Abstract
Introduction
Unvaccinated older adults with COVID-19 are at higher risk for severe illness and complications compared with those have been vaccinated. Vaccine literacy and attitudes are important factors that enhance healthy behaviors and choices, including vaccination intention.
Objective
To explore vaccine literacy, attitudes, and vaccination intention toward COVID-19 among Thai older adults and examine associations between vaccine literacy, attitudes, and vaccination intention.
Methods
This study used a cross-sectional online design. We surveyed 408 older adults who met our inclusion criteria. Participants were recruited online via social media and websites. The survey covered demographic data, vaccine literacy, attitudes, and intention to get the COVID-19 vaccine.
Results
COVID-19 vaccination intention among Thai older adults was high (81.3%). Females and those aged 60–69 years had higher COVID-19 vaccine literacy scores than males (t = −2.120, p < 0.05) and those aged ≥70 years (t = 2.438, p < 0.05). Participants with postgraduate education and those who were health professionals scored higher for vaccine literacy than less educated (t = −3.501, p < 0.01) and non-health professional (t = 5.437, p < 0.001) participants. Those with an adequate income or that had been vaccinated against COVID-19 scored significantly higher for vaccine literacy and attitudes toward the COVID-19 vaccine than participants with an inadequate income (t = 4.626, p < 0.001) or that had not been vaccinated (t = 2.842, p < 0.01). Vaccine literacy (r = 0.219, p < 0.001) and attitudes (r = 0.459, p < 0.001) were significantly associated with vaccination intention.
Conclusion
COVID-19 vaccine literacy and attitudes are significant factors related to vaccination intention. Health professionals could play an important role in enhancing vaccine literacy among older adults. Positive attitudes and COVID-19 vaccine literacy may enhance vaccination uptake in older adults.
Keywords: vaccine literacy, attitudes, vaccination intention, COVID-19, older adults
Introduction
COVID-19 vaccination has an important role in mitigating the transmission and severity of COVID-19. Vaccination showed 50% efficacy in reducing the incidence of COVID-191 and limiting the disease trajectory.2 Older adults are at high risk for mortality from COVID-19. In March 2020, the Centers for Disease Control and Prevention (CDC) reported that 80% of deaths among patients with COVID-19 occurred in those aged ≥60 years.3 In addition, a 10-year increase in age was significantly associated with increased mortality.4 The death rate in those aged ≥85 years was 330 times higher compared with those aged 18–29 years.5 Case fatality rates also increased with age; that is, from 1% to 3% in patients aged 55–64 years, from 3% to 11% in those aged 65–84 years, and from 10% to 27% in those aged ≥85 years.3 The mortality rate in Thailand was 3.7% in patients aged 60–69 years and 12.1% in those aged ≥70 years.6
The CDC reported that the percentage of hospitalization and intensive care unit (ICU) admissions for older adults with COVID-19 in 2020 increased with increasing age,3 especially for those aged ≥70 years.7 The highest rate of hospitalization was in patients aged ≥85 years (70.3%) compared with those aged 45–55 years (28.3%)6 and was 10 times higher compared with those aged 18–29 years.5 A narrative review of 19 studies conducted in North America, Europe, and Asia among older patients with COVID-19 admitted to the ICU showed the rates of ICU admission in patients aged ≥60 years varied, with the highest rate being 79.6% and the highest ICU mortality rate being 91%.8 Therefore, older adults should be prioritized in receiving COVID-19 vaccination to reduce mortality and morbidity.
