The full-scale Russian invasion of Ukraine on February 24, 2022, brought the largest humanitarian disaster since World War II to the heart of Europe. The Russian army has caused absolute destruction and chaos for everyone in its path, and Ukraine has lost tens of thousands of civilian lives, out of which many were innocent children. Many more have been wounded, and approximately one-third of the population of Ukraine has been displaced: 7 million as refugees and 7.1 million as internally displaced people.1 The Russian army is obliterating Ukrainian cities, targeting critical civilian infrastructure with missiles, and deliberately damaging and destroying hospitals and clinics in violation of Article IV of the Geneva Convention.2 According to Ukraine's Minister of Health, Viktor Lyashko, during the first 100 days of war, more than 600 health care facilities sustained damage, 105 of which were rendered damaged beyond repair.3 Even if the war stopped today, the damage to the health care infrastructure will remain for years to come without the world's continuing support.
Before the full-scale Russian invasion, according to unpublished Ukrainian National Cancer Institute (Tumor Registry) data, an estimated 139,000 people in Ukraine (which has a population of 44 million) were living with newly diagnosed cancer, and between 1000 and 1200 children were receiving active cancer treatment.4 With regard to radiation therapy, Ukraine is classified by the International Atomic Energy Agency's Directory of Radiotherapy Centres as a low- to middle-income country, with the level of availability of external beam radiation therapy (EBRT) machines being 2.6 per 1 million people.5 Until Russia annexed Crimea and parts of the Donbas region in 2014, Ukraine had 52 radiation therapy centers with 86 Co-60 machines (81%) and 20 linear accelerators (19%).5 Since 2014, Ukraine has lost control of 10 cancer centers and more than 13 EBRT machines in the occupied parts of Donbas and 5 machines in Crimea (in total, 17% of Ukrainian EBRT machines).6 To address the growing need for cancer treatment, 16 linear accelerators were installed by 2022, and the ratio of Co-60 machines to linear accelerators became 54% to 46% (without taking into account EBRT machines in the occupied territories since 2014). The Ministry of Health of Ukraine planned to purchase 20 additional linear accelerators, but this plan did not materialize because the Russian full-scale invasion shattered Ukraine in the early hours of February 24. In the fourth month of the war, the situation in Ukraine was fluid, and as of June 10, 2022, 3 additional cancer centers were under occupation, 3 cancer centers had suspended operation, and 2 cancer centers were under constant shelling (Fig 1). Some of the centers in the west of Ukraine operate with double the volume of patients.
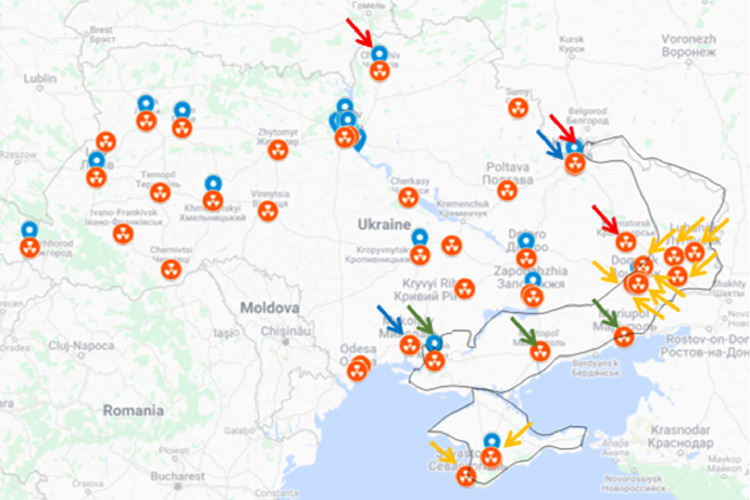
Fig. 1.
Map of the cancer centers providing external beam radiation therapy in Ukraine as of June 2022. The orange radiation symbol denotes Co-60 machines and the blue symbol denotes linear accelerators. Orange arrows show the radiation therapy centers under Russian occupation since 2014, green arrows show the radiation therapy centers under Russian occupation after full-scale invasion in 2022, blue arrows show the centers working under constant shelling as of June 2022, and red arrows show the centers that suspended operation as of June 2022. Source: https://dirac.iaea.org/, supplemented by the data from Ruslan Zelinskyi.
Ruslan Zelinskyi, president of the Ukrainian Association of Medical Physicists, and Nataliya Kovalchuk, a clinical associate professor at Stanford University, interviewed radiation oncologists from 2 radiation oncology centers: Dr Andrii Hanych, the chair of the Radiation Oncology Department at Mariupol Oncological Dispensary, and Dr Yuliia Severyn, a radiation oncologist at the National Specialized Children's Hospital OKHMATDYT in Kyiv.
