Abstract
Background:
Collagen meniscal implant (CMI) is a biologic scaffold that can be used to replace meniscus host tissue after partial meniscectomy. The short-term results of this procedure have already been described; however, little is known about risk factors for failure.
Purpose:
To determine the factors that predict failure of meniscal scaffold implantation in a large series of patients treated at a single institution and to better define the indications for surgery.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
The analysis included 186 consecutive patients with a minimum 5-year follow-up who underwent CMI scaffold implantation or combined procedures. Patients’ characteristics and details of the surgery were obtained via chart review. Patients with a Lysholm score <65 were considered to have experienced clinical failure. Surgical failure was defined as partial or total scaffold removal.
Results:
The final analysis included 156 patients (84%) at a mean follow-up of 10.9 ± 4.3 years. The patients’ mean age at surgery was 42.0 ± 11.1 years, and the survival rate was 87.8%. Subgroup analysis identified Outerbridge grade 3-4 (Hazard ratio [HR], 3.8; P = .004) and a lateral meniscal implant (HR, 3.2; P = .048) as risk factors for failure. The survival rate was 90.4% for medial implants and 77.4% for lateral implants. An Outerbridge grade 3-4 (HR, 2.8; P < .001) and time from meniscectomy to scaffold >10 years (HR, 2.8; P = .020) were predictive of surgical or clinical failure.
Conclusion:
CMI for partial meniscal deficiency provided good long-term results, with 87.8% of the implants still in situ at a mean 10.9 years of follow-up. Outerbridge grade 3-4, lateral meniscal implants, and longer time from the meniscectomy to implantation of the CMI were identified as risk factors for clinical and surgical failure.
Keywords: meniscal scaffold, lateral meniscus, collagen meniscal implant, CMI, meniscal allograft transplant, long-term follow-up
Biomechanical and clinical studies have demonstrated the essential role that the meniscus plays in joint health, and the deleterious effects of meniscectomy have been well documented.1,13,27 Despite the well-known importance of the meniscus, meniscectomy remains one of the most performed knee procedures.14,16 Although meniscectomy may provide short-term relief of symptoms in many patients, a subgroup of patients will experience the so-called postmeniscectomy syndrome. This condition is characterized by pain, recurrent swelling, and radiological signs such as bone marrow edema, with progression to osteoarthritis in some patients. 5
Replacement of the removed meniscal tissue with a meniscal scaffold has been proposed as one treatment option.6,9 At the present time, the only options available are the collagen meniscal implant (CMI, Ivy Sports Medicine GmbH, Germany), which is composed of purified bovine collagen, and the Actifit implant (Actifit, Orteq, United Kingdom), which is a synthetic implant made of polyurethane.
Although meniscal substitution procedures have been performed for >15 years and are widely accepted as a possible treatment for patients with partial meniscal deficiency, the literature lacks a long-term study evaluating risk factors for failure and the appropriateness of the current indications for this surgery. Currently, only 3 studies have reported the outcomes of scaffold implants at 10 years of follow-up.11,24,38 However, these studies evaluated a limited number of patients with only a few failures. Two other studies with a large number of patients were not designed to evaluate risk factors for failure and were limited to 5 years of follow-up.28,32 In the randomized controlled trial by Rodkey et al, 28 only medial CMIs were included, and only a few patients underwent associated procedures at the time of implantation. The effect of time from the meniscectomy to implantation of the scaffold was also not investigated. For all these reasons, little is known about patient and surgical characteristics that could affect the survival of meniscal scaffolds.
The goals of this retrospective study were to report the long-term survivorship and risk factors for failure of CMIs in a large series of patients treated at a single institution. Our hypothesis was that patient age, body mass index (BMI), time from meniscectomy to implantation, and the intraoperative degree of cartilage injury would negatively affect the survival of the CMI.
Methods
Ethics
Institutional review board approval was obtained for the study (Prot. Gen. No. 0015074 del 03/11/2020). The informed consent was collected via mail for each patient included.
Patient Selection Criteria
This long-term study was based on the Rizzoli Orthopaedic Institute database of consecutive CMI scaffold procedures performed between 1998 and 2015. Consecutive patients with a minimum 5-year follow-up who underwent isolated CMI scaffold implantation or combined procedures were included in the analysis. Patient characteristics and details of the surgery were obtained via chart review. Patients with intraoperative Outerbridge grade 3-4 who had a CMI and additional procedures such as anterior cruciate ligament (ACL) reconstruction, high tibial osteotomy (HTO), or cartilage surgery were also included in the study and were considered to have “complex cases.”
All patients with a minimum of 5 years of follow-up were contacted via telephone between January and June 2020 and were asked to complete the Lysholm questionnaire. Patients were also questioned about whether they had undergone any additional surgeries on the operated knee during the follow-up period and whether they were satisfied with the results of the CMI.
Surgical failures were defined as any reoperations that required a partial or total scaffold removal, including those due to (1) infection, (2) scaffold-related complications such as CMI fragmentation or dislocation, (3) conversion to meniscal allograft transplant (MAT), (4) unicompartmental knee arthroplasty, and (5) total knee arthroplasty.