The effectiveness of COVID-19 vaccines is evidenced in terms of minimizing severe illness, hospitalization, and deaths due to COVID-19,9 especially among older adults.10,11 The COVID-19 vaccination program in Thailand began in March 2021. It started with frontline healthcare workers, followed by older adults aged ≥60 years and other high-risk groups. The Oxford-Astra Zeneca vaccine was the first available vaccine to be given to older adults aged ≥60 years. To receive vaccination, the target population was invited to register via an official COVID-19 vaccine application. However, some older adults were hesitant or refused to get vaccinated and did not register for the vaccine program. Vaccine hesitancy led to lower vaccination rates and was a substantial obstacle to achieving coverage and community immunity in the target population.12
Frequently-reported hesitancy factors related to the vaccine delivery program included underlying diseases and other barriers to COVID-19 vaccination among older adults. These barriers can be divided into structural- and attitude-related barriers.13 Common structural barriers included cost, time, transportation, and clinic location.13 Attitude-related barriers included individuals’ beliefs or perceptions that may have reduced their willingness to seek out or accept vaccination. Misinformation and misconceptions of vaccination because of lack of knowledge about COVID-19 vaccine and vaccine literacy could lead to negative attitudes. Negative attitudes about vaccines have a significant link to vaccine hesitancy14 whereas positive attitudes significantly increase vaccination intention.14–17 Attitudes toward COVID-19 vaccination remain one of the most important factors affecting vaccination intention.14–17
Health literacy is a key factor for enhancing healthy behaviors and choices. Previous studies on COVID-19 vaccination have shown that inadequate health or vaccine literacy was significantly associated with attitudes towards COVID-19 vaccination17–19 and an unwillingness to get vaccinated against COVID-19.15 In addition, vaccine literacy has been shown to be a significant factor that influences vaccination intention20 and reduces vaccine hesitancy.21,22 Recently, a COVID-19 vaccine literacy scale was developed to measure and assess a person’s ability to understand, appraise, and apply existing information about the COVID-19 vaccine to make an appropriate decision about vaccination.23,24 This highlighted that vaccine literacy is an essential factor affecting vaccination intention.14–17
Research about vaccine literacy, attitudes, and vaccination intention has not been conducted among older adults in Thailand in the context of the COVID-19 pandemic. Therefore, this study aimed to explore COVID-19 vaccine literacy, attitudes toward COVID-19 vaccination, and intention to receive the COVID-19 vaccine among Thai older adults. We also examined associations between COVID-19 vaccine literacy, attitudes, and vaccination intention. The findings of this study will provide information for health professionals to develop strategies to enhance acceptance of COVID-19 vaccination among older adults.
Materials and Methods
Study Design
A cross-sectional survey design was used to collect data about COVID-19 vaccine literacy, attitudes, and vaccination intention among older adults in Thailand between May and July 2021.
Study Sample
A convenience sample of older adults was recruited via online methods. The inclusion criteria were (1) aged ≥60 years, (2) ability to read and understand Thai, (3) access to a smartphone or tablet, and (4) willingness to participate in this study. The exclusion criterion was any physical, psychological, or anatomical impairment that would prevent interaction with a computer device.
The sample size was calculated using the G*power statistical program (version 3.9.1.4) to achieve power (1-β) of 0.80 and a 0.05 level of confidence.25 The effect size was determined based on prior research23 using the smallest correlation value of r = 0.140. Although the estimated sample size was 395, we increased the sample size by 5% to account for possible incomplete answers. In the final dataset, there were seven incomplete surveys, resulting in a total sample of 408 surveys from older adults included in the data analysis.
Data Collection and Instruments
Participants were recruited online via announcements about the study on websites, Facebook, a Line Group (https://line.me), and a Line application for individuals’ networks and community social groups. Messages inviting people to participate in this study containing a URL and a quick response code were circulated via these social media channels. The online survey was developed using Google Forms and data were automatically saved on Google Drive. The data were downloaded and placed in a Microsoft Excel file. The online survey covered participants’ demographic characteristics, COVID-19 vaccination status, vaccination intention, attitudes towards COVID-19 vaccination, and COVID-19 vaccine literacy.
Demographic Characteristics and Vaccination Status
The characteristics collected were: age, sex, marital status, education level, and income. Participants were also asked whether they were vaccinated, were health professionals, and if they had an underlying disease. In addition, participants were asked to respond to two questions: “Have you already received the COVID-19 vaccination?” (1 = Yes, 0 = No), and “Will you get the COVID-19 vaccine?” (1 = Will not get, 2 = Not sure, or 3 = Will get for sure). This scale was used in a previous study.26
Attitudes Toward COVID-19 Vaccination
Attitudes were measured using a 10-item scale developed by the researchers, responses to each item were on an ordinal 7-point Likert scale (from 1 = totally disagree to 7 = totally agree). There were five positively worded items and five negatively worded items. For example, “I think the COVID-19 vaccine is helpful” (positive) and “The COVID-19 vaccination can have adverse effects” (negative). Negatively worded items were reverse scored. Total scores ranged from 10 to 70 points, with higher scores indicating a more positive attitude toward COVID-19 vaccination. This scale was reviewed for face validity by experts in epidemiology, communicable diseases, and nursing. It was pilot tested and showed an acceptable Cronbach’s alpha coefficient (α = 0.706).
