Introduction
Salivary gland tumors are a very heterogeneous group of lesions. According to the histological classification published by WHO in 2005, 10 types of benign and 24 types of malignant tumors of the salivary glands can be distinguished. All of these lesions are relatively rare, and represent only 3–4% of head and neck tumors. 80% of them are located within the parotid gland, and they usually present as a single parotid lesion.1 Unilateral parotid neoplasms are very uncommon, and they usually have the same histological type. The most common type of such a lesion is Warthin tumor (6–12% of all adenolymphomas).2 The coexistence of tumors of different histological types in the same parotid gland constitutes less than 0.3% of all salivary gland neoplasms.3 The most common histological combination is Warthin tumor and pleomorphic adenoma. Two different unilateral parotid neoplasms can be metachronous or synchronous. However, even when more than one tumor occur at the same time, they must be distinguished from hybrid tumors, in which we can find two or more distinct histological types of neoplasms having an identical origin in the same tissue.4
Synchronous benign and malignant ipsilateral parotid tumors are an extremely rare phenomenon. It was described for the first time by Tanaka in 1953 as mucoepidermoid carcinoma associated with Warthin tumor.5 To our knowledge no case in the literature mentioned the occurrence of a tumor consisting of carcinoma ex pleomorphic adenoma and Warthin tumor, which is reported in the present paper.
Case report
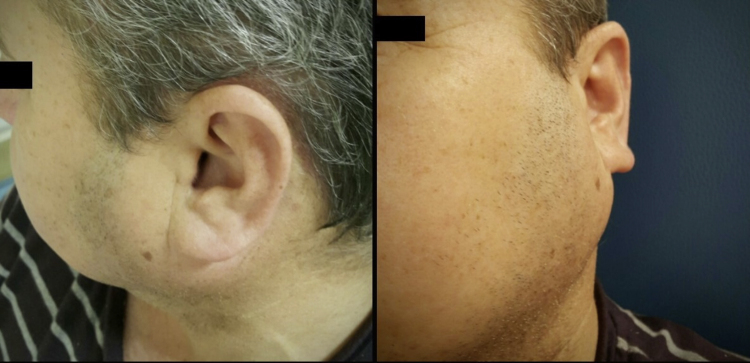
61 year-old man presented with a 10 year history of a nontender, growing, left parotid mass. On clinical examination a firm, mobile mass was evident, with no overlying skin changes. The diameter of the lesion was 4 cm. No facial nerve palsy or lymphadenopathy was detected (Fig. 1).
Figure 1.
61-Year old patient with left parotid mass, on admission to the hospital.
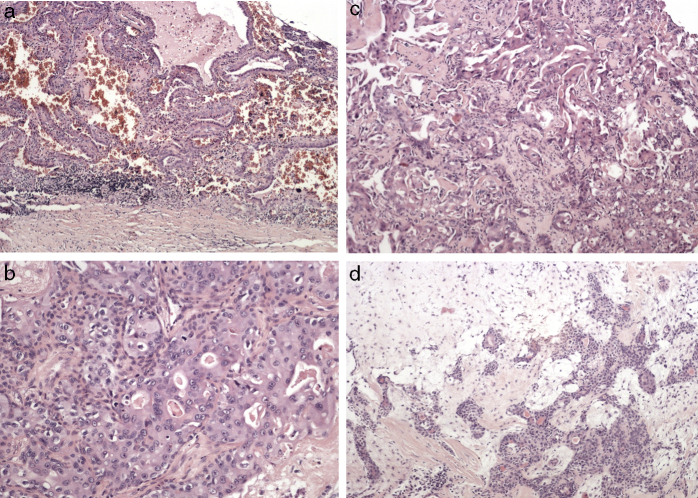
A CT scan revealed a 57 mm × 40 mm × 27 mm heterogeneously enhanced left parotid mass, involving both lobes of the gland (Fig. 2). There was no evidence of osteolytic changes in mandibular bones. Moreover, no invasions of the masseter muscle or of the parapharyngeal space were showed. A few 15–19 mm lymph nodes in the retro- and submandibular space were described. Fine needle aspiration biopsy confirmed pleomorphic adenoma. The patient underwent surgical treatment involving left subtotal parotidectomy. En bloc removal of the tumor was achieved with the excision of the superficial lobe. The facial nerve was preserved. Macroscopically, the mass was enveloped, solid and yellowish, with one cyst (1.5 cm in diameter) on the marginal part. Microscopically, the tumor mass included three different morphological patterns (Fig. 3). Pleomorphic adenoma was the dominant component. Within its tissue atypical cells of carcinoma ex pleomorphic adenoma were found. The marginal part of the solid mass included Warthin tumor cells. Surgical margins were free from neoplasm.