Patients considered to have experienced clinical failure were those patients who required a second surgery because of increasing pain or knee symptoms (arthrolysis, stem cell injections, or HTO) and those with a poor Lysholm score (<65 points).12,23
Indications for surgery were (1) irreparable acute meniscal tears requiring partial meniscectomy, (2) localized unicompartmental knee pain in patients who underwent previous partial meniscectomy, and/or (3) intact meniscal rim and functional anterior and posterior horn attachments.
Inclusion criteria for patients in this study were (1) an intact ACL (stable knee) or an ACL-deficient knee in which an ACL reconstruction was performed at the time of CMI surgery, (2) no varus or valgus deformity or a knee in which an osteotomy was performed to correct the mechanical axis deviation if >5°, and/or (3) Outerbridge grade 1-3 changes in the compartment where the meniscectomy had been performed or a focal grade 4 cartilage lesion in the involved compartment that underwent a cartilage repair procedure at the time of the CMI surgery.
Exclusion criteria were (1) diagnosis of Outerbridge grade 4 degenerative cartilage disease in the affected joint, (2) inflammatory or systemic autoimmune diseases, (3) collagen allergies, (4) concomitant injuries to ligaments other than the ACL, (5) systemic or local infection, (6) systemic administration of corticosteroid or immunosuppressive agents within 30 days of surgery, (7) evidence of osteonecrosis in the involved knee, and/or (8) pregnancy. 38
Surgical Technique and Rehabilitation
The technique for arthroscopic CMI surgery has been previously described.11,38 In brief, a standard diagnostic arthroscopy was performed to confirm the indication of CMI: The ACL should be intact or concomitantly reconstructed. Diffuse grade 4 Outerbridge cartilage degeneration represents a contraindication to scaffold implant; however, if a focal full-thickness cartilage lesion is present, it could be treated with standard cartilages procedures such as microfracture, mosaicplasty, or scaffold implants.
During arthroscopy, the stability of the meniscal horns was checked, and any unstable meniscal tissue was debrided. Moreover, the area of meniscal deficiency was trimmed square and then measured using the appropriate instrumentation. Using these measurements, the surgeon cut the CMI using a scalpel to fit into the defect in the meniscus. The CMI was inserted into the knee joint via an enlarged lateral arthroscopic portal and placed in the correct position via an arthroscopic probe. The surgeon sutured the CMI to the native meniscal tissue using an all-inside device. After the CMI was sutured into place, any associated procedures such as an ACL reconstruction, osteotomy, and cartilage repair surgery were performed.
Rehabilitation Protocol
A knee brace locked in full extension was applied for 6 weeks. To avoid knee stiffness, patients performed continuous passive motion from 0° to 60° 4 times per day during the first 2 weeks. The range of motion then increased to 90° during the second, the third and the fourth weeks, in the fifth week ROM 0-90° is permitted, and complete range of motion was allowed starting at the sixth week. The patient was asked to avoid weightbearing for 3 weeks. After this period, progressive weightbearing was encouraged; at 6 weeks, full and unrestricted weightbearing was permitted. Quadriceps isometric exercises were performed beginning on the second postoperative day; cycling was allowed starting from the fourth postoperative week. Return to sports and cutting activity were permitted at 6 months after surgery. 38
Statistical Analysis
Statistical analysis was performed using SPSS (Version 26; IBM Corp). The continuous variables were expressed as mean ± standard deviation, whereas the categorical variables were expressed as number and percentage. A comparison among various follow-up points was performed using unpaired-samples t test in case of continuous variables, and differences in categorical variables were analyzed using the chi-square test. Patients undergoing reintervention and scaffold removal were considered to have experienced surgical failure. In contrast, patients who had a Lysholm score <65 or surgery due to knee symptoms possibly related to CMI (arthrolysis, stem cell injection, and HTO) were considered to have experienced clinical failure. When present, the surgical failure time was retrieved so as not to overestimate the survival time. Survival analysis was performed via the Kaplan-Meier method, with clinical failure, surgical failure, and surgical or clinical failure used as endpoints. The mean estimated survival time was calculated from the Kaplan-Meier curves. We performed logistic regression using these endpoints, with sex, BMI (<25 vs ≥25), age at surgery (<43 years vs ≥43 years), 30 CMI laterality, Outerbridge grade (0-2 vs 3-4), combined versus isolated procedure, complex cases (defined as CMI plus Outerbridge grade at least 3 plus 1 other surgical procedure) versus standard cases, and time from meniscectomy to scaffold implantation (≤1 year vs 1-10 years vs >10 years) used as independent variables. The variables with P < .10 were chosen to perform the survival analysis using the log-rank test. Moreover, the hazard ratio (HR) with 95% CI was calculated. Differences were considered significant with P < .05.
Results
A total of 186 patients met the inclusion criteria; of them, 156 (84%) completed the long-term assessment at a mean follow-up of 10.9 ± 4.3 years (95% CI, 10.2-11.6 years) (Figure 1). The study population included 117 (75%) male patients and 39 (25%) female patients. In total, 125 (80%) of the patients had a medial implant, whereas 31 (20%) had a lateral implant. The mean age at surgery was 42.0 ± 11.1 years, and the mean time from meniscectomy to CMI was 8.8 ± 8.5 years. Patient and surgical data are shown in Table 1.
Figure 1.