COVID-19 Vaccine Literacy
The COVID-19 Vaccine Literacy Scale was developed by Biasio et al23 with two dimensions: vaccine literacy functional skills (four items, negatively worded) and vaccine literacy interactive/critical skills (eight items, positively worded).The stem of the four items in the first dimension was, “When reading or listening to information about future COVID-19 vaccines or current vaccines: Did you … ? The stem of the eight items in the second dimension was, “When looking for information about future COVID-19 vaccines or current vaccines: Have you/Did you … ? Each of the 12 items had an ordinal 4-point response option (1 = Never, 2 = Rarely, 3 = Sometimes, and 4 = Often). Negatively worded items were reversed scored. Higher scores indicated an improved level of vaccine literacy. The scale was translated from English into the Thai language by Maneesriwongul et al26 using back-translation. The scale had acceptable subscale and overall internal consistency reliability: Cronbach’s alpha coefficients for vaccine literacy functional skills (α = 0.85), vaccine literacy interactive/critical skills (α = 0.86), and the overall scale (α = 0.81).
Ethical Considerations
This study was approved by the Committee on Human Rights Related to Research Involving Human Subjects, Faculty of Medicine Ramathibodi Hospital, Mahidol University (MURA2021/381, 2022/19). After reading the informed consent outlining the survey’s purpose, anonymity, and data confidentiality in accordance with the Declaration of Helsinki, eligible older adults indicated their willingness to participate by tapping on the online “Accept” button. They could complete the online survey in about 20 minutes in private and in their own time, and could exit the survey at any time.
Data Analysis
Frequencies, means, and percentages were calculated to assess participants’ demographic data, COVID-19 vaccine literacy, attitudes, and vaccination intention. Independent t-tests were used to examine differences between participants’ characteristics and attitudes and vaccine literacy. Pearson product-moment correlation and point biserial correlation tests were used to examine the relationships between vaccine literacy, attitudes, and vaccination intention. SPSS version 18.0 for Windows was used for the data analysis.
Results
Most participants (n = 340, 83.3%) were aged 60–69 years (Table 1). About half (51.7%) lived in Bangkok and 21% lived in the central region of Thailand. Most participants were female (n = 296, 72.5%), married (n = 222, 54.4%), had a postgraduate education (n = 202, 49.5%), were not healthcare professionals (n = 307, 75.2%), and had an adequate income (n = 373, 91.4%). Most participants reported having one or more underlying diseases: hypertension (n = 148, 36.3%), diabetes (n = 53, 13%), and cardiovascular disease (n = 33, 8.1%). Less than half of the participants had been vaccinated against COVID-19 (n = 184, 45.1%). Of those who had not been vaccinated, most accepted vaccines and intended to receive the COVID-19 vaccine (n = 182, 81.3%). Less than one-fifth of participants were hesitant to be vaccinated (n = 40, 17.8%) and two refused any vaccination.