Mariupol Oncological Dispensary
Dr Andrii Hanych: “We were not really prepared for the war. The only provision we made was for a large quantity of bandages to care for the wounded. After constant attacks on Mariupol, we started to experience the shutdown of electricity. To continue treating our patients, we tried to connect the generator, which proved to be very challenging, as the simultaneous gantry rotation with compressor was very power consuming. We eventually stopped treating as the situation in the city deteriorated and there was nobody to pick up the dead on the streets. In our hospital, [corpses were] stored for 5 to 6 days. At that point, we decided that we could not continue treating in these conditions. Our foremost goal was to preserve the lives of our patients and to make their stay at our hospital acceptable.
“At the time when the military action started, we had 12 patients in our care. Those were the patients who had nowhere to go, as their homes were either destroyed or were without electricity, water, or gas. We believe we saved the lives of these patients. The most important task for us at the time was to find the potable and technical water. Fortunately, in March it was still snowing, so sufficient technical water could be sourced from the melted snow. Then, the gas supply was cut off. The only source of heat that remained was the generator with a small amount of gasoline. We abandoned using the generator for treatment, but rather used it for cooking and feeding our patients and staff. To hide from the missiles, we decided to house our patients in the corridors and vault of the Co-60 machine.
“One night I heard a noise from the shattered glass and found a piece of shrapnel (Fig 2). I realized it was becoming very dangerous for our patients to stay in the hospital, as the fighting was approaching and becoming more intense. I made a decision to ask the Ukrainian military to start evacuating our patients. It was a well-timed decision, as only 2 hours after the evacuation bus departed, a missile hit our department (Fig 3).
Fig. 2.
Dr Andrii Hanych, chair of the Radiation Oncology department at Mariupol Oncological Dispensary during the interview, shows a piece of shrapnel that hit the hospital while he and his patients were sheltering inside. He made a decision to contact the Ukrainian military to evacuate the patients immediately. A few hours after the evacuation bus departed, the missile hit the radiation oncology department (Video 1 in the Supplement).
Fig. 3.
A Mariupol oncological dispensary hit by a missile 2 hours after the patients evacuated. The fate of the Co-60 source is unknown (Video 2 in the Supplement).
“As the shelling intensified to approximately every minute, we decided to leave Mariupol. We did not have any transportation and had to leave the city on foot. While walking out of the city, we were under fire, and one of my fellow oncologists was wounded in the leg, but luckily we all survived, and after walking 15 to 18 km along the beach of the Sea of Azov, arrived to a relatively safer area.”
Dr Hanych took a long, contemplative pause and continued: “While staying in the bunker and hearing the whistling of the shells falling next to me, I felt the loss of faith in the big international peace organizations and the purpose they serve. This should not be happening in the 21st century in the heart of Europe. This should not be happening anywhere.
“Currently, in the occupied Mariupol, we cannot control the radiation equipment or sources. There are no radiation oncologists, physicists, or radiation safety officers there. It really hurts to say that I cannot guarantee the radiation safety; I couldn't guarantee it then when I was there, but at least it was under my supervision. I do not know what is happening there now nor the fate of the Co-60 source.”
Dr Hanych was lucky to escape Mariupol alive and currently works as a radiation oncologist at the Khmelnytskyi antitumor center in the west of Ukraine. According to the mayor of Mariupol, an estimated 22,000 Mariupol residents died in the first 2 months of war, although The Guardian reported a staggering 50,000 dead in Mariupol alone.7
National Specialized Children's Hospital OKHMATDYT, Kyiv
Dr Yuliia Severyn: “I received the notification about the start of invasion through my work chat channels (Video 3 in the Supplement). The radiation therapy department at the National Specialized Children's Hospital OKHMATDYT was treating 17 patients, 13 of them pediatric patients, using the recently upgraded linear accelerator Elekta Synergy. Due to the collapse in [the] transportation system, many of the staff could not get to work, and some of the staff decided to live in the department to enable treatments to continue. The radiation therapy department located on the first floor was used as a bomb shelter: we were housing not only our staff and patients but also the patients from [the] hematology and neurosurgery departments.
