Abstract
Monkeypox virus (MPXV), which causes disease in humans, has for many years been restricted to the African continent, with only a handful of sporadic cases in other parts of the world. However, unprecedented outbreaks of monkeypox in non-endemic regions have recently taken the world by surprise. In less than 4 months, the number of detected MPXV infections has soared to more than 48,000 cases, recording a total of 13 deaths. In this Review, we discuss the clinical, epidemiological and immunological features of MPXV infections. We also highlight important research questions and new opportunities to tackle the ongoing monkeypox outbreak.
Subject terms: Viral infection, Viral immune evasion
In this Review, Ng and colleagues examine the clinical, epidemiological and immunological aspects of monkeypox virus (MPXV) infections, with a focus on mechanisms of host immunity to MPXV. The authors also consider the unique epidemiological and pathological characteristics of the current non-endemic outbreak of the virus and discuss vaccines, therapeutics and outstanding research questions.
Introduction
Monkeypox is a zoonotic viral disease caused by the monkeypox virus (MPXV), an orthopoxvirus belonging to the Poxviridae family of viruses1. MPXV was first identified in 1958 in research monkeys that were shipped from Singapore2, which is the likely reason for the disease being called ‘monkeypox’. However, the natural hosts of MPXV are more likely to be rodents and other small mammals3. The Orthopoxvirus genus also includes variola virus (VARV), the causative agent of lethal smallpox disease. The symptoms of monkeypox in humans are relatively similar to those of smallpox, but with a lower mortality rate1,4.
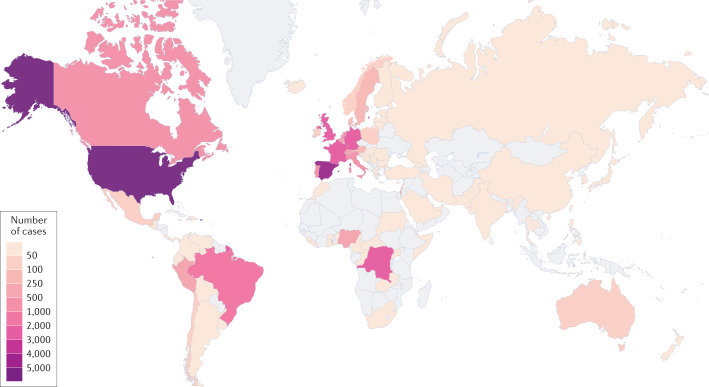
Sporadic cases of MPXV in humans were first identified in the 1970s in several African countries, but the virus became more widespread within the African continent over the past 20 years (see Box 1 for details). Since May 2022, there has been a drastic increase in the number of MPXV cases worldwide (Fig. 1), leading the World Health Organization (WHO) to declare the monkeypox outbreak a global health emergency5.
Fig. 1. Geographical distribution of confirmed and suspected monkeypox cases during the outbreak between May and August 2022.
Data presented as of 5 August 2022 were obtained from Global.health. Diagram generated with Datawrapper.
Possible reasons for this current outbreak could be attributed to waning smallpox immunity in the general population and termination of the smallpox vaccination regime6. Vaccination against smallpox has been shown to offer protection against monkeypox. An early study from Zaire in 1988 (ref.7) reported that individuals vaccinated against smallpox (during a national smallpox vaccination campaign beginning 12 years before the start of data collection) were approximately 85% less likely to contract monkeypox than those who were not vaccinated. In another study, severe complications and long-term effects of MPXV infection were found to be less common (39.5% versus 74%) with lower death rates in patients vaccinated against smallpox4. Recently, a study on 528 infections diagnosed during this current outbreak reported that only 9% of the individuals who were infected received prior smallpox vaccination8. Interestingly, one characteristic of the recent outbreaks is a disproportionate number of infections in men who have sex with men (MSM)8,9.
Phylogenetically, MPXV can be divided into two distinct clades — Central African (also commonly known as Congo Basin) and West African. Depending on the source of the West African MPXV, sequence similarity of ~95%10 or >99% between the two clades11 was reported. The Central African clade is generally considered to be more virulent, with an average fatality rate of 10.6% (95% CI 8.4–13.3%) compared with the 3.6% (95% CI 1.7–6.8%) reported for the West African clade12. MPXV of the Central African clade has been identified in cases appearing in the Democratic Republic of the Congo (DRC) and South Sudan12, whereas cases in Nigeria between 2010 and 2019 appeared to be due to the West African clade12. Cases reported outside Africa, including those currently in circulation, have all been caused by the West African clade9,13. Whether genetic changes in the MPXV genome could be responsible for this current outbreak is currently being investigated14 (see Box 2 for details).
Here, we discuss our current understanding of the transmission and immunopathogenesis of MPXV and the unique epidemiological and pathological characteristics observed in this outbreak. Specifically, we examine the potential mechanisms of host immunity against MPXV, drawing parallels from other poxviruses where necessary. We also discuss vaccines and therapeutics, and highlight remaining critical gaps in our knowledge. Of note, nomenclature for- orthopoxviruses gene/protein orthologues is very complex. In this Review, we refer to orthopoxvirus genes and proteins according to publicly available reference genomes: NC_063383 for the West African MPXV strain, NC_003310.1 for the Central African MPXV Zaire strain and NC_006998 for the vaccinia virus (VACV) Western Reserve strain. MPXV genes/proteins are referenced to the Central African MPXV Zaire strain, unless otherwise stated.
Box 1 History of monkeypox.
Epidemiological surveys to identify residual clusters of smallpox in the 1970s also led to the identification of the first cases of monkeypox virus (MPXV) in humans212. A total of 48 confirmed and/or suspected cases were reported across six African countries: the Democratic Republic of the Congo (DRC), Cameroon, Liberia, Nigeria, Sierra Leone and Côte d’Ivoire12,213–215. Between 1980 and 2000, MPXV was confined to the African continent, with no reports of infection or transmission in other parts of the world. The number of MPXV cases in Africa continued to climb, mainly in the DRC (>800 confirmed and/or suspected cases), with sporadic cases reported in Gabon, Cameroon, Côte d’Ivoire and the Central African Republic (CAR)12,216–222. Between 2000 and 2020, MPXV became more widespread within the African continent, with cases reported in the Republic of the Congo29,223,224, Liberia12,215, South Sudan225, Sierra Leone226, Nigeria, Cameroon222, the CAR227,228 and the DRC1,12. During this period, Nigeria229 reported 181 confirmed and/or suspected cases, and the DRC reported more than 20,000 suspected cases12. The first report of MPXV infection outside Africa was in 2003, when an outbreak of 47 confirmed and/or suspected cases was reported in the United States27,230. This outbreak was caused by human exposure to prairie dogs that had been infected by imported Gambian pouched rats27. Other countries with reported MPXV infections were Israel (2018; one case)231, the United Kingdom (2018–2021; seven cases)28,232–234, Singapore (2019; one case)235 and the United States (2021; two cases)236,237 (reviewed in ref.12).
As described above, MPXV was largely restricted to endemic regions prior to the current outbreak12,238. Particularly, it is noteworthy to highlight that between 2017 and 2022, Nigeria reported more than 650 confirmed cases, where nine patients eventually succumbed to the infection. The majority of the infected patients were male and aged between 21 and 40 years239.
Since May 2022 there has been a drastic increase in the number of MPXV cases reported from Europe, the Americas, the Middle East and Australia9,13,240 (see Fig. 1). The current spread of MPXV is unprecedented, with outbreak clusters expanding each day. By 28 August 2022, close to 50,000 confirmed and suspected cases were reported from more than 100 countries240, with 13 deaths240. Recently, Singapore confirmed several imported and local cases of monkeypox, which are the first reported in Southeast Asia during this recent outbreak241 and the first time that monkeypox has reappeared in Singapore since 2019 (ref.235). On 23 July 2022, the World Health Organization (WHO) declared the monkeypox outbreak a global health emergency5.
Box 2 Genetic changes in current circulating MPXV.
Understanding whether the recent monkeypox outbreaks are a result of genetic changes in monkeypox virus (MPXV) remains a research challenge. The 2022 outbreak is caused by lineage B.1 of the West African clade (MPXV Clade 3)242. At least 46 single-nucleotide polymorphisms have been found to be specific for this lineage, including 24 non-synonymous single-nucleotide polymorphisms243. Recent molecular epidemiology studies have shown a higher than expected rate of genomic variance among the outbreak sequences, suggesting accelerated evolution242 and, potentially, APOBEC3 editing244. One preprint publication (not peer reviewed) reports the presence of insertions and deletions in the DNA of the MPXV strain that is circulating in the 2022 outbreak compared with MPXV strains that were circulating prior to 2017 and suggests that these changes may be responsible for the current outbreak14. However, it remains unclear whether and how these genetic differences drive the epidemiological phenotype. A leading hypothesis proposes that the three non-synonymous single-nucleotide polymorphisms (D209N, P722S and M1741I), which are found in the surface glycoprotein B21R, a key antibody target, are enhancing the transmissibility of the virus243,245. However, MPXV is a complex virus, with a DNA-based genome that is approximately six times as large (~197 kb) compared with the RNA-based genome of SARS-CoV-2. It encodes more than 190 open reading frames (ORFs), many of which do not have well-defined functions15–17. Identifying the potential impact of particular genetic mutations on the viral phenotype is therefore complex and time-consuming. That said, the DNA-based genome of MPXV has a much greater capacity to repair errors incurred during viral replication246 compared with the RNA-based coronaviruses. However, the related orthopoxvirus vaccinia virus (VACV) is capable of ‘phenotypic mutations’ in the form of genetic accordions (multistep events involving gene application and mutation(s) that allow poxviruses to subvert host antiviral responses)247. Specifically, a variant of VACV was identified that has a significant amplification of the K3L gene, which, together with a beneficial point mutation in the same gene, allows the virus to largely overcome the host protein kinase R (PKR)-mediated antiviral responses247. Such genetic accordions have not been reported in MPXV and further investigations are needed to investigate whether such a phenomenon could be a plausible mechanism for MPXV evolution and spread.
MPXV genome and phylogeny
Computational analysis of the Central African MPXV Zaire strain revealed the presence of at least 190 open reading frames (ORFs)15–17. Genes known to be important for orthopoxviruses are present within the central region of the MPXV genome (between ORFs C10L and A25R)16,17. However, a subset of ORFs are either missing or truncated in the MPXV genome compared with the genomes of other orthopoxviruses11,16,18. Disruptions to several ORFs that code for genes involved in immune evasion have been reported in the West African clade, and these may be responsible for this clade’s lower virulence relative to the Central African clade6,11,18.
The virus exists in two distinct infectious forms, the intracellular mature virus and the extracellular enveloped virus, which differ in their surface glycoproteins and infect cells via different mechanisms19. MPXV replication is a complex process but is generally thought to be identical to other orthopoxviruses19. Entry receptors for MPXV have not been clearly identified, although it was suggested that viral entry is dependent on the viral strain and host cell type and involves multiple surface receptors, including chondroitin sulfate20 or heparan sulfate21,22. In VACV, surface proteins H3, A27 and D8 have been associated with viral binding20–22. Following binding, VACV gains entry into the cell through 11 conserved proteins, which form a complex known as the entry fusion complex23.
Monkeypox pathology
MPXV infection has an incubation period of 5–21 days, and common symptoms include fever (between 38.5 °C and 40.5 °C), headache and myalgia. A distinguishing feature of MPXV infection is the presence of swelling at the maxillary, cervical or inguinal lymph nodes (lymphadenopathy)1,4. In the recent outbreak, a report from Portugal suggested that inguinal lymphadenopathy was more common than cervical and axillary lymphadenopathy24. Rashes appear following the onset of fever, beginning on the face, tongue and oral cavity (enanthem) before spreading across the body. In the later stages of infection, lesions in the oral cavity can cause difficulties in drinking and eating4. However, in the recent outbreaks, several atypical clinical observations have been reported. In patients who are MSM, these include the presence of genital lesions that subsequently spread to other sites in the body, as well as anal ulcers, and it appears that skin lesions may be more limited in distribution than reported in previous outbreaks24–26.
Disease severity can be classified using the lesion count, as higher lesion counts correlate with increased risk of severe complications4. Patients with severe complications may experience respiratory and gastrointestinal issues27, encephalitis4, septicaemia27,28 and ocular infections leading to permanent vision loss29. Skin lesions also increase the likelihood of dermal bacterial infections, especially in patients who are not vaccinated against smallpox4.
Lesions typically progress through four stages — macular, papular, vesicular and pustular — before falling off as scabs1. Patients are typically considered non-contagious once lesions have crusted over. However, scabs have been reported to contain significant quantities of MPXV DNA even after falling off30, which may indicate the presence of infectious viral material. Of note, viable VARV has been isolated from scabs of patients with smallpox31.
During pregnancy, MPXV can be vertically transmitted from the mother to the fetus32. In one study involving four pregnant women who were infected with MPXV in the DRC, only one gave birth to a healthy infant. Two women experienced miscarriage in the first trimester and one had a stillbirth. In the stillborn, skin lesions were observed across the body32. In another study, four out of five women who were infected with MPXV in the DRC had fetal demise and lesions were observed on the maternal surface of the placenta30. The studies did not report which clade of MPXV these patients were infected with, although given the location of the studies it is very likely the Central African clade30.
A study conducted in Zaire during 1980–1985 reported a higher incidence of fatal disease in young children infected with MPXV, with a case fatality rate of 14.9% in children aged between 0 and 4 years compared with a rate of 0% in individuals aged 10 years or older4. This disparity could potentially be due to differences in their immune responses4. Currently, data on severity of infection in children infected with the West African clade are lacking33. Nevertheless, the severe outcomes of monkeypox in pregnant women and in young children highlight the importance of future public health efforts to limit the spread of MPXV and minimize the risk of adverse events.