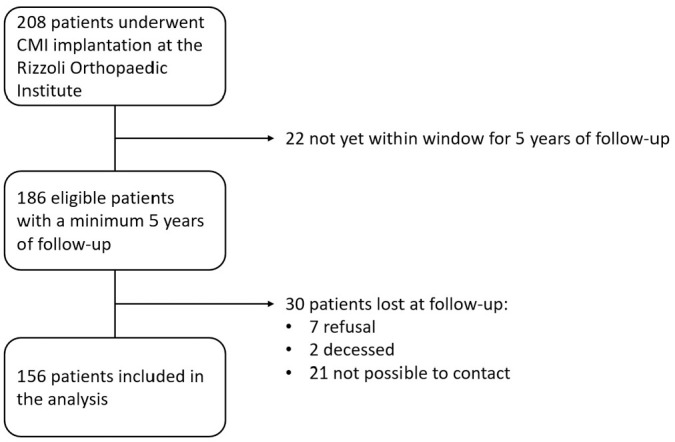
STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) diagram. CMI, collagen meniscal implant.
Table 1.
Patient Characteristics at the Time of Collagen Meniscal Implantation a
| Characteristic | Value |
|---|---|
| Age, y | 42.0 ± 11.1 |
| Sex | |
| Male | 117 (75) |
| Female | 39 (25) |
| Body mass index | 24.9 ± 3.2 |
| Laterality | |
| Medial | 125 (80) |
| Lateral | 31 (20) |
| Time of implant | |
| Acute | 34 (22) |
| Chronic | 122 (78) |
| Time from meniscectomy to collagen meniscal implantation, y | 8.8 ± 8.5 |
| Outerbridge grade | |
| 0-2 | 80 (51) |
| 3-4 | 76 (49) |
| Associated procedures | |
| No | 71 (46) |
| Yes | 85 (54) |
| Complex cases | |
| No | 93 (60) |
| Yes | 63 (40) |
| Follow-up, y | 10.9 ± 4.3 |
Values are expressed as mean ± SD or n (%).
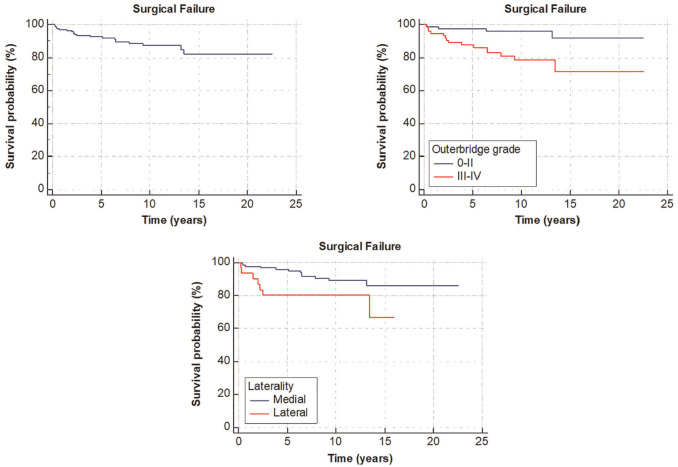
With a mean follow-up of 10.9 years, the overall survival rate for the CMI was 87.8%. Overall, 85% of the patients were satisfied or partially satisfied with the results of implantation. During the considered follow-up period, 19 surgical failures (12.2%) were identified: 3 patients had postoperative early infection that required arthroscopic lavage and scaffold removal, 1 patient had a fragmentation of the scaffold at 3 months after surgery, 5 patients underwent MAT, 6 patients underwent unicompartmental knee arthroplasty, and 4 patients underwent total knee arthroplasty (Table 2). When further evaluating the different subgroups of patients, we identified Outerbridge grade 3-4 (HR, 3.8; P = .004) and lateral scaffold (HR, 3.2; P = .048) as risk factors for surgical failure (Table 3; Figure 2).
Table 2.