“Since the full invasion began, we never halted operations and started providing radiation therapy not only for children but also for adults. On March 2nd, with the help of “Tabletochki,” a nonprofit foundation in Ukraine,8 a few pediatric cancer patients were evacuated to safer areas in the west of Ukraine or abroad, but the majority of parents had not realized the gravity of the situation, and the department still treated approximately 10 pediatric patients a day. On March 9th, only 5 patients remained on treatment in the department, but due to radiation therapy department closures in the surrounding areas of Kyiv, more adult patients were referred to us. On March 25th, we treated only 6 adult patients, some of whom lived in the department due to the constant air raids in Kyiv and the long curfew hours. Patients felt very grateful, and despite the risk of falling missiles, found and brought flowers for the staff.
“The chair of the department, Lyudmyla Vintsevych, 2 radiation therapists, and 1 medical physicist made the decision to live in the hospital 24/7 to provide diagnostic services for the wounded. The Toshiba CT [computed tomography] scanner, usually used for CT simulations, began to be used for diagnostic purposes (Fig 4). As the missiles hit and damaged the hospital multiple times, it was important to minimize patient transportation outside between the separate hospital buildings, to keep them safe.
Fig. 4.
OKHMATDYT's simulation computed tomography is used for diagnostic purposes. This individual, unfortunately, died of his wounds.
“We started diagnosing the wounded using our CT scanner on April 26th. Our first diagnostic patients were a family with 2 children: a 6-year-old boy and a 12-year-old girl who had been shot at. The boy was already dead upon arrival, and the girl's leg was wounded. Parents were in a very difficult physiological state. Almost every day we had a similar case, scanning around 5 trauma patients a day, many of whom were children. Bohdana Bachynska, OKHMATDYT's Radiation Therapy Technician, recounted a 5-year-old boy with [a] large wound on his lower back (Fig 5). She asked him if he was in pain, and he responded, ‘I am holding on despite the pain.’ I think this 5-year-old boy is a great metaphor for Ukraine. Ukraine is bleeding but holding on. Another of our radiation therapists, Yana Kuts, served as an emergency technician in the Ukrainian army and frequently accompanied the wounded to OKHMATDYT (Fig 6). They are our department's heroes.
Fig. 5.
OKHMATDYT's staff is taking care of a 5-year-old boy wounded in the back (Video 4 in the Supplement).
Fig. 6.
OKHMATDYT's Radiation Therapy Technician heroes: Bohdana Bachynska (left) and Yana Kuts (right). Bohdana stayed in OKHMATDYT 24/7 to scan wounded patients, and Yana serves in the Ukrainian army as an emergency medical technician.
“Around mid-April, pediatric patients started to arrive for radiation therapy treatment. As of June 9, we are treating 10 patients, 6 of whom are children. Since the invasion, under the constant threat of missiles and air raids, we treated 26 patients; among them, 11 were pediatric patients.” Dr Severyn took a long pause, then said, “I will never forget the long row of shoes at the entrance to the department.”
How Can We Help?
We previously spoke to Dr Andriy Beznosenko, chief medical officer of the National Cancer Institute in Kyiv and the president of the Ukrainian Society of Medical Oncology,9 who said, “There is an acute need for chemotherapy medications and disposable medical devices. The supply chains became disrupted by the war, and the hospital is running out of medication.” Many medical warehouses were destroyed or are unavailable owing to logistical issues, airports are not operational, and many bridges and highways are damaged. For the centers in the west of Ukraine, with the patient volume doubling, humanitarian help with medication, supplies, and staffing is needed to meet the demands. Ruslan Zelinskyi, president of the Ukrainian Association of Medical Physicists; Oleksandr Sakharenko, counsel of Aretera Public Affairs; Viktor Iakovenko, a medical physicist at UT Southwestern; and Nataliya Kovalchuk, a medical physicist at Stanford University organized to collect and fundraise for the currently needed disposable immobilization devices for radiation therapy. Vendors (Orfit and CIVCO) are very receptive to helping Ukraine. The Union for International Cancer Control created the Solidarity Fund for Ukraine to bridge the gap and help the organizations caring for cancer patients in Ukraine and the surrounding region.10
People can petition hospitals to help Ukraine. Stanford Hospital donated $165,000 worth of medical supplies to Ukraine via the Nova Ukraine foundation,11 and the Ukrainian Student Association at Stanford University, together with Nova Ukraine, shipped 80 tons ($4 million worth) of medical supplies to Ukraine. The Mayo Clinic organized a matched-donation fundraiser. John Hopkins Medicine and the University of Maryland Medical System donated $4 million worth of medical supplies: personal protective equipment, medical air compressors, syringes, respirator kits, and even hospital beds. The administration of Zaporizzhia city is petitioning for a field hospital to take care of wounded civilians, and we are currently helping with connecting them to donors.