Table 1.
Summary of the Characteristics of Participants (n = 408)
| Characteristics | n | Percentage |
|---|---|---|
| Age (range 60–89 years, M = 65.2, SD = 4.50) | ||
| Age range (years) | ||
| 60–64 | 226 | 55.4 |
| 65–69 | 114 | 27.9 |
| 70–74 | 55 | 13.5 |
| 75 up | 13 | 3.2 |
| Gender | ||
| Male | 112 | 27.5 |
| Female | 296 | 72.5 |
| Marital status | ||
| Single | 108 | 26.5 |
| Married | 222 | 54.4 |
| Widowed/divorced | 78 | 19.1 |
| Education | ||
| Primary level or lower | 21 | 5.1 |
| Secondary level or diploma | 44 | 10.8 |
| Bachelor’s degree | 141 | 34.6 |
| Postgraduate | 202 | 49.5 |
| Health professional | ||
| Yes | 101 | 24.8 |
| No | 307 | 75.2 |
| Income adequacy | ||
| Adequate | 373 | 91.4 |
| Inadequate | 35 | 8.6 |
| Underlying disease | ||
| Yes | 299 | 73.3 |
| No | 109 | 26.7 |
| Type of underlying disease (Multiple responses) | ||
| Hypertension | 148 | 36.3 |
| Diabetes | 53 | 13.0 |
| Cardiovascular disease (heart) | 33 | 8.1 |
| Obesity (BMI > 30 kg/m2) | 30 | 7.4 |
| Cancer | 16 | 3.9 |
| Neurovascular disease (Stroke) | 14 | 3.4 |
| Chronic respiratory disease | 11 | 2.7 |
| Vaccination against COVID-19 | ||
| Yes | 184 | 45.1 |
| No but accept | 182 | 44.6 |
| No but hesitate | 40 | 9.8 |
| No and refuse | 2 | 0.5 |
| Vaccination intention to get COVID-19 vaccine (n = 224) | ||
| Acceptance | 182 | 81.3 |
| Hesitancy | 40 | 17.8 |
| Refusing | 2 | 0.9 |
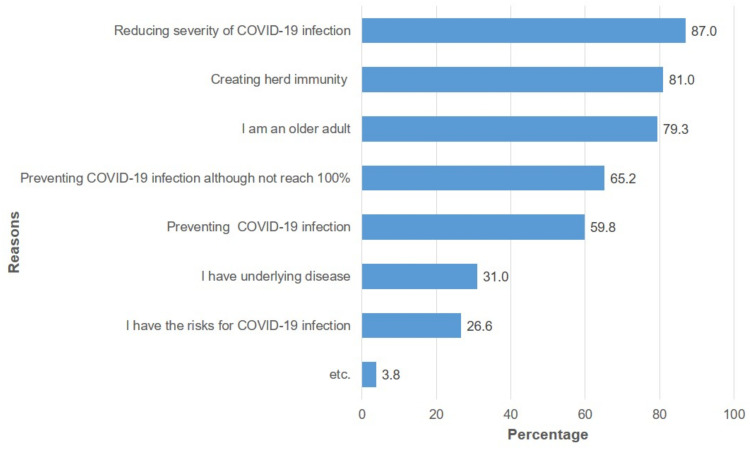
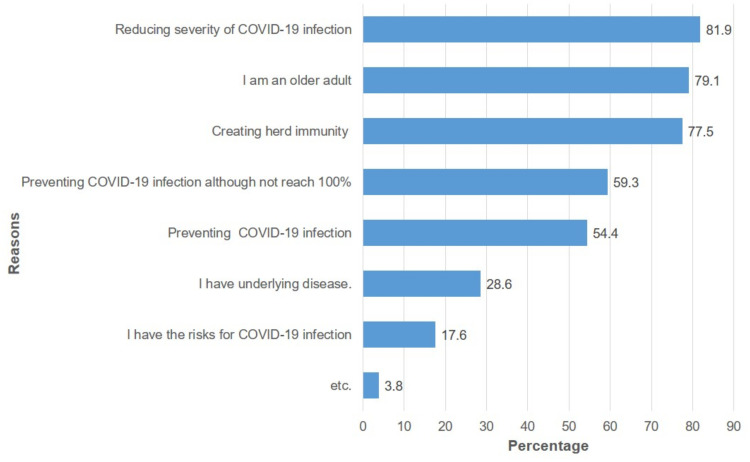
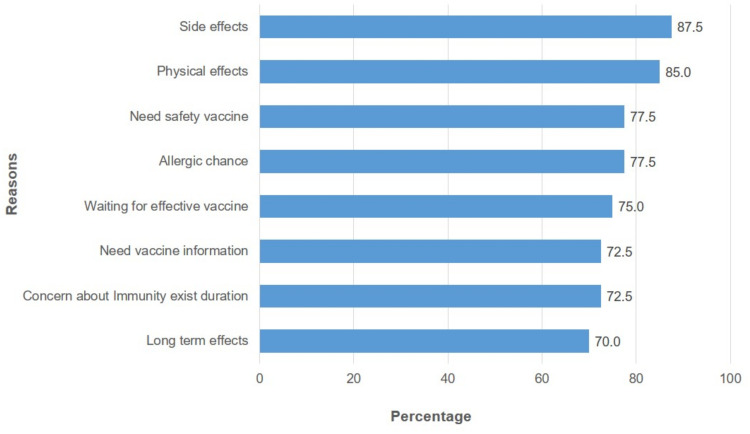
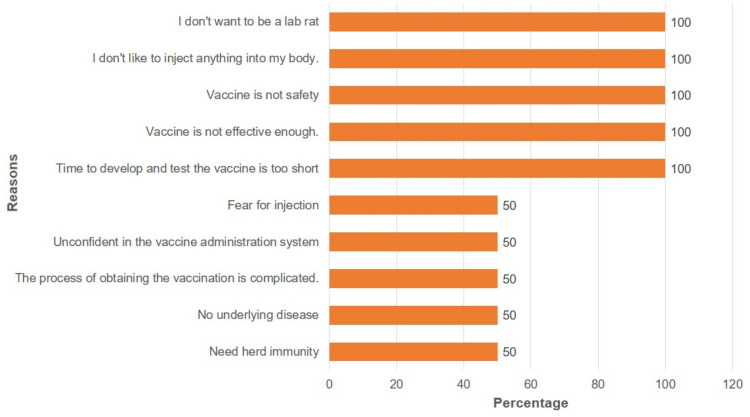
For participants who had already received the COVID-19 vaccine, the most common reasons for vaccine acceptance were that it would reduce the severity of the disease (n = 160, 87%), create herd immunity (n = 149, 81%), and reduce their perceived risk (n = 146, 79.3%) (Figure 1). Those who intended to get the COVID-19 vaccine reported similar reasons for vaccine acceptance in that it would reduce the severity of the disease (n = 149, 81.9%), reduce their perceived risk (n = 144, 79.1%), and create herd immunity (n = 141, 77.5%) (Figure 2). The main reasons participants were hesitant to be vaccinated were fears of potential side effects (n = 35, 87.5%), physical effects (n = 34, 85%), allergic reactions (n = 31, 77.5%), and vaccine safety (n = 31, 77.5%) (Figure 3). The two participants who refused vaccination reported they were concerned about the short vaccine development time and vaccine effectiveness and safety (Figure 4).
