high-flow nasal cannula on cultured human airway epithelial cells. Pulm Med. 2012;2012:380686. doi: 10.1155/2012/380686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chanques G, Constantin JM, Sauter M, et al. Discomfort associated with underhumidified high-flow oxygen therapy in critically ill patients. Intensive Care Med. 2009;35(6):996–1003. doi: 10.1007/s00134-009-1456-x [DOI] [PubMed] [Google Scholar]
- 31.Hernández G, Vaquero C, González P, et al. Effect of Postextubation High-Flow Nasal Cannula vs Conventional Oxygen Therapy on Reintubation in Low-Risk Patients: a Randomized Clinical Trial. JAMA. 2016;315(13):1354–1361. doi: 10.1001/jama.2016.2711 [DOI] [PubMed] [Google Scholar]
- 32.Lee MK, Choi J, Park B, et al. High flow nasal cannulae oxygen therapy in acute-moderate hypercapnic respiratory failure. Clin Respir J. 2018;12(6):2046–2056. doi: 10.1111/crj.12772 [DOI] [PubMed] [Google Scholar]
- 33.Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am J Respir Crit Care Med. 2019;199(11):1368–1376. doi: 10.1164/rccm.201803-0589OC [DOI] [PubMed] [Google Scholar]
- 34.Karim HMR, Bharadwaj A, Mohammed Mujahid O. Relationship of ROX and Modified ROX index with High Flow Nasal Cannula Oxygen therapy in COVID-19 patients: an observational, pilot study. J Am Osteopath Assoc. 2022. doi: 10.21203/rs.3.rs-1680854/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karim HMR, Esquinas AM. Success or Failure of High-Flow Nasal Oxygen Therapy: the ROX Index Is Good, but a Modified ROX Index May Be Better. Am J Respir Crit Care Med. 2019;200(1):116–117. doi: 10.1164/rccm.201902-0419LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duan J, Han X, Bai L, et al. Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients. Intensive Care Med. 2017;43(2):192–199. doi: 10.1007/s00134-016-4601-3 [DOI] [PubMed] [Google Scholar]
- 37.Longhini F, Pan C, Xie J, et al. New setting of neurally adjusted ventilatory assist for noninvasive ventilation by facial mask: a physiologic study. Crit Care. 2017;21(1):170. doi: 10.1186/s13054-017-1761-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bruni A, Garofalo E, Pelaia C, et al. Patient-ventilator asynchrony in adult critically ill patients. Minerva Anestesiol. 2019;85(6):676–688. doi: 10.23736/S0375-9393.19.13436-0 [DOI] [PubMed] [Google Scholar]
- 39.Elshof J, Duiverman ML. Clinical evidence of nasal high-flow therapy in chronic obstructive pulmonary disease patients. Respiration. 2020;99(2):140–153. doi: 10.1159/000505583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raza HA, Nokes B, Wesselius L, Long-Term Oxygen AN. Therapy in patients with chronic obstructive pulmonary disease and moderate hypoxemia. J Am Osteopath Assoc. 2018;118(10):663–665. doi: 10.7556/jaoa.2018.145 [DOI] [PubMed] [Google Scholar]
- 41.Jiang M, Song JJ, Guo XL, Tang YL, Li HB. Airway Humidification Reduces the Inflammatory Response During Mechanical Ventilation. Respir Care. 2015;60(12):1720–1728. doi: 10.4187/respcare.03640 [DOI] [PubMed] [Google Scholar]
- 42.Rittayamai N, Phuangchoei P, Tscheikuna J, Praphruetkit N, Brochard L. Effects of high-flow nasal cannula and non-invasive ventilation on inspiratory effort in hypercapnic patients with chronic obstructive pulmonary disease: a preliminary study. Ann Intensive Care. 2019;9(1):122. doi: 10.1186/s13613-019-0597-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jacobs SS, Krishnan JA, Lederer DJ, et al. Home Oxygen Therapy for Adults with Chronic Lung Disease. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(10):e121–e141. doi: 10.1164/rccm.202009-3608ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sang L, Nong L, Zheng Y, et al. Effect of high-flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation for preventing reintubation: a Bayesian network meta-analysis and systematic review. J Thorac Dis. 2020;12(7):3725–3736. doi: 10.21037/jtd-20-1050 [DOI] [PMC free article] [PubMed] [Google Scholar]