Abstract
Background
Improving the quality of care in community settings for people with ‘Complex Emotional Needs’ (CEN—our preferred working term for services for people with a “personality disorder” diagnosis or comparable needs) is recognised internationally as a priority. Plans to improve care should be rooted as far as possible in evidence. We aimed to take stock of the current state of such evidence, and identify significant gaps through a scoping review of published investigations of outcomes of community-based psychosocial interventions designed for CEN.
Methods
We conducted a scoping review with systematic searches. We searched six bibliographic databases, including forward and backward citation searching, and reference searching of relevant systematic reviews. We included studies using quantitative methods to test for effects on any clinical, social, and functioning outcomes from community-based interventions for people with CEN. The final search was conducted in November 2020.
Results
We included 226 papers in all (210 studies). Little relevant literature was published before 2000. Since then, publications per year and sample sizes have gradually increased, but most studies are relatively small, including many pilot or uncontrolled studies. Most studies focus on symptom and self-harm outcomes of various forms of specialist psychotherapy: most result in outcomes better than from inactive controls and similar to other specialist psychotherapies. We found large evidence gaps. Adaptation and testing of therapies for significant groups (e.g. people with comorbid psychosis, bipolar disorder, post-traumatic stress disorder, or substance misuse; older and younger groups; parents) have for the most part only reached a feasibility testing stage. We found little evidence regarding interventions to improve social aspects of people’s lives, peer support, or ways of designing effective services.
Conclusions
Compared with other longer term mental health problems that significantly impair functioning, the evidence base on how to provide high quality care for people with CEN is very limited. There is good evidence that people with CEN can be helped when specialist therapies are available and when they are able to engage with them. However, a much more methodologically robust and substantial literature addressing a much wider range of research questions is urgently needed to optimise treatment and support across this group.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-022-04171-z.
Keywords: Complex emotional needs, Personality disorder, Scoping review
Introduction
People who have received a diagnosis of “personality disorder” are reported to experience a range of difficulties with social functioning, mental and physical health [1, 2]. Substantial economic burdens are associated, especially due to treatment costs and productivity losses [3, 4]. Historically a “personality disorder” diagnosis was seen as indicating a lack of treatability [5]. More recently, there has been greater recognition of the needs for support and the provision of effective treatment for this group, and improving care has been identified as a priority in a variety of countries [6–9].
A heavy burden of stigma is associated with a “personality disorder” diagnosis, with negative views and discriminatory behaviour from some health professionals having especially immediate impacts [10–14]. We are sympathetic to the critique that the therapeutic nihilism and stigma accompanying a “personality disorder” diagnosis, and the lack of progress in delivering care that consistently helps rather than harms, are such that this diagnostic label—also criticised on grounds of validity—is now best left behind. Further work is needed on assessing and describing the difficulties that people who may receive this diagnostic label experience in more useful and acceptable ways: pending this, we prefer the term complex emotional needs (CEN) as a working description of the difficulties experienced by people who may receive a “personality disorder” diagnosis, and therefore use it as our headline description in this paper, as in our other publications on this topic. We are guided especially by members of our research team who have relevant lived experience in making this choice. However, the literature we have reviewed for the most part is based on “personality disorder” diagnoses of various types: thus, below we use this term where it is used in the papers included in our review.
Mental health services and mental health research are widely acknowledged not to have achieved parity in terms of resources and status with physical health care, and services for people with a “personality disorder” diagnosis are doubly disadvantaged as they appear to significantly lag behind services for people with other long-term mental health conditions [6, 15–17]. Recurrently reported difficulties include large variations in accessibility and quality of services, difficulty accessing specialist “personality disorder” services, and lack of therapeutic interventions outside them, a tendency for interventions to focus narrowly on self-harm rather than on the broader range of psychological and social outcomes that service users and carers identify as important, lack of focus on trauma experiences despite these being very frequent, and exclusion from care of people with common comorbidities such as substance misuse or bipolar disorder, or at the younger or older end of the age range [10, 17–20].
Internationally, service user activists, professional bodies and policy makers have advocated for better quality services for people with CEN [15–17]. Ideally, service improvement should be rooted in evidence-based practice [21, 22]. A number of systematic reviews have reported on the trial literature on psychological interventions for people with a “borderline personality disorder” (“BPD”) diagnosis, including Dialectal Behaviour Therapy (DBT), Mentalisation Based Therapy (MBT), Cognitive Behavioural Therapy (CBT), and psychodynamic therapies, amongst others [23–25]. Reviews tend to conclude that these specialist treatments are all more effective than treatment as usual (TAU) in achieving clinical improvements in self-harm and “borderline symptoms”, although no single intervention type has emerged as dominant [26].
However, these relatively narrowly focused systematic reviews have left unanswered a range of questions that are key to improving care holistically for the full spectrum of people who have received a “personality disorder” diagnosis, or have comparable needs [26]. Questions not addressed include how to improve important social outcomes including employment, social inclusion, relationships and parenting, and how to provide care that takes account of very frequent and extensive trauma histories. These previous reviews have also not focused on the needs of important groups, such as older adults and younger people, people with comorbidities such as substance misuse, psychosis or bipolar disorder, and people who may have received “personality disorder” diagnoses other than borderline or emotionally unstable, or who have received multiple diagnoses. The key question of service design, and what kinds of teams and networks of services most effectively meet needs and deliver continuity of care also remains largely unanswered.
Given these crucial gaps in the evidence to underpin improvement of care, our intention in the current scoping paper was to cast the net widely, seeking any quantitative evidence that may have potential as building blocks for future intervention and service design and research in this area. Our aim was to conduct a scoping review of the evidence on the effectiveness of community-based psychological interventions designed for people with CEN. In order to capture a broad range of relevant evidence, we aimed to include in our searches a broad range of diagnoses and related difficulties, interventions focused not only on self-harm and symptoms but also on social targets, and delivered at team and catchment area as well as individual levels. Observational studies can yield helpful evidence on treatment outcomes in naturalistic settings, sometimes providing pointers to interventions worth researching through randomised trials or allowing questions to be addressed, such as about area-level service design, that are difficult to investigate through trials [27]: we thus aimed also to capture evidence from such designs. We further aimed to identify preliminary investigations of feasibility and reports on adaptations of interventions to new populations or new settings, as these have potential to inform further research and intervention development. Thus, by considering this broader evidence base, we aim to take stock of what is known so far, highlight important gaps, and inform future research in this area.
Methods
Study design
We conducted a scoping review [28, 29] to map the evidence from studies using a range of quantitative designs on community-based treatments for CEN and to identify gaps in the literature. We followed guidelines to conducting and reporting scoping reviews [30].
Search strategy
The current review was part of a programme of work commissioned from the National Institute for Health Research Mental Health Policy Research Unit to inform policy on services for CEN. This programme of work included evidence reviews and studies of stakeholder views and experiences, and was supported by a working group that included people with relevant lived experience of using services and clinicians from a range of disciplines and service contexts.
The programme included four individual (systematic) reviews, for which we used a single overall search strategy which was developed in collaboration with the working group of researchers, clinicians, people with relevant lived experience, and an information scientist with experience in mental health. Of the four reviews two synthesised qualitative evidence on service user experience of community mental health care for CEN [10] and clinician perspectives on what constitutes good practice, and what helps or prevents it being achieved, in community mental health services for CEN [20]. The third review evaluated international guidance regarding community service delivery and organisation for CEN [31]. The protocol for the wider programme of work was prospectively registered (CRD42019131834). This review, which constitutes the fourth part of the programme, follows the PRISMA guidelines [32] and the specific protocol for this scoping review was also registered on PROSPERO (CRD42019143165). This protocol originally encompassed a meta-analysis of quantitative data, however, the extent and heterogeneity of important literature led to a decision to conduct such analyses on a more limited subset of data. This will be reported in a separate paper.
We conducted a comprehensive search of MEDLINE (Ovid), Embase (Ovid), HMIC (Ovid), Social Policy and Practice (Ovid), CINAHL (EBSCO), and ASSIA (ProQuest), from database inception to December 2019. Search terms included terms relating to CEN, community/outpatient setting, and psychological or psychosocial treatments. An update search was conducted in November 2020 (PB). The search strategy was supplemented with a reference search of relevant systematic reviews following the original and updated search. Forward and backward citation searches using Web of Science were also performed for all included papers. No limits were placed on the language or country. Details of the search strategy are available in Additional file 1: Appendix 1.
Study selection
All titles and abstracts were independently screened by a team of 12 people. Reliability was ensured by double checking the first 100 articles screened by each person, and a random 10% of all results were double screened by a senior researcher (LSR). Studies not meeting inclusion criteria were excluded. Subsequently, full-text articles were screened according to the specific inclusion criteria for this review by two researchers. Unclear cases and disagreements were resolved through discussion with the wider research team, including clinical members and a senior systematic reviewer.
Selection criteria
Studies were included if they met the following criteria:
Participants: Adults (operationalised as 90% of the sample over 16 years old or mean sample age of 18 or over) in which a majority (> 50%) had received a diagnosis of “personality disorder”. In order not to exclude studies in which authors wished to avoid use of this diagnostic term, or which focused on participants who had not received a formal diagnosis, we also ran searches using search terms intended to capture difficulties comparable to those experienced by people with a “personality disorder” diagnosis, including searches for samples presenting with repeated self-harm or suicide attempts, complex trauma or complex post-traumatic stress disorder (PTSD), and emotional dysregulation or instability. Clinical members in the team were consulted to achieve a consensus on the inclusion of such papers, although the large majority of the included papers focused on participants identified by a “personality disorder” diagnosis.
Interventions: Treatments with a primary focus on “personality disorder” or associated needs (as defined above), including psychotherapeutic treatments and service models, conducted in a community mental health care setting, or delivered to participants living in the community during treatment.
Controls: All comparators were considered (randomised and non-randomised), and we also included before and after study designs with no specific comparator group and studies in which the primary aim was uncontrolled preliminary testing of a new or newly adapted intervention.
Outcomes: Any measure of global clinical or symptom severity; psychiatric hospitalisation or emergency hospital presentations; self-harm or suicide-related outcomes; quality of life or general wellbeing; general, occupational, or social functioning (including interpersonal relations).
Study design: Quantitative studies, including randomised and non-randomised comparison studies and non-controlled studies with pre-post comparisons.
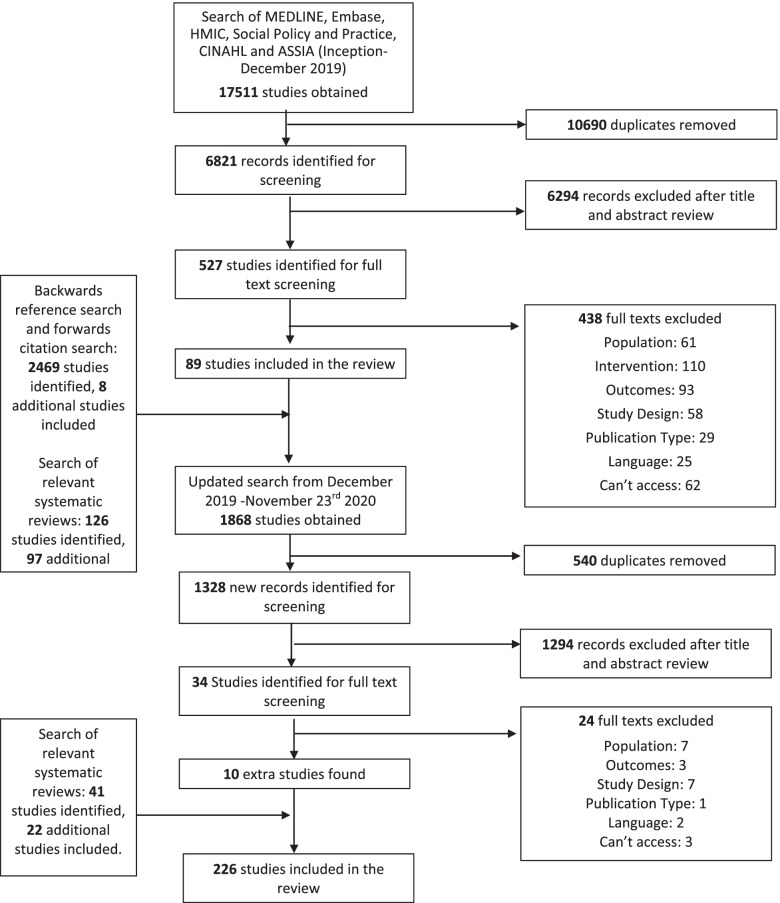
We excluded studies whose primary focus of treatment was not “personality disorder” diagnoses or comparable needs (as defined above), or if the treatment was conducted in forensic, crisis care, or inpatient care settings. We also excluded theses and conference abstracts. Given the very broad nature of our searches, for feasibility we included only studies published in English. The full search and screening process is depicted in Fig. 1.
Fig. 1.
PRISMA Diagram
Data extraction and synthesis
Data was extracted by a team of 21 people using a standardised extraction form and was double checked for accuracy by the lead researchers. Disagreements or errors were resolved by discussion with the team including a senior member and corrected where required. Data extracted included study aims, study design, treatment and comparator details, sample characteristics and size, outcome measures, and study results. To present extracted data, papers were grouped by treatment modality, treatment/comparator category, and study design category. Treatment modality categories were developed through discussion with senior clinicians and researchers (including SP, an international expert in evaluation of psychological treatments), and included: 1) DBT; 2) cognitive and behavioural therapies; 3) MBT; 4) psychodynamic therapy; 5) schema therapy; 6) mixed modality psychotherapy; 7) other individual psychotherapy modalities; 8) social or functional orientated therapy; 9) tests of service models or service re-organisation; 10) self-management or care planning; 11) family, couple, or parenting therapies. Treatment/comparator categories included: 1) non-active or non-specialist comparator; 2) specialist or active comparator; 3) test of a modified version of the intervention; 4) test of a therapy adapted to a particular population. Study designs were categorised as follows: 1) Randomised Controlled Trials (RCTs) (noting where the study is clearly described as a pilot); 2) observational studies, including non-randomised controlled studies, and studies making pre-post comparisons within the same cohort; 3) intervention development studies. We also noted whether or not studies had an identified primary outcome.
In keeping with guidance for scoping reviews, we did not carry out quality appraisal, but have placed a greater emphasis on more robust designs in our reporting [30].
Results
Searches of bibliographic databases returned a total of 17,511 papers of which 10,690 papers were duplicates. After screening 6,821 titles and abstracts, reviewers screened 527 full texts. 438 papers did not meet our inclusion criteria and were excluded, resulting in 88 studies included in the review. Ninety-six additional studies were identified by searching relevant systematic reviews and eight studies through reference and citation searches. The search was updated on 23/11/2020 obtaining 1,868 records. After screening 34 full texts, 10 additional studies were included in the scoping review. Overall, we identified 226 papers for inclusion (Fig. 1), reporting data from 210 distinct trials.
Intervention types
Tables 1,2,3,4 provide summaries of included studies by intervention type, and more detailed summaries are shown in Additional file 1: Appendices 2–5. Additional file 1: Appendices 6–9 present descriptions of individual papers. There have been more studies of DBT (Table 1, Additional file 1: Appendix 2 and 6) than any other therapy modality or community-based treatment in this group (n = 66). We found 49 papers reporting studies of cognitive and behavioural therapies (Table 2, Additional file 1: Appendix 3 and 7), six of schema therapy (Table 2, Additional file 1: Appendix 3 and 7), 54 of psychodynamic therapy (Table 3, Additional file 1: Appendix 4 and 8), 20 of MBT (Table 3, Additional file 1: Appendix 4 and 8), ten of mixed modality psychotherapy (Table 4, Additional file 1: Appendix 5 and 9), seven of other individual psychotherapy modalities (Table 4, Additional file 1: Appendix 5 and 9), five of socially or functionally orientated therapy (Table 4, Additional file 1: Appendix 5 and 9), six of self-management or care planning (Table 4, Additional file 1: Appendix 5 and 9), and 13 tests of novel mental health service models (Table 4, Additional file 1: Appendix 5 and 9). Some studies included more than one intervention type.
Table 1.
DBT
| Study design and number of studies (n) with references | Sample size, date, and country of publication | Cohort diagnoses and demographics | Main findings |
|---|---|---|---|
| DBT vs inactive/non-specialist comparators | |||
| RCT (n = 12) [33–44] |
Sample size: 20–100 (n = 12). Date: 1990–1999 (n = 2); 2000–2009 (n = 4); 2010–2019 (n = 6). Country: Asia (n = 1); Europe (n = 4); North America (n = 4); Oceania (n = 1); UK (n = 2). |
Diagnoses: “BPD” diagnosis (n = 10); “BPD” or “personality disorder” diagnosis and self-harm (n = 2). Demographics: 100% female (n = 5); 50–79% (n = 2) White. |
RCTs with primary outcomes: On the primary outcomes of RCTs, compared to inactive/non-specialist controls, participants receiving DBT showed improvement in self-harm in 2/3 studies that examined self-harm (in 1 study this was only the case for clinician-rated self-harm), symptoms at discharge (1/1), global distress (0/1), hospital admissions (0/1), and “BPD” symptoms (1/1). On non-primary outcomes, compared to controls, participants receiving DBT showed improvement on approximately half of the outcomes. For some of the outcomes, differences were no longer significant at follow-up compared to post-treatment. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 15) [45–59] |
Sample size: < 20 (n = 2); 20–100 (n = 13). Date: 2000–2009 (n = 7); 2010–2019 (n = 8). Country: Europe (n = 5); North America (n = 8); UK (n = 1); Oceania (n = 1). |
Diagnoses: “BPD”, “personality disorder”, or emotionally unstable “personality disorder” diagnosis (n = 11); “BPD” diagnosis and self-harm or a comorbid diagnosis (n = 3); severe impairment and history of suicide attempts or crisis service use (n = 1). Demographics: 100% female (n = 5); 50–79% White (n = 2), 80–99% White (n = 5). |
Non-randomised experiments: In 1 study with two control groups, the DBT group was superior compared to TAU on the primary outcome “BPD” symptoms (1/1). In studies with comparisons over time only, participants improved on the one reported primary outcome and on close to all secondary outcomes. Studies focusing on patients with comorbid severe mental illness, substance dependence, or an extensive history of suicide attempts or crisis service use all showed improvement in above-mentioned outcomes. |
| Uncontrolled intervention development studies and single case study with multiple measures (n = 3) [60–62] |
Sample size: < 20 (n = 1); 20–100 (n = 2). Date: 2000–2009 (n = 1); 2010–2019 (n = 2). Country: North America (n = 3). |
Diagnoses: “Personality disorder” or “BPD” diagnosis (n = 2); severe impairment and history of suicide attempt or crisis service use (n = 1). Demographics: 80–99% White (n = 2); 100% White (n = 1). | Studies with comparisons over time only: In 1 study with a primary outcome, participants with severe impairment and an extensive history of suicide attempts or crisis service use improved on the primary outcome, but this was no longer significant one year later. Across studies, participants also improved on all secondary/other outcomes. |
| Implementation studies (n = 1) [63] |
Sample size: > 100 (n = 1). Date: 2020 – (n = 1). Country: Europe (n = 1). |
Diagnoses: “BPD” or “emotionally unstable personality disorder” diagnosis (n = 1). Demographics: no data reported. |
In 1 study with comparison over time only, participants improved over time on all outcomes (1/1). |
| DBT vs specialist comparators | |||
| RCT (N = 6) [64–69] |
Sample size: 20–100 (n = 3); > 100 (n = 3). Date: 2000–2009 (n = 4); 2010–2019 (n = 2). Country: North America (n = 5); Oceania (n = 1). |
Diagnoses: “BPD” diagnosis (n = 2); “BPD” diagnosis and self-harm (n = 3); “BPD” diagnosis and opiate dependence diagnosis (n = 1). Demographics: 100% female (n = 1); 50–79% White (n = 2), 80–99% White (n = 1). | RCTs with primary outcomes: DBT was not different or inferior to the specialist comparator in 2 RCTs (including a follow-up study) on the primary outcomes (suicidal episodes (0/2)). In 1 RCT, DBT was superior to the specialist comparator on the primary outcome (suicide attempts (1/1)). In 1 RCT no direct comparisons were made between specialist comparators. Across RCTs, compared to controls, DBT did not show improvement on non-primary outcomes, except for service use (1/1). |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 2) [70, 71] |
Sample size: 20–100 (n = 2). Date: 2010–2019 (n = 2). Country: Europe (n = 1), UK (n = 1). |
Diagnoses: “BPD” diagnosis (n = 2). Demographics: 50–79% White (n = 1). | Non-randomised experiments without primary outcomes: Participants in the DBT group showed no improvement compared to controls in the MBT group on any outcome. Participants in the combined DBT group showed no improvement compared to controls in the individual DBT group on outcomes. |
| Studies of partial/modified DBT | |||
| RCT (n = 6 including 1 pilot) [72–77] |
Sample size: 20–100 (n = 6). Date: 2000–2009 (n = 1); 2010–2019 (n = 5). Country: Asia (n = 1); Europe (n = 3); North America (n = 2). |
Diagnoses: “BPD” diagnosis (n = 4); “BPD” diagnosis and self-harm (n = 2). Demographics: 100% female (n = 6); 50–79% White (n = 2); 100% White (n = 2). |
RCTs without primary outcomes: In 3 RCTs, there was no difference between the adapted versions of DBT on all or most outcomes. In 3 other RCTs, compared to controls, participations receiving (adapted) DBT showed improvements on all or most outcomes. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 10) [78–87] |
Sample size: < 20 (n = 2); 20–100 (n = 6); > 100 (n = 2). Date: 2000–2009 (n = 4); 2010–2019 (n = 2); 2020 – (n = 4). Country: Europe (n = 2); North America (n = 3); Oceania (n = 3); Republic of Ireland and Northern Ireland (n = 1); UK (n = 1). |
Diagnoses: “BPD” diagnosis and/or experiencing emotional dysregulation (n = 8); self-harm (n = 1); “BPD” and self-harm (n = 1) Demographics: 100% female (n = 2); 80–99% White (n = 1). | In 1 non-randomised experiment, compared to standard DBT, participants in the DBT skills training group showed no improvement in “BPD” symptoms, symptom severity, and suicidality (0/1). In studies with comparison over time only, participants improved on the primary outcome service use (1/1) and most secondary outcomes. |
| Uncontrolled intervention development studies and single case study with multiple measures (n = 3) [88–90] |
Sample size: < 20 (n = 2); 20–100 (n = 1). Date: 2000–2009 (n = 1); 2010–2019 (n = 2). Country: Europe (n = 1); Oceania (n = 2). |
Diagnoses: “BPD” or cluster B diagnosis (n = 3). Demographics: no data reported. |
In 3 studies with comparisons over time only, participants improved on all secondary/other outcomes, except of anxiety symptoms (0/1). |
| Studies of adapted DBT | |||
| RCT (n = 3 including 1 pilot) [91–93] |
Sample size: 20–100 (n = 2); > 100 (n = 1). Date: 2010–2019 (n = 2); 2020- (n = 1). Country: Asia (n = 1); Europe (n = 1); North America (n = 1). |
Diagnoses: “BPD” diagnosis (n = 1); “BPD” diagnosis/criteria and PTSD diagnosis (n = 2). Demographics: 100% female (n = 2); 80–99% White (n = 1); 100% male, 18–50-year-olds and married (n = 1). |
RCTs with primary outcomes: In 1 RCT, compared to Cognitive Processing Therapy (CPT), participants with comorbid PTSD receiving DBT-PTSD showed improvement on primary outcomes (diagnostic and symptom remission of PTSD: 1/1) and secondary outcomes. In 1 RCT focusing on married men, compared to waitlist controls, participants receiving Couple-DBT showed improvement in all outcomes. One RCT did not report significance results. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 3) [94–96] |
Sample size: 20–100 (n = 2); > 100 (n = 1). Date: 2010–2019 (n = 3). Country: Europe (n = 2); Oceania (n = 1). |
Diagnoses: “BPD” diagnosis (n = 2); “BPD” and eating disorder diagnosis (n = 1). Demographics: 100% female (n = 2); only 18–25-year-olds (n = 1); only primary caregivers of child younger than 3-years-old (n = 1). |
Non-randomised experiments: In 1 study, compared to CBT, participants with a comorbid eating disorder receiving DBT showed improvement on some primary outcomes and most secondary outcomes. In 1 study, compared to the general DBT group, participants in the young adult only DBT group showed improvement in non-primary symptom outcomes. In 1 study with comparisons over time only, participants, i.e. caregivers of young children, improved on all outcomes. |
| Uncontrolled intervention development studies and single case study with multiple measures (n = 2) [97, 98] |
Sample size: < 20 (n = 1); 20–100 (n = 1). Date: 2010–2019 (n = 2). Country: Europe (n = 2). |
Diagnoses: “BPD” diagnosis or criteria (n = 2). Demographics: 100% female (n = 2); only 18–25-year-olds (n = 1). |
In studies with comparisons over time only, participants improved over time on all outcomes. |
Table 2.
