ABSTRACT
Hypertension and diabetes are modifiable cardiovascular disease (CVD) risk factors that contribute to nearly one-third of all deaths in the Americas Region each year (2.3 million deaths). Despite advances in the detection and clinical management of hypertension and diabetes, there are substantial gaps in their implementation globally and in the Region. The considerable overlap in risk factors, prognosis, and treatment of hypertension and diabetes creates a unique opportunity for a unified implementation model for management at the population level. This report highlights one such high-profile effort, the Pan American Health Organization’s “HEARTS in the Americas” program, based on the World Health Organization’s HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care. The HEARTS program aims to improve the implementation of preventive CVD care in primary health systems using six evidence-based, pragmatic components: Healthy-lifestyle counseling, Evidence-based protocols, Access to essential medicines and technology, Risk-based CVD management, Team-based care, and Systems for monitoring. To date, HEARTS implementation projects have focused primarily on hypertension given that it is the leading modifiable CVD risk factor and can be treated cost-effectively. The objective of this report is to describe opportunities for integration of diabetes clinical care and policy within the HEARTS hypertension framework. A substantial global burden of disease could be averted with integrated primary care management of these conditions. Thus, there is an urgency in applying lessons from HEARTS to close these implementation gaps and improve the integrated detection, treatment, and control of diabetes and hypertension.
Keywords: Diabetes mellitus, cardiovascular diseases, delivery of health care, Americas
RESUMEN
La hipertensión y la diabetes son los factores de riesgo modificables de las enfermedades cardiovasculares asociados a casi un tercio de todas las muertes en la Región de las Américas cada año (2,3 millones). A pesar de los avances en la detección y el manejo clínico de la hipertensión y la diabetes, existen brechas sustanciales en la implementación a nivel regional y mundial. El considerable solapamiento en los factores de riesgo, el pronóstico y el tratamiento de la hipertensión y la diabetes crea una oportunidad única para un modelo unificado de implementación para el manejo a nivel poblacional. En este informe se pone de relieve una iniciativa importante de este tipo, el programa HEARTS en las Américas de la Organización Panamericana de la Salud, basado en el paquete técnico HEARTS para el manejo de las enfermedades cardiovasculares en la atención primaria de salud. El programa HEARTS tiene como objetivo mejorar la implementación de la atención preventiva de las enfermedades cardiovasculares en los sistemas de atención primaria de salud mediante seis componentes pragmáticos basados en la evidencia: Hábitos y estilos de vida saludables: asesoramiento para los pacientes; Evidencia: protocolos basados en la evidencia; Acceso a medicamentos y tecnologías esenciales; Riesgo cardiovascular: manejo de las enfermedades cardiovasculares basado en el riesgo; Trabajo en equipos; y Sistemas de monitoreo. Hasta la fecha, los proyectos de implementación de HEARTS se han centrado principalmente en la hipertensión, dado que es el principal factor de riesgo modificable de las enfermedades cardiovasculares y puede tratarse de una manera costo-eficaz. El objetivo de este informe es describir las oportunidades para la integración de la política y la atención clínica en el marco HEARTS para la hipertensión. Se podría evitar una significativa carga mundial de enfermedad con un manejo integrado de la atención primaria de estos problemas de salud. Por lo tanto, existe una urgencia en la aplicación de las enseñanzas de HEARTS para salvar estas brechas en la implementación y mejorar la detección, el tratamiento y el control integrados de la diabetes y la hipertensión.
Palabras clave: Diabetes mellitus, enfermedades cardiovasculares, atención a la salud, Américas
RESUMO
Hipertensão e diabetes são fatores de risco modificáveis para doenças cardiovasculares (DCV) que contribuem para quase um terço de todas as mortes na Região das Américas a cada ano (2,3 milhões de mortes). Apesar dos avanços na detecção e no manejo clínico da hipertensão e do diabetes, existem lacunas importantes em sua implementação mundialmente e na região. A sobreposição considerável de fatores de risco, prognóstico e tratamento da hipertensão e do diabetes cria uma oportunidade única para um modelo de implementação unificado para o manejo dessas doenças em nível populacional. Este relatório destaca um desses esforços de alto nível, o programa “HEARTS nas Américas” da Organização Pan-Americana da Saúde, baseado no Pacote Técnico HEARTS da Organização Mundial da Saúde para o manejo de DCV na atenção primária à saúde. O programa HEARTS visa melhorar a implementação de cuidados preventivos de DCV nos sistemas de atenção primária utilizando seis componentes pragmáticos e baseados em evidências: Hábitos saudáveis (aconselhamento a pacientes), protocolos baseados em Evidências, Acesso a medicamentos e tecnologias essenciais, manejo das DCV baseado em Risco, Trabalho de equipe como base para a atenção e Sistemas de monitoramento. Até hoje, os projetos de implementação do HEARTS têm se concentrado principalmente na hipertensão, considerando que é o principal fator de risco modificável de DCV e pode ser tratada de forma custo-efetiva. O objetivo deste relatório é descrever as oportunidades de integração do manejo clínico e de políticas para o diabetes dentro da estrutura HEARTS de manejo da hipertensão. Uma importante carga global de doença poderia ser evitada com o manejo integrado dessas duas afecções na atenção primária. Assim, há uma urgência na aplicação das lições de HEARTS para fechar estas lacunas de implementação e melhorar a detecção, o tratamento e o controle integrados do diabetes e da hipertensão.
Palavras-chave: Diabetes mellitus, doenças cardiovasculares, atenção à saúde, América
Cardiovascular disease (CVD) is the leading cause of death and disability worldwide. In the Region of the Americas, there were 7.3 million CVD cases and 2.1 million CVD deaths in 2019 (1). Hypertension and diabetes are two important modifiable CVD risk factors with shared pathophysiology and clinical approaches. Adequate diagnosis, treatment, and control of hypertension and diabetes can mitigate a substantial portion of death and disability. There is a need to scale up evidence-based care for hypertension and diabetes within primary health systems throughout the Americas. This report highlights one such high-profile effort, the Pan American Health Organization (PAHO) “HEARTS in the Americas” initiative, which targets prevention of CVD in primary health systems in the Americas. To date, HEARTS implementation projects globally and in the Region have primarily focused on hypertension given that it is the most epidemiologically significant modifiable CVD risk factor (2).
