Abstract
Objective
To determine whether rural Medicare FFS beneficiaries are more likely to be admitted to an urban hospital in 2018 than in 2010.
Data Sources
We combined data from the 2010 to 2018 Hospital Service Area File (HSAF) and the 2010–2017 American Hospital Association (AHA) survey.
Study Design
We conducted a fixed‐effects negative‐binomial regression to determine whether urban hospital admissions from rural ZIP codes were increasing over time. We also conducted an exploratory geographically weighted regression.
Data Collection
We transformed the HSAF data into a ZIP code‐level file with all rural ZIP codes. We defined rural as having a Rural‐Urban Commuting Area (RUCA) code ≥4. A hospital's system affiliation status was incorporated from the AHA survey.
Principal Findings
Controlling for distance to the nearest hospitals, an increase of 1 year was associated with a 2.0% increase (p < 0.001) in the number of admissions to urban hospitals from each rural ZIP code. New system affiliation of the nearest rural hospital was associated with an increase of 1.7% (p < 0.001).
Conclusions
Even when controlling for distance to the nearest rural hospital (which reflects hospital closures), rural patients were increasingly likely to be admitted to an urban hospital.
Keywords: geographic/spatial factors/small area variations, health care organizations and systems, hospitals, Medicare, rural health
What is known on this topic
Rural hospital are continuing to close nationwide, especially in the South, which poses challenges to rural communities.
Rural hospitals are going through decreases in inpatient utilization, and these declines are disproportionately large when compared to declines in rural population.
Hospitals, both urban and rural, are joining or being acquired by larger health systems more frequently.
What this study adds
Rural hospital closures and decreased total inpatient use are not the only drivers of reduced inpatient admissions to rural hospitals; service availability and quality considerations may also contribute to this trend.
Rural patients are increasingly likely to be admitted to urban hospitals, regardless of their proximity to hospital closures.
When the nearest rural hospital joins a system, the likelihood of rural residents being admitted to an urban hospital increases, indicating that joining health systems may not increase utilization.
1. INTRODUCTION
Rural hospital inpatient volume has been decreasing steadily over the past decade. 1 , 2 MedPAC analysis finds that the average number of annual admissions per Critical Access Hospital fell from 624 in 2003 to 335 in 2016. 3 There are many possible reasons for this decline. A decline in overall utilization of inpatient services resulting from (e.g.) a decrease in rural population, an increase in payment models disincentivizing inpatient use, or a technological shift to outpatient services, may lead to fewer admissions from rural communities. Alternatively, the total inpatient volume from rural populations may be relatively unchanged but may have shifted to urban hospitals; this change in rural care‐seeking patterns may be a result of a cessation of specific services in local hospitals, patient bypass of rural hospitals (e.g., due to quality concerns), or payment models (such as accountable care organizations) enticing admission to larger urban hospitals. 4 Previous research has shown that the removal of specialty services, such as OB/GYN care, may force patients to bypass the local rural hospital and travel farther. 5 Furthermore, these service reductions may lead to declining admissions, which may, in turn, lead to a further reduction in services, feeding into a death spiral for financially vulnerable rural hospitals.
A previous study has shown that hospitals that are smaller, less profitable, and without obstetric services are more likely to be bypassed. 1 This study examines what is behind the decline in rural hospital inpatient volume, specifically, whether this decline is a result of the decline in overall patient use by rural populations or a shift in admissions from rural hospitals toward urban hospitals. We analyze changes in hospital admissions among rural Medicare FFS beneficiaries from 2010 to 2018 to determine the relative importance of (1) a change in the overall volume of acute care versus (2) a transition to urban hospitals.
2. CONCEPTUAL MODEL
Our central hypothesis was that rural hospitals are going through a decline in acute care volume, not due to a decrease in acute care used by rural residents, but to an increasing propensity for rural residents to travel farther and bypass their local hospital (Figure 1). Strictly speaking, we do not examine bypass (when a resident receives acute care from a hospital other than the closest to their residence) per se; our focus is on the type (e.g., rurality) of the hospital from which rural Medicare FFS beneficiaries are receiving inpatient care. The latter more closely aligns with the focus of work that examines aggregate volume by hospital type; a resident who bypasses a local rural hospital yet receives care from another rural hospital has different implications than one who receives it from a large urban hospital.