Figure 2.
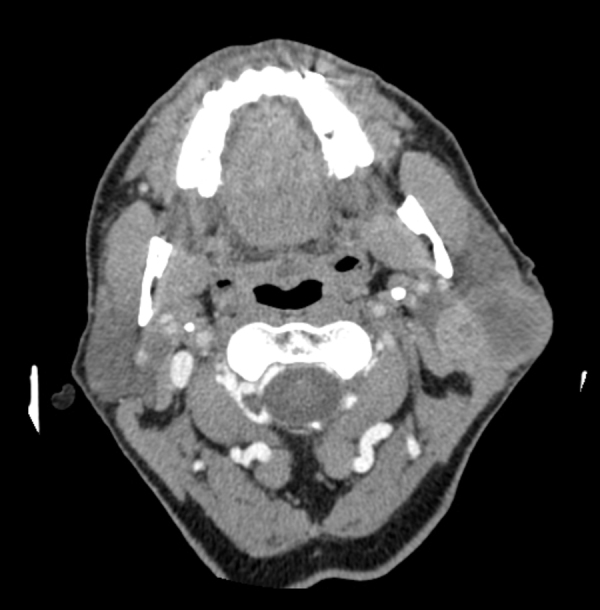
An enhanced CT scan of the parotid gland. Heterogeneously enhanced, left parotid mass, involving both lobes of the gland.
Figure 3.
The histopatology of the resected specimen showing (A) Warthin tumor composed of lymphoid and epithelial cells, (B, C) malignant epithelial cells of carcinoma ex pleomorphic adenoma, in the background of (D) pleomorphic adenoma.
Due to the postoperative histopathological finding of malignant components of the tumor the patient was proposed a re-operation, involving the removal of the deep lobe of the parotid gland and elective neck dissection of I and II cervical lymph node groups. The patient did not give consent to surgical re-treatment. Therefore, even though CT scans did not indicate the presence of positive lymph nodes, the patient was referred for radiation treatment. No signs of recurrence were revealed during a follow-up after 5 years.
Discussion
Multiple salivary gland tumors are occasionally seen, and account for 1.7–5% of parotid lesions. The vast majority of this phenomenon belongs to the same histological type of tumors, with Warthin tumor being the most common. Multifocal pleomorphic adenoma occurs rather infrequently.6, 7 Synchronous parotid tumors of different histology account for less than 0.3% of all salivary gland neoplasms. The most common combination is Warthin tumor and pleomorphic adenoma.3 Benign and malignant tumors in the ipsilateral parotid gland are extremely rare. Since Tanaka first reported the case of coexisting bilateral Warthin tumor and mucoepidermoid carcinoma, only 25 papers have reported the incidence of synchronous unilateral tumors of the parotid or periparotid region.5
According to previous reports, this type of lesions was more commonly observed in male patients, with the male-to-female ratio 1.3:1. The median patient's age was 66 years, and the average age – 64.1 years, which is almost 1 decade later than the incidence of malignancies in salivary glands in general.1 Warthin tumor was the most commonly described benign neoplasm (22 of 38 cases), pleomorphic adenoma was described less frequently (11 of 38 cases). There were solitary cases of other benign tumors, such as sebaceous lymphadenoma, oncocytoma and myoepithelioma. The most frequently observed malignant component was mucoepidermoid carcinoma (11 of 38 cases) and acinic cell carcinoma (8 of 38 cases). Hence, the most popular histological combination of neoplasms was Warthin tumor and mucoepidermoid carcinoma (9 of 38 cases) (Table 1).3, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28
Table 1.
