Abstract
Objective
The Covid-19 health crisis has disrupted the organization and functioning of European mental health and psychiatric services, impacting the working conditions – already difficult before the epidemic – of professionals working therein. The Psy-GIPO2C project investigated the impact of the pandemic on these professionals. The Psy-GIPOC2C project has been co-funded by the Agence Nationale de la Recherche française (ANR, French National Research Agency) and the Centre-Val de Loire region (France).
Method
This research took the form of a collaborative mixed methods study. The data collected through qualitative and quantitative research were analyzed during a working session held by the research consortium, which resulted in the formulation of recommendations for action to optimize the occupational health of European mental health professionals.
Results
This research made it possible to identify and explain the extent to which, and the ways in which, the reorganization of European mental health services has impacted the mental health of the professionals working therein, and, in particular, to highlight the fact that the unprecedented use of digital devices has generated stress, and even tension, within these services.
Conclusions
It is important to promote well-being at work among European mental health professionals, by involving them in the development of ad hoc measures (in addition to the existing psychological support measures available) to enable them to recharge their batteries. It is also important to support current and future professionals in their appropriation of digital tools for professional use.
Keywords: SARS-CoV-2, COVID-19, epidemic, pandemic, health crisis, mental health, psychiatry, occupational health, prevention, burnout, telepsychiatry, professional practices, information, training, ethics
Introduction
The Covid-19 health crisis has had a major impact on the organization and functioning of all national health services, including mental health services (Cabrera et al., 2020). The implementation of public health measures to limit the transmission of SARS-CoV-2 has had a direct impact on the working conditions of health professionals around the world, including mental health professionals (Gourret Baumgart et al., 2021; Kane et al., 2021). In addition to compliance with barrier measures, including social distancing, mask wearing, handwashing, disinfecting and ventilation of surfaces and spaces, numerous reorganizations have also been implemented. Some facilities have set up areas exclusively for receiving users awaiting the results of their screening tests or who have tested positive for Covid-2019. Certain establishments have also had to reduce beds, or even temporarily close day care and/ or outpatient services, and stop therapeutic activities which do not meet the requirements of Covid measures, as well as stopping visits to which hospitalized patients were previously entitled. Institutions have also had to adapt the composition of the teams, schedules and working methods of their professionals, limiting physical meetings, encouraging the use of digital devices and, in some cases, teleworking.
In this context of the Covid-19 pandemic engendering reorganizations, healthcare professionals in general have been recognized as an at-risk group, being more exposed to risks to their mental health (García-Iglesias et al., 2020; Huang & Zhao, 2021; Muller et al., 2020; Vancappel et al., 2021). Indeed, they incur an increased risk of anxiety, depression, burnout, post-traumatic stress and addiction, and even suicide (El-Hage et al., 2020; Raudenská et al., 2020). For mental health professionals, this risk is increased because the onset of this pandemic and the reorganizations required have occurred in a context wherein working conditions in psychiatry and mental health have already been difficult in many countries for years, even before the emergence of the epidemic (Bourdeux, 2003; Petho, 2008). Added to the double challenge of psychological and physical work inherent to psychiatric and mental health work (Estryn-Behar et al., 2006), is the lack of resources which prevents the professionals in these services from working in conditions conducive to ensuring the quality of care they should provide. As these difficulties are regularly reported, especially by practitioners, recruiting new professionals willing to be trained and to work in mental health has become increasingly complicated over the past several years (Lunn, 2011). This is all the more problematic as the mental health care needs of the European population have steadily increased over the years, and researchers and professionals predict a "psychiatric wave" following the Covid-19 health crisis (Han et al., 2020), suggesting a further increase in workload for these professionals.
In this context of uncertainty and anxiety, the aim of the Psy-GIPO2C project was to observe the reorganizations generated in European psychiatric and mental health services, and to study how professionals in these services have adapted to ensure both continuity and quality of mental health care.
Materials and methods:
Study design
This was a collaborative study using mixed methods – qualitative and quantitative (Creswell, 2011; Guével & Pommier, 2012) conducted between March and November 2021 in Europe, in order to document the impact of the Covid-19 health crisis on European mental health professionals. The objective of the research was to develop recommendations for decision-makers in order to support a coherent response to the crisis situation in national mental health services (Fond-Harmant et al., 2021).