FIGURE 1.
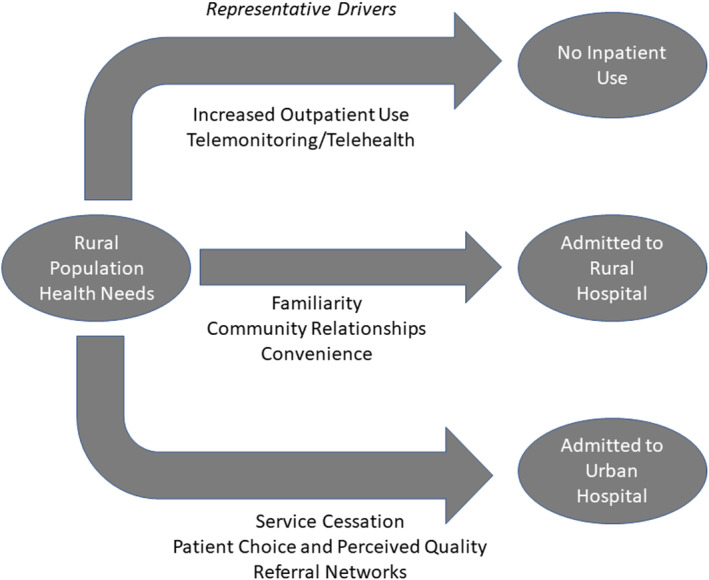
Conceptual model: drivers of patient care‐seeking behaviors [Color figure can be viewed at wileyonlinelibrary.com]
Overall per‐capita inpatient admissions have been declining for some time as more patients are treated in the outpatient setting. 6 We hypothesized that rural residents are more likely to receive care from urban hospitals for a number of reasons. First, a reduction in the services offered may drive patients to seek care elsewhere. One study found that 9% of all rural counties lost hospital‐based obstetrics services between 2004 and 2014, while others found that the gaps in access to surgical specialties, such as thoracic surgery and acute care surgery, were increasing over the same period. 7 , 8 , 9 Hospitals that lack obstetrics services are more likely to be bypassed, even for nonobstetric services. 10 Second, changes in the acute care marketplace—for example, value‐based payment and consolidation of hospitals and practices—might entice more rural patients to seek care at larger urban facilities. Recent research has shown that system‐affiliated rural hospitals were more likely to lose imaging services, obstetrics services, and primary care departments following affiliation. 11 Older research demonstrated that patients were more likely to seek certain types of care from hospitals in a network and with greater market share, typically larger hospitals. 12 Finally, rural residents may be increasingly drawn to seek care at urban hospitals due to higher perceived quality or other “consumer choice” factors.
3. METHODS
The primary data source was the Hospital Service Area File (Centers for Medicare & Medicaid Services), which contains the annual number of admissions to a hospital from each residence ZIP for Medicare FFS beneficiaries. We calculated the aerial (Euclidean) distance between the geocoded hospital and the centroid of a patient's residence ZIP. Patient residences and hospitals were classified by rurality using the ZIP modification of the 2010 Rural–Urban Commuting Area (RUCA) codes, collapsing the primary RUCA code into four categories (Metropolitan RUCA 1–3, Micropolitan: RUCA 4–6, Large rural: RUCA 7–9, and Isolated rural town: RUCA 10) for select analyses. RUCAs were classified as “Rural” if they were 4 or above, and Metropolitan RUCAs are referred to as “Urban.” For a subset of the analytic sample tested to compare travel distance versus Euclidean distance, we used the Open Source Routing Machine (OSRM) and conducted an analysis using R, and we found a high (p = 0.99) correlation between network and Euclidean distances. 13 A binary indicator of system affiliation, which indicates whether the hospital belonged to any health system, was derived from the American Hospital Association survey from 2010 to 2017.
