Abstract
Introduction
Changes in carbohydrate metabolism may lead to recurrence of benign paroxysmal positional vertigo.
Objective
To evaluate the influence of the disturbance of carbohydrate metabolism in the recurrence of idiopathic BPPV.
Methods
A longitudinal prospective study of a cohort, with 41 months follow-up. We analyzed the results of 72 glucose–insulin curves in patients with recurrence of BPPV. The curves were classified into intolerance, hyperinsulinemia, hyperglycemia and normal.
Results
The RR for hyperinsulinism was 4.66 and p = 0.0015. Existing hyperglycemia showed an RR = 2.47, with p = 0.0123. Glucose intolerance had a RR of 0.63, with p = 0.096. When the examination was within normal limits, the result was RR = 0.2225 and p = 0.030.
Discussion
Metabolic changes can cause dizziness and vertigo and are very common in people who have cochleovestibular disorders. However, few studies discuss the relationship between idiopathic BPPV and alterations in carbohydrate metabolism. In the present study, we found that both hyperglycemia and hyperinsulinemia are risk factors for the recurrence of BPPV, whereas a normal test was considered a protective factor; all these were statistically significant. Glucose intolerance that was already present was not statistically significant in the group evaluated.
Conclusion
Hyperinsulinemia and hyperglycemia are risk factors for the recurrence of idiopathic BPPV and a normal exam is considered a protective factor.
Keywords: Vertigo, Glucose metabolism disorders, Carbohydrate metabolism, Dizziness
Resumo
Introdução
As alterações do metabolismo do carboidrato podem levar a recorrência de vertigem posicional paroxística benigna.
Objetivo
Avaliar a influência dos distúrbios do carboidrato na recorrência da VPPB idiopática.
Método
Estudo longitudinal, do tipo coorte, prospectivo, com 41 meses de acompanhamento. Analisaram-se 72 resultados de curvas glicoinsulinêmicas em pacientes portadores de recorrência de VPPB. As curvas foram classificadas em intolerância, hiperinsulinemia, hiperglicemia e normal.
Resultados
O hiperinsulinismo teve RR = 4,66 e p = 0,0015. A hiperglicemia apresentou um RR = 2,47 e p = 0,0123. Na intolerância a glicose o RR = 0,63 e p = 0,096. No exame normal, o RR = 0,2225 e p = 0,030.
Discussão
As alterações metabólicas podem causar tontura e vertigem e são muito frequentes na população que apresenta distúrbios cocleovestibulares. Contudo, poucos trabalhos falam sobre a relação entre a VPPB idiopática e as alterações nos carboidratos. No presente estudo, verificou-se que tanto a hiperglicemia, quanto o hiperinsulinismo são fatores de risco para recorrência de VPPB, ao passo que o exame normal foi considerado fator protetor, todos estes estatisticamente significantes. Já a intolerância à glicose não teve significância estatística no grupo avaliado.
Conclusão
O hiperinsulinismo e a hiperglicemia se comportam como fatores de risco para a recorrência de VPPB idiopática, assim como o exame normal como um fator protetor.
Palavras-chave: Vertigem, Transtornos do metabolismo de glucose, Metabolismo dos carboidratos, Tontura
Introduction
Benign postural (or positional) paroxysmal vertigo (BPPV) is the most common cause of dizziness in the adult population, and is classified as a peripheral vestibular syndrome.1, 2, 3 BPPV predominates in females and in those aged greater than 50–60 years. In addition, approximately 30% of the elderly aged over 70 years will experience at least one episode of BPPV in their lives.4, 5
In most cases, the patient suffers from idiopathic BPPV. In secondary BPPV, some causes have been found, such as: traumatic brain injury, post-operative ear surgery, vertebrobasilar insufficiency, vestibular neuronitis and Ménière's disease.6 However, few studies have related metabolic changes with BPPV, or even identified such changes as a cause of secondary BPPV.7
Numerous metabolic disorders can affect the cochleovestibular apparatus.8, 9, 10, 11, 12 Changes in carbohydrate metabolism, more precisely in glucose metabolism, have been associated with frequent causes of inner ear disorders.8, 9, 10, 11, 12
In carbohydrate disorders, especially those affecting glucose, some authors propose that, in patients with chronically hyperglycemic diabetes mellitus, the histopathological changes of microangiopathy and peripheral neuropathy are present.11, 13 Considering that the inner ear receives vascularization through terminal branches, such changes might compromise vestibular function, due to a decreased blood supply to this organ.