MPXV pathogenesis
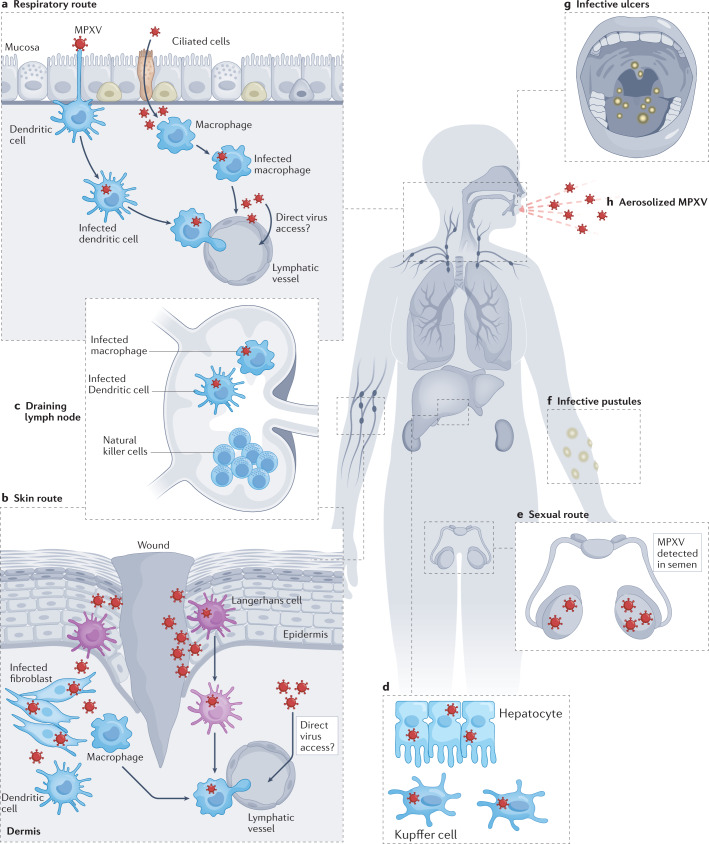
The clinical outcome of orthopoxviral infection in a vertebrate host is strongly dependent on the entry route used by the virus to establish the primary infection34 (Fig. 2). For several orthopoxviruses, such as the highly contagious VARV and MPXV, the respiratory/oral cavity is a possible common entry route following the inhalation of aerosolized respiratory secretions or the ingestion of bodily fluids from individuals who are infected35. The virus then infects the oral and respiratory tract mucosae, with the upper, middle and lower airway epithelium as main targets for primary infection36. This phase of infection is asymptomatic, with no signs of oropharyngeal lesions34. Virus spread progresses with the infection of nearby tissue-resident immune cells, potentially including antigen-presenting cells such as monocytes, macrophages, B cells and dendritic cells37–41. The mechanisms whereby orthopoxviruses relocate from the initial site of infection to nearby draining lymph nodes are a matter of debate. It has been observed, for example, that VACV-infected murine dendritic cells migrate from the lung epithelium to draining lymph nodes, likely contributing to virus dissemination42. Conversely, VACV infection of human monocyte-derived dendritic cells has been shown to be abortive, affecting dendritic cell maturation and their migratory potential39,43–45, and arguing against a role of dendritic cells supporting the initial lymphatic spread of VACV. Importantly, the rapid relocation of VACV to draining lymph nodes within hours of inoculation46,47 indicates direct viral access to lymphatic vessels as a dissemination mechanism.
Fig. 2. Immunopathogenesis of human monkeypox.
a–h | Monkeypox virus (MPXV) might enter the body via the respiratory (panel a) or skin (panel b) route. In the respiratory tract, the virus can infect airway epithelial cells such as ciliated cells. Antigen-presenting cells such as dendritic cells and macrophages (MΦ) are also susceptible to MPXV infection. Upon inoculation in the skin, the virus infects keratinocytes and fibroblasts. Skin-resident immune cells such as Langerhans cells, dendritic cells and macrophages are also targeted. In both scenarios (panels a and b), it is hypothesized that infected antigen-presenting cells travel to nearby draining lymph nodes and facilitate its spread through the lymphatic system (panel c). Direct viral access to the lymphatics has been also speculated. A common feature of human monkeypox is swelling of lymph nodes (lymphadenopathy). The abnormal proliferation and retention of natural killer cells might be one of the causes. Following its spread through lymphoid tissue, MPXV may target other large organs such as the spleen and liver (panel d). Of note, MPXV antigens have been previously been detected in both hepatocytes and Kupffer cells in non-human primate (NHP) models. The viraemia wave could then allow the virus to further spread to distant organs such as the skin and gonads. Recently, MPXV was isolated from semen of infected individuals, highlighting the possibility of sexual transmission (panel e). The infection of skin and mucosae leads to the appearance of infective pustules (panel f) and ulcers (panel g). The latter release high quantities of virus into the saliva, which potentially leads to aerosolized transmission of MPXV (panel h).
Following the infection of nearby draining lymph nodes, orthopoxviruses replicate extensively in lymphoid tissues. Clinical studies of human monkeypox suggest that lymphoid tissues in the neck and throat are areas of primary MPXV replication37. This was supported by studies in a cynomolgus macaque model of aerosolized MPXV infection, where the tonsils and the mandibular and mediastinal lymph nodes were active areas of early virus replication36. Poxvirus tropism in lymphoid tissue has been associated with infection of monocyte/macrophages, dendritic cells, B cells and activated T cells, which could also be targets for MPXV48. The processes leading to abnormal lymph node swelling upon natural MPXV infection have not been elucidated; however, during experimental infection of non-human primates (NHPs) with MPXV, massive proliferation and accumulation of natural killer cells was observed in the lymph nodes surrounding the site of inoculation37.
After the development of low-grade primary viraemia resulting from the infection of the lymphoid tissues, orthopoxviruses can disseminate to distant organs via the lymphohaematogenous route36,49. In experimental mousepox models, the spleen and liver are the main targets for infection after primary lymphatic spread50. Virus infection in these organs releases a second major viraemia wave (believed to be through infected cells) that results in viral dissemination to the lungs, kidneys, intestines, skin and other organs50. Similarly, in an NHP model of aerosolized MPXV infection, viral antigen was observed in the liver, particularly in highly specialized macrophages such as Kupffer cells36. Antigen was also detected in hepatocytes, although to a lower extent. Enlarged spleen and liver have also been reported during MPXV infection in humans30. In VARV infection, it is believed that lymphoid organs such as the spleen and bone marrow support virus replication, but there is less evidence for hepatic involvement51.
The presence of orthopoxviruses in the small dermal blood vessels marks the start of skin infection and development of skin lesions51. However, how the virus reaches the upper skin layers, which lack blood and lymphatic vessels, is not well understood. It is possible that infected migratory skin dendritic cells such as Langerhans cells might be responsible, as they are known to be susceptible to VACV infection36. Infiltration of macrophages, dendritic cells and CD3+ T cells has been observed around the infective pustule52. The role of skin-infiltrating CD3+ T cells in the context of MPXV infection requires characterization; this is particularly true for cytotoxic T lymphocyte responses, which have been associated with better virus control in vaccinated rhesus macaques53. Importantly, epithelial lesions (enanthema) also appear during MPXV infection in the oropharyngeal mucosa, tongue, pharynx, larynx, trachea and oesophagus51, eventually evolving into ulcers which release infectious viral particles into the saliva51.
Infection can also occur via the skin. It has been postulated that infection of the dermal keratinocytes, fibroblasts and tissue-resident antigen-presenting cells such as monocytes, macrophages, Langerhans cells and dendritic cells might occur and migratory antigen-presenting cells could contribute to virus dissemination through the lymphatics46,54,55. Nonetheless, recent evidence from a mouse model of orthopoxvirus skin infection suggested that dendritic cell migration from the skin to draining lymph nodes is impaired on VACV56. The relocation of the virus from the skin to the lymphatics might also be supported by other mechanisms such as direct lymphatic vessel access, as observed in skin infection models of Zika virus57.
Sexual transmission of monkeypox has been speculated52, and MPXV was recently identified in the semen of three male patients in Italy26. Cases of monkeypox with exclusive genital lesions have also been reported58, which might indicate preferential MPXV tropism into the testes. Being an immune-privileged tissue59, the testes could act as a site for latent MPXV infection, but this requires further investigation. Nonetheless, recent animal studies showed that the related VACV exhibits tropism for testicular and ovarian tissues60,61. Viral shedding was also reported in faeces and contact with the rectal mucosa might increase the likelihood of MPXV transmission35. It was previously noted in patients with human immunodeficiency virus 1 (HIV-1) that these tissues could act as a reservoir for the virus62. A recent study63 determined that the rectal mucosa immune environment in MSM was significantly different compared with individuals who are heterosexual, with a higher presence of immune activities indicative of mucosal injuries. This condition could lead to the recruitment of immune cells, which could then be easily targeted by infectious agents, such as observed with HIV-1 (ref.64). This could similarly apply to MPXV transmission and infection in MSM. However, this does not indicate that monkeypox has become a sexually transmitted disease, as MPXV can spread through any form of close contact with the infectious pustules that are symptomatic of monkeypox.
Immunity to MPXV
Even though the virus was identified decades ago, human immunity to MPXV infection has not been extensively characterized. As such, inferences on MPXV interaction with the host immune system are often drawn from studies performed with VACV and related orthopoxviruses. In the following sections, we highlight the potential mechanisms of host immunity against MPXV and discuss the immune evasion strategies utilized by MPXV during active infection.
Innate immune responses to MPXV
Innate immune cells typically act as the first line of defence following active viral infection, but these cells also serve as targets for some viruses. Numerous in vitro and in vivo studies have demonstrated that monocytes are the initial targets of poxviruses36,65–68. Early detection of poxvirus antigen in both monocytes and neutrophils has been suggested to be a strong predictor of MPXV lethality69. Susceptible monocytes are actively recruited to sites of infection, with marked expansion of CD14+ monocytes in the lungs of cynomolgus macaques experiencing viral pneumonia following MPXV infection70. Mouse CD45+CD11b+GR-1int inflammatory monocytes have also been shown to be permissive to VACV replication and may be plausible vehicles for virus dissemination47. It was also reported that human primary M2-like macrophages allowed VACV replication and dissemination71. Following VACV infection, these primary macrophages formed actin tails, cell linkages, lamellipodia and branching structures associated with the VACV virions, indicating that these cells might participate in virus spread71. However, it was also reported that depletion of phagocytic cells did not abolish spread of VACV72 in infected mice, suggesting that monocytes and macrophages are not the only immune cells that are capable of facilitating virus dissemination. Nevertheless, Ly6G+ innate immune cells (both neutrophils and Ly6G+ monocytes72) were responsible for infiltrating and controlling virus-infected cells, thus limiting viral tissue damage47,72. These results were indirectly confirmed by a study that found an association between low numbers of blood neutrophils with moribundity in MPXV-infected animals73. It is also worth noting that immune cells recruited to the site of infection control only local pathogenesis and tissue pathology, but not virus dissemination, and a systemic immune response is required to prevent widespread infection74.
Natural killer cells are an important component of innate immunity and, similar to monocytes, are capable of shaping the adaptive immune response75. In MPXV-infected rhesus macaques, numbers of natural killer cells expand significantly in both peripheral blood (a mean 23-fold increase by day 7 post infection) and lymph nodes (a mean 46.1-fold increase by days 8–9 post infection)37. Prior to this rapid proliferation, the migratory capacity of the various natural killer cell subsets was significantly impaired by MPXV infection, which severely affected their recruitment into the lymphoid and/or inflamed tissues37. A downregulation of chemokine receptors such as CXCR3, CCR5, CCR6 and CCR7 on these cells was also reported37. Moreover, natural killer cells isolated from both lymph nodes and blood were reported to lose their ability to degranulate and to secrete IFNγ and TNF37. Although no correlation between viral clearance and natural killer cell numbers and activities was reported in this NHP model37, the importance of natural killer cells in controlling MPXV viral load was demonstrated in CAST/EiJ mice. This strain is exceptionally susceptible to orthopoxvirus infection76 owing to low numbers of natural killer cells. IL-15 treatment protected CAST/EiJ mice from lethal MPXV infection even when both CD4+ and CD8+ T cells were depleted76. This implies that the expanded natural killer cells were responsible for the protective effect as treatment with IL-15 is known to transiently increase the numbers of IFNγ-secreting natural killer cells and CD8+ T cells77.
Similarly, natural killer cells are also needed to control both Ectromelia virus (ECTV) and VACV infection in C57BL/6 mice78,79. ECTV is a natural orthopoxviral pathogen of mice, and is often used to induce experimental mousepox as a model for other clinically important orthopoxviruses80. Interestingly, it was suggested that the expression of CD94 on natural killer cells in C57BL/6 mice is absolutely essential for conferring resistance to ECTV infection81. This is mediated by the NKG2E and CD94 receptors on natural killer cells, which bind complexes of MHC class I with the peptide Qa-1b, which are expressed by infected cells81. NKG2D has also been reported to participate in natural killer cell-mediated protection against ECTV infection79 and it was postulated that CD94-NKG2E and NKG2D may have synergistic activity in inducing optimally protective natural killer cells81. However, the exact mechanisms behind this apparent synergism remain to be elucidated, and further studies will be required to better understand the roles of natural killer cells in mousepox infections. Given that CD94 and NKG2 are highly conserved between humans and rodents82, these receptors may also play a protective role against MPXV infection in humans.
In humans infected with MPXV, the roles of many innate immune cells — including monocytes/macrophages, neutrophils, natural killer cells, conventional dendritic cells, plasmacytoid dendritic cells and innate lymphoid cells — are currently unknown. The characterization and profiling of these immune cells during MPXV infection will be essential for understanding their functions and identifying important biomarkers for disease prognosis.
VARV infection in animal models triggers systemic cytokine responses that correlate with disease outcomes. In unvaccinated cynomolgus macaques, significant changes in host gene expression were detected following infection with VARV66. In particular, transcription of a cluster of interferon-associated genes was upregulated; this cluster was enriched for genes regulated by both type I and type II interferons, including PKR, STAT1, STAT2, MX1, MX2, IP10, OAS1, OAS2 and OAS3 (ref.66). The animals that succumbed to the infection (two out of seven) had minimal interferon responses, indicating that this early interferon response protects against fatality66. Human IFNβ has been demonstrated to inhibit MPXV replication and spread83. However, MPXV does not robustly activate TNF-regulated and NF-κB-regulated genes, especially in animals that succumb to infection66. This is not surprising, given that VARV and other orthopoxviruses harbour genes that can modulate TNF84,85 and NF-κB86,87 pathways.
Although host immunity is required to combat infections, aberrant immune signalling can adversely affect infection outcomes. In another study of VARV-infected cynomolgus macaques, the levels of IL-8, CCL2 (also known as MCP1), CCL4 (also known as MIP1β), IL-6 and IFNγ were significantly increased during the first 4 days post infection67. These cytokines drive monocytosis88, which might facilitate enhanced virus dissemination through monocytic cell-associated viraemia67. Importantly, the macaques eventually succumbed to VARV infection, where high levels of these cytokines might have contributed to a ‘cytokine storm’ leading to their demise67. Likewise, the levels of IL-1RA, IL-2, IL-6, IL-8, IFNγ, CCL2, CCL5 (also known as RANTES), G-CSF, GM-CSF and sCD40L were found to be elevated in MPXV-infected cynomolgus macaques70. Furthermore, a relative expansion (0.97-fold to 16.3-fold) of CD14+ monocytes was reported during acute infection, suggesting that the general immune milieu promoted the development and recruitment of monocytes following MPXV infection70.
In reported cases of human MPXV infection, numerous cytokines are elevated following infection (regardless of disease severity) — these include IL-1β, IL-1RA, IL-2R, IL-4, IL-5, IL-6, IL-8, IL-13, IL-15, IL-17, CCL2 and CCL589. However, in patients with serious disease (defined as having >250 lesions), concentrations of IL-2R, IL-10, GM-CSF and CCL5 were higher compared with those in patients with less severe disease, whereas the concentration of pro-inflammatory IL-6 was lower89. This cytokine profile suggests a dominant T helper 2 cell response characterized by higher levels of IL-4, IL-13 and IL-10. Likewise, the reduced levels of IL-2, TNF, IFNα and IFNγ also suggest an anti-inflammatory microenvironment involving regulatory T cells89.
VACV can evade immune responses by downregulating inflammatory and antiviral immune responses44,90,91, and MPXV may use a similar strategy to subvert host immunity92. Given that immune mediators often facilitate crosstalk between immune cells93, future studies should identify the functional relationships between cytokine profiles and immune cells in order to clarify the mechanisms of pathogenesis and determine immune correlates of protection during MPXV infection.