Cognitive and behavioural and schema therapies
| Study design and number of studies (n) with references | Sample size, date, and country of publication | Cohort diagnoses and demographics | Main findings |
|---|---|---|---|
| Cognitive and behavioural treatment vs inactive/non-specialist comparators | |||
| RCT (n = 18 including 4 pilot) [99–116] |
Sample size: 20–100 (n = 12); > 100 (n = 6). Date: 1990–1999 (n = 2); 2000–2009 (n = 7); 2010–2019 (n = 9). Country: Europe (n = 4); North America (n = 6); Oceania (n = 1); UK (n = 7). |
Diagnoses: “BPD” or other “personality disorder” diagnoses/criteria (n = 13); mixed clinical diagnoses including “personality disorder” diagnosis (n = 1); “BPD” diagnosis/criteria and recent or previous (repeated) self-harm (n = 3); recent and previous self-harm (n = 1). Demographics: 100% female (n = 4); 0–49% White (n = 1), 80–99% White (n = 5); 100% White (n = 5). | RCTs with primary outcomes: On the primary outcomes of RCTs, compared to controls, a greater proportion of participants receiving cognitive and behavioural therapies recovered on symptoms (1/1) and also showed improvement in “personality disorder” symptoms (3/3), symptom severity (1/2), and social functioning (1/2), but not depressive (0/1) or (social) anxiety symptoms (0/1), service use (0/1), or frequency/number of participants with self-harming/suicidal behaviour (0/4). On non-primary outcomes, compared to controls, participants receiving cognitive and behavioural therapies showed improvement in approximately half of the outcomes. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 8) [117–124] |
Sample size: < 20 (n = 1); 20–100 (n = 7). Date: 1990–1999 (n = 1); 2000–2009 (n = 2); 2010–2019 (n = 5). Country: Europe (n = 2); North America (n = 3); UK (n = 3). |
Diagnoses: “BPD” (n = 3) or avoidant “personality disorder” diagnosis (n = 1); “BPD” diagnosis/criteria, mood disorder, history of self-harm, with our without emotional and behavioural dysregulation (n = 3); childhood sexual abuse (n = 1). Demographics: 100% female (n = 1); 50–79% White (n = 1); 80–99% White (n = 1). |
In studies with comparisons over time only, participants improved on the one reported primary outcome (self-harm: 1/1) and most secondary outcomes. |
| Uncontrolled intervention development studies and single case study with multiple measures (n = 11) [125–135] |
Sample size: < 20 (n = 8); 20–100 (n = 3). Date: 2000–2009 (n = 2); 2010–2019 (n = 9). Country: Asia (n = 2); Europe (n = 3); North America (n = 1); Oceania (n = 1); UK (n = 4). |
Diagnoses: “BPD” (n = 4) or other “personality disorder” diagnoses (n = 4); “BPD” diagnosis/features and comorbid mood disorder (n = 2) or drug/alcohol disorder (n = 1). Demographics: 80–99% White (n = 1); 100% White (n = 1); older age (n = 1). |
In studies with comparisons over time only, participants improved over time on the primary outcomes symptoms/distress (2/2) and quality of life (1/1), and also showed no dropouts (1/1). Participants improved on secondary outcomes. Patients with a current substance misuse disorder showed a reduction in drug use (1/1). Elderly patients with a chronic mood or adjustment disorder improved in symptom distress (1/1) and some but not all aspects of schema and coping variables (1/1). |
| Cognitive and behavioural treatment vs specialist comparators | |||
| RCT (n = 4) [136–139] |
Sample size: 20–100 (n = 4). Date: 2000–2009 (n = 3), 2010–2019 (n = 1). Country: Europe (n = 3); Europe and North America (n = 1). |
Diagnoses: “BPD” features/diagnosis (n = 2) or other “personality disorder” diagnosis (n = 2) Demographics: 100% White (n = 1). |
RCTs with primary outcomes: In 3 RCTs comparing cognitive and behavioural therapy with specialist comparators, there were no between-group differences on primary outcomes (symptom improvement: 0/1; symptoms severity: 0/1; interpersonal problems: 0/1) or secondary outcomes. In 1 RCT, significantly more participants receiving Schema Focused Therapy (SFT) recovered on the primary outcome (“BPD” symptoms: 1/1) as well as on three secondary outcomes compared to cognitive therapy. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 3) [140–142] |
Sample size: 20–100 (n = 1); > 100 (n = 2). Date: 2000–2009 (n = 1); 2010–2019 (n = 2). Country: Europe (n = 3). |
Diagnoses: “Personality disorder” diagnosis (n = 2); cluster B “personality disorder” diagnosis with comorbid Axis I disorder (n = 1). Demographics: no data report. |
In 3 non-randomised experiments, there were no differences between the cognitive behavioural treatment and specialist comparators on primary outcomes (personality functioning: 0/1; symptom severity: 0/1) and all or most secondary outcomes (0/3). |
| Uncontrolled intervention development studies and single case study with multiple measures (n = 1) [143] |
Sample size: < 20 (n = 1). Date: 2010–2019 (n = 1). Country: North America (n = 1). |
Diagnoses: NSSI disorder (n = 1). Demographics: 50–79% White (n = 1). | One study with comparisons over time only did not report significant results for outcomes on patients with NSSI disorder. However, 8/10 participants reported meaningful reductions in self-harming behaviour. |
| Studies of modified cognitive and behavioural treatments | |||
| RCT (n = 2 including 1 pilot) [144, 145] |
Sample size: < 20 (n = 1); 20–100 (n = 1). Date: 1990–1999 (n = 1); 2010–2019 (n = 1). Country: North America (n = 1); UK (n = 1). |
Diagnoses: “BPD” diagnosis (n = 1); previous suicide attempts, antidepressants taken as part of an overdose, and suicidal behaviour (n = 1). Demographics: 80–99% White (n = 1). |
RCTs with primary outcomes: On the primary outcome of 1 RCT, findings for differences between the cognitive Behavioural Problem Solving and TAU group on suicidality were mixed (0/1). Findings were mixed or showed no between-group differences for non-primary outcomes (0/2). |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 1) [146] |
Sample size: 20–100 (n = 1). Date: 2000–2009 (n = 1). Country: Europe (n = 1). |
Diagnoses: “Personality disorder” diagnosis, excluding borderline, schizotypal, schizoid, antisocial, or NOS “personality disorder” diagnoses (n = 1). Demographics: no data reported. | The 1 study utilised a crossover design and showed significant improvements over the treatment period as a whole, but no between-group differences. |
| Studies of adapted cognitive and behavioural treatments | |||
| Uncontrolled intervention development studies and single case study with multiple measures (n = 1) [147] |
Sample size: < 20 (n = 1). Date: 2010–2019 (n = 1). Country: Oceania (n = 1). |
Diagnoses: “Personality disorder” diagnosis (n = 1). Demographics: no data reported. |
In 1 study with comparisons over time only, no statistical analysis was conducted. However, 5/8 patients no longer met criteria for an avoidant “personality disorder” at end of follow-up. |
| Schema therapy vs inactive/non-specialist comparators | |||
| RCT (n = 1) [148] |
Sample size: > 100 (n = 1). Date: 2010–2019 (n = 1). Country: Europe (n = 1). |
Diagnoses: Avoidant, dependent, obsessive–compulsive, paranoid, histrionic, or narcissistic “personality disorder” diagnosis (n = 1). Demographics: no data reported. |
On the primary outcome of the 1 RCT, compared to controls, a greater proportion of participants receiving schema therapy recovered (1/1). Compared to controls, participants also improved on some non-primary outcomes. |
| Uncontrolled intervention development studies and single case study with multiple measures (n = 4) [149–152] |
Sample size: < 20 (n = 4). Date: 2000–2009 (n = 1); 2010–2019 (n = 3). Country: Europe (n = 3); North America (n = 1). |
Diagnoses: “BPD” (n = 3) or other “personality disorder” diagnosis (n = 1). Demographics: 100% female (n = 3); old age (n = 1). |
In the 1 study that reported significant results with comparisons over time only, participants improved on “BPD” symptoms (1/1) and most other outcomes. |
| Studies of modified schema therapy | |||
| RCT (n = 1) [153] |
Sample size: 20–100 (n = 1). Date: 2000–2009 (n = 1). Country: Europe (n = 1). |
Diagnoses: “BPD” diagnosis (n = 1). Demographics: 80–99% (n = 1). | RCTs with primary outcomes: On the primary outcome of 1 RCT, there was no difference between participants receiving schema therapy with and those without phone support on recovery from “BPD” (0/1). There was also no significant difference on non-primary outcomes (0/1). |
Table 3.
Psychodynamic and MBT studies
| Study design and number of studies (N) with references | Sample size, date, and country of publication | Cohort diagnoses and demographics | Main findings |
|---|---|---|---|
| MBT vs inactive/non-specialist comparators | |||
| RCT (n = 4) [43, 154–156] |
Sample size: 20–100 (n = 4). Date: 1990–1999 (n = 1); 2000–2009 (n = 2); 2010–2019 (n = 1). Country: Asia (n = 1); UK (n = 3). |
Diagnoses: “BPD” diagnosis (n = 4). Demographics: no data reported. | RCTs with primary outcomes: In the primary outcomes of 2 RCTs, compared to controls, participants receiving MBT showed improvement in the proportion of patients making suicide attempts (1/1) and in “BPD” symptoms (1/1). Compared to controls, participants receiving MBT showed improvement in all non-primary outcomes. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 6) [157–162] |
Sample size: < 20 (n = 2); 20–100 (n = 3); > 100 (n = 1). Date: 2010–2019 (n = 6). Country: Europe (n = 6). |
Diagnoses: “BPD” (n = 4) or other “personality disorder” diagnosis (n = 1); “personality disorder” diagnosis and poor functioning (n = 1). Demographics: 100% female (n = 1). |
In 1 non-randomised experiments, compared to controls, participants improved on some non-primary outcomes. In studies with comparisons over time only, participants showed improvements on all primary and non-primary outcomes. |
| MBT vs specialist comparators | |||
| RCT (n = 4) [163–166] |
Sample size: 20–100 (n = 1); > 100 (n = 3). Date: 2000–2009 (n = 1); 2010–2019 (n = 3). Country: Europe (n = 3); UK (n = 1). |
Diagnoses: “BPD” diagnosis (n = 3); “BPD” and suicide attempt or life-threatening self-harm (n = 1). Demographics: 50–79% White (n = 1). | RCTs with primary outcomes: In the primary outcomes of RCTs, compared to specialist controls, participants receiving MBT showed improvement in suicidal behaviours (1/1) and number of hospitalisations (1/1), but not in “borderline symptoms” (0/1). Compared to specialist comparators, participants receiving MBT did not show improvements in most non-primary outcomes. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 5) [70, 167–170] |
Sample size: 20–100 (n = 4); > 100 (n = 1). Date: 2010–2019 (n = 5). Country: Europe (n = 1), UK (n = 4). |
Diagnoses: “BPD” (n = 2) or “personality disorder” diagnosis (n = 3). Demographics: 50–79% White (n = 1); 80–99% White (n = 3). |
In non-randomised studies, compared to an alternative psychoanalytic model, the MBT group did not significantly improve on the primary outcome of bed use (0/1). Compared to specialist treatments, participants receiving MBT did not show improvements in more than half of non-primary outcomes. In 2 studies with comparisons over time only, participants improved on less than half of the outcomes. |
| Studies of modified MBT | |||
| RCT (n = 1) [171] |
Sample size: > 100 (n = 1). Date: 2020- (n = 1). Country: Europe (n = 1). |
Diagnoses: “Personality disorder” diagnosis (n = 1). Demographics: no data reported. |
RCTs with primary outcomes: Compared to lower intensity outpatient MBT, higher intensity day hospital MBT showed no difference in the primary outcome of symptom severity and non-primary outcomes. |
| Psychodynamic treatment vs inactive/non-specialist comparators | |||
| RCT (n = 6) [109, 172–176] |
Sample size: 20–100 (n = 4); > 100 (n = 2). Date: 1990–1999 (n = 2); 2000–2009 (n = 3); 2010–2019 (n = 1). Country: Europe (n = 3); North America (n = 3). |
Diagnoses: “BPD” (n = 1) or other “personality disorder” diagnosis (n = 4); long term psychiatric difficulties disrupting functioning (n = 1). Demographics: no data reported. |
RCTs with primary outcomes: In the primary outcomes of RCTs, compared to controls, participants receiving psychodynamic therapy showed improvement in symptom severity (2/2), social functioning (1/2), and interpersonal functioning (1/1), but not dysfunctional “borderline beliefs” (0/1), anxiety symptoms (0/1), or the number of participants meeting diagnostic criteria for a “personality disorder” diagnosis (0/1). Compared to controls, participants receiving psychodynamic therapy improved on most non-primary outcomes. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 26) [48, 177–201] |
Sample size: < 20 (n = 1); 20–100 (n = 18); > 100 (n = 7). Date: 1990–1999 (n = 6); 2000–2009 (n = 12); 2010–2019 (n = 7); 2020- (n = 1). Country: Australia (n = 7); Europe (n = 10); North America (n = 6); UK (n = 3). |
Diagnoses: “Personality disorder” (n = 11) or “BPD” diagnosis/criteria (n = 8); “personality disorder” diagnosis and comorbid Axis I mental health problems (n = 3); treatment resistant depression with comorbid “personality disorder” and childhood trauma (n = 1); “personality disorder” diagnosis and poor interpersonal functioning (n = 2); poor interpersonal functioning (n = 1). Demographics: 100% female (n = 1); 80–99% White (n = 3); 100% White (n = 1). |
In non-randomised experiments, participants showed improvements compared to controls on the following primary measures: reflective functioning (2/2), “personality disorder” symptoms (1/1), social functioning (1/1), and depressive symptoms (1/1). Compared to controls, participants improved on almost all non-primary outcomes. In studies with comparisons over time only, participants improved in all primary outcomes in interpersonal functioning (3/3) and symptom severity (1/1) and close to all non-primary outcomes. |
| Uncontrolled intervention development studies and single case study with multiple measures (n = 1) [202] |
Sample size: 20–100 (n = 1). Date: 2000–2009 (n = 1). Country: North America (n = 1). |
Diagnoses: “BPD” symptoms and suicidal or self-injurious behaviour (n = 1). Demographics: 100% female (n = 1); > 50% White (n = 1). |
Studies with comparisons over time only: One uncontrolled feasibility trial found that patients given psychodynamic therapy improved over time on outcomes (1/1). |
| Psychodynamic treatment vs specialist comparators | |||
| RCT (n = 8) [67, 138, 139, 203–207] |
Sample size: 20–100 (n = 8) Date: 1990–1999 (n = 1); 2000–2009 (n = 2); 2010–2019 (n = 5). Country: Europe (n = 5); Europe and North America (n = 1); North America (n = 2). |
Diagnoses: “BPD” (n = 5) or other “personality disorder” diagnosis (n = 3). Demographics: 50–79% White (n = 1); 80–99% White (n = 2); 100% White (n = 1). |
RCTs with primary outcomes: In primary outcomes of RCTs, compared to cognitive therapy, participants receiving psychodynamic therapy did not significantly improve in symptom severity (0/1). In 1/3 RCTs, compared to General Psychiatric Management, participants receiving psychodynamic therapy made significantly more overall progress in therapy overall. Compared to specialist controls, participants receiving psychodynamic therapy did not show improvements on almost any non-primary outcomes. One RCT did not make direct comparisons between groups. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 4) [208–211] |
Sample size: 20–100 (n = 3); > 100 (n = 1). Date: 1990–1999 (n = 1); 2010–2019 (n = 3). Country: Europe (n = 3); North America (n = 1). |
Diagnoses: “BPD” (n = 2) or other “personality disorder” diagnosis (n = 1); “personality disorder” diagnosis with or without comorbid substance misuse (n = 1). Demographics: no data reported. |
In 1 non-randomised experiment, compared to DBT, participants given Dynamic Deconstructive Psychotherapy had significantly greater improvement in the primary outcome of symptom severity (1/1). Compared to controls, participants improved on all or most non-primary outcomes. In 1 study with comparisons over time only, patients with and without comorbid substance misuse improved on outcomes. |
| Comparisons of psychodynamic treatment settings | |||
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 6) [141, 212–216] |
Sample size: > 100 (n = 6). Date: 2000–2009 (n = 2); 2010–2019 (n = 4). Country: Europe (n = 3), UK (n = 2); Europe and UK (n = 1). |
Diagnoses: “Personality disorder” diagnosis (n = 5); severe “personality disorder” diagnosis (n = 1). Demographics: no data reported. | Six non-randomised experiments compared psychodynamic treatment in varying contexts. There were no significant differences between day hospital, outpatient, and inpatient services on the primary outcome (symptom severity) or non-primary outcomes. Community or step-down services resulted in significantly improved non-primary outcomes compared to residential services. |
| Studies of adapted psychodynamic treatment | |||
| RCT (n = 2) [217, 218] |
Sample size: 20–100 (n = 2). Date: 2000–2009 (n = 1); 2010–2019 (n = 1). Country: North America (n = 2). |
Diagnoses: “BPD” diagnosis and alcohol use or substance dependence (n = 2). Demographics: no data reported. |
RCTs with primary outcomes: In the primary outcomes of RCTs, comparing Dynamic Deconstructive Psychotherapy combined with alcohol rehabilitation to TAU with alcohol rehabilitation for patients with co-occurring substance use disorders, Dynamic Deconstructive Psychotherapy patients showed significantly greater clinically meaningful improvement (1/1) and improved in alcohol misuse (1/1) and use of institutional care (1/1). Participants receiving Dynamic Deconstructive Psychotherapy showed significant improvements in more than half of non-primary outcomes compared to TAU. |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 1) [219] |
Sample size: 20–100 (n = 1). Date: 2011–2019 (n = 1). Country: Europe (n = 1). |
Diagnoses: “BPD” diagnosis (n = 1). Demographics: relatively low socio-economic status (n = 1). |
In 1 non-randomised experiment, a brief psychoeducational program based on General Psychiatric Management was more effective than generic outpatient treatment (1/1). |
Table 4.