The post-mortem study of temporal bones performed by Yoda et al.10 found that patients with type 1 diabetes mellitus exhibit a much higher prevalence of otocone debris coming from the utricle, compared to healthy patients. In addition, these authors found that the prevalence of migration of such debris also was increased, in proportion to the years of illness. Thus, there is a greater chance of BPPV in patients with type 1 diabetes mellitus. Cohen et al.14 observed a 20% prevalence of diabetes mellitus in patients with BPPV aged between 65 and 74 years, and a 43% prevalence in people over 75 years.
In the literature, recurrence of BPPV varies between 20% and 30%.1, 15 Several factors have been linked to the development of recurrence, including age, gender, and etiology of BPPV.1, 15 However, it still remains uncertain whether or not there is a correlation with metabolic disorders.
The aim of this study was to evaluate the influence of carbohydrate disorders in the recurrence of idiopathic BPPV.
Methods
This study was approved by the Ethics Committee of the hospital where it was conducted, according to CAEE protocol number 06181512.2.0000.5442.
This is a longitudinal cohort study, which evaluated medical records of patients with an objective diagnosis of benign paroxysmal positional vertigo established by the otoneurology outpatient clinic of the Otolaryngology Department of a tertiary hospital during the period from December 2009 to May 2013. This diagnosis was reviewed more than once in those cases where recurrence of the disease occurred.
Patients with objective idiopathic benign paroxysmal positional vertigo monitored in the otoneurology outpatient clinic until their discharge (which occurred only after an asymptomatic period of 6 months), and who submitted to a requested 3-h glucose tolerance test were included.
Patients with subjective benign paroxysmal positional vertigo or with other causes of dizziness not associated with BPPV, as well as patients who discontinued or were lost to follow-up before discharge, those failing to make the required tests, or patients with a previous diagnosis and treatment for BPPV were excluded. Patients diagnosed with secondary BPPV of undetermined etiology, such as traumatic brain injury, Ménière's disease, vestibular neuronitis, post-operative of ear surgery, and vertebrobasilar insufficiency were also excluded.
All clinical records of patients with a diagnosis of BPPV registered at the otoneurology outpatient clinic, Department of Otolaryngology, were surveyed. In these charts, we collected the relevant data at diagnosis.
A survey of the records of all patients who had a diagnosis of BPPV registered at the otoneurology outpatient clinic, Otolaryngology Department, was conducted. In these clinical records, all data were obtained at the date of diagnosis.
Recurrence of the disease was evaluated both qualitatively and quantitatively; “recurrence” was defined as that clinical picture in which disappearance of vertigo and positional nystagmus occurred after repositioning maneuvers (RM), with assessment by Dix-Hallpike maneuver and roll test, but with return of these signs and symptoms verified by an ENT physician within six months of follow-up. After RM repetition, these patients were again asymptomatic. Finally, patients whose nystagmus and vertigo did not disappear when RM were carried out under the supervision of an otolaryngologist were classified as having persistent BPPV. It must be emphasized that the recurrences of episodes of BPPV were evaluated through anamnesis and also by Dix-Hallpike maneuver and roll test.
The results of the glycemic curve test were analyzed and classified according to American Diabetes Association (ADA) criteria published in 2013, and the interpretation of the insulinemic curve was based on those criteria proposed by Kraft (1975).14, 15 Therefore, our patients were classified into four groups, according to the results of their glucose-insulin curves: patients with a normal test, patients with impaired glucose tolerance (who, according to ADA, are called pre-diabetic patients), patients with hyperinsulinism, and patients with hyperglycemia (who, according to ADA, are called diabetics); in these patients, the relationship with the recurrence of BPPV was evaluated.