Details of CMI Surgical Failures a
| Patient Characteristics | Failure | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient | Age at Surgery, y | Sex | Laterality | Time from Meniscectomy | Intraoperative Cartilage Injury, n | Associated Procedures | Type of Failure | Cause of Failure | Timing of Failure |
| 1 | 42.8 | M | Lateral | 15 y | 3 | Microfracture | CMI removal | Infection | 2 mo |
| 2 | 44.5 | F | Lateral | 0 (acute) | 0 | No | CMI removal | Infection | 2 mo |
| 3 | 43.3 | F | Lateral | 1 y | 1 | DFO | CMI removal | Scaffold fragmentation | 3 mo |
| 4 | 36.1 | M | Lateral | 14 y | 3 | Medial meniscal suture | MAT | Scaffold removal | 2 y |
| 5 | 53.3 | M | Lateral | 12 y | 3 | No | MAT | Increasing pain | 2.5 y |
| 6 | 33.9 | M | Lateral | 10 y | 4 | Microfracture + ACI | UKA | OA progression | 13 y |
| 7 | 52.7 | F | Lateral | 6 y | 4 | Microfracture | TKA | OA progression | 2 y |
| 8 | 40.0 | M | Medial | 10 y | 3 | HTO + cartilage scaffold | CMI removal | Infection | 2 mo |
| 9 | 47.2 | M | Medial | 25 y | 3 | HTO + revision ACL | MAT | Scaffold removal | 6 mo |
| 10 | 37.3 | M | Medial | 18 y | 3 | Revision ACL | MAT | Scaffold removal | 1 y |
| 11 | 43.8 | F | Medial | 27 y | 3 | ACL reconstruction | MAT | Scaffold removal | 4 y |
| 12 | 61.4 | M | Medial | 0 (acute) | 3 | No | UKA | Symptomatic OA | 1 y |
| 13 | 50.4 | M | Medial | 5 y | 3 | HTO | UKA | Symptomatic OA | 6 y |
| 14 | 34.1 | M | Medial | 5 y | 4 | Mosaicplasty | UKA | Symptomatic OA | 7 y |
| 15 | 39.4 | M | Medial | 9 y | 3 | No | UKA | Symptomatic OA | 7 y |
| 16 | 51.9 | M | Medial | 8 y | 4 | Microfracture | UKA | Symptomatic OA | 9 y |
| 17 | 33.2 | M | Medial | 14 y | 4 | Microfracture | TKA | Symptomatic OA | 5 y |
| 18 | 35.3 | M | Medial | 14 y | 4 | Microfracture + revision ACL | TKA | Symptomatic OA | 9 y |
| 19 | 51.4 | M | Medial | 10 y | 3 | No | TKA | Symptomatic OA | 13 y |
ACI, autologous chondrocyte implantation; ACL, anterior cruciate ligament; CMI, collagen meniscal implant; DFO, distal femoral osteotomy; F, female; HTO, high tibial osteotomy; M, male; MAT, meniscal allograft transplant; OA, osteoarthritis; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Table 3.
Risk Factors for Surgical Failure
| No. of Events/Total Cases | Survival Rate, % | P Value | Hazard Ratio (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| 2 y | 5 y | 10 y | 15 y | Overall | ||||
| Overall | 19/156 | 95.5 | 92.2 | 88.2 | 83.6 | 87.8 | ||
| Outerbridge grade | ||||||||
| 0-2 | 4/80 | 97.5 | 97.5 | 96.0 | 92.5 | 95 | ||
| 3-4 | 15/76 | 93.4 | 86.7 | 80.3 | 73.6 | 80.3 | .004 | 3.8 (1.5-9.4) |
| Laterality | ||||||||
| Medial | 12/125 | 96.8 | 95.1 | 90.1 | 87.2 | 90.4 | ||
| Lateral | 7/31 | 87.1 | 80.6 | 80.6 | 67.2 | 77.4 | .048 | 3.2 (1.0-10.0) |
Figure 2.
Kaplan-Meier curves describing the survivorship of collagen meniscal implant considering only surgical failures (defined as reoperations that required a partial or total scaffold removal). Outerbridge grade of 3-4 (HR, 3.8; P = .004) and lateral scaffold (HR, 3.2; P = .048) were identified as risk factors for surgical failures. HR, hazard ratio.
A total of 21 patients underwent an additional surgical procedure during the study period; 6 patients required surgery because of mechanical symptoms or increasing pain (1 arthrolysis, 2 HTOs, and 3 stem cell injections) and were considered to have experienced clinical failure. Patients requiring hardware removal (n = 11) and ACL reconstruction or revision (n = 4) were not considered to have experienced failure because the second surgery was not related to the CMI.
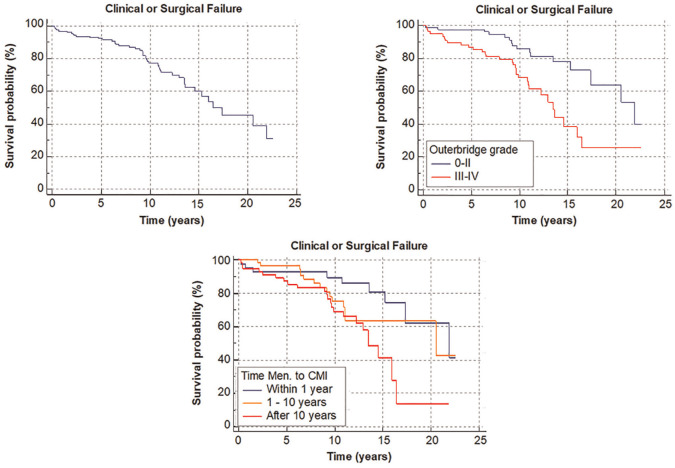
In the final analysis, 47 patients (30.1%) were considered to have experienced either a surgical or a clinical failure. An Outerbridge grade of 3-4 (HR, 2.8; P < .001) and time from meniscectomy to scaffold implantation >10 years (HR, 2.8; P = .020) were identified as risk factors for clinical or surgical failure (Table 4; Figure 3). The survival rate was similar between patients who underwent scaffold implantation during the first year after meniscectomy and those who underwent implantation 1 to 10 years after meniscectomy (78.0% and 75.0%, respectively). However, the survival rate decreased to 58.2% in patients who underwent surgery >10 years after meniscectomy.
Table 4.