Research consortium
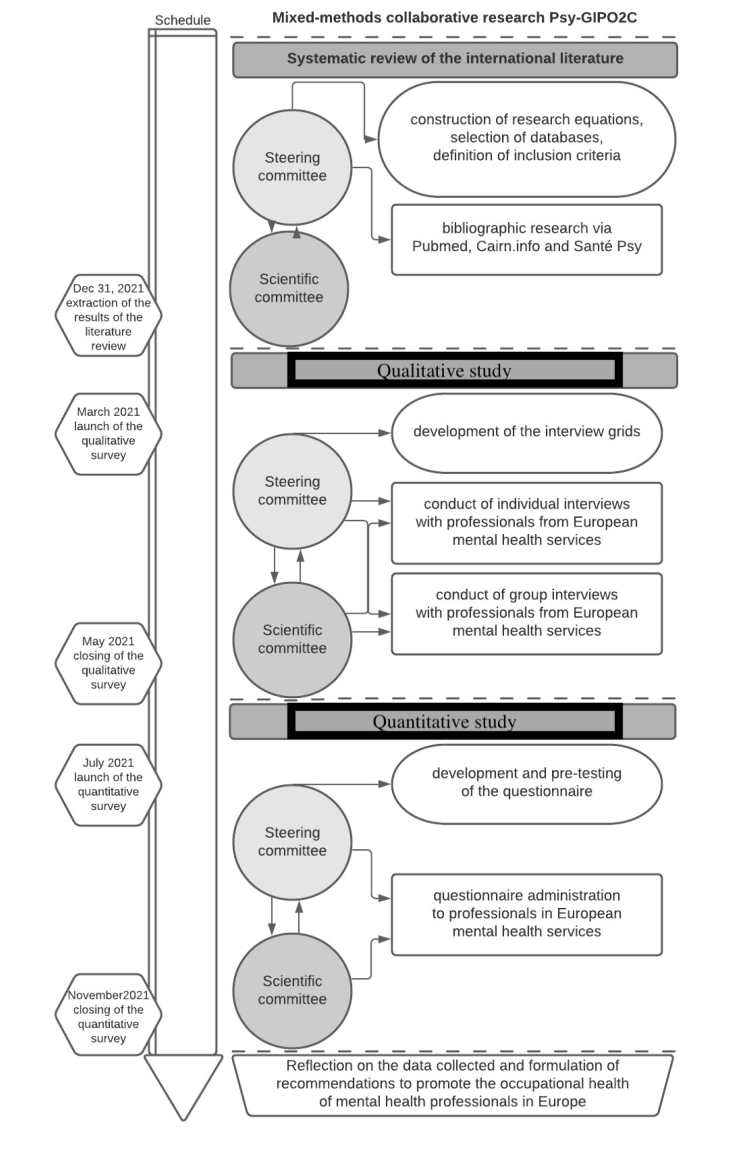
The research consortium which initiated this study comprised the project coordinator, study and research designers as well as European researchers – specialists in public health, mental health, psychiatry, psychology, health sociology, health anthropology, health-related law and ethics (Appendix 1). These researchers are associated as both partners and experts. The members of the research consortium collaborated in the successive phases of this research (figure 1). Steering committee (Copil) meetings took place weekly, and scientific committee (SC) meetings were held approximately monthly. These steering committee meetings and 5 of the 6 scientific committee meetings were held by videoconference.
Figure 1.
Organizational chart of the Psy-GIPO2C mixed methods collaborative research project
Systematic literature review of the international
A systematic review of the international literature (Gourret Baumgart et al., 2021; Kane et al., 2021) was undertaken in accordance with PRISMA recommendations (Moher et al., 2010). The search equations to be implemented were developed and then the search, on titles and abstracts, was carried out on PubMed, Cairn.info and SantéPsy databases. This literature review included articles published in 2020, in English or French, addressing adaptations implemented within mental health facilities in different countries of the world in response to the Covid-19 health crisis. The results of this bibliographical research contributed to the development of the interview grids (Appendix 2) – for the qualitative survey – as well as the questionnaire format (Appendix 3) – for the quantitative survey -, formulated around three salient themes: organizational adaptations, the use of digital devices, and professional and personal experiences reported regarding the health crisis.
Qualitative research
In order to investigate the experiences of professionals, individual and group interviews were conducted between March and May 2021, with professionals from mental health services in European countries: Germany, Belgium, France, Italy and Luxembourg, these being the countries in which the partners involved in the present research were based.
Developing the interview grids
The interview grids developed by the researchers from the results of the literature review were reworked and validated by the members of the research consortium, some of whom also work in psychiatry. These ad hoc grids are structured around the above-mentioned lines of questioning (Appendix 2). The questions are adaptable to the work context, and the order of the questions are interchangeable in order to respect the specific dynamics of each interview.
Conducting the interviews
The group interviews (GI) were organized by the German, Belgian, French, Italian and Luxembourg partners of this research in the countries in which they practice. The researchers ensured that the methodological approaches adopted for the group interviews were standardized prior to them being conducted, and they participated as observers. They also conducted the individual interviews (II) scheduled by the Belgian and French partners of the research. The professionals surveyed were recruited on a voluntary basis. Due to the context of the health crisis, all group interviews and some individual interviews were conducted remotely. The interviews were continued until the data saturation threshold was reached (Guest et al., 2006).
Method of analysis for qualitative data
The recordings were professionally transcribed and the German and Italian verbatims were then translated into English. These transcriptions and translations were then imported into the NVivo© software. This software was used to analyze the interviews using a thematic analysis tree developed by the researchers, who first coded some of the interviews in order to check the consistency of the coding and to adjust the thematic analysis tree by re-specifying the content of some of the branches, before coding all of the remaining interviews.
Quantitative survey
In order to measure the varying impacts of this crisis on professionals, an online questionnaire was circulated between the beginning of July and the end of November 2021 among professionals in mental health and psychiatric services in European countries: Belgium, Czech Republic, Finland, France, Germany, Greece, Iceland, Italy, Luxembourg, the Netherlands, Poland, Portugal, Spain, Sweden, Switzerland, Romania and the United Kingdom, these being the countries in which the partners and experts involved in the present research were based.