Other studies
| Study design and number of studies (N) with references | Sample size, date, and country of publication | Cohort diagnoses and demographics | Main findings |
|---|---|---|---|
| Mixed therapeutic modalities vs inactive/non-specialist comparators | |||
| RCT (n = 3) [220–222] |
Sample size: 20–100 (n = 2); > 100 (n = 1) Date: 2010–2019 (n = 3) Country: Europe (n = 3) |
Diagnoses: “BPD” diagnosis (n = 3). Demographics: 100% female (n = 1) | RCTs with primary outcomes: On the primary outcomes of RCTs, compared to controls, fewer participants in the intervention group dropped out (1/1) and attempted suicide (1/1), but there was no between-group difference in “BPD” symptoms (0/1). Compared to controls, participants in the intervention group showed greater improvement in most non-primary outcomes |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 6) [223–228] |
Sample size: 20–100 (n = 3); > 100 (n = 3) Date: 1990–1999 (n = 1); 2000–2009 (n = 3); 2010–2019 (n = 2) Country: Europe (n = 5); North America (n = 1) |
Diagnoses: “BPD” (n = 1) or other “personality disorder” diagnosis (n = 4); “personality disorder” diagnosis with self-harm, suicidal, or impulsive behaviour (n = 1). Demographics: not reported | In studies with comparisons over time only, participants improved on following primary outcomes: “BPD” symptoms (1/1), symptom distress, interpersonal relations and social functioning (1/1), and service use (1/1), as well as non-primary outcomes |
| Mixed therapeutic modalities vs specialist comparators | |||
| RCT (n = 1) [229] |
Sample size: > 100 (n = 1) Date: 2010–2019 (n = 1) Country: Europe (n = 1) |
Diagnoses: “Personality disorder” diagnosis (n = 1). Demographics: not reported | RCTs with primary outcomes: In the 1 RCT, cost-effectiveness did not differ between the step-down treatment and outpatient control group (0/1) |
| Other individual therapy vs inactive/non-specialist comparators | |||
| RCT (n = 5 including 1 pilot. 1 also reported in specialist comparators) [175, 230–233] |
Sample size: 20–100 (n = 4); > 100 (n = 1) Date: 1990–1999 (n = 1); 2000–2009 (n = 1); 2010–2019 (n = 3) Country: Europe (n = 3); North America (n = 2) |
Diagnoses: “BPD” (n = 1) or other “personality disorder” diagnosis (n = 3); “BPD” diagnosis and major depressive disorder (n = 1) Demographics: 100% female (n = 2); 50–79% White (n = 1) |
RCTs with primary outcomes: In 1 RCT, compared to TAU, participants with “BPD” and major depressive disorder receiving Abandonment psychotherapy improved on the primary outcomes (suicidal relapse: 1/1; hospitalisation: 1/1) and non-primary outcomes. In 1 RCT, there was no difference between the immediate and delayed psychoeducation group on the primary outcome (“BPD” severity: 0/1). In 1 RCT, compared to Group Psychotherapy, participants receiving Body-Awareness Group Therapy showed improvement in all non-primary outcomes. In 1 RCT, compared to waitlist controls, participants receiving Brief Adaptive Psychotherapy and Psychodynamic Psychotherapy showed improvement in all non-primary outcomes |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 1) [234] |
Sample size: 20–100 (n = 1). Date: 2010–2019 (n = 1) Country: North America (n = 1) |
Diagnoses: Adverse childhood experiences (n = 1) Demographics: 50–79% White (n = 1) |
In 1 study with comparisons over time only, participants with adverse childhood experiences improved on all outcomes |
| Other individual therapy vs specialist comparators | |||
| RCT (n = 2 including 1 also reported in non-specialist) [67, 231] |
Sample size: 20–100 (n = 1); > 100 (n = 1) Date: 2000–2009 (n = 1); 2010–2019 (n = 1) Country: Europe (n = 1); North America (n = 1) |
Diagnoses: “BPD” diagnosis (n = 1); “BPD” diagnosis and major depressive disorder (n = 1). Demographics: 50–79% White (n = 1) | RCTs with primary outcomes: In 1 RCT focusing on patients with major depressive disorder and “BPD”, there was no difference between Abandonment psychotherapy and TAU on the primary outcome (suicidal relapse: 0/1) and non-primary outcomes. Though no direct contrasts were made, in one RCT of DBT, supportive treatment, and psychodynamic therapy, participants receiving supportive treatment improved on some non-primary outcomes |
| Social-interpersonal and functional therapies vs non-specialist/inactive comparators | |||
| RCT (n = 3) [235–237] |
Sample size: 20–100 (n = 1); > 100 (n = 2) Date: 1990–1999 (n = 1); 2000–2009 (n = 1); 2010–2019 (n = 1) Country: Europe (n = 1); North America (n = 1); UK (n = 1) |
Diagnoses: “Personality disorder” (n = 1) or “BPD” diagnosis (n = 2) Demographics: not reported |
RCTs with primary outcomes: On the primary outcomes of RCTs, compared to controls, participants in the intervention group showed improvement in social functioning (1/1) and social problem-solving skills (1/1), but not general functioning (0/1). Compared to controls, participants in the intervention group showed greater improvement on half of the non-primary outcomes |
| Social-interpersonal and functional therapies vs specialist comparators | |||
| RCT (n = 2 including 1 pilot) [238, 239] |
Sample size: 20–100 (n = 2) Date: 1990–1999 (n = 1); 2020- (n = 1) Country: North America (n = 1); UK (n = 1) |
Diagnoses: Avoidant “personality disorder” diagnosis (n = 1); at least 3 episodes of self-harm in the past 3 months (n = 1) Demographics: not reported |
RCTs with primary outcomes: On the primary and secondary outcomes of RCTs, there were no significant differences between skills training in vivo and skills training in the clinic as well as between Functional Imagery Training (FIT) and delayed FIT across outcomes (0/2) |
| Self-management and care planning vs self-management | |||
| RCT (n = 2) [240, 241] |
Sample size: 20–100 (n = 2) Date: 2010–2019 (n = 2) Country: Europe (n = 1); UK (n = 1) |
Diagnoses: “BPD” diagnosis and past self-harm (n = 1); “personality disorder” diagnosis (n = 1). Demographics: 50–79% White (n = 1); 100% White (n = 1) | RCTs with primary outcomes: On the primary outcomes of 1 RCT, the Joint Crisis Plan and TAU group did not differ in the frequency or proportion of participants who self-harm (0/1). In non-primary outcomes, compared to TAU, participants receiving Joint Crisis planning did not differ in outcomes. Compared to Structured Goal-Focused Pre-Treatment Intervention (GFPTI), participants receiving therapeutic assessment showed improvements in more than half of non-primary outcomes |
| Self-management and care planning vs established generic or specialist mental health services | |||
| RCT (n = 1) [242] |
Sample size: 20–100 (n = 1) Date: 2000–2010 (n = 1) Country: UK (n = 1) |
Diagnoses: Severe mental illness and comorbid personality disorder or difficulty (n = 1) | In 1 RCT with primary outcomes, there were no differences between Nidotherapy enhanced assertive outreach and standard assertive outreach in primary outcomes (number of admissions: 0/1; duration of bed use: 0/1) or non-primary outcomes |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 3) [243–245] |
Sample size: 20–100 (n = 2); > 100 (n = 1) Date: 2010–2019 (n = 3) Country: Europe (n = 1); North America (n = 1); UK (n = 1) |
Diagnoses: “Personality disorder” diagnosis (n = 2); major depressive disorder with or without a “personality disorder” diagnosis (n = 1) Demographics: not reported |
Non-randomised experiments: In 1 study, compared to TAU, participants receiving collaborative care management showed improvement on the primary outcome (remission of depression: 1/1). In 1 study, compared to TAU, participants in the Collaborative Care Programme (CCP) improved on one of two non-primary outcomes In 1 study with comparisons over time, participants improved on outcomes |
| Novel mental health service model vs day hospital | |||
| RCT (n = 5) [246–250] |
Sample size: 20–100 (n = 1); > 100 (n = 4) Date: 2000–2009 (n = 1); 2010–2019 (n = 4) Country: Europe (n = 5) |
Diagnoses: “Personality disorder” (n = 4) or “BPD” diagnosis (n = 1) Demographics: not reported |
RCTs with primary outcomes: Four RCTs reported results for the same sample at different time points. Compared to outpatient controls, participants in the step-down day hospital group showed no difference in non-primary outcomes at 18 months. On primary outcomes, compared to outpatient controls, participants in the step-down group showed less improvement in functioning (0/1) at 37 months. There were not between-group differences in social and occupational functioning (0/2), interpersonal problems (0/2), depressive symptoms (0/2), symptom severity (0/2), and quality of life (0/2) at 37 months and 6 years as well as functioning (0/1) at 6 years. There were no between-group differences in non-primary outcomes at 37 months and 6 years. In 1 RCT only including patients with a “BPD” diagnosis, compared to outpatient controls, participants in the step-down intervention group showed greater improvement in half of the non-primary outcomes at 6 years |
| Novel mental health service model vs established generic or specialist mental health services | |||
| RCT (n = 2) [251, 252] |
Sample size: > 100 (n = 2) Date: 2010–2019 (n = 2) Country: Oceania (n = 1); UK (n = 1) |
Diagnoses: “BPD” (n = 1) or “personality disorder” diagnosis (n = 1) Demographics: not reported |
RCTs with primary outcomes: On the primary outcomes of 1 RCT, compared to TAU, participants receiving stepped care psychological therapy showed improvement in bed days (1/1) and A&E attendance (1/1). In 1 RCT, compared TAU, participants in the democratic therapeutic community group did not differ in hospital admission (0/1), but showed greater improvement in some non-primary outcomes |
| Non-randomised experiments, observational studies, quasi experiment, and natural experiment with pre-post comparison (n = 5) [253–257] |
Sample size: 20–100 (n = 2); > 100 (n = 3) Date: 2010–2019 (n = 5) Country: North America (n = 1); Oceania (n = 1); UK (n = 3) |
Diagnoses: “Personality disorder” (n = 4) or “BPD” diagnosis (n = 1). Demographics: 50–79% White (n = 1) | In studies with comparisons over time only, participants improved on most outcomes |
| Uncontrolled intervention development studies and single case study with (n = 1) [258] |
Sample size: < 20 (n = 1) Date: 2010–2019 (n = 1) Country: UK (n = 1) |
Diagnoses: “Personality disorder” diagnosis (n = 1). Demographics: older adults, + 65 (n = 1) | In 1 intervention study with comparisons over time only, there was some evidence for improvement on outcomes, but no statistical analysis was conducted (1/1) |
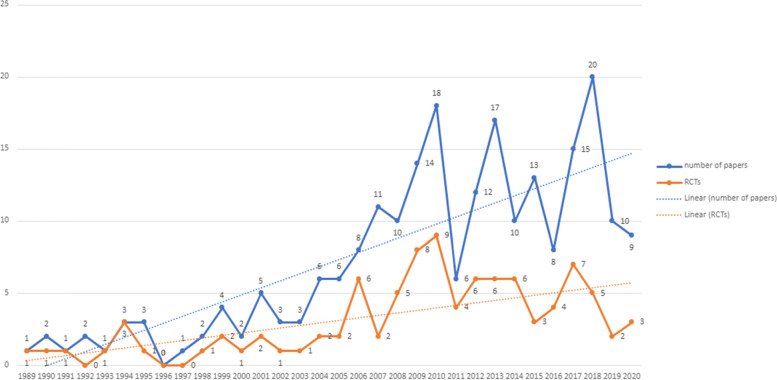
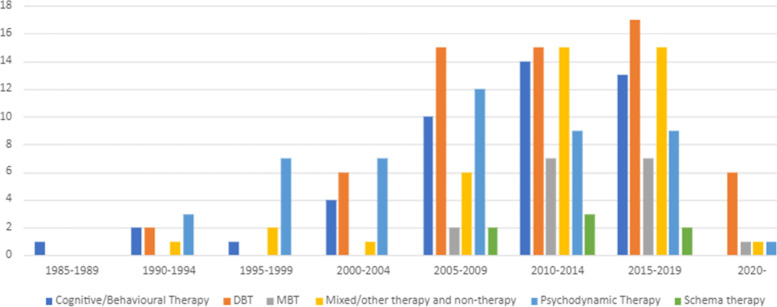
Included papers were published between 1989 and 2020. As shown in Fig. 2, there has been a progressive increase in papers over this time, with both the number of RCTs and other study designs increasing from a very small number per year in the 1990s, to 10–20 per year from 2010 onwards. However, the dearth of studies of any type prior to 2000 and the slow rate of increase in numbers of RCTs examining interventions for CEN are notable. As shown by Fig. 3, studies testing psychodynamic therapy were the most frequent until 2005, with studies of cognitive and behavioural therapies and DBT becoming the most prevalent in the last 15 years. There has also been an increase in the number of studies evaluating mixed therapeutic approaches over time. However, the number of studies exploring service models has remained very low (n = 13; 2010 to 2019) (see Table 4).
Fig. 2.
Number of Papers by Year
Fig. 3.
Number of Papers by Treatment Type and by Year
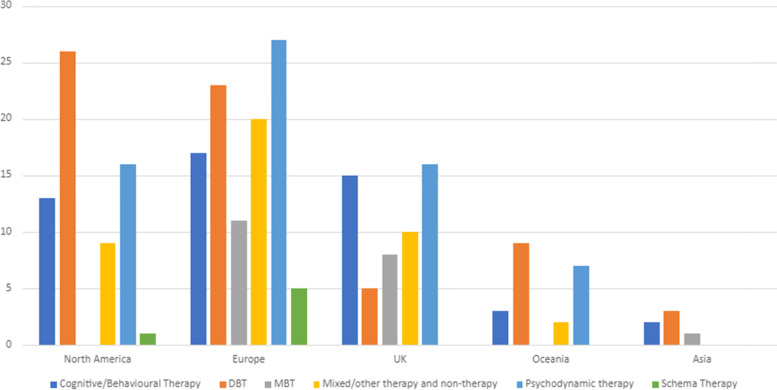
Locations of interventions
Studies were conducted in a range of countries across Asia (n = 6), Europe (European countries other than the UK) (n = 98), North America (n = 60), Oceania (n = 21), and the UK (n = 43) (Fig. 4). Two studies were conducted in more than one continent. DBT studies made up around half of all studies conducted in North America (n = 26) and Oceania (n = 9), but a much smaller proportion in Europe (n = 22), the UK (n = 5), and Asia (n = 3). Cognitive and behavioural and schema therapy studies made up around a third or more of studies in Asia (n = 2) and the UK (n = 15), but a lower proportion in Europe (n = 22), North America (n = 14), and Oceania (n = 3). Psychodynamic and MBT therapies also made up a third or more of studies in the UK (n = 14) as well as in Oceania (n = 7) and Europe (n = 38), but a lower proportion elsewhere (Asia n = 1; North America n = 16). Studies exploring other types of treatment were mainly conducted in Europe (n = 20), followed by the UK (n = 10), North America (n = 9), and Oceania (n = 2).
Fig. 4.
Locations of Interventions
Study sample sizes varied from five to 9,614 and have generally increased over the last 30 years. Overall, around half to two thirds of studies of each therapeutic modality had samples between 20 and 100. Cognitive and behavioural and schema therapy studies were generally smaller (samples < 20 = 16/55; > 100 = 9/55), and psychodynamic and MBT therapies were larger (samples < 20 = 3/74; > 100 = 22/74). Sample sizes of RCTs have also risen during this period. The mean sample size rose from 55.3 (SD = 35.7) between 1990 and 1999 to 97.4 (SD = 98.1) between 2010 and 2019.
Outcomes
Overall, “BPD” was the most studied diagnosis, with 128 studies (57%) including samples partially or wholly made up of people given a diagnosis of “BPD”, followed by studies including participants with a mixture of “personality disorder” diagnoses (n = 79, 35%). Fourteen (6%) studies did not have “personality disorder” diagnosis as an inclusion criterion, but used inclusion criteria that in the judgement of the team, including clinicians, appeared to encompass similar difficulties, for example focusing on repeated self-harm or suicide attempts, complex trauma or PTSD, and emotional dysregulation or instability. These studies were included in an attempt to capture studies relevant to people with CEN in which investigators had decided not to use the “personality disorder” label as a primary way of identifying participants. “BPD” was the most studied diagnosis across treatment types, except for psychodynamic therapies and other therapies, where the largest category was studies in which participants had a mixture of “personality disorder” diagnoses. Most samples of studies that reported the sex or gender and/or ethnicity of participants were mostly female and White with 39 studies including only women and 13 studies only White participants. One study included a 100% male sample. The remaining studies included mixed samples or did not report sex or gender and/or ethnicity.
Ninety-six out of 226 studies had specified primary outcomes, including 21/65 studies on DBT, 10/20 studies on MBT, 23/54 studies on psychodynamic therapy, 24/49 studies on cognitive and behavioural therapy, 5/6 studies on schema therapy, and 20/41 studies on other treatment. The most studied outcomes were improvement in overall symptom severity (approximately N = 106), personality symptoms/functioning/diagnosis (approx. N = 113), as well as other symptoms, such as anxiety, depressive, or PTSD symptoms (approx. N = 115). Other commonly examined outcomes were social functioning and interpersonal symptoms and problems (approx. N = 88), self-harm, suicide attempts, and suicidality (approx. N = 87), service use, such as crisis service use and length and number of hospitalisations (approx. N = 66), as well as quality of life (approx. N = 44) and general functioning (approx. N = 48). Approximately 145 studies also examined a range of other outcomes.
Main findings
In the following sections we highlight the main findings for each intervention type by focusing on results of studies with an identified primary outcome, and on those with sample sizes greater than 100 participants. Findings are further described in Tables 1, 2, 3, 4 with more detailed summarise shown in Additional file 1: Appendices 2–5, including findings of uncontrolled studies which only made comparisons over time within the same subjects: the Tables indicate that these almost always showed a tendency for improvements over time. For this reason and because of their relative methodological weaknesses we do not summarise them further in the text below (unless of interest because adaptations have been made and feasibility of treatment tested for specific groups who are not usually the focus of trials, such as people with comorbidities, or older or younger people or ethnic or sexual minorities).
DBT
Table 1, Additional file 1: Appendix 2 and Appendix 6 summarise studies investigating the effectiveness of DBT (n = 66), of which the largest group was RCTs (n = 27), followed by uncontrolled studies making only pre-post comparisons (n = 24), non-randomised studies with contemporaneous comparators (including quasi and natural experiments) (n = 6), uncontrolled intervention development studies (n = 8), and one implementation study. Detailed study findings on the effectiveness of DBT are listed by study design in Table 1 and Additional file 1: Appendix 2.
DBT interventions: inactive/non-specialist comparators
As shown in Table 1 and Additional file 1: Appendix 2, 13 studies involved comparisons with an inactive or non-specialist treatment control, such as TAU or waitlist. Of these 13 studies, 12 were RCTs and one a non-randomised study with a contemporaneous comparator. Six of these had identified primary outcomes, including self-harm, symptoms, global distress, and hospital admission, and DBT was found to be superior to comparators on some but not all of these outcomes (sample sizes ranging from 20 to 100 participants). Across all 13 studies, there was again a mixture of findings, some suggesting superiority for DBT and some no clear difference (see Table 1 and Additional file 1: Appendix 2).
DBT interventions: specialist comparators
For studies comparing DBT with other forms of specialist psychotherapy, including General Psychiatric Management, Community Treatment by Experts, Comprehensive Validation Therapy plus 12 step programme, and clinical case management (n = 8), DBT was not superior to comparators on the majority of outcomes in RCTs (n = 6) and non-randomised studies with contemporaneous comparators (n = 2) (see Table 1 and Additional file 1: Appendix 2). For studies with specified primary outcomes, DBT showed similar or less improvement in self-harm and suicidality compared to controls in 2/3 RCTs, but was superior to Community Treatment by Experts on suicide attempts in the third RCT. Three of these RCTs had sample sizes greater than 100.
DBT interventions: partial or modified comparators
Table 1 and Additional file 1: Appendix 2 include 19 studies that investigated partial or modified DBT therapies. In these studies, DBT was superior to comparators on some outcomes in RCTs (n = 6), including three RCTs with sample sizes greater than 100 and one pilot RCT, but inferior to controls on all outcomes in one non-randomised trial with a contemporaneous comparator. No study that investigated partial or modified DBT therapies had both a specified primary outcome and a control group (n = 19).
DBT interventions in samples not defined only by “personality disorder”
As shown in the Table 1 and Additional file 1: Appendix 2 cohort diagnoses and demographics columns, seven of the studies so far described focused on samples defined by having comorbid conditions in addition to a “personality disorder” diagnosis (severe mental illness (n = 1) or substance misuse (n = 2)). Four DBT studies used criteria other than “personality disorder” diagnosis, including emotional dysregulation (n = 1), parasuicidal behaviours in the past six months (n = 1), and severe difficulty in functioning together with frequent suicide attempts (n = 1), or crisis service use (n = 1). These studies included one RCT, one intervention development study, and five studies involving only pre-post comparisons.
DBT intervention: adaptions for specific populations
Additionally, a total of eight studies examined the effectiveness and/or feasibility of DBT adapted for specific clinical or demographic populations, including people with comorbid PTSD (n = 3) or eating disorders (n = 1), young adults (n = 2), female caregivers of children under 3 (n = 1), and married men receiving couples therapy n = 1). Three of these studies were RCTs. One of the RCTs had 193 participants and found DBT-PTSD to be superior to Cognitive Processing Therapy (CPT) for participants with complex PTSD and a history of childhood abuse, on the primary outcome, PTSD diagnosis, as well as secondary outcomes. In a non-randomised controlled study with 118 participants, DBT was superior to CBT on some primary outcomes and most non-primary outcomes.
DBT interventions: summary
Overall, DBT tended to be superior or not different in outcomes from inactive/non-specialist comparators. Findings for specialist DBT and modified DBT treatments were mixed. DBT interventions adapted to specific populations were superior to comparators on most outcomes. Out of the 66 studies investigating the effectiveness of DBT only eight had sample sizes greater than 100 and of these only four were RCTs. Power calculations were rare, limiting interpretation of findings of no difference.