B cell and antibody protection
The importance of B cells and immunoglobulins against poxviruses was first demonstrated with the successful global vaccination campaign that eradicated smallpox, which used a live VACV vaccine94,95. It was further demonstrated that treatment with vaccinia immune globulin (VIG) isolated from the serum of vaccinees successfully protected close contacts of patients with smallpox from infection96. In rhesus macaques, VACV-specific B cell responses were instrumental in protecting against a lethal MPXV infection53. Importantly, epidemiological studies have further demonstrated that the VACV vaccine confers protection against other poxviruses, including MPXV97. The VACV-specific memory B cells and antibody levels induced by vaccination were exceptional, in some cases lasting longer than 50 years98,99. However, only ~50% of vaccinated individuals at >20 years after vaccination65 had neutralizing antibody titres greater than 1:32, a correlate of protection suggested to confer protective immunity against smallpox100. It is likely that cross-protective immunity against monkeypox may similarly wane over time.
Fourteen MPXV proteins have been shown to be recognized by cross-reactive VACV-induced immunoglobulins from human vacinees101. Three proteins in particular — MPXV (Zaire-1979_005) proteins D8, H3 and A26 — were targeted by neutralizing antibodies against MPXV in infected macaques101. In VACV, orthologue D8 and H3 proteins are involved in the attachment of mature virions22, whereas A26 associates with A27 (ref.102) to bind surface laminin103. MPXV (Zaire-1979_005) proteins C19, A33 and A44 were also prominent antigens for IgM isolated from MPXV-infected macaques during the acute phase of infection — these proteins could thus be further developed as antigen-based serological diagnostic tools101. In another study, prophylactic treatment with a cocktail of two mAbs — c7D11 and c8A — successfully protected marmosets against lethal MPXV infection104. C7D11 and c8A target the VACV proteins L1 (ref.105) and B5 (ref.106), respectively, and have been recently formulated as a potential mRNA vaccine encapsulated in lipid nanoparticles107. Gilchuk et al.108 showed that a mixture of human-derived mAbs targeting the VACV proteins D8, H3, A33, A27, B5 and L1 effectively cross-neutralized four clinically relevant orthopoxviruses, including MPXV and live VARV. However, despite knowledge of the MPXV proteins that are recognized by neutralizing antibodies, MPXV-specific epitopes (both conformational and linear) have not been extensively characterized.
The isotype composition of the anti-MPXV response may provide an important clue to pre-existing immunity and protection, as IgM antibodies typically dominate in primary immune responses, whereas IgG antibodies dominate in secondary immune responses. In a cohort of 200 patients infected with MPXV who were recruited between March 2007 and August 2011 in the DRC, individuals with both IgM and IgG responses were 5.09 times more likely to develop severe lesions compared with individuals who had IgG-only responses30. Similarly, in a cohort of infected individuals from the 2003 MPXV outbreak in the United States, patients with moderate/severe disease had an overall higher titre of anti-orthopoxvirus IgM109 compared with those with mild disease, and anti-orthopoxvirus IgG responses were much reduced and less frequent in patients with moderate/severe disease109. It is plausible that an IgG-only response reflects robust levels of cross-protective IgG+ memory B cells that produce a dominant secondary antibody response, whereas the lack of such memory necessitates an IgM-dominated primary response that is less effective at preventing disease. Thus, IgM responses may be a biomarker for disease severity. This also emphasizes the critical and immediate need to extensively characterize the antibody profile of patients with MPXV in different cohorts. Likewise, VACV vaccine correlates of protection must be determined to explain why certain vaccinated patients experience breakthrough infections.
T cell immunity
CD4+ T cells, particularly T follicular helper cells, play a role in enhancing recall and differentiation of memory B cells into antibody-secreting cells110. Memory CD4+ T cells were found to persist for up to 50 years or longer following VACV vaccine, with an estimated half-life of 8–15 years99. These VACV-specific CD4+ T cells were capable of producing IFNγ and TNF following stimulation99. However, no direct correlation was reported between numbers of virus-specific CD4+ T cells and anti-VACV antibody titres99. By contrast, the number of CD4+ T cells was shown to be critically important in inducing a protective antibody response against lethal MPXV infection in VACV-vaccinated rhesus macaques53. Simian immunodeficiency virus (SIV)-infected macaques with CD4+ T cell counts <300 cells mm–3 were not able to produce VACV-specific IgG following vaccination and died when challenged with MPXV53. This observation is of high concern to both VACV-vaccinated and unvaccinated individuals with uncontrolled HIV-1 infection, as their CD4+ T cell counts are typically very low111. This group of individuals is therefore at high risk of developing severe MPXV infection if exposed112. They might also experience a more complicated pathology and provide the virus with an opportunity to acquire mutations that result in higher virulence or transmission potential113. By contrast, a recent patient infected with MPXV who was on antiretroviral treatment for HIV-1 had a CD4+ T cell count >700 cells mm–3 and did not experience a severe disease outcome25. This may suggest an important role for CD4+ T cells in regulating monkeypox severity. Nevertheless, more studies will need to be carried out to fully understand the role of CD4+ T cells during MPXV infection.
In addition to supporting antibody development, T cells can play direct antiviral roles. Given that orthopoxviruses, including MPXV, infect and disseminate in macrophages36,65–68, cytolytic T cells can be instrumental in killing infected macrophages to prevent viral spread. CD8+ T cells have been shown to eradicate virus-infected monocytes and minimize virus dissemination in a mouse model of VACV infection47. In fact, activation of CD8+ T cells in response to VACV infection has been shown to be dependent on γδT cells, which present VACV peptides via MHC class I molecules114. Moreover, γδT cells also upregulate co-stimulatory molecules CD80 and CD86 and secrete IL-1 and IFNα for activation of CD8+ T cells114. In a mouse model of VACV respiratory infection, IFNγ secretion by primary activated effector CD8+ T cells was shown to protect against lethality115. Indeed, CD8+ T cell-derived IFNγ was sufficient for protection even in the absence of CD4+ T cells and B cells115, highlighting the possibility that CD8+ T cells also confer protection against infection with other orthopoxviruses. Likewise, memory CD8+ T cells, which are induced following VACV immunization, were also demonstrated to protect against lethal ECTV infection in mice116. These memory CD8+ T cells execute their protective effects via a combination of IFNγ and perforin secretion, and work concomitantly with primary effector CD8+ T cells to achieve optimal protection116. In humans, standard smallpox vaccine administered by scarification117 was also able to induce primary cytotoxic CD8+ T cells and IFNγ-producing T cells118. This observation was supported by another study, in which participants received live vaccinia smallpox vaccine (Dryvax)119. High levels of IFNγ-producing CD8+ and CD4+ T cells were detected following immunization119. In humans infected with VACV, activated CD4+ T cells were shown to upregulate genes related to cytolytic activities120. Interestingly, MHC class II-restricted cytolytic CD4+ T cells have also been reported in individuals immunized with VACV121. These cells could be responsible for virus clearance in vaccinees with reduced or missing memory CD8+ T cell responses99. In the experimental mousepox model, perforin-dependent cytolytic CD4+ T cells have been reported122. Taken together, these observations highlight the importance of T lymphocytes in controlling orthopoxviral infections.
Across the orthopoxvirus proteome, numerous CD4+ and CD8+ T cell epitopes have been identified in humans, mice and NHPs123–125. Many are conserved among the major orthopoxviruses and bind to human MHC class I and class II molecules126–128. In particular, CD8+ T cells specific for two identified epitopes (MHC class II-restricted GRVFDKADGKSKRDA and MHC class I-restricted NPVTVINEY) in the immediate-early E3 protein of VACV were capable of killing infected cells and halting the spread of VACV129. Both epitopes are conserved in the MPXV homologue, which is encoded by the MPXV F3L gene130. An earlier study showed that VACV missing the E3 protein did not protect cynomolgus macaques from subsequent MPXV infection131. As E3 protein is detected within 30 min of VACV infection132, it should be readily processed and presented by infected cells, allowing T cell-mediated lysis at an early infection stage before virion production and release. These properties make E3 an excellent possible candidate for future vaccine designs targeting all major orthopoxviruses.
Despite the potential importance of T cells in disease protection, smallpox vaccination does not necessarily provide robust T cell-mediated immunity against MPXV. In two out of five vaccinated individuals who subsequently contracted MPXV, orthopoxvirus-specific CD4+ and CD8+ T cells were not detectable throughout convalescence109. Furthermore, similar levels of orthopoxvirus-specific CD4+ T cell reactivity were observed in vaccinated and unvaccinated patients, and orthopoxvirus-specific CD8+ T cell responses were in fact higher in unvaccinated patients109. The association of CD4+ and CD8+ T cell responses with the severity of MPXV infection remains inconclusive in human studies.
MPXV immune evasion
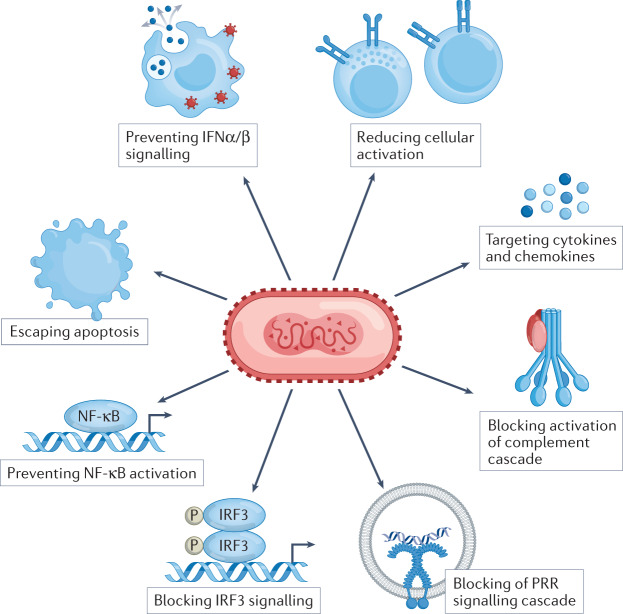
Orthopoxviruses have accrued an arsenal of genes that encode proteins which interfere with host cell signalling pathways that are involved in virus recognition, apoptosis and immune regulation18,84,85,133–136 (Fig. 3). Here, we discuss some of the evasion mechanisms used by MPXV during active infection (Table 1). For a more in-depth review of orthopoxvirus immune evasion strategies, see refs.85,133–136.
Fig. 3. Immune evasion by MPXV.
Monkeypox virus (MPXV) is known to encode numerous viral proteins that are involved in evading the host immunity. These can be involved in interfering with the signalling cascade of pathogen recognition receptors, disrupting key transcription factors for the expression of inflammatory genes, such as interferon regulatory factor 3 (IRF3) and NF-κB. MPXV can also interfere with interferon signalling by blocking IFNα/β binding or suppressing IFNα/β production and by blocking protein kinase R (PKR)-mediated pathways. In addition, MPXV secretes proteins that can target key inflammatory molecules such as TNF, IFNγ, IL-1β, IL-18 and IL-6. Moreover, MPXV can prevent apoptosis in infected cells by expressing numerous viral proteins that target the apoptotic pathways. The Central African MPXV Zaire strain also expresses D14 which blocks the activation of the complement cascade. However, this viral protein is not expressed in the West African MPXV strain. Lastly, MPXV can also downregulate the activities of natural killer cells and T cells by interfering with their activation processes (see also Table 1). PRR, pattern recognition receptor.
Table 1.
Virulence and immune evasion genes of monkeypox virus (MPXV)
| Protein function | VACV (Western Reserve) | MPXV (Central African) | MPXV (Western African) | |||
|---|---|---|---|---|---|---|
| Accession No. NC_006998 | Accession No. NC_003310 | Accession No. NC_063383 | ||||
| Genea | Size, amino acids | Gene | Size, amino acids | Gene | Size, amino acids | |
| Inhibitor of NF-κB activation; BCL-2-like protein | A46R | 240 | A47R | 240 | OPG176 | 240 |
| Inhibitor of NF-κB activation; BCL-2-like protein | B15R | 149 | B13R | 149 | OPG200 | 149 |
| Inhibitor of IRF3 and NF-κB activation, apoptosis inhibitor; BCL-2-like protein | N1L | 117 | P1L | 117 | OPG035 | 117 |
| Inhibitor of IRF3 NF-κB activation; BCL-2-like protein | K7R | 149 | C6R | 149 | OPG044 | 149 |
| Inhibitor of IRF3 and IRF7 activation; BCL-2-like protein | C6L | 151 | D11L | 153 | OPG029 | 155 |
| Double-stranded RNA-binding protein, inhibitor of interferon signalling, apoptosis inhibitor | E3L | 190 | F3L | 153 | OPG065 | 153 |
| IFNα/β binding proteins | B19R | 351 | B16R | 352 | OPG204 | 351 |
| IFNγ binding proteins | B8R | 272 | B9R | 267 | OPG193 | 267 |
| Dephosphorylation of STAT1; phosphatase | H1L | 171 | H1L | 171 | OPG106 | 171 |
| Ankyrin-like protein | C19L | 112 | J3L | 587 | OPG003 | 588 |
| Ankyrin-like protein | – | – | D1L | 437 | OPG015 | 437 |
| Ankyrin-like protein | VACWR017 | 71 | D7L | 660 | OPG023 | 660 |
| Ankyrin-like protein | C9L | 634 | D9L | 630 | OPG025 | 630 |
| Ankyrin-like protein | M1L | 472 | O1L | 442 | OGP037 | 442 |
| Ankyrin-like protein | K1L | 284 | C1L | 284 | OPG039 | 284 |
| Ankyrin-like protein | B4R | 558 | B5R | 561 | OPG189 | 561 |
| Ankyrin-like protein | – | – | B17R | 793 | OPG205 | 787 |
| Ankyrin-like protein | – | – | N4R | 437 | OPG015 | 437 |
| Ankyrin-like protein | B25R | 112 | J1R | 587 | OPG003 | 588 |
| Apoptosis inhibitor, caspase 1 and caspase 8 inhibitor, SPI-2 | B13R | 345 | B12R | 344 | OPG199 | 344 |
| Apoptosis inhibitor, SPI-1 | C12L | 353 | B19R | 357 | OPG208 | 357 |
| Apoptosis inhibitor | F1L | 226 | C7L | 219 | OPG045 | 219 |
| Apoptosis inhibitor | VACWR013 | 181 | D5R | 242 | OPG021 | 242 |
| TNF and chemokine binding protein, CrmB | C22L | 122 | J2R | 348 | OPG002 | 349 |
| IL-1β binding protein | VACWR197 | 326 | B14R | 326 | – | – |
| IL-18 binding protein | VACWR013 | 126 | D6L | 126 | OPG022 | 126 |
| Inhibitor of complement enzyme | C3L | 263 | D14L | 216 | – | – |
| CC chemokine binding protein | C23L | 244 | J3R | 246 | OPG001 | 246 |
| CC and CXC chemokine binding protein | A41L | 219 | A41L | 221 | OPG170 | 221 |
| OMCP, inhibitor of natural killer cell-mediated NKG2D-dependent cell lysis | – | – | N3R | 176 | OPG016 | 176 |
| Inhibitor of intracellular trafficking of MHC class I molecules | B9R | 77 | B10R | 221 | OPG195 | 221 |
| Inhibitor of MHC class II antigen presentation | A35R | 176 | A37R | 176 | OPG163 | 176 |
| Viral growth factor; EGF-like protein | C11R | 140 | D3R | 142 | OPG019 | 142 |
Data obtained from refs.18,84,85,133–136. Size of each protein encoded by the displayed genes shown as number of amino acids. BCL-2, B cell lymphoma 2; EGF, epidermal growth factor; IRF3, interferon regulatory factor 3; MPXV, monkeypox virus; OMCP, orthopoxvirus MHC class I-like protein; SPI-2, serine protease inhibitor 2; VACV, vaccinia virus; –, no corresponding gene can be identified in the respective virus genome. aName or Gene ID is provided. Locus tags are provided in the event that name or Gene ID is not available.