Ukraine, a country of 44 million people, has only 3 positron emission tomography (PET) / CT scanners, all in Kyiv, and only 2 of them are functioning after the full-scale Russian invasion in February; thus, patients from all over Ukraine have to risk their life traveling to Kyiv for a diagnostic scan or follow-up PET/CT scan. According to the European Association of Nuclear Medicine, there should be at least 1 PET/CT scanner per 1.5 to 2 million people, which would translate into 22 scanners for Ukraine. Together with Nelya Melnitchouk, Oleh Duda, and Andriy Beznosenko, we are petitioning PET/CT scanner and cyclotron vendors to donate at least one PET/CT scanner and cyclotron to the Lviv Oncology Regional Therapeutic and Diagnostic Center to overcome disparities for Ukrainian cancer patients during the war. Furthermore, Ukraine has cyclotrons with only 18FDG production. Highly specialized centers such as OKHMATDYT and the National Cancer Institute in Kyiv need a cyclotron that produces different tracers.
Asya Agulnik, director of St. Jude's Global Critical Care Program, has been an amazing driving force at coordinating evacuation and triaging of pediatric patients from Ukraine in collaboration with Tabletochki (a Ukrainian nonprofit organization helping with evacuation of more than 850 pediatric cancer patients) and organizations in Poland, Moldova, Italy, Spain, Romania, and Germany. The SAFER Ukraine website12 shows a map of the countries and institutions that have volunteered to accept hematology and oncology patients and their families from Ukraine. People can petition cancer centers to help bring Ukrainian pediatric patients for treatment or donate to help fundraising efforts that support evacuation of pediatric cancer patients.8
In a speech at a European Cancer Organisation–American Society of Clinical Oncology meeting, Andriy Hrynkiv, a surgical oncologist at the Lviv Regional Cancer Center, called for the development of a cancer support network for Ukrainian refugees. Both European Cancer Organisation and American Society of Clinical Oncology are urging cancer groups that are able to contribute services, resources, or contacts to join the network.13 We are organizing sessions on Ukraine at various annual professional meetings (American Society for Radiation Oncology, American Association of Physicists in Medicine, Canadian Organization of Medical Physicists, Medical Physics for World Benefit, and the 2022 World Congress on Medical Physics and Biomedical Engineering) to inform on the situation in Ukraine with constructive suggestions on how to help.
Upon Dr Beznosenko's request, Nelya Melnitchouk, a surgeon at Brigham and Women's Hospital, and Nataliya Kovalchuk are organizing a training program in the US and Canada for Ukrainian female physicians of various specialties (radiation oncologists, medical oncologists, surgeons, anesthesiologists, and pathologists). In parallel, Ruslan Zelinskyi has compiled a list of curriculum vitae from Ukrainian female medical physicists, some of whom are currently displaced. Viktor Iakovenko and Nataliya Kovalchuk are working on finding positions for female Ukrainian medical physicists. Institutions willing to provide funding for a visiting scholarship or fellowship for Ukrainian female doctors or medical physicists can contact the authors. Nelya Melnitchouk, through her 501(c)(3) nonprofit organization Global Medical Knowledge Alliance,14 created a fundraiser to help collect funds to cover the travel and initial expenses for Ukrainian female physicians and physicists.15
Roman Kowalchuk, a radiation oncology resident at the Mayo Clinic, is collaborating with the Ukrainian Medical Association of North America (UMANA),16 a nonprofit organization composed of 19 branches throughout the US and Canada, to help organize telemedicine support for Ukrainian patients. The Ukrainian Medical Association of North America is working on telemedicine efforts, partnering with Viveo, a telemedicine platform from Estonia, and Doctors4UA, a platform developed by BeKey. A team of medical and computer science students at Stanford University, led by Solomiia Savchuk, created the TeleHelp Ukraine initiative to provide remote medical advice and mental health support for Ukrainians with the help of American doctors, volunteers, and a team of interpreters. We are grateful to MIM Software Inc for providing a free software license to host a MIM cloud Digital Imaging and Communication in Medicine repository for medical images for Ukrainian patients to further inform the video consultations. These telemedicine efforts urgently need physicians of every specialty.17, 18, 19
We call on radiation oncology vendors represented in Ukraine, such as Varian, Elekta, and Accuray, to enhance their support, donate equipment, and facilitate the maintenance and service of radiation oncology equipment. Ukrainians are grateful to Varian/Siemens Healthineers for creating a €1 million matched fundraiser to help Ukraine with humanitarian needs. Siemens also donated 3 x-ray systems and 4 C-arm machines to various locations in Ukraine. We are also grateful to Limbus AI Inc and RADformation for providing free licenses for automatic contouring software, plan check, 3D planning to Ukrainian cancer centers, which will facilitate streamlining the treatment planning workflow.