Risk Factors for Clinical or Surgical Failure a
| No. of Events/Total Cases | Survival Rate, % | P Value | Hazard Ratio (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| 2 y | 5 y | 10 y | 15 y | Overall | ||||
| Overall | 47/156 | 95.5 | 91.6 | 77.2 | 60.1 | 69.9 | ||
| Outerbridge grade | ||||||||
| 0-2 | 16/80 | 97.5 | 97.5 | 85.6 | 77.9 | 80.0 | ||
| 3-4 | 31/76 | 93.4 | 85.4 | 68.5 | 38.5 | 59.2 | .000 | 2.8 (1.5-4.9) |
| Time from meniscectomy to CMI | ||||||||
| ≤ 1 y | 9/41 | 92.7 | 92.7 | 89.6 | 80.8 | 78.0 | ||
| 1-10 y | 15/60 | 98.3 | 96.6 | 75.2 | 63.7 | 75.0 | 1.7 (0.9-3.5) | |
| >10 y | 23/55 | 92.7 | 87.3 | 69.1 | 41.6 | 58.2 | .020 | 2.8 (1.4-5.6) |
CMI, collagen meniscal implant.
Figure 3.
Kaplan-Meier curves describing the survivorship of collagen meniscal implants (CMIs) considering both clinical and surgical failures. Outerbridge grade of 3-4 (HR, 2.8; P < .001) and time from meniscectomy (Men.) to scaffold >10 years (HR, 2.8; P = .020) were identified as risk factors for implant failure. HR, hazard ratio.
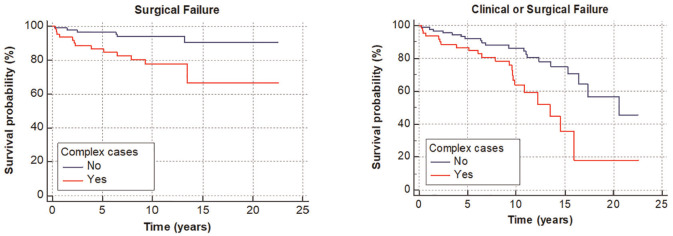
A comparison of complex cases versus standard cases revealed that the first group of patients had an increased risk of surgical failure (HR, 4.0; P = .004) and combined clinical or surgical failure (HR, 2.4; P = .005). The overall rate of surgical failure in the complex cases was 38.1% (Table 5; Figure 4).
Table 5.
Survival Rate in Complex Cases
| No. of Events/Total Cases | Survival Rate, % | P Value | Hazard Ratio (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| 2 y | 5 y | 10 y | 15 y | Overall | ||||
| Surgical failure | ||||||||
| No | 6/93 | 97.8 | 96.8 | 94.3 | 91.2 | 93.5 | ||
| Yes | 13/63 | 92.1 | 85.6 | 79.6 | 69.6 | 79.4 | .004 | 4.0 (1.6-10.3) |
| Clinical or surgical failure | ||||||||
| No | 23/93 | 97.8 | 95.6 | 83.1 | 72.2 | 75.3 | ||
| Yes | 24/63 | 92.1 | 85.6 | 68.2 | 36.2 | 61.9 | .005 | 2.4 (1.3-4.5) |
Figure 4.
Kaplan-Meier curves reporting the survivorship of collagen meniscal implants in complex cases (defined as collagen meniscal implant plus Outerbridge grade at least 3 plus 1 other surgical procedure) and survivorship in standard cases. Note that complex cases had a worse prognosis.
Discussion
The most important finding of the present study was that CMI for partial meniscal defects provided good long-term survivorship, with 87.8% of patients still having the implant in situ after a mean 10.9 years of follow-up. Moreover, 85% of the patients were completely or partially satisfied with the surgical intervention. However, we found an overall significant difference in survival between the medial and lateral implants, with the latter showing a higher rate of surgical failure. We also identified advanced cartilage damage, time from previous meniscectomy >10 years, and complex cases as risk factors for clinical or surgical failure. The results of the present study provide novel insights into the current meniscal substitution literature for different reasons: the large number of patients treated, the single-center location of the study, the high response rate, and the long-term follow-up.