Preventing cellular signalling
Mammalian cells can detect the presence of microbial infection through pattern recognition receptors (PRRs). These can trigger intracellular signalling cascades involving numerous host cofactors such as MYD88, TRAM, TIRAP and TRIF, eventually activating important immune transcription factors such as NF-κB and interferon regulatory factors (IRFs)137,138. Numerous orthopoxviral proteins can antagonize these signalling processes18,84,85,133. For example, the VACV genome encodes numerous B cell lymphoma 2 (BCL-2)-like proteins that inhibit NF-κB and IRF3 activation by interacting with cofactors that are recruited following PRR binding85,139–141. BCL-2-like proteins are generally conserved across orthopoxviruses — A47, B13, P1, C6 and D11 are orthologues of BCL-2-like proteins in MPXV17,84. VACV also encodes the E3 protein, which binds to double-stranded RNA (dsRNA)142 that is produced late in its replication cycle143, and prevents the dsRNA from being detected by host intracellular PRRs54. This leads to complete inhibition of the protein kinase R (PKR)-mediated pathway54, which can otherwise block protein synthesis by phosphorylating the eukaryotic translation initiation factor subunit 2α (eIF2α)144. The F3 protein of MPXV is a homologue of the VACV E3 protein with a 37 amino acid truncation at the amino terminus130. Unlike a similarly truncated recombinant VACV (VACVΔ37N), MPXV can still inhibit host immune responses130. Interestingly, another recombinant VACV expressing the MPVX F3L gene (VACV-F3L) did not inhibit host PKR activation, suggesting that MPXV has evolved to encode for yet undiscovered proteins that compensate for the missing N-terminal amino acids of F3 in limiting host antiviral activities130.
One of the most important transcription factors downstream of PRR binding is IRF3, which controls the expression of the crucial antiviral molecules IFNα and IFNβ145. The VACV B19 protein directly interacts with soluble interferons and inhibits their binding to receptors146. Although deletion of the B19R gene in VACV did not affect its virulence, deletion of B19 in ECTV did severely attenuate its ability to establish infection147. The MPXV orthologue B16 can inhibit IFNβ signalling83,148. Interestingly, the interferon response is known to be stronger in children and has been shown to protect against severe SARS-CoV-2 (ref.149) and RSV150 infections, but the reverse was observed in children infected with MPXV1,4. This emphasizes the need to better understand host–pathogen interactions and further characterize the mechanisms of MPXV pathogenesis.
The activation of NF-κB is controlled by proteins of the IκB family, which contain ankyrin repeats151. NF-κB consists of two subunits (p65/p50), and in its inactive form the p65 subunit is bound by the inhibitory protein IκBα (which contains six ankyrin repeats). During NF-κB activation, IκBα is phosphorylated by IκBα kinase (IKK), followed by ubiquitination and subsequent degradation151. To prevent NF-κB activation, orthopoxviruses express ankyrin-like proteins that compete with IκBα for phosphorylation by IKK84,85. Eight ankyrin-like genes (J3L, D1L, D7L, D9L, O1L, C1L, B5R, B17R, N4R and J1R) are encoded by the MPXV genome84 — J3L and J1R as well as D1L and N4R are duplicated ORFs in left and right inverted terminal repeats within the viral genome84.
Regulation of apoptosis
Another mechanism of orthopoxvirus immune evasion involves regulating apoptosis. The BCL-2-like proteins encoded by orthopoxviruses may interfere with the BCL-2-mediated regulation of the intrinsic apoptotic pathway. Numerous orthopoxvirus-encoded serine protease inhibitors (SPIs; serpins) have also been reported85,133,152,153, such as CrmA in cowpox virus (CPXV)153; its homologue SPI-2 (B13) in VACV is considered the virus’s most potent inhibitor of apoptosis154. CrmA interferes with granzyme B155, which is secreted by cytotoxic T cells to initiate cell death in the virus-infected target cells156. It also inhibits caspase 1 and caspase 8, thereby interfering with their respective pyroptotic or apoptotic pathways152. In MPXV, an SPI-2 orthologue is encoded by the B12R gene84.
TNFR orthologues are also commonly used by orthopoxviruses to interfere with host inflammation and apoptotic events85,86. Decoy viral TNFRs, which lack signalling domains, are secreted and compete for the binding of TNF157. Five orthopoxviral viral TNFRs — CrmB, CrmC, CrmD, CrmE and vCD30 — have been identified84,85,157. The MPXV genome encodes only CrmB, which is reported to bind to both TNF and TNFβ based on investigations performed with the CPXV CrmB158. Interestingly, CrmB from VARV is extremely potent and exhibits an affinity for TNF159 that is stronger than etanercept, a commercially available competitive inhibitor of TNF160.
Antagonism of immune mediators
Orthopoxviruses also evade host immune responses by secreting proteins that antagonize the functions of host IFNγ, CC and CXC chemokines, IL-1β and the complement system161–166. Interestingly, the West African MPXV clade does not express any complement-modulating proteins11,18, whereas the Central African strains encode the monkeypox inhibitor of complement enzyme (MOPICE) from the D14L gene11,167. Despite truncation in one of its short consensus repeat (SCR) domains, MOPICE inhibits complement activation by binding to C3 and C5 convertases11,168. However, deletion of MOPICE did not affect MPXV virulence in rhesus macaques infected with a Central African isolate, although it did dampen the adaptive immune response169.
Reduction of cellular activation
Orthopoxviruses also evade T cell-mediated and natural killer cell-mediated cytotoxicity. T cells identify virus-infected cells by detecting foreign peptides loaded on surface-expressed MHC class I. Meanwhile, natural killer cells continually survey cells via NKG2D for the absence of MHC class I, thereby ensuring that the MHC system is not compromised. MPXV overcomes this system first by secreting the orthopoxvirus MHC class I-like protein (OMCP) encoded by the N3R gene, which resembles the MHC class I molecule and binds to NKG2D. This suppresses the typical NKG2D-dependent natural killer cell lysis of infected cells that do not express MHC class I170. Evasion of natural killer cell surveillance allows the virus to reduce MHC class I expression, thus reducing T cell recognition171. In addition, CPXV also expresses proteins D10 and B8 that impair peptide loading and MHC class I trafficking within the endoplasmic reticulum172. In MPXV, the B10R gene encodes for an orthologue of the CPXV B8 protein84. Orthopoxviruses also directly modulate natural killer cells and T cells in a paracrine fashion. For instance, orthopoxviruses produce an IL-18-binding protein that further blocks the cytotoxic activities of natural killer cells173. MPXV also suppresses T cell-mediated immunity by triggering a state of T cell unresponsiveness via an MHC-independent mechanism65. Subversion of T cell responses may explain why orthopoxvirus-specific memory T cells in vaccinated NHPs failed to protect against lethal MPXV infection in the absence of neutralizing antibodies53.
Vaccines
Vaccines against smallpox are known to have cross-protective activity against monkeypox. Two vaccines are approved by the US Food and Drug Administration (FDA) for pre-exposure vaccination against orthopoxviruses including monkeypox: a second-generation live VACV vaccine, ACAM2000, and an attenuated third-generation vaccine based on modified vaccinia Ankara (MVA), JYNNEOS174,175. National stockpiles of second-generation vaccines such as ACAM2000 are most common176. However, these vaccines are associated with several rare side effects including myocarditis and pericarditis176, with higher risks for certain groups of individuals, such as those with eczema and those who are pregnant. Nevertheless, a study demonstrated the efficacy of ACAM2000 smallpox vaccination in eliciting VACV-specific T cell responses by reporting the presence of activated CD4+ and CD8+ T cell responses at 1, 3, 6 and 12 months post vaccination177. Following VACV stimulation, activated CD8+ T cells expressed much higher levels of the degranulation marker CD107, as well as IFNγ, TNF, IL-2 and CCL4 (ref.177), indicating the presence of robust memory T cell responses. The elevated CD8+ T cell responses were also observed in another study that compared the efficacy of the MVA vaccination with the first-generation Dryvax immunization178. In both vaccination groups, VACV-specific CD8+ T cells were observed to secrete IFNγ, TNF, IL-2 and CCL4 following stimulation178. Moreover, both ACAM2000 and Dryvax also triggered the production of VACV-neutralizing antibodies in the vaccinees177,179, despite apparent differences in the viral proteins being targeted179.
In unvaccinated individuals, post-exposure vaccination can be effective both for preventing disease and for reducing disease severity. Protection is strongest if vaccination is carried out immediately after exposure, and decreases with increasing time since exposure, with most studies agreeing that vaccination up to 3 days post exposure provides significant clinical benefit180. In animal studies, post-exposure vaccination against monkeypox varies in efficacy depending on the animal model used, the challenge dose and the timing of post-exposure vaccination181. Notably, vaccination with ACAM2000 at 1–3 days after a 50× median lethal dose MPXV challenge in prairie dogs resulted in survival for 50–62% of the animals, compared with only 25% survival in the unvaccinated group181. Human clinical studies are currently in progress to determine the efficacy of post-exposure vaccination against monkeypox182.
Third-generation attenuated vaccines such as JYNNEOS have a better safety profile compared with earlier vaccines183. However, because JYNNEOS is given in two doses 28 days apart, the second dose would likely be too late to help protect from disease in cases of post-exposure vaccination, and it is not known whether the first dose is sufficient for therapeutic efficacy. However, at 2 weeks post vaccination, neutralizing antibody titres from one dose of JYNNEOS were equivalent to those from ACAM2000, although they subsequently became inferior to those of the ACAM2000 group183. Thus, if viral neutralization correlates with protection, the efficacy of a single dose of JYNNEOS may be similar to ACAM2000 within the first critical weeks of post-exposure prophylaxis. In the same prairie dog study referenced above, post-exposure vaccination with JYNNEOS resulted in 38–88% survival181.
A critical aspect of vaccine development is understanding the mechanisms by which different vaccines elicit immune responses, as different formulations can induce either specific B cell-mediated or T cell-mediated immunity184. Likewise, the immunocompetency of vaccine recipients as well as the route of immunization will also affect the quality of the immune response184. Given the frequent mucosal route of infection, the specific induction of mucosal immunity may be crucial in the context of MPXV, as documented for other infectious pathogens that transmit via the mucosal route185. Currently, it is not well understood whether any of the available vaccines are able to induce mucosal immunity, and this remains a key future research need.
Another research need is to understand whether there is a risk of creating new virus strains when individuals infected with monkeypox are vaccinated. Co-infecting poxviruses can evolve by exchanging genetic information via homologous or non-homologous recombination186. It is currently unknown how frequently genes from live or attenuated poxvirus-based vaccines may recombine with monkeypox.
In addition to the VACV or MVA-based vaccines, newer genetically engineered VACV or other poxvirus strains such as NYVAC and ALVAC have also been experimented with as potential vaccine vectors for other diseases. However, they generally induce lower antibody titres187, and their effectiveness against monkeypox is unclear.
Therapeutics
Several therapeutics that were developed for smallpox are available for monkeypox, but their effectiveness for monkeypox is based on preclinical evidence with little supporting clinical data from humans. The antiviral drug tecovirimat does not affect the intracellular form of the virus (the intracellular mature virus), but targets the VP37 membrane protein of MPXV to prevent the formation of enveloped virions that are capable of cell egress, thus disrupting viral spread188. Tecovirimat was effective at reducing monkeypox severity in NHP models189,190, but its effectiveness is reduced if treatment is given more than 5 days post challenge191. This suggests a caveat if tecovirimat is given based on the onset of symptoms, which may appear much later following infection1,4. Nevertheless, a small study used tecovirimat in a single patient infected with monkeypox, who then showed a shorter duration of viral shedding and illness compared with six untreated patients28.
Another smallpox therapeutic is brincidofovir, which is approved by the FDA but not the European Medicines Agency (EMA). Brincidofovir inhibits orthopoxvirus DNA polymerase-mediated DNA synthesis. It has shown efficacy against monkeypox in prairie dog and mouse models192,193. In the same small study discussed above28, three patients were treated with brincidofovir, but all three ceased therapy owing to toxicity (elevated liver enzymes). Cidofovir28, the active drug form of brincidofovir, also shows anti-poxvirus activity in vitro and in animal studies194, but it is nephrotoxic195–197.
VIG showed promising activity in preventing smallpox in exposed individuals198 and has exhibited cross-neutralizing activity against MPXV in rhesus macaques53. However, neither VIG nor other mAbs or antibody cocktails have yet been studied against monkeypox in the clinic.
Concluding remarks
Immunotherapeutics and preventive strategies are important public health tools that complement stringent contact tracing in curbing the spread of monkeypox. Similarly, serology-based diagnostics are valuable surveillance tools for contact tracing and understanding exposure history. However, such serological diagnostic tools must be specific for MPXV, given the baseline of vaccine-induced poxvirus immunity199. Expansion of surveillance networks and identification of surveillance gaps are also critical for a successful ring-fencing strategy (see Box 3 for details). Notably, there is a major need in public health to better inform potentially exposed persons of the benefits and risks of vaccination.
Historically, the collection of clinical data on monkeypox has been hindered by the sparseness and unpredictability of cases in endemic countries, impeding accurate risk–benefit calculations in managing monkeypox. The current outbreaks provide an opportunity to evaluate current and novel treatments and vaccine options and to establish correlates of vaccine protection. Notably, the ring vaccination trial design can provide high statistical power with relatively few subjects owing to the high potential attack rate200. However, in generalizing such findings, caution must be taken to account for variance in the route of transmission.
Several key research questions remain to be answered. Studies of the human systemic and mucosal immune responses during MPXV infection are currently limited and will be required to better understand the mechanisms of immune defence against MPXV. Importantly, it is not currently known whether prior infection with VACV or MPXV, or smallpox vaccination, induces any form of mucosal immunity. It will be critical to characterize the mucosal immune responses given that MPXV and other poxviruses can be transmitted via respiratory aerosols1. Knowledge of the roles of IgA and tissue-resident memory T cells in MPXV infection would be particularly critical, enabling a deeper understanding of MPXV-related respiratory complications22. Likewise, the preputial mucosal immunity should also be characterized, as MPXV DNA has been identified in semen26.
Defining the immunological correlates of protection is also an important goal for the evaluation of newer vaccines, especially those targeted towards the vulnerable populations of pregnant women and children. Therefore, other than being unvaccinated, what other factors (for example, behavioural, geographical, nutritional, medical, immunological or genetic factors) are involved? It was recently reported that the quality of innate immune responses in young children determines the severity of respiratory viral infection201. Likewise, as reported for SARS-CoV-2 infections, children who are infected tend to have reduced B cell202 and T cell203 responses compared with adults. The characterization of adaptive immune responses in children infected with MPXV could clarify why children tend to exhibit a more severe disease and lower vaccine effectiveness1,4,7. It is also important to understand the risks of vaccination in vulnerable populations, especially young children and pregnant women1,4,30,32. Clinical studies are lacking in these populations for most of the available therapeutics and vaccines. Furthermore, some important vaccines and therapeutics (for example, ACAM2000 and brincidofovir) are not recommended or are even contraindicated for these populations due to increased potential risk of side effects204. Nevertheless, it was recommended by the UK Health Security Agency that vaccination should be given to men who are homosexual or bisexual who are at a higher risk of exposure to help control the current outbreak205.