Cognitive and behavioural and schema therapies
Table 2, Additional file 1: Appendix 3, and Appendix 7 present study characteristics and findings of cognitive and behavioural and schema therapies (n = 55). There were 26 RCTs, 17 uncontrolled intervention development studies, three non-randomised studies with contemporaneous controls, and nine uncontrolled studies making only pre-post-treatment comparisons. Detailed findings of the effectiveness of cognitive and behavioural and schema therapies by study design are listed in Table 2 and Additional file 1: Appendix 3 as well as summarised below.
Cognitive and behavioural and schema therapy interventions: inactive/non-specialist comparators
Nineteen studies of interventions based on cognitive and behavioural principles and/or the related schema approaches had inactive/non-specialist comparators as shown in Table 2 and Additional file 1: Appendix 3. In RCTs (n = 19 including 4 pilot studies), compared to inactive/non-specialist controls, participants receiving cognitive and behavioural or schema therapy showed improvement on some outcomes. 12/19 RCTs had specified primary outcomes, with sample sizes ranging from 34 to 480. Cognitive and behavioural or schema therapy was superior compared to controls on primary outcomes in some studies, including for “personality disorder” symptoms (n = 3), “recovery” (n = 1), and symptom severity and social functioning in 1/2 RCTs. Cognitive and behavioural or schema therapy was not shown to be superior for other primary outcomes, including depressive or (social) anxiety symptoms (n = 1), service use (n = 1), and/or self-harm (n = 4) (see Table 3 and Additional file 1: Appendix 3).
Cognitive and behavioural and schema therapy interventions: specialist comparators
In studies with specialist treatment comparators, including Rogerian Supportive Therapy, Transference-Focused Therapy, Dynamic psychotherapy, group-based CBT, individual Cognitive-Evolution Therapy, Mindful Emotion Awareness and Cognitive Reappraisal, and different treatment settings (n = 7), cognitive and behavioural therapy was inferior to or showed similar improvements to control treatments for all outcomes in RCTs (n = 4) and non-randomised studies with contemporaneous comparators (n = 3) (see Table 2 and Additional file 1: Appendix 3). This included the results of three RCTs and two non-randomised studies with contemporaneous controls with specified primary outcomes (“BPD” symptoms, symptom severity, personality functioning, and interpersonal problems). Sample sizes of studies with primary outcomes ranged from 46 to 205.
Cognitive and behavioural and schema therapy interventions: partial or modified interventions
Table 2 and Additional file 1: Appendix 3 report three RCTs, including one pilot RCT, which examined modifications of cognitive and behavioural or schema therapies. Modifications included addition of phone support, or therapeutic assessments, and interventions delivered at home. These interventions were not superior to unmodified comparators on any outcomes, including the primary outcome in the two RCTs which reported these: one study with 20 participants found no difference in “BPD” recovery with the addition of phone support to schema therapy, and one study with 62 participants found mixed findings on the primary outcome suicidality with delivery of a CBT-based treatment at home.
Cognitive and behavioural and schema therapy interventions in samples not defined only by “personality disorder”
As shown in Table 2 and Additional file 1: Appendix 3, of the above studies nine examined the effectiveness of cognitive and behavioural treatments for clinical populations with “personality disorder” diagnoses and comorbid mental health problems, or individuals with related difficulties but not a formal “personality disorder” diagnosis. These studies looked at individuals with “BPD” symptoms and comorbidities including substance use (n = 1) and mood disorder (n = 4), or at populations that met our criteria for difficulties that appeared comparable to those of people receiving “personality disorder” diagnoses (n = 4), including repeated self-harm (n = 1), non-suicidal self-injury disorder (n = 1), previous suicide attempts (n = 1), and history of childhood sexual abuse (n = 1).
Cognitive and behavioural and schema therapy interventions: summary
Overall, cognitive and behavioural and schema interventions with inactive/non-specialist comparators showed showed improvements on only some measures compared to controls. Studies with active/specialist comparators and studies investigating modified interventions were inferior to or showed similar improvements to controls. Of the 55 studies investigating the effectiveness of cognitive and behavioural and schema treatments, nine studies included > 100 participants of which seven were RCTs (six with inactive/non-specialist comparators).
Psychodynamic and MBT studies
Table 3, Additional file 1: Appendix 4, and Appendix 8 summarise studies investigating the effectiveness of MBT (n = 20) and psychodynamic interventions (n = 54). There were 25 RCTs, and 48 non-randomised studies, which included non-randomised studies with contemporaneous controls (n = 17) and studies without control groups making only pre-post comparisons (n = 31). One uncontrolled study focused on intervention development.
MBT interventions: inactive/non-specialist comparators
As shown in Table 3 and Additional file 1: Appendix 4, four RCTs compared MBT with an inactive/non-specialist treatment control (as did a non-randomised study comparing with a historical cohort). MBT was superior to the inactive/non-specialist controls on most outcomes. Two RCTs specified primary outcomes, and MBT proved superior in reducing both “BPD” symptoms (n = 1) and suicide attempts (n = 1). The 2/4 RCTs with primary outcomes included 41 and 51 participants.
MBT interventions: specialist comparators
For studies comparing MBT with other forms of specialist treatment, including specialist TAU, supportive group therapy, Structured Clinical Management, and DBT, (n = 9), MBT showed no significant difference in most outcomes in 3/4 RCTs, with the fourth (sample size 107) reporting greater improvements in the primary outcomes of parasuicidal behaviours and number of hospitalisations compared with Structured Clinical Management (see Table 3 and Additional file 1: Appendix 4). In three non-randomised studies, results were mixed with few additional benefits reported for MBT compared with other specialist treatments. In primary outcomes, one study reported similar reductions in bed days to the specialist treatment comparator.
MBT interventions: treatment setting comparisons
Table 3 and Additional file 1: Appendix 4 include one RCT comparing MBT delivered in different settings (sample size 114) which found no differences on primary (symptom severity) or secondary outcomes between MBT at a day hospital compared to an intensive out-patient MBT.
Psychodynamic interventions: inactive/non-specialist comparators
Table 3 and Additional file 1: Appendix 4 show 13 studies on psychodynamic treatments with inactive/non-specialist comparators including six RCTs and seven non-randomised studies. Participants receiving psychodynamic therapy showed greater improvements compared to inactive/non-specialist comparators in the majority of outcomes in RCTs and close to all outcomes in non-randomised studies with control groups. Greater improvement in the primary outcome than control was reported in the 2/3 RCTs (sample sizes 27–62) and all four non-randomised studies (sample sizes 45–143) that specified a primary outcome (see Table 3 and Additional file 1: Appendix 4).
Psychodynamic interventions: specialist comparators
In studies with specialist comparators (n = 11), including manual-based Psychiatric-Psychodynamic sessions, General Psychiatric Management, cognitive therapy, and Transference-Focused Therapy plus supportive treatment, the intervention group was superior to the control group on only a few outcomes in RCTs (n = 8), but most outcomes in non-randomised studies (n = 3) (see Table 3 and Additional file 1: Appendix 4). Of RCTs specifying primary outcomes (sample sizes 25–99), only 1/3 RCTs reported greater progress in therapy (n = 1) compared to specialist comparators, and one RCT did not report differences between groups in symptom severity and interpersonal symptoms. One non-randomised study reported greater improvement in “personality disorder” symptoms for Dynamic Deconstructive Psychotherapy compared to controls and DBT.
Psychodynamic interventions: treatment setting comparisons
Table 3 and Additional file 1: Appendix 4 list the six non-randomised studies which compared the outcomes of psychodynamic therapy delivered in different settings. There was no difference in outcomes, including the primary outcome symptom severity, in four studies comparing day hospital, outpatient, and inpatient services (sample sizes 143–371). However, community and step-down services were superior to residential services on all outcomes.
Psychodynamic and MBT interventions in samples not defined only by “personality disorder”
As shown in Table 3 and Additional file 1: Appendix 4, of the above studies, six focused on clinical populations with “personality disorder” diagnoses and comorbid mental health problems, or individuals with related difficulties but not a formal “personality disorder” diagnosis. Study samples included people with alcohol use and comorbid “personality disorder” diagnosis (n-1) with treatment resistant depression and a history of early childhood trauma together with comorbid “personality disorder” diagnosis (n = 1) and with poor personal, social, and/or interpersonal functioning with or without “personality disorder” diagnosis (n = 4).
Psychodynamic and MBT interventions: adaptions for specific populations
Additionally, two RCTs (n = 30), one being the follow-up study, examined the effectiveness of psychodynamic treatments that were adapted to specific clinical or demographic populations. Compared to controls, Dynamic Deconstructive Psychotherapy adapted for people with a “BPD” diagnosis and active alcohol use or dependence, was superior on the majority of outcomes, including all primary outcomes (“BPD” symptom severity, parasuicidal behaviour, alcohol misuse, and institutional care).
Psychodynamic interventions: summary
Overall, psychodynamic and MBT interventions were superior to inactive/non-specialist comparators on most outcomes. Compared to specialist therapies, MBT and psychodynamic interventions tended to be similar on most outcomes in RCTs. While psychodynamic interventions were superior to specialist comparators on most outcomes in non-randomised studies, there were mixed findings for non-randomised studies investigating the effectiveness of MBT. In studies comparing different treatment settings, there was some evidence of superiority of community and step-down over residential services. There was no difference in the effectiveness between MBT settings. Lastly, psychodynamic interventions adapted to specific populations were superior to comparators on most outcomes. 23/74 studies investigating the effectiveness of psychodynamic and MBT interventions included > 100 participants of which seven were RCTs (three of which had specialist comparators).
Other studies
Table 4, Additional file 1: Appendix 5, and Appendix 9 present studies on any treatment type other than the psychotherapies listed above (n = 41). These included studies of mixed therapeutic modalities (n = 10), other individual therapies (n = 7), social-interpersonal and functional therapies (n = 5), self-management and care planning interventions (n = 6), as well as studies investigating outcomes of different approaches to service design and delivery (n = 13). Most studies were RCTs (n = 25), while three studies made comparisons with contemporaneous control groups, and 13 only pre-post comparisons. Table 4 and Additional file 1: Appendix 5 list detailed findings of studies on the effectiveness of other interventions by study design. Findings are summarised below.
Mixed interventions
As shown in Table 4 and Additional file 1: Appendix 5, in RCTs with inactive/non-specialist comparators examining mixed therapeutic modalities, the intervention group was superior to controls on most outcomes (n = 3), including the primary outcomes (drop out and suicide attempts) of an RCT with 104 participants, but not “BPD” symptoms, the primary outcome of an RCT with 71 participants.
In one RCT with a specialist comparator, cost-effectiveness did not differ between the step-down treatment and outpatient control group (0/1).
Other individual therapies
Compared to controls, participants receiving individual therapies other than the psychotherapies listed above (including Art therapy, Abandonment psychotherapy, Body Awareness Group therapy, short-term psychotherapy, and psychoeducation) showed greater improvements in close to all outcomes in RCTs with inactive/non-specialist comparators (n = 5 including one pilot RCT). However, in the two RCTs with specified primary outcomes Abandonment psychotherapy was superior to the control for suicidal relapse and hospitalisation (n = 1), but psychoeducation was not superior to control for “BPD” severity (n = 1).
Other individual therapies were not superior to controls in two RCTs with specialist treatment comparators, including one RCT included one RCT comparing to Abandonment psychotherapy delivered by nurses instead of trained psychotherapists, and another comparing to Transference-Focused Therapy and DBT, on all outcomes including primary outcomes.
Sample sizes of RCTs with primary outcomes ranged from 50 to 170.
Social-interpersonal and functional interventions
Table 4 and Additional file 1: Appendix 5 show that similar results were found for social and interpersonal interventions, with the intervention group being superior compared to controls on up to half of the outcomes in RCTs with inactive/non-specialist comparators (n = 3). Additionally, the intervention group was superior on primary outcomes in only 1/2 RCTs with identified primary outcomes: Psychoeducation plus problem-solving therapy showed greater improvement in social functioning and social problem-solving skills compared to waitlist, however, the cognitive rehabilitation and psychoeducation groups improved similarly in general functioning. RCTs with primary outcomes included 70 and 176 participants.
There were no between-group differences found in RCTs with specialist comparators, including delayed Functional Imagery Training and Social Skills Training in the clinic/hospital only (n = 2 including one pilot RCT).
Self-management and care planning
There were no between-group differences on outcomes in 1/2 RCTs on self-management and care planning compared to self-management only or established generic or specialist mental health services (n = 1). As shown in Table 4 and Additional file 1: Appendix 5, this included the primary outcomes of two RCTs: The Joint Crisis Plan group and TAU group had similar rates of self-harm in one RCT including 88 participants (the RCT was not powered to find an effect). The second RCT with a sample size of 52 found no difference in service admissions in Nidotherapy-enhanced assertive outreach compared to standard assertive outreach. In one RCT without identified primary outcomes, compared to Structured Goal-Focused Pre-Treatment Intervention (GFPTI), participants receiving therapeutic assessment improved in more than half of the outcomes.
Novel mental health service models compared to day hospital
Regarding service design models, one RCT comprising four papers comparing step-down treatment with outpatient treatment showed no between-group differences on outcomes, including a range of primary outcomes (see Table 4 and Additional file 1: Appendix 5). In the other RCT only including patients with a “BPD” diagnosis, the step-down intervention group was superior compared to the outpatient group on half of the outcomes.
Lastly, two RCTs with samples > 100 examining novel mental health service models compared to established generic or specialist mental health services found the intervention group to be superior on some outcomes compared to the control group, but on primary outcomes related to service use only in 1/2 RCTs.
Other treatments in samples not defined only by “personality disorder”
As depicted in the Table 4 and Additional file 1: Appendix 5 cohort columns, six of the above studies on other treatments focused on specific populations, including three RCTs, one non-randomised study with a contemporaneous control, and one uncontrolled study making only pre-post comparisons. One RCT compared the effectiveness of Abandonment psychotherapy and intensive TAU for individuals with major depression and a comorbid “BPD” diagnosis. Another RCT investigated a joint crisis plan and TAU for young people without a “personality disorder” diagnosis but at least two episodes of self-harm in the previous three months. A third RCT compared the effectiveness of Nidotherapy and TAU for individuals with severe mental illness and a comorbid “personality disorder” diagnosis. One non-randomised study examined collaborative care management and TAU for individuals with major depression with or without a comorbid “personality disorder” diagnosis. Lastly, an uncontrolled study investigated emotion regulation skills training for a community-based sample of individuals with adverse childhood experiences over time.
Discussion
Our scoping review collated quantitative evidence regarding community-based psychological, psychosocial, and service level interventions designed for people with CEN. Most studies focused on people given a “personality disorder” diagnosis, with a small number relating to people who appeared to have comparable difficulties (6%). Some observations may be made from this literature, but large gaps are prominent.
What does the literature tell us?
We identified 226 papers reporting on 210 distinct studies carried out in a range of countries, the majority in Europe or North America. The largest group of studies evaluated the effectiveness of DBT, followed by psychodynamic therapy, cognitive and behavioural therapy, MBT, and schema therapy. Research on psychological treatments dominated, with only a small handful of studies using any method to investigate interventions with primarily social targets, self-management, care planning, or models of service delivery.
The total quantity of studies, given the breadth of the search and inclusion of uncontrolled studies and studies with very small samples, is small. Little literature was published in the twentieth century, with most included studies published after 2005, since when annual publication rates have slowly risen. This may reflect a shift internationally away from the view of “personality disorder” as untreatable and justifying exclusion from mental health services that prevailed in the twentieth century [259]. In the early 2000s, factors including the publication of trials that held out prospects for successful treatment, service user activism, and key policy documents such as the UK’s “Personality Disorder: No longer a diagnosis of exclusion” may have contributed to greater confidence that research in this area is potentially fruitful [6, 260, 261]. However, stigma, therapeutic pessimism, and difficulty accessing any kind of helpful care are still widely reported [10, 11, 14, 20, 262]. The results of our searches suggest that investment in large well-designed studies that test clear primary hypotheses has remained very limited around the world, which may reflect a continuing lack of optimism, and the impacts of the particularly severe stigma that appears associated with CEN.
The evidence base that has been established thus far relates mainly to specialist psychotherapies, delivered especially to people with a “BPD” diagnosis. Many studies are small and/or non-randomised, but studies with any methodology have tended to suggest benefits for specialist psychotherapies of a range of types compared with inactive/non-specialist controls, both in studies focused on people with a “BPD” diagnosis and with broader groups. However, results do not tend to suggest one kind of specialist treatment is clearly superior to another – this coheres with the results of more narrowly focused systematic reviews that do not identify a clear gold standard but suggest a variety of psychological treatments are helpful for those who engage with them [23, 26]: a focus on what works well for whom, and why, would be helpful in further work.
Contrary to the pessimistic outlook often reported regarding potential for improvement among people with a “personality disorder” diagnosis, a large majority of studies involving before and after comparisons find significant reductions in symptoms and self-harm as well as improvements in other outcomes. This seems to be the case across treatment types as well as diagnoses, often to the extent that a substantial minority of participants were assessed as no longer meeting criteria for a “personality disorder” diagnosis. Study methods often made it hard to assess how far this was a result of treatments received, including those being investigated, and how far of the natural improvement in symptoms and difficulties (people may also tend to be recruited to studies at times when difficulties are especially severe). Findings from these studies suggest the value of uncontrolled studies and of before and after treatment comparisons is very limited except where the main purpose is to test the feasibility and acceptability of delivering an intervention: it appears likely that improvement will be found whatever interventions are offered.
Regarding specific populations such as those who are younger or older or who have some of the conditions that are frequently comorbid with CEN, such as substance misuse or psychosis, we found substantial numbers of interesting small studies, mainly aimed at intervention development, or establishing that treatments are feasible and acceptable in specific populations. These provide potential building blocks for further design and testing of interventions in important populations where substantial trials have yet to be reported.
What does the literature not tell us?
Gaps in the evidence needed to underpin high quality service delivery for people with CEN are large. Service users and clinicians report that mental health care systems appear ill-equipped to deliver accessible care of high quality [10, 15, 20], yet there are hardly any published investigations of the best approaches to designing teams and systems. Care planning, crisis planning, and self-management are to a large extent not investigated as applied to people with CEN. We identified very few studies of interventions with social targets, including employment and social relationships, even though people with CEN identify these as a priority [14, 263]. We found very little evidence of co-production or service user leadership in either research or intervention design, despite the benefits of these in producing research that aligns to service user needs and priorities [264]. We also found very little quantitative research on either trauma-informed care for this group, or interventions for people with comorbid PTSD, despite calls to place trauma at the centre of thinking about CEN [14, 262, 265].
Only a few studies evaluated treatments adapted to specific populations of interest, such as younger or older age groups, parents or patients with comorbid severe mental illnesses, substance misuse, or childhood trauma. As above, a number of small-scale initial studies appeared promising, but were limited by small sample sizes and/or observational or feasibility/intervention development study designs. Lack of more substantial evaluations of well-designed interventions for these groups who have tended to be still more under-served than others with CEN appears an important gap.
Most studies were conducted with participants with a “BPD” diagnosis, so that there is little evidence on effective interventions for people with other diagnoses, or who may have comparable difficulties but not have received a diagnosis. Samples are largely White and female with close to no papers focusing on diverse gender and sexual identities (despite some evidence of LGBTQ + groups being more likely to receive a “personality disorder” diagnosis [266, 267]), or other ethnicities. Studies generally measured effectiveness of interventions by examining improvement in whether diagnostic criteria continued to be met for “personality disorder”, symptom outcomes, self-harm, and service use. However, outcomes prioritised by service users such as personal achievements, employment, and social connections were reported much less [263], and the possibility of iatrogenic harm was also rarely examined. Interventions addressing social needs are especially important in the light of findings of longitudinal studies showing that while symptoms and suicidal behaviour tend to improve with time, this is less the case for psychosocial functioning including rate of employment [268, 269]. Implementation studies examining how to embed successful interventions in real-world settings were also largely absent.
Limitations
Despite the breath of our approach, the findings of the present review must be considered in light of several limitations. In order to provide an overview of evidence acquired so far and identify gaps, we have created broad, often heterogenous, categories of study designs. This approach is inevitably superficial and limits how far meaningful comparisons can be made across study types, treatments, and subpopulations. In keeping with scoping review methodology recommendations, we did not formally assess the quality of the studies, although we have commented on some obvious limitations, for example relating to small trial populations or uncontrolled study designs.
Additionally, while inclusion criteria were kept broad, and a variety of search terms applied to try to include studies with paalthough the number of studies excluded on these grounds was smallrticipants with any diagnosis of “personality disorder” as well as those with comparable difficulties, capturing the latter reliably is likely to have been particularly difficult, and only a small number of studies not based on such criteria were included. We also have not included many studies that are transdiagnostic or include mixed populations of mental health service users. While our search strategy was developed by a team of researchers, clinicians, people with relevant lived experience, and an information scientist, it was not peer reviewed. Lastly, in order to make this very broad search feasible, we included only studies published in English as well as published and peer-reviewed evidence, excluding pre-prints and theses. This may well have excluded some relevant evidence, although the number of studies excluded on these grounds was small.
Conclusions
Our overall conclusion from this scoping review is that people with CEN, despite being numerous among community mental health service users [270] have thus far been poorly served by clinical research. Mental health research is in general under-funded compared with other areas of health [271]. Our findings suggest that this is especially striking in the field of CEN, in which little was published prior to 2005 and the tally has increased only gradually subsequently, now only just exceeding two hundred quantitative studies including 96 RCTs of community and outpatient interventions, even including studies of any scale using any method.
Much therefore needs to be done to develop a robust evidence base in this area, especially beyond a narrow focus on specialist psychotherapies for people with a “BPD” diagnosis, where a substantial number of trials have resulted in a finding that several specialist therapies appear better than treatment as usual, but not in a clear finding that any treatment is clearly superior. Future research should address outcomes valued by patients rather than being limited to a focus on self-harm and symptoms: relevance to service users is much more likely to be achieved by the adoption of co-production in design of both interventions and research studies. The recent service user-led StopSIM campaign against the Serenity Integrated Monitoring intervention [272], which involved the police in responses to some people with frequent contact with emergency services, exemplifies the potential for iatrogenic harm from interventions that are unevaluated, or where the potential for harm has not been assessed. Research on important populations such as older and younger people and people with major comorbidities, and on interventions focusing on people with CEN as parents, partners or relatives needs to progress beyond the feasibility studies conducted so far. Larger and more diverse samples are needed to be confident of relevance across service user populations.