In the present research, the implant of a lateral scaffold was identified as a risk factor for surgical failure, with a 10-year survival rate of 77.4% for lateral CMI versus 90.4% for medial CMI. In the literature, only 3 case reports have evaluated the long-term outcomes of medial CMI (59 patients in total),21,24,38 and 1 study reported the results of lateral CMI. 11 Regarding the medial scaffold, Zaffagnini et al 38 reported no failures in a series of 17 patients at 10 years of follow-up, whereas another study reported that 2 of 25 patients required medial MAT because of increasing knee pain several years after surgery. 24 Similar to the present study results, the long-term outcomes of lateral CMI have been reported to be less favorable, with a 64% survival rate at 12.5 years. 11 The only study with a comparable sample size investigated the outcomes of the Actifit, a polyurethane scaffold. In that research, the authors did not detect any differences in terms of survival rate between the medial and the lateral scaffolds. 32 However, that study was limited to 5 years of follow-up, and although the survival rate of the medial scaffold was stable between 2 and 5 years of follow-up, the lateral implants demonstrated an increased failure rate over time. 32
The worse results of the lateral scaffold compared with the medial scaffold could be related to several factors, including different mobility of the menisci, bony morphology, and load distribution across these 2 compartments.2,7 Studies of meniscal kinematics have shown that the lateral meniscus is markedly more mobile than the medial meniscus is. 8 Moreover, these menisci have notable differences in segmental motion: Because of the reduced anteroposterior ratio, the lateral meniscus moves more as a single unit compared with the medial meniscus. 31 Therefore, it is possible that after CMI surgery, it is more difficult for the lateral meniscus to articulate with the tibia and the femur throughout flexion. Moreover, the reduced mobility of the lateral meniscus may increase the risk of further injury. 31 In addition, because of bony morphology, the lateral compartment is more dependent on meniscal function than is the medial compartment. The meniscus transfers a higher percentage of the load on the lateral side because of the more concave tibial plateau. In contrast, on the medial side, a relevant amount of load is transferred directly by the cartilage.22,29,34
In line with other clinical studies,15,28,37 we found few device-related complications, with 3 patients having a deep infection and 1 patient experiencing scaffold fragmentation in the early postoperative period. Moreover, no device-related complications such as late infections, synovitis, or immunological reactions were reported even at long-term assessment. These results demonstrate the safety of the CMI and the higher biocompatibility of this meniscal scaffold compared with other nonbiodegradable devices such as synthetic ligaments.10,20,33
Contrary to our primary hypothesis, patient age and BMI were not associated with clinical or surgical failure. However, we cannot compare our results with the literature because the long-term effect of these 2 variables on survivorship of the meniscal scaffold has never been investigated. Patient age and BMI have been extensively studied with respect to the outcomes of MAT, which has similar indications and patient characteristics. However, the evidence is inconclusive; some investigators have reported that patient age and BMI are independent risk factors for failure, whereas others have reported that these parameters did not contribute to graft failure after MAT.17,18,25,36
An interesting analysis of the effect of age on MAT was performed by Kim et al 18 in a large group of consecutive patients. Older age was associated with a lower survival rate, but after matching patients for cartilage status and time from the previous meniscectomy, the investigators found no significant difference in MAT survivorship between younger and older patients. Thus, similar to our study, Kim et al concluded that MAT survivorship was predominantly affected by age-related prognostic factors, such as cartilage damage and time from meniscectomy, rather than age itself.
Regarding meniscal substitution surgery, one controversial topic is the ideal time between meniscectomy and the surgical implant of the scaffold. In the present research, the survival rate of the scaffold dropped from 75% to 58.2% when CMI surgery was performed >10 years after meniscectomy (Figure 3; Table 4). Even though the use of CMI has been advocated only in a chronic setting, recent studies have supported the indication of CMI even after a recent meniscectomy.4,21,28 Rodkey et al 28 compared the outcomes of 311 patients who underwent CMI in an acute or chronic setting versus patients who underwent isolated meniscectomy: Only in the chronic group did CMI show superior results in terms of subjective scores and patient satisfaction compared with meniscectomy. Nonetheless, because the development of symptomatic cartilage damage after meniscectomy takes many years, 26 it is possible that the follow-up time of 5 years in the study of Rodkey et al was insufficient to detect significant changes. The need for a more aggressive approach when dealing with meniscectomy has been advocated by Condello et al. 4 Their results suggested that delayed scaffold implantation of >6 months correlates with lower clinical outcomes at 3 years of follow-up. These findings are in line with the outcomes of our research and seem to suggest a window of opportunity in which the use of a meniscal scaffold could result in a greater benefit.
In the present study, a subgroup of patients with complex cases was analyzed separately; those patients had advanced cartilage lesions, meniscal defects, and other concomitant knee pathologies requiring surgical management. Even though those patients had worse clinical results and higher failure rates when compared with the patients with standard cases, the overall survival of 69.9% at a mean 10.9 years of follow-up could be considered satisfactory, considering the preoperative condition and the limited possible treatment options for this subgroup of patients.
The current study’s findings represent an important message to share with the orthopaedic community. A combined biological and mechanical approach could result in satisfactory results for relatively young patients affected by multiple knee problems who are eligible for total knee replacement. In addition, studies investigating the outcomes of total knee replacement performed in younger patients have found lower survivorship, a higher reoperation rate, and a higher incidence of infections and extensor mechanism complications when compared with an older population.3,35
The present study has several limitations. It was a retrospective study. Moreover, we did not include a control group of patients who underwent isolated meniscectomy, and magnetic resonance imaging was not performed at the last follow-up. Therefore, it was impossible to prove whether the scaffold implant could provide a real benefit in terms of chondroprotection or symptom relief compared with isolated meniscectomy. It was not possible to analyze whether the location of the meniscal lesion, the degree of meniscectomy, and the size of the CMI were risk factors for failure.
Another limitation is that a considerable percentage of patients underwent an associated surgical procedure during the CMI surgery. However, this heterogeneous population represented the typical patient profile referred to high-level knee surgery centers. No objective evaluation was performed, and the patients were contacted via telephone. However, a previous study demonstrated that the Lysholm score could be reliably completed through telephone interview 19 and the patients could easily recall data such as surgical failures even without an in-office evaluation. The last limitation of the study entails the assessment of clinical failure in survivorship analysis. The exact time the Lysholm dropped under 65 points was underestimated; however, the data added relevant information because not all of the patients with unsatisfactory outcomes decided to undergo a subsequent arthroscopy to remove or revise the implant.