Many other infectious diseases are endemic to Africa206, and co-infection with MPXV is possible. For instance, co-infection of alphaviral infections and malaria can significantly modulate host immunity and affect infection outcomes207–209. Given the current transmission among MSM in non-endemic countries, there is also a need to understand monkeypox disease and vaccination in the context of co-infection with other diseases that have a disproportionate burden in the community of MSM; this is especially true for HIV-1, which can severely impair adaptive immune responses210.
Risk factors for severe MPXV should also be identified. Pregnant women, young children and unvaccinated individuals are known to be especially susceptible1,4,30,32. However, other populations also need characterization, including older people, individuals on long-term medications and individuals with underlying metabolic diseases who may manifest the disease differently.
Long-term disease sequelae should be tracked in patients, including children born to mothers infected with MPXV. Experience with the Zika outbreak showed that children with in utero exposure can develop some developmental issues later in life211. This research focus should be given more urgency, given that available data suggest that only 20–25% of pregnant women infected with MPXV would successfully give birth30,32. Moreover, young children are apparently more susceptible to severe monkeypox4. Currently, data on fetal development following congenital MPXV infection are lacking. In addition, longitudinal monitoring of patients with MPXV would also allow the determination of whether infection with MPXV can lead to long-term effects, as observed after infection with SARS-CoV-2 during the current pandemic.
Box 3 Ring-fencing vaccination against monkeypox.
To halt the potential spread of monkeypox virus (MPXV) globally, ring vaccination has been implemented in several countries including the United Kingdom, the United States and Canada. This usually involves vaccinating people who may have been exposed to the virus through interactions with an infected person. Vaccination is performed using smallpox vaccines, which are thought to offer protection against MPXV. Some of the challenges facing a successful ring vaccination are discussed below.
Contact tracing: to identify all individuals who are potentially exposed, extensive contact tracing and robust testing needs to be carried out. For logistic reasons this may not be possible in every country. Furthermore, given the current characterization of non-endemic monkeypox as a disease that spreads primarily within the community of men who have sex with men (MSM), patients may be reluctant to come forward for diagnosis, especially in countries where homosexuality is stigmatized or criminalized248.
Efficiencies of second-generation and third-generation vaccines: past data showed that smallpox vaccination was 85% protective against MPXV60. However, this value was obtained from individuals vaccinated with the first-generation vaccine. Nevertheless, currently available second-generation and third-generation vaccines were also reported to be approximately 85% protective against MPXV in animals models249,250, but there are no data on their efficacy in humans exposed to MPXV.
Willingness to comply: not everyone identified will be willing to receive the vaccine. In a recent report, only ~14% of community contacts and ~69% of potentially exposed health-care workers in the United Kingdom were willing to be vaccinated40. Moreover, the stigmatization of potentially being associated with the community of MSM might further deter vaccination efforts.
Acknowledgements
The authors thank D. Ackerman of Insight Editing London for his valuable inputs on an early draft. This work was supported by core funds at the A*STAR Infectious Diseases Labs (ID Labs) through the Biomedical Medical Research Council (BMRC), A*STAR and the PREPARE (Programme for Research in Epidemic Preparedness and REsponse) Outbreak Research Strategic Funds (PREPARE-SF-2022-001).
Glossary
- Genetic accordions
Multistep events involving gene application and mutations that allow poxviruses to subvert host antiviral responses.
- Monocytosis
An elevated number of infection-fighting monocytes in the blood circulation.
- Cytokine storm
A sudden increase in levels of circulating cytokines leading to an over-activated immune response, which can be life-threatening.
- Ring vaccination trial design
A recently developed approach that recruits subjects linked to an infected case and allows for the simultaneous evaluation of vaccine efficacy and effectiveness during ongoing outbreaks.
Author contributions
All authors contributed equally to all aspects of the article.
Peer review
Peer review information
Nature Reviews Immunology thanks Jacqueline Williams who co-reviewed with Bertram Jacobs, Sathesh Panayampalli and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McCollum AM, Damon IK. Human monkeypox. Clin. Infect. Dis. 2014;58:260–267. doi: 10.1093/cid/cit703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho CT, Wenner HA. Monkeypox virus. Bacteriol. Rev. 1973;37:1–18. doi: 10.1128/br.37.1.1-18.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen J. Monkeypox outbreak questions intensify as cases soar. Science. 2022;376:902–903. doi: 10.1126/science.add1583. [DOI] [PubMed] [Google Scholar]
- 4.Jezek Z, Szczeniowski M, Paluku KM, Mutombo M. Human monkeypox: clinical features of 282 patients. J. Infect. Dis. 1987;156:293–298. doi: 10.1093/infdis/156.2.293. [DOI] [PubMed] [Google Scholar]
- 5.Kimball, S. WHO declares rapidly spreading monkeypox outbreak a global health emergency. CNBChttps://www.cnbc.com/2022/07/23/who-declares-spreading-monkeypox-outbreak-a-global-health-emergency.html (2022).
- 6.Reynolds MG, Damon IK. Outbreaks of human monkeypox after cessation of smallpox vaccination. Trends Microbiol. 2012;20:80–87. doi: 10.1016/j.tim.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Fine PEM, Jezek Z, Grab B, Dixon H. The transmission potential of monkeypox virus in human populations. Int. J. Epidemiol. 1988;17:643–650. doi: 10.1093/ije/17.3.643. [DOI] [PubMed] [Google Scholar]
- 8.Thornhill JP, et al. Monkeypox virus infection in humans across 16 countries — April–June 2022. N. Engl. J. Med. 2022 doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 9.Otu A, Ebenso B, Walley J, Barcelo JM, Ochu CL. Global human monkeypox outbreak: atypical presentation demanding urgent public health action. Lancet Microbe. 2022 doi: 10.1016/S2666-5247(22)00153-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Likos AM, et al. A tale of two clades: monkeypox viruses. J. Gen. Virol. 2005;86:2661–2672. doi: 10.1099/vir.0.81215-0. [DOI] [PubMed] [Google Scholar]
- 11.Chen N, et al. Virulence differences between monkeypox virus isolates from West Africa and the Congo Basin. Virology. 2005;340:46–63. doi: 10.1016/j.virol.2005.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bunge EM, et al. The changing epidemiology of human monkeypox — a potential threat? A systematic review. PLoS Negl. Trop. Dis. 2022;16:e0010141. doi: 10.1371/journal.pntd.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Minhaj FS, et al. Monkeypox outbreak — nine states, May 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71:764–769. doi: 10.15585/mmwr.mm7123e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Desingu PA, Nagarajan K. Genomic regions insertion and deletion in monkeypox virus causing multi-country outbreak — 2022. bioRxiv. 2022 doi: 10.1101/2022.06.28.497936. [DOI] [Google Scholar]
- 15.Kugelman JR, et al. Genomic variability of monkeypox virus among humans, Democratic Republic of the Congo. Emerg. Infect. Dis. 2014;20:232–239. doi: 10.3201/eid2002.130118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shchelkunov SN, et al. Human monkeypox and smallpox viruses: genomic comparison. FEBS Lett. 2001;509:66–70. doi: 10.1016/S0014-5793(01)03144-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shchelkunov SN, et al. Analysis of the monkeypox virus genome. Virology. 2002;297:172–194. doi: 10.1006/viro.2002.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weaver JR, Isaacs SN. Monkeypox virus and insights into its immunomodulatory proteins. Immunol. Rev. 2008;225:96–113. doi: 10.1111/j.1600-065X.2008.00691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McFadden G. Poxvirus tropism. Nat. Rev. Microbiol. 2005;3:201–213. doi: 10.1038/nrmicro1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsiao JC, Chung CS, Chang W. Vaccinia virus envelope D8L protein binds to cell surface chondroitin sulfate and mediates the adsorption of intracellular mature virions to cells. J. Virol. 1999;73:8750–8761. doi: 10.1128/JVI.73.10.8750-8761.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung CS, Hsiao JC, Chang YS, Chang W. A27L protein mediates vaccinia virus interaction with cell surface heparan sulfate. J. Virol. 1998;72:1577–1585. doi: 10.1128/JVI.72.2.1577-1585.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin CL, Chung CS, Heine HG, Chang W. Vaccinia virus envelope H3L protein binds to cell surface heparan sulfate and is important for intracellular mature virion morphogenesis and virus infection in vitro and in vivo. J. Virol. 2000;74:3353–3365. doi: 10.1128/JVI.74.7.3353-3365.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moss B. Membrane fusion during poxvirus entry. Semin. Cell Dev. Biol. 2016;60:89–96. doi: 10.1016/j.semcdb.2016.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perez Duque M, et al. Ongoing monkeypox virus outbreak, Portugal, 29 April to 23 May 2022. Eurosurveillance. 2022;27:2200424. doi: 10.2807/1560-7917.ES.2022.27.22.2200424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hammerschlag Y, et al. Monkeypox infection presenting as genital rash, Australia, May 2022. Eurosurveillance. 2022;27:2200411. doi: 10.2807/1560-7917.ES.2022.27.22.2200411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Antinori A, et al. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Eurosurveillance. 2022;27:2200421. doi: 10.2807/1560-7917.ES.2022.27.22.2200421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huhn GD, et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin. Infect. Dis. 2005;41:1742–1751. doi: 10.1086/498115. [DOI] [PubMed] [Google Scholar]
- 28.Adler H, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect. Dis. 2022 doi: 10.1016/S1473-3099(22)00228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Learned LA, et al. Extended interhuman transmission of monkeypox in a hospital community in the Republic of the Congo, 2003. Am. J. Trop. Med. Hyg. 2005;73:428–434. doi: 10.4269/ajtmh.2005.73.428. [DOI] [PubMed] [Google Scholar]
- 30.Pittman PR, et al. Clinical characterization of human monkeypox infections in the Democratic Republic of the Congo. medRxiv. 2022 doi: 10.1101/2022.05.26.22273379. [DOI] [Google Scholar]
- 31.Downie AW, Dumbell KR. Survival of variola virus in dried exudate and crusts from smallpox patients. Lancet. 1947;1:550–553. doi: 10.1016/S0140-6736(47)91671-1. [DOI] [PubMed] [Google Scholar]
- 32.Mbala PK, et al. Maternal and fetal outcomes among pregnant women with human monkeypox infection in the Democratic Republic of Congo. J. Infect. Dis. 2017;216:824–828. doi: 10.1093/infdis/jix260. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Clinical considerations for Monkeypox in children and adolescents. CDChttps://www.cdc.gov/poxvirus/monkeypox/clinicians/pediatric.html (2022).