The Chi-squared test was used to assess quantitatively the relationship between changes in carbohydrate metabolism and rate of recurrence. The statistical significance level was set at p = 0.05.
Results
In this study, 103 medical records of patients with benign paroxysmal positional vertigo during the period from December 2009 to May 31, 2013 were evaluated. Of these, 31 patients were excluded from the study (11 patients for having subjective BPPV; 5 patients whose medical records were not found in the hospital medical file; 7 patients for not having performed the required tests and/or for discontinuation of clinical follow-up; and 8 patients for not being considered as idiopathic cases). Thus, the final number of cases was 72 patients, whose sample was divided as follows:
-
•
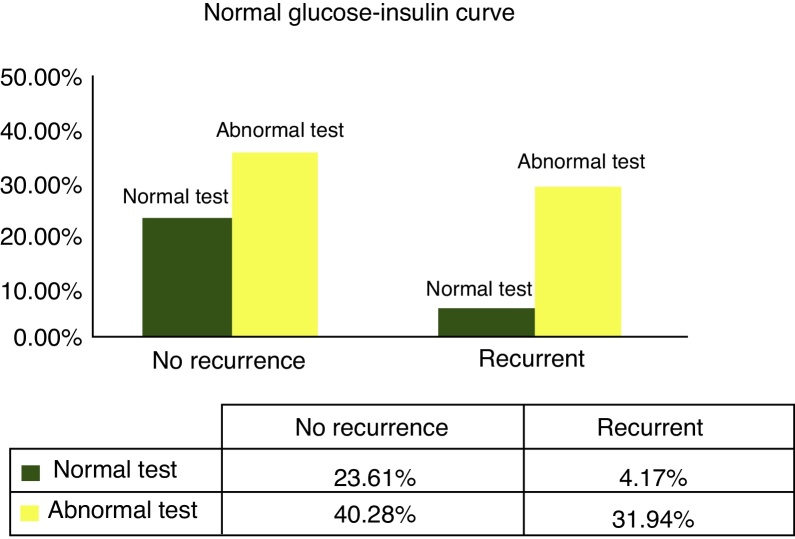
With a normal result in glucose–insulin tests (Fig. 1), a relative risk (RR) of 0.2225 was found, with p = 0.03054.
-
•
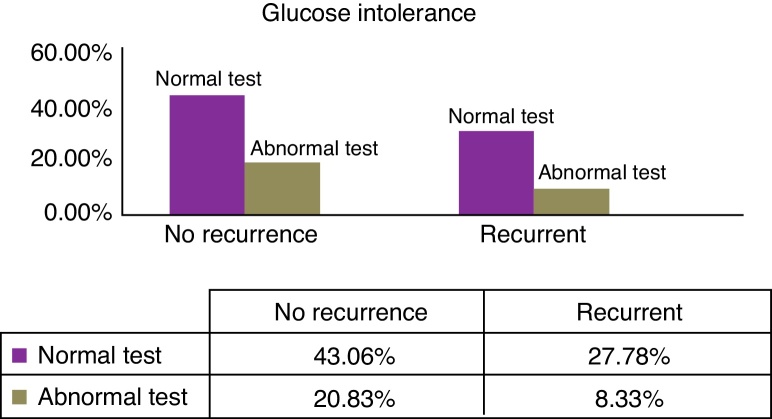
With a result of impaired glucose tolerance in glucose–insulin tests (Fig. 2), RR = 0.6315, p = 0.096.