The objective of this report is to describe opportunities for integration of diabetes clinical care and policy within the HEARTS hypertension framework. We focus on type 2 diabetes given that type 1 diabetes is much less prevalent and generally managed in specialty rather than primary care settings in the Region.
CONTRIBUTION OF HYPERTENSION AND DIABETES TO CVD AND THE TOTAL BURDEN OF DISEASE
CVD refers to several diseases mediated by atherosclerosis and vascular injury. Many risk factors that predispose individuals to CVD can be controlled through pharmacologic and non-pharmacologic interventions. The Prospective Urban Rural Epidemiology (PURE) study in 21 low-, middle-, and high-income countries found that most CVD cases and deaths are attributable to a small number of modifiable CVD risk factors (3). This report focuses on the modifiable CVD risk factors of hypertension and diabetes.
The number of adults with hypertension and diabetes is rising across the world. In the Americas, the age-standardized hypertension prevalence appears to be declining though the absolute number with hypertension is increasing due to aging and population growth (4). There also have been sharp increases both in age-standardized and crude diabetes prevalence in the Region. Epidemiologic cohorts in the Region show a substantially increased risk of both cardiovascular and renal death among people with diabetes or hypertension (5). These cohorts also suggest that individuals with both hypertension and diabetes, occurring together in about one-third of cases with diabetes (6), have a higher risk of death than individuals with either condition alone. The Global Burden of Disease study estimates that elevated blood pressure and elevated blood glucose accounted for 16.9% and 14.7%, respectively, of the population-attributable percentage of deaths in the Region in 2019, amounting to a total of 2.3 million annual deaths (Table 1) (1).
TABLE 1. Deaths attributable to modifiable risk factors in the Americas.
|
|
Leading risks 1990 |
Percentage of deaths 1990 |
|
Leading risks 2019 |
Percentage of deaths 2019 |
Total deaths 2019 (thousands) |
|---|---|---|---|---|---|---|
|
1 |
Tobacco |
18.8 |
1 |
High systolic blood pressure |
16.9 |
1 230 |
|
2 |
High systolic blood pressure |
18.0 |
2 |
High fasting plasma glucose |
14.7 |
1 064 |
|
3 |
Dietary risks |
14.5 |
3 |
Tobacco |
14.4 |
1 043 |
|
4 |
High LDL cholesterol |
10.9 |
4 |
High body-mass index |
13.0 |
940 |
|
5 |
High fasting plasma glucose |
10.4 |
5 |
Dietary risks |
12.6 |
916 |
|
6 |
High body-mass index |
8.9 |
6 |
Kidney dysfunction |
7.6 |
550 |
|
7 |
Child and maternal malnutrition |
7.9 |
7 |
High LDL cholesterol |
7.3 |
528 |
|
8 |
Air pollution |
7.0 |
8 |
Alcohol use |
5.1 |
370 |
|
9 |
Kidney dysfunction |
5.2 |
9 |
Air pollution |
4.1 |
298 |
|
10 |
Alcohol use |
4.5 |
10 |
Non-optimal temperature |
3.1 |
225 |
Source: Prepared by the authors using estimates from the Global Burden of Disease study (1).
Note: The arrows refer to changes in order ranking for high systolic blood pressure and high fasting plasma glucose from 1990 to 2019.
Evidence-based clinical management of hypertension and diabetes in primary care includes pharmacologic interventions (e.g., antihypertensive, glucose-lowering, and statin therapies) and non-pharmacologic interventions (e.g., healthy lifestyle counseling) (7,8). Widespread adoption of these interventions in some settings has reduced population-level mortality from CVD and diabetes. However, there are “implementation gaps” in the delivery of hypertension and diabetes care: in the case of hypertension, approximately 35% of women and 23% of men in Latin America and the Caribbean control blood pressure under 140/90 mmHg (9). Studies including data from several countries in the Americas report that approximately 30% of people with diabetes achieve glycemic control, only 20% take statins, and 50% or fewer receive recommended lifestyle counseling on diet or physical activity (6). There is an urgent need for population-based initiatives to address these implementation gaps and improve the population-level management of hypertension and diabetes.
HYPERTENSION AND DIABETES: THE NEED FOR AN INTEGRATED APPROACH
Hypertension and diabetes have overlapping risk factors that lead to common pathways of complications, resulting in premature morbidity and mortality (Figure 1) (10). Elevated glucose and blood pressure accelerate atherosclerosis, endothelial dysfunction, and vascular injury. These mechanisms give rise to macrovascular disease in the form of ischemic heart disease, stroke, aortic disease, and peripheral arterial disease. These pathologic processes also predispose individuals to microvascular disease in the form of kidney disease, neuropathy (and risk of limb amputations), and vision loss (from retinopathy and cataracts). Other complications partially driven by hypertension and diabetes include dementia, atrial fibrillation, and heart failure. To compound the urgency, hypertension independently increases diabetes risk, and diabetes independently increases hypertension risk.
Figure 1. Overlapping risk factors and management of hypertension and diabetes.
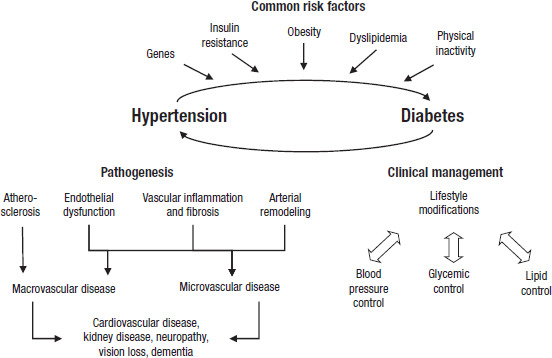
Source: Adapted by the authors with permission from Petrie et al (10).
Evidence-based clinical management of hypertension and diabetes addresses these shared risk factors through lifestyle modifications to improve diet, increased physical activity, smoking cessation, and weight loss. These lifestyle modifications must accompany pharmacologic and non-pharmacologic interventions to control blood sugar, blood pressure, and lipids. The overlap in the management of hypertension and diabetes creates an opportunity for a unified model for detection and management at the population level.