Summary of papers concerning synchronous benign and malignant unilateral parotid gland tumors.
| Author | Year | Benign tumor | Malignant tumor | Age | Gender |
|---|---|---|---|---|---|
| Our case | 2015 | Warthin tumor | Carcinoma ex pleomorphic adenoma | 61 | M |
| Jin J8 | 2011 | Pleomorphic adenoma | Lymphoepithelial carcinoma | ND | ND |
| Srivastava S9 | 2009 | Warthin tumor | Mucoepidermoid carcinoma | 52 | M |
| Roh JL10 | 2007 | Warthin tumor | Adenocarcinoma | 71 | M |
| Tanaka S11 | 2007 | Warthin tumor + pleomorphic adenoma | Salivary duct carcinoma | 67 | M |
| Ethunandan M6 | 2006 | Warthin tumor | Acinic cell carcinoma | ND | ND |
| Bień S12 | 2006 | Pleomorphic adenoma | Adenocarcinoma | 51 | M |
| Pleomorphic adenoma | Adenocarcinoma | 66 | M | ||
| Pleomorphic adenoma | Salivary duct carcinoma | 72 | F | ||
| Azua-Romeo J13 | 2005 | Oncocytoma | Acinic cell carcinoma | 77 | M |
| Yu G-Y7 | 2004 | Warthin tumor | Squamous cell carcinoma | ND | ND |
| Zeegregts CJ2 | 2003 | Pleomorphic adenoma | Acinic cell carcinoma | ND | ND |
| Shukla M14 | 2003 | Sebaceous lymphadenoma | Squamous cell carcinoma | 68 | F |
| Curry JL15 | 2002 | Pleomorphic adenoma | Salivary duct carcinoma | 67 | F |
| Warthin tumor | Mucoepidermoid carcinoma | 51 | F | ||
| Mayorga M16 | 1999 | Sebaceus lymphadenoma | Acinic cell carcinoma | 78 | F |
| Misselevich I17 | 1997 | Pleomorphic adenoma | Acinic cell carcinoma | 44 | F |
| Seifert G18 | 1997 | Warthin tumor | Mucoepidermoid carcinoma | 73 | M |
| Hanada T19 | 1995 | Myoepithelioma | Adenoid cystic carcinoma | 71 | F |
| Gnepp DR3 | 1989 | Warthin tumor | Mucoepidermoid carcinoma | 60 | M |
| Warthin tumor | Acinic cell carcinoma | 84 | M | ||
| Warthin tumor | Acinic cell carcinoma | 56 | M | ||
| Warthin tumor | Ductal adenocarcinoma | 69 | M | ||
| Warthin tumor | Adenoid cystic carcinoma | 66 | M | ||
| Janecka IP20 | 1983 | Pleomorphic adenoma | Mucoepidermoid carcinoma | 45 | F |
| Warthin tumor | Adenocarcinoma | 64 | M | ||
| Warthin tumor | Mucoepidermoid carcinoma | 58 | M | ||
| Volmer J21 | 1982 | Warthin tumor | Squamous cell carcinoma | 85 | F |
| Pontilena N22 | 1979 | Pleomorphic adenoma | Mucoepidermoid carcinoma | 45 | F |
| Bab IA23 | 1979 | Sebaceous cell adenoma | Adenoid cystic carcinoma | 6th decade | F |
| Oncocytoma | Carcinoma ex pleomorphic adenoma | 6th decade | F | ||
| Bird RJ24 | 1979 | Warthin tumor | Acinic cell carcinoma | ND | ND |
| Gadient SE25 | 1975 | Warthin tumor | Mucoepidermoid carcinoma | 60 | M |
| Iannaccone P26 | 1975 | Warthin tumor | Mucoepidermoid carcinoma | 70 | F |
| Lumerman H27 | 1975 | Warthin tumor | Mucoepidermoid carcinoma | 65 | M |
| Turnbul AD28 | 1969 | Warthin tumor | Carcinoma ex pleomorphic adenoma | ND | ND |
| Pleomorphic adenoma | Adenocarcinoma | ND | ND | ||
| Tanaka N5 | 1953 | Warthin tumor | Mucoepidermoid carcinoma | ND | ND |
ND, no data.