This study has several strengths that are important to highlight. This study was the first to investigate clinical and surgical failures in a large population of patients who received CMI for partial meniscal defects at a mean of 10.9 years of follow-up. Moreover, the follow-up rate was excellent (84%), and a secondary statistical analysis confirmed that there were no differences in patient characteristics and surgical parameters between the patients included in the study and the patients who dropped out.
The good long-term survival rate and the high patient satisfaction reported in the present study confirm that CMI is a safe and valuable procedure for treating symptomatic meniscal defects. Patients with a lateral meniscal defect, high-grade cartilage lesion, and time from previous meniscectomy >10 years should be informed of this treatment’s higher failure rate.
On the basis of the present study results, we recommend using a meniscal scaffold to treat symptomatic meniscal deficit even in a chronic setting. However, to achieve a satisfactory survival rate, it is crucial to address ligament instability and axial malalignment at the index surgery and to perform meniscal replacement surgery <10 years after meniscectomy.
Conclusion
Collagen meniscal implant for partial meniscal deficiency provided good long-term results, with 87.8% of the implants still in situ at a mean 10.9 years of follow-up. Outerbridge grade 3-4, lateral meniscal implants, and longer time from meniscectomy to CMI were identified as risk factors for clinical and surgical failures.
Footnotes
Submitted November 2, 2021; accepted May 31, 2022.
Presented at the annual meeting of the AOSSM, Colorado Springs, Colorado, July 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.Z. is a consultant surgeon for Smith & Nephew and DePuy Synthes. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abram SGF, Judge A, Beard DJ, Carr AJ, Price AJ. Long-term rates of knee arthroplasty in a cohort of 834 393 patients with a history of arthroscopic partial meniscectomy. Bone Joint J. 2019;101(9):1071-1080. [DOI] [PubMed] [Google Scholar]
- 2. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med. 1986;14(4):270-275. [DOI] [PubMed] [Google Scholar]
- 3. Chalmers BP, Pallante GD, Sierra RJ, Lewallen DG, Pagnano MW, Trousdale RT. Contemporary revision total knee arthroplasty in patients younger than 50 years: 1 in 3 risk of re-revision by 10 years. J Arthroplasty. 2019;34(7)(suppl):S266-S270. [DOI] [PubMed] [Google Scholar]
- 4. Condello V, Dei Giudici L, Perdisa F, et al. Polyurethane scaffold implants for partial meniscus lesions: delayed intervention leads to an inferior outcome. Knee Surg Sports Traumatol Arthrosc. 2021;29(1):109-116. [DOI] [PubMed] [Google Scholar]
- 5. Drobnič M, Ercin E, Gamelas J, et al. Treatment options for the symptomatic post-meniscectomy knee. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1817-1824. [DOI] [PubMed] [Google Scholar]
- 6. Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M. Meniscal scaffolds: results and indications: a systematic literature review. Int Orthop. 2015;39(1):35-46. [DOI] [PubMed] [Google Scholar]
- 7. Fithian DC, Kelly MA, Mow VC. Material properties and structure-function relationships in the menisci. Clin Orthop Relat Res. 1990;252:19-31. [PubMed] [Google Scholar]
- 8. Fox AJS, Bedi A, Rodeo SA. The basic science of human knee menisci. Sports Health. 2012;4(4):340-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Getgood A, LaPrade RF, Verdonk P, et al. International Meniscus Reconstruction Experts Forum (IMREF) 2015 consensus statement on the practice of meniscal allograft transplantation. Am J Sports Med. 2017;45(5):1195-1205. [DOI] [PubMed] [Google Scholar]
- 10. Glezos CM, Waller A, Bourke HE, Salmon LJ, Pinczewski LA. Disabling synovitis associated with LARS artificial ligament use in anterior cruciate ligament reconstruction: a case report. Am J Sports Med. 2012;40(5):1167-1171. [DOI] [PubMed] [Google Scholar]
- 11. Grassi A, Lucidi GA, Filardo G, et al. Minimum 10-year clinical outcome of lateral collagen meniscal implants for the replacement of partial lateral meniscal defects: further results from a prospective multicenter study. Orthop J Sports Med. 2021;9(5):2325967121994919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grassi A, Macchiarola L, Lucidi GA, et al. Long-term outcomes and survivorship of fresh-frozen meniscal allograft transplant with soft tissue fixation: minimum 10-year follow-up study. Am J Sports Med. 2020;48(10):2360-2369. [DOI] [PubMed] [Google Scholar]
- 13. Hede A, Larsen E, Sandberg H. The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop. 1992;16(2):122-125. [DOI] [PubMed] [Google Scholar]
- 14. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. Sports Health. 2018;10(6):523-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hirschmann MT, Keller L, Hirschmann A, et al. One-year clinical and MR imaging outcome after partial meniscal replacement in stabilized knees using a collagen meniscus implant. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):740-747. [DOI] [PubMed] [Google Scholar]