HEARTS AS A UNIFYING IMPLEMENTATION MODEL FOR HYPERTENSION AND DIABETES MANAGEMENT IN PRIMARY CARE
The World Health Organization (WHO) has spearheaded development of models and tools to decrease CVD through its Global Hearts initiative. Within this initiative, the HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care provides a population-based approach to prevent CVD (11). The HEARTS model consists of six evidence-based modules: Healthy-lifestyle counseling, Evidence-based protocols, Access to essential medicines and technology, Risk-based CVD management, Team-based care, and Systems for monitoring (Table 2). The HEARTS initiative seeks to integrate these strategies into existing health systems with an emphasis on prevention of CVD at the primary care level.
Table 2. Components of the HEARTS Technical Package.
|
|
Component |
Description |
|---|---|---|
|
|
Healthy lifestyle counseling |
Counseling on diet, physical activity, disease self-care |
|
|
Evidence-based protocols |
Simplified and standardized drug treatment algorithms |
|
|
Access to essential medicines and technologies |
Procurement, distribution, and handling of essential supplies |
|
|
Risk-based CVD management |
Treatment using cardiovascular risk assessment |
|
|
Team-based care: |
Shifting and sharing tasks among health workers in a team |
|
|
Systems for monitoring |
Using data to monitor and improve the quality of care |
Source: Prepared by the authors based on the information in the HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care (11).
CVD, cardiovascular disease.
In the Americas, PAHO aims to make HEARTS the model for the prevention of CVD in primary care within health systems across the Region by 2025. The first cohort of four countries implemented the HEARTS program beginning in 2015-2017 (Barbados, Colombia, Chile, and Cuba). To date, Ministries of Health in 22 countries in the Region have signed on to implement HEARTS, and more are in the process of joining.
INTEGRATION OF HYPERTENSION AND DIABETES CARE WITHIN HEARTS
The HEARTS Technical Package addresses multiple modifiable CVD risk factors including hypertension, diabetes, dyslipidemia, and tobacco use (11). In the Americas, PAHO has assisted countries in the practical aspects of implementing HEARTS by providing detailed guidance on implementation barriers, standardized hypertension treatment protocols, fixed-dose combination antihypertensive therapy, and validated blood pressure-measuring device use.
In the case of diabetes, the “HEARTS-D” module (12) focuses on clinical diabetes recommendations aligned with the WHO Package of Essential Noncommunicable Disease Interventions in Primary Health Care (WHO PEN) (7). However, there is a need for practical guidance—or “implementation strategies”—to integrate management of diabetes into the HEARTS platform. The remainder of this paper focuses on considerations for integrating hypertension and diabetes care within the unified HEARTS framework (Table 3).
Table 3. Key considerations for the integration of hypertension and diabetes primary care management within the HEARTS framework.
|
HEARTS component |
Key considerations |
|---|---|
|
Healthy-lifestyle counseling |
|
|
Evidence-based protocols |
|
|
Access to essential medicines and technology |
|
|
Risk-based CVD management |
|
|
Team-based care |
|
|
Systems for monitoring |
|
Source: Prepared by the authors.
CVD, cardiovascular disease; PAHO, Pan American Health Organization; WHO, World Health Organization.
Healthy lifestyle counseling
This HEARTS module focuses on behavioral changes and motivational interviewing to improve diets, increase physical activity, reduce tobacco use, and limit harmful alcohol use. As described above, lifestyle counseling is a foundational element of the clinical management of both hypertension and diabetes.
While this report does not primarily emphasize the prevention of diabetes, intensive lifestyle interventions are effective in preventing diabetes onset among high-risk individuals (e.g., prediabetes and obesity), including in real-world settings outside of clinical trials (13). Intensive lifestyle interventions to prevent diabetes are cost effective, but they also are perceived as infeasible in many countries given the resources required to implement and sustain them (13). Thus, health systems should consider innovative strategies to reduce the cost of diabetes prevention services within the HEARTS framework such as mobile health tools, delivery by non-physician workers, group classes, and prioritizing individuals most likely to benefit.
Among people with diabetes, high-quality counseling goes beyond straightforward messages on diet and physical activity. Diabetes self-management education and support (DSMES) addresses the clinical, psychological, and social needs of people living with diabetes (14). Key components of DSMES include developing coping skills, eating a healthy diet, promoting physical activity, taking medication, monitoring disease, reducing modifiable risks, and solving problems. The American Diabetes Association recommends DSMES at diagnosis, at least annually or when not meeting treatment targets, upon the development of diabetes complications, and during important changes in care—each of which are junctures in which hypertension education is also important (14).
It is important to consider the evidence underlying the effectiveness of diabetes behavioral interventions. One large trial of intensive lifestyle counseling found no reduction in mortality or CVD events over approximately 10 years of follow up, though other benefits were observed including improvements in blood pressure and reduced need for antihypertensive medications (15). Another large trial of intensive weight management found that an intensive weight-loss intervention could lead to remission in nearly one-third of people with diabetes not using insulin at 24 months and also improve blood pressure (16). A meta-analysis of 132 randomized trials of behavioral programs for type 2 diabetes concluded that the level of contact intensity plays a role in the effectiveness of a given DSMES program, and programs delivering fewer than 10 contact hours confer minimal benefit (17).
Given this evidence, as in the case of diabetes prevention, health systems choosing to invest in DSMES within the HEARTS framework may wish to consider innovative, low-cost delivery strategies to lower cost and maintain high intervention intensity. One team-based approach that has improved glycemic status and blood pressure among people with diabetes is the delivery of DSMES by peers with diabetes or community health workers (13). Such delivery models also may tailor messages to local communities, an important consideration given the cultural and linguistic diversity of populations across the Region.
Evidence-based protocols
Complementing the Healthy Lifestyle Counseling module, this module focuses on standardized protocols for pharmacological treatment, coupled with a small formulary of effective, safe, and affordable medications. HEARTS recommends protocols that are simple and standardized, meaning that they (a) can be implemented by both physicians and non-physician health workers under supervision at the primary care level, (b) include specific drugs and dosages for titration, and (c) are applicable to most patients in primary care. The use of simple, standardized treatment protocols is synergistic with the HEARTS modules of Access to Essential Medicines and Technologies and Team-Based Care. In its prior efforts, PAHO has expanded on the HEARTS framework by providing detailed guidance on hypertension protocols, including the use of two anti-hypertensive medications in the initial treatment step of the newly diagnosed individual with hypertension, either as two separate pills or preferably in a single, fixed-dose combination pill (18). Building on PAHO’s experience and the HEARTS-D module, we highlight three opportunities for the integration of hypertension and diabetes treatment protocols. Of note, a discussion of the effectiveness, feasibility, and cost-effectiveness of pharmacologic therapies such as metformin for the prevention of diabetes is beyond the scope of this manuscript.