Models of service delivery have been largely neglected in research so far despite recurrent complaints from service users and clinicians that current systems are fragmented and inaccessible. Realist evaluations may shed a light on what mechanisms underly the effectiveness of different interventions as well as what type of intervention works for which patient group and in what context. Relevant contexts may be individual, such as personal life and stage of life, as well as systemic. Additionally, services need to deliver holistic and person-centred care that addresses service users’ interconnected needs and intersecting experiences over several years: large-scale observational designs may be helpful in understanding outcomes over longer periods [10, 14]. Lastly, patients and carers with relevant experiences need to be invited to co-produce the development and evaluation of treatments to not only ask the right questions but also examine these in a meaningful way (Table 5).
Table 5.
Lived experience commentary written by Sarah Labovitch and Jennie Parker
| In light of the Community Mental Health Framework (CMHFA), this review is well timed to revise thinking around what should be available to people who may meet the diagnostic criteria for “personality disorder”/CEN. It may also prompt researchers and service-providers to consider what is important to us—it was disappointing to see that only 44/226 studies reported on quality of life, whilst most primary outcomes focused on diagnostic-related criteria |
| Time to follow-up in many studies discussed is limited. Side-effects of funding constraints typically lead to quantitative research and RCTs being prioritised. We agree with the question of what underlies reported improvements, and would say this is not just in relation to observational studies. It would be interesting to delve further into this |
| Despite advancements in recent years, community service-provision for “personality disorder”/CEN is nevertheless lagging behind other areas of mental health. Treatment in the community must be patient-centred: adapted to factors such as age, culture, comorbidity, substance misuse and trauma. Some health professionals still display discriminatory attitudes towards CEN, or simply don’t know how to help. Finding a clinician with the right skills and compassion is depressingly arduous. Further, exclusion criteria and high thresholds can make “specialist” services inaccessible. Meanwhile, the notion of individuals actually having a choice in therapist is vanishingly slim, adding to the risk of iatrogenic harm and a “cliff-edge” of care. Services need to commit to consistent long-term contact, as well as tailoring treatment to individual needs |
| As with others, we have experienced stigma, rejection, and repeated/inappropriate referrals. This paper leaves us with a conundrum, both in relation to the integrated approach proposed by the |
| CMHFA and access to good and timely support. Whilst this is a scoping review of quantitative research, our recommendation is for further investigation into the active ingredients of therapy: what makes good outcomes for some but not others, the importance of the relationship, and whether we have a choice of therapist (considerate of age, culture, gender, etc.) or of intervention. We also noted the limited research on peer support, compared to our experience of its value. With such a diverse population and diverse range of therapies (and variance within specific models), clearer guidance would be helpful so that we can all make fully-informed choices |
Supplementary Information
Additional file 1: Appendix 1. Search strategy. Appendix 2. Dialectical Behavioural Therapy (DBT) treatments. Appendix 3. Cognitive and Behavioural Therapy and Schema Therapy treatments. Appendix 4. MBT and Psychodynamic Therapy treatments. Appendix 5. Other treatments. Appendix 6. Table of studies testing Dialectical Behavioural Therapy (DBT) treatments. Appendix 7. Table of studies testing Cognitive and Behavioural Therapy and Schema Therapy treatments. Appendix 8. Table of studies testing MBT and Psychodynamic Therapy treatments. Appendix 9. Table of studies testing other treatments.
Acknowledgements
List of the CEN Mental Health Policy Research Group members : Alexandra Papamichail (Health Service and Population Research Department, Section of Women Mental health, IoPPN, King’s College London, London, UK), Ava Mason (Division of Psychiatry, University College London, London, UK), Avithaa Thayaparan (Division of Psychiatry, University College London, London, UK), Baihan Wang (Division of Psychiatry, University College London, London, UK), Christian Dalton Locke (NIHR Mental Health Policy Research Unit, Division of Psychiatry, University College London, London, UK), Jasmine Harju-Seppänen (Division of Psychiatry, University College London, London, UK), Jiping Mo (Division of Psychiatry, University College London, London, UK), Magdalena Tomaskova (Division of Psychiatry, University College London, London, UK), Natasha Lyons (NIHR Mental Health Policy Research Unit, Division of Psychiatry, University College London, London, UK), Spyros Spyridonidis (Division of Psychiatry, University College London, London, UK), Tiffeny James, (Division of Psychiatry, University College London, London, UK), Zainab Dedat (NIHR Mental Health Policy Research Unit, Division of Psychiatry, University College London, London, UK), Zoë Haime (Division of Psychiatry, University College London, London, UK).
Authors’ contributions
SL, LSR, MS, PB contributed to the conception and design of the manuscript, screening, acquisition, analysis, and interpretation of data, as well as drafted and revised the manuscript. PB also contributed to running and re-running the literature searches. BCFC, BH, MMG, TS contributed to the acquisition of data and revised the manuscript. BCFC and TS also contributed to the screening. JP and SL contributed to the interpretation of data, as well as drafted and revised the manuscript. SO contributed to the conception and design of the manuscript. SP contributed to the conception and design of the work and revised the manuscript. SJ contributed to the conception and design of the manuscript, interpretation of data, and revised the manuscript. Members of the CEN Mental Health Policy Research Group have made substantial contributions to the screening and/or acquisition of the data. The author(s) read and approved the final manuscript.
Authors’ information
Not applicable.
Funding
This paper presents independent research commissioned and funded by the National Institute for Health Research (NIHR) Policy Research Programme, conducted by the NIHR Policy Research Unit (PRU) in Mental Health (grant no. PR-PRU-0916–22003). The views expressed are those of the authors and not necessarily those of the NIHR, the Department of Health and Social Care or its arm’s length bodies, or other government departments. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sarah Ledden, Luke Sheridan Rains and Merle Schlief are joint first authors.
Contributor Information
Merle Schlief, Email: merle.schlief.19@ucl.ac.uk.
the C. E. N. Mental Health Policy Research Unit Group:
Alexandra Papamichail, Ava Mason, Avithaa Thayaparan, Baihan Wang, Christian Dalton Locke, Jasmine Harju-Seppänen, Jiping Mo, Magdalena Tomaskova, Natasha Lyons, Spyros Spyridonidis, Tiffeny James, Zainab Dedat, and Zoë Haime
References
- 1.Moran P, Romaniuk H, Coffey C, Chanen A, Degenhardt L, Borschmann R, Patton GC. The influence of personality disorder on the future mental health and social adjustment of young adults: a population-based, longitudinal cohort study. The Lancet Psychiatry. 2016;3(7):636–645. doi: 10.1016/S2215-0366(16)30029-3. [DOI] [PubMed] [Google Scholar]
- 2.Quirk SE, El-Gabalawy R, Brennan SL, Bolton JM, Sareen J, Berk M, Chanen AM, Pasco JA, Williams LJ. Personality disorders and physical comorbidities in adults from the United States: data from the National Epidemiologic Survey on Alcohol and Related Conditions. Soc Psychiatry Psychiatr Epidemiol. 2015;50(5):807–820. doi: 10.1007/s00127-014-0974-1. [DOI] [PubMed] [Google Scholar]
- 3.Soeteman DI. Roijen LH-v, Verheul R, Busschbach JJ: The economic burden of personality disorders in mental health care. J Clin Psychiatry. 2008;69(2):259. doi: 10.4088/jcp.v69n0212. [DOI] [PubMed] [Google Scholar]
- 4.Hastrup L, Jennum P, Ibsen R, Kjellberg J, Simonsen E. Societal costs of Borderline Personality Disorders: a matched-controlled nationwide study of patients and spouses. Acta Psychiatr Scand. 2019;140(5):458–467. doi: 10.1111/acps.13094. [DOI] [PubMed] [Google Scholar]
- 5.Tyrer P, Mulder R, Crawford M, Newton-Howes G, Simonsen E, Ndetei D, Koldobsky N, Fossati A, Mbatia J, Barrett B. Personality disorder: a new global perspective. World Psychiatry. 2010;9(1):56. doi: 10.1002/j.2051-5545.2010.tb00270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of Mental Health . Personality disorder: No longer a diagnosis of exclusion. London: Department of Health; 2003. [Google Scholar]
- 7.National Health and Medical Research Council . Clinical Practice Guideline for the Management of Borderline Personality Disorder. Melbourne: National Health and Medical Research Council; 2012. [Google Scholar]
- 8.Royal College of Psychiatrists . Personality Disorder in Scotland. 2018. [Google Scholar]
- 9.Northern Ireland Personality Disorder Strategy . Personality Disorder: A Diagnosis for Inclusion. 2010. [Google Scholar]
- 10.Sheridan Rains L, Echave A, Rees J, Scott HR, Lever Taylor B, Broeckelmann E, Steare T, Barnett P, Cooper C, Jeynes T. Service user experiences of community services for complex emotional needs: A qualitative thematic synthesis. PLoS ONE. 2021;16(4):e0248316. doi: 10.1371/journal.pone.0248316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lester R, Prescott L, McCormack M, Sampson M. North West Boroughs Healthcare NFT: Service users' experiences of receiving a diagnosis of borderline personality disorder: A systematic review. Personal Ment Health. 2020;14(3):263–283. doi: 10.1002/pmh.1478. [DOI] [PubMed] [Google Scholar]
- 12.Ring D, Lawn S. Stigma perpetuation at the interface of mental health care: a review to compare patient and clinician perspectives of stigma and borderline personality disorder. J Ment Health. 2019:1–21. 10.1080/09638237.2019.158133. [DOI] [PubMed]
- 13.RITB Position Statement On Borderline Personality Disorder [https://recoveryinthebin.org/2019/04/03/ritb-position-statement-on-borderline-personality-disorder/]
- 14.Trevillion K, Stuart R, Ocloo J, Broeckelmann E, Jeffreys S, Jeynes T, Allen D, Russell J, Billings J, Crawford MJ. Service user perspectives of community mental health services for people with complex emotional needs: A co-produced qualitative interview study. BMC Psychiatry. 2022;22(1):1–18. doi: 10.1186/s12888-021-03605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Royal College of Psychiatrists . Services for people diagnosable with personality disorder: Position statement. 2020. [Google Scholar]
- 16.National Confidential Inquiry into Suicide and Homicide by People with Mental Illness . Safer Care for Patients with Personality Disorder. Manchester: University of Manchester; 2018. [Google Scholar]
- 17.Mental Health Council of Australia BaMI HRaEOC . Not for service: experiences of injustice and despair in mental health care in Australia. Canberra: Mental Health Council of Australia; 2005. [Google Scholar]
- 18.Dale O, Sethi F, Stanton C, Evans S, Barnicot K, Sedgwick R, Goldsack S, Doran M, Shoolbred L, Samele C. Personality disorder services in England: findings from a national survey. BJPsych bulletin. 2017;41(5):247–253. doi: 10.1192/pb.bp.116.055251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ng F, Townsend ML, Jewell M, Marceau EM, Grenyer BF. Priorities for service improvement in personality disorder in Australia: perspectives of consumers, carers and clinicians. Personal Ment Health. 2020;14(4):350–360. doi: 10.1002/pmh.1485. [DOI] [PubMed] [Google Scholar]
- 20.Troup J, Lever Taylor B, Sheridan Rains L, Broeckelmann E, Russell J, Jeynes T, Cooper C, Steare T, Dedat Z, McNicholas S. Clinician perspectives on what constitutes good practice in community services for people with Complex Emotional Needs: A qualitative thematic meta-synthesis. PLoS ONE. 2022;17(5):e0267787. doi: 10.1371/journal.pone.0267787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fanaian M, Lewis KL, Grenyer BF. Improving services for people with personality disorders: Views of experienced clinicians. Int J Ment Health Nurs. 2013;22(5):465–471. doi: 10.1111/inm.12009. [DOI] [PubMed] [Google Scholar]
- 22.Flynn S, Raphael J, Graney J, Nyathi T, Williams A, Kapur N, Appleby L, Shaw J. The personality disorder patient pathway: Service user and clinical perspectives. Personal Ment Health. 2019;13(3):134–143. doi: 10.1002/pmh.1444. [DOI] [PubMed] [Google Scholar]
- 23.Oud M, Arntz A, Hermens ML, Verhoef R, Kendall T. Specialized psychotherapies for adults with borderline personality disorder: a systematic review and meta-analysis. Aust N Z J Psychiatry. 2018;52(10):949–961. doi: 10.1177/0004867418791257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barnicot K, Katsakou C, Bhatti N, Savill M, Fearns N, Priebe S. Factors predicting the outcome of psychotherapy for borderline personality disorder: A systematic review. Clin Psychol Rev. 2012;32(5):400–412. doi: 10.1016/j.cpr.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiat. 2017;74(4):319–328. doi: 10.1001/jamapsychiatry.2016.4287. [DOI] [PubMed] [Google Scholar]
- 26.Storebø OJ, Stoffers-Winterling JM, Völlm BA, Kongerslev MT, Mattivi JT, Jørgensen MS, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2020;5:1–512. doi: 10.1002/14651858.CD012955.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharma M, Nazareth I, Petersen I. Observational studies of treatment effectiveness: worthwhile or worthless? Clin Epidemiol. 2019;11:35. doi: 10.2147/CLEP.S178723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peters MD, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Scoping reviews. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. 2020. [Google Scholar]
- 30.Peters MD, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, Khalil H. Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis. 2020;18(10):2119–2126. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- 31.Yuen NWZ, Barnett P, Rains LS, Johnson S, Billings J: Evaluation of international guidance for the community treatment of complex emotional needs: A systematic review. medRxiv. 2022.
- 32.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE: The PRISMA, statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McMain SF, Guimond T, Barnhart R, Habinski L, Streiner DL. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatr Scand. 2017;135(2):138–148. doi: 10.1111/acps.12664. [DOI] [PubMed] [Google Scholar]
- 34.Kramer U, Pascual-Leone A, Berthoud L, De Roten Y, Marquet P, Kolly S, Despland JN, Page D. Assertive anger mediates effects of dialectical behaviour-informed skills training for borderline personality disorder: A randomized controlled trial. Clin Psychol Psychother. 2016;23(3):189–202. doi: 10.1002/cpp.1956. [DOI] [PubMed] [Google Scholar]
- 35.Feigenbaum JD, Fonagy P, Pilling S, Jones A, Wildgoose A, Bebbington PE. A real-world study of the effectiveness of DBT in the UK National Health Service. Br J Clin Psychol. 2012;51(2):121–141. doi: 10.1111/j.2044-8260.2011.02017.x. [DOI] [PubMed] [Google Scholar]
- 36.Priebe S, Bhatti N, Barnicot K, Bremner S, Gaglia A, Katsakou C, Molosankwe I, McCrone P, Zinkler M. Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: A pragmatic randomised controlled trial. Psychother Psychosom. 2012;81(6):356–365. doi: 10.1159/000338897. [DOI] [PubMed] [Google Scholar]
- 37.Carter GL, Willcox CH, Lewin TJ, Conrad AM, Bendit N. Hunter DBT project: randomized controlled trial of dialectical behaviour therapy in women with borderline personality disorder. Aust N Z J Psychiatry. 2010;44(2):162–173. doi: 10.3109/00048670903393621. [DOI] [PubMed] [Google Scholar]
- 38.Soler J, Pascual JC, Tiana T, Cebrià A, Barrachina J, Campins MJ, Gich I, Alvarez E, Pérez V. Dialectical behaviour therapy skills training compared to standard group therapy in borderline personality disorder: A 3-month randomised controlled clinical trial. Behav Res Ther. 2009;47(5):353–358. doi: 10.1016/j.brat.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 39.Van den Bosch LM, Koeter MW, Stijnen T, Verheul R, van den Brink W. Sustained efficacy of dialectical behaviour therapy for borderline personality disorder. Behav Res Ther. 2005;43(9):1231–1241. doi: 10.1016/j.brat.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 40.Verheul R, Van Den Bosch LM, Koeter MW, De Ridder MA, Stijnen T, Van Den Brink W. Dialectical behaviour therapy for women with borderline personality disorder: 12-month, randomised clinical trial in The Netherlands. Br J Psychiatry. 2003;182(2):135–140. doi: 10.1192/bjp.182.2.135. [DOI] [PubMed] [Google Scholar]
- 41.Linehan MM, Tutek DA, Heard HL, Armstrong HE. Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. Am J Psychiatry. 1994;151(12):1771–1775. doi: 10.1176/ajp.151.12.1771. [DOI] [PubMed] [Google Scholar]
- 42.Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- 43.Khabir L, Mohamadi N, Rahimi C, Dastgheib SA. The Effectiveness of Group Therapy based on Mentalization and Dialectical Behavior on Clinical Symptoms of Borderline Personality Disorder: A randomized controlled clinical trial. J Health Sci Surveillance System. 2018;6(2):80–88. [Google Scholar]
- 44.Koons CR, Robins CJ, Tweed JL, Lynch TR, Gonzalez AM, Morse JQ, Bishop GK, Butterfield MI, Bastian LA. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behav Ther. 2001;32(2):371–390. [Google Scholar]
- 45.Robinson S, Lang JE, Hernandez AM, Holz T, Cameron M, Brannon B. Outcomes of dialectical behavior therapy administered by an interdisciplinary team. Arch Psychiatr Nurs. 2018;32(4):512–516. doi: 10.1016/j.apnu.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 46.Flynn D, Kells M, Joyce M, Corcoran P, Gillespie C, Suarez C, Weihrauch M, Cotter P. Standard 12 month dialectical behaviour therapy for adults with borderline personality disorder in a public community mental health setting. Borderline Personal Disord Emot Dysregul. 2017;4(1):1–11. doi: 10.1186/s40479-017-0070-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rizvi SL, Hughes CD, Hittman AD, Vieira Oliveira P. Can trainees effectively deliver dialectical behavior therapy for individuals with borderline personality disorder? Outcomes from a training clinic. J Clin Psychol. 2017;73(12):1599–1611. doi: 10.1002/jclp.22467. [DOI] [PubMed] [Google Scholar]
- 48.Gregory RJ, Sachdeva S. Naturalistic outcomes of evidence-based therapies for borderline personality disorder at a medical university clinic. Am J Psychother. 2016;70(2):167–184. doi: 10.1176/appi.psychotherapy.2016.70.2.167. [DOI] [PubMed] [Google Scholar]
- 49.Stiglmayr C, Stecher-Mohr J, Wagner T, Meiβner J, Spretz D, Steffens C, Roepke S, Fydrich T, Salbach-Andrae H, Schulze J. Effectiveness of dialectic behavioral therapy in routine outpatient care: The Berlin Borderline Study. Borderline Personal Disord Emot Dysregul. 2014;1(1):1–11. doi: 10.1186/2051-6673-1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koons CR, O’Rourke B, Carter B, Erhardt EB. Negotiating for improved reimbursement for dialectical behavior therapy: A successful project. Cogn Behav Pract. 2013;20(3):314–324. [Google Scholar]
- 51.Gutteling BM, Montagne B, Nijs M, van den Bosch LW. Dialectical behavior therapy: Is outpatient group psychotherapy an effective alternative to individual psychotherapy? Preliminary conclusions. Comprehensive Psychiatry. 2012;53(8):1161–1168. doi: 10.1016/j.comppsych.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 52.Axelrod SR, Perepletchikova F, Holtzman K, Sinha R. Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. Am J Drug Alcohol Abuse. 2011;37(1):37–42. doi: 10.3109/00952990.2010.535582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blennerhassett R, Bamford L, Whelan A, Jamieson S, O'Raghaillaigh JW. Dialectical behaviour therapy in an Irish community mental health setting. Irish J Psychol Med. 2009;26(2):59–63. doi: 10.1017/S0790966700000227. [DOI] [PubMed] [Google Scholar]