Questionnaire design
The online questionnaire developed by the researchers was pre-tested among all the members of the research consortium, who validated the final version. This questionnaire (Appendix 3), structured around the above-mentioned lines of questioning, comprises 59 questions, – yes/no, multiple choice and open-ended, including some conditional questions. The questionnaire was structured in three parts : the first part of questions concerning the organizational adaptations, the second part investigating the use of digital devices, and the third part questioning the professional and personal experience of the health crisis. The online questionnaire was created and distributed via the SphinxOnline© software.
Conducting the questionnaires
Targets for the number of respondents per country were set between 60 and 120 ; these targets were determined by considering the number of inhabitants per country. Distribution of the questionnaire among professionals working in the national mental health services of the countries concerned was mainly undertaken by the research partners and experts. They communicated the link to the online questionnaire on their professional social networks and/or those of their institutions, transmitted the link directly via email lists, and invited individual professionals to respond. Regular follow-ups were conducted between July and December 2021. In addition to this, national associations representing professional groups in the field of psychiatry and mental health, or involved in actions related to these themes, were asked to distribute the questionnaire to their networks.
Method of analysis for quantitative data
The SphinxOnline© software was used to analyze research responses. Using the analysis tools featured by the software, the researchers extracted flat-sorted and cross-sorted tables and performed textual analyses on responses to the open questions.
Developing recommendations
Following on from the meetings held by video conference throughout the study, some members of the research consortium met in September 2021 in Paris for an enlarged scientific committee meeting proposing a collective workshop to reflect on the qualitative and quantitative data collected, in view of formulating recommendations to optimize the occupational health of mental health professionals in Europe (figure 1).
Ethics
The Psy-GIPOC2C project has been co-funded by the Agence Nationale de la Recherche française (ANR, French National Research Agency) and the Centre-Val de Loire region (France). This research received ethical approval from the ethics committee of the Centre Hospitalier Régional Universitaire de Tours on 4 February 2021 (n° 2021 006).
Results
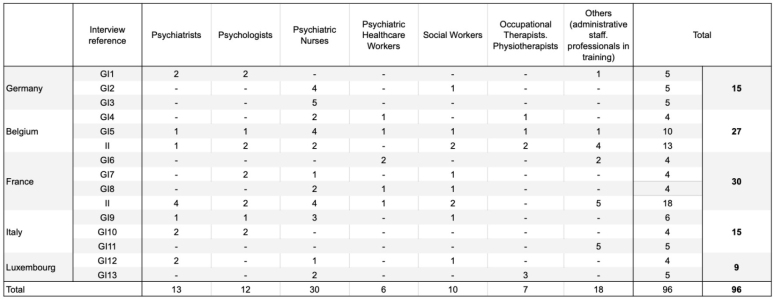
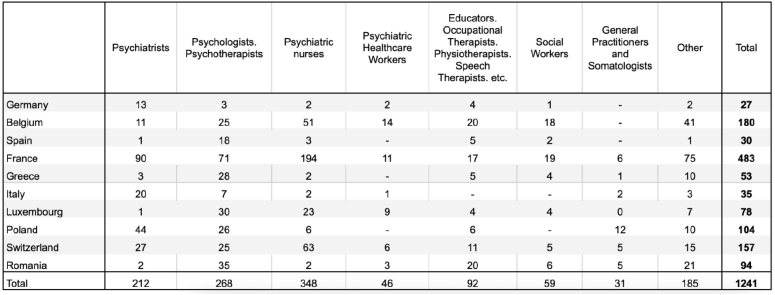
In total, 13 group interviews (GI) and 31 individual interviews (II) were conducted among 96 professionals (table 1) and the questionnaire (Q0) was completed by 1264 professionals (table 2). However, countries with fewer than 25 respondents were not included and thus the responses of 1241 mental health workers from 10 European countries were included in the analysis.
Table 1.
Occupational distribution of European mental health professionals participating in the qualitative survey
Table 2.
Occupational distribution of European mental health professionals participating in the quantitative survey
The cross-analysis of qualitative and quantitative data collected from 1337 European mental health professionals highlighted the fact that the new working conditions and the unprecedented use of e-mental health devices affected the mental health of European mental health service professionals, generating stress and creating tension within European mental health services.
New working conditions affecting the mental health of European mental health service professionals
The research highlighted the fact that, in addition to a general context marked by restrictions and fear and, for some, difficult personal situations, the upheavals in their professional life contributed to a deterioration in mental health for some of the European professionals surveyed.
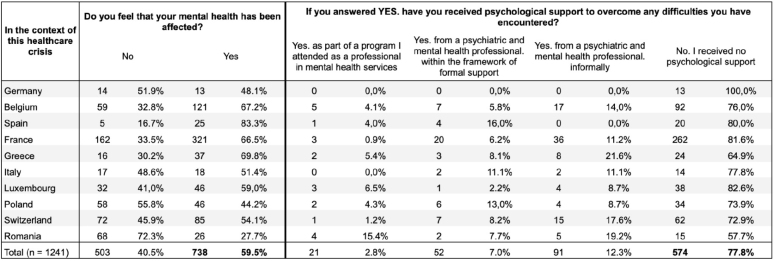
The professionals interviewed cited the organizational and relational changes which contributed to this phenomenon. For example, they explained that it may have been difficult for them to: be obliged to work from home, have to take on new tasks which are not part of their usual duties, or even having to take on new roles sometimes far removed from the reasons why they became involved in psychiatric care, or having the feeling that the quality of the care provided to the users they support has deteriorated. The questionnaire made it possible to estimate the proportion of professionals concerned: among the 1241 people surveyed, 59.5% considered that their own mental health has been affected by the context of the Covid-19 health crisis (table 3).