One opportunity is to construct routine primary care clinical pathways to improve the detection and treatment of hypertension and diabetes. The WHO-PEN guidelines recommend that blood pressure be assessed in adults during all primary care visits and that diabetes screening be performed among high-risk individuals, specifically those who are age 40 years or older and with a body-mass index of 25 kg/m2 or greater (7). This diabetes screening recommendation is consistent with Latin American Diabetes Association (ALAD) guidelines (19). Among individuals diagnosed with either hypertension or diabetes, routine testing for the other condition is particularly important (e.g., detecting hypertension among individuals with diabetes and vice versa) given the shared risk factors and frequent co-occurrence described above. A similar approach must be used for the detection of chronic kidney disease among people with diabetes and hypertension.
Within this integrated approach to detection, making a diagnosis of hypertension or detecting kidney involvement such as proteinuria and/or chronic kidney disease is particularly important given that treatment with renin-angiotensin system inhibitors such as angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers can reduce the progression of diabetic kidney disease and also play a role in preventing diabetes (20). Integrated approaches to improve the detection of hypertension and diabetes might include work- or community-based outreach programs (2), use of validated measurement devices and protocols, and subsidized screening in other health facilities such as dental offices or pharmacies. In the case of diabetes, one approach to improve detection is to implement routine clinic screening among high-risk individuals, in line with WHO-PEN guidelines (7). The efficiency of routine screening might be improved by implementing testing protocols that incorporate point-of-care random capillary glucose measurements, which are less costly than hemoglobin A1c (HbA1c) and more convenient than venous or fasting glucose.
The most critical opportunity to integrate hypertension and diabetes treatment is to emphasize the role of multifactorial approaches to reduce CVD risk. In the case of diabetes, pharmacologic treatment must not only address hyperglycemia, but also address CVD risk factors including hypertension and dyslipidemia. Put simply, hypertension and lipid control are cornerstones of diabetes management (21). A modeling study of multifactorial treatment among people with diabetes in 67 low- and middle-income countries found that scaling up treatment with antihypertensive and statin medications would provide greater population benefit than treatment focusing on glycemic control (22). While management of dyslipidemia is not the focus of this report, statin treatment is a core management strategy to prevent CVD among people with hypertension and/or diabetes. WHO PEN recommends statins for the primary prevention of CVD for people with diabetes who are ≥40 years of age and for people without diabetes who have CVD risk >20% (7). Yet across low- and middle-income countries, including countries in the Region of the Americas, only 10% of people who are eligible for statin therapy for primary prevention receive treatment (6,23). Pragmatic strategies in the HEARTS framework to improve statin use among eligible people with hypertension and/or diabetes include simplified statin treatment protocols that may limit routine cholesterol measurements, use of ”polypills” containing both antihypertensive and statin agents, addition of other statins beyond simvastatin (e.g., atorvastatin) to national formularies via the PAHO Strategic Fund, and task sharing with non-physician health workers to routinely calculate CVD risk (24) (complementing the Team-Based Care module below).
Another opportunity for the integration of diabetes treatment protocols into the HEARTS framework relates to the role of glucose-lowering medication treatment and glycemic targets (12). A few points are key. First, at the population level, prioritization achievement of strict glycemic control will have less benefit than prioritization of hypertension and statin management (22,25). While many international guidelines recommend strict glycemic targets of HbA1c <7% among most people with diabetes (7,19), the population-level effectiveness, safety, cost-effectiveness, and feasibility of this recommendation in resource-constrained health systems merits considerable scrutiny. Second, there is a need to develop simple, standardized protocols for glucose-lowering treatment to minimize the population of patients with poor glycemic control, as diabetes-related mortality rises sharply when HbA1c increases above approximately 8% (26). HEARTS-aligned strategies to improve glucose-lowering treatment protocols could include simplified titration algorithms for use by non-physician health workers under protocol, preference for certain drugs within drug classes (e.g., sulfonylureas with lower risk for hypoglycemia), using fixed-dose combination medications (e.g., combinations of metformin and sulfonylureas), reducing refill frequency among patients with adequate glycemic control, and reserving insulin for symptomatic or uncontrolled patients most likely to benefit. Finally, future efforts to unify hypertension and diabetes protocols under the HEARTS framework should consider the role of newer diabetes medicines, in particular sodium-glucose co-transporter-2 (SGTL-2) inhibitors. These drugs are effective in improving cardiovascular and kidney outcomes among people with diabetes, though the current evidence is stronger for secondary prevention than primary prevention of CVD (27). The implementation of SGLT-2 inhibitors into practice in low- and middle-income countries has the potential to improve population-level diabetes outcomes and prevent downstream health care costs, such as hospital admissions for heart attacks or heart failure and dialysis for end-stage kidney disease (28). Issues of access to these drugs are discussed in the next section.
Access to essential medicines and technology
This HEARTS module describes the procurement, distribution, and handling of essential medicines and technology in primary care. Given the importance of blood pressure control in the management of diabetes, PAHO’s ongoing efforts to ensure access to essential hypertension medicines including fixed-dose combinations within the PAHO Strategic Fund is critical to improving population diabetes outcomes (18). Fixed-dose combination anti-hypertensive agents have recently been included in the WHO Essential Medication List. In addition, the initiation of two anti-hypertensive medications each at half-maximal doses, preferably in a single-pill, fixed dose combination, in the newly diagnosed individual with hypertension was supported by the 2021 WHO Guideline for the Pharmacological Treatment of Hypertension in Adults (8).
A key challenge with diabetes compared to hypertension management is the greater need for laboratory equipment and consumables to monitor blood glucose, HbA1c, cholesterol, creatinine, urine albumin, and urine ketones. The WHO Model List of Essential Diagnostics recommends these technologies in primary care, but there is inadequate availability in many countries. Opportunities within the HEARTS framework to improve access to diabetes laboratory technologies might include standardization of glucometer models to ensure glucose strip compatibility, the addition of validated and low-cost devices to the PAHO Strategic Fund, point-of-care HbA1c testing, and novel monitoring algorithms that incorporate both glucose and HbA1c testing.