We used two types of regression models for our analysis. First, we used a negative binomial regression with ZIP‐specific indicators “ZIP fixed effects” to calculate the change in admissions to an urban hospital from each rural ZIP code over time, holding constant the total number of admissions. Second, for exploratory analysis, we used a geographically weighted fixed‐effects Poisson regression (GWR) to visually determine which areas were experiencing the largest secular change in propensity to be admitted to rural hospitals. 14 The GWR allows parameters to vary across space by running multiple regressions at reference points across the country, with weights determined by distance from each ZIP to the point. In this case, our central points were defined as the county centroids, and thus, an individual result is interpreted as the parameter estimates in the region “close” to the point. 15 Both regressions controlled for total hospital admissions from the ZIP code, the distance to the nearest urban hospital in that year, and the distance to the nearest rural hospital in that year. Alaska and Hawaii were removed from this model because of the distinct challenges of using Euclidean distance in those areas (e.g., islands, limited road networks). We conducted a sensitivity analysis on the kernel weight used for the model and found that changes to the weight did not have a significant effect on the results of the analysis.
4. RESULTS
First, we compared admissions from rural ZIP codes with admissions to rural hospitals. If patient behavior were unchanged, then we would expect to observe similar patterns between the two as rural hospital utilization responds only to overall inpatient demand from rural areas. We found that the total number of admissions for Medicare FFS beneficiaries residing in rural RUCAs decreased only slightly from 2010 to 2018 (3.0%, 3,080,118 to 2,988,595). During the same period, admissions from urban areas increased by 7.9%, from 10,956,774 to 11,818,260. Despite only a slight decrease in total admissions from rural areas, we observed a much larger decline in admissions to rural hospitals (14.2%, 2,068,545 to 1,774,411). Figure 2 shows the distribution of admissions from each rural ZIP code to urban hospitals in 2010 and 2018. The figure suggests a broad shift in admission patterns across all rural ZIP codes rather than significant changes at either extreme (rural ZIP codes with 0% or 100% of all admissions to urban hospitals). We concluded that declines in rural hospital census could not be fully explained by declines in overall inpatient use by rural beneficiaries, and therefore, we turned to examin patient admission patterns.
FIGURE 2.
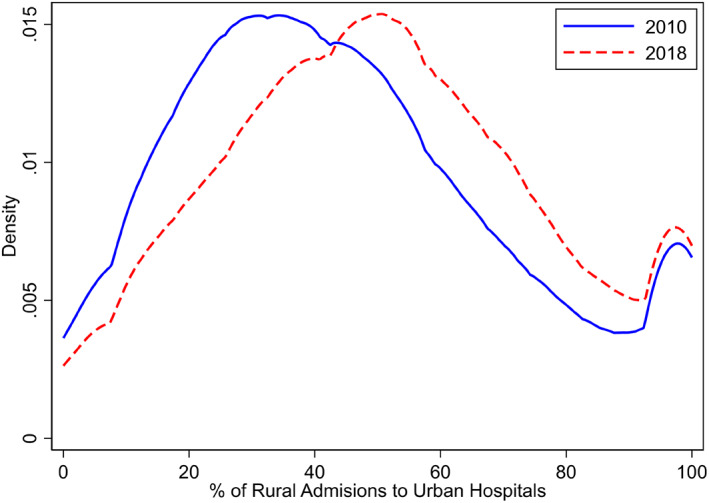
Urban hospital admissions from rural ZIP codes, 2010 and 2018 [Color figure can be viewed at wileyonlinelibrary.com]
To assess whether the change in admitting hospital rurality from rural ZIP codes could be explained by rural hospital closures, we estimated a fixed‐effects negative binomial regression, which controlled for distance to both the nearest urban and rural hospitals, with results in Table 1. Exponentiated estimated coefficients, interpreted as incidence rate ratios, are presented in brackets. Therefore, if a rural hospital closed, the distance to the nearest rural hospital would change (increase) and be accounted for in the model. Sixty‐seven ZIP codes present in Model 1 were excluded in Model 2 due to missing system‐affiliation data.
TABLE 1.