- 16. Jacquet C, Pujol N, Pauly V, Beaufils P, Ollivier M. Analysis of the trends in arthroscopic meniscectomy and meniscus repair procedures in France from 2005 to 2017. Orthop Traumatol Surg Res. 2019;105(4):677-682. [DOI] [PubMed] [Google Scholar]
- 17. Kempshall PJ, Parkinson B, Thomas M, et al. Outcome of meniscal allograft transplantation related to articular cartilage status: advanced chondral damage should not be a contraindication. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):280-289. [DOI] [PubMed] [Google Scholar]
- 18. Kim C, Bin SI, Kim JM, et al. Medial and lateral meniscus allograft transplantation showed no difference with respect to graft survivorship and clinical outcomes: a comparative analysis with a minimum 2-year follow-up. Arthroscopy. 2020;36(12):3061-3068. [DOI] [PubMed] [Google Scholar]
- 19. Kose O, Deniz G, Ozcan H, Guler F. A comparison of telephone interview versus on-site completion of Lysholm knee score in patients who underwent arthroscopic ACL reconstruction: are the results equivalent? Eur J Orthop Surg Traumatol. 2015;25(6):1069-1072. [DOI] [PubMed] [Google Scholar]
- 20. Li H, Yao Z, Jiang J, et al. Biologic failure of a ligament advanced reinforcement system artificial ligament in anterior cruciate ligament reconstruction: a report of serious knee synovitis. Arthroscopy. 2012;28(4):583-586. [DOI] [PubMed] [Google Scholar]
- 21. Lucidi GA, Grassi A, Al-Zu’bi BBH, et al. Satisfactory clinical results and low failure rate of medial collagen meniscus implant (CMI) at a minimum 20 years of follow-up. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4270-4277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88(12):1549-1556. [DOI] [PubMed] [Google Scholar]
- 23. Mitsou A, Vallianatos P, Piskopakis N, Maheras S. Anterior cruciate ligament reconstruction by over-the-top repair combined with popliteus tendon plasty. J Bone Joint Surg Br. 1990;72(3):398-404. [DOI] [PubMed] [Google Scholar]
- 24. Monllau JC, Gelber PE, Abat F, et al. Outcome after partial medial meniscus substitution with the collagen meniscal implant at a minimum of 10 years’ follow-up. Arthroscopy. 2011;27(7):933-943. [DOI] [PubMed] [Google Scholar]
- 25. Noyes FR, Barber-Westin SD. Long-term survivorship and function of meniscus transplantation. Am J Sports Med. 2016;44(9):2330-2338. [DOI] [PubMed] [Google Scholar]
- 26. Papalia R, Del Buono A, Osti L, Denaro V, Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011;99:89-106. [DOI] [PubMed] [Google Scholar]
- 27. Persson F, Turkiewicz A, Bergkvist D, Neuman P, Englund M. The risk of symptomatic knee osteoarthritis after arthroscopic meniscus repair vs partial meniscectomy vs the general population. Osteoarthritis Cartilage. 2018;26(2):195-201. [DOI] [PubMed] [Google Scholar]
- 28. Rodkey WG, DeHaven KE, Montgomery WH, et al. Comparison of the collagen meniscus implant with partial meniscectomy: a prospective randomized trial. J Bone Joint Surg Am. 2008;90(7):1413-1426. [DOI] [PubMed] [Google Scholar]
- 29. Seedhom BB, Dowson D, Wright V. Proceedings: functions of the menisci. A preliminary study. Ann Rheum Dis. 1974;33(1):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Song JH, Bin SI, Kim JM, Lee BS, Son DW. Does age itself have an adverse effect on survivorship of meniscal allograft transplantation? A cartilage status and time from previous meniscectomy-matched cohort study. Am J Sports Med. 2020;48(7):1696-1701. [DOI] [PubMed] [Google Scholar]
- 31. Thompson WO, Thaete FL, Fu FH, Dye SF. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med. 1991;19(3):210-215. [DOI] [PubMed] [Google Scholar]
- 32. Toanen C, Dhollander A, Bulgheroni P, et al. Polyurethane meniscal scaffold for the treatment of partial meniscal deficiency: 5-year follow-up outcomes. A European multicentric study. Am J Sports Med. 2020;48(6):1347-1355. [DOI] [PubMed] [Google Scholar]
- 33. Tulloch SJ, Devitt BM, Norsworthy CJ, Mow C. Synovitis following anterior cruciate ligament reconstruction using the LARS device. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2592-2598. [DOI] [PubMed] [Google Scholar]
- 34. Walker PS, Hajek JV. The load-bearing area in the knee joint. J Biomech. 1972;5(6):581-589. [DOI] [PubMed] [Google Scholar]
- 35. Walker-Santiago R, Tegethoff JD, Ralston WM, Keeney JA. Revision total knee arthroplasty in young patients: higher early reoperation and rerevision. J Arthroplasty. 2021;36(2):653-656. [DOI] [PubMed] [Google Scholar]
- 36. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Survivorship and clinical outcomes of 147 consecutive isolated or combined arthroscopic bone plug free meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1432-1439. [DOI] [PubMed] [Google Scholar]
- 37. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Two-year clinical results of lateral collagen meniscus implant: a multicenter study. Arthroscopy. 2015;31(7):1269-1278. [DOI] [PubMed] [Google Scholar]
- 38. Zaffagnini S, Marcheggiani Muccioli GM, Lopomo N, et al. Prospective long-term outcomes of the medial collagen meniscus implant versus partial medial meniscectomy: a minimum 10-year follow-up study. Am J Sports Med. 2011;39(5):977-985. [DOI] [PubMed] [Google Scholar]