Figure 1.
Reasons for vaccination acceptance in vaccinated persons (n = 184).
Figure 2.
Reasons for vaccination acceptance in intentional persons (n = 182).
Figure 3.
Reasons for vaccination hesitancy (n = 40).
Figure 4.
Reasons for vaccination refusal (n = 2).
On average, participants reported means above the midpoints on the overall COVID-19 vaccine literacy (M = 3.19, SD = 0.44) and the two dimensions: functional literacy (M = 2.88, SD = 0.68) and interactive/critical literacy (M = 3.34, SD = 0.49). Females and those aged 60–69 years scored significantly higher on overall vaccine literacy than males (t = −2.120, p < 0.05) and participants aged ≥70 years (t = 2.438, p < 0.05) (Table 2). Participants with postgraduate education and those who were health professionals scored higher on overall vaccine literacy than those with less education (t = −3.501, p < 0.01) and non-health professionals (t = 5.437, p < 0.001). Similarly, participants reported means above the midpoints on their attitudes toward the COVID-19 vaccine (M = 4.9, SD = 0.83). Participants who reported an adequate income or had been vaccinated against COVID-19 scored significantly higher for attitudes about the COVID-19 vaccine than those who reported an inadequate income (t = 4.626, p < 0.001) or had not been vaccinated (t = 2.842, p < 0.01).
Table 2.
Differences Between Participants’ Characteristics by Groups on Vaccine Literacy and Attitudes (n = 408)
| Characteristics | Vaccine Literacy | Attitudes | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | Mean (SD) | t | P-value | Mean (SD) | t | P-value | |
| Age range | ||||||||
| 60–69 | 340 | 83.3 | 3.21 (0.44) | 2.438 | 0.015* | 4.89 (0.84) | −0.796 | 0.112 |
| 70+ | 68 | 16.7 | 3.07 (0.43) | 5.07 (0.76) | ||||
| Gender | ||||||||
| Male | 112 | 27.5 | 3.11 (0.45) | −2.120 | 0.035* | 4.96 (0.86) | 0.624 | 0.533 |
| Female | 296 | 72.5 | 3.22 (0.43) | 4.92 (0.82) | ||||
| Education | ||||||||
| Bachelor or lower | 141 | 34.6 | 3.15 (0.43) | −3.501 | <0.01* | 4.89 (0.83) | −1.073 | 0.284 |
| Postgraduate | 202 | 49.5 | 3.30 (0.39) | 4.98 (0.76) | ||||
| Health professional | ||||||||
| Yes | 101 | 75.2 | 3.39 (0.42) | 5.437 | <0.001* | 4.89 (0.69) | −0.548 | 0.584 |
| No | 307 | 24.8 | 3.12 (0.43) | 4.93 (0.88) | ||||
| Income adequacy | ||||||||
| Adequate | 373 | 91.4 | 3.20 (0.44) | 1.879 | 0.061 | 4.98 (0.80) | 4.626 | <0.001* |
| Inadequate | 35 | 8.6 | 3.05 (0.39) | 4.32 (0.89) | ||||
| Underlying disease | ||||||||
| Yes | 299 | 73.3 | 3.17 (0.45) | −1.285 | 0.200 | 4.89 (0.82) | −1.449 | 0.148 |
| No | 109 | 26.7 | 3.23 (0.41) | 5.02 (0.85) | ||||
| Vaccination | ||||||||
| Yes | 184 | 45.1 | 3.22 (0.42) | 1.504 | 0.133 | 5.05 (0.72) | 2.842 | 0.005* |
| No | 224 | 54.9 | 3.16 (0.45) | 4.82 (0.91) | ||||
Note: *Significant if p-value < 0.05.