Table 3.
Distribution of the European mental health professionals surveyed according to their reported mental health and concerning their use of a specific psychological support system
Furthermore, the qualitative and quantitative data converge on the fact that, in this context of health crisis, some of the professionals surveyed encountered more difficulties in reconciling their professional and personal lives. The professionals concerned mentioned, in particular, the fact that they only had “rare times alone” (psychiatric nurse, male, Switzerland), “the constant presence of relatives without the possibility of escape” (psychiatrist, male, France). Other professionals cited the fact of “not having many places to recharge their batteries” (social worker, female, France), “nowhere to relax due to sports and cultural activities having stopped…” (social worker, female, France). Many professionals also stressed during the interviews the importance of informal sociability at work, complaining that the constraints imposed in the context of the health crisis had led to a reduction or even suppression of informal time with colleagues, time which they considered important for their well-being at work.
Of the 738 respondents who reported via the questionnaire survey that their own mental health had been affected (table 4): 77.8% said that they had not received specific psychological support to cope with their difficulties. Some professionals mentioned during the interviews the fact that the psychological support services offered on a local level – by mental health care structures, for professionals working there – are generally implemented with the participation of professionals working within these structures. As such, they cite this as a reason for their own reluctance to use these services. Regarding those professionals who replied via the questionnaire survey that they had received specific support: 12.3% said that they had received psychological support from a mental health professional informally, 7.0% said they had received psychological support from a mental health professional as part of a formal care program, and 2.8% said they had received psychological support as part of a special program they had followed as professionals in mental health services.
Table 4.
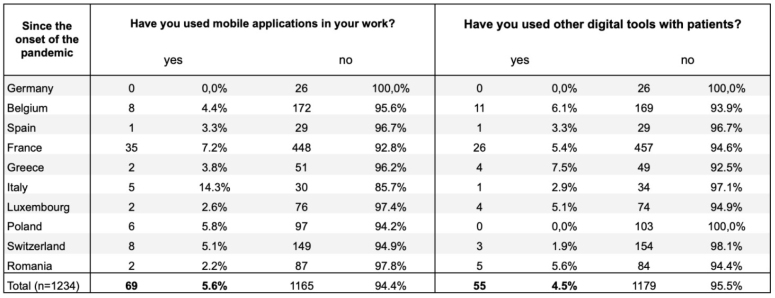
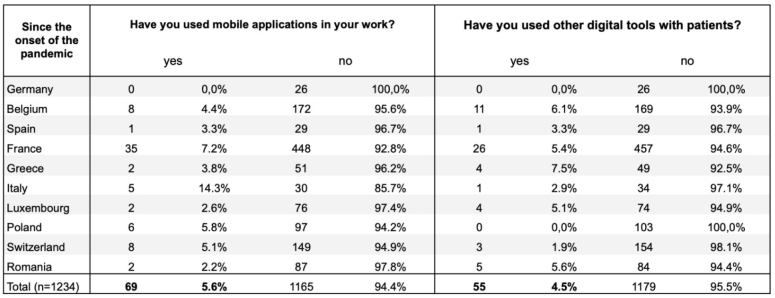
Distribution of European mental health professionals surveyed according to their reported use of mobile applications or other digital tools in their professional practice
Unprecedented use of e-mental health devices has created stress and tension within European mental health services
The surveys highlighted the fact that, since the onset of the Covid-19 health crisis – due the physical distancing measures implemented to limit the spread of the virus – there has been an unprecedented use of digital devices for business purposes among the European professionals surveyed.
Although the questionnaire survey tends to show that relatively few healthcare professionals have used mobile applications (5.6%) or devices other than mobile applications and videoconferencing platforms – connected objects, for example – (4.5%) (table 4), the results nevertheless show that many have used videoconferencing in their professional practice, for their exchanges with both users and colleagues (tables 5 and 6).
Table 5.
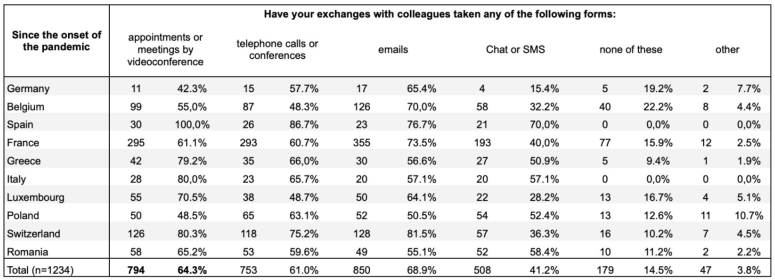
Distribution of the European mental health professionals surveyed according to their reported use of the different digital devices in their professional practice with patients
Table 6.
Distribution of the European mental health professionals surveyed according to their reported use of the different digital devices in their professional practice with colleagues
Indeed, since the onset of the Covid-19 pandemic, 39.1% of the professionals surveyed have used videoconferencing for individual exchanges with users of European mental health services. For 71.2% of these, the use of videoconferencing for the therapeutic follow-up of users was a novelty, something they had never experienced before; for 22.4%, it was a practice initiated before the pandemic; and for 6.4% of them, it was a habit adopted before the pandemic. The professionals interviewed who had experimented with videoconferencing for exchanging with users unanimously agreed, however, that interacting with a patient via a videoconferencing platform is not the same as interacting face-to-face.