-
•
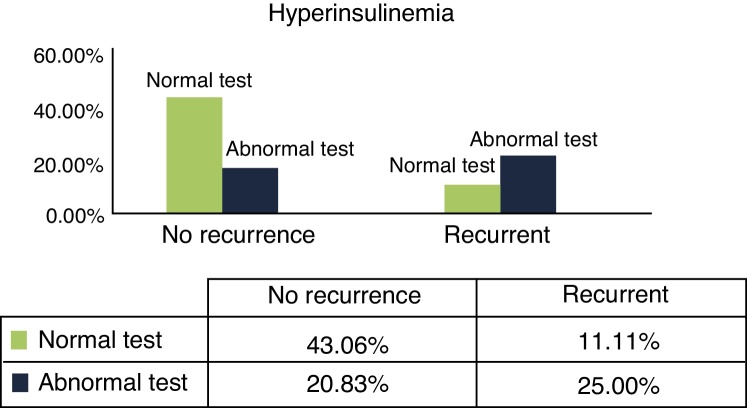
With a result of hyperinsulinemia in glucose–insulin tests (Fig. 3), RR = 4.6647, p = 0.0015.
-
•
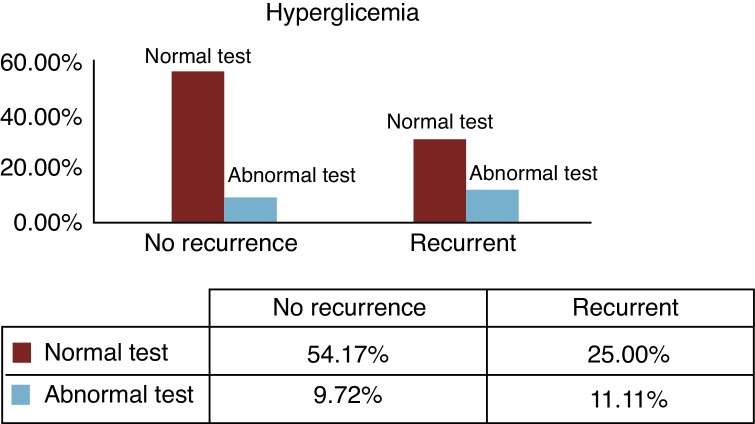
With a result of hyperglycemia in glucose–insulin tests (Fig. 4), RR = 2.4761, p = 0.0123.
Figure 1.
Distribution of patients with BPPV recurrence, regarding glucose–insulin tests within normal limits.
Figure 2.
Distribution of patients with BPPV recurrence, regarding tests with glucose intolerance.
Figure 3.
Distribution of patients with BPPV recurrence, regarding tests with hyperinsulinemia.
Figure 4.
Distribution of patients with BPPV recurrence, regarding tests with hyperglycemia.
Discussion
Dizziness is a major limiting factor in the daily life of the general population, with exacerbation in the elderly because it affects movements of those who experience it, and it can interfere with domestic and even social activities.16 The elderly lose their autonomy and become dependent individuals, which further decreases their quality of life.17, 18, 19, 20 An important consequence of dizziness is the occurrence of falls, especially for those over 60 years of age, because the effects are even more severe.4 In Brazil, 6802 elderly people died from falls in the year 201021 – an alarming fact in terms of public health. This can be partly explained by BPPV in the elderly.4
Although benign paroxysmal positional vertigo has been a recognized entity for decades, its etiology remains predominantly idiopathic.6, 22, 23 However, few studies have been conducted with the aim to clarify the relationship between BPPV and other comorbidities, and how they could influence the disease severity and the prognosis of these clinical pictures.
There is good evidence that metabolic disorders can be associated with BPPV7, 8, 9, 10, 11, 12 but it is difficult to confirm a causal relationship, since it is impossible to observe the histopathological changes in vivo. These metabolic disorders can act as a principal etiological factor in vestibular dysfunction, as well as an aggravating factor of a pre-existing vestibular disorder.9
We did not find statistical significance for patients with glucose intolerance in relation to the number of recurrences, compared to normal subjects. This finding may suggest that this degree of change in carbohydrate metabolism is not significant to the point of an association with the evolution of BPPV. However, no theories can be proposed until a larger number of patients with impaired glucose tolerance and also with BPPV have been evaluated.