Participants who reported having a positive attitude toward the COVID-19 vaccines recognized the benefits of vaccination and how it minimized the severity of the disease. They trusted health professionals. Conversely, participants with negative attitudes toward the vaccines were concerned about their potential side effects and life-threatening problems. They also thought other prevention choices were better than vaccination. COVID-19 vaccine literacy was significantly and positively associated with participants’ attitudes about the vaccines (r = 0.344, p < 0.001) and their vaccination intention (r = 0.219, p < 0.001) (Table 3). Vaccine attitudes were also significantly and positively associated with vaccination intention (r = 0.459, p < 0.001).
Table 3.
Correlations Between COVID-19 Vaccine Literacy, Attitudes Toward COVID-19 Vaccine, and Vaccination Intention to Get COVID-19 Vaccine Among Persons Not Vaccinated (n = 224)
| Variables | Vaccine Literacy | Attitudesa | Vaccination Intentionb |
|---|---|---|---|
| COVID-19 Vaccine Literacy | 1 | 0.344* | 0.219* |
| Attitudes toward COVID-19 | 1 | 0.459* | |
| Vaccination Intention to get COVID-19 vaccine | 1 |
Note: *Significant if p-value < 0.01, aPearson product-moment correlation test, bPoint biserial correlation test.
Discussion
COVID-19 vaccine functional and interactive/critical literacy among older adults in Thailand were similar to those reported in Italy, with the Thai mean scores falling within the Italian study’s 95% confidence intervals.23 Our result that Thai older adults aged under 70 years had higher vaccine literacy was consistent with results reported for Chinese adults.27 In both cultures, families and peers may play an important role in motivating adults and older adults to receive vaccination,28 but this could be less influential among older adults aged ≥70 years. COVID-19 vaccine literacy was also improved in Thai older adults who had postgraduate degrees. Educational level has been associated with both vaccine literacy23,27 and health literacy.18
We found that participating Thai older adults that were health professionals scored higher on vaccine literacy than non-health professionals. Thai female older adults also had a higher mean score for COVID-19 vaccine literacy than males, which was consistent with previous study from Asia that reported similar results.27 However, the study from Italy showed that Italian females’ mean scores on vaccine literacy were lower than males, although their median scores were identical.23
The COVID-19 vaccination intention among Thai older adults (81.3%) was similar to that reported in a general population survey conducted in Southeast Asia (83.5%)29 but higher than the responses to a multi-country survey (71.3%).30 Other studies of vaccination intention specific to older adults showed intention rates varied widely from 52.7% to 91.3%.31–33 The responses given for vaccination intention among Thai older adults may have been because this study was conducted during the third wave of the COVID-19 pandemic when the incidence of COVID-19 and mortality were increasing, particularly among older adults. As the perception of the severity of COVID-19 infection worsened, vaccination intention increased. This was congruent with what has been reported elsewhere.34 The reasons for vaccination hesitancy given by Thai older adults (potential side effects and vaccine safety) were also the most common reasons for the unwillingness to get vaccinated reported in other studies.28,31,35–37 In addition, lack of trust in COVID-19 vaccines and concern about side effects were voiced by respondents in another study.27
The scores for attitudes toward COVID-19 vaccine among Thai older adults who perceived they had an adequate income were higher than those with a perceived inadequate income. Similar results for household income associated with positive attitudes towards COVID-19 have previously been reported.17,18 Older adults with a perceived adequate income may have greater opportunities to access more information about the COVID-19 vaccine, resulting in a more favorable attitude. Our results that Thai older adults who either received the COVID-19 vaccination or were accepting of the vaccination had more positive attitudes than their non-vaccinated or non-accepting counterparts were consistent with other studies.14,16,38
We found significant relationships between COVID-19 vaccine literacy, attitudes toward vaccines, and COVID-19 vaccination intention. Other studies found similar connections, such as (1) between attitudes toward vaccination intention14,16,38,39 and vaccine hesitancy,14,39 and (2) between COVID-19 vaccine literacy, vaccination intention,20 and vaccine acceptance and uptake.24 Older adults with a high level of vaccine literacy were less likely to have COVID-19 vaccine hesitancy.22 Conversely, inadequate vaccine literacy was associated with a reluctance to get COVID-19 vaccination.15
This cross-sectional study had some limitations. The online data collection might have produced some bias. The method of recruitment might also have facilitated responses from participants who may have been similar to the researchers. Not only were the participants better educated than the general Thai population, but the number of health professionals was disproportionately high. However, the self-selection of participants and the cross-sectional design do not negate the results but provide context to this study. Results may change with a larger sample and as the pandemic enters into different phases.