This paper is the first one to present an in-depth study of a rare case of Warthin tumor coexisting with carcinoma ex pleomorphic adenoma in the same salivary gland. Only one occurrence of this kind has been just sparingly mentioned, without any study or analysis, in the English language literature in the 1960s.12, 28 The occurrence of carcinoma ex pleomorphic adenoma in our patient is typical for this type of malignancy (6th–7th decade of life), which may suggest that the synchronous concomitance of Warthin tumor was coincidental, and the initial state was the most popular combination of histologically different tumors – pleomorphic adenoma and Warthin tumor. The etiology of carcinoma ex pleomorphic adenoma is associated with the accumulation of genetic instabilities in long-standing pleomorphic adenomas, hence in the present case, the primary tumor was present for many years, what is important for process of malignization.1, 6, 7 Although there are some data about the incidence of multiple parotid tumors after radiotherapy, our patient had no history of radiation before.12
Clinical examination, imaging investigation and fine needle biopsy proved inefficient in this case. Although no particular type of radiological investigation has been defined in the detection of unilateral parotid tumors, the combination of ultrasound and MRI seems to have the best effectiveness rates in differentiating malignant lesions from benign ones.29 Fine needle aspiration cytology is crucial in the evaluation of parotid tumors. However, its role in case of unilateral synchronous tumor is controversial.30
Previous studies implied that the treatment and anticipated survival rate should be analogous to the cases of malignant neoplasms of the same histological type. Surgery is the gold standard in treatment of this kind of lesions. The presence of a malignancy might require a more aggressive approach, hence, depending on the nature and the location of the tumor – total or subtotal parotidectomy is indicated.6 Intraoperative frozen section biopsy might add important information that could alter the management and improve the final outcome of the treatment. Our case seems to confirm that a routine use of this examination may have influenced the extent of the surgical management in the way that the total parotidectomy and the elective I and II level lymph node removal would be performed. Thus, re-operation would not be necessary.31
Adjuvant radiotherapy is highly recommended for high-grade malignancies like carcinoma ex pleomorphic adenoma, due to a high risk of locoregional recurrence. Due to the fact that the surgical treatment was not optimal in this case, the patient was qualified for radiation therapy in order to minimize the risk of subclinical microscopic spread of the disease.32
Conclusions
Multiple synchronous unilateral parotid tumors may cause significant discrepancies between the preliminary and definitive histopathological prognosis, especially when pre-operative clinical assessment and FNAC did not indicate the presence of two different neoplasms within one gland. The awareness of the coexistence of benign and malignant lesions in ipsilateral parotid gland should raise the clinical vigilance in the process of evaluation of a parotid mass.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Ochal-Choińska A, Bruzgielewicz A, Osuch-Wójcikiewicz E. Synchronous multiple unilateral parotid gland tumors of benign and malignant histological types: case report and literature review. Braz J Otorhinolaryngol. 2019;85:388–92.