- 34.Stanford MM, McFadden G, Karupiah G, Chaudhri G. Immunopathogenesis of poxvirus infections: forecasting the impending storm. Immunol. Cell Biol. 2007;85:93–102. doi: 10.1038/sj.icb.7100033. [DOI] [PubMed] [Google Scholar]
- 35.Rimoin AW, et al. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc. Natl Acad. Sci. USA. 2010;107:16262–16267. doi: 10.1073/pnas.1005769107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zaucha GM, Jahrling PB, Geisbert TW, Swearengen JR, Hensley L. The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis) Lab. Invest. 2001;81:1581–1600. doi: 10.1038/labinvest.3780373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Song H, et al. Monkeypox virus infection of rhesus macaques induces massive expansion of natural killer cells but suppresses natural killer cell functions. PLoS ONE. 2013;8:e77804. doi: 10.1371/journal.pone.0077804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dai P, et al. Modified vaccinia virus ankara triggers type I IFN production in murine conventional dendritic cells via a cGAS/STING-mediated cytosolic DNA-sensing pathway. PLoS Pathog. 2014;10:e1003989. doi: 10.1371/journal.ppat.1003989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Engelmayer J, et al. Vaccinia virus inhibits the maturation of human dendritic cells: a novel mechanism of immune evasion. J. Immunol. 1999;163:6762–6768. [PubMed] [Google Scholar]
- 40.Li P, et al. Disruption of MHC class II-restricted antigen presentation by vaccinia virus. J. Immunol. 2005;175:6481–6488. doi: 10.4049/jimmunol.175.10.6481. [DOI] [PubMed] [Google Scholar]
- 41.Humlová Z, Vokurka M, Esteban M, Mělková Z. Vaccinia virus induces apoptosis of infected macrophages. J. Gen. Virol. 2002;83:2821–2832. doi: 10.1099/0022-1317-83-11-2821. [DOI] [PubMed] [Google Scholar]
- 42.Beauchamp NM, Busick RY, Alexander-Miller MA. Functional divergence among CD103+ dendritic cell subpopulations following pulmonary poxvirus infection. J. Virol. 2010;84:10191–10199. doi: 10.1128/JVI.00892-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Humrich JY, et al. Vaccinia virus impairs directional migration and chemokine receptor switch of human dendritic cells. Eur. J. Immunol. 2007;37:954–965. doi: 10.1002/eji.200636230. [DOI] [PubMed] [Google Scholar]
- 44.Liu L, et al. Vaccinia virus induces strong immunoregulatory cytokine production in healthy human epidermal keratinocytes: a novel strategy for immune evasion. J. Virol. 2005;79:7363–7370. doi: 10.1128/JVI.79.12.7363-7370.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walzer T, Galibert L, De Smedt T. Poxvirus semaphorin A39R inhibits phagocytosis by dendritic cells and neutrophils. Eur. J. Immunol. 2005;35:391–398. doi: 10.1002/eji.200425669. [DOI] [PubMed] [Google Scholar]
- 46.Norbury CC, Malide D, Gibbs JS, Bennink JR, Yewdell JW. Visualizing priming of virus-specific CD8+ T cells by infected dendritic cells in vivo. Nat. Immunol. 2002;3:265–271. doi: 10.1038/ni762. [DOI] [PubMed] [Google Scholar]
- 47.Hickman HD, et al. Anatomically restricted synergistic antiviral activities of innate and adaptive immune cells in the skin. Cell Host Microbe. 2013;13:155–168. doi: 10.1016/j.chom.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chahroudi A, et al. Vaccinia virus tropism for primary hematolymphoid cells is determined by restricted expression of a unique virus receptor. J. Virol. 2005;79:10397–10407. doi: 10.1128/JVI.79.16.10397-10407.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chapman JL, Nichols DK, Martinez MJ, Raymond JW. Animal models of orthopoxvirus infection. Vet. Pathol. 2010;47:852–870. doi: 10.1177/0300985810378649. [DOI] [PubMed] [Google Scholar]
- 50.Moulton EA, Atkinson JP, Buller RML. Surviving mousepox infection requires the complement system. PLoS Pathog. 2008;4:e1000249. doi: 10.1371/journal.ppat.1000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Institute of Medicine (US) Committee on the Assessment of Future Scientific Needs for Live Variola Virus. Assessment of Future Scientific Needs for Live Variola Virus (National Academies Press (US), 1999). [PubMed]
- 52.Alakunle E, Moens U, Nchinda G, Okeke MI. Monkeypox virus in Nigeria: infection biology, epidemiology, and evolution. Viruses. 2020;12:1257. doi: 10.3390/v12111257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Edghill-Smith Y, et al. Smallpox vaccine-induced antibodies are necessary and sufficient for protection against monkeypox virus. Nat. Med. 2005;11:740–747. doi: 10.1038/nm1261. [DOI] [PubMed] [Google Scholar]
- 54.Deng L, et al. Vaccinia virus subverts a mitochondrial antiviral signaling protein-dependent innate immune response in keratinocytes through its double-stranded RNA binding protein, E3. J. Virol. 2008;82:10735–10746. doi: 10.1128/JVI.01305-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cann JA, Jahrling PB, Hensley LE, Wahl-Jensen V. Comparative pathology of smallpox and monkeypox in man and macaques. J. Comp. Pathol. 2013;148:6–21. doi: 10.1016/j.jcpa.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aggio JB, Krmeská V, Ferguson BJ, Wowk PF, Rothfuchs AG. Vaccinia virus infection inhibits skin dendritic cell migration to the draining lymph node. J. Immunol. 2021;206:776–784. doi: 10.4049/jimmunol.2000928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Reynoso GV, et al. Lymph node conduits transport virions for rapid T cell activation. Nat. Immunol. 2019;20:602–612. doi: 10.1038/s41590-019-0342-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Davido B, D’anglejan E, Jourdan J, Robinault A, Davido G. Monkeypox 2022 outbreak: cases with exclusive genital lesions. J. Travel. Med. 2022 doi: 10.1093/jtm/taac077. [DOI] [PubMed] [Google Scholar]
- 59.Forrester JV, Mölzer C, Kuffova L. Immune privilege furnishes a niche for latent infection. Front. Ophthalmol. 2022 doi: 10.3389/fopht.2022.869046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Prow NA, et al. A vaccinia-based single vector construct multi-pathogen vaccine protects against both Zika and chikungunya viruses. Nat. Commun. 2018;9:1230. doi: 10.1038/s41467-018-03662-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhao Y, Adams YF, Croft M. Preferential replication of vaccinia virus in the ovaries is independent of immune regulation through IL-10 and TGF-β. Viral Immunol. 2011;24:387–396. doi: 10.1089/vim.2011.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khoury G, et al. Human immunodeficiency virus persistence and T-cell activation in blood, rectal, and lymph node tissue in human immunodeficiency virus-infected individuals receiving suppressive antiretroviral therapy. J. Infect. Dis. 2017;215:911–919. doi: 10.1093/infdis/jix039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kelley CF, et al. The rectal mucosa and condomless receptive anal intercourse in HIV-negative MSM: implications for HIV transmission and prevention. Mucosal Immunol. 2017;10:996–1007. doi: 10.1038/mi.2016.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mikulak J, Di Vito C, Zaghi E, Mavilio D. Host immune responses in HIV-1 infection: the emerging pathogenic role of siglecs and their clinical correlates. Front. Immunol. 2017;8:314. doi: 10.3389/fimmu.2017.00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hammarlund E, et al. Monkeypox virus evades antiviral CD4+ and CD8+ T cell responses by suppressing cognate T cell activation. Proc. Natl Acad. Sci. USA. 2008;105:14567–14572. doi: 10.1073/pnas.0800589105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rubins KH, et al. The host response to smallpox: analysis of the gene expression program in peripheral blood cells in a nonhuman primate model. Proc. Natl Acad. Sci. USA. 2004;101:15190–15195. doi: 10.1073/pnas.0405759101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jahrling PB, et al. Exploring the potential of variola virus infection of cynomolgus macaques as a model for human smallpox. Proc. Natl Acad. Sci. USA. 2004;101:15196–15200. doi: 10.1073/pnas.0405954101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rubins KH, Hensley LE, Relman DA, Brown PO. Stunned silence: gene expression programs in human cells infected with monkeypox or vaccinia virus. PLoS ONE. 2011;6:e15615. doi: 10.1371/journal.pone.0015615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Song H, et al. Poxvirus antigen staining of immune cells as a biomarker to predict disease outcome in monkeypox and cowpox virus infection in non-human primates. PLoS ONE. 2013;8:e60533. doi: 10.1371/journal.pone.0060533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Johnson RF, et al. Comparative analysis of monkeypox virus infection of cynomolgus macaques by the intravenous or intrabronchial inoculation route. J. Virol. 2011;85:2112–2125. doi: 10.1128/JVI.01931-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Byrd D, et al. Primary human macrophages serve as vehicles for vaccinia virus replication and dissemination. J. Virol. 2014;88:6819–6831. doi: 10.1128/JVI.03726-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fischer MA, et al. CD11b+, Ly6G+ cells produce type I interferon and exhibit tissue protective properties following peripheral virus infection. PLoS Pathog. 2011;7:e1002374. doi: 10.1371/journal.ppat.1002374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nagata N, et al. Pathogenesis of fulminant monkeypox with bacterial sepsis after experimental infection with West African monkeypox virus in a cynomolgus monkey. Int. J. Clin. Exp. Pathol. 2014;7:4359–4370. [PMC free article] [PubMed] [Google Scholar]
- 74.Davies ML, et al. A systemic macrophage response is required to contain a peripheral poxvirus infection. PLoS Pathog. 2017;13:e1006435. doi: 10.1371/journal.ppat.1006435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Paust S, Senman B, von Andrian UH. Adaptive immune responses mediated by natural killer cells. Immunol. Rev. 2010;235:286–296. doi: 10.1111/j.0105-2896.2010.00906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Earl PL, Americo JL, Moss B. Natural killer cells expanded in vivo or ex vivo with IL-15 overcomes the inherent susceptibility of CAST mice to lethal infection with orthopoxviruses. PLoS Pathog. 2020;16:e1008505. doi: 10.1371/journal.ppat.1008505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jayaraman A, et al. IL-15 complexes induce NK- and T-cell responses independent of type I IFN signaling during rhinovirus infection. Mucosal Immunol. 2014;7:1151–1164. doi: 10.1038/mi.2014.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bukowski JF, Woda BA, Habu S, Okumura K, Welsh RM. Natural killer cell depletion enhances virus synthesis and virus-induced hepatitis in vivo. J. Immunol. 1983;131:1531–1538. [PubMed] [Google Scholar]
- 79.Fang M, Lanier LL, Sigal LJ. A role for NKG2D in NK cell-mediated resistance to poxvirus disease. PLoS Pathog. 2008;4:e30. doi: 10.1371/journal.ppat.0040030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fenner F. Adventures with poxviruses of vertebrates. FEMS Microbiol. Rev. 2000;24:123–133. doi: 10.1111/j.1574-6976.2000.tb00536.x. [DOI] [PubMed] [Google Scholar]
- 81.Fang M, et al. CD94 is essential for NK cell-mediated resistance to a lethal viral disease. Immunity. 2011;34:579–589. doi: 10.1016/j.immuni.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vance RE, Jamieson AM, Raulet DH. Recognition of the class Ib molecule Qa-1b by putative activating receptors CD94/NKG2C and CD94/NKG2E on mouse natural killer cells. J. Exp. Med. 1999;190:1801–1812. doi: 10.1084/jem.190.12.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Johnston SC, et al. In vitro inhibition of monkeypox virus production and spread by Interferon-β. Virol. J. 2012;9:5. doi: 10.1186/1743-422X-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shchelkunov SN. Orthopoxvirus genes that mediate disease virulence and host tropism. Adv. Virol. 2012;2012:524743. doi: 10.1155/2012/524743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Suraweera CD, Hinds MG, Kvansakul M. Poxviral strategies to overcome host cell apoptosis. Pathogens. 2020;10:6. doi: 10.3390/pathogens10010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mohamed MR, McFadden G. NF-κB inhibitors: strategies from poxviruses. Cell Cycle. 2009;8:3125–3132. doi: 10.4161/cc.8.19.9683. [DOI] [PubMed] [Google Scholar]
- 87.Shisler JL, Jin XL. The vaccinia virus K1L gene product inhibits host NF-κB activation by preventing IκBα degradation. J. Virol. 2004;78:3553–3560. doi: 10.1128/JVI.78.7.3553-3560.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dutta P, Nahrendorf M. Regulation and consequences of monocytosis. Immunol. Rev. 2014;262:167–178. doi: 10.1111/imr.12219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Johnston SC, et al. Cytokine modulation correlates with severity of monkeypox disease in humans. J. Clin. Virol. 2015;63:42–45. doi: 10.1016/j.jcv.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Howell MD, et al. Cytokine milieu of atopic dermatitis skin subverts the innate immune response to vaccinia virus. Immunity. 2006;24:341–348. doi: 10.1016/j.immuni.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 91.van Den Broek M, et al. IL-4 and IL-10 antagonize IL-12-mediated protection against acute vaccinia virus infection with a limited role of IFN-γ and nitric oxide synthetase 2. J. Immunol. 2000;164:371–378. doi: 10.4049/jimmunol.164.1.371. [DOI] [PubMed] [Google Scholar]
- 92.Thakur A, Mikkelsen H, Jungersen G. Intracellular pathogens: host immunity and microbial persistence strategies. J. Immunol. Res. 2019;2019:1356540. doi: 10.1155/2019/1356540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Srivastava RM, Marincola FM, Shanker A. Editorial: lymphocyte functional crosstalk and regulation. Front. Immunol. 2019;10:2916. doi: 10.3389/fimmu.2019.02916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Strassburg MA. The global eradication of smallpox. Am. J. Infect. Control. 1982;10:53–59. doi: 10.1016/0196-6553(82)90003-7. [DOI] [PubMed] [Google Scholar]
- 95.Cherry JD, et al. Clinical and serologic study of four smallpox vaccines comparing variations of dose and route of administration. Primary percutaneous vaccination. J. Infect. Dis. 1977;135:145–154. doi: 10.1093/infdis/135.1.145. [DOI] [PubMed] [Google Scholar]
- 96.Kempe CH, et al. The use of vaccinia hyperimmune γ-globulin in the prophylaxis of smallpox. Bull. World Health Organ. 1961;25:41–48. [PMC free article] [PubMed] [Google Scholar]
- 97.Jacobs BL, et al. Vaccinia virus vaccines: past, present and future. Antivir. Res. 2009;84:1–13. doi: 10.1016/j.antiviral.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Crotty S, et al. Cutting edge: long-term B cell memory in humans after smallpox vaccination. J. Immunol. 2003;171:4969–4973. doi: 10.4049/jimmunol.171.10.4969. [DOI] [PubMed] [Google Scholar]
- 99.Hammarlund E, et al. Duration of antiviral immunity after smallpox vaccination. Nat. Med. 2003;9:1131–1137. doi: 10.1038/nm917. [DOI] [PubMed] [Google Scholar]
- 100.Mack TM, Noble J, Jr., Thomas DB. A prospective study of serum antibody and protection against smallpox. Am. J. Trop. Med. Hyg. 1972;21:214–218. doi: 10.4269/ajtmh.1972.21.214. [DOI] [PubMed] [Google Scholar]
- 101.Keasey S, et al. Proteomic basis of the antibody response to monkeypox virus infection examined in cynomolgus macaques and a comparison to human smallpox vaccination. PLoS ONE. 2011;5:e15547. doi: 10.1371/journal.pone.0015547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Howard AR, Senkevich TG, Moss B. Vaccinia virus A26 and A27 proteins form a stable complex tethered to mature virions by association with the A17 transmembrane protein. J. Virol. 2008;82:12384–12391. doi: 10.1128/JVI.01524-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chiu WL, Lin CL, Yang MH, Tzou DL, Chang W. Vaccinia virus 4c (A26L) protein on intracellular mature virus binds to the extracellular cellular matrix laminin. J. Virol. 2007;81:2149–2157. doi: 10.1128/JVI.02302-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mucker EM, et al. Intranasal monkeypox marmoset model: prophylactic antibody treatment provides benefit against severe monkeypox virus disease. PLoS Negl. Trop. Dis. 2018;12:e0006581. doi: 10.1371/journal.pntd.0006581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wolffe EJ, Vijaya S, Moss B. A myristylated membrane protein encoded by the vaccinia virus L1R open reading frame is the target of potent neutralizing monoclonal antibodies. Virology. 1995;211:53–63. doi: 10.1006/viro.1995.1378. [DOI] [PubMed] [Google Scholar]
- 106.Chen Z, et al. Chimpanzee/human mAbs to vaccinia virus B5 protein neutralize vaccinia and smallpox viruses and protect mice against vaccinia virus. Proc. Natl Acad. Sci. USA. 2006;103:1882–1887. doi: 10.1073/pnas.0510598103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mucker EM, Thiele-Suess C, Baumhof P, Hooper JW. Lipid nanoparticle delivery of unmodified mRNAs encoding multiple monoclonal antibodies targeting poxviruses in rabbits. Mol. Ther. Nucleic Acids. 2022;28:847–858. doi: 10.1016/j.omtn.2022.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gilchuk I, et al. Cross-neutralizing and protective human antibody specificities to poxvirus infections. Cell. 2016;167:684–694.e9. doi: 10.1016/j.cell.2016.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Karem KL, et al. Monkeypox-induced immunity and failure of childhood smallpox vaccination to provide complete protection. Clin. Vaccin. Immunol. 2007;14:1318–1327. doi: 10.1128/CVI.00148-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.MacLeod MK, Clambey ET, Kappler JW, Marrack P. CD4 memory T cells: what are they and what can they do? Semin. Immunol. 2009;21:53–61. doi: 10.1016/j.smim.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jayani I, Susmiati E, Sulistyawati W. The correlation between CD4 count cell and opportunistic infection among HIV/AIDS patients. J. Phys. Conf. Ser. 2020;1569:032066. doi: 10.1088/1742-6596/1569/3/032066. [DOI] [Google Scholar]