Change in number of urban hospital admissions from rural ZIP codes
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variable | Coefficient [incident rate ratio] | Std. error | Coefficient [incident rate ratio] | Std. error |
| Year | 0.0201*** [1.0203] | 0.0002 | 0.0196*** [1.0198] | 0.0002 |
| Total admissions | 0.0007*** [1.0007] | 0.0000 | 0.0007*** [1.0007] | 0.0000 |
| Distance to nearest urban hospital (mi) | −0.0014*** [0.9986] | 0.0002 | −0.0015*** [0.9986] | 0.0002 |
| Distance to nearest rural hospital (mi) | 0.0010*** [1.0010] | 0.0002 | 0.0010*** [1.0010] | 0.0002 |
| Rural hospital system affiliation | 0.0169*** [1.0170] | 0.0028 | ||
| Log‐likelihood | −414,482.01 | −352,523.71 | ||
| N of ZIP codes | 16,146 | 16,079 | ||
Note: N of total admissions = 26,953,014 (Model 1), 23,543,983 (Model 2).
*p < 0.05; **p < 0.01; ***p < 0.001.
Model 1 is the base model, including only year, total admissions, and distance to the nearest urban and rural hospitals. Model 2 includes a flag for whether the nearest rural hospital was part of a system (system affiliation of the nearest urban hospital was tested and found insignificant). System affiliation of the nearest rural hospital increased significantly over time, with 42.4% of ZIP codes being near a rural hospital in a system in 2010 compared to 50.7% in 2017. After exponentiating the coefficients, both models show a 2.0% yearly increase in the number of admissions from each rural ZIP code to urban hospitals, implying a change of 15% (1.020^7–1) over 7 years. Distance to the nearest urban hospital has a similar negative effect on the number of rural patients admitted to urban hospitals, while a one‐mile increase in distance to the nearest rural hospital (due to closure or move) was associated with an increase in the number of patients treated at urban hospitals of 0.10%. If a hospital 10 miles away from a ZIP code closed, leaving the nearest hospital now 25 miles away, this increase of 15 miles would be associated with a 1.5% (1.0010^15–1) decrease in the number of rural admissions. When compared to the yearly change in urban hospital admissions, the effect of hospital closure is significantly smaller in magnitude. New system affiliation of the nearest rural hospital is associated with a 1.8% increase in admissions to urban hospitals.
Rural hospital closures during the study period have been concentrated in the South, with 70 of 138 closures occurring in the Southeastern states along with Texas, Arkansas, and Louisiana. To assess whether changes in patient behavior reflected regional trends in closures, we conducted a fixed‐effects geographically weighted Poisson regression with observation weights decaying in distance from the ZIP of interest. The median coefficient estimate was 0.021 (indicating a 2.1% annual increase in the number of urban admissions), with an IQR of 0.011–0.031. We found no statistically significant differences in the estimates for ZIP codes in different regions (including the Southeast), and also found no differences when stratifying ZIP codes into rural subgroups of micropolitan, largely rural, and isolated. Visual assessment of the regression results did not reveal any obvious geographic patterns, with high and low rates of change present throughout different parts of the country and not clustered in one area. These results demonstrate that changes in rural patient behavior do not correlate with regional trends in hospital closures.
5. DISCUSSION
There are four primary findings from this study. Between 2010 and 2018: (1) no large change in the total number of inpatient admissions from rural areas occurred; (2) rural Medicare FFS beneficiaries are increasingly likely to be admitted to urban hospitals and less likely to be admitted to rural hospitals; (3) system affiliation of rural hospitals may be a factor in the decision to bypass; and (4) changes in urban hospital admissions from urban areas are not geographically concentrated nor concentrated around areas with hospital closures. The decline in acute volume in rural hospitals, combined with the finding of relatively unchanged total admissions from rural areas, appears to be far more driven by changes in care‐seeking behaviors such as increased hospital bypass rather than by a secular decline in admissions of rural beneficiaries.