References
- 1.Eveson J.W., Auclair P., Gnepp D.R., El-Naggar A.K. In: Pathology and genetics of head and neck tumours. World Health Organization classification of tumours. Barnes L., editor. IARC Press; Lyon: 2005. Tumours of the salivary glands; pp. 209–282. [Google Scholar]
- 2.Zeebregts C.J., Mastboom W.J., van Noort G., van Det R.J. Synchronous tumours of the unilateral parotid gland: rare or undetected? J Craniomaxillofac Surg. 2003;31:62–66. doi: 10.1016/s1010-5182(02)00165-8. [DOI] [PubMed] [Google Scholar]
- 3.Gnepp D.R., Schroeder W., Heffner D. Synchronous tumors arising in a single major salivary gland. Cancer. 1989;63:1219–1224. doi: 10.1002/1097-0142(19890315)63:6<1219::aid-cncr2820630631>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 4.Seifert G., Donath K. Multiple tumours of the salivary glands – terminology and nomenclature. Eur J Cancer B Oral Oncol. 1996;32B:3–7. doi: 10.1016/0964-1955(95)00063-1. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka N., Chen W. A case of bilateral papillary cystadenoma lymphomatosum (Warthin's tumor) of the parotid complicated with muco-epidermoid tumor. Gan. 1953;44:229. [PubMed] [Google Scholar]
- 6.Ethunandan M., Pratt C.A., Morrison A., Anand R., Macpherson D.W., Wilson A.W. Multiple synchronous and metachronous neoplasms of the parotid gland: the Chichester experience. Br J Oral Maxillofac Surg. 2006;44:397–401. doi: 10.1016/j.bjoms.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 7.Yu G., Ma D., Zhang Y., Peng X., Cai Z., Gao Y., et al. Multiple primary tumours of the parotid gland. Int J Oral Maxillofac Surg. 2004;33:531–534. doi: 10.1016/j.ijom.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Jin J., Chen Y. Unilateral parotid gland involvement with synchronous pleomorphic adenoma and lymphoepithelial carcinoma: a case report and literature review. Shanghai Kou Qiang Yi Xue. 2011;20:556–558. [PubMed] [Google Scholar]
- 9.Srivastava S., Nadelman C. Synchronous ipsilateral Warthin tumor encased by a separate mucoepidermoid carcinoma of the parotid gland: a case report and review of the literature. Diagn Cytopathol. 2010;38:533–537. doi: 10.1002/dc.21267. [DOI] [PubMed] [Google Scholar]
- 10.Roh J., Kim J., Park C.I. Synchronous benign and malignant tumors in the ipsilateral parotid gland. Acta Otolaryngol. 2007;127:110–112. doi: 10.1080/00016480600606707. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka S., Tabuchi K., Oikawa K., Kohanawa R., Okubo H., Ikebe D., et al. Synchronous unilateral parotid gland neoplasms of three different histological types. Auris Nasus Larynx. 2007;34:263–266. doi: 10.1016/j.anl.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Bień S., Kamiński B., Kopczyński J., Sygut J. The synchroneous tumors of different histopathology in the parotid salivary gland. Otolaryngol Pol. 2005;60:703–708. [PubMed] [Google Scholar]
- 13.Azúa-Romeo J., Saura Fillat E., Usón Bouthelier T., Tovar Lázaro M., Azúa Blanco J. Tumores sincrónicos de glándula salivar: a propósito de dos casos. Rev Esp Cirug Oral Maxilofac. 2005:27. [Google Scholar]
- 14.Shukla M., Panicker S. Synchronous sebaceous lymphadenoma with squamous cell carcinoma – case report. World J Surg Oncol. 2003;1:30. doi: 10.1186/1477-7819-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curry J.L., Petruzzelli G.J., McClatchey K.D., Lingen M.W. Synchronous benign and malignant salivary gland tumors in ipsilateral glands: a report of two cases and a review of literature. Head Neck. 2002;24:301–306. doi: 10.1002/hed.10048. [DOI] [PubMed] [Google Scholar]