Conclusion and Recommendations
Older adults in this study reported high level of vaccination and vaccination intention. COVID-19 vaccine literacy and attitudes are significant factors related to vaccination intention. Side effects of vaccines and vaccine safety remain major concerns among older adults in Thailand, especially among the group with vaccine hesitancy. The older adult population should be targeted for improving COVID-19 vaccine literacy, particularly those aged ≥70 years and who are less educated. These findings provide essential insights for policy makers to design effective communications with vulnerable groups about vaccine safety so that they understand that the benefits of COVID-19 vaccine outweigh the possible risks. Health professionals could play an important role in enhancing vaccine literacy among older adults. Positive attitudes and COVID-19 vaccine literacy can enhance vaccination uptake in older adults.
Acknowledgments
The researchers would like to thank the older adults who participated in this study. We also extend our appreciation for the research facilities provided by the Ramathibodi School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Thailand.
Funding Statement
There is no funding to report.
Ethics Approval and Informed Consent
This study was approved by the Committee on Human Rights Related to Research Involving Human Subjects, Faculty of Medicine Ramathibodi Hospital, Mahidol University (MURA2021/381, 2022/19). Consent to participate was obtained from all participants.
Disclosure
The authors report no conflicts of interest related to this research study.
References
- 1.Krause P, Fleming TR, Longini I, et al. COVID-19 vaccine trials should seek worthwhile efficacy. Lancet. 2020;396(10253):741–743. doi: 10.1016/S0140-6736(20)31821-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teo SP. Review of COVID-19 vaccines and their evidence in older adults. Ann Geriatr Med Res. 2021;25(1):4–9. doi: 10.4235/agmr.21.0011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bialek S, Boundy E, Bowen V; Centers for Disease Control and Prevention. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grasselli G, Greco M, Zanella A, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180(10):1345–1355. doi: 10.1001/jamainternmed.2020.3539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Age group rate ratios compared to ages 18 to 29 years; 2021. Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html. Accessed August 17, 2022.
- 6.World Health Organization. Coronavirus disease 2019 (COVID19): WHO Thailand situation report; 2020. Available from: https://www.who.int/docs/default-source/searo/thailand/2020-04-28-tha-sitrep-66-covid19-en.pdf?sfvrsn=328a4910_2. Accessed July 19, 2022.
- 7.Cardoso FS, Borges A, Botelho I, et al. Access to intensive care unit care for elderly patients with COVID-19 in Portugal. Port J Public Health. 2020;38(2):91–93. doi: 10.1159/000511150 [DOI] [Google Scholar]
- 8.Gkoufa A, Maneta E, Ntoumas GN, et al. Elderly adults with COVID-19 admitted to intensive care unit: a narrative review. World J Crit Care Med. 2021;10(5):278–289. doi: 10.5492/wjccm.v10.i5.278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohammed I, Nauman A, Paul P, et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: a systematic review. Hum Vaccin Immunother. 2022;18(1):2027160. doi: 10.1080/21645515.2022.2027160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moline HL, Whitaker M, Deng L, et al. Effectiveness of COVID-19 vaccines in preventing hospitalization among adults aged ≥65 years — COVID-NET, 13 States, February–April 2021. Morb Mortal Wkly Rep. 2021;70:1088–1093. doi: 10.15585/mmwr.mm7032e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373:n1088. doi: 10.1136/bmj.n1088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2). doi: 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gonzales A, Lee EC, Grigorescu V, Smith SR, De Lew N, Sommers BD. Overview of barriers and facilitators in COVID-19 vaccine outreach; 2021. Available from: https://aspe.hhs.gov/sites/default/files/2021-09/vaccine-outreach-research-report-sept-release.pdf. Accessed July 19, 2022.