Decreasing admissions could negatively affect the financial health of a hospital, which may, in turn, affect the ability of the hospital to remain open or to provide the same level of services. 16 , 17 Increased travel distance and hospital bypass behavior also have implications for access and can increase the burden for patients and families. 18 , 19 Isolated rural Medicare beneficiaries are already less likely to have follow‐up care, while micropolitan and small‐town rural beneficiaries have a greater risk of readmission and ED visits. 20 Particularly in emergencies, longer travel time and distance can be detrimental to health outcomes. 21
This trend of the declining rural census may support the creation or increase of alternative rural care delivery models, such as freestanding emergency departments (EDs) or the frontier community health care models, which can address some of the potential detriments of increased travel distance by reducing emergency response time. 22 , 23 Indeed, MedPAC's recommendation to create rural stand‐alone emergency departments specifically draws from this volume trend. 3 Currently, most freestanding EDs are near existing EDs, limiting their effectiveness for this purpose, but the strategic placement could improve their potential impact. 22 However, Congress authorized the creation of Rural Emergency Hospitals (REHs) in 2020, which do not have to provide inpatient care but may offer 24‐hour emergency services, and the effects of this policy have yet to be borne out. 24
Despite potentially negative financial consequences for rural health systems, rural patients may benefit from treatment at urban hospitals. Larger, typically urban hospitals may be more appropriate for complex patients and those receiving some types of surgical care. 10 , 25 , 26 Comparisons of quality at urban and rural hospitals have found that some but not all quality measure scores may be lower for rural hospitals, and the benefit of bypassing a rural to an individual patient may depend on the patient's clinical characteristics, as well as characteristics of the hospital. 27 , 28 , 29 , 30
The analysis has some limitations. The data used exclude admissions not insured by Medicare FFS, such as Medicare Advantage, Medicaid, and commercial. Enrollment in Medicare Advantage is nonrandom and may lead to different outcomes, although the effect is unclear, with some studies finding mixed associations for Medicare Advantage enrollment and hospital admissions. 31 , 32 , 33 Enrollment in Medicare Advantage in rural areas is small but rising, and the effects of Medicare Advantage on rural hospitals will increase correspondingly. 34 Medicare admission patterns may differ from patterns for those insured by other programs. Last, as the distance is calculated as aerial miles, the distance does not reflect actual travel time. However, we tested potential differences by calculating a subsample of travel distances using a road network, and regression of network travel distance on Euclidean distance resulted in an R 2 of 0.991, indicating that Euclidean distance is a very strong linear predictor of travel distance. Additionally, other studies have supported the use of aerial distance and found that in the case of nonemergency hospital visits, the difference between Euclidean distance and road network distance is inconsequential. 35
6. CONCLUSION
Between 2010 and 2018, the proportion of rural residents admitted to rural hospitals decreased. This was driven more by changes in care‐seeking than secular declines in admission rates among rural residents. If fewer rural residents continue to seek care from rural hospitals, more rural hospitals could find it difficult to maintain their current level of services or to remain open at all, leading to reduced access to care for those still relying on them for inpatient care. Rural hospitals will need to adapt to changing patient care‐seeking behaviors as rural residents continue to travel farther to urban hospitals for care.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
This study was partially supported by the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), US Department of Health and Human Services (HHS) under cooperative agreement # U1GRH03714. The information, conclusions, and opinions expressed in this manuscript are those of the authors, and no endorsement by FORHP, HRSA, HHS, or The University of North Carolina is intended or should be inferred. Any interpretations, conclusions, and/or opinions reached as a result of analyses of the data sets are those of the authors and do not constitute the findings, policies, or recommendations of the US Government, the US Department of Health and Human Services, or AHRQ. This research was also partially supported by a National Research Service Award Pre‐Doctoral Traineeship from the Agency for Health care Research and Quality sponsored by The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, Grant No. T32‐HS000032.
Friedman HR, Holmes GM. Rural Medicare beneficiaries are increasingly likely to be admitted to urban hospitals. Health Serv Res. 2022;57(5):1029‐1034. doi: 10.1111/1475-6773.14017
Funding information Agency for Healthcare Research and Quality, Grant/Award Number: T32‐HS000032; Federal Office of Rural Health Policy, Grant/Award Number: # U1GRH03714; US Department of Health and Human Services (HHS); Health Resources and Services Administration (HRSA)
REFERENCES
- 1. Malone T, Holmes M. Patterns of hospital bypass and inpatient care‐seeking by rural residents. NC Rural Health Research Program. 2019.
- 2. Malone TL, Pink GH, Holmes GM. Decline in inpatient volume at rural hospitals. J Rural Health. 2020;37:347‐352. doi: 10.1111/jrh.12553 [DOI] [PubMed] [Google Scholar]
- 3. Matthews JE. Ensuring access to emergency services for Medicare beneficiaries in rural communities. Medicare Payment Advisory Commission (MedPAC). 2018.