SGLT-2 inhibitors and insulin glargine were added to the WHO Essential Medicine List in 2021. Given evidence of the effectiveness for SGLT-2 inhibitors and presence in ALAD guidelines (19), health systems may wish to investigate incorporating these drugs into national formularies as prices permit (28). In some countries like India, the entry of generic SGLT-2 inhibitors into the market has substantially decreased prices (29). With respect to insulin, analog insulins (e.g., insulin glargine) confer limited clinical benefit above human insulins (e.g., NPH insulin) for most people with type 2 diabetes (30), and NPH insulin is preferred for this population in ALAD guidelines (19). Given the complexity of the topic of insulin access, including issues of procurement, distribution, and storage, we refer interested readers to a recent WHO report for details (31). Finally, glucagon-like peptide-1 (GLP-1) receptor agonists have proven CVD benefit and are featured in ALAD guidelines (19), but achieving population level cost effectiveness across low- to middle-income countries would require a 95% cost reduction (28).
Risk-based CVD management
This HEARTS module focuses on using estimated CVD risk to guide clinical management to prevent CVD. In the case of diabetes, WHO guidelines recommend that all people with type 2 diabetes ≥40 years receive statins (7) and target a blood pressure of <130/80 mmHg (8). However, these recommendations may not be feasible in all settings. The HEARTS-D module suggests using CVD risk prediction tools to identify diabetes patients who would have greatest benefit from statins for primary prevention of CVD (32). A similar risk-based approach could guide the intensity of blood pressure treatment or lifestyle interventions among people with diabetes. Note that all people with diabetes and CVD are at high risk and should receive statins irrespective of predicted risk (7).
There are practical challenges to implementing a CVD-risk approach in primary care settings, including limited staffing capacity to generate CVD risk assessments and the lack of laboratory capacity to generate required input data. PAHO has developed electronic tools to facilitate implementation of the 2019 region-specific WHO CVD risk scores into routine primary care (33). An evidence-based strategy for the staffing challenge is the use of non-physician health workers to calculate CVD risk scores; this approach aligns with the Team-Based Care module of HEARTS. In primary care settings with limited access to clinical laboratories, the WHO also has constructed non-laboratory-based CVD risk equations that do not require total cholesterol measurements. However, it should be noted non-laboratory-based CVD risk equations are less accurate in people with diabetes (32).
Researchers also have developed diabetes-specific equations to estimate the risk of microvascular complications including nephropathy, retinopathy, and neuropathy (34). These equations allow the application of a risk-based approach, as advocated in HEARTS, to glucose-lowering treatment protocols. At the population level, risk-guided diabetes treatment strategies hold promise in improving treatments while reducing harms (35). Yet diabetes-focused risk equations must be validated across populations before implementation.
Team-based care
This HEARTS module focuses on the use of multidisciplinary teams to prevent CVD. Team-based care can refer to task shifting (i.e., reassignment of clinical tasks) or task sharing (i.e., shared responsibility of clinical tasks). As discussed above in complementary HEARTS modules, non-physician health workers can effectively counsel on healthy lifestyles, manage pharmacologic treatment protocols, and assess CVD risk. Team-based care is an evidence-based strategy to improve the coverage and quality of both hypertension and diabetes care and is associated with reductions in HbA1c of 0.5-1.0% (36,37).
Within the HEARTS framework, team-based care integration can be either horizontal or vertical. Horizontal care teams operate across the same primary health facility. Examples of members of horizontal care teams for both hypertension and diabetes include primary care physicians, nurses, pharmacists, nutritionists, social workers, and community health workers. One crucial difference between team-based care for diabetes versus hypertension is the greater role for vertical teams, which are teams that operate at different levels of the health care system, in particular primary care in the community and specialized referral care at secondary or tertiary health facilities. Team-based care for diabetes must be vertical to prevent common chronic complications (e.g., retinopathy or kidney disease) and to manage common acute complications (e.g., hyperglycemic crises or diabetic foot infections). Vertical teams for diabetes must thus comprise both outpatient specialists (e.g., endocrinologists, ophthalmologists, nephrologists) and acute care physicians. As with pharmacologic treatment, the new WHO guideline on hypertension supports team-based care to include non-physicians prescribing anti-hypertensive medications under certain conditions such as established evidence-based protocols, supervision by a physician, and compliance with regulatory requirements.
Systems for monitoring
This HEARTS module focuses on monitoring and improving the quality of health care to prevent CVD at primary health facilities. In the case of hypertension, PAHO has expanded the HEARTS monitoring framework to recommend a total of six core indicators and many other optional indicators. These indicators evaluate the three major components of health care quality—structure, process, and outcome—at different levels of the health system and in the population (38). In the case of diabetes, there is a need to expand on the existing HEARTS monitoring framework and to develop supplementary diabetes-specific monitoring indicators, especially in the domains of structure and process. At the system level, PAHO’s hypertension monitoring framework could provide a template for diabetes as it provides structure and process indicators relating to program development, stakeholder support, financing, operational planning, and other goals (38). At the health facility level, potential structure and process indicators include completion of important clinical tasks such as retinopathy screening, use of preferred classes of glucose-lowering medications, frequency of follow-up visits, or specific task-sharing processes such as a visit with a diabetes educator (39). Diabetes outcome indicators should align with four population-level diabetes targets put forth by the WHO (40). These WHO targets are that at least 80% of people with diabetes are aware of their diagnosis, and among those diagnosed, at least 80% achieve glycemic control (HbA1c <8.0%), at least 80% achieve blood pressure control (<140/90 mmHg), and at least 60% use a statin (40).
Conclusion
Management of hypertension and diabetes in primary care is effective at preventing morbidity and mortality from CVD. However, there is a critical need for knowledge on how to close the implementation gap in primary health systems. The HEARTS model has been successfully implemented in 22 countries, covering treatment for more than 3 million patients. This report leverages these successful implementation experiences to suggest opportunities to scale up integrated hypertension and diabetes management in primary care using the HEARTS framework. Given the substantial burden of preventable disease that could be averted with improved management of hypertension and diabetes, there is an urgency in applying lessons from HEARTS to close these implementation gaps.
Disclaimer.
Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH or the Pan American Health Organization (PAHO).
Acknowledgements.
DJD is a Health Sciences Distinguished Professor of the University of South Carolina and University of South Carolina School of Medicine, Columbia, South Carolina, United States of America.