Moreover, since the Covid-19 pandemic, 64.3% of the professionals surveyed have used videoconferencing in their interactions with colleagues. For 70,5% of respondents, the use of videoconferencing for exchanges with colleagues was new to them and they had never experienced it before; for 22.5% of them, it was a practice initiated prior to the pandemic; while for 6.9%, it was a habit already established before the pandemic.
Furthermore, 65.5% of the European professionals surveyed who had used videoconferencing since the start of the Covid-19 pandemic stated that they still use videoconferencing platforms for their work: 35.9% reported using it once or several times a month, 48.2% once or several times a week and 15.3% once or several times a day.
As reported by the professionals interviewed, in a context characterized by urgency, mental health professionals received a lot of practical information, particularly concerning the use of these new tools, information which was not unambiguous and frequently changing. The interviews also highlighted the fact that most of these professionals were neither sufficiently informed of the issues inherent to the use of digital devices in this particular context, nor were they specifically trained in their use of such devices – telepsychiatry platforms in particular – in their professional practices in psychiatry and mental health. The qualitative and quantitative data converge on the fact that the use of these new digital tools has raised ethical questions for the professionals concerned, to which they have not yet found answers, and that this may have led to stress, or even tension between colleagues. This was all the more true given that some of the professionals, who were sometimes forced to adopt these new tools, reported that they had not been provided with the appropriate equipment for these new practices.
Discussion
The analysis of qualitative data (collected from 96 professionals) and quantitative data (collected from 1241 professionals) gathered for the Psy-GIPO2C study, carried out in the context of the COVID-19 health crisis, highlights the importance of promoting well-being at work and supporting mental health professionals in their process of appropriating the use of digital devices.
Promoting well-being at work and preventing burnout, psychological distress and post-traumatic stress disorder among European mental health professionals
Since the onset of the Covid-19 pandemic, various national organizations around the world have issued a number of recommendations aimed at safeguarding the occupational health of health service professionals in general in this crisis context (Institut de recherche Robert-Sauvé en santé et en sécurité au travail, 2020). In Canada, for example, the teams of the Robert-Sauvé Occupational Health and Safety Research Institute have published a fact sheet aimed at “Preventing psychological distress among staff in the health and social services network”. In this regard, it is particularly recommended to “provide a rest area in a calm environment in a room with soft lighting, comfortable furniture, hot drinks, access to a telephone (...) tissues, glasses of water, healthy snacks, blankets”, to “offer short breathing, relaxation or meditation exercises which staff are able to practice in the workplace” and to “establish places or times for the team to engage in brief calming activities in the workplace”. Although these proposals are probably not specifically designed to take into account the particular aspects of work in psychiatry and mental health, this type of recommendation could nevertheless constitute avenues of reflection for devising "customized" systems (Maccaferri et al., 2021), on a local level and with the participation of the professionals concerned.
Indeed, it seems relevant to the members of the research consortium that all professionals working in mental health services should have access – in addition to the existing psychological support facilities already available to them – to ad hoc facilities to enable them to relax and recharge their batteries. It would be useful to involve mental health professionals who are supposed to benefit from these schemes in their design and implementation, or at least to involve representatives of the different categories of professionals who will benefit from these schemes. As a result of such a participatory approach, and given the need for "time for oneself" expressed by the professionals surveyed, it is possible, for example, to imagine equipped spaces – designed to enable each professional who feels the need to do so to take time for themselves – being established in certain mental health services. Given the importance of socializing with colleagues, which was emphasized by many of the professionals surveyed, it is also possible to imagine setting up spaces adapted to and dedicated to sharing social time with colleagues. These ad hoc arrangements could be developed in addition to existing psychological support measures, which have been and continue to be offered to professionals in mental health services, to promote their well-being at work.
Supporting European mental health professionals in their appropriation of the uses of digital devices
In this context, the members of the research consortium feel that all professionals working in mental health services should be better informed about the issues inherent to using new technologies in their professional practice, and that they be better supported in their appropriation of these digital tools. In this sense, it would be appropriate to involve mental health professionals in awareness campaigns, or even to provide training on the ethical uses of digital devices which can be used in professional practice in psychiatry and mental health. At the end of the training program, resulting in a diploma, the professionals trained in this way could be certified in the use of digital devices used in mental health. In addition to practicing professionals, there is also the issue of training future mental health professionals of all professions – i.e. psychiatric interns, psychologists, psychiatric nurses, specialized educators in training, etc. It seems furthermore appropriate to add a module on the ethical use of digital devices in psychiatric care to the training content targeted at these professions.
In some countries, training programs devoted to the use of digital devices have been developed for health professionals (Pathipati et al., 2016) – and this is particularly true in France (Yaghobian et al., 2020). The specific characteristics of work in psychiatry and mental health justify implementing specific programs for professionals and future professionals in mental healthcare. In this sense, researchers interested in the subject of telepsychiatry have been arguing for several years – even before the Covid-19 pandemic – that providing quality mental health care to users in the context of videoconferencing consultations requires specific skills in professionals (Hilty et al., 2015) and argue they should be trained, both as part of initial and ongoing training (Saeed et al., 2017). This being said, for an ethical and proper use of digital devices – insofar as it would preserve occupational health and guarantee quality of care – training professionals is probably a necessary but not sufficient condition. It is important not only to support the professionals of the various professions in their appropriation of these new tools, but also to provide them with the appropriate equipment, depending on the uses they wish to make of these tools (Smith et al., 2020). Digital transitions require professionals to have the right skills for their wellbeing at work and for their success.