- 4. Abrams K, Balan‐Cohen A, Durbha P. Growth in outpatient care: the role of quality and value incentives. Deloitte. 2018.
- 5. Hung P, Kozhimannil KB, Casey MM, Moscovice IS. Why are obstetric units in rural hospitals closing their doors? Health Serv Res. 2016;51(4):1546‐1560. doi: 10.1111/1475-6773.12441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McDermott KW, Elixhauser A, Sun R. Patient trends in hospital inpatient stays in the United States, 2005–2014. Healthcare Cost and Utilization Project (HCUP). 2017.
- 7. Hung P, Henning‐Smith CE, Casey MM, Kozhimannil KB. Access to obstetric services in rural counties still declining, with 9 percent losing services, 2004‐14. Health Aff. 2017;36(9):1663‐1671. doi: 10.1377/hlthaff.2017.0338 [DOI] [PubMed] [Google Scholar]
- 8. Eberth JM, Crouch EL, Josey MJ, et al. Rural‐urban differences in access to thoracic surgery in the United States, 2010 to 2014. Ann Thorac Surg. 2019;108(4):1087‐1093. doi: 10.1016/j.athoracsur.2019.04.113 [DOI] [PubMed] [Google Scholar]
- 9. Khubchandani JA, Ingraham AM, Daniel VT, Ayturk D, Kiefe CI, Santry HP. Geographic diffusion and implementation of acute care surgery: an uneven solution to the national emergency general surgery crisis. JAMA Surg. 2018;153(2):150‐159. doi: 10.1001/jamasurg.2017.3799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weigel PAM, Ullrich F, Finegan CN, Ward MM. Rural bypass for elective surgeries. J Rural Health. 2017;33(2):135‐145. doi: 10.1111/jrh.12163 [DOI] [PubMed] [Google Scholar]
- 11. O'Hanlon CE, Kranz AM, DeYoreo M, Mahmud A, Damberg CL, Timbie J. Access, quality, and financial performance of rural hospitals following health system affiliation. Health Aff. 2019;38(12):2095‐2104. doi: 10.1377/hlthaff.2019.00918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Roh C‐Y, Lee K‐H, Fottler MD. Determinants of hospital choice of rural hospital patients: the impact of networks, service scopes, and market competition. J Med Syst. 2008;32(4):343‐353. doi: 10.1007/s10916-008-9139-7 [DOI] [PubMed] [Google Scholar]
- 13. Project OSRM. http://project-osrm.org/. Accessed October 12, 2020.
- 14. Bui LV, Mor Z, Chemtob D, Ha ST, Levine H. Use of geographically weighted Poisson regression to examine the effect of distance on tuberculosis incidence: a case study in Nam Dinh, Vietnam. PLoS One. 2018;13(11):e0207068. doi: 10.1371/journal.pone.0207068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ricketts TC, Holmes GM. Mortality and physician supply: does region hold the key to the paradox? Health Serv Res. 2007;42(6 Pt 1):2233‐2251; discussion 2294. doi: 10.1111/j.1475-6773.2007.00728.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Holmes GM, Kaufman BG, Pink GH. Predicting financial distress and closure in rural hospitals. J Rural Health. 2017;33(3):239‐249. doi: 10.1111/jrh.12187 [DOI] [PubMed] [Google Scholar]
- 17. Thomas SR, Holmes GM, Pink GH. To what extent do community characteristics explain differences in closure among financially distressed rural hospitals? J Health Care Poor Underserved. 2016;27(4A):194‐203. doi: 10.1353/hpu.2016.0176 [DOI] [PubMed] [Google Scholar]
- 18. Mohr NM, Harland KK, Shane DM, et al. Rural patients with severe sepsis or septic shock who bypass rural hospitals have increased mortality: an instrumental variables approach. Crit Care Med. 2017;45(1):85‐93. doi: 10.1097/CCM.0000000000002026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hoffman AF, Pink GH, Kirk DA, Randolph RK, Holmes GM. What characteristics influence whether rural beneficiaries receiving care from urban hospitals return home for skilled nursing care? J Rural Health. 2020;36(1):94‐103. doi: 10.1111/jrh.12365 [DOI] [PubMed] [Google Scholar]
- 20. Toth M, Holmes M, Van Houtven C, Toles M, Weinberger M, Silberman P. Rural Medicare beneficiaries have fewer follow‐up visits and greater emergency department use postdischarge. Med Care. 2015;53(9):800‐808. doi: 10.1097/MLR.0000000000000401 [DOI] [PubMed] [Google Scholar]
- 21. Bazzoli GJ, Lee W, Hsieh H‐M, Mobley LR. The effects of safety net hospital closures and conversions on patient travel distance to hospital services. Health Serv Res. 2012;47(1 Pt 1):129‐150. doi: 10.1111/j.1475-6773.2011.01318.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Freeman RE, Boggs KM, Sullivan AF, Faridi MK, Freid RD, Camargo CA. Distance from freestanding emergency departments to nearby emergency care. Ann Emerg Med. 2020;77:48‐56. doi: 10.1016/j.annemergmed.2020.07.036 [DOI] [PubMed] [Google Scholar]
- 23. Centers for Medicare and Medicaid Services . Demonstration project on community health integration models in certain rural counties. Department of Health and Human Services. 2020.