On the other hand, the presence of hyperinsulinism can negatively impact inner ear hemostasis, as a result of the ionic and metabolic characteristics of the stria vascularis, which is responsible for maintaining the endocochlear potential through potassium secretion into endolymphatic space.8, 9 Furthermore, the labyrinth is very sensitive to small changes in plasma insulin levels, due to the large number of insulin receptors present in the endolymphatic sac.11
Based on these suggestive signs (i.e., that glucose metabolism may be associated to clinical pictures of benign paroxysmal positional vertigo), this study found some relations, such as: the hyperinsulinemic patient has a RR 4.6 times higher for BPPV recurrence, compared with the general population – a statistically significant finding. Likewise, the hyperglycemic patient has a RR 2.47 times higher for BPPV recurrence, also statistically significant. On the other hand, patients with a normal glucose–insulin curve test have a RR of only 0.22, also statistically significant. This means that having a normal value may be a protective factor for recurrence of BPPV.
Tanimoto et al.24 found that the only risk factor for recurrence of BPPV was the presence of endolymphatic hydrops. Considering that the literature is pretty consistent regarding the association between hyperinsulinism and endolymphatic hydrops, we can call into question whether, in fact, hyperinsulinism would not be an underlying event to endolymphatic hydrops – this latter being the actual risk factor for those recurrence values found by the author in his series.
Furthermore, Tanimoto et al.24 reported that the recurrence of benign paroxysmal positional vertigo was associated with secondary causes, more than to idiopathic BPPV. This statement, combined with the results of our study, makes it possible to propose the hypothesis of a form of BPPV secondary to glucose metabolism disorders.
Conclusion
Glucose metabolism disorders are related to BPPV recurrence in the group evaluated. In this study, we found that both hyperinsulinism and hyperglycemia behaved as risk factors for recurrence of idiopathic BPPV, and also that a normal glucose tolerance test acted as a protective factor.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Webster G, Sens PM, Salmito MC, Cavalcante JD, dos Santos PR, da Silva AL, et al. Hyperinsulinemia and hyperglycemia: risk factors for recurrence of benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2015;81:347–51.
Institution: Hospital do Servidor Público Municipal de São Paulo, São Paulo, SP, Brazil.
References
- 1.Perez P., Franco V., Cuesta P., Aldama P., Alvarez M.J., Mendez J.C. Recurrence of benign paroxysmal positional vertigo. Otol Neurotol. 2012;33:437–443. doi: 10.1097/MAO.0b013e3182487f78. [DOI] [PubMed] [Google Scholar]
- 2.Balatsouras D.G. Benign paroxysmal positional vertigo with multiple canal involvement. Am J Otolaryngol. 2012;33:250–258. doi: 10.1016/j.amjoto.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Y., Chen X., Wang X., Cao L., Dong Z., Zhen J., et al. A clinical epidemiological study in 187 patients with vertigo. Cell Biochem Biophys. 2011;59:109–112. doi: 10.1007/s12013-010-9120-1. [DOI] [PubMed] [Google Scholar]
- 4.Ganança F.F., Gazzola J.M., Ganança C.F., Caovilla H.H., Ganança M.M., Cruz O.L.M. Quedas em idosos com vertigem posicional paroxística benigna. Braz J Otorhinolaryngol. 2010;76:113–120. doi: 10.1590/S1808-86942010000100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho E.I., White J.A. Positional vertigo: as occurs across all age groups. Otolaryngol Clin N Am. 2011;44:347–360. doi: 10.1016/j.otc.2011.01.006. viii. [DOI] [PubMed] [Google Scholar]