Footnotes
Author contributions.
DJD conceived the original idea. DF, EWE, and DJD developed the key elements and wrote the first draft. All authors provided iterative feedback and interpretation of the manuscript on multiple rounds of co-author review. All authors reviewed and approved the final version.
Funding.
None declared.
Conflicts of interest.
None declared.
REFERENCES
- 1.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]; Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020; 76(25): 2982-3021. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization . Improving hypertension control in 3 million people: country experiences of programme development and implementation. Geneva: WHO; 2020. [Google Scholar]; World Health Organization. Improving hypertension control in 3 million people: country experiences of programme development and implementation. Geneva: WHO; 2020.
- 3.Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395(10226):795–808. doi: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020; 395(10226):795-808. [DOI] [PMC free article] [PubMed]
- 4.NCD Risk Factor Collaboration-Americas Working Group Trends in cardiometabolic risk factors in the Americas between 1980 and 2014: a pooled analysis of population-based surveys. Lancet Glob Health. 2020;8(1):e123–e133. doi: 10.1016/S2214-109X(19)30484-X. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCD Risk Factor Collaboration-Americas Working Group. Trends in cardiometabolic risk factors in the Americas between 1980 and 2014: a pooled analysis of population-based surveys. Lancet Glob Health. 2020;8(1): e123-e33. [DOI] [PMC free article] [PubMed]
- 5.Alegre-Diaz J, Herrington W, Lopez-Cervantes M, Gnatiuc L, Ramirez R, Hill M, et al. Diabetes and Cause-Specific Mortality in Mexico City. N Engl J Med. 2016;375(20):1961–1971. doi: 10.1056/NEJMoa1605368. [DOI] [PMC free article] [PubMed] [Google Scholar]; Alegre-Diaz J, Herrington W, Lopez-Cervantes M, Gnatiuc L, Ramirez R, Hill M, et al. Diabetes and Cause-Specific Mortality in Mexico City. N Engl J Med. 2016;375(20):1961-71. [DOI] [PMC free article] [PubMed]
- 6.Flood D, Seiglie JA, Dunn M, Tschida S, Theilmann M, Marcus ME, et al. The state of diabetes treatment coverage in 55 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data in 680 102 adults. Lancet Healthy Longev. 2021;2(6):e340–e351. doi: 10.1016/s2666-7568(21)00089-1. [DOI] [PMC free article] [PubMed] [Google Scholar]; Flood D, Seiglie JA, Dunn M, Tschida S, Theilmann M, Marcus ME, et al. The state of diabetes treatment coverage in 55 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data in 680 102 adults. Lancet Healthy Longev. 2021;2(6):e340–e51. [DOI] [PMC free article] [PubMed]
- 7.World Health Organization . WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Geneva: WHO; 2020. [Google Scholar]; World Health Organization. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Geneva: WHO; 2020.
- 8.World Health Organization . Guideline for the pharmacological treatment of hypertension in adults. Geneva: WHO; 2021. [PubMed] [Google Scholar]; World Health Organization. Guideline for the pharmacological treatment of hypertension in adults. Geneva: WHO; 2021. [PubMed]
- 9.Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–980. doi: 10.1016/S0140-6736(21)01330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]; Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957-980. doi: 10.1016/S0140-6736(21)01330-1 [DOI] [PMC free article] [PubMed]
- 10.Petrie JR, Guzik TJ, Touyz RM. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can J Cardiol. 2018;34(5):575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]; Petrie JR, Guzik TJ, Touyz RM. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can J Cardiol. 2018;34(5):575-84. [DOI] [PMC free article] [PubMed]
- 11.World Health Organization . Hearts: Technical package for cardiovascular disease management in primary health care. Geneva: WHO; 2016. [Google Scholar]; World Health Organization. Hearts: Technical package for cardiovascular disease management in primary health care. Geneva: WHO; 2016.
- 12.World Health Organization . HEARTS-D: Diagnosis and management of type 2 diabetes. Geneva: WHO; 2020. [Google Scholar]; World Health Organization. HEARTS-D: Diagnosis and management of type 2 diabetes. Geneva: WHO; 2020.
- 13.Ali MK, Siegel KR, Chandrasekar E, Tandon R, Montoya PA, Mbanya JC, et al. In: Cardiovascular, Respiratory, and Related Disorders. Prabhakaran D, Anand S, et al., editors. Washington (DC): World Bank; 2017. Diabetes: An Update on the Pandemic and Potential Solutions. [Google Scholar]; Ali MK, Siegel KR, Chandrasekar E, Tandon R, Montoya PA, Mbanya JC, et al. Diabetes: An Update on the Pandemic and Potential Solutions. In: rd, Prabhakaran D, Anand S, et al., eds. Cardiovascular, Respiratory, and Related Disorders. Washington (DC): World Bank; 2017. [PubMed]
- 14.Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. Diabetes Self-management Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. 2020;43(7):1636–1649. doi: 10.2337/dci20-0023. [DOI] [PubMed] [Google Scholar]; Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. Diabetes Self-management Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. 2020;43(7):1636-49. [DOI] [PubMed]
- 15.Look Ahead Research Group. Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369(2):145–154. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]; Look Ahead Research Group, Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369(2):145-54. [DOI] [PMC free article] [PubMed]
- 16.Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019;7(5):344–355. doi: 10.1016/S2213-8587(19)30068-3. [DOI] [PubMed] [Google Scholar]; Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019;7(5):344-55. [DOI] [PubMed]
- 17.Pillay J, Armstrong MJ, Butalia S, Donovan LE, Sigal RJ, Vandermeer B, et al. Behavioral Programs for Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-analysis. Ann Intern Med. 2015;163(11):848–860. doi: 10.7326/M15-1400. [DOI] [PubMed] [Google Scholar]; Pillay J, Armstrong MJ, Butalia S, Donovan LE, Sigal RJ, Vandermeer B, et al. Behavioral Programs for Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-analysis. Ann Intern Med. 2015;163(11):848-60. [DOI] [PubMed]
- 18.DiPette DJ, Skeete J, Ridley E, Campbell NRC, Lopez-Jaramillo P, Kishore SP, et al. Fixed-dose combination pharmacologic therapy to improve hypertension control worldwide: Clinical perspective and policy implications. J Clin Hypertens (Greenwich) 2019;21(1):4–15. doi: 10.1111/jch.13426. [DOI] [PMC free article] [PubMed] [Google Scholar]; DiPette DJ, Skeete J, Ridley E, Campbell NRC, Lopez-Jaramillo P, Kishore SP, et al. Fixed-dose combination pharmacologic therapy to improve hypertension control worldwide: Clinical perspective and policy implications. J Clin Hypertens (Greenwich). 2019;21(1):4-15. [DOI] [PMC free article] [PubMed]
- 19.Asociación Latinoamericana de Diabetes (ALAD) Guías ALAD sobre el Diagnóstico, Control y Tratamiento de la Diabetes Mellitus Tipo 2 con Medicina Basada en Evidencia Edición 2019. Revista de la ALAD 2019 [Google Scholar]; Asociación Latinoamericana de Diabetes (ALAD). Guías ALAD sobre el Diagnóstico, Control y Tratamiento de la Diabetes Mellitus Tipo 2 con Medicina Basada en Evidencia Edición 2019. Revista de la ALAD 2019.