Even if the war were to stop today, the effects of the decimated health care system in Ukraine will last for years to come. It is imperative that the effective cancer recovery plan in Ukraine should have radiation therapy at its heart, with precise coordination between governing bodies, professional organizations, multidisciplinary professionals, volunteers, and industry.20 However, all of these efforts start with individuals, and the individual power and will of Ukrainians to fight for their people, including their cancer patients, is truly inspiring. Let's help these Ukrainian doctors and heroes to win over 2 evils: cancer and the war.
Acknowledgments
Interview videos were translated and subtitled by Natalka Suchowerska and Ruslan Zelinskyi. They attest that the subtitles are correct to the best of their abilities.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.adro.2022.101027.
Appendix. Supplementary materials
References
- 1.OCHA Services. Ukraine humanitarian crisis. Available at: https://reliefweb.int/topics/ukraine-humanitarian-crisis. Accessed July 1, 2022.
- 2.United Nations. Geneva Convention relative to the protection of civilian persons in time of war of 12 August 1949. Available at:https://www.un.org/en/genocideprevention/documents/atrocity-crimes/Doc.33_GC-IV-EN.pdf. Accessed July 1, 2022.
- 3.Available at: https://moz.gov.ua/. Accessed July 1, 2022.
- 4.Kizub D, Melnitchouk N, Beznosenko A, et al. Resilience and perseverance under siege: Providing cancer care during the invasion of Ukraine. Lancet Oncol. 2022;23:579–583. doi: 10.1016/S1470-2045(22)00189-9. [DOI] [PubMed] [Google Scholar]
- 5.Directory of Radiotherapy Centres. What is DIrectory of RAdiotherapy Centres (DIRAC)? International Atomic Energy Agency (IAEA). Available at: https://dirac.iaea.org/. Accessed July 1, 2022.
- 6.Starenkiy VP, Petrichenko OO, Averyanova L. External beam radiotherapy facilities in Ukraine: Trends and challenges. Problems of Atomic Science and Technology. 2017;112:126–129. [Google Scholar]
- 7.The Guardian. Makeshift graves and notes on doors: The struggle to find and bury Mariupol's dead. Available at: https://www.theguardian.com/world/2022/jun/01/makeshift-graves-and-notes-on-doors-the-struggle-to-find-and-bury-mariupol-dead-ukraine. Accessed July 1, 2022.
- 8.Tabletochki. Available at: https://tabletochki.org/en/. Accessed July 1, 2022.
- 9.Kovalchuk N, Beznosenko A, Kowalchuk R, Ryzhkova J, Iakovenko V, Kacharian A. While Ukrainian soldiers are fearlessly defending their country, Ukrainian oncologists are bravely battling cancer. Adv Radiat Oncol. 2022;7 doi: 10.1016/j.adro.2022.100965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Union for International Cancer Control UICC Solidarity Fund for Ukraine opens call for grants to qualifying organisations. https://www.uicc.org/news/uicc-solidarity-fund-ukraine-opens-call-grants-qualifying-organisations Available at:
- 11.Available at: https://novaukraine.org/ Accessed July 1, 2022.
- 12.Available at: https://global.stjude.org/en-us/saferukraine.html. Accessed July 1, 2022.
- 13.European Cancer Organisation. ECO-ASCO Special Network: Impact of the war in Ukraine on cancer. Available at: https://www.europeancancer.org/topic-networks/20:impact-war-in-ukraine-on-cancer.html. Accessed July 1, 2022.
- 14.Available at: https://gmka.org/. Accessed July 1, 2022.
- 15.Available at: https://gofund.me/1b461c3a. Accessed August 23, 2022.
- 16.Available at: https://www.umana.org/. Accessed July 1, 2022.
- 17.Available at: https://doctors4ua.com/. Accessed July 1, 2022.
- 18.Available at: https://viveohealth.com/free-online-doctor-consultation-for-ukraine/. Accessed July 1, 2022.
- 19.Available at: https://www.telehelpukraine.com/i-want-to-help-1. Accessed July 1, 2022.
- 20.Price P, Sullivan R, Zubarev M, Zelinskyi R. Radiotherapy in conflict: Lessons from Ukraine. Lancet Oncol. 2022;23:845–847. doi: 10.1016/S1470-2045(22)00298-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.