Limitations
First of all, it is important to mention a bias concerning qualitative and quantitative surveys, which is due to the fact that the professionals interviewed were recruited on a voluntary basis and that the online questionnaire was self-administered: this inevitably results in self-selection bias. Secondly, it is important to mention that, for obvious reasons related to the health context, some of the interviews had to be conducted by videoconference. Despite certain disadvantages inherent to videoconference interviews compared to face-to-face interviews, VoIP technology tools represented an adequate medium for qualitative data collection in this context, enabling the qualitative survey to be successfully carried out (Hjorth et al., 2017). Finally, it is necessary to specify that the data presented are not intended for the purpose of making comparisons between countries. This is not only because there are large differences in the number of respondents between the countries in which the online questionnaire was administered (with some countries having statistically insignificant response rates) but also because the individual and group interviews were only conducted in 5 of the 10 countries covered by the quantitative survey. Furthermore, the socio-political contexts of the 10 European countries included in the study are diverse, and the results of the survey were not contextualized in terms of the macro dimension of the situations, but only in terms of the subjective experiences reported by the professionals. Nevertheless, important recurrences and similarities can be observed in the feedback provided by the professionals surveyed, which make it possible for us to consider the results as a whole and tend to justify the validity of the proposed recommendations (Pink et al., 2018).
Despite these limitations, the Psy-GIPO2C project enabled the researchers to document the experiences of European mental health professionals during the first year and a half of the Covid-19 health crisis and, from this feedback, to propose relatively inexpensive recommendations for positive action to improve their occupational health. This research highlights the importance of optimizing the occupational health conditions of mental health professionals as far as possible (World Health Organisation (WHO), 1946). Behind this central issue is an underlying issue intimately linked to the fact that work in psychiatry and mental health is "relational work" (Bautzer, 2016). As the relational dimension of care is very important in the provision of care to people affected by mental disorders, it is essential to preserve the psychic availability of these professionals, which can be altered when their own mental health is affected. Therefore, not rendering the suffering of mental health professionals invisible and promoting their well-being at work is essential and contributes to indirectly improving the quality of care provided to people with mental health problems.
Acknowledgments
The authors would like to especially thank the participants who participated in the qualitative survey and/or in the quantitative survey for their time and participation.
Annex 1.
Presentation of the members of the research consortium and their involvement in the Psy-GIPO2C mixed methods collaborative research project
| SURNAME First_name | Affiliation | Implication in the project: | Copil | CS1 15/12 2021 | CS2 19/02 2021 | CS3 30/03 2021 | CS4 11/05 2021 | CS5 23/06 2021 | CS6 15-17/09/2021 | Quali | Quanti | Country of practice |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RUSCH Emmanuel | EA 75-05 Laboratory of Education, Ethics, Health, Faculty of Medicine, François- Rabelais University, Tours, France | Director of the Education, Ethics and Health Laboratory | France | |||||||||
| DENIS Frédéric | EA 75-05 Laboratory of Education, Ethics, Health, Faculty of Medicine, François- Rabelais University, Tours, France | Project Coordinator | X | X | X | X | X | X | X | X | X | France |
| FOND-HARMANT Laurence | Agency Cooperation, for Europe-Luxembourg, Africa Scientific Luxembourg | Partner | X | X | X | X | X | X | X | X | X | Luxembourg |
| GOURRET BAUMGART Jade | EA 75-05 Laboratory of Education, Ethics, Health, Faculty of Medicine, François-Rabelais University, Tours, France | Study Engineer | X | X | X | X | X | X | X | X | X | France |
| KANE Hélène | EA Health, 75-05 Faculty Laboratory of Medicine, of Education, François- Ethics, Rabelais University, Tours, France | Research Engineer | X | X | X | X | X | X | X | X | X | France |
| ABSIL Gaëtan | Laboratory of Social and Cultural Anthropology, École Libre Mosane, Social Department, University of Haute Liège, Liège, Belgium | Expert | X | X | Belgium | |||||||
| DELOYER Jocelyn | St-Belgium Martin Neuro Psychiatric Center, Namur, Belgium | Partner | X | X | X | X | X | X | X | X | Belgium | |