- 54.Comtois KA, Elwood L, Holdcraft LC, Smith WR, Simpson TL. Effectiveness of dialectical behavior therapy in a community mental health center. Cogn Behav Pract. 2007;14(4):406–414. [Google Scholar]
- 55.Harley RM, Baity MR, Blais MA, Jacobo MC. Use of dialectical behavior therapy skills training for borderline personality disorder in a naturalistic setting. Psychother Res. 2007;17(3):351–358. [Google Scholar]
- 56.Zinkler M, Gaglia A, Arokiadass SR, Farhy E. Dialectical behaviour treatment: implementation and outcomes. Psychiatr Bull. 2007;31(7):249–252. [Google Scholar]
- 57.Brassington J, Krawitz R. Australasian dialectical behaviour therapy pilot outcome study: effectiveness, utility and feasibility. Australas Psychiatry. 2006;14(3):313–318. doi: 10.1080/j.1440-1665.2006.02285.x. [DOI] [PubMed] [Google Scholar]
- 58.Ben-Porath DD, Peterson GA, Smee J. Treatment of individuals with borderline personality disorder using dialectical behavior therapy in a community mental health setting: Clinical application and a preliminary investigation. Cogn Behav Pract. 2004;11(4):424–434. [Google Scholar]
- 59.Perseius K-I, Samuelsson M, Andersson E, Berndtsson T, Götmark H, Henriksson F, Kåver A, Nilsonne Å, Åsberg M. Does dialectical behavioural therapy reduce treatment costs for patients with borderline personality disorder. A pilot study. Vård I Norden. 2004;24(2):27–30. [Google Scholar]
- 60.Lopez A, Chessick CA. DBT graduate group pilot study: A model to generalize skills to create a “life worth living”. Soc Work Ment Health. 2013;11(2):141–153. [Google Scholar]
- 61.Comtois KA, Kerbrat AH, Atkins DC, Harned MS, Elwood L. Recovery from disability for individuals with borderline personality disorder: a feasibility trial of DBT-ACES. Psychiatr Serv. 2010;61(11):1106–1111. doi: 10.1176/ps.2010.61.11.1106. [DOI] [PubMed] [Google Scholar]
- 62.Stanley B, Brodsky B, Nelson JD, Dulit R. Brief dialectical behavior therapy (DBT-B) for suicidal behavior and non-suicidal self injury. Arch Suicide Res. 2007;11(4):337–341. doi: 10.1080/13811110701542069. [DOI] [PubMed] [Google Scholar]
- 63.Flynn D, Kells M, Joyce M, Corcoran P, Hurley J, Gillespie C, Suarez C, Swales M, Arensman E. Multisite implementation and evaluation of 12-month standard Dialectical Behavior Therapy in a public community setting. J Pers Disord. 2020;34(3):377–393. doi: 10.1521/pedi_2018_32_402. [DOI] [PubMed] [Google Scholar]
- 64.McMain SF, Guimond T, Streiner DL, Cardish RJ, Links PS. Dialectical behavior therapy compared with general psychiatric management for borderline personality disorder: Clinical outcomes and functioning over a 2-year follow-up. Am J Psychiatry. 2012;169(6):650–661. doi: 10.1176/appi.ajp.2012.11091416. [DOI] [PubMed] [Google Scholar]
- 65.Pasieczny N, Connor J. The effectiveness of dialectical behaviour therapy in routine public mental health settings: An Australian controlled trial. Behav Res Ther. 2011;49(1):4–10. doi: 10.1016/j.brat.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 66.McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, Streiner DL. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1365–1374. doi: 10.1176/appi.ajp.2009.09010039. [DOI] [PubMed] [Google Scholar]
- 67.Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: A multiwave study. Am J Psychiatry. 2007;164(6):922–928. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- 68.Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- 69.Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, Kivlahan DR. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;67(1):13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- 70.Barnicot K, Crawford M. Dialectical behaviour therapy v. mentalisation-based therapy for borderline personality disorder. Psychol Med. 2019;49(12):2060–2068. doi: 10.1017/S0033291718002878. [DOI] [PubMed] [Google Scholar]
- 71.Andión Ó, Ferrer M, Matali J, Gancedo B, Calvo N, Barral C, Valero S, Di Genova A, Diener MJ, Torrubia R. Effectiveness of combined individual and group dialectical behavior therapy compared to only individual dialectical behavior therapy: A preliminary study. Psychotherapy. 2012;49(2):241. doi: 10.1037/a0027401. [DOI] [PubMed] [Google Scholar]
- 72.Carmona i Farrés C, Elices M, Soler J, Domínguez-Clavé E, Martín-Blanco A, Pomarol-Clotet E, Salvador R, Martinez-Horta S, Pascual JC. Effects of mindfulness training on the default mode network in borderline personality disorder. Clin Psychol Psychother. 2019;26(5):562–571. doi: 10.1002/cpp.2382. [DOI] [PubMed] [Google Scholar]
- 73.Lin T-J, Ko H-C. Wu JY-W, Oei TP, Lane H-Y, Chen C-H: The effectiveness of dialectical behavior therapy skills training group vs. cognitive therapy group on reducing depression and suicide attempts for borderline personality disorder in Taiwan. Arch Suicide Res. 2019;23(1):82–99. doi: 10.1080/13811118.2018.1436104. [DOI] [PubMed] [Google Scholar]
- 74.Elices M, Pascual JC, Portella MJ, Feliu-Soler A, Martín-Blanco A, Carmona C, Soler J. Impact of mindfulness training on borderline personality disorder: A randomized trial. Mindfulness. 2016;7(3):584–595. doi: 10.1186/s40479-015-0035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, McDavid J, Comtois KA, Murray-Gregory AM. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: A randomized clinical trial and component analysis. JAMA Psychiat. 2015;72(5):475–482. doi: 10.1001/jamapsychiatry.2014.3039. [DOI] [PubMed] [Google Scholar]
- 76.Turner RM. Naturalistic evaluation of dialectical behavior therapy-oriented treatment for borderline personality disorder. Cogn Behav Pract. 2000;7(4):413–419. [Google Scholar]
- 77.Feliu-Soler A, Pascual JC, Elices M, Martín-Blanco A, Carmona C, Cebolla A, Simón V, Soler J. Fostering self-compassion and loving-kindness in patients with borderline personality disorder: A randomized pilot study. Clin Psychol Psychother. 2017;24(1):278–286. doi: 10.1002/cpp.2000. [DOI] [PubMed] [Google Scholar]
- 78.Kells M, Joyce M, Flynn D, Spillane A, Hayes A. Dialectical behaviour therapy skills reconsidered: applying skills training to emotionally dysregulated individuals who do not engage in suicidal and self-harming behaviours. Borderline Personal Disord Emot Dysregul. 2020;7(1):3. doi: 10.1186/s40479-020-0119-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lakeman R, Emeleus M, Davies S, Anderson S. A pragmatic evaluation of a high-fidelity dialectical behaviour therapy programme for youth with borderline personality disorder. Adv Mental Health. 2020;19(2):1–11. [Google Scholar]
- 80.Lyng J, Swales MA, Hastings RP, Millar T, Duffy DJ, Booth R. Standalone DBT group skills training versus standard (i.e. all modes) DBT for borderline personality disorder: A natural quasi-experiment in routine clinical practice. Comm Mental Health J. 2020;56(2):238–250. doi: 10.1007/s10597-019-00485-7. [DOI] [PubMed] [Google Scholar]
- 81.Aafjes-van Doorn K, Kamsteeg C, Portier K, Chitre G. A dialectical behavior therapy skills group in a psychoanalytic community service: A pilot study. J Cogn Psychother. 2020;34(1):21–46. doi: 10.1891/0889-8391.34.1.21. [DOI] [PubMed] [Google Scholar]
- 82.Sandage SJ, Long B, Moen R, Jankowski PJ, Worthington EL, Jr, Wade NG, Rye MS. Forgiveness in the treatment of borderline personality disorder: A quasi-experimental study. J Clin Psychol. 2015;71(7):625–640. doi: 10.1002/jclp.22185. [DOI] [PubMed] [Google Scholar]
- 83.Williams SE, Hartstone MD, Denson LA. Dialectical behavioural therapy and borderline personality disorder: Effects on service utilisation and self-reported symptoms. Behav Chang. 2010;27(4):251. [Google Scholar]
- 84.Yen S, Johnson J, Costello E, Simpson EB. A 5-day dialectical behavior therapy partial hospital program for women with borderline personality disorder: Predictors of outcome from a 3-month follow-up study. J Psychiatr Pract. 2009;15(3):173. doi: 10.1097/01.pra.0000351877.45260.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Prendergast N, McCausland J. Dialectic behaviour therapy: A 12-month collaborative program in a local community setting. Behav Chang. 2007;24(1):25. [Google Scholar]
- 86.Sambrook S, Abba N, Chadwick P. Evaluation of DBT emotional coping skills groups for people with parasuicidal behaviours. Behav Cogn Psychother. 2007;35(2):241. [Google Scholar]
- 87.McQuillan A, Nicastro R, Guenot F, Girard M, Lissner C, Ferrero F. Intensive dialectical behavior therapy for outpatients with borderline personality disorder who are in crisis. Psychiatr Serv. 2005;56(2):193–197. doi: 10.1176/appi.ps.56.2.193. [DOI] [PubMed] [Google Scholar]
- 88.Conrad AM, Sankaranarayanan A, Lewin TJ, Dunbar A. Effectiveness of a 10-week group program based on Dialectical Behaviour Therapy skills among patients with personality and mood disorders: Findings from a pilot study. Australas Psychiatry. 2017;25(5):466–470. doi: 10.1177/1039856217707393. [DOI] [PubMed] [Google Scholar]
- 89.Meaney-Tavares R, Hasking P. Coping and regulating emotions: A pilot study of a modified dialectical behavior therapy group delivered in a college counseling service. J Am Coll Health. 2013;61(5):303–309. doi: 10.1080/07448481.2013.791827. [DOI] [PubMed] [Google Scholar]
- 90.Pozzi E, Ridolfi ME, Manganaro D, Daniel DB, Berardi D. Multiple integrated treatment of borderline personality disorders. Psychoanal Psychother. 2008;22(3):218–234. [Google Scholar]
- 91.Bohus M, Kleindienst N, Hahn C, Müller-Engelmann M, Ludäscher P, Steil R, Fydrich T, Kuehner C, Resick PA, Stiglmayr C. Dialectical Behavior Therapy for Posttraumatic Stress Disorder (DBT-PTSD) compared with Cognitive Processing Therapy (CPT) in complex presentations of PTSD in women survivors of childhood abuse: A randomized clinical trial. JAMA Psychiat. 2020;77(12):1235–1245. doi: 10.1001/jamapsychiatry.2020.2148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kamalabadi MJ, Ahmadi SA, Etemadi O, Fatehizadeh M, Bahrami F, Firoozabadi A. A study of the effect of couple dialectical behavioral therapy on symptoms and quality of marital relationships and mental health of Iranian borderline personality couples: a controlled trial. Interdisciplinary J Contemporary Res Business. 2012;3(9):1480–1487. [Google Scholar]
- 93.Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of Dialectical Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behav Res Ther. 2014;55:7–17. doi: 10.1016/j.brat.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Navarro-Haro MV, Botella C, Guillen V, Moliner R, Marco H, Jorquera M, Baños R, Garcia-Palacios A. Dialectical behavior therapy in the treatment of borderline personality disorder and eating disorders comorbidity: A pilot study in a naturalistic setting. Cogn Ther Res. 2018;42(5):636–649. [Google Scholar]
- 95.Williams AES, Yelland C, Hollamby S, Wigley M, Aylward P. A new therapeutic group to help women with borderline personality disorder and their infants. J Psychiatr Pract. 2018;24(5):331–340. doi: 10.1097/PRA.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 96.Lyng J, Swales MA, Hastings RP, Millar T, Duffy DJ. Outcomes for 18 to 25-year-olds with borderline personality disorder in a dedicated young adult only DBT programme compared to a general adult DBT programme for all ages 18+ Early Interv Psychiatry. 2019;14(1):61–68. doi: 10.1111/eip.12808. [DOI] [PubMed] [Google Scholar]
- 97.Steil R, Dittmann C, Müller-Engelmann M, Dyer A, Maasch A-M, Priebe K. Dialectical behaviour therapy for posttraumatic stress disorder related to childhood sexual abuse: A pilot study in an outpatient treatment setting. Eur J Psychotraumatol. 2018;9(1):1423832. doi: 10.1080/20008198.2018.1423832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lyng J, Swales M, Hastings R. Dialectical behaviour therapy for younger adults: Evaluation of 22 weeks of community delivered dialectical behaviour therapy for females 18–25 years. Irish J Psychol Med. 2015;32(4):299–305. doi: 10.1017/ipm.2014.69. [DOI] [PubMed] [Google Scholar]
- 99.McMurran M, Day F, Reilly J, Delport J, McCrone P, Whitham D, Tan W, Duggan C, Montgomery AA, Williams HC. Psychoeducation and Problem Solving (PEPS) therapy for adults with personality disorder: A pragmatic randomized-controlled trial. J Pers Disord. 2017;31(6):810–826. doi: 10.1521/pedi_2017_31_286. [DOI] [PubMed] [Google Scholar]
- 100.Clarke S, Kingston J, James K, Bolderston H, Remington B. Acceptance and commitment therapy group for treatment-resistant participants: A randomized controlled trial. J Contextual Behav Sci. 2014;3(3):179–188. [Google Scholar]
- 101.Clarke S, Thomas P, James K. Cognitive analytic therapy for personality disorder: randomised controlled trial. Br J Psychiatry. 2013;202(2):129–134. doi: 10.1192/bjp.bp.112.108670. [DOI] [PubMed] [Google Scholar]
- 102.Gratz K, Tull M, Levy R. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychol Med. 2013;44(10):2099. doi: 10.1017/S0033291713002134. [DOI] [PubMed] [Google Scholar]
- 103.Bos EH, Van Wel EB, Appelo MT, Verbraak MJ. Effectiveness of systems training for emotional predictability and problem solving (STEPPS) for borderline personality problems in a ‘real-world’sample: Moderation by diagnosis or severity? Psychother Psychosom. 2011;80(3):173–181. doi: 10.1159/000321793. [DOI] [PubMed] [Google Scholar]
- 104.Bos EH, van Wel EB, Appelo MT, Verbraak MJ. A randomized controlled trial of a Dutch version of systems training for emotional predictability and problem solving for borderline personality disorder. J Nerv Ment Dis. 2010;198(4):299–304. doi: 10.1097/NMD.0b013e3181d619cf. [DOI] [PubMed] [Google Scholar]
- 105.Davidson KM, Tyrer P, Norrie J, Palmer SJ, Tyrer H. Cognitive therapy v. usual treatment for borderline personality disorder: Prospective 6-year follow-up. Br J Psychiatry. 2010;197(6):456–462. doi: 10.1192/bjp.bp.109.074286. [DOI] [PubMed] [Google Scholar]
- 106.Farrell JM, Shaw IA, Webber MA. A schema-focused approach to group psychotherapy for outpatients with borderline personality disorder: A randomized controlled trial. J Behav Ther Exp Psychiatry. 2009;40(2):317–328. doi: 10.1016/j.jbtep.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 107.Blum N, St. John D, Pfohl B, Stuart S, McCormick B, Allen J, Arndt S, Black DW. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165(4):468–478. doi: 10.1176/appi.ajp.2007.07071079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, Palmer S. The effectiveness of cognitive behavior therapy for borderline personality disorder: Results from the borderline personality disorder study of cognitive therapy (BOSCOT) trial. J Pers Disord. 2006;20(5):450–465. doi: 10.1521/pedi.2006.20.5.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Emmelkamp PM, Benner A, Kuipers A, Feiertag GA, Koster HC, van Apeldoorn FJ. Comparison of brief dynamic and cognitive behavioural therapies in avoidant personality disorder. Br J Psychiatry. 2006;189(1):60–64. doi: 10.1192/bjp.bp.105.012153. [DOI] [PubMed] [Google Scholar]
- 110.Weinberg I, Gunderson JG, Hennen J, Cutter CJ., Jr Manual assisted cognitive treatment for deliberate self-harm in borderline personality disorder patients. J Pers Disord. 2006;20(5):482–492. doi: 10.1521/pedi.2006.20.5.482. [DOI] [PubMed] [Google Scholar]
- 111.Tyrer P, Tom B, Byford S, Schmidt U, Jones V, Davidson K, Knapp M, MacLeod A, Catalan J. Differential effects of manual assisted cognitive behavior therapy in the treatment of recurrent deliberate self-harm and personality disturbance: The POPMACT study. J Pers Disord. 2004;18(1):102–116. doi: 10.1521/pedi.18.1.102.32770. [DOI] [PubMed] [Google Scholar]
- 112.Alden L. Short-term structured treatment for avoidant personality disorder. J Consult Clin Psychol. 1989;57(6):756. doi: 10.1037//0022-006x.57.6.756. [DOI] [PubMed] [Google Scholar]
- 113.Popolo R, MacBeth A, Canfora F, Rebecchi D, Toselli C, Salvatore G, Dimaggio G. Metacognitive Interpersonal Therapy in group (MIT-G) for young adults with personality disorders: A pilot randomized controlled trial. Psychol Psychother Theory Res Pract. 2018;92(3):342–358. doi: 10.1111/papt.12182. [DOI] [PubMed] [Google Scholar]
- 114.Morton J, Snowdon S, Gopold M, Guymer E. Acceptance and commitment therapy group treatment for symptoms of borderline personality disorder: A public sector pilot study. Cogn Behav Pract. 2012;19(4):527–544. [Google Scholar]
- 115.Gratz KL, Gunderson JG. Preliminary data on an acceptance-based emotion regulation group intervention for deliberate self-harm among women with borderline personality disorder. Behav Ther. 2006;37(1):25–35. doi: 10.1016/j.beth.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 116.Evans K, Tyrer P, Catalan J, Schmidt U, Davidson K, Dent J, Tata P, Thornton S, Barber J, Thompson S. Manual-assisted cognitive-behaviour therapy (MACT): A randomized controlled trial of a brief intervention with bibliotherapy in the treatment of recurrent deliberate self-harm. Psychol Med. 1999;29(1):19–25. doi: 10.1017/s003329179800765x. [DOI] [PubMed] [Google Scholar]
- 117.MacIntosh HB, Cloitre M, Kortis K, Peck A, Weiss BJ. Implementation and evaluation of the skills training in affective and interpersonal regulation (STAIR) in a community setting in the context of childhood sexual abuse. Res Soc Work Pract. 2018;28(5):595–602. [Google Scholar]
- 118.Sahlin H, Bjureberg J, Gratz KL, Tull MT, Hedman E, Bjärehed J, Jokinen J, Lundh L-G, Ljótsson B, Hellner C. Emotion regulation group therapy for deliberate self-harm: A multi-site evaluation in routine care using an uncontrolled open trial design. BMJ Open. 2017;7(10):e016220. doi: 10.1136/bmjopen-2017-016220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hill N, Geoghegan M, Shawe-Taylor M. Evaluating the outcomes of the STEPPS programme in a UK community-based population; implications for the multidisciplinary treatment of borderline personality disorder. J Psychiatr Ment Health Nurs. 2016;23(6–7):347–356. doi: 10.1111/jpm.12315. [DOI] [PubMed] [Google Scholar]
- 120.Alesiani R, Boccalon S, Giarolli L, Blum N, Fossati A. Systems Training for Emotional Predictability and Problem Solving (STEPPS): Program efficacy and personality features as predictors of drop-out - An Italian study. Compr Psychiatry. 2014;55(4):920–927. doi: 10.1016/j.comppsych.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 121.Harvey R, Black DW, Blum N. Systems training for emotional predictability and problem solving (STEPPS) in the United Kingdom: A preliminary report. J Contemp Psychother. 2010;40(4):225–232. [Google Scholar]
- 122.Brown GK, Newman CF, Charlesworth SE, Crits-Christoph P, Beck AT. An open clinical trial of cognitive therapy for borderline personality disorder. J Personality Dis. 2004;18(3: Special issue):257–271. doi: 10.1521/pedi.18.3.257.35450. [DOI] [PubMed] [Google Scholar]
- 123.Ryle A, Golynkina K. Effectiveness of time-limited cognitive analytic therapy of borderline personality disorder: Factors associated with outcome. Br J Med Psychol. 2000;73(2):197–210. doi: 10.1348/000711200160426. [DOI] [PubMed] [Google Scholar]
- 124.Renneberg B, Goldstein AJ, Phillips D, Chambless DL. Intensive behavioral group treatment of avoidant personality disorder. Behav Ther. 1990;21(3):363–377. [Google Scholar]
- 125.Nordahl HM, Wells A. Metacognitive therapy of early traumatized patients with borderline personality disorder: A phase-II baseline controlled trial. Front Psychol. 2019;10:1694. doi: 10.3389/fpsyg.2019.01694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hall K, Simpson A, O'donnell R, Sloan E, Staiger PK, Morton J, Ryan D, Nunn B, Best D, Lubman DI. Emotional dysregulation as a target in the treatment of co-existing substance use and borderline personality disorders: A pilot study. Clin Psychol. 2018;22(2):112–125. [Google Scholar]
- 127.Mohammadi F, Bakhtiari M, Masjedi Arani A, Dolatshahi B, Habibi M: The applicability and efficacy of transdiagnostic cognitive behavior therapy on reducing signs and symptoms of borderline personality disorder with co-occurring emotional disorders: A pilot study. Iranian J Psychiatry Behavioral Sci. 2018, 12(1).