- 14.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine. Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dodd RH, Cvejic E, Bonner C, et al. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21(3):318–319. doi: 10.1016/S1473-3099(20)30559-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graffigna G, Palamenghi L, Boccia S, Barello S. Relationship between citizens’ health engagement and intention to take the COVID-19 vaccine in Italy: a mediation analysis. Vaccines. 2020;8(4):576. doi: 10.3390/vaccines8040576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kadoya Y, Watanapongvanich S, Yuktadatta P, Putthinun P, Lartey ST, Khan MSR. Willing or hesitant? A socioeconomic study on the potential acceptance of COVID-19 vaccine in Japan. Int J Environ Res Public Health. 2021;18(9):4864. doi: 10.3390/ijerph18094864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.An L, Bacon E, Hawley S, et al. Relationship between coronavirus-related eHealth literacy and COVID-19 knowledge, attitudes, and practices among US adults: web-based survey study. J Med Internet Res. 2021;23(3):e25042–e25042. doi: 10.2196/25042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Motoki K, Saito T, Takano Y. Scientific literacy linked to attitudes toward COVID-19 vaccinations: a pre-registered study. Brief research report. Front commun. 2021;6. doi: 10.3389/fcomm.2021.707391 [DOI] [Google Scholar]
- 20.Carmosino E, Ruisinger JF, Kinsey JD, Melton BL. Vaccination approval literacy and its effects on intention to receive future COVID-19 immunization. J Am Pharm Assoc. 2022;62(4):1374–1378.e2. doi: 10.1016/j.japh.2022.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magon A, Arrigoni C, Graffigna G, et al. The effect of health literacy on vaccine hesitancy among Italian anticoagulated population during COVID-19 pandemic: the moderating role of health engagement. Hum Vaccin Immunother. 2021;17(12):5007–5012. doi: 10.1080/21645515.2021.1984123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang H, Li Y, Peng S, Jiang Y, Jin H, Zhang F. The effect of health literacy on COVID-19 vaccine hesitancy: the moderating role of stress. medRxiv. 2021;2021. doi: 10.1101/2021.06.16.21258808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biasio LR, Bonaccorsi G, Lorini C, Pecorelli S. Assessing COVID-19 vaccine literacy: a preliminary online survey. Hum Vaccin Immunother. 2021;17(5):1304–1312. doi: 10.1080/21645515.2020.1829315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Michel J-P, Goldberg J. Education, healthy ageing and vaccine literacy. J Nutr Health Aging. 2021;25(5):698–701. doi: 10.1007/s12603-021-1627-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen J. Statistical Power Analysis for Behavioral Sciences. 2nd ed. New York: Routledge; 1988. [Google Scholar]
- 26.Maneesriwongul W, Butsing N, Visudtibhan PJ, Leelacharas S, Kittipimpanon K. Translation and psychometric testing of the Thai COVID-19 Vaccine Literacy Scale. Pac Rim Int J Nurs Res. 2021;26(1):175–186. [Google Scholar]
- 27.Zhang F, Or PP-L, Chung JW-Y. The effects of health literacy in influenza vaccination competencies among community-dwelling older adults in Hong Kong. BMC Geriatr. 2020;20(1):103. doi: 10.1186/s12877-020-1504-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siu JY, Cao Y, Shum DHK. Perceptions of and hesitancy toward COVID-19 vaccination in older Chinese adults in Hong Kong: a qualitative study. BMC Geriatr. 2022;22(1):288. doi: 10.1186/s12877-022-03000-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong LP, Alias H, Danaee M, et al. COVID-19 vaccination intention and vaccine characteristics influencing vaccination acceptance: a global survey of 17 countries. Infect Dis Poverty. 2021;10(1):122. doi: 10.1186/s40249-021-00900-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhagianadh D, Arora K. COVID-19Vaccine hesitancy among community-dwelling older adults: the role of information sources. J Appl Gerontol. 2021;07334648211037507. doi: 10.1177/07334648211037507 [DOI] [PubMed] [Google Scholar]
- 32.Nikolovski J, Koldijk M, Weverling GJ, et al. Factors indicating intention to vaccinate with a COVID-19 vaccine among older U.S. adults. PLoS One. 2021;16(5):e0251963. doi: 10.1371/journal.pone.0251963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ren J, Zheng Y, Luo Y, Li M, Xie R, Zhang D. Hesitancy towards COVID-19 vaccine among older people in Luzhou, China: a cross-sectional study. EuropePMC. 2021. Preprint in English. doi: 10.21203/rs.3.rs-757239/v1 [DOI] [Google Scholar]
- 34.Zampetakis LA, Melas C. The health belief model predicts vaccination intentions against COVID-19: a survey experiment approach. Appl Psychol Health Well Being. 2021;13(2):469–484. doi: 10.1111/aphw.12262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asadi Faezi N, Gholizadeh P, Sanogo M, et al. Peoples’ attitude toward COVID-19 vaccine, acceptance, and social trust among African and Middle East countries. Health Promot Perspect. 2021;11(2):171–178. doi: 10.34172/hpp.2021.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pogue K, Jensen JL, Stancil CK, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines. 2020;8(4):582. doi: 10.3390/vaccines8040582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Syed Alwi SAR, Rafidah E, Zurraini A, Juslina O, Brohi IB, Lukas S. A survey on COVID-19 vaccine acceptance and concern among Malaysians. BMC Public Health. 2021;21(1):1129. doi: 10.1186/s12889-021-11071-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Callow MA, Callow DD. Older adults’ behavior intentions once a COVID-19 vaccine becomes available. J Appl Gerontol. 2021;40(9):943–952. doi: 10.1177/07334648211019205 [DOI] [PubMed] [Google Scholar]
- 39.Guidry JPD, Laestadius LI, Vraga EK, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]