- 112.Smith YE, et al. Smallpox vaccine does not protect macaques with AIDS from a lethal monkeypox virus challenge. J. Infect. Dis. 2005;191:372–381. doi: 10.1086/427265. [DOI] [PubMed] [Google Scholar]
- 113.Sklenovská N, Van Ranst M. Emergence of monkeypox as the most important orthopoxvirus infection in humans. Front. Public Health. 2018;6:241. doi: 10.3389/fpubh.2018.00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Dai R, Huang X, Yang Y. γδT cells are required for CD8+ T cell response to vaccinia viral infection. Front. Immunol. 2021;12:727046. doi: 10.3389/fimmu.2021.727046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Goulding J, et al. CD8 T cells use IFN-γ to protect against the lethal effects of a respiratory poxvirus infection. J. Immunol. 2014;192:5415. doi: 10.4049/jimmunol.1400256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Remakus S, et al. Memory CD8+ T cells can outsource IFN-γ production but not cytolytic killing for antiviral protection. Cell Host Microbe. 2013;13:546–557. doi: 10.1016/j.chom.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.McClain DJ, et al. Immunologic responses to vaccinia vaccines administered by different parenteral routes. J. Infect. Dis. 1997;175:756–763. doi: 10.1086/513968. [DOI] [PubMed] [Google Scholar]
- 118.Ennis FA, Cruz J, Demkowicz WE, Jr, Rothman AL, McClain DJ. Primary induction of human CD8+ cytotoxic T lymphocytes and interferon-γ-producing T cells after smallpox vaccination. J. Infect. Dis. 2002;185:1657–1659. doi: 10.1086/340517. [DOI] [PubMed] [Google Scholar]
- 119.Miller JD, et al. Human effector and memory CD8+ T cell responses to smallpox and yellow fever vaccines. Immunity. 2008;28:710–722. doi: 10.1016/j.immuni.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 120.Munier CML, et al. The primary immune response to vaccinia virus vaccination includes cells with a distinct cytotoxic effector CD4 T-cell phenotype. Vaccine. 2016;34:5251–5261. doi: 10.1016/j.vaccine.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 121.Littaua RA, Takeda A, Cruz J, Ennis FA. Vaccinia virus-specific human CD4+ cytotoxic T-lymphocyte clones. J. Virol. 1992;66:2274–2280. doi: 10.1128/jvi.66.4.2274-2280.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Fang M, et al. Perforin-dependent CD4+ T-cell cytotoxicity contributes to control a murine poxvirus infection. Proc. Natl Acad. Sci. USA. 2012;109:9983–9988. doi: 10.1073/pnas.1202143109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kennedy R, Poland GA. T-cell epitope discovery for variola and vaccinia viruses. Rev. Med. Virol. 2007;17:93–113. doi: 10.1002/rmv.527. [DOI] [PubMed] [Google Scholar]
- 124.Sette A, et al. Definition of epitopes and antigens recognized by vaccinia specific immune responses: their conservation in variola virus sequences, and use as a model system to study complex pathogens. Vaccine. 2009;27:G21–G26. doi: 10.1016/j.vaccine.2009.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Walsh SR, et al. Diverse recognition of conserved orthopoxvirus CD8+ T cell epitopes in vaccinated rhesus macaques. Vaccine. 2009;27:4990–5000. doi: 10.1016/j.vaccine.2009.05.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Calvo-Calle JM, Strug I, Nastke MD, Baker SP, Stern LJ. Human CD4+ T cell epitopes from vaccinia virus induced by vaccination or infection. PLoS Pathog. 2007;3:1511–1529. doi: 10.1371/journal.ppat.0030144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kennedy RB, Poland GA. The identification of HLA class II-restricted T cell epitopes to vaccinia virus membrane proteins. Virology. 2010;408:232–240. doi: 10.1016/j.virol.2010.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Molero-Abraham M, Glutting JP, Flower DR, Lafuente EM, Reche PA. EPIPOX: immunoinformatic characterization of the shared T-cell epitome between variola virus and related pathogenic orthopoxviruses. J. Immunol. Res. 2015;2015:738020. doi: 10.1155/2015/738020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ando J, Ngo MC, Ando M, Leen A, Rooney CM. Identification of protective T-cell antigens for smallpox vaccines. Cytotherapy. 2020;22:642–652. doi: 10.1016/j.jcyt.2020.04.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Arndt WD, et al. Evasion of the innate immune type I interferon system by monkeypox virus. J. Virol. 2015;89:10489–10499. doi: 10.1128/JVI.00304-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Denzler KL, et al. Attenuated NYCBH vaccinia virus deleted for the E3L gene confers partial protection against lethal monkeypox virus disease in cynomolgus macaques. Vaccine. 2011;29:9684–9690. doi: 10.1016/j.vaccine.2011.09.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Resch W, Hixson KK, Moore RJ, Lipton MS, Moss B. Protein composition of the vaccinia virus mature virion. Virology. 2007;358:233–247. doi: 10.1016/j.virol.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 133.Nichols DB, De Martini W, Cottrell J. Poxviruses utilize multiple strategies to inhibit apoptosis. Viruses. 2017;9:215. doi: 10.3390/v9080215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shchelkunov SN, Shchelkunova GA. Genes that control vaccinia virus immunogenicity. Acta Nat. 2020;12:33–41. doi: 10.32607/actanaturae.10935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Smith GL, et al. Vaccinia virus immune evasion: mechanisms, virulence and immunogenicity. J. Gen. Virol. 2013;94:2367–2392. doi: 10.1099/vir.0.055921-0. [DOI] [PubMed] [Google Scholar]
- 136.Yu H, Bruneau RC, Brennan G, Rothenburg S. Battle royale: innate recognition of poxviruses and viral immune evasion. Biomedicines. 2021;9:765. doi: 10.3390/biomedicines9070765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Franz KM, Kagan JC. Innate immune receptors as competitive determinants of cell fate. Mol. Cell. 2017;66:750–760. doi: 10.1016/j.molcel.2017.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Mogensen TH. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin. Microbiol. Rev. 2009;22:240–273. doi: 10.1128/CMR.00046-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Di Pilato M, Mejias-Perez E, Sorzano COS, Esteban M. Distinct roles of vaccinia virus NF-κB inhibitor proteins A52, B15, and K7 in the immune response. J. Virol. 2017;91:e00575-17. doi: 10.1128/JVI.00575-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Graham SC, et al. Vaccinia virus proteins A52 and B14 share a Bcl-2-like fold but have evolved to inhibit NF-κB rather than apoptosis. PLoS Pathog. 2008;4:e1000128. doi: 10.1371/journal.ppat.1000128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Maluquer de Motes C, et al. Inhibition of apoptosis and NF-κB activation by vaccinia protein N1 occur via distinct binding surfaces and make different contributions to virulence. PLoS Pathog. 2011;7:e1002430. doi: 10.1371/journal.ppat.1002430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chang HW, Watson JC, Jacobs BL. The E3L gene of vaccinia virus encodes an inhibitor of the interferon-induced, double-stranded RNA-dependent protein kinase. Proc. Natl Acad. Sci. USA. 1992;89:4825–4829. doi: 10.1073/pnas.89.11.4825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Silverman RH. Caps off to poxviruses. Cell Host Microbe. 2015;17:287–289. doi: 10.1016/j.chom.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 144.Zhang P, Jacobs BL, Samuel CE. Loss of protein kinase PKR expression in human HeLa cells complements the vaccinia virus E3L deletion mutant phenotype by restoration of viral protein synthesis. J. Virol. 2008;82:840–848. doi: 10.1128/JVI.01891-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Jefferies CA. Regulating IRFs in IFN driven disease. Front. Immunol. 2019;10:325. doi: 10.3389/fimmu.2019.00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Colamonici OR, Domanski P, Sweitzer SM, Larner A, Buller RM. Vaccinia virus B18R gene encodes a type I interferon-binding protein that blocks interferon α transmembrane signaling. J. Biol. Chem. 1995;270:15974–15978. doi: 10.1074/jbc.270.27.15974. [DOI] [PubMed] [Google Scholar]
- 147.Xu RH, et al. The orthopoxvirus type I IFN binding protein is essential for virulence and an effective target for vaccination. J. Exp. Med. 2008;205:981–992. doi: 10.1084/jem.20071854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Fernandez de Marco Mdel M, Alejo A, Hudson P, Damon IK, Alcami A. The highly virulent variola and monkeypox viruses express secreted inhibitors of type I interferon. FASEB J. 2010;24:1479–1488. doi: 10.1096/fj.09-144733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yoshida M, et al. Local and systemic responses to SARS-CoV-2 infection in children and adults. Nature. 2022;602:321–327. doi: 10.1038/s41586-021-04345-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hijano DR, et al. Role of type I interferon (IFN) in the respiratory syncytial virus (RSV) immune response and disease severity. Front. Immunol. 2019;10:566. doi: 10.3389/fimmu.2019.00566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Oeckinghaus A, Ghosh S. The NF-κB family of transcription factors and its regulation. Cold Spring Harb. Perspect. Biol. 2009;1:a000034. doi: 10.1101/cshperspect.a000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bloomer DT, et al. CrmA orthologs from diverse poxviruses potently inhibit caspases-1 and -8, yet cleavage site mutagenesis frequently produces caspase-1-specific variants. Biochem. J. 2019;476:1335–1357. doi: 10.1042/BCJ20190202. [DOI] [PubMed] [Google Scholar]
- 153.Komiyama T, et al. Inhibition of interleukin-1β converting enzyme by the cowpox virus serpin CrmA. An example of cross-class inhibition. J. Biol. Chem. 1994;269:19331–19337. doi: 10.1016/S0021-9258(17)32171-3. [DOI] [PubMed] [Google Scholar]
- 154.Veyer DL, et al. Analysis of the anti-apoptotic activity of four vaccinia virus proteins demonstrates that B13 is the most potent inhibitor in isolation and during viral infection. J. Gen. Virol. 2014;95:2757–2768. doi: 10.1099/vir.0.068833-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Quan LT, Caputo A, Bleackley RC, Pickup DJ, Salvesen GS. Granzyme B is inhibited by the cowpox virus serpin cytokine response modifier A. J. Biol. Chem. 1995;270:10377–10379. doi: 10.1074/jbc.270.18.10377. [DOI] [PubMed] [Google Scholar]
- 156.Devadas S, et al. Granzyme B is critical for T cell receptor-induced cell death of type 2 helper T cells. Immunity. 2006;25:237–247. doi: 10.1016/j.immuni.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 157.Alvarez-de Miranda FJ, Alonso-Sanchez I, Alcami A, Hernaez B. TNF decoy receptors encoded by poxviruses. Pathogens. 2021;10:1065. doi: 10.3390/pathogens10081065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hu FQ, Smith CA, Pickup DJ. Cowpox virus contains two copies of an early gene encoding a soluble secreted form of the type II TNF receptor. Virology. 1994;204:343–356. doi: 10.1006/viro.1994.1539. [DOI] [PubMed] [Google Scholar]
- 159.Pontejo SM, Alejo A, Alcami A. Comparative biochemical and functional analysis of viral and human secreted tumor necrosis factor (TNF) decoy receptors. J. Biol. Chem. 2015;290:15973–15984. doi: 10.1074/jbc.M115.650119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Marotte H, Cimaz R. Etanercept–TNF receptor and IgG1 Fc fusion protein: is it different from other TNF blockers? Expert. Opin. Biol. Ther. 2014;14:569–572. doi: 10.1517/14712598.2014.896334. [DOI] [PubMed] [Google Scholar]
- 161.Bahar MW, et al. Structure and function of A41, a vaccinia virus chemokine binding protein. PLoS Pathog. 2008;4:e5. doi: 10.1371/journal.ppat.0040005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kotwal GJ, Moss B. Vaccinia virus encodes a secretory polypeptide structurally related to complement control proteins. Nature. 1988;335:176–178. doi: 10.1038/335176a0. [DOI] [PubMed] [Google Scholar]
- 163.Miller CG, Shchelkunov SN, Kotwal GJ. The cowpox virus-encoded homolog of the vaccinia virus complement control protein is an inflammation modulatory protein. Virology. 1997;229:126–133. doi: 10.1006/viro.1996.8396. [DOI] [PubMed] [Google Scholar]
- 164.Ruiz-Arguello MB, et al. An ectromelia virus protein that interacts with chemokines through their glycosaminoglycan binding domain. J. Virol. 2008;82:917–926. doi: 10.1128/JVI.02111-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Seregin SV, Babkina IN, Nesterov AE, Sinyakov AN, Shchelkunov SN. Comparative studies of γ-interferon receptor-like proteins of variola major and variola minor viruses. FEBS Lett. 1996;382:79–83. doi: 10.1016/0014-5793(96)00069-5. [DOI] [PubMed] [Google Scholar]
- 166.Upton C, Mossman K, McFadden G. Encoding of a homolog of the IFN-γ receptor by myxoma virus. Science. 1992;258:1369–1372. doi: 10.1126/science.1455233. [DOI] [PubMed] [Google Scholar]
- 167.Uvarova EA, Shchelkunov SN. Species-specific differences in the structure of orthopoxvirus complement-binding protein. Virus Res. 2001;81:39–45. doi: 10.1016/S0168-1702(01)00332-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Liszewski MK, et al. Structure and regulatory profile of the monkeypox inhibitor of complement: comparison to homologs in vaccinia and variola and evidence for dimer formation. J. Immunol. 2006;176:3725–3734. doi: 10.4049/jimmunol.176.6.3725. [DOI] [PubMed] [Google Scholar]
- 169.Estep RD, et al. Deletion of the monkeypox virus inhibitor of complement enzymes locus impacts the adaptive immune response to monkeypox virus in a nonhuman primate model of infection. J. Virol. 2011;85:9527–9542. doi: 10.1128/JVI.00199-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Campbell JA, Trossman DS, Yokoyama WM, Carayannopoulos LN. Zoonotic orthopoxviruses encode a high-affinity antagonist of NKG2D. J. Exp. Med. 2007;204:1311–1317. doi: 10.1084/jem.20062026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Dasgupta A, Hammarlund E, Slifka MK, Fruh K. Cowpox virus evades CTL recognition and inhibits the intracellular transport of MHC class I molecules. J. Immunol. 2007;178:1654–1661. doi: 10.4049/jimmunol.178.3.1654. [DOI] [PubMed] [Google Scholar]
- 172.Byun M, et al. Two mechanistically distinct immune evasion proteins of cowpox virus combine to avoid antiviral CD8 T cells. Cell Host Microbe. 2009;6:422–432. doi: 10.1016/j.chom.2009.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Born TL, et al. A poxvirus protein that binds to and inactivates IL-18, and inhibits NK cell response. J. Immunol. 2000;164:3246–3254. doi: 10.4049/jimmunol.164.6.3246. [DOI] [PubMed] [Google Scholar]
- 174.Petersen BW, Harms TJ, Reynolds MG, Harrison LH. Use of vaccinia virus smallpox vaccine in laboratory and health care personnel at risk for occupational exposure to orthopoxviruses — recommendations of the Advisory Committee on Immunization Practices (ACIP), 2015. MMWR Morb. Mortal. Wkly. Rep. 2016;65:257–262. doi: 10.15585/mmwr.mm6510a2. [DOI] [PubMed] [Google Scholar]
- 175.Rao AK, et al. Use of JYNNEOS (smallpox and monkeypox vaccine, live, nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses: recommendations of the Advisory Committee on Immunization Practices — United States, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71:734–742. doi: 10.15585/mmwr.mm7122e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Nalca A, Zumbrun EE. ACAM2000: the new smallpox vaccine for United States strategic national stockpile. Drug Des. Devel. Ther. 2010;4:71–79. doi: 10.2147/DDDT.S3687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sukhumvittaya S, Ampol S, Pattanapanyasat K, Kantakamalakul W. Polyfunctional T cell and neutralizing antibody responses to ACAM2000TM smallpox vaccine immunization in primary-vaccinated individuals. Adv. Microbiol. 2016;6:169–177. doi: 10.4236/aim.2016.63017. [DOI] [Google Scholar]
- 178.Precopio ML, et al. Immunization with vaccinia virus induces polyfunctional and phenotypically distinctive CD8+ T cell responses. J. Exp. Med. 2007;204:1405–1416. doi: 10.1084/jem.20062363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Pugh C, et al. Human antibody responses to the polyclonal Dryvax vaccine for smallpox prevention can be distinguished from responses to the monoclonal replacement vaccine ACAM2000. Clin. Vaccin. Immunol. 2014;21:877–885. doi: 10.1128/CVI.00035-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Keckler MS, Reynolds MG, Damon IK, Karem KL. The effects of post-exposure smallpox vaccination on clinical disease presentation: addressing the data gaps between historical epidemiology and modern surrogate model data. Vaccine. 2013;31:5192–5201. doi: 10.1016/j.vaccine.2013.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Keckler MS, et al. IMVAMUNE® and ACAM2000® provide different protection against disease when administered postexposure in an intranasal monkeypox challenge prairie dog model. Vaccines. 2020;8:396. doi: 10.3390/vaccines8030396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Luong Nguyen LB, et al. A prospective national cohort evaluating ring MVA vaccination as post-exposure prophylaxis for monkeypox. Nat. Med. 2022 doi: 10.1038/d41591-022-00077-1. [DOI] [PubMed] [Google Scholar]
- 183.Yang, S. & Yonts, A. BLA clinical review memorandum. FDAhttps://www.fda.gov/media/131870/download (2019).