| EL-HAGE Wissam | CIC 1415, U 1253 iBrain, National Institute of Health Hospitalier and Medical Régional Research, Universitaire Centre de Tours CHRU, Tours, France | Partner | X | X | X | X | X | X | X | France | ||
| FUENZALIDA Claudio | Intrafamily Therapy Center, Elche, Spain | Expert | X | X | Spain | |||||||
| GAVRILA Mihaela | Faculty of Education, Psychology and Social Sciences, Aurel Vlaicu University, Arad, Romania | Expert | X | X | Romania | |||||||
| KELEMEN Gabriela | Faculty of Education, Psychology and Social Sciences, Aurel Vlaicu University, Arad, Romania | Expert | X | X | Romania | |||||||
| KRYSTA Krzysztof | Psychiatric Rehabilitation Department, Silesia University of Medicine, Katowice, Poland | Expert | X | X | Poland | |||||||
| KRZYSTANEK Marek | Psychiatric Silesia University Rehabilitation of Medicine, Department, Katowice, | Expert | X | Poland | ||||||||
| LE SAINT Laurent | Poland Luxembourg Hospital, Luxembourg | Expert | X | X | Luxembourg | |||||||
| LEBAS Marie-Clotilde | Department of Public Health Sciences and Motricity. Haute Ecole de la Province de Namur. Namur, Belgium | Partner | X | X | X | Belgium | ||||||
| MAES Christine | St-Martin Neuro Psychiatric Center, Namur, Belgium | Partner | X | X | X | X | X | X | X | X | Belgium | |
| MARAZZITI Donatella | Department of Clinical and Experimental Medicine, Psychiatry, University of Pisa, Pisa, Italy | Partner | X | X | X | X | X | X | X | X | Italy | |
| MORAITOU Margarita | Social Kepsipi, and Korydallos, Educational Greece Support Center, | Expert | X | X | Greece | |||||||
| POZZA Andrea | Department of Clinical and Experimental Medicine, Psychiatry, University of Pisa, Pisa, Italy | Expert | X | X | X | X | X | X | Italy | |||
| REUNANEN Merja | Department of Healthcare, University of Applied Sciences of Mikkeli, Savonlinna, Finland | Expert | X | Finland | ||||||||
| REXHAJ Shyherete | La Source Institute and School of Nursing, Lausanne, Switzerland | Expert | X | Switzerland | ||||||||
| THOME Johannes | Psychiatry Rostock, Germany Department, Rostock University, | Partner | X | X | X | X | Germany | |||||
| TUCHA Oliver | Psychiatry Rostock, Germany Department, Rostock University, | Partner | X | X | Germany | |||||||
| VERWAEST Wim | Luxembourg Hospital, Luxembourg | Expert | X | X | Luxembourg |
References
- Bautzer, É. R. (2016). Chapitre 2. Une approche sociologique du soin comme travail relationnel. Journal international de bioethique et d'ethique des sciences, 27(1), 41-57. [PubMed] [Google Scholar]
- Bourdeux, C. (2003). Psychiatry is in crisis! Soins Psychiatr(224), 5-7. (La psychiatrie est en crise!) [PubMed]
- Cabrera, M. A., Karamsetty, L., & Simpson, S. A. (2020). Coronavirus and Its Implications for Psychiatry: A Rapid Review of the Early Literature. Psychosomatics, 61(6), 607-615. 10.1016/j.psym.2020.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell, J. W. P. C. V. L. (2011). Designing and conducting mixed methods research. SAGE Publications. [Google Scholar]
- El-Hage, W., Hingray, C., Lemogne, C., Yrondi, A., Brunault, P., Bienvenu, T., Etain, B., Paquet, C., Gohier, B., Bennabi, D., Birmes, P., Sauvaget, A., Fakra, E., Prieto, N., Bulteau, S., Vidailhet, P., Camus, V., Leboyer, M., Krebs, M. O., & Aouizerate, B. (2020). Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks? Encephale, 46(3s), S73-s80. 10.1016/j.encep.2020.04.008 (Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19) : quels risques pour leur santé mentale ?) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estryn-Behar, D., Duville, N., Menini, M. L., Foll, S., Nézet, O., & Bocher, R. (2006). Mots à maux… Expression de la souffrance chez les soignants en psychiatrie. Étude comparative en France et dans trois autres pays européens. Annales Medico-psychologiques – ANN MEDICO-PSYCHOL, 164, 732-748. 10.1016/j.amp.2006.02.007 [DOI] [Google Scholar]
- Fond-Harmant, L., Kane, H., Gourret Baumgart, J., Rusch, E., Breton, H., El-Hage, W., Deloyer, J., Lebas, M. C., Marazziti, D., Thome, J., & Denis, F. (2021). International professional practices in mental health, organization of psychiatric care, and COVID-19: A survey protocol. PLOS ONE, 16(12), e0261818. 10.1371/journal.pone.0261818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Iglesias, J. J., Gómez-Salgado, J., Martín-Pereira, J., Fagundo-Rivera, J., Ayuso-Murillo, D., Martínez-Riera, J. R., & Ruiz-Frutos, C. (2020). Impact of SARS-CoV-2 (Covid-19) on the mental health of healthcare professionals: a systematic review. Revista espanola de salud publica, 94. Retrieved 2020/07//, from http://europepmc.org/abstract/MED/32699204 [PubMed]
- Gourret Baumgart, J., Kane, H., El-Hage, W., Deloyer, J., Maes, C., Lebas, M. C., Marazziti, D., Thome, J., Fond-Harmant, L., & Denis, F. (2021). The Early Impacts of the COVID-19 Pandemic on Mental Health Facilities and Psychiatric Professionals. Int J Environ Res Public Health, 18(15). 10.3390/ijerph18158034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field methods, 18(1), 59-82. [Google Scholar]