- 128.Sauer-Zavala S, Bentley KH, Wilner JG. Transdiagnostic treatment of borderline personality disorder and comorbid disorders: A clinical replication series. J Pers Disord. 2016;30(1):35–51. doi: 10.1521/pedi_2015_29_179. [DOI] [PubMed] [Google Scholar]
- 129.Videler A, Rossi G, Schoevaars M, Van der Feltz-Cornelis C, Van Alphen S. Effects of schema group therapy in older outpatients: A proof of concept study. Int Psychogeriatr. 2014;26(10):1709. doi: 10.1017/S1041610214001264. [DOI] [PubMed] [Google Scholar]
- 130.Kellett S, Bennett D, Ryle T, Thake A. Cognitive analytic therapy for borderline personality disorder: Therapist competence and therapeutic effectiveness in routine practice. Clin Psychol Psychother. 2013;20(3):216–225. doi: 10.1002/cpp.796. [DOI] [PubMed] [Google Scholar]
- 131.Lucre KM, Corten N. An exploration of group compassion-focused therapy for personality disorder. Psychol Psychother Theory Res Pract. 2013;86(4):387–400. doi: 10.1111/j.2044-8341.2012.02068.x. [DOI] [PubMed] [Google Scholar]
- 132.Renner F, van Goor M, Huibers M, Arntz A, Butz B, Bernstein D. Short-term group schema cognitive-behavioral therapy for young adults with personality disorders and personality disorder features: Associations with changes in symptomatic distress, schemas, schema modes and coping styles. Behav Res Ther. 2013;51(8):487–492. doi: 10.1016/j.brat.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 133.Clarke S, Kingston J, Wilson KG, Bolderston H, Remington B. Acceptance and commitment therapy for a heterogeneous group of treatment-resistant clients: A treatment development study. Cogn Behav Pract. 2012;19(4):560–572. [Google Scholar]
- 134.Ng RM. Cognitive therapy for obsessive-compulsive personality disorder - A pilot study in Hong Kong Chinese patients. Hong Kong J Psychiatry. 2005;15(2):50–54. [Google Scholar]
- 135.Wildgoose A, Clarke S, Waller G. Treating personality fragmentation and dissociation in borderline personality disorder: A pilot study of the impact of cognitive analytic therapy. Br J Med Psychol. 2001;74(1):47–55. [PubMed] [Google Scholar]
- 136.Cottraux J, Note ID, Boutitie F, Milliery M, Genouihlac V, Yao SN, Note B, Mollard E, Bonasse F, Gaillard S. Cognitive therapy versus Rogerian supportive therapy in borderline personality disorder. Psychother Psychosom. 2009;78(5):307–316. doi: 10.1159/000229769. [DOI] [PubMed] [Google Scholar]
- 137.Giesen-Bloo J, Van Dyck R, Spinhoven P, Van Tilburg W, Dirksen C, Van Asselt T, Kremers I, Nadort M, Arntz A. Outpatient psychotherapy for borderline personality disorder: Randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry. 2006;63(6):649–658. doi: 10.1001/archpsyc.63.6.649. [DOI] [PubMed] [Google Scholar]
- 138.Kallestad H, Valen J, McCullough L, Svartberg M, Høglend P, Stiles TC. The relationship between insight gained during therapy and long-term outcome in short-term dynamic psychotherapy and cognitive therapy for cluster C personality disorders. Psychother Res. 2010;20(5):526–534. doi: 10.1080/10503307.2010.492807. [DOI] [PubMed] [Google Scholar]
- 139.Svartberg M, Stiles TC, Seltzer MH. Randomized, controlled trial of the effectiveness of short-term dynamic psychotherapy and cognitive therapy for cluster C personality disorders. Am J Psychiatry. 2004;161(5):810–817. doi: 10.1176/appi.ajp.161.5.810. [DOI] [PubMed] [Google Scholar]
- 140.Chakhssi F, Janssen W, Pol SM, Van Dreumel M, Westerhof GJ. Acceptance and commitment therapy group-treatment for non-responsive patients with personality disorders: An exploratory study. Personal Ment Health. 2015;9(4):345–356. doi: 10.1002/pmh.1311. [DOI] [PubMed] [Google Scholar]
- 141.Horn EK, Bartak A, Meerman AM, Rossum BV, Ziegler UM, Thunnissen M, Soons M, Andrea H, Hamers EF, Emmelkamp PM. Effectiveness of psychotherapy in personality disorders not otherwise specified: A comparison of different treatment modalities. Clin Psychol Psychother. 2015;22(5):426–442. doi: 10.1002/cpp.1904. [DOI] [PubMed] [Google Scholar]
- 142.Ivaldi A, Fassone G, Rocchi M, Mantione G. The integrated model (individual and group treatment) of cognitive-evolutionary therapy for outpatients with borderline personality disorder and axis I/II comorbid disorders: outcome results and a single case report. Group. 2007;31(1/2):63–88. [Google Scholar]
- 143.Bentley KH, Nock MK, Sauer-Zavala S, Gorman BS, Barlow DH. A functional analysis of two transdiagnostic, emotion-focused interventions on nonsuicidal self-injury. J Consult Clin Psychol. 2017;85(6):632–646. doi: 10.1037/ccp0000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Salkovskis PM, Atha C, Storer D. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide a controlled trial. Br J Psychiatry. 1990;157(6):871–876. doi: 10.1192/bjp.157.6.871. [DOI] [PubMed] [Google Scholar]
- 145.Morey LC, Lowmaster SE, Hopwood CJ. A pilot study of manual-assisted cognitive therapy with a therapeutic assessment augmentation for borderline personality disorder. Psychiatry Res. 2010;178(3):531–535. doi: 10.1016/j.psychres.2010.04.055. [DOI] [PubMed] [Google Scholar]
- 146.Weertman A, Arntz A. Effectiveness of treatment of childhood memories in cognitive therapy for personality disorders: A controlled study contrasting methods focusing on the present and methods focusing on childhood memories. Behav Res Ther. 2007;45(9):2133–2143. doi: 10.1016/j.brat.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 147.Skewes SA, Samson RA, Simpson SG, van Vreeswijk M. Short-term group schema therapy for mixed personality disorders: A pilot study. Front Psychol. 2015;5:1592. doi: 10.3389/fpsyg.2014.01592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bamelis LL, Evers SM, Spinhoven P, Arntz A. Results of a multicenter randomized controlled trial of the clinical effectiveness of schema therapy for personality disorders. Am J Psychiatry. 2014;171(3):305–322. doi: 10.1176/appi.ajp.2013.12040518. [DOI] [PubMed] [Google Scholar]
- 149.Videler AC, van Alphen SP, van Royen RJ, van der Feltz-Cornelis CM, Rossi G, Arntz A. Schema therapy for personality disorders in older adults: A multiple-baseline study. Aging Ment Health. 2018;22(6):738–747. doi: 10.1080/13607863.2017.1318260. [DOI] [PubMed] [Google Scholar]
- 150.Fassbinder E, Schuetze M, Kranich A, Sipos V, Hohagen F, Shaw I, Farrell J, Arntz A, Schweiger U. Feasibility of group schema therapy for outpatients with severe borderline personality disorder in Germany: A pilot study with three year follow-up. Front Psychol. 1851;2016:7. doi: 10.3389/fpsyg.2016.01851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Dickhaut V, Arntz A. Combined group and individual schema therapy for borderline personality disorder: A pilot study. J Behav Ther Exp Psychiatry. 2014;45(2):242–251. doi: 10.1016/j.jbtep.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 152.Nordahl HM, Nysæter TE. Schema therapy for patients with borderline personality disorder: A single case series. J Behav Ther Exp Psychiatry. 2005;36(3):254–264. doi: 10.1016/j.jbtep.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 153.Nadort M, Arntz A, Smit JH, Giesen-Bloo J, Eikelenboom M, Spinhoven P, van Asselt T, Wensing M, van Dyck R. Implementation of outpatient schema therapy for borderline personality disorder with versus without crisis support by the therapist outside office hours: A randomized trial. Behav Res Ther. 2009;47(11):961–973. doi: 10.1016/j.brat.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 154.Bateman A, Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: mentalization-based treatment versus treatment as usual. Am J Psychiatry. 2008;165(5):631–638. doi: 10.1176/appi.ajp.2007.07040636. [DOI] [PubMed] [Google Scholar]
- 155.Bateman A, Fonagy P. Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: an 18-month follow-up. Am J Psychiatry. 2001;158(1):36–42. doi: 10.1176/appi.ajp.158.1.36. [DOI] [PubMed] [Google Scholar]
- 156.Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry. 1999;156(10):1563–1569. doi: 10.1176/ajp.156.10.1563. [DOI] [PubMed] [Google Scholar]
- 157.Beattie D, Murphy S, Jamieson S, Lee A. Running a mentalization-based treatment (MBT) programme within a public community adult mental health service setting: a feasibility study. Irish J Psychol Med. 2022;39(1):28–38. doi: 10.1017/ipm.2019.7. [DOI] [PubMed] [Google Scholar]
- 158.Carrera S, Pandolfi G, Cappelletti JY, Padoani W, Salcuni S. Oriented mentalization-based treatment for borderline personality disorder patients: preliminary results at camposampiero mental health center. Res Psychother. 2018;21(3):336. doi: 10.4081/ripppo.2018.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kvarstein EH, Pedersen G, Urnes Ø, Hummelen B, Wilberg T, Karterud S. Changing from a traditional psychodynamic treatment programme to mentalization-based treatment for patients with borderline personality disorder - Does it make a difference? Psychol Psychother Theory Res Pract. 2015;88(1):71–86. doi: 10.1111/papt.12036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Löf J, Clinton D, Kaldo V, Rydén G. Symptom, alexithymia and self-image outcomes of Mentalisation-based treatment for borderline personality disorder: A naturalistic study. BMC Psychiatry. 2018;18(1):1–9. doi: 10.1186/s12888-018-1699-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bales D, van Beek N, Smits M, Willemsen S, Busschbach JJ, Verheul R, Andrea H. Treatment outcome of 18-month, day hospital mentalization-based treatment (MBT) in patients with severe borderline personality disorder in the Netherlands. J Pers Disord. 2012;26(4):568–582. doi: 10.1521/pedi.2012.26.4.568. [DOI] [PubMed] [Google Scholar]
- 162.Petersen B, Toft J, Christensen NB, Foldager L, Munk-jørgensen P, Windfeld M, Frederiksen CK, Valbak K. A 2-year follow-up of mentalization-oriented group therapy following day hospital treatment for patients with personality disorders. Personal Ment Health. 2010;4(4):294–301. [Google Scholar]
- 163.Laurenssen E, Luyten P, Kikkert MJ, Westra D, Peen J, Soons MB, van Dam A-M, van Broekhuyzen AJ, Blankers M, van Busschbach J. Day hospital mentalization-based treatment versus specialist treatment as usual in patients with borderline personality disorder: Randomized controlled trial. Psychol Med. 2018;48(15):2522–2529. doi: 10.1017/S0033291718000132. [DOI] [PubMed] [Google Scholar]
- 164.Jørgensen C, Freund C, Bøye R, Jordet H, Andersen D, Kjølbye M. Outcome of mentalization-based and supportive psychotherapy in patients with borderline personality disorder: A randomized trial. Acta Psychiatr Scand. 2013;127(4):305–317. doi: 10.1111/j.1600-0447.2012.01923.x. [DOI] [PubMed] [Google Scholar]
- 165.Jørgensen CR, Bøye R, Andersen D, Døssing Blaabjerg AH, Freund C, Jordet H, Kjølbye M. Eighteen months post-treatment naturalistic follow-up study of mentalization-based therapy and supportive group treatment of borderline personality disorder: Clinical outcomes and functioning. Nordic Psychol. 2014;66(4):254–273. [Google Scholar]
- 166.Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1355–1364. doi: 10.1176/appi.ajp.2009.09040539. [DOI] [PubMed] [Google Scholar]
- 167.Bales DL, Timman R, Andrea H, Busschbach JJ, Verheul R, Kamphuis JH. Effectiveness of day hospital mentalization-based treatment for patients with severe borderline personality disorder: A matched control study. Clin Psychol Psychother. 2015;22(5):409–417. doi: 10.1002/cpp.1914. [DOI] [PubMed] [Google Scholar]
- 168.Jones B, Juett G, Hill N. A two-model integrated personality disorder service: two-year follow up of effect upon psychiatric bed use. Therapeutic Commun Int J Therapeutic Commun. 2013;34(2/3):104–111. [Google Scholar]
- 169.Jones B, Juett G, Hill N. Initial outcomes of a therapeutic community-based outpatient programme in the management of personality disorder. Therapeutic Commun Int J Therapeutic Commun. 2013;34(1):41–52. [Google Scholar]
- 170.Jones B, Juett G, Hill N. A two-model integrated personality disorder service: effect on bed use. Psychiatrist. 2012;36(8):293–298. [Google Scholar]
- 171.Smits ML, Feenstra DJ, Eeren HV, Bales DL, Laurenssen EM, Blankers M, Soons MB, Dekker JJ, Lucas Z, Verheul R. Day hospital versus intensive out-patient mentalisation-based treatment for borderline personality disorder: Multicentre randomised clinical trial. Br J Psychiatry. 2020;216(2):79–84. doi: 10.1192/bjp.2019.9. [DOI] [PubMed] [Google Scholar]
- 172.Reneses B, Galian M, Serrano R, Figuera D. Fernandez del Moral A, López-Ibor JJ, Fuentes M, Trujillo M: A new time limited psychotherapy for BPD: Preliminary results of a randomized and controlled trial. Actas Esp Psiquiatr. 2013;41(3):139–48. [PubMed] [Google Scholar]
- 173.Abbass A, Sheldon A, Gyra J, Kalpin A. Intensive short-term dynamic psychotherapy for DSM-IV personality disorders: A randomized controlled trial. J Nerv Ment Dis. 2008;196(3):211–216. doi: 10.1097/NMD.0b013e3181662ff0. [DOI] [PubMed] [Google Scholar]
- 174.Vinnars B, Barber JP, Norén K, Gallop R, Weinryb RM. Manualized supportive-expressive psychotherapy versus nonmanualized community-delivered psychodynamic therapy for patients with personality disorders: bridging efficacy and effectiveness. Am J Psychiatry. 2005;162(10):1933–1940. doi: 10.1176/appi.ajp.162.10.1933. [DOI] [PubMed] [Google Scholar]
- 175.Winston A, Laikin M, Pollack J, Wallner Samstag L, McCullough L, Muran JC. Short-term psychotherapy of personality disorders. Am J Psychiatry. 1994;151(2):190–194. doi: 10.1176/ajp.151.2.190. [DOI] [PubMed] [Google Scholar]
- 176.Piper WE, Rosie JS, Azim HF, Joyce AS. A randomized trial of psychiatric day treatment for patients with affective and personality disorders. Psychiatr Serv. 1993;44(8):757–763. doi: 10.1176/ps.44.8.757. [DOI] [PubMed] [Google Scholar]
- 177.Chiesa M, Luyten P, Fonagy P. Two-year follow-up and changes in reflective functioning in specialist and nonspecialist treatment models for personality disorder. Personal Disord: Theory, Research, and Treatment. 2020;12(3):249–260. doi: 10.1037/per0000464. [DOI] [PubMed] [Google Scholar]
- 178.Kealy D, Joyce AS, Weber R, Ehrenthal JC, Ogrodniczuk JS. What the patient wants: Addressing patients’ treatment targets in an integrative group psychotherapy programme. Psychol Psychother Theory Res Pract. 2019;92(1):20–38. doi: 10.1111/papt.12174. [DOI] [PubMed] [Google Scholar]
- 179.Joyce AS, Ogrodniczuk JS, Kealy D. Intensive evening outpatient treatment for patients with personality dysfunction: Early group process, change in interpersonal distress, and longer-term social functioning. Psychiatry. 2017;80(2):184–195. doi: 10.1080/00332747.2016.1230985. [DOI] [PubMed] [Google Scholar]
- 180.Kvarstein EH, Nordviste O, Dragland L, Wilberg T. Outpatient psychodynamic group psychotherapy–outcomes related to personality disorder, severity, age and gender. Personal Ment Health. 2017;11(1):37–50. doi: 10.1002/pmh.1352. [DOI] [PubMed] [Google Scholar]
- 181.Stevenson J, Haliburn J, Halovic S. Trauma, personality disorders and chronic depression - the role of the conversational model of psychodynamic psychotherapy in treatment resistant depression. Psychoanal Psychother. 2015;30(1):23–41. [Google Scholar]
- 182.Joyce AS, Stovel LE, Ogrodniczuk JS, Fujiwara E. Defense style as a predictor of change in interpersonal problems among patients attending day treatment for personality disorder. Psychodynamic Psychiatry. 2013;41(4):597–617. doi: 10.1521/pdps.2013.41.4.597. [DOI] [PubMed] [Google Scholar]
- 183.Berghout CC, Zevalkink J, Katzko MW, de Jong JT. Changes in symptoms and interpersonal problems during the first 2 years of long-term psychoanalytic psychotherapy and psychoanalysis. Psychol Psychother Theory Res Pract. 2012;85(2):203–219. doi: 10.1111/j.2044-8341.2011.02022.x. [DOI] [PubMed] [Google Scholar]
- 184.Berghout CC, Zevalkink J. Clinical significance of long-term psychoanalytic treatment. Bull Menninger Clin. 2009;73(1):7–33. doi: 10.1521/bumc.2009.73.1.7. [DOI] [PubMed] [Google Scholar]
- 185.Chiesa M, Fonagy P, Gordon J. Community-based psychodynamic treatment program for severe personality disorders: Clinical description and naturalistic evaluation. J Psychiatr Pract. 2009;15(1):12–24. doi: 10.1097/01.pra.0000344915.61706.d4. [DOI] [PubMed] [Google Scholar]
- 186.Joyce AS, Ennis LP, O'Kelly JG, Ogrodniczuk JS, Piper WE. Depressive manifestations and differential patterns of treatment outcome in an intensive partial hospitalization treatment program. Psychol Serv. 2009;6(2):154. [Google Scholar]
- 187.Gerull F, Meares R, Stevenson J, Korner A, Newman L. The beneficial effect on family life in treating borderline personality. Psychiatry. 2008;71(1):59–70. doi: 10.1521/psyc.2008.71.1.59. [DOI] [PubMed] [Google Scholar]
- 188.Korner A, Gerull F, Meares R, Stevenson J. The nothing that is something: Core dysphoria as the central feature of borderline personality disorder Implications for treatment. Am J Psychother. 2008;62(4):377–394. doi: 10.1176/appi.psychotherapy.2008.62.4.377. [DOI] [PubMed] [Google Scholar]
- 189.Petersen B, Toft J, Christensen NB, Foldager L, Munk-Jörgensen P, Lien K, Valbak K. Outcome of a psychotherapeutic programme for patients with severe personality disorders. Nord J Psychiatry. 2008;62(6):450–456. doi: 10.1080/08039480801984271. [DOI] [PubMed] [Google Scholar]
- 190.Jørgensen CR, Kjølbye M. Outcome of psychoanalytically oriented outpatient treatment of borderline personality disorder. Nordic Psychology. 2007;59(2):164–180. [Google Scholar]
- 191.Korner A, Gerull F, Meares R, Stevenson J. Borderline personality disorder treated with the conversational model: A replication study. Compr Psychiatry. 2006;47(5):406–411. doi: 10.1016/j.comppsych.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 192.Stevenson J, Meares R, D'angelo R. Five-year outcome of outpatient psychotherapy with borderline patients. Psychol Med. 2005;35(1):79. doi: 10.1017/s0033291704002788. [DOI] [PubMed] [Google Scholar]
- 193.Wilberg T, Karterud S, Pedersen G, Urnes Ø, Irion T, Brabrand J, Haavaldsen G, Leirvåg H, Johnsen K, Andreasen H. Outpatient group psychotherapy following day treatment for patients with personality disorders. J Pers Disord. 2003;17(6):510–521. doi: 10.1521/pedi.17.6.510.25357. [DOI] [PubMed] [Google Scholar]
- 194.Lorentzen S, Bøgwald KP, Høglend P. Change during and after long-term analytic group psychotherapy. Int J Group Psychother. 2002;52(3):419–429. doi: 10.1521/ijgp.52.3.419.45511. [DOI] [PubMed] [Google Scholar]
- 195.Cookson A, Espie J, Yates K. The Edinburgh Project: A pilot study for the psychotherapeutic treatment of borderline and other severe personality disorders. Br J Psychother. 2001;18(1):68–88. [Google Scholar]
- 196.Meares R, Stevenson J, Comerford A. Psychotherapy with borderline patients: I. A comparison between treated and untreated cohorts. Aust N Z J Psychiatry. 1999;33(4):467–472. doi: 10.1080/j.1440-1614.1999.00594.x. [DOI] [PubMed] [Google Scholar]
- 197.Barber JP, Morse JQ, Krakauer ID, Chittams J, Crits-Christoph K. Change in obsessive-compulsive and avoidant personality disorders following time-limited supportive-expressive therapy. Psychother Theory Res Pract Training. 1997;34(2):133. [Google Scholar]
- 198.Monsen J, Odland T, Faugli A, Daae E, Eilertsen D. Personality disorders: Changes and stability after intensive psychotherapy focusing on affect consciousness. Psychother Res. 1995;5(1):33–48. [Google Scholar]
- 199.Monsen J, Odland T, Faugli A, Daae E, Eilertsen DE. Personality disorders and psychosocial changes after intensive psychotherapy: A prospective follow-up study of an outpatient psychotherapy project, 5 years after end of treatment. Scand J Psychol. 1995;36(3):256–268. doi: 10.1111/j.1467-9450.1995.tb00985.x. [DOI] [PubMed] [Google Scholar]
- 200.Karterud S, Vaglum S, Friis S, Irion T, Johns S, Vaglum P. Day hospital therapeutic community treatment for patients with personality disorders: An empirical evaluation of the containment function. J Nerv Ment Dis. 1992;180(4):238–43. doi: 10.1097/00005053-199204000-00005. [DOI] [PubMed] [Google Scholar]
- 201.Meares R, Stevenson J. An outcome study of psychotherapy for patients with borderline personality disorder. Am J Psychiatry. 1992;149(3):358–362. doi: 10.1176/ajp.149.3.358. [DOI] [PubMed] [Google Scholar]
- 202.Clarkin JF, Foelsch PA, Levy KN, Hull JW, Delaney JC, Kernberg OF. The development of a psychodynamic treatment for patients with borderline personality disorder: A preliminary study of behavioral change. J Pers Disord. 2001;15(6):487–495. doi: 10.1521/pedi.15.6.487.19190. [DOI] [PubMed] [Google Scholar]
- 203.Berthoud L, Pascual-Leone A, Caspar F, Tissot H, Keller S, Rohde KB, de Roten Y, Despland J-N, Kramer U. Leaving distress behind: A randomized controlled study on change in emotional processing in borderline personality disorder. Psychiatry. 2017;80(2):139–154. doi: 10.1080/00332747.2016.1220230. [DOI] [PubMed] [Google Scholar]