- 184.Pollard AJ, Bijker EM. A guide to vaccinology: from basic principles to new developments. Nat. Rev. Immunol. 2021;21:83–100. doi: 10.1038/s41577-020-00479-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Lavelle EC, Ward RW. Mucosal vaccines — fortifying the frontiers. Nat. Rev. Immunol. 2022;22:236–250. doi: 10.1038/s41577-021-00583-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Qin L, Evans DH. Genome scale patterns of recombination between coinfecting vaccinia viruses. J. Virol. 2014;88:5277–5286. doi: 10.1128/JVI.00022-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Midgley CM, Putz MM, Weber JN, Smith GL. Vaccinia virus strain NYVAC induces substantially lower and qualitatively different human antibody responses compared with strains Lister and Dryvax. J. Gen. Virol. 2008;89:2992–2997. doi: 10.1099/vir.0.2008/004440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Russo AT, et al. An overview of tecovirimat for smallpox treatment and expanded anti-orthopoxvirus applications. Expert. Rev. Anti Infect. Ther. 2021;19:331–344. doi: 10.1080/14787210.2020.1819791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Berhanu A, et al. Treatment with the smallpox antiviral tecovirimat (ST-246) alone or in combination with ACAM2000 vaccination is effective as a postsymptomatic therapy for monkeypox virus infection. Antimicrob. Agents Chemother. 2015;59:4296–4300. doi: 10.1128/AAC.00208-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Huggins J, et al. Nonhuman primates are protected from smallpox virus or monkeypox virus challenges by the antiviral drug ST-246. Antimicrob. Agents Chemother. 2009;53:2620–2625. doi: 10.1128/AAC.00021-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Russo AT, et al. Effects of treatment delay on efficacy of tecovirimat following lethal aerosol monkeypox virus challenge in cynomolgus macaques. J. Infect. Dis. 2018;218:1490–1499. doi: 10.1093/infdis/jiy326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Hutson CL, et al. Pharmacokinetics and efficacy of a potential smallpox therapeutic, brincidofovir, in a lethal monkeypox virus animal model. mSphere. 2021;6:e00927-20. doi: 10.1128/mSphere.00927-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Stabenow J, et al. A mouse model of lethal infection for evaluating prophylactics and therapeutics against monkeypox virus. J. Virol. 2010;84:3909–3920. doi: 10.1128/JVI.02012-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Andrei G, Snoeck R. Cidofovir activity against poxvirus infections. Viruses. 2010;2:2803–2830. doi: 10.3390/v2122803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lalezari JP, et al. (S)-1-[3-hydroxy-2-(phosphonylmethoxy)propyl]cytosine (cidofovir): results of a phase I/II study of a novel antiviral nucleotide analogue. J. Infect. Dis. 1995;171:788–796. doi: 10.1093/infdis/171.4.788. [DOI] [PubMed] [Google Scholar]
- 196.Ortiz A, et al. Tubular cell apoptosis and cidofovir-induced acute renal failure. Antivir. Ther. 2005;10:185–190. doi: 10.1177/135965350501000110. [DOI] [PubMed] [Google Scholar]
- 197.Wachsman M, et al. Pharmacokinetics, safety and bioavailability of HPMPC (cidofovir) in human immunodeficiency virus-infected subjects. Antivir. Res. 1996;29:153–161. doi: 10.1016/0166-3542(95)00829-2. [DOI] [PubMed] [Google Scholar]
- 198.Hopkins RJ, Lane JM. Clinical efficacy of intramuscular vaccinia immune globulin: a literature review. Clin. Infect. Dis. 2004;39:819–826. doi: 10.1086/422999. [DOI] [PubMed] [Google Scholar]
- 199.Dubois ME, Hammarlund E, Slifka MK. Optimization of peptide-based ELISA for serological diagnostics: a retrospective study of human monkeypox infection. Vector Borne Zoonotic Dis. 2012;12:400–409. doi: 10.1089/vbz.2011.0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Ebola ça Suffit Ring Vaccination Trial Consortium. The ring vaccination trial: a novel cluster randomised controlled trial design to evaluate vaccine efficacy and effectiveness during outbreaks, with special reference to Ebola. BMJ. 2015;351:h3740. doi: 10.1136/bmj.h3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Heinonen S, et al. Immune profiles provide insights into respiratory syncytial virus disease severity in young children. Sci. Transl. Med. 2020;12:eaaw0268. doi: 10.1126/scitranslmed.aaw0268. [DOI] [PubMed] [Google Scholar]
- 202.Toh ZQ, et al. Comparison of seroconversion in children and adults with mild COVID-19. JAMA Netw. Open. 2022;5:e221313. doi: 10.1001/jamanetworkopen.2022.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Cohen CA, et al. SARS-CoV-2 specific T cell responses are lower in children and increase with age and time after infection. Nat. Commun. 2021;12:4678. doi: 10.1038/s41467-021-24938-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Ryan MA, Seward JF, Smallpox Vaccine in Pregnancy Registry Team. Pregnancy, birth, and infant health outcomes from the national smallpox vaccine in pregnancy registry, 2003–2006. Clin. Infect. Dis. 2008;46:S221–S226. doi: 10.1086/524744. [DOI] [PubMed] [Google Scholar]
- 205.UK Health Security Agency. Monkeypox outbreak: vaccination strategy. gov.ukhttps://www.gov.uk/guidance/monkeypox-outbreak-vaccination-strategy (2022).
- 206.Nkengasong JN, Tessema SK. Africa needs a new public health order to tackle infectious disease threats. Cell. 2020;183:296–300. doi: 10.1016/j.cell.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Teo TH, et al. Co-infection with chikungunya virus alters trafficking of pathogenic CD8+ T cells into the brain and prevents Plasmodium-induced neuropathology. EMBO Mol. Med. 2018;10:121–138. doi: 10.15252/emmm.201707885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Teo TH, et al. Plasmodium co-infection protects against chikungunya virus-induced pathologies. Nat. Commun. 2018;9:3905. doi: 10.1038/s41467-018-06227-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Torres-Ruesta A, et al. Malaria abrogates O’nyong-nyong virus pathologies by restricting virus infection in nonimmune cells. Life Sci. Alliance. 2022;5:e202101272. doi: 10.26508/lsa.202101272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Yohannes, E. & Chance, M. R. in Encyclopedia of Systems Biology (eds Dubitzky, W., Wolkenhauer, O., Cho, K. H. & Yokota, H.) 2078–2084 (Springer, 2013).
- 211.Mulkey SB, et al. Neurodevelopmental abnormalities in children with in utero Zika virus exposure without congenital Zika syndrome. JAMA Pediatr. 2020;174:269–276. doi: 10.1001/jamapediatrics.2019.5204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Heymann DL, Szczeniowski M, Esteves K. Re-emergence of monkeypox in Africa: a review of the past six years. Br. Med. Bull. 1998;54:693–702. doi: 10.1093/oxfordjournals.bmb.a011720. [DOI] [PubMed] [Google Scholar]
- 213.Breman JG, et al. Human monkeypox, 1970–79. Bull. World Health Organ. 1980;58:165–182. [PMC free article] [PubMed] [Google Scholar]
- 214.Breman JG, Nakano JH, Coffi E, Godfrey H, Gautun JC. Human poxvirus disease after smallpox eradication. Am. J. Trop. Med. Hyg. 1977;26:273–281. doi: 10.4269/ajtmh.1977.26.273. [DOI] [PubMed] [Google Scholar]
- 215.Foster SO, et al. Human monkeypox. Bull. World Health Organ. 1972;46:569–576. [PMC free article] [PubMed] [Google Scholar]
- 216.Centers for Disease Control and Prevention. Human monkeypox — Kasai Oriental, Democratic Republic of Congo, February 1996–October 1997. MMWR Morb. Mortal. Wkly. Rep. 1997;46:1168–1171. [PubMed] [Google Scholar]
- 217.Jezek Z, et al. Four generations of probable person-to-person transmission of human monkeypox. Am. J. Epidemiol. 1986;123:1004–1012. doi: 10.1093/oxfordjournals.aje.a114328. [DOI] [PubMed] [Google Scholar]
- 218.Jezek Z, Grab B, Szczeniowski M, Paluku KM, Mutombo M. Clinico-epidemiological features of monkeypox patients with an animal or human source of infection. Bull. World Health Organ. 1988;66:459–464. [PMC free article] [PubMed] [Google Scholar]
- 219.Khodakevich L, et al. Monkey pox virus infection in humans in the Central African Republic [French] Bull. Soc. Pathol. Exot. Filiales. 1985;78:311–320. [PubMed] [Google Scholar]
- 220.Merouze F, Lesoin JJ. Monkeypox: second human case observed in Ivory Coast (rural health sector of Daloa) [French] Med. Trop. 1983;43:145–147. [PubMed] [Google Scholar]
- 221.Meyer A, et al. First appearance of monkey pox in human beings in Gabon [French] Med. Trop. 1991;51:53–57. [PubMed] [Google Scholar]
- 222.Tchokoteu PF, et al. Variola or a severe case of varicella? A case of human variola due to monkeypox virus in a child from the Cameroon [French] Ann. Soc. Belg. Med. Trop. 1991;71:123–128. [PubMed] [Google Scholar]
- 223.Doshi RH, et al. Epidemiologic and ecologic investigations of monkeypox, Likouala department, Republic of the Congo, 2017. Emerg. Infect. Dis. 2019;25:281–289. doi: 10.3201/eid2502.181222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Reynolds MG, et al. Detection of human monkeypox in the Republic of the Congo following intensive community education. Am. J. Trop. Med. Hyg. 2013;88:982–985. doi: 10.4269/ajtmh.12-0758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Formenty P, et al. Human monkeypox outbreak caused by novel virus belonging to Congo Basin clade, Sudan, 2005. Emerg. Infect. Dis. 2010;16:1539–1545. doi: 10.3201/eid1610.100713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Reynolds MG, et al. Human monkeypox in Sierra Leone after 44-year absence of reported cases. Emerg. Infect. Dis. 2019;25:1023–1025. doi: 10.3201/eid2505.180832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Berthet N, et al. Maculopapular lesions in the Central African Republic. Lancet. 2011;378:1354. doi: 10.1016/S0140-6736(11)61142-2. [DOI] [PubMed] [Google Scholar]
- 228.Nakoune E, et al. A nosocomial outbreak of human monkeypox in the Central African Republic. Open Forum Infect. Dis. 2017;4:ofx168. doi: 10.1093/ofid/ofx168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Yinka-Ogunleye A, et al. Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report. Lancet Infect. Dis. 2019;19:872–879. doi: 10.1016/S1473-3099(19)30294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Reynolds MG, et al. Spectrum of infection and risk factors for human monkeypox, United States, 2003. Emerg. Infect. Dis. 2007;13:1332–1339. doi: 10.3201/eid1309.070175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Erez N, et al. Diagnosis of imported monkeypox, Israel, 2018. Emerg. Infect. Dis. 2019;25:980–983. doi: 10.3201/eid2505.190076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Vaughan A, et al. Two cases of monkeypox imported to the United Kingdom, September 2018. Eurosurveillance. 2018;23:1800509. doi: 10.2807/1560-7917.ES.2018.23.38.1800509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Vaughan A, et al. Human-to-human transmission of monkeypox virus, United Kingdom, October 2018. Emerg. Infect. Dis. 2020;26:782–785. doi: 10.3201/eid2604.191164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Hobson G, et al. Family cluster of three cases of monkeypox imported from Nigeria to the United Kingdom, May 2021. Eurosurveillance. 2021;26:2100745. doi: 10.2807/1560-7917.ES.2021.26.32.2100745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Yong SEF, et al. Imported monkeypox, Singapore. Emerg. Infect. Dis. 2020;26:1826–1830. doi: 10.3201/eid2608.191387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Costello V, et al. Imported monkeypox from international traveler, Maryland, USA, 2021. Emerg. Infect. Dis. 2022;28:1002–1005. doi: 10.3201/eid2805.220292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Rao AK, et al. Monkeypox in a traveler returning from Nigeria — Dallas, Texas, July 2021. MMWR Morb. Mortal. Wkly. Rep. 2022;71:509–516. doi: 10.15585/mmwr.mm7114a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Zumla A, et al. Monkeypox outbreaks outside endemic regions: scientific and social priorities. Lancet Infect. Dis. 2022 doi: 10.1016/S1473-3099(22)00354-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Nigeria Centre for Disease Control. Update on monkeypox (MPX) in Nigeria. NCDChttps://ncdc.gov.ng/themes/common/files/sitreps/4f9bc59b967d1f4b19d61358595d3546.pdf (2022).
- 240.Kraemer MUG, et al. Tracking the 2022 monkeypox outbreak with epidemiological data in real-time. Lancet Infect. Dis. 2022 doi: 10.1016/S1473-3099(22)00359-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Channel News Asia. Singapore confirms imported case of monkeypox after flight attendant develops fever and rashes. CNAhttps://www.channelnewsasia.com/singapore/monkeypox-singapore-imported-case-flight-attendant-fever-rashes-moh-2760996 (2022).
- 242.Isidro J, et al. Phylogenomic characterization and signs of microevolution in the 2022 multi-country outbreak of monkeypox virus. Nat. Med. 2022 doi: 10.1038/s41591-022-01907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Luna N, et al. Phylogenomic analysis of the monkeypox virus (MPXV) 2022 outbreak: emergence of a novel viral lineage. Travel. Med. Infect. Dis. 2022 doi: 10.1016/j.tmaid.2022.102402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Gigante CM, et al. Multiple lineages of monkeypox virus detected in the United States, 2021–2022. bioRxiv. 2022 doi: 10.1101/2022.06.10.495526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Hammarlund E, et al. Multiple diagnostic techniques identify previously vaccinated individuals with protective immunity against monkeypox. Nat. Med. 2005;11:1005–1011. doi: 10.1038/nm1273. [DOI] [PubMed] [Google Scholar]
- 246.Sanjuan R, Domingo-Calap P. Mechanisms of viral mutation. Cell Mol. Life Sci. 2016;73:4433–4448. doi: 10.1007/s00018-016-2299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Elde NC, et al. Poxviruses deploy genomic accordions to adapt rapidly against host antiviral defenses. Cell. 2012;150:831–841. doi: 10.1016/j.cell.2012.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Daskalakis D, McClung RP, Mena L, Mermin J. Monkeypox: avoiding the mistakes of past infectious disease epidemics. Ann. Intern. Med. 2022 doi: 10.7326/M22-1748. [DOI] [PubMed] [Google Scholar]
- 249.Centers for Disease Control and Prevention. Monkeypox and smallpox vaccine guidance. CDChttps://www.cdc.gov/poxvirus/monkeypox/clinicians/smallpox-vaccine.html (2022).
- 250.Kimball, S. U.S. has more than 36,000 Jynneos monkeypox vaccine doses immediately available in national stockpile. CNBChttps://www.cnbc.com/2022/06/06/us-has-36000-doses-of-jynneos-monkeypox-vaccine-immediately-available-in-national-stockpile.html (2022).