- 6.Caldas M.A., Ganança C.F., Ganança F.F., Ganança M.M., Caovilla H.H. Clinical features of benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2009;75:502–506. doi: 10.1016/S1808-8694(15)30487-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerber K.A., Helmchen C. Benign paroxysmal positional vertigo: new opportunities but still old challenges. Neurology. 2012;78:154–156. doi: 10.1212/WNL.0b013e318241f2a2. [DOI] [PubMed] [Google Scholar]
- 8.Angeli R.D., Lavinsky L., Dolganov A. Alterations in cochlear function during induced acute hyperinsulinemia in an animal model. Braz J Otorhinolaryngol. 2009;75:760–764. doi: 10.1016/S1808-8694(15)30530-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serra A.P., Lopes Kde C., Dorigueto R.S., Ganança F.F. Blood glucose and insulin levels in patients with peripheral vestibular disease. Braz J Otorhinolaryngol. 2009;75:701–705. doi: 10.1016/S1808-8694(15)30521-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoda S., Cureoglu S., Yildirim-Baylan M., Morita N., Fukushima H., Harada T., et al. Association between type 1 diabetes mellitus and deposits in the semicircular canals. Otolaryngol Head Neck Surg. 2011;145:458–462. doi: 10.1177/0194599811407610. [DOI] [PubMed] [Google Scholar]
- 11.Bittar R.S.M., Bottino M.A., Simoceli L., Venosa A.R. Labirintopatia secundária aos distúrbios do metabolismo do açúcar: realidade ou fantasia? Braz J Otorhinolaryngol. 2004;70:800–805. [Google Scholar]
- 12.Bittar R.S.M., Bottino M.A., Zerati F.E., Moraes C.L.d.O., Cunha A.U., Bento R.F. Prevalência das alterações metabólicas em pacientes portadores de queixas vestibulares. Braz J Otorhinolaryngol. 2003;69:64–68. [Google Scholar]
- 13.Cohen H.S. New epidemiological findings on benign paroxysmal positional vertigo. J Neurol Neurosurg Psychiatry. 2007;78:663. doi: 10.1136/jnnp.2006.109447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen H.S., Kimball K.T., Stewart M.G. Benign paroxysmal positional vertigo and comorbid conditions. ORL. 2004;66:11–15. doi: 10.1159/000077227. [DOI] [PubMed] [Google Scholar]
- 15.Dorigueto R.S., Mazzetti K.R., Gabilan Y.P.L., Ganança F.F. Benign paroxysmal positional vertigo recurrence and persistence. Braz J Otorhinolaryngol. 2009;75:565–572. doi: 10.1016/S1808-8694(15)30497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Standards of medical care in diabetes – 2013. Diabetes Care. 2013;36(Suppl. 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kraft L.R. Detection of diabetes mellitus in situ (occult diabetes) Lab Med. 1975;6:10–22. [Google Scholar]
- 18.Takano N.A., Cavalli S.S., Ganança M.M., Caovilla H.H., Santos M.A.d.O., Peluso É.d.T.P., et al. Qualidade de vida de idosos com tontura. Braz J Otorhinolaryngol. 2010;76:769–775. doi: 10.1590/S1808-86942010000600016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ribeiro A.P., Souza E.R.d., Atie S., Souza A.C.d., Schilithz A.O. A influência das quedas na qualidade de vida de idosos. Ciênc Saúde Colet. 2008;13:1265–1273. doi: 10.1590/s1413-81232008000400023. [DOI] [PubMed] [Google Scholar]
- 20.Vaz D.P., Gazzola J.M., Lanca S.M., Dorigueto R.S., Kasse C.A. Clinical and functional aspects of body balance in elderly subjects with benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2013;79:150–157. doi: 10.5935/1808-8694.20130027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brasil. Ministério da Saúde. Available at: www.datasus.gov.br [accessed 29.07.13].
- 22.Soto-Varela A., Rossi-Izquierdo M., Santos-Perez S. Benign paroxysmal positional vertigo simultaneously affecting several canals: a 46-patient series. Eur Arch Otorhinolaryngol. 2013;270:817–822. doi: 10.1007/s00405-012-2043-2. [DOI] [PubMed] [Google Scholar]
- 23.von Brevern M., Radtke A., Lezius F., Feldmann M., Ziese T., Lempert T., et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78:710–715. doi: 10.1136/jnnp.2006.100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tanimoto H., Doi K., Nishikawa T., Nibu K. Risk factors for recurrence of benign paroxysmal positional vertigo. J Otolaryngol Head Neck Surg. 2008;37:832–835. [PubMed] [Google Scholar]