- 204.Kramer U, Stulz N, Berthoud L, Caspar F, Marquet P, Kolly S, De Roten Y, Despland J-N. The shorter the better? A follow-up analysis of 10-session psychiatric treatment including the motive-oriented therapeutic relationship for borderline personality disorder. Psychother Res. 2017;27(3):362–370. doi: 10.1080/10503307.2015.1110635. [DOI] [PubMed] [Google Scholar]
- 205.Kramer U, Kolly S, Berthoud L, Keller S, Preisig M, Caspar F, Berger T, De Roten Y, Marquet P, Despland J-N. Effects of motive-oriented therapeutic relationship in a ten-session general psychiatric treatment of borderline personality disorder: A randomized controlled trial. Psychother Psychosom. 2014;83(3):176–186. doi: 10.1159/000358528. [DOI] [PubMed] [Google Scholar]
- 206.Kramer U, Berger T, Kolly S, Marquet P, Preisig M, de Roten Y, Despland J-N, Caspar F. Effects of motive-oriented therapeutic relationship in early-phase treatment of borderline personality disorder: A pilot study of a randomized trial. J Nerv Ment Dis. 2011;199(4):244–250. doi: 10.1097/NMD.0b013e3182125d19. [DOI] [PubMed] [Google Scholar]
- 207.Hellerstein DJ, Rosenthal RN, Pinsker H, Samstag LW, Muran JC, Winston A. A randomized prospective study comparing supportive and dynamic therapies: Outcome and alliance. J Psychother Pract Res. 1998;7(4):261. [PMC free article] [PubMed] [Google Scholar]
- 208.Penzenstadler L, Kolly S, Rothen S, Khazaal Y, Kramer U. Effects of substance use disorder on treatment process and outcome in a ten-session psychiatric treatment for borderline personality disorder. Subst Abuse Treat Prev Policy. 2018;13(1):1–11. doi: 10.1186/s13011-018-0145-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Van Manen JG, Horn EK, Stijnen T, Timman R, Busschbach JJ, Verheul R. Tailoring psychotherapy in patients with personality disorders: Matching the level of psychological strengths to the level of stabilizing versus destabilizing psychotherapy. Personal Ment Health. 2015;9(2):133–149. doi: 10.1002/pmh.1281. [DOI] [PubMed] [Google Scholar]
- 210.Sachdeva S, Goldman G, Mustata G, Deranja E, Gregory RJ. Naturalistic outcomes of evidence-based therapies for borderline personality disorder at a university clinic: A quasi-randomized trial. J Am Psychoanal Assoc. 2013;61(3):578–584. doi: 10.1177/0003065113490637. [DOI] [PubMed] [Google Scholar]
- 211.Wilberg T, Friis S, Karterud S, Mehlum L, Urnes Ø, Vaglum P. Outpatient group psychotherapy: A valuable continuation treatment for patients with borderline personality disorder treated in a day hospital? A 3-year follow-up study. Nord J Psychiatry. 1998;52(3):213–221. [Google Scholar]
- 212.Chiesa M, Cirasola A, Fonagy P. Four years comparative follow-up evaluation of community-based, step-down, and residential specialist psychodynamic programmes for personality disorders. Clin Psychol Psychother. 2017;24(6):1331–1342. doi: 10.1002/cpp.2109. [DOI] [PubMed] [Google Scholar]
- 213.Bartak A, Andrea H, Spreeuwenberg MD, Ziegler UM, Dekker J, Rossum BV, Hamers EF, Scholte W, Aerts J, Busschbach JJ. Effectiveness of outpatient, day hospital, and inpatient psychotherapeutic treatment for patients with cluster B personality disorders. Psychother Psychosom. 2011;80(1):28–38. doi: 10.1159/000321999. [DOI] [PubMed] [Google Scholar]
- 214.Bartak A, Spreeuwenberg MD, Andrea H, Holleman L, Rijnierse P, Rossum BV, Hamers EF, Meerman AM, Aerts J, Busschbach JJ. Effectiveness of different modalities of psychotherapeutic treatment for patients with cluster C personality disorders: results of a large prospective multicentre study. Psychother Psychosom. 2010;79(1):20–30. doi: 10.1159/000254902. [DOI] [PubMed] [Google Scholar]
- 215.Chiesa M, Fonagy P, Holmes J, Drahorad C. Residential versus community treatment of personality disorders: A comparative study of three treatment programs. Am J Psychiatry. 2004;161(8):1463–1470. doi: 10.1176/appi.ajp.161.8.1463. [DOI] [PubMed] [Google Scholar]
- 216.Chiesa M, Bateman A, Wilberg T, Friis S. Patients' characteristics, outcome and cost-benefit of hospital-based treatment for patients with personality disorder: A comparison of three different programmes. Psychol Psychother Theory Res Pract. 2002;75(4):381–392. doi: 10.1348/147608302321151899. [DOI] [PubMed] [Google Scholar]
- 217.Gregory RJ, DeLucia-Deranja E, Mogle JA. Dynamic deconstructive psychotherapy versus optimized community care for borderline personality disorder co-occurring with alcohol use disorders: A 30-month follow-up. J Nerv Ment Dis. 2010;198(4):292–298. doi: 10.1097/NMD.0b013e3181d6172d. [DOI] [PubMed] [Google Scholar]
- 218.Gregory RJ, Chlebowski S, Kang D, Remen AL, Soderberg MG, Stepkovitch J, Virk S. A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychotherapy (Chic) 2008;45(1):28. doi: 10.1037/0033-3204.45.1.28. [DOI] [PubMed] [Google Scholar]
- 219.Ridolfi ME, Rossi R, Occhialini G, Gunderson JG. A clinical trial of a psychoeducation group intervention for patients with borderline personality disorder. J Clin Psychiatry. 2019;81(1):0–0. doi: 10.4088/JCP.19m12753. [DOI] [PubMed] [Google Scholar]
- 220.Leppänen V, Hakko H, Sintonen H, Lindeman S. Comparing effectiveness of treatments for borderline personality disorder in communal mental health care: The Oulu BPD Study. Community Ment Health J. 2016;52(2):216–227. doi: 10.1007/s10597-015-9866-4. [DOI] [PubMed] [Google Scholar]
- 221.Amianto F, Ferrero A, Pierò A, Cairo E, Rocca G, Simonelli B, Fassina S, Abbate-Daga G, Fassino S. Supervised team management, with or without structured psychotherapy, in heavy users of a mental health service with borderline personality disorder: a two-year follow-up preliminary randomized study. BMC Psychiatry. 2011;11(1):1–14. doi: 10.1186/1471-244X-11-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Doering S, Hörz S, Rentrop M, Fischer-Kern M, Schuster P, Benecke C, Buchheim A, Martius P, Buchheim P. Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: Randomised controlled trial. Br J Psychiatry. 2010;196(5):389–395. doi: 10.1192/bjp.bp.109.070177. [DOI] [PubMed] [Google Scholar]
- 223.Savard C, Chrétien M, Gamache D, Maranda J, Villeneuve E. Effectiveness of a 6-week day hospital treatment for personality disorders: Data from a naturalistic study. J Psychiatr Pract. 2019;25(3):199–205. doi: 10.1097/PRA.0000000000000382. [DOI] [PubMed] [Google Scholar]
- 224.Lana F, Sánchez-Gil C, Ferrer L, López-Patón N, Litvan L, Marcos S, Sierra AC, Soldevilla JM, Feixas G, Pérez V. Effectiveness of an integrated treatment for severe personality disorders. A 36-month pragmatic follow-up. Revista de Psiquiatría y Salud Mental (English Edition) 2015;8(1):3–10. doi: 10.1016/j.rpsm.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 225.Nysæter TE, Nordahl HM, Havik OE. A preliminary study of the naturalistic course of non-manualized psychotherapy for outpatients with borderline personality disorder: Patient characteristics, attrition and outcome. Nord J Psychiatry. 2010;64(2):87–93. doi: 10.3109/08039480903406731. [DOI] [PubMed] [Google Scholar]
- 226.Halsteinli V, Karterud S, Pedersen G. When costs count: The impact of staff size, skill mix and treatment intensity on patient outcome for psychotherapeutic day treatment programmes. Health Policy. 2008;86(2–3):255–265. doi: 10.1016/j.healthpol.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 227.Karterud S, Pedersen G, Bjordal E, Brabrand J, Friis S, Haaseth Ø, Haavaldsen G, Irion T, Leirvåg H, Tørum E. Day treatment of patients with personality disorders: Experiences from a Norwegian treatment research network. J Pers Disord. 2003;17(3):243–262. doi: 10.1521/pedi.17.3.243.22151. [DOI] [PubMed] [Google Scholar]
- 228.Wilberg T, Urnes Ø, Friis S, Irion T, Pedersen G, Karterud S. One-year follow-up of day treatment for poorly functioning patients with personality disorders. Psychiatr Serv. 1999;50(10):1326–1330. doi: 10.1176/ps.50.10.1326. [DOI] [PubMed] [Google Scholar]
- 229.Kvarstein EH, Arnevik E, Halsteinli V, Rø FG, Karterud S, Wilberg T. Health service costs and clinical gains of psychotherapy for personality disorders: a randomized controlled trial of day-hospital-based step-down treatment versus outpatient treatment at a specialist practice. BMC Psychiatry. 2013;13(1):1–13. doi: 10.1186/1471-244X-13-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Haeyen S, van Hooren S, van der Veld W, Hutschemaekers G. Efficacy of art therapy in individuals with personality disorders cluster B/C: A randomized controlled trial. J Pers Disord. 2018;32(4):527–542. doi: 10.1521/pedi_2017_31_312. [DOI] [PubMed] [Google Scholar]
- 231.Andreoli A, Burnand Y, Cochennec M-F, Ohlendorf P, Frambati L, Gaudry-Maire D, Di Clemente T, Hourton G, Lorillard S, Canuto A. Disappointed love and suicide: a randomized controlled trial of “abandonment psychotherapy” among borderline patients. J Pers Disord. 2016;30(2):271–287. doi: 10.1521/pedi_2015_29_196. [DOI] [PubMed] [Google Scholar]
- 232.Leirvåg H, Pedersen G, Karterud S. Long-term continuation treatment after short-term day treatment of female patients with severe personality disorders: Body awareness group therapy versus psychodynamic group therapy. Nord J Psychiatry. 2010;64(2):115–122. doi: 10.3109/08039480903487525. [DOI] [PubMed] [Google Scholar]
- 233.Zanarini MC, Frankenburg FR. A preliminary, randomized trial of psychoeducation for women with borderline personality disorder. J Pers Disord. 2008;22(3):284–290. doi: 10.1521/pedi.2008.22.3.284. [DOI] [PubMed] [Google Scholar]
- 234.Cameron LD, Carroll P, Hamilton WK. Evaluation of an intervention promoting emotion regulation skills for adults with persisting distress due to adverse childhood experiences. Child Abuse Negl. 2018;79:423–433. doi: 10.1016/j.chiabu.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 235.Pascual JC, Palomares N, Ibáñez Á, Portella MJ, Arza R, Reyes R, Feliu-Soler A, Díaz-Marsá M, Saiz-Ruiz J, Soler J. Efficacy of cognitive rehabilitation on psychosocial functioning in borderline personality disorder: A randomized controlled trial. BMC Psychiatry. 2015;15(1):1–9. doi: 10.1186/s12888-015-0640-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Huband N, McMurran M, Evans C, Duggan C. Social problem-solving plus psychoeducation for adults with personality disorder: pragmatic randomised controlled trial. Br J Psychiatry. 2007;190(4):307–313. doi: 10.1192/bjp.bp.106.023341. [DOI] [PubMed] [Google Scholar]
- 237.Munroe-Blum H, Marziali E. A controlled trial of short-term group treatment for borderline personality disorder. J Pers Disord. 1995;9(3):190–198. [Google Scholar]
- 238.Di Simplicio M, Appiah-Kusi E, Wilkinson P, Watson P, Meiser-Stedman C, Kavanagh DJ, Holmes EA. Imaginator: A proof-of-concept feasibility trial of a brief imagery-based psychological intervention for young people who self-Harm. Suicide and Life Threat Behav. 2020;50(3):724–740. doi: 10.1111/sltb.12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Stravynski A, Belisle M, Marcouiller M, Lavallée Y-J, Eue R. The treatment of avoidant personality disorder by social skills training in the clinic or in real-life settings. Can J Psychiatry. 1994;39(8):377–383. doi: 10.1177/070674379403900805. [DOI] [PubMed] [Google Scholar]
- 240.De Saeger H, Kamphuis JH, Finn SE, Smith JD, Verheul R, van Busschbach JJ, Feenstra DJ, Horn EK. Therapeutic assessment promotes treatment readiness but does not affect symptom change in patients with personality disorders: Findings from a randomized clinical trial. Psychol Assess. 2014;26(2):474. doi: 10.1037/a0035667. [DOI] [PubMed] [Google Scholar]
- 241.Borschmann R, Barrett B, Hellier JM, Byford S, Henderson C, Rose D, Slade M, Sutherby K, Szmukler G, Thornicroft G. Joint crisis plans for people with borderline personality disorder: feasibility and outcomes in a randomised controlled trial. Br J Psychiatry. 2013;202(5):357–364. doi: 10.1192/bjp.bp.112.117762. [DOI] [PubMed] [Google Scholar]
- 242.Ranger M, Tyrer P, Miloseska K, Fourie H, Khaleel I, North B, Barrett B. Cost-effectiveness of nidotherapy for comorbid personality disorder and severe mental illness: Randomized controlled trial. Epidemiol Psychiatric Sci. 2009;18(2):128–136. [PubMed] [Google Scholar]
- 243.Graham S, Sullivan K, Briggs L, Goodall M, Iraci Capucinello R. A preliminary service evaluation of a personality disorder case management service. Personal Ment Health. 2019;13(2):65–74. doi: 10.1002/pmh.1439. [DOI] [PubMed] [Google Scholar]
- 244.Solberg JJ, Deyo-Svendsen ME, Nylander KR, Bruhl EJ, Heredia D, Jr, Angstman KB. Collaborative care management associated with improved depression outcomes in patients with personality disorders, compared to usual primary care. J Prim Care Community Health. 2018;9:2150132718773266. doi: 10.1177/2150132718773266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Stringer B, van Meijel B, Karman P, Koekkoek B, Hoogendoorn A, Kerkhof A, et al. Feasibility and preliminary results of a Collaborative Care program for patients with severe personality disorders: a comparative multiple case study. https://www.semanticscholar.org/paper/Feasibility-and-preliminary-results-of-a-Care-for-Stringer-Meijel/f06a4c0474bb3542bc544195e72fbc97ae3d043a.
- 246.Antonsen BT, Kvarstein EH, Urnes Ø, Hummelen B, Karterud S, Wilberg T. Favourable outcome of long-term combined psychotherapy for patients with borderline personality disorder: Six-year follow-up of a randomized study. Psychother Res. 2017;27(1):51–63. doi: 10.1080/10503307.2015.1072283. [DOI] [PubMed] [Google Scholar]
- 247.Antonsen BT, Klungsøyr O, Kamps A, Hummelen B, Johansen MS, Pedersen G, Urnes Ø, Kvarstein EH, Karterud S, Wilberg T. Step-down versus outpatient psychotherapeutic treatment for personality disorders: 6-year follow-up of the Ullevål personality project. BMC Psychiatry. 2014;14(1):1–12. doi: 10.1186/1471-244X-14-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Gullestad FS, Wilberg T, Klungsøyr O, Johansen MS, Urnes Ø, Karterud S. Is treatment in a day hospital step-down program superior to outpatient individual psychotherapy for patients with personality disorders? 36 months follow-up of a randomized clinical trial comparing different treatment modalities. Psychother Res. 2012;22(4):426–441. doi: 10.1080/10503307.2012.662608. [DOI] [PubMed] [Google Scholar]
- 249.Arnevik E, Wilberg T, Urnes Ø, Johansen M, Monsen JT, Karterud S. Psychotherapy for personality disorders: 18 months' follow-up of the Ullevål Personality Project. J Pers Disord. 2010;24(2):188–203. doi: 10.1521/pedi.2010.24.2.188. [DOI] [PubMed] [Google Scholar]
- 250.Arnevik E, Wilberg T, Urnes Ø, Johansen M, Monsen JT, Karterud S. Psychotherapy for personality disorders: Short-term day hospital psychotherapy versus outpatient individual therapy - a randomized controlled study. Eur Psychiatry. 2009;24(2):71–78. doi: 10.1016/j.eurpsy.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 251.Grenyer BF, Lewis KL, Fanaian M, Kotze B. Treatment of personality disorder using a whole of service stepped care approach: A cluster randomized controlled trial. PLoS ONE. 2018;13(11):e0206472. doi: 10.1371/journal.pone.0206472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Pearce S, Scott L, Attwood G, Saunders K, Dean M, De Ridder R, Galea D, Konstantinidou H, Crawford M. Democratic therapeutic community treatment for personality disorder: Randomised controlled trial. Br J Psychiatry. 2017;210(2):149–156. doi: 10.1192/bjp.bp.116.184366. [DOI] [PubMed] [Google Scholar]
- 253.Huxley E, Lewis KL, Coates AD, Borg WM, Miller CE, Townsend ML, Grenyer BF. Evaluation of a brief intervention within a stepped care whole of service model for personality disorder. BMC Psychiatry. 2019;19(1):1–12. doi: 10.1186/s12888-019-2308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Laporte L, Paris J, Bergevin T, Fraser R, Cardin JF. Clinical outcomes of a stepped care program for borderline personality disorder. Personal Ment Health. 2018;12(3):252–264. doi: 10.1002/pmh.1421. [DOI] [PubMed] [Google Scholar]
- 255.Barr W, Kirkcaldy A, Horne A, Hodge S, Hellin K, Göpfert M. Quantitative findings from a mixed methods evaluation of once-weekly therapeutic community day services for people with personality disorder. J Ment Health. 2010;19(5):412–421. doi: 10.3109/09638230903469145. [DOI] [PubMed] [Google Scholar]
- 256.Miller S, Crawford MJ. Open access community support groups for people with personality disorder: Attendance and impact on use of other services. Psychiatrist. 2010;34(5):177–181. [Google Scholar]
- 257.Pretorius JL, Albeniz A, Broome M. Olive Tree community treatment centre for individuals with personality disorder: Naturalistic service evaluation. Psychiatrist. 2010;34(1):12–20. [Google Scholar]
- 258.Scott L, Kemp E. Personality disorder in later life: no longer a diagnosis of exclusion. Mental Health Rev J. 2010;15(4):63–70. [Google Scholar]
- 259.Dingfelder SF. Treatment for the untreatable. Monit Psychol. 2004;35(3):46–50. [Google Scholar]
- 260.Simonsen S, Bateman A, Bohus M, Dalewijk HJ, Doering S, Kaera A, Moran P, Renneberg B, Ribaudi JS, Taubner S. European guidelines for personality disorders: past, present and future. Borderline Personal Disord Emot Dysregul. 2019;6(1):1–10. doi: 10.1186/s40479-019-0106-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Chanen A, Sharp C, Hoffman P. for Prevention GA: Prevention and early intervention for borderline personality disorder: a novel public health priority. World Psychiatry. 2017;16(2):215. doi: 10.1002/wps.20429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Foye U, Stuart R, Trevillion K, Oram S, Allan D, Broecklemann E, et al. Clinician views on best practice community care for people with complex emotional needs and how it can be achieved: a qualitative study. medRxiv. 2021. [DOI] [PMC free article] [PubMed]
- 263.Katsakou C, Marougka S, Barnicot K, Savill M, White H, Lockwood K, Priebe S. Recovery in borderline personality disorder (BPD): a qualitative study of service users' perspectives. PLoS ONE. 2012;7(5):e36517. doi: 10.1371/journal.pone.0036517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Lambert N, Carr S. ‘Outside the Original Remit’: Co-production in UK mental health research, lessons from the field. Int J Ment Health Nurs. 2018;27(4):1273–1281. doi: 10.1111/inm.12499. [DOI] [PubMed] [Google Scholar]
- 265.Walker P, Kulkarni J. We need to treat borderline personality disorder for what it really is – a response to trauma. 2019. [Google Scholar]
- 266.Reich DB, Zanarini MC. Sexual orientation and relationship choice in borderline personality disorder over ten years of prospective follow-up. J Pers Disord. 2008;22(6):564–572. doi: 10.1521/pedi.2008.22.6.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Reuter TR, Sharp C, Kalpakci AH, Choi HJ, Temple JR. Sexual orientation and borderline personality disorder features in a community sample of adolescents. J Pers Disord. 2016;30(5):694–707. doi: 10.1521/pedi_2015_29_224. [DOI] [PubMed] [Google Scholar]
- 268.Alvarez-Tomás I, Soler J, Bados A, Martín-Blanco A, Elices M, Carmona C, Bauzà J, Pascual JC. Long-term course of borderline personality disorder: a prospective 10-year follow-up study. J Pers Disord. 2017;31(5):590–605. doi: 10.1521/pedi_2016_30_269. [DOI] [PubMed] [Google Scholar]
- 269.Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, Zanarini MC, Yen S, Markowitz JC, Sanislow C. Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Arch Gen Psychiatry. 2011;68(8):827–837. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Newton-Howes G, Tyrer P, Anagnostakis K, Cooper S, Bowden-Jones O, Weaver T. The prevalence of personality disorder, its comorbidity with mental state disorders, and its clinical significance in community mental health teams. Soc Psychiatry Psychiatr Epidemiol. 2010;45(4):453–460. doi: 10.1007/s00127-009-0084-7. [DOI] [PubMed] [Google Scholar]
- 271.Woelbert E, Kirtley A, Balmer N, Dix S. How much is spent on mental health research: developing a system for categorising grant funding in the UK. Lancet Psychiatry. 2019;6(5):445–452. doi: 10.1016/S2215-0366(19)30033-1. [DOI] [PubMed] [Google Scholar]
- 272.StopSIM Coalition Consensus Statement [https://stopsim.co.uk/2021/04/21/stopsim-coalition-consensus-statement/]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix 1. Search strategy. Appendix 2. Dialectical Behavioural Therapy (DBT) treatments. Appendix 3. Cognitive and Behavioural Therapy and Schema Therapy treatments. Appendix 4. MBT and Psychodynamic Therapy treatments. Appendix 5. Other treatments. Appendix 6. Table of studies testing Dialectical Behavioural Therapy (DBT) treatments. Appendix 7. Table of studies testing Cognitive and Behavioural Therapy and Schema Therapy treatments. Appendix 8. Table of studies testing MBT and Psychodynamic Therapy treatments. Appendix 9. Table of studies testing other treatments.
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].