- 24. Pink G, Thompson K, Howard A, Holmes GM. How many hospitals might convert to a rural emergency hospital (REH)? UNC Sheps Center: NC Rural Health Research Program. 2021.
- 25. Schroeder MC, Gao X, Lizarraga I, Kahl AR, Charlton ME. The impact of commission on cancer accreditation status, hospital rurality and hospital size on quality measure performance rates. Ann Surg Oncol. 2022;29(4):2527‐2536. doi: 10.1245/s10434-021-11304-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang Y, Malone T, Cantrell S, et al. Predictors of hospital choice among rural patients seeking elective surgery: a scoping review. Cecil G. Sheps Center for Health Services Research: NC Rural Health Research Program; 2022.
- 27. Joynt KE, Harris Y, Orav EJ, Jha AK. Quality of care and patient outcomes in critical access rural hospitals. JAMA. 2011;306(1):45‐52. doi: 10.1001/jama.2011.902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Joynt KE, Orav EJ, Jha AK. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Ann Intern Med. 2011;154(2):94‐102. doi: 10.7326/0003-4819-154-2-201101180-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ambardekar AV, Fonarow GC, Dai D, et al. Quality of care and in‐hospital outcomes in patients with coronary heart disease in rural and urban hospitals (from get with the guidelines‐coronary artery disease program). Am J Cardiol. 2010;105(2):139‐143. doi: 10.1016/j.amjcard.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 30. Lansing SS, Diaz A, Hyer M, Tsilimigras D, Pawlik TM. Rural hospitals are not associated with worse postoperative outcomes for colon cancer surgery. J Rural Health. 2021;38:650‐659. doi: 10.1111/jrh.12596 [DOI] [PubMed] [Google Scholar]
- 31. Li Y, Cen X, Cai X, Thirukumaran CP, Zhou J, Glance LG. Medicare advantage associated with more racial disparity than traditional medicare for hospital readmissions. Health Aff. 2017;36(7):1328‐1335. doi: 10.1377/hlthaff.2016.1344 [DOI] [PubMed] [Google Scholar]
- 32. Clement JP, Khushalani J, Baernholdt M. Urban‐rural differences in skilled nursing facility rehospitalization rates. J Am Med Dir Assoc. 2018;19(10):902‐906. doi: 10.1016/j.jamda.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 33. Baicker K, Chernew ME, Robbins JA. The spillover effects of Medicare managed care: Medicare advantage and hospital utilization. J Health Econ. 2013;32(6):1289‐1300. doi: 10.1016/j.jhealeco.2013.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gold M, Casillas G. What do we know about health care access and quality in Medicare advantage versus the traditional Medicare program? The Kaiser Family Foundation. 2014.
- 35. Boscoe FP, Henry KA, Zdeb MS. A nationwide comparison of driving distance versus straight‐line distance to hospitals. Prof Geogr. 2012;64(2):188‐196. doi: 10.1080/00330124.2011.583586 [DOI] [PMC free article] [PubMed] [Google Scholar]