- Guével, M.-R., & Pommier, J. (2012). Recherche par les méthodes mixtes en santé publique : enjeux et illustration. Santé Publique, 24(1), 23-38. 10.3917/spub.121.0023 [DOI] [PubMed] [Google Scholar]
- Han, R. H., Schmidt, M. N., Waits, W. M., Bell, A. K. C., & Miller, T. L. (2020). Planning for Mental Health Needs During COVID-19. Current Psychiatry Reports, 22(12), 66. 10.1007/s11920-020-01189-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilty, D. M., Crawford, A., Teshima, J., Chan, S., Sunderji, N., Yellowlees, P. M., Kramer, G., O'Neill, P., Fore, C., Luo, J., & Li, S. T. (2015). A framework for telepsychiatric training and e-health: Competency-based education, evaluation and implications. Int Rev Psychiatry, 27(6), 569-592. 10.3109/09540261.2015.1091292 [DOI] [PubMed] [Google Scholar]
- Hjorth, L., Horst, H. A., Galloway, A., & Bell, G. (2017). The Routledge companion to digital ethnography. Routledge; New York. [Google Scholar]
- Huang, Y., & Zhao, N. (2021). Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychology, health & medicine, 26(1), 23-34. [DOI] [PubMed] [Google Scholar]
- Institut de recherche Robert-Sauvé en santé et en sécurité au travail. (2020). Prévenir la détresse psychologique chez le personnel du réseau de la santé et des services sociaux. https://www.irsst.qc.ca/covid-19/avis-irsst/id/2664/prevenir-la-detresse-psychologique-chez-le-personnel-du-reseau-de-la-sante-et-des-services-sociaux
- Kane, H., Gourret Baumgart, J., El Hage, W., Deloyer, J., Maes, C., Lebas, M. C., Marazziti, D., Thome, J., Fond-Harmant, L., & Denis, F. (2021). Uses of digital technologies in the time of Covid-19: opportunities and challenges for professionals in psychiatry and mental health care. JMIR Hum Factors. 10.2196/30359 [DOI] [PMC free article] [PubMed]
- Lunn, B. (2011). Recruitment into Psychiatry: An International Challenge. Australian & New Zealand Journal of Psychiatry, 45(10), 805-807. 10.3109/00048674.2011.615730 [DOI] [PubMed] [Google Scholar]
- Maccaferri, G. E., Fernandes, K. D. S., Khazaal, Y., Solomon, A. R., & Villars, J. (2021). Développement d’un outil de prévention destiné aux soignants d’un hôpital régional suisse en période COVID-19. Swiss Archives of Neurology, Psychiatry and Psychotherapy(5).
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2010). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg, 8(5), 336-341. [DOI] [PubMed] [Google Scholar]
- Muller, A. E., Hafstad, E. V., Himmels, J. P. W., Smedslund, G., Flottorp, S., Stensland, S., Stroobants, S., Van de Velde, S., & Vist, G. E. (2020). The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res, 293, 113441. 10.1016/j.psychres.2020.113441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathipati, A. S., Azad, T. D., & Jethwani, K. (2016). Telemedical Education: Training Digital Natives in Telemedicine. J Med Internet Res, 18(7), e193. 10.2196/jmir.5534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petho, B. (2008). Recent crisis of psychiatry in the context of modern and postmodern science. Psychiatr Hung, 23(6), 396-419. (A pszichiátria mai krízise a modern és posztmodern tudomány kontextusában.) [PubMed] [Google Scholar]
- Pink, S., Heather, H., Postill, J., Hjorth, L., Lewis, T., Tacchi, J. (2018). Digital ethnography: Principles and practice. In: SAGE Publications Sage UK: London, England. [Google Scholar]
- Raudenská, J., Steinerová, V., Javůrková, A., Urits, I., Kaye, A. D., Viswanath, O., & Varrassi, G. (2020). Occupational burnout syndrome and post-traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID-19) pandemic. Best Pract Res Clin Anaesthesiol, 34(3), 553-560. 10.1016/j.bpa.2020.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed, S. A., Johnson, T. L., Bagga, M., & Glass, O. (2017). Training Residents in the Use of Telepsychiatry: Review of the Literature and a Proposed Elective. Psychiatr Q, 88(2), 271-283. 10.1007/s11126-016-9470-y [DOI] [PubMed] [Google Scholar]
- Smith, K., Ostinelli, E., Macdonald, O., & Cipriani, A. (2020). COVID-19 and Telepsychiatry: Development of Evidence-Based Guidance for Clinicians. JMIR Ment Health, 7(8), e21108. 10.2196/21108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancappel, A., Jansen, E., Ouhmad, N., Desmidt, T., Etain, B., Bergey, C., d'Ussel, M., Krebs, M.-O., Paquet, C., Réveillère, C., Hingray, C., & El-Hage, W. (2021). Psychological Impact of Exposure to the COVID-19 Sanitary Crisis on French Healthcare Workers: Risk Factors and Coping Strategies [Original Research]. Frontiers in Psychiatry, 12. 10.3389/fpsyt.2021.701127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation (WHO). (1946). Charte d'Ottawa. https://www.euro.who.int/fr/publications/policy-documents/ottawa-charter-for-health-promotion,-1986
- Yaghobian, S., Ohannessian, R., Mathieu-Fritz, A., & Moulin, T. (2020). National survey of telemedicine education and training in medical schools in France. J Telemed Telecare, 26(5), 303-308. 10.1177/1357633x18820374 [DOI] [PubMed] [Google Scholar]