- 20.Nazarzadeh M, Bidel Z, Canoy D, Copland E, Wamil M, Majert J, et al. Blood pressure lowering and risk of new-onset type 2 diabetes: an individual participant data meta-analysis. Lancet. 2021;398(10313):1803–1810. doi: 10.1016/S0140-6736(21)01920-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Nazarzadeh M, Bidel Z, Canoy D, Copland E, Wamil M, Majert J, et al. Blood pressure lowering and risk of new-onset type 2 diabetes: an individual participant data meta-analysis. Lancet. 2021;398(10313):1803-10. [DOI] [PMC free article] [PubMed]
- 21.Joseph JJ, Deedwania P, Acharya T, Aguilar D, Bhatt DL, Chyun DA, et al. Comprehensive Management of Cardiovascular Risk Factors for Adults With Type 2 Diabetes: A Scientific Statement From the American Heart Association. Circulation. 2022;145:e722–e759. doi: 10.1161/CIR.0000000000001040. [DOI] [PubMed] [Google Scholar]; Joseph JJ, Deedwania P, Acharya T, Aguilar D, Bhatt DL, Chyun DA, et al. Comprehensive Management of Cardiovascular Risk Factors for Adults With Type 2 Diabetes: A Scientific Statement From the American Heart Association. Circulation. 2022;145:e722-e759. [DOI] [PubMed]
- 22.Basu S, Flood D, Geldsetzer P, Theilmann M, Marcus ME, Ebert C, et al. Estimated effect of increased diagnosis, treatment, and control of diabetes and its associated cardiovascular risk factors among low-income and middle-income countries: a microsimulation model. Lancet Glob Health. 2021;9(11):e1539–e1552. doi: 10.1016/S2214-109X(21)00340-5. [DOI] [PMC free article] [PubMed] [Google Scholar]; Basu S, Flood D, Geldsetzer P, Theilmann M, Marcus ME, Ebert C, et al. Estimated effect of increased diagnosis, treatment, and control of diabetes and its associated cardiovascular risk factors among low-income and middle-income countries: a microsimulation model. Lancet Glob Health. 2021;9(11):e1539-e52. [DOI] [PMC free article] [PubMed]
- 23.Marcus ME, Manne-Goehler J, Theilmann M, Farzadfar F, Moghaddam SS, Keykhaei M, et al. Use of statins for the prevention of cardiovascular disease in 41 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data. Lancet Glob Health. 2022;10(3):e369–e379. doi: 10.1016/S2214-109X(21)00551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]; Marcus ME, Manne-Goehler J, Theilmann M, Farzadfar F, Moghaddam SS, Keykhaei M, et al. Use of statins for the prevention of cardiovascular disease in 41 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data. Lancet Glob Health. 2022;10(3):e369-e79. [DOI] [PMC free article] [PubMed]
- 24.Gaziano TA, Abrahams-Gessel S, Denman CA, Montano CM, Khanam M, Puoane T, et al. An assessment of community health workers' ability to screen for cardiovascular disease risk with a simple, non-invasive risk assessment instrument in Bangladesh, Guatemala, Mexico, and South Africa: an observational study. Lancet Glob Health. 2015;3(9):e556–e563. doi: 10.1016/S2214-109X(15)00143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gaziano TA, Abrahams-Gessel S, Denman CA, Montano CM, Khanam M, Puoane T, et al. An assessment of community health workers' ability to screen for cardiovascular disease risk with a simple, non-invasive risk assessment instrument in Bangladesh, Guatemala, Mexico, and South Africa: an observational study. Lancet Glob Health. 2015;3(9):e556-63. [DOI] [PMC free article] [PubMed]
- 25.Yudkin JS, Richter B, Gale EA. Intensified glucose lowering in type 2 diabetes: time for a reappraisal. Diabetologia. 2010;53(10):2079–2085. doi: 10.1007/s00125-010-1864-z. [DOI] [PubMed] [Google Scholar]; Yudkin JS, Richter B, Gale EA. Intensified glucose lowering in type 2 diabetes: time for a reappraisal. Diabetologia. 2010;53(10):2079-85. [DOI] [PubMed]
- 26.Currie CJ, Peters JR, Tynan A, Evans M, Heine RJ, Bracco OL, et al. Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375(9713):481–489. doi: 10.1016/S0140-6736(09)61969-3. [DOI] [PubMed] [Google Scholar]; Currie CJ, Peters JR, Tynan A, Evans M, Heine RJ, Bracco OL, et al. Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375(9713):481-9. [DOI] [PubMed]
- 27.McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, et al. Association of SGLT2 Inhibitors With Cardiovascular and Kidney Outcomes in Patients With Type 2 Diabetes: A Meta-analysis. JAMA Cardiol. 2021;6(2):148–158. doi: 10.1001/jamacardio.2020.4511. [DOI] [PMC free article] [PubMed] [Google Scholar]; McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, et al. Association of SGLT2 Inhibitors With Cardiovascular and Kidney Outcomes in Patients With Type 2 Diabetes: A Meta-analysis. JAMA Cardiol. 2021;6(2):148-58. [DOI] [PMC free article] [PubMed]
- 28.Basu S, Yudkin JS, Mezhrahid J, Flood D, Lipska K, Beran D, et al. Expanding access to newer medicines for people with type 2 diabetes in low-income and middle-income countries: a cost-effectiveness and price target analysis. Lancet Diabetes Endocrinol. 2021;9(12):825–836. doi: 10.1016/S2213-8587(21)00240-0. [DOI] [PubMed] [Google Scholar]; Basu S, Yudkin JS, Mezhrahid J, Flood D, Lipska K, Beran D, et al. Expanding access to newer medicines for people with type 2 diabetes in low-income and middle-income countries: a cost-effectiveness and price target analysis. Lancet Diabetes Endocrinol. 2021;9(12):825-836. [DOI] [PubMed]
- 29.Unnikrishnan R, Mohan V. Newer antidiabetic agents: at what price will they be cost effective? Lancet Diabetes Endocrinol. 2021;9(12):801–803. doi: 10.1016/S2213-8587(21)00264-3. [DOI] [PubMed] [Google Scholar]; Unnikrishnan R, Mohan V. Newer antidiabetic agents: at what price will they be cost effective? Lancet Diabetes Endocrinol. 2021;9(12):801-803. [DOI] [PubMed]
- 30.World Health Organization . Guidelines on second- and third-line medicines and type of insulin for the control of blood glucose levels in non- pregnant adults with diabetes mellitus. Geneva: WHO; 2018. [PubMed] [Google Scholar]; World Health Organization. Guidelines on second- and third-line medicines and type of insulin for the control of blood glucose levels in non- pregnant adults with diabetes mellitus. Geneva: WHO; 2018. [PubMed]
- 31.World Health Organization . Keeping the 100-year-old promise: making insulin access universal. Geneva: WHO; 2021. [Google Scholar]; World Health Organization. Keeping the 100-year-old promise: making insulin access universal. Geneva: WHO; 2021.
- 32.Kaptoge S, Pennells L, De Bacquer D, Cooney MT, Kavousi M, Stevens G, et al. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kaptoge S, Pennells L, De Bacquer D, Cooney MT, Kavousi M, Stevens G, et al. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332-e45. [DOI] [PMC free article] [PubMed]
- 33.Ordunez P, Tajer C, Gaziano T, Rodriguez Y, Rosende A, Jaffe M. The HEARTS app: a clinical tool for cardiovascular risk and hypertension management in primary health care. Rev Panam Salud Publica. 2022;46:e12. doi: 10.26633/RPSP.2022.12. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ordunez P, Tajer C, Gaziano T, Rodriguez Y, Rosende A, Jaffe M. The HEARTS app: a clinical tool for cardiovascular risk and hypertension management in primary health care. Rev Panam Salud Publica. 2022;46:e12. [DOI] [PMC free article] [PubMed]
- 34.Basu S, Sussman JB, Berkowitz SA, Hayward RA, Yudkin JS. Development and validation of Risk Equations for Complications Of type 2 Diabetes (RECODe) using individual participant data from randomised trials. Lancet Diabetes Endocrinol. 2017;5(10):788–798. doi: 10.1016/S2213-8587(17)30221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]; Basu S, Sussman JB, Berkowitz SA, Hayward RA, Yudkin JS. Development and validation of Risk Equations for Complications Of type 2 Diabetes (RECODe) using individual participant data from randomised trials. Lancet Diabetes Endocrinol. 2017;5(10):788-98. [DOI] [PMC free article] [PubMed]
- 35.Basu S, Shankar V, Yudkin JS. Comparative effectiveness and cost-effectiveness of treat-to-target versus benefit-based tailored treatment of type 2 diabetes in low-income and middle-income countries: a modelling analysis. Lancet Diabetes Endocrinol. 2016;4(11):922–932. doi: 10.1016/S2213-8587(16)30270-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Basu S, Shankar V, Yudkin JS. Comparative effectiveness and cost-effectiveness of treat-to-target versus benefit-based tailored treatment of type 2 diabetes in low-income and middle-income countries: a modelling analysis. Lancet Diabetes Endocrinol. 2016;4(11):922-32. [DOI] [PMC free article] [PubMed]
- 36.Maria JL, Anand TN, Dona B, Prinu J, Prabhakaran D, Jeemon P. Task-sharing interventions for improving control of diabetes in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. 2021;9(2):e170–e180. doi: 10.1016/S2214-109X(20)30449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Maria JL, Anand TN, Dona B, Prinu J, Prabhakaran D, Jeemon P. Task-sharing interventions for improving control of diabetes in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. 2021;9(2):e170-e80. [DOI] [PMC free article] [PubMed]
- 37.Flood D, Hane J, Dunn M, Brown SJ, Wagenaar BH, Rogers EA, et al. Health system interventions for adults with type 2 diabetes in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020;17(11):e1003434. doi: 10.1371/journal.pmed.1003434. [DOI] [PMC free article] [PubMed] [Google Scholar]; Flood D, Hane J, Dunn M, Brown SJ, Wagenaar BH, Rogers EA, et al. Health system interventions for adults with type 2 diabetes in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020;17(11):e1003434. [DOI] [PMC free article] [PubMed]
- 38.Pan American Health Organization . Monitoring and Evaluation Framework for Hypertension Control Programs. Washington, DC: PAHO; 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]; Pan American Health Organization. Monitoring and Evaluation Framework for Hypertension Control Programs. Washington, DC:PAHO; 2018. [DOI] [PMC free article] [PubMed]
- 39.Jiang DH, O'Connor PJ, Huguet N, Golden SH, McCoy RG. Modernizing Diabetes Care Quality Measures. Health Aff (Millwood) 2022 doi: 10.1377/hlthaff.2022.00233. 101377hlthaff202200233. [DOI] [PMC free article] [PubMed] [Google Scholar]; Jiang DH, O'Connor PJ, Huguet N, Golden SH, McCoy RG. Modernizing Diabetes Care Quality Measures. Health Aff (Millwood). 2022:101377hlthaff202200233. [DOI] [PMC free article] [PubMed]
- 40.Gregg E, Buckley J, Ali M, Davies J, Flood D, Griffiths B, et al. Improving health outcomes of people with diabetes mellitus: target setting to reduce the global burden of diabetes mellitus. Geneva: World Health Organization; 2021. [Google Scholar]; Gregg E, Buckley J, Ali M, Davies J, Flood D, Griffiths B, et al. Improving health outcomes of people with diabetes mellitus: target setting to reduce the global burden of diabetes mellitus. Geneva: World Health Organization;, 2021.