- 16.Mayorga M., Fernández N., Val-Bernal J.F. Synchronous ipsilateral sebaceous lymphadenoma and acinic cell adenocarcinoma of the parotid gland. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:593–596. doi: 10.1016/s1079-2104(99)70091-0. [DOI] [PubMed] [Google Scholar]
- 17.Misselevich I., Fradis M., Podoshin L., Boss J.H. Salivary gland double tumor: synchronous ipsilateral pleomorphic adenoma and acinic cell carcinoma of the parotid gland. Ann Otol Rhinol Laryngol. 1997;106:226–229. doi: 10.1177/000348949710600308. [DOI] [PubMed] [Google Scholar]
- 18.Seifert G. Bilateral mucoepidermoid carcinomas arising in bilateral pre-existing Warthin's tumours of the parotid gland. Oral Oncol. 1997;33:284–287. doi: 10.1016/s0964-1955(97)00018-3. [DOI] [PubMed] [Google Scholar]
- 19.Hanada T., Hirase H., Ohyama M. Unusual case of myoepithelioma associated with adenoid cystic carcinoma of the parotid gland. Auris Nasus Larynx. 1995;22:65–70. doi: 10.1016/s0385-8146(12)80185-4. [DOI] [PubMed] [Google Scholar]
- 20.Janecka I.P., Perzin K.H., Sternschein M.J. Rare synchronous parotid tumors of different histologic types. Plast Reconstr Surg. 1983;72:798–802. doi: 10.1097/00006534-198312000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Volmer J. Multiple unilateral tumors of the salivary parotid gland. Zentralbl Allg Pathol. 1982;126:327–334. [PubMed] [Google Scholar]
- 22.Pontilena N., Rankow R.M. Coexisting benign mixed tumor and mucoepidermoid carcinoma of the parotid gland. Ann Otol Rhinol Laryngol. 1979;88:327–330. doi: 10.1177/000348947908800305. [DOI] [PubMed] [Google Scholar]
- 23.Bab I.A., Ulmansky M. Simultaneously occurring salivary gland tumors of different types. J Oral Surg. 1979;37:826–828. [PubMed] [Google Scholar]
- 24.Bird R.J., Chait G.E., Snell G.E., van Nostrand A.W. Multiple tumors of the parotid gland. J Otolaryngol. 1979;8:435–438. [PubMed] [Google Scholar]
- 25.Gadient S.E., Kalfayan B. Mucoepidermoid carcinoma arising within a Warthin's tumor. Oral Surg Oral Med Oral Pathol. 1975;40:391–398. doi: 10.1016/0030-4220(75)90426-0. [DOI] [PubMed] [Google Scholar]
- 26.Iannaccone P.R. Multiple primary tumors. Four distinct head and neck tumors. Arch Pathol. 1975;99:270–272. [PubMed] [Google Scholar]
- 27.Lumerman H., Freedman P., Caracciolo P., Remigio P.S. Synchronous malignant mucoepidermoid tumor of the parotid gland and Warthin's tumor in adjacent lymph node. Oral Surg Oral Med Oral Pathol. 1975;39:953–958. doi: 10.1016/0030-4220(75)90117-6. [DOI] [PubMed] [Google Scholar]
- 28.Turnbull A.D., Frazell E.L. Multiple tumors of the major salivary glands. Am J Surg. 1969;118:787–789. doi: 10.1016/0002-9610(69)90230-x. [DOI] [PubMed] [Google Scholar]
- 29.Goto T.K., Yoshiura K., Nakayama E., Yuasa K., Tabata O., Nakano T., et al. The combined use of US and MR imaging for the diagnosis of masses in the parotid region. Acta Radiol. 2001;42:88–95. doi: 10.1080/028418501127346305. [DOI] [PubMed] [Google Scholar]
- 30.Snyderman N.L., Myers E.N., Robbins K.T., Suen J.Y. Bilateral parotid neoplasms. Head Neck. 1994;16:598–602. doi: 10.1002/hed.2880160619. [DOI] [PubMed] [Google Scholar]
- 31.Arabi Mianroodi A.A., Sigston E.A., Vallance N.A. Frozen section for parotid surgery: should it become routine? ANZ J Surg. 2006;8:736–739. doi: 10.1111/j.1445-2197.2006.03844.x. [DOI] [PubMed] [Google Scholar]
- 32.Lim C.M., Hobson C., Kim S., Johnson J.T. Clinical outcome of patients with carcinoma ex pleomorphic adenoma of the parotid gland: a comparative study from a single tertiary center. Head Neck. 2015;37:543–547. doi: 10.1002/hed.23638. [DOI] [PubMed] [